Abstract
Purpose:
To examine the association of race/ethnicity with urinary incontinence subtypes and overactive bladder and associated bother in older men.
Methods:
This cross-sectional analysis utilized data from Multi-Ethnic Study of Atherosclerosis, an observational cohort of four racial/ethnic groups. At the sixth follow-up exam (age 60 to 98 years, 2015–16), urinary symptoms were ascertained with the International Consultation on Incontinence Questionnaire. Prevalence ratios (PR) of urinary incontinence subtypes and overactive bladder without incontinence by race/ethnicity were calculated while adjusting for demographics, comorbidities and medications. Degree of bother was based on scale of 0 (none) to 10 (most) with bother presence defined as a score ≥3.
Results:
Among 1536 men, 94% completed the questionnaire. Among completers, race/ethnicity was 40.7% Non-Hispanic White, 14.3% Chinese, 23.0% Non-Hispanic Black and 22.1% Hispanic. Urinary incontinence was reported by 11.1%, and urgency urinary incontinence accounted for 78.0% of all urinary incontinence. Highest prevalence of urgency urinary incontinence was noted among Non-Hispanic Black men (13.0%) followed by Hispanic (11.3%), Non-Hispanic White (6.8%) and Chinese (2.9%) men. NH Black men showed higher prevalence of any urinary incontinence (PR 1.62; 95% CI 1.06, 2.47) and urgency urinary incontinence (1.63; 1.01, 2.61) compared to NH White men after adjustments for covariates. No significant association was noted with other urinary incontinence subtypes by race/ethnicity after adjustment for covariates. Over 70% of urinary incontinence was associated with bother for all racial/ethnic groups.
Conclusion:
Urinary incontinence prevalence differs by race/ethnicity but most urinary incontinence is associated with bother regardless of race/ethnicity.
Keywords: Incontinence, race/ethnicity, overactive bladder, urgency, bother, health disparities, lower urinary tract symptoms
Introduction
Urinary incontinence (UI), affects over two million men in the U.S. age 50 years and older1 with an annual economic impact exceeding 23 billion dollars annually.2,3 Because risk of UI increases with advancing age,4 the prevalence of UI and its economic and social impact will only increase as the population ages over the next decade.5 UI is associated with embarrassment and self-blame,6 psychological distress,7 and reduced quality of life.8 Although UI is less frequent among men compared to women,1 men with UI are more likely to experience social isolation9 and require assistance with activities of daily living10 and less likely to seek treatment for their urinary symptoms8 compared to women with UI.
Urinary urgency with or without UI is called overactive bladder (OAB) and is often accompanied by urinary frequency and/or nocturia.11 The two main subtypes of UI include stress UI (SUI) and OAB with UI, often called urgency urinary incontinence (UUI). Presence of both SUI and UUI defines mixed UI (MUI).11 The reported frequency of UI subtypes among men varies widely across studies due to differences in UI ascertainment and populations studied.12–15 While racial differences in UI subtypes among women has been consistently demonstrated, two studies have shown no racial differences in UI among men.14, 16 Information on bother for UI subtypes and OAB also remain limited for men. We used data from the Multi-ethnic Study of Atherosclerosis (MESA) to examine the prevalence of any UI, UI subtypes, OAB without UI and associated bother by race/ethnicity. We hypothesized that prevalence of UI subtypes, OAB without UI and associated bother differs by race/ethnicity. We also examined prevalence of other lower urinary tract symptoms (LUTS) by UI subtype.
Materials and Methods
This cross-sectional study focused on men who completed the sixth exam of MESA, an observational study which recruited 6814 men and women, age 45 to 84 years, from six communities in the U.S. (Baltimore, MD; Chicago, IL; Forsyth County, NC; Los Angeles County, CA; Northern Manhattan, NY; and St. Paul, MN) during years 2000–2002 and then follow-up exams occurred approximately every two years. Sampling and recruitment procedures have been previously described in detail.17 All participants were free of clinical cardiovascular disease and heart failure at baseline per study design. Because the study included imaging to measure coronary artery calcium, adults weighing >300 pounds were not eligible for participation. The Institutional Review Boards at all participating sites approved the study, and all participants gave informed consent. Questions on urinary symptoms were included in the sixth MESA visit conducted during July 2015-June 2016. A total of 1536 men returned for the sixth MESA exam and 1446 of these men (94.1%) completed the questionnaire on urinary symptoms. During the recruitment process, potential participants were asked about their race and ethnicity using questions based on the U.S. 2000 census questionnaire. Potential participants who self-reported their race/ethnicity group as White or Caucasian, Black or African-American, Chinese, or Spanish/Hispanic/Latino were asked to participate. Race and ethnicity variables were then categorized as non-Hispanic (NH) White, NH Black, Chinese, and Hispanic.
Information on urinary symptoms was collected using the International Consultation on Incontinence Questionnaire (ICIQ).18 This questionnaire measures an individual’s experience with urinary symptoms (e.g., urgency, pain) over the past four weeks and the degree to which each of these symptoms bothered the individual. This tool has been used internationally with established reliability and validity18 and is recommended by the International Continence Society for assessment of incontinence and its severity in research studies.19, 20 The ICIQ Male Lower Urinary tract symptoms module (ICIQ-MLUTS) long form has 14 questions. For each question, respondents were queried on frequency of a symptom as “never” (0 points), “occasionally” (1 point), “sometimes” (2 points), “most of the time” (3 points) or “all of the time” (4 points). Presence of pure SUI was defined as a score of 2 points or higher for the question, “Does urine leak when you are physically active, exert yourself, cough or sneeze?” in combination with the absence of UUI. UUI was based on two questions: “Do you have a sudden need to rush to the toilet to urinate?” and “Does urine leak before you can get to the toilet?” with a score of 2 points or higher in the absence of SUI for both questions. MUI was defined as presence of both UUI and SUI with a score of 2 points or higher for all the above questions. Any UI prevalence was calculated as sum of SUI, UUI and MUI prevalence. OAB without UI was defined as scores of 2 points or higher for “Do you have a sudden need to rush to the toilet to urinate?” and negative response to the question, “Does urine leak before you can get to the toilet?” in the absence of SUI. All other urinary symptoms (delay in urination, hesitancy, weak urine stream) were defined as present if men reported a score of 2 points or higher. Nocturia was defined as waking from sleep ≥2 times during sleep to urinate. Bother was queried for each symptom with the individual asked to circle a number between 0 (none) and 10 (great deal of bother) for each urinary symptom. Presence of bother was defined as a score ≥3. Prevalence of a UI subtype with bother was defined as of UI subtype with accompanying bother scores ≥ 3.
