Abstract
Objective
To identify, critique and synthesise the research findings that evaluate the use of resistance training (RT) programmes on return to sport outcome measures for people following ACL repair (ACLR).
Design and data sources
This systematic review included a comprehensive search of electronic databases (EBSCO health databases (CINAHL, MEDLINE, SPORTDiscus), Scopus and Pedro) performed in June 2020 and was guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist. Studies were appraised using the Downs and Black checklist.
Eligibility criteria
Randomised and non-randomised controlled trials, longitudinal cohort studies and case series were considered for inclusion where an adequate description of the RT intervention was provided as a part of the study’s ACLR rehabilitation protocol. Articles that did not include outcome measures related to return to sport criteria were excluded.
Results
Eleven articles met the inclusion criteria and were subjected to appraisal and data extraction. Study quality ranged from poor to excellent. RT intensity varied considerably among studies (between 5% and >80% of one repetition maximum). Only one identified study specifically investigated the effect of a low-intensity versus high-intensity RT protocol. The majority of studies reported participant outcomes that would not meet commonly used return to sport criteria.
Conclusion
There appears to be considerable variation in the intensity of RT prescribed in research for people following ACLR. Furthermore, in most of the identified studies, RT protocols promoted muscle endurance and hypertrophy without progressing to strength or power-based RT. The findings of this review provide insight into potential factors limiting returning to sport and contributing to reinjury for people following ACLR.
Keywords: rehabilitation, knee ACL, sport, ACL, sports rehabilitation programmes
Key messages.
What is already known
Resistance training (RT) is an integral component of an ACL repair (ACLR) rehabilitation programme.
Reinjury following ACLR remains high, and associated physical deficits relating to return to sport criteria are commonly observed even after a return to sport.
What are the new findings
There is no consensus regarding optimal RT intensity (among other RT parameters) throughout ACLR rehabilitation literature.
RT intensities found in the ACLR rehabilitation literature do not align with strength and conditioning principles and are often not optimised to develop the desired neuromuscular qualities required of return to sport criteria. This may contribute to suboptimal prescription of rehabilitation programmes and poorly prepared athletes.
Introduction
The incidence rate of primary ACL repair (ACLR) in Australia is the highest globally and continues to rise.1 Following surgery, rehabilitation is essential to ensure a return to full function by addressing postoperative strength and neuromuscular control deficits associated with reinjury.2–6 A comprehensive rehabilitation programme following ACLR is crucial for those who intend to return to sport, as reinjury rates are high in this population7; literature indicates that rerupture rates are 18% or higher in the young athletic population.8 Despite the importance placed on rehabilitation, modifiable deficits in lower limb strength and function can extend beyond 12 months following surgery and commonly persist after returning to sport.9 Of concern, Leister et al9 reported that up to 70% of people who have already returned to sport could not pass return to sport criteria 12 months after surgery.
ACLR rehabilitation should address postoperative deficits and facilitate a safe return to sport through a wide range of exercise modalities.10 Rehabilitation aims to restore muscular strength, with resistance training (RT) being a crucial programme component.10 The utilisation of RT principles, while concurrently considering the stage of healing following ACLR, is a considerable challenge faced by clinicians and patients. Intensity is considered the primary component of RT to achieve the desired training effect.10–12 RT intensity is defined as the magnitude of load of a given exercise, often expressed as a percentage of an individual’s one repetition maximum (1RM).10 13 RT is optimised to improve different aspects of neuromuscular function depending on the prescribed intensity.14 The purpose of the exercise and corresponding intensity must be well understood to succinctly prescribe an RT programme following ACLR. Varying demands must be placed on the patient through RT to address deficiencies in muscle endurance, size, strength and power to restore the full neuromuscular function of the affected limb.14 Panariello et al5 recommended a criteria-driven framework for rehabilitation following ACLR, breaking the rehabilitation process into distinct phases. The framework was based on the hierarchy of athletic development, recognising the needs of an ACLR patient as equal to the athlete preparing for sport.
