Abstract
High serum phosphate levels have been associated with increased morbidity and mortality in dialysis patients. Nephrologists routinely counteract the positive phosphate balance in dialysis patients through nutritional counselling, stronger phosphate removal by dialysis and prescription of phosphate binders. An individualized choice of phosphate binders is a desirable option to improve the poor adherence with these medications’ prescription that has been associated with hyperphosphataemia.
Keywords: adherence, CKD-MBD, dialysis, phosphate binder
Phosphate binders are prescribed to about 80% of dialysis patients as single therapy, while 50% receive a prescription of two phosphate binders [1]. Is ‘drug prescription’ equivalent to ‘taking medication’? Of course the answer is negative.
High serum phosphate levels have been associated with increased morbidity and mortality in several observational studies, conducted among dialysis cohorts [2]. Furthermore, dialysis patients receiving phosphate binders were exposed to lower mortality risk compared with controls [3], with a 30% reduction of mortality risk, independent of the type of binder, calcium-based or calcium-free [4]. Poor adherence with phosphate binder prescription has been associated with hyperphosphataemia. The major problem is that dialysis patients do not feel ‘high phosphate’, except when it is too late and the signs and symptoms of chronic kidney disease–mineral bone disorder (CKD-MBD) appear in all their wickedness [5].
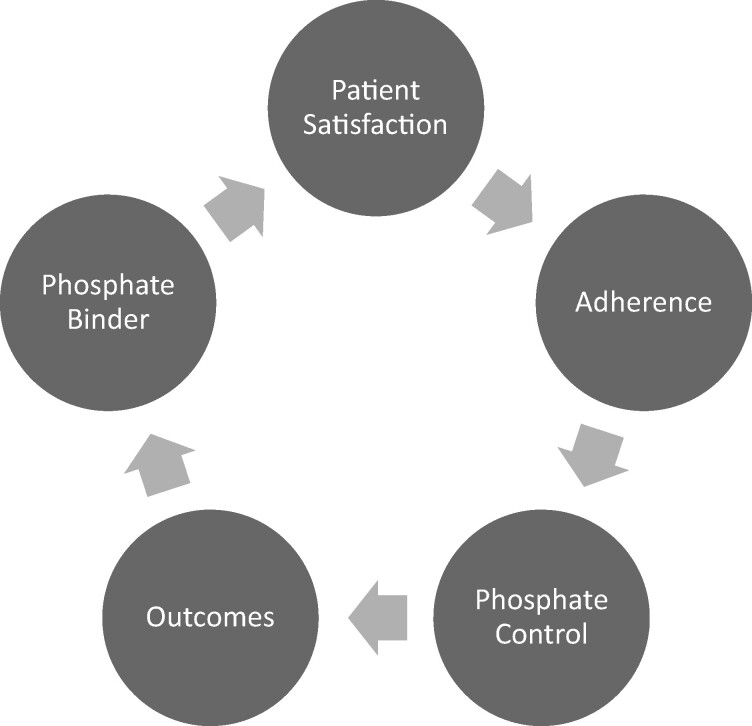
In Figure 1, we graphically represent the vicious circle of hyperphosphataemia and its treatment. Is it possible to break it?
FIGURE 1:
The vicious circle of adherence for phosphate binders in dialysis.
In their article, McCullough et al. [6] investigated the associations between patient satisfaction with prescribed phosphate binders and serum phosphorus levels and mortality rates. Adult haemodialysis patients in different European countries (Germany, Italy, Spain and the UK) in the Dialysis Outcomes and Practice Patterns Study (DOPPS Study) were asked about their satisfaction with phosphate binders, measured through three questions: difficulty, inconvenience and dissatisfaction. Interestingly, patients having poorer serum phosphate level control reported greater difficulty, inconvenience and dissatisfaction with their phosphate binders. Furthermore, dissatisfaction was associated with increased risk of mortality.