Demographics, physical activity, education level, medical history, and current medication use at exam 6 along with a fasting blood sample were collected during the standardized interview. Information on physical activity was collected using the MESA Typical Week Physical Activity Survey, which was adapted from the Cross-Cultural Activity Participation Study21 and designed to identify the time spent in and frequency of various physical activities during a typical week in the past month. Impaired fasting glucose was defined as a fasting glucose between 100–125 mg/dl and diabetes was based on a self-reported physician diagnosis, fasting blood glucose ≥ 126 mg/dl and/or use of insulin or oral hypoglycemic agents. Information on prostate cancer history was obtained at the baseline visit via questionnaire. After the baseline visit, MESA participants were contacted every 6–9 months and queried on changes in health status including new cancer diagnoses and cancer type type.
Statistical Analysis
Participant characteristics were examined by completion of the ICIQ. The Chi-square test was used to compare categorical variables and an unpaired t-test was used to compare continuous variables. To address the non-parametric distribution of bother, reported scores from 0 to 10 were log transformed and then compared across racial/ethnic groups using ANOVA among men with UI. The Generalized linear model with binomial family and log link function was used to estimate the prevalence of UI subtypes and OAB without UI by race/ethnicity while adjusting for potential confounders.22 Several regression models were used to examine the robustness of the association of race/ethnicity with prevalence of UI subtypes with NH White race as the referent group while controlling for the potential confounding effects of demographic, behavioral and clinical characteristics measured at exam 6. We created a set of sequentially adjusted models for analysis. Model 1 included age and BMI. Model 2 added history of prostate cancer, impaired fasting glucose and diabetes status, cigarette smoking status and physical activity to Model 1, and Model 3 added use of diuretics, calcium channel blockers, beta-blockers, alpha-blockers, education and field site to Model 2. Interaction terms of age*race/ethnicity were fitted in the fully adjusted model to examine interactions between age and race/ethnicity on UI subtype prevalence. Stata version 14 (College Station, TX) was used to conduct the statistical analyses.
Results
Study population
Table 1 shows the characteristics of men by completion of the ICIQ at exam 6. Men who did not complete the ICIQ were older (mean age 81 [standard deviation [SD] 9.2] vs. 73.7 [SD 8.4] years; p <0.01) and were more likely to report poor health (9% vs. 1.1%; p <0.01) at exam 6. The prevalence of obesity, diabetes, and use of diuretics, and alpha blockers did not differ significantly by completion of the ICIQ at exam 6.
Table 1.
Characteristics of male MESA participants by completion of the International Consultation on Incontinence Questionnaire (ICIQ), 2015–2016
| Completed ICIQ (n=1446) | Did not complete ICIQ (n=90) | P value | |
|---|---|---|---|
| Age, mean (SD), y | 73.7 (8.4) | 81.0 (9.2) | <0.001 |
| Age Categories, (%) | <0.001 | ||
| 55–64 y | 15.3 | 5.6 | |
| 65–74 y | 41.6 | 18.9 | |
| 75–84 y | 31.0 | 43.3 | |
| >= 85 y | 11.9 | 32.2 | |
| Race/ethnicity (%) | 0.05 | ||
| Non-Hispanic White | 40.7 | 41.1 | |
| Chinese | 14.2 | 4.4 | |
| Non-Hispanic Black | 22.9 | 28.9 | |
| Hispanic | 22.1 | 25.6 | |
| BMI, kg/m2 (SD) | 28.2 (4.8) | 26.7 (5.2) | 0.004 |
| Obese (%) | 31.9 | 22.4 | 0.2 |
| Diabetes and 2003 ADA Fasting criteria (%) | 0.35 | ||
| Impaired fasting | 26.3 | 18.3 | |
| Diabetes mellitus | 26.5 | 35 | |
| General Health, (%) | <0.01 | ||
| Excellent | 14.2 | 6.7 | |
| Very Good | 36.2 | 27 | |
| Good | 35.7 | 40.4 | |
| Fair | 12.7 | 16.8 | |
| Poor | 1.1 | 9 | |
| Any Diuretic use, (%) | 16.9 | 23.3 | 0.1 |
| Current Cigarette Use, (%) | 6 | 2.3 | 0.01 |
| Prostate cancer, (%) | 1.3 | 0 | 0.3 |
| Any Calcium channel blockers use, (%) | 21.9 | 27.8 | 0.2 |
| Alpha Blockers use, (%) | 4.1 | 5.6 | 0.5 |
| Beta blockers, (%) | 22.8 | 33.3 | 0.02 |
Table 2 shows the characteristics of the men who completed the ICIQ by race/ethnicity. Among the 1446 men who completed the ICIQ, 40.7% were NH White, 14.2% were Chinese, 23.0% were NH Black and 22.0% were Hispanic. At exam 6, mean age was similar across the four racial/ethnic groups and over 40% of the men in each racial/ethnic group were age 75 years and older. Prevalence of obesity and diabetes and use of diuretics and calcium channel blockers differed by race/ethnicity. The reported prevalence of prostate cancer was overall low among all racial/ethnic groups.