Return to sport criteria following ACLR have been developed to objectively determine when a safe return to sport following ACLR is indicated.3 15 There is a consensus that passing the objective return to sport criteria is vital in reducing injury risk following ACLR; however, the association between current criteria and the risk of ACL graft injury is not yet clear.16 Kyritsis et al15 found a fourfold increased risk of ACL graft rupture for those patients who did not pass the return to sport criteria. Additionally, Grindem et al3 estimated an 84% lower knee reinjury rate among people who passed return to sport criteria. Following a meta-analysis of return to sport criteria, Losciale et al16 advocated for stricter criteria, in particular, that 100% strength and function Limb Symmetry Index (LSI) scores should be used to improve the sensitivity of criteria in predicting rerupture.
There appear to be confusion and a lack of consensus among physiotherapists surrounding ACLR rehabilitation. Physiotherapists have shown a lack of consistency when determining return to sport clearance,17 18 and Greenberg et al18 reported that 56% of physiotherapists believed 5 months of rehabilitation was sufficient following ACLR. Yet, Toole et al19 demonstrated that only 44% of patients had achieved an acceptable quadriceps LSI before gaining clearance to return to sport. These findings show an inadequate return to sport decision-making process and may suggest that suboptimal rehabilitation is being prescribed.3 Physiotherapists have also reported confusion surrounding the prescription and progression of exercises throughout ACLR rehabilitation.20 This confusion is likely accentuated by wide variability in rehabilitation protocols, most of which do not stress the importance of addressing deficits related to reinjury.21
Although the causes of reinjury are multifactorial, an RT protocol that fails to address postoperative neuromuscular deficits is likely to be a crucial factor.22 Currently, there does not appear to be any consensus for the application and progression of RT intensity throughout the ACLR rehabilitation process to address postoperative neuromuscular deficits optimally.20 21 The objective of this systematic review was to identify, critique and synthesise the findings of research that has evaluated the effectiveness of RT programmes (where intensity has been defined) on physical return to sport outcome measures. (1) What is the quality of the literature that evaluates the effectiveness of an RT protocol (where intensity has been defined) following ACLR? (2) Does the intensity of RT described in ACLR rehabilitation literature align with recommended guidelines for RT? (3) Is the recommended intensity of RT, as detailed by the literature, sufficient to ensure that postoperative physical deficits are adequately addressed?
Methods
This systematic review was guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist (2009) and registered with PROSPERO (ID: CRD42020136001).
Data sources
A comprehensive search of electronic databases was performed in June 2020. Databases included: EBSCO health databases (CINAHL, MEDLINE, SPORTDiscus), Scopus and Pedro. Two key concepts being ‘anterior cruciate ligament’ and ‘strength training’, and their alternative terms were identified and searched separately (table 1).
Table 1.
Search terms and Boolean operators
| Order of terms searched | Search terms and operators |
| Search 1 (S1) | (ACL OR ‘anterior cruciate ligament’) AND (repair or ‘post-operative’ OR ‘post-operative’ OR surgery OR ‘post-surg*’ OR reconstruction) |
| Search 2 (S2) | (strength* OR resistance OR weight* OR exercise OR intensity OR maximal) N5/W5 (train* OR program* OR protocol*) |
Inclusion/exclusion criteria
Studies were included if they were randomised or non-randomised controlled trials, longitudinal cohort studies or case series, where an adequate description of an RT intervention as a part of an ACLR rehabilitation protocol for 6 weeks or greater was provided. Exercise descriptors deemed necessary included the number of sets and repetitions, the type of exercise and exercise intensity. Articles were excluded if they did not include outcome measures related to common objective return to sport criteria,16 did not report on primary data, were questionnaires and qualitative research, where full texts were not available, and were not published in a peer-reviewed journal or where an English version was not available.
Screening and study selection
Studies titles and then abstracts identified by the search were screened and read by the primary author. Full-text versions of each of these studies were reviewed to determine if the study met the inclusion and exclusion criteria. Reference lists from the identified studies were checked for possible additional studies not identified by the database search. The texts of all remaining articles were subject to quality appraisal and data extraction. Each study included in this systematic review was independently critiqued by the primary author and a second reviewer (both clinical physiotherapists). When all studies had been independently critiqued, the primary author and the second reviewer deliberated on individual results to reach a consensus on final scores.