CKD-MBD therapy adherence is a very real problem for nephrologists. In several studies, the most commonly reported side effects are gastrointestinal (nausea, vomiting, diarrhoea, etc.), which are experienced by approximately 30–50% of patients [7], conditioning treatment discontinuation associated with the use of phosphate binders. Thus, as with most medicinal products, the efficacy of a phosphate binder is poorer in patients who are not adherent with the prescribed treatment schedule. The problem of treatment adherence therefore plays a crucial role in CKD-MBD therapy [8].
Commonly prescribed phosphate binders require patients to take multiple pills three to five times daily, resulting in a very high total daily pill burden [9]. Clearly, high pill burden represents a potential barrier to adherence to therapy, which may in turn reduce efficacy. A previous analysis of data from the DOPPS Study found that only 45% of US dialysis patients reported taking all of their prescribed phosphate binders during the prior month [10], and several studies have shown an inverse relationship between phosphate binder pill burden and serum phosphorus control [11].
In summary, when nephrologists prescribe phosphate binders, they should consider a patient-tailored treatment. Adherence is always negatively related to higher pill burden and serum phosphorus levels. We should aim to have adherence positively related to patients in the phosphorus target range, and to better outcomes. In fact, poor long-term adherence to drug therapy is universally recognized as one of the major clinical issues in the management of CKD patients. Moreover, dialysis patients belong to the group of subjects with one of the highest burdens of daily pill intake, with up to >20 pills per day. The development of new strategies to improve the diagnosis and management of poor adherence in patients receiving maintenance dialysis is still necessary.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Galassi A, Cupisti A, Santoro A. et al. Phosphate balance in ESRD: diet dialysis and binders against the low evident masked pool. J Nephrol 2015; 28: 415–429 [DOI] [PubMed] [Google Scholar]
- 2. Kestenbaum B, Sampson JN, Rudser KD. et al. Serum phosphate levels and mortality risk among people with chronic kidney disease. J Am Soc Nephrol 2005; 16: 520–528 [DOI] [PubMed] [Google Scholar]
- 3. Isakova T, Gutierrez OM, Chang Y. et al. Phosphorus binders and survival on hemodialysis. J Am Soc Nephrol 2009; 20: 388–396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cannata-Andia JB, Fernandez-Martin JL, Locatelli F. et al. Use of phosphate-binding agents is associated with a lower risk of mortality. Kidney Int 2013; 84: 998–1008 [DOI] [PubMed] [Google Scholar]
- 5. Cozzolino M, Ureña-Torres P, Vervloet MG. et al. ; CKD-MBD Working Group of ERA-EDTA. Is chronic kidney disease-mineral bone disorder (CKD-MBD) really a syndrome? Nephrol Dial Transplant 2014; 29: 1815–1820 [DOI] [PubMed] [Google Scholar]
- 6. McCullough K, Port FK, de Sequera P et al. European hemodialysis patient satisfaction with phosphate binders is associated with serum phosphorus levels: the Dialysis Outcomes and Practice Patterns Study Clin Kidney J 2021; 14: 1886–1893 [DOI] [PMC free article] [PubMed]
- 7. Bover J, Ureña-Torres P, Mateu S. et al. Evidence in chronic kidney disease-mineral and bone disorder guidelines: is it time to treat or time to wait? Clin Kidney J 2020; 13: 513–521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Alfieri C, Regalia A, Zanoni F. et al. The importance of adherence in the treatment of secondary hyperparathyroidism. Blood Purif 2019; 47: 37–44 [DOI] [PubMed] [Google Scholar]
- 9. Chiu YW, Teitelbaum I, Misra M. et al. Pill burden, adherence, hyperphosphatemia, and quality of life in maintenance dialysis patients. Clin J Am Soc Nephrol 2009; 4: 1089–1096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fissell RB, Karaboyas A, Bieber BA. et al. Phosphate binder pill burden, patient-reported non-adherence, and mineral bone disorder markers: Findings from the DOPPS. Hemodial Int 2016; 20: 38–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wang S, Alfieri T, Ramakrishnan K. et al. Serum phosphorus levels and pill burden are inversely associated with adherence in patients on hemodialysis. Nephrol Dial Transplant 2014; 29: 2092–2099 [DOI] [PMC free article] [PubMed] [Google Scholar]