Table 2.
Characteristics of men who completed the International Consultation on Incontinence Questionnaire (ICIQ) by race/ethnicity (n=1446), 2015–2016
| NH White (n=589) | Chinese (n=206) | NH Black (n=331) | Hispanic (n=320) | P value | |
|---|---|---|---|---|---|
| N, (% total sample) | 589 (40.7) | 206 (14.3) | 331 (22.9) | 320 (22.1) | |
| Age, years (SD) | 74 (8.5) | 73.7 (8.1) | 73.3 (8.4) | 73.4 (8.4) | 0.5 |
| Age Category (%) | 0.08 | ||||
| 55–64 years | 14.4 | 14.1 | 14.8 | 18.4 | |
| 65–74 years | 40.6 | 40.8 | 47.4 | 38.1 | |
| 75 – 84 years | 31.6 | 34 | 25.1 | 34.4 | |
| ≥ 85 years | 13.4 | 11.2 | 12.7 | 9.1 | |
| Education | <0.001 | ||||
| Less than High school | 2.0 | 11.2 | 3.0 | 30.0 | |
| High school/GED and/or some college | 26.8 | 25.2 | 42.0 | 41.6 | |
| College degree or higher | 71.1 | 63.6 | 55.0 | 28.4 | |
| BMI, kg/m2 (SD) | 28.3 (4.4) | 24.6 (3.4) | 29.1 (5.1) | 29.5 (4.9) | <0.001 |
| Obese, (%) | 26.8 | 8.2 | 40.2 | 40.3 | <0.001 |
| Impaired Fasting Glucose (%) | 27.1 | 33 | 21.3 | 25.8 | <0.001 |
| Diabetes (%) | 19.1 | 27.3 | 30.4 | 35.7 | <0.001 |
| General Health reported, (%) | <0.001 | ||||
| Excellent | 22.4 | 3.9 | 9.7 | 10.3 | |
| Very Good | 43.6 | 23.8 | 36.2 | 30.6 | |
| Good | 26.7 | 43.2 | 40.8 | 42.5 | |
| Fair | 6.6 | 25.7 | 13 | 15.3 | |
| Poor | 0.7 | 3.4 | 0.3 | 1.2 | |
| Current smoker (%) | 5.3 | 4.4 | 8.8 | 5.6 | <0.004 |
| 1Physical activity (met-min/week) | 4140 (2182, 7500) | 2347 (1095, 5190) | 4860 (1890, 9360) | 3011 (1425, 6517) | |
| Diuretic use (%) | 16.9 | 7.8 | 24.9 | 14.4 | <0.001 |
| Alpha blockers use, (%) | 3.2 | 5.4 | 4.3 | 4.7 | 0.5 |
| Beta blocker use (%) | 22.9 | 21.5 | 23.1 | 23.2 | 0.9 |
| Calcium Blocker use (%) | 16.9 | 21.9 | 32.2 | 20.7 | <0.001 |
| Prostate cancer (%) | 1.1 | 0.5 | 1.6 | 1.8 | 0.6 |
| Anticholinergics use (%) | 0.7 | 0.5 | 2.4 | 0.6 | 0.05 |
Data shown as median (interquartile range)
Categorical data are presented as column percentages except for N (% total)
Figure 1 shows prevalence of any UI, UI subtypes and OAB without UI by race/ethnicity. Prevalence of any UI ranged from as high as 15.7% and 15.3% among NH Black and Hispanic men, respectively, to as low as 7.9% and 5.8% among NH White and Chinese men, respectively. Prevalence of SUI and MUI were overall low and did not differ by race/ethnicity. UUI accounted for the majority of all UI and the highest prevalence was noted among NH Black men (13.0%) followed by Hispanic (11.2%), NH White (6.8%) and Chinese (2.9%) men, (p value < 0.01) (see Figure 1). Prevalence of OAB without UI was similar across the racial/ethnic groups. Table 3 shows the prevalence urinary symptoms by presence of UI subtype and OAB without UI. Nocturia, urinary retention, hesitancy and weak urine stream were common for all UI subtypes and OAB without UI. Highest prevalence of urinary symptoms occurred in men with MUI followed by those with OAB with UI, OAB without UI and SUI.
Figure 1.