Study quality appraisal and data extraction
A modified Downs and Black appraisal tool was used to assess the quality of selected articles.23 This tool is sufficiently reliable and valid for determining the methodological quality of randomised controlled trials and non-randomised trials.23 The modified tool has previously been used in other published systematic reviews.16 24–27 The total of the appraisal scores for each study was used to indicate the overall study quality, categorised as follows: poor (14 or below), fair (15–19), good (20–25) and excellent (26–28).24
Results
Study selection
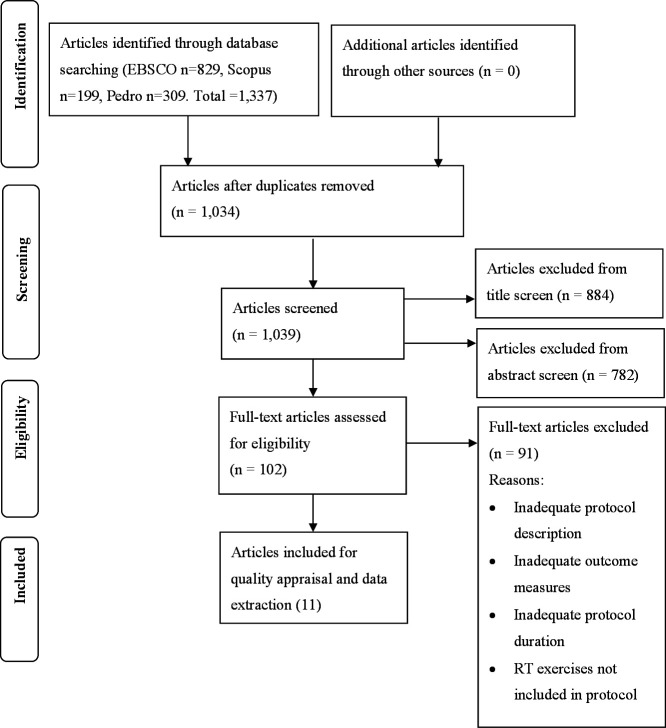
Figure 1 illustrates the process undertaken to select the studies included for quality appraisal and data extraction. The search and screening process identified 11 articles for final quality appraisal and data extraction.
Figure 1.
Search strategy and results. RT, resistance training. (Adapted from Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA), 2009).
Quality of included studies
Studies varied in quality, with scores ranging from 13 to 26 out of a possible 28 (table 2). One study was categorised as excellent quality,28 four studies as good quality,29–32 four studies as fair quality33–36 and two studies as poor quality.37 38 Table 2 shows most studies scored well in reporting objectives, outcome measures, interventions and results. Studies commonly scored poorly on the items related to the inherent difficulties with researching this type of intervention and mainly affected the internal validity, such as a lack of blinding. Other items that were commonly scored poorly among studies affected the generalisability of results, including insufficient power due to a lack of participants, insufficient description of participant characteristics and facilities and equipment used not typically available to the general population.
Table 2.
Downs and Black quality critique
| Studies | Downs and Black item number | |||||||||||||||||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 | Total | |
| Berschin et al29 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 21 |
| Bieler et al30 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 25 |
| Friedmann-Bette et al37 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 13 |
| Fukuda et al28 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 26 |
| Kang et al33 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 15 |
| Kınıklı et al34 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 16 |
| Lepley et al35 | 1 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 15 |
| Perry et al31 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 20 |
| Risberg et al32 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 22 |
| Santos et al38 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 14 |
| Welling et al36 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 15 |
Characteristics of included studies
Extracted data relating specifically to the research question, including RT intensities and the corresponding outcome measures associated with return to sport criteria, are summarised in the online supplemental table 1. Further information regarding the general characteristics of each reviewed study can also be found in the online supplemental table 2.