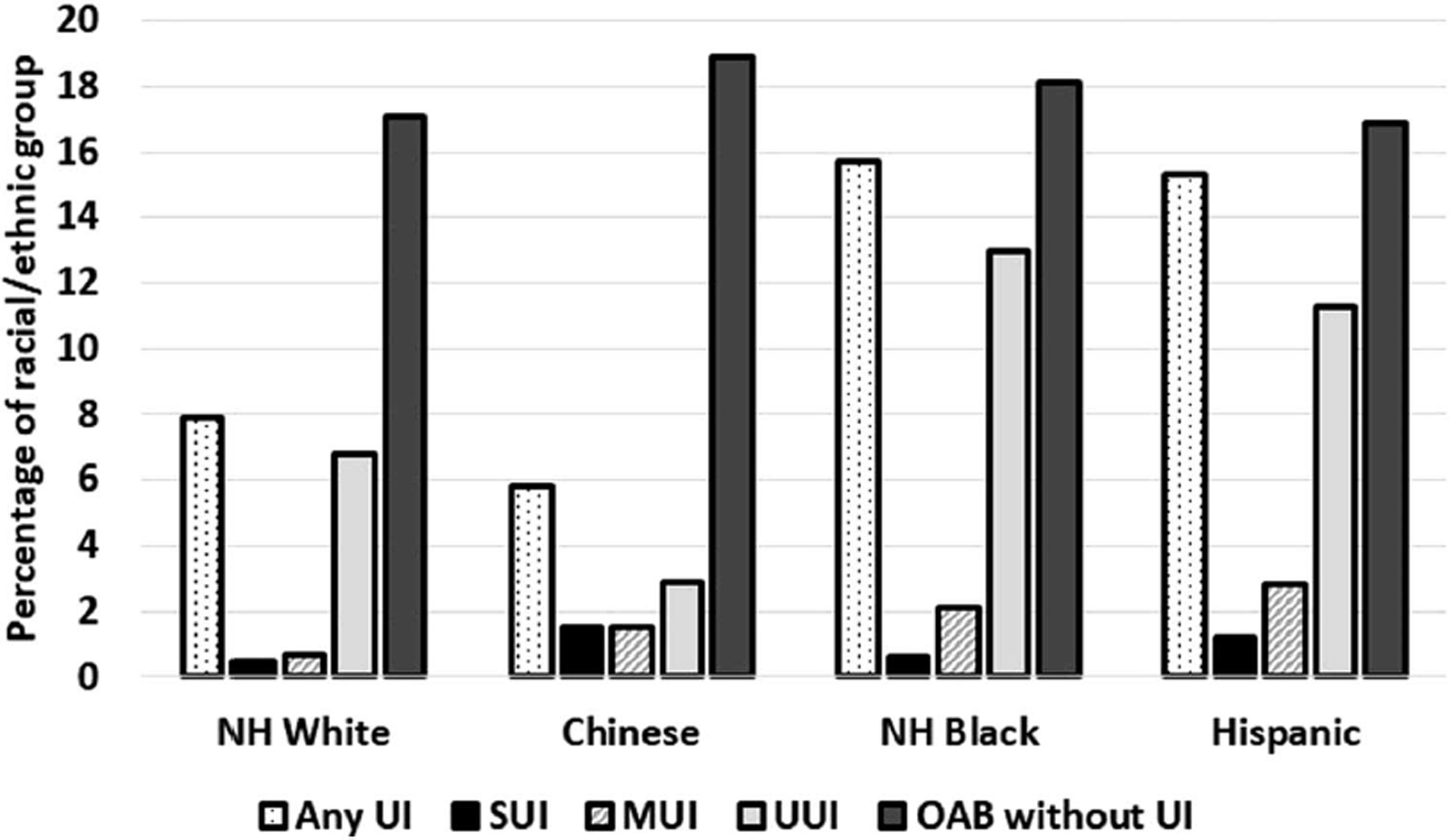
Percentage with urinary incontinence subtypes and overactive bladder without UI associated by race/ethnicity. UI=urinary incontinence, SUI = stress urinary incontinence, UUI = Urgency urinary incontinence, MUI = mixed urinary incontinence, OAB without UI = overactive bladder without urinary incontinence
Table 3.
Prevalence of lower urinary symptoms by presence of urinary incontinence subtype and overactive bladder without urinary incontinence in male MESA participants (n=1446), 2015–2016
| 1Urinary symptom | Any UI (n=160) | Stress UI (n=12) | MUI (n=23) | UUI (n=125) | OAB without UI (n=254) |
|---|---|---|---|---|---|
| Delay in urination,%(n) | 21.9 (n=35) | 16.7 (n=2) | 34.8 (n=8) | 20.0 (n=25) | 29.1 (n=74) |
| Strain to urinate,%(n) | 23.8 (n=38) | 0 | 34.8 (n=8) | 24.0 (n=30) | 15.3 (n=39) |
| Weak urine stream, %(n) | 40.6 (n=65) | 25.0 (n=3) | 65.2 (n=15) | 37.6 (n=47) | 31.2 (n=79) |
| 2Urinary retention,%(n) | 48.8 (n=78) | 25.0 (n=3) | 65.2 (n=15) | 48.0 (n=60) | 32 (n=81) |
| 3Hesitancy,%(n) | 41.9 (n=67) | 16.7 (n=2) | 65.2 (n=15) | 40.0 (n=50) | 27.9 (n=71) |
| 4Frequent urination (> 8x/day),%(n) | 26.4 (n=42) | 8.3 (n=1) | 39.1 (n=9) | 25.6 (N=32) | 21.3 (n=54) |
| 5Nocturia | 68.7 (n=110) | 25.0 (n=3) | 82.6 (n=19) | 70.4 (n=88) | 59.7 (n=151) |
All urinary symptoms were reported occurring at least “sometimes” or more frequently over the past four weeks.
Urinary retention defined as feeling of incomplete bladder emptying after urination;
Hesitancy defined as starting and stopping urination more than once during micturition;
Frequent urination defined as > 8x/day;
Nocturia defined as urinating awaking two or more times during night to urinate;
After adjusting for demographics, co-morbidities and use of diuretics, calcium blockers, beta blockers, alpha blockers, and field center site, any UI was significantly more prevalent among NH Black (Prevalent Ratio (PR) 1.62; 95% CI 1.06, 2.47) compared to NH White men (Table 4). Similarly, NH Black men had higher prevalence of UUI (PR 1.63; 95% CI 1.01, 2.61) compared to NH White men after adjustment for covariates. No significant association was noted with SUI, MUI or OAB without UI and race/ethnicity after adjustment for covariates. No significant interaction was noted between age and race/ethnicity with any UI subtype.
Table 4.