bmjsem-2021-001144supp001.pdf (58.6KB, pdf)
bmjsem-2021-001144supp002.pdf (69KB, pdf)
RT intensity
Seven of the studies expressed intensity as a percentage of 1RM, ranging from 5 to greater than 80% of 1RM.28 29 32–36 Five studies expressed intensity as a repetition maximum, ranging from 30RM to 6RM (<65% of 1RM–85% of 1RM).28 30 31 37 38 Six of the 11 studies reported interventions progressing in intensity from low to moderate high intensity in a periodised manner throughout the programme.29–32 34 36 The majority of RT interventions were optimised for the development of muscle endurance and hypertrophy between 60% and 80% of 1RM (>15RM–8RM).28–30 32–38 Perry et al’s31 study was the only study to include RT intensities optimised to develop muscle strength (6RM or 85% of 1RM). The RT protocol described by Welling et al36 stated intensities greater than 80% of 1RM in the final rehabilitation phase; however, it did not describe specifics.
Efficacy of interventions
Strength
Strength was measured in all studies except for the study performed by Perry et al.31 The strength of either the quadriceps (knee extensors) or hamstrings (knee flexors) was assessed most commonly with an isokinetic dynamometer. Other measures relating to muscle strength that were evaluated included knee extensor muscle power,30 quadriceps peak torque normalised to body weight36 and extensor and flexor muscle endurance and ‘squat’ strength.33
Seven of the studies measured the LSIs.28–30 32 36–38 Bieler et al30 reported 98% (±4) LSI of the injured leg extensor power in the high-intensity RT group in comparison to 84% (±3) LSI in the low-intensity RT group following the intervention period (20 weeks post-ACLR), a statistically significant difference. Santos et al38 assessed the subjects between 2 and 5 years post-ACLR and reported 111% and 128% quadriceps and hamstring LSIs, respectively, following the intervention, the highest among the included studies.
Quadriceps LSI among the remaining studies ranged from 62% (±18) to 94.1% (±14.6),28 29 32 36 37 while hamstring LSI results ranged from 72% (±11) to 97.9% (±7.5).28 29 32 36 37 Fukuda et al28 and Welling et al36 recorded the highest quadriceps LSI (94.1%±6 and 94.1±14.6) at approximately 6 and 10 months following ACLR, respectively. Welling et al36 also recorded the highest hamstring LSI (97.9%±7.5). It should be noted that the study by Fukuda et al28 included only participants who had undergone an ACLR using a hamstring tendon graft, while Welling et al36 included participants who underwent a hamstring tendon or bone-patellar tendon graft.
Function
A variety of hop tests were used in six of the 11 studies. Bieler et al30 reported 69% (±5) and 75% (±4) LSIs of the affected leg for a single and triple hop test in the high-intensity RT group, and 65% (±5) and 68% (±4) for the same measures in the low-intensity RT group following the intervention; these differences were not statistically significant. The single hop test results ranged from 65% (±5) to 95% (±8).28 30–32 34 38 Results of the triple hop tests varied between 68% (±4) and 94%,30 32 38 and results of the triple cross-over hop tests varied between 79% (±15) and 102%.28 31 38
Two studies reported hop test results and included participants approaching a traditional return to sport period immediately following intervention completion (6 months post-ACLR).28 32 Both intervention groups in the study by Fukuda et al28 achieved greater than 90% LSI or higher for the single hop test (92.3%±8.1 and 94.9±6.7) and cross-over hop tests (94.0±6.4 and 92.5±7.6). Risberg et al32 reported the highest single hop and triple hop test LSI values in the neuromuscular training group (85%±11 and 89%±11, respectively) at 6 months post-ACLR, failing to achieve the return to sport criteria thresholds.
Objectives
Typically, the objectives of each study were focused on determining the effectiveness of different modes of RT, RT protocols or novel adjuncts to rehabilitation programmes against standard rehabilitation protocols, rather than explicitly investigating conventional RT as a cornerstone of the rehabilitation protocol. Only one study30 expressly investigated a high-intensity versus low-intensity RT protocol.
Participants
The mean age of participants across all studies ranged from 22 to 33 years old; the mean age of participants across all studies was 27 years old. Males and females were included in all studies; however, the majority of participants were male. Participants who underwent either a hamstring tendon, quadriceps tendon or patella tendon graft ACLR were represented across studies.