Prevalence ratios (PR) ratios of incontinence subtypes and overactive bladder without urinary incontinence by race/ethnicity among men in MESA (n=1446), 2015–2016
| Race/ethnicity | Model 1 | Model 1 | Model 3 | |
|---|---|---|---|---|
| Any UI | %(n) | PR (95% CI) | PR (95% CI) | PR (95% CI) |
| NH White | 7.9 (47) | Referent | Referent | Referent |
| Chinese | 5.8 (12) | 0.93 (0.49, 1.73) | 1.14 (0.61, 2.11) | 1.04 (0.54, 2.01) |
| NH Black | 15.7 (52) | 1.88 (1.29, 2.72) | 1.70 (1.16, 2.49) | 1.62 (1.06, 2.47) |
| Hispanic | 15.3 (49) | 1.78 (1.22, 2.59) | 1.69 (1.19, 2.41) | 1.57 (0.96, 2.54) |
| Stress UI | ||||
| NH White | 0.5 (3) | Referent | Referent | Referent |
| Chinese | 1.5 (3) | 3.73 (0.70, 19.74) | 3.61 (0.63, 20.73) | 2.05 (0.32, 13.12) |
| NH Black | 0.6 (2) | 1.14 (0.19, 6.85) | 1.53 (0.25, 9.25) | 1.17 (0.18, 2.88) |
| Hispanic | 1.2 (4) | 2.28 (0.51, 10.23) | 2.27 (0.51, 10.17) | 0.85 (0.15, 4.89) |
| Urgency UI | ||||
| NH White | 6.8 (40) | Referent | Referent | Referent |
| Chinese | 2.9 (6) | 0.51 (0.22, 1.21) | 0.62 (0.26, 1.46) | 0.62 (0.25, 1.54) |
| NH Black | 13.0 (43) | 1.86 (1.23, 2.79) | 1.66 (1.06, 2.59) | 1.63 (1.01, 2.61) |
| Hispanic | 11.3 (36) | 1.56 (1.02, 2.41) | 1.58 (1.01, 2.47) | 1.50 (0.84, 2.67) |
| Mixed UI | ||||
| NH White | 0.7 (4) | Referent | Referent | Referent |
| Chinese | 1.5 (3) | 3.86 (0.84, 17.66) | 4.49 (0.92, 21.98) | 3.28 (0.56, 19.12) |
| NH Black | 2.1 (7) | 2.68 (0.78, 9.16) | 1.88 (0.45, 7.79) | 1.57 (0.27, 9.28) |
| Hispanic | 2.8 (9) | 3.31 (1.02, 10.80) | 1.95 (0.53, 7.13) | 1.95 (0.34, 11.30) |
| OAB without UI | ||||
| NH White | 17.1 (101) | Referent | Referent | Referent |
| Chinese | 18.9 (39) | 1.07 (0.75, 1.51) | 0.98 (0.68, 1.41) | 1.21 (0.80, 1.85) |
| NH Black | 18.1 (60) | 1.07 (0.80, 1.43) | 1.07 (0.78, 1.47) | 1.07 (0.76, 1.43) |
| Hispanic | 16.9 (54) | 0.99 (0.74, 1.35) | 0.79 (0.56, 1.12) | 0.79 (0.52, 1.21) |
UI=Urinary incontinence; OAB=Overactive Bladder; NH=Non Hispanic
Adjusted for age and BMI;
Adjusted for age, BMI, prostate cancer, DM, physical activity, smoking status;
Adjusted for age, BMI, prostate cancer, DM, physical activity, smoking status, use of diuretics, calcium channel blockers, beta blockers, alpha blockers, education and site.
The majority of MUI, UUI and OAB without UI was associated with bother for all racial/ethnic groups (see Figure 2). Bother scores ≥ 3 were reported in 33.3% of SUI, 88.8% of UUI, 91.3% of MUI and 72.2% of OAB without UI. Figure 3 shows boxplots of bother scores by race/ethnicity for men with any UI. No significant difference in log transformed bother scores were noted by race/ethnicity (overall p value = 0.3).
Figure 2.
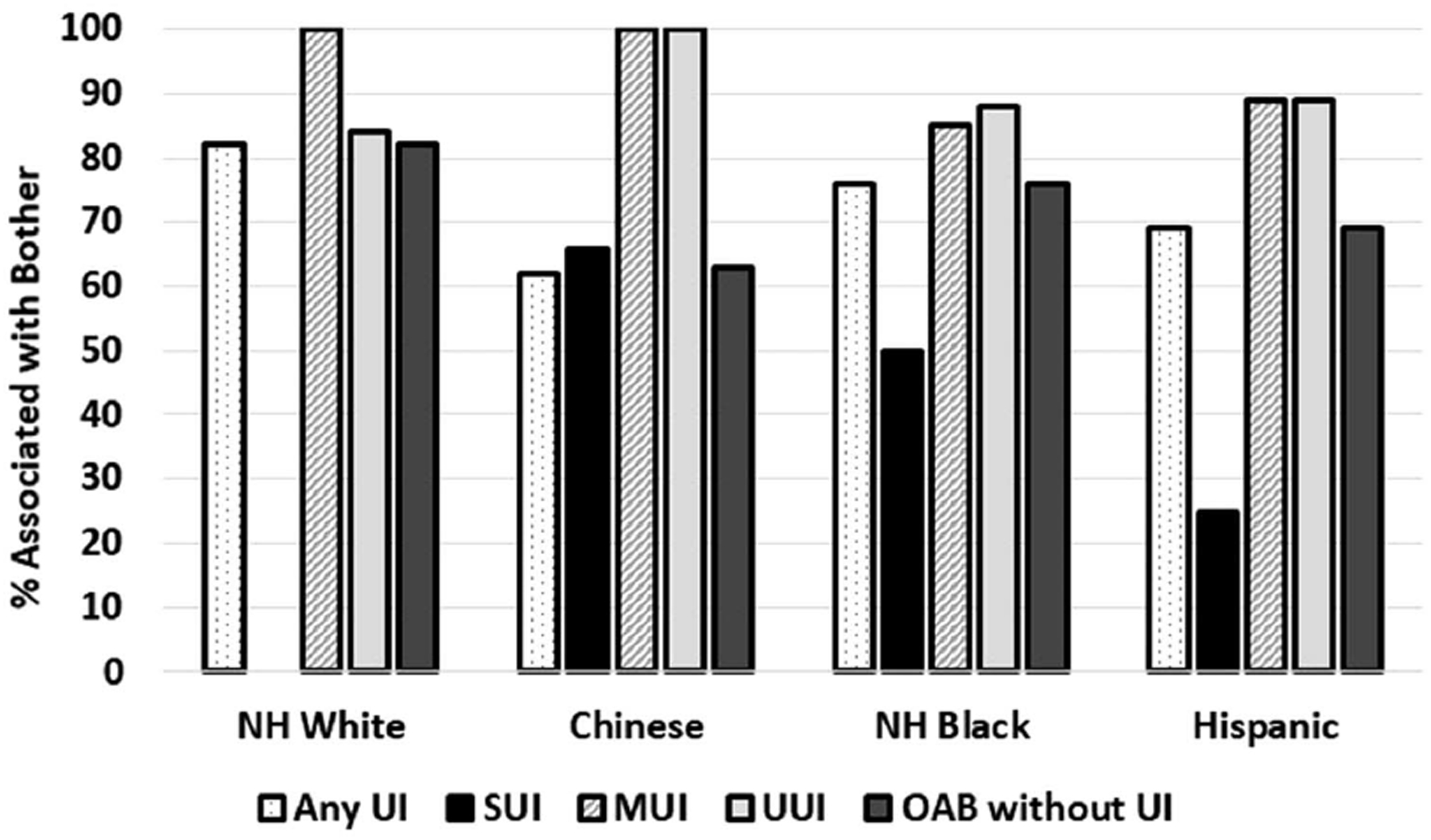
Proportion of Urinary Incontinence (UI) subtypes and Overactive Bladder (OAB) without UI associated with bother scores ≥ 3 by race/ethnicity. UI=urinary incontinence, SUI = stress urinary incontinence, UUI = Urgency urinary incontinence, MUI = mixed urinary incontinence, OAB without UI = overactive bladder without urinary incontinence
Figure 3.