Intervention duration
Intervention duration ranged from 6 to 41 weeks; participants completed two to three sessions per week. Interventions commenced between 1 and 12 weeks postoperatively, except Santos et al38 who included participants between 2 and 5 years following ACLR. The majority of intervention periods were 12 weeks or greater in duration (n=8).28–31 33–36 38 Fukuda et al,28 Risberg et al32 and Welling et al36 represent the most complete rehabilitation protocols of included studies. Interventions commenced 1–2 weeks post-ACLR and were 25 weeks, 6 months and 10 months in duration, respectively. Aspects of the Risberg et al32 and Welling et al’s36 rehabilitation programmes were specifically designed to facilitate a return to sport.
RT effect on graft laxity
Five of the studies reviewed measured arthrometric graft laxity over the course of the intervention.28–32 All studies reported no significant differences in graft laxity between intervention groups or any deleterious increases in joint laxity as a result of the intervention. Furthermore, no studies reported significant injury over the course of the study periods.
Adherence
Three studies specifically described adherence to RT protocols, measured by the number of planned sessions completed. Adherence rates were generally high, between 85% and 100%.29 30 32
Discussion
This systematic review shows the disparity between the intensity of RT protocols found in the ACLR rehabilitation literature and the recommended intensities required for optimal neuromuscular development. Furthermore, it demonstrates the large variances between studies in using RT parameters post-ACLR, particularly the intensity of exercises. Protocols used RT with intensities as low as 50% of 1RM and as high as 85% of 1RM, the latter representing the lower end of the strength development continuum and only constitutes moderate intensity.10 14 39 40 Protocols mostly incorporated RT intensities between 60% and 80% of 1RM in the mid and late stages of rehabilitation, sufficient to develop muscular endurance and stimulate hypertrophy.14 41 42 Two studies incorporated RT that would facilitate the development of maximal force production (strength). Perry et al31 prescribed exercises at 85% of 1RM and Welling et al36 reported prescribing exercises above 80% of 1RM in the final phase of rehabilitation.
RT at the intensities primarily observed in the included studies limits the potential for participants to develop maximal strength.12 14 42 43 Furthermore, these intensities fail to replicate the high physical demands required of a person during return to sport testing and of an athlete performing their sport.43–47 This factor may contribute to the results of the included studies reflecting research that demonstrates ACLR patients often fail to achieve return to sport criteria.3 9 15 28–32 34 37 Welling et al’s36 study was the only study to report a greater than 90% LSI of both hamstring and quadriceps muscle groups among the participants. However, comparison between graft types revealed quadriceps LSI values below 90% for people who underwent a bone-patellar tendon-bone graft at 10 months post-ACLR (98.3%±8.4 and 87.1±12.5 quadriceps LSI for hamstring tendon and bone-patellar tendon-bone grafts, respectively).36 Additionally, no other study reported restoration of strength to 90% LSI or greater of the muscle group from which the ACL graft was harvested. In the case of the person returning to sport following ACLR, it is crucial that these people eventually progress to RT employed by the injury-free population at high intensities (90% of 1RM and greater). This requirement would help to ensure that an adequate level of physical conditioning is achieved to sufficiently prepare the athlete for the rigours of sport.10 11 48–50
Periodisation allows a person to safely and effectively progress the RT protocol to higher intensities and facilitates maximal increases in strength.10 51 However, only five of the 11 studies29–32 36 used some form of linear periodisation, increasing intensity over the training period. The study by Welling et al36 provides the clearest example of periodisation. The RT protocol in this study included four phases and three distinct RT microcycles over 10 months; intensity was progressed from <50% of 1RM (muscle endurance) to between 60% and 80% of 1RM (muscle hypertrophy), and finally to greater than 80% of 1RM (strength) with an emphasis on a fast concentric phase (power). The findings show that RT protocols typically only progressed from intensities optimised to promote muscle endurance to intensities optimised for muscle hypertrophy, without a further progression to strength and power. Inadequate periodisation can hinder the patient’s performance in strength and function testing through a lack of progressive overload, limiting potential improvements.52 Furthermore, RT protocols without periodisation, particularly when training at intensities optimised for hypertrophy, have been suggested to hinder physical performance through overtraining induced physical and/or mental fatigue.12 50 51
In athletic training, periodisation typically builds towards the athlete performing power-based RT.10 The development of power through RT is considered an essential characteristic of an RT protocol as it reflects the demands placed on an athlete’s neuromuscular system during maximal effort tasks.53 Not only is power a defining feature of the hop test battery and agility tests commonly used in return to sport criteria, injury mechanisms typically involve maximal effort tasks that require a high power output.3 15 54 Consequently, the patient must progress to power exercises to facilitate the greatest transfer of training effect.3 14 48 49 54 Welling et al’s36 study was the only study included in this review to incorporate elements of RT that considered the development of power. Although Bieler et al30 acknowledged the importance of power by measuring the effects of the intervention on leg extensor power, the protocol did not include RT optimised for power development. While a superior improvement in leg extensor power in the high-intensity compared with the low-intensity RT group was reported, a difference in hop test performance improvement was not seen.30 The lack of distinction between group’s hop test results may be explained by the RT protocol not progressing to power-based RT to facilitate a cross-over of training effect.
RT has been posited as the most important aspect of a rehabilitation programme following musculoskeletal injury.10 However, rather than focusing on the application of testing foundational elements of RT, ACLR research has focused on novel interventions, accelerated protocols, training adjuncts and different types of RT.28 29 33–35 52 55 The study carried out by Lepley et al35 reflects this sentiment, which demonstrated that the addition of neuromuscular electrical stimulation to a 12-week RT protocol had no affect when comparing it to the RT protocol alone. Although current evidence-based guidelines promote the inclusion of RT from as early as 2 weeks post-ACLR, guidance for the application of RT variables including intensity is not defined.56 More focus should be placed on investigating the foundational elements related to RT, such as exercise intensity, in this population.10 The lack of attention on these elements in the literature reduces the importance of this aspect of ACLR rehabilitation and highlights an area that clinicians can improve.
Clinical practice
The findings of this systematic review include several implications that could affect clinical practice. The inconsistencies in RT protocols highlighted in this review reflect the existing research, which suggests that physiotherapists do not have the required information to develop suitable ACLR rehabilitation protocols.20 21 The variability of current ACLR rehabilitation protocols in clinical practice and concurrent high reinjury rates may be explained by the lack of consistency across rehabilitation protocols used in the literature.18 57 58
A scarcity of literature exists that has investigated the protocols extending beyond 6 months post-ACLR. This is important for clinical practice because strength and function deficits commonly extend well beyond this time frame, suggesting that rehabilitation programmes should continue past this period.3 9 19 22 56 59 At 6 months post-ACLR, the graft progresses through the ligamentisation phase, has undergone considerable structural and biological changes and can tolerate higher external loads.60 Rehabilitation protocols completed before 6 months post-ACLR limit the opportunity to progress RT to higher intensities necessary for adequate physical preparation. The current literature leaves uncertainty for clinicians prescribing late-stage RT, which may be contributing to the discrepancy between clinicians’ expected rehabilitation duration and a return to sport.18 Evidence-based guidelines recommend rehabilitation continues for 9–12 months post-ACLR; however, the lack of literature accurately describing late-stage rehabilitation may be encouraging the premature completion of rehabilitation protocols and a subsequent return to sport.56 59
Fear of damaging the ACL graft may cause clinicians to underprescribe RT intensity. Fears about graft injury, particularly in the early and middle phases of graft healing through poor or aggressive exercise prescription, have historically been a well-debated topic.31 61 Results reported by studies included in this review contribute to the notion that rehabilitation is safe and is not commonly the cause of complications following ACLR. No studies in this review reported serious injury or deleterious increases in graft laxity due to the exercise protocols.28–32 Bieler et al30 provide the most direct reassurance about the safety of higher intensity RT during graft proliferation and early ligamentisation (12 weeks post-ACLR). No difference was found in knee joint laxity between high-intensity and low-intensity RT groups. Furthermore, the study by Perry et al31 prescribed the highest RT intensities (6RM) observed in this review during graft proliferation (from 8 weeks post-ACLR), typically considered to be a vulnerable stage of graft healing,57 and reported no harmful effects to ligament laxity. While other parameters such as exercise type, range of movement and tempo should be considered when determining the safety of an exercise, intensities prescribed up to 6RM have been demonstrated to be safe in the early and middle stages of ACLR rehabilitation.31
Future research recommendations
A future trial should investigate the efficacy of a 12-month, criteria-driven, periodised rehabilitation protocol. The protocol should incorporate foundational RT principles to maximise the cross-over effect, including RT intensities up to or greater than 90% of 1RM and a microcycle focused on power development. The rehabilitation protocol should take place in a standard gym setting and progress towards independent patient-led sessions. Outcome measures should include an accepted return to sport criteria test battery, exercise tolerance (pain and swelling), training volume, adherence, long-term reinjury reporting and level of return to sport achieved.62 Additional research investigating other foundational RT elements, particularly manipulating volume and frequency within a rehabilitation protocol, would provide further information to develop optimal RT programmes following ACLR.