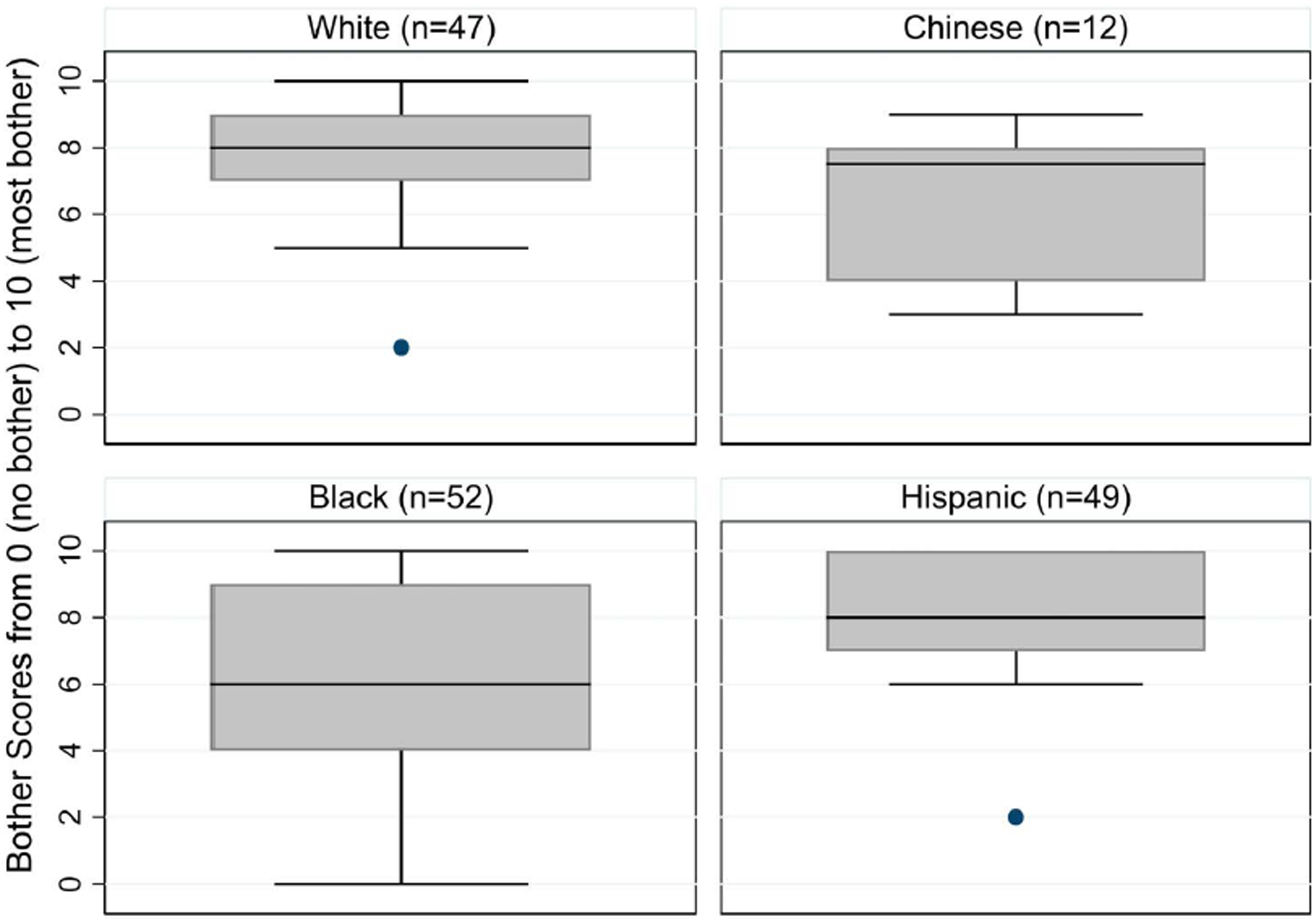
Boxplot of bother scores for men with any urinary incontinence by race/ethnicity
Discussion
In this older racially diverse cohort of men, 11.1% had any UI and UUI accounted for the majority of UI while MUI and SUI were infrequent across all racial/ethnic groups. Most UI was associated with bother, and bother scores did not differ significantly by race/ethnicity. We also found that UUI prevalence varies by race/ethnicity with NH Black men showing the highest prevalence. After adjustment for covariates, we found that overall prevalence of any UI was significantly higher among NH Black as compared to NH White men. Almost half of all men with UUI reported urinary retention and up to one-third reported urinary hesitancy and a weak urine stream.