Limitations
The review included studies where RT was not the primary variable being investigated. Because of this, the authors may have placed a reduced emphasis on the RT component of the protocol. The RT intensity used in these protocols may not be as applicable compared with the interventions that investigated RT as a primary variable. Furthermore, the specific outcome measures and interpretation of results were not used as inclusion criteria in this systematic review. This issue limited the ability to directly compare RT intensities and the efficacy of protocols between studies. Statistical analysis of the extracted data, such as analysing the relationship between RT intensity and outcome, was out of the scope of this systematic review. However, this could provide valuable information regarding the optimal prescription of RT intensity post-ACLR.
Conclusion
This systematic review highlights an area of ACLR rehabilitation that merits more high-quality research so that physiotherapists are better equipped to manage the patients successfully. There is currently no universally accepted best practice guideline for the prescription of RT following ACLR despite RT being a cornerstone of rehabilitation. Available literature detailing RT intensity within ACLR protocols is inconsistent, incomplete and mostly not aligned with recommended RT principles. Optimisation of the prescription of RT for people following ACLR could lead to improvements in strength and functional outcomes and possibly reduce reinjury rates. Recent ACLR rehabilitation research incorporating RT principles and emphasising the importance of RT has provided promising results; however, further research is required to develop guidelines to improve clarity, and in particular, to identify optimal RT variables in this population.
Acknowledgments
I would like to extend a sincere thank you to my supervisors DOB and SGW. Their sharing of expertise and their support, input and guidance throughout this project have been generous and invaluable. A thank you must also be extended to my work colleague Julia Wilkinson who enthusiastically completed a quality critique of all of the studies included in the systematic review while working full time as a clinical physiotherapist. Finally, Dr Jennifer Baldwin (Casual Academic, Priority Research Centre in Physical Activity and Nutrition, Faculty of Health and Medicine, University of Newcastle, Australia) provided much appreciated assistance in editing and proofreading (service provided for a fee).
Footnotes
Twitter: @zakwnichols
Contributors: ZWN designed and conceptualised the review, collected the data, analysed the results, and drafted and revised the paper. He is the guarantor of the study. DOB and SGW contributed to the study design and provided supervision over and revised the paper.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Zbrojkiewicz D, Vertullo C, Grayson JE. Increasing rates of anterior cruciate ligament reconstruction in young Australians, 2000-2015. Med J Aust 2018;208:354–8. 10.5694/mja17.00974 [DOI] [PubMed] [Google Scholar]
- 2.Edwards PK, Ebert JR, Joss B, et al. Patient characteristics and predictors of return to sport at 12 months after anterior cruciate ligament reconstruction: the importance of patient age and postoperative rehabilitation. Orthop J Sports Med 2018;6:2325967118797575. 10.1177/2325967118797575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grindem H, Snyder-Mackler L, Moksnes H, et al. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med 2016;50:804–8. 10.1136/bjsports-2016-096031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hewett TE, Di Stasi SL, Myer GD. Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am J Sports Med 2013;41:216–24. 10.1177/0363546512459638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Panariello R, Stump T, Allen A. Rehabilitation and return to play following anterior cruciate ligament reconstruction. Operative Techniques in Sports Medicine 2017;25:181–93. [Google Scholar]
- 6.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med 2010;38:1968–78. 10.1177/0363546510376053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med 2009;37:246–51. 10.1177/0363546508325665 [DOI] [PubMed] [Google Scholar]
- 8.Webster KE, Feller JA. Exploring the high reinjury rate in younger patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med 2016;44:2827–32. 10.1177/0363546516651845 [DOI] [PubMed] [Google Scholar]
- 9.Leister I, Kulnik ST, Kindermann H, et al. Functional performance testing and return to sport criteria in patients after anterior cruciate ligament injury 12-18 months after index surgery: a cross-sectional observational study. Phys Ther Sport 2019;37:1–9. 10.1016/j.ptsp.2019.01.010 [DOI] [PubMed] [Google Scholar]
- 10.Lorenz DS, Reiman MP, Walker JC. Periodization: current review and suggested implementation for athletic rehabilitation. Sports Health 2010;2:509–18. 10.1177/1941738110375910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoover DL, VanWye WR, Judge LW. Periodization and physical therapy: bridging the gap between training and rehabilitation. Phys Ther Sport 2016;18:1–20. 10.1016/j.ptsp.2015.08.003 [DOI] [PubMed] [Google Scholar]
- 12.Kraemer W, Fleck S. A review: factors in exercise prescription of resistance training. J Strength Cond 1988;10:36–41. [Google Scholar]
- 13.Goff AJ, Page WS, Clark NC. Reporting of acute programme variables and exercise descriptors in rehabilitation strength training for tibiofemoral joint soft tissue injury: a systematic review. Phys Ther Sport 2018;34:227–37. 10.1016/j.ptsp.2018.10.012 [DOI] [PubMed] [Google Scholar]
- 14.Potter S. Review of the literature. guidelines for resistance training for Australian rules football. JASC 2016;24:59–68. [Google Scholar]
- 15.Kyritsis P, Bahr R, Landreau P, et al. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med 2016;50:946–51. 10.1136/bjsports-2015-095908 [DOI] [PubMed] [Google Scholar]
- 16.Losciale JM, Zdeb RM, Ledbetter L, et al. The association between passing return-to-sport criteria and second anterior cruciate ligament injury risk: a systematic review with meta-analysis. J Orthop Sports Phys Ther 2019;49:43–54. 10.2519/jospt.2019.8190 [DOI] [PubMed] [Google Scholar]
- 17.Ebert JR, Webster KE, Edwards PK, et al. Current perspectives of Australian therapists on rehabilitation and return to sport after anterior cruciate ligament reconstruction: A survey. Phys Ther Sport 2019;35:139–45. 10.1016/j.ptsp.2018.12.004 [DOI] [PubMed] [Google Scholar]
- 18.Greenberg EM, Greenberg ET, Albaugh J, et al. Rehabilitation practice patterns following anterior cruciate ligament reconstruction: a survey of physical therapists. J Orthop Sports Phys Ther 2018;48:801–11. 10.2519/jospt.2018.8264 [DOI] [PubMed] [Google Scholar]
- 19.Toole AR, Ithurburn MP, Rauh MJ, et al. Young athletes cleared for sports participation after anterior cruciate ligament reconstruction: how many actually meet recommended return-to-sport criterion cutoffs? J Orthop Sports Phys Ther 2017;47:825–33. 10.2519/jospt.2017.7227 [DOI] [PubMed] [Google Scholar]
- 20.von Aesch AV, Perry M, Sole G. Physiotherapists' experiences of the management of anterior cruciate ligament injuries. Phys Ther Sport 2016;19:14–22. 10.1016/j.ptsp.2015.08.004 [DOI] [PubMed] [Google Scholar]
- 21.Makhni EC, Crump EK, Steinhaus ME, et al. Quality and variability of online available physical therapy protocols from academic orthopaedic surgery programs for anterior cruciate ligament reconstruction. Arthroscopy 2016;32:1612–21. 10.1016/j.arthro.2016.01.033 [DOI] [PubMed] [Google Scholar]
- 22.Welling W, Benjaminse A, Seil R, et al. Low rates of patients meeting return to sport criteria 9 months after anterior cruciate ligament reconstruction: a prospective