Our findings of racial/ethnic differences in UUI are similar to findings from a previous online survey of 9416 men age 40 years and older from the U.S which found that frequency of UUI and OAB without UI was highest among NH Black.12 Other studies have reported no racial/ethnic differences in UI prevalence among men.8, 14, 16 However, prevalence of at least moderate LUTS assessed with the American Urological Association Symptom Index was higher among Hispanic and NH Black men compared to NH White men after controlling for differences in demographics and co-morbidities.23 In our study, we found a significantly higher prevalence of UUI among NH Black men compared to NH White men even after adjustment for demographics, co-morbidities and medication use. It should be noted that we did not have information on history of benign prostatic hyperplasia (BPH) and the low rates of self-reported prostate cancer in this group of older men likely reflects under reporting. However, higher prevalence of LUTS among Hispanic and NH Black men in previous studies could not be explained by differences in demographics and co-morbidities.
UI in men is often the result of multiple factors including medications use, detrusor muscle dysfunction, prostatic hypertrophy or cancer and neurological disease, depending on UI subtype. OAB is a clinical syndrome that is currently believed to be associated with multiple risk factors including BPH, bladder wall inflammation and ageing of the detrusor.24, 25 Evidence also suggests that bladder volume sensitivity is heightened in OAB due to higher activity in the brain areas that sense bladder volume.26, 27 While OAB is the result of multiple factors, BPH often incites, or exacerbates LUTS. The most common risk factor for BPH is advancing age, but obesity, diabetes and hypertension are also operative.28 We found little attenuation in the association of race/ethnicity with UUI and OAB without UI after adjustment for co-morbidities. Race/ethnicity may also reflect differences in lifetime occupational patterns, access to healthcare, physical activity and diet which may influence development of BPH and OAB29 but are difficult to measure accurately in an observational cohort. Race/ethnicity may also influence the reporting of urinary symptoms but this hypothesis has not been well tested.
This study utilized data collected with an established multi-ethnic cohort of adults recruited from six U.S. communities. Information on UI and OAB and associated bother and urinary symptoms was collected using the ICIQ, a previously validated questionnaire. The ICIQ asks persons to recall urinary symptoms over the past four weeks, a time period that has been utilized with other surveys of urinary health.12 While recall bias can affect the response variable for any survey, a longer time frame of querying past urinary symptoms will exacerbate bias.8, 14 Our study also includes information on associated bother which differs from most previous studies on UI in men.12, 14 This study lacked direct measures of bladder function such as uroflowmetry or urodynamic measurements which can give different results from self-reported symptoms.30 While the response rate for the ICIQ in MESA men exceeded 94%, the men who did not complete the ICIQ were older. Thus, our findings likely underestimate the prevalence of UI. The reported prevalence of prostate cancer was low and likely under reported and our study lacked information on cancer treatment or physician diagnosis of BPH or use of 5-alpha-reductse inhibitors.
Conclusion:
In conclusion, UUI differs by race/ethnicity and more studies are needed to determine reasons for these differences. The majority of UI is associated with bother in men regardless of race/ethnicity.
Funding Source:
NIDDK 1R01DK104842-01 and by contracts 75N92020D00001, HHSN268201500003I, N01-HC-95159, 75N92020D00005, N01-HC-95160, 75N92020D00002, N01-HC-95161, 75N92020D00003, N01-HC-95162, 75N92020D00006, N01-HC-95163, 75N92020D00004, N01-HC-95164, 75N92020D00007, N01-HC-95165, N01-HC-95166, N01-HC-95167, N01-HC-95168 and N01-HC-95169 from the National Heart, Lung, and Blood Institute, and by grants UL1-TR-000040, UL1-TR-001079, and UL1-TR-001420 from the National Center for Advancing Translational Sciences (NCATS) and NIDDK 1R01DK104842-01 from the National Institute of Diabetes, Digestive and Kidney Diseases (NIDDK).
Abbreviation key:
- UI
urinary incontinence
- UUI
urgency urinary incontinence
- MUI
mixed urinary incontinence
- SUI
stress urinary incontinence
- OAB
overactive bladder
- NH
Non-Hispanic
- BPH
benign prostatic hyperplasia
Footnotes
Disclosures: LB: Editorial stipends from Journal of the American Medical Association, Reconstructive Surgery and Up to Date. All authors report no disclosures.
References
- 1.Daugirdas SP, Markossian T, Mueller E et al. : Urinary incontinence and chronic conditions in the US population age 50 years and older. Int Urogynecol J 2020; doi: 10.1007/s00192-019-04137-y:. [DOI] [PubMed] [Google Scholar]
- 2.Coyne KS, Wein A, Nicholson S et al. : Economic burden of urgency urinary incontinence in the United States: a systematic review. Journal of Managed Care Pharmacy 2014; 20: 130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ganz ML, Smalarz AM, Krupski TL et al. : Economic costs of overactive bladder in the United States. Urology 2010; 75: 526. [DOI] [PubMed] [Google Scholar]
- 4.Buckley BS, Lapitan MC, Epidemiology Committee of the Fourth International Consultation on Incontinence, Paris, 2008: Prevalence of urinary incontinence in men, women, and children--current evidence: findings of the Fourth International Consultation on Incontinence. Urology 2010; 76: 265. [DOI] [PubMed] [Google Scholar]
- 5.Mather M, Jacobsen L, Jarosz, Kilduff L, Lee A, Pollard KM, Scommegna P Vonorman A. America’s Changing Population. Population Bulletin. 2019: 74(1). www.prb.org [Google Scholar]
- 6.Siddiqui NY, Levin PJ, Phadtare A et al. : Perceptions about female urinary incontinence: a systematic review. Int Urogynecol J 2014; 25: 863–871. [DOI] [PubMed] [Google Scholar]
- 7.de Vries HF, Northington GM, Bogner HR: Urinary incontinence (UI) and new psychological distress among community dwelling older adults. Arch Gerontol Geriatr 2012; 55: 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tennstedt SL, Chiu GR, Link CL et al. : The effects of severity of urine leakage on quality of life in Hispanic, White, and Black men and women: the Boston community health survey. Urology 2010; 75: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lagro-Janssen TA, Hilkens CJ, Klaasen RI et al. : Greater emotional and social effect of urinary incontinence in men than women. J Am Geriatr Soc 2008; 56: 1779. [DOI] [PubMed] [Google Scholar]
- 10.Langa KM, Fultz NH, Saint S et al. : Informal caregiving time and costs for urinary incontinence in older individuals in the United States. J Am Geriatr Soc 2002; 50: 733. [DOI] [PubMed] [Google Scholar]
- 11.Milson I., Altman D., Lapitan MC et al. : Epidemiology of urinary (UI) and faecal (FI) incontinence and pelvic organ prolape.. In: Incontinence, 5th ed. Edited by Abrams P, Cardozo L, Khoury S et al. Paris, France: European Association of Urology; 2009. [Google Scholar]
- 12.Coyne KS, Margolis MK, Kopp ZS et al. : Racial differences in the prevalence of overactive bladder in the United States from the epidemiology of LUTS (EpiLUTS) study. Urology 2012; 79: 95. [DOI] [PubMed] [Google Scholar]
- 13.Irwin DE, Milsom I, Hunskaar S et al. : Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol 2006; 50: 1306. [DOI] [PubMed] [Google Scholar]
- 14.Markland AD, Goode PS, Redden DT et al. : Prevalence of urinary incontinence in men: results from the national health and nutrition examination survey. J Urol 2010; 184: 1022. [DOI] [PubMed] [Google Scholar]
- 15.Prevalence of and risk factors for urine leakage in a racially and ethnically diverse population of adults: the Boston Area Community Health (BACH) Survey. Am J Epidemiol 2008; 167: 390. [DOI] [PubMed] [Google Scholar]
- 16.Hu JC, Gold KF, Pashos CL et al. : Temporal trends in radical prostatectomy complications from 1991 to 1998. J Urol 2003; 169: 1443. [DOI] [PubMed] [Google Scholar]
- 17.Bild DE, Bluemke DA, Burke GL et al. : Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol 2002; 156: 871. [DOI] [PubMed] [Google Scholar]
- 18.Avery K, Donovan J, Peters TJ et al. : ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourology & Urodynamics 2004; 23: 322. [DOI] [PubMed] [Google Scholar]
- 19.Abrams P, Avery K, Gardener N et al. : The International Consultation on Incontinence Modular Questionnaire: www.iciq.net. J Urol 2006; 175: 1063. [DOI] [PubMed] [Google Scholar]
- 20.Kelleher C, Staskin D, Cherian P et al. : Milson I, Altman D, Lapitan MC, Nelson R, Sillen U, Thom D. Epidemiology of urinary (UI) and faecal (FI) incontinence and pelvic organ prolape. 2009:35–111. In: Incontinence, 5th ed. Edited by Abrams P, Cardozo L, Khoury S et al. Paris, France: European Association of Urology; 2009. [Google Scholar]
- 21.Whitt MC, DuBose KD, Ainsworth BE et al. : Walking patterns in a sample of African American, Native American, and Caucasian women: the cross-cultural activity participation study. Health Education & Behavior 2004; 31: 45S. [DOI] [PubMed] [Google Scholar]
- 22.Zocchetti C, Consonni D, Bertazzi PA: Estimation of prevalence rate ratios from cross-sectional data. Int J Epidemiol 1995; 24: 1064–1065. [DOI] [PubMed] [Google Scholar]
- 23.Sarma AV, Wei JT, Jacobson DJ et al. : Comparison of lower urinary tract symptom severity and associated bother between community-dwelling Black and White men: the Olmsted County Study of Urinary Symptoms and Health Status and the Flint Men’s Health Study. Urology 2003; 61: 1086. [DOI] [PubMed] [Google Scholar]
- 24.Patra PB, Patra S: Research Findings on Overactive Bladder. Curr Urol 2015; 8: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reynolds WS, Fowke J, Dmochowski R: The Burden of Overactive Bladder on US Public Health. Curr Bladder Dysfunct Rep 2016; 11: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Suskind AM: The Aging Overactive Bladder: A Review of Aging-Related Changes from the Brain to the Bladder. Curr Bladder Dysfunct Rep 2017; 12: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jorgensen JB, Jensen KM: Uroflowmetry. Urol Clin North Am 1996; 23: 237. [DOI] [PubMed] [Google Scholar]
- 28.Kristal AR, Arnold KB, Schenk JM et al. : Race/ethnicity, obesity, health related behaviors and the risk of symptomatic benign prostatic hyperplasia: results from the prostate cancer prevention trial. J Urol 2007; 177: 1395. [DOI] [PubMed] [Google Scholar]
- 29.Kristal AR, Arnold KB, Schenk JM et al. : Dietary patterns, supplement use, and the risk of symptomatic benign prostatic hyperplasia: results from the prostate cancer prevention trial. Am J Epidemiol 2008; 167: 925. [DOI] [PubMed] [Google Scholar]
- 30.Howard D, Delancey JO, Tunn R et al. : Racial differences in the structure and function of the stress urinary continence mechanism. Obstet Gynecol 2000; 95: 713. [DOI] [PMC free article] [PubMed] [Google Scholar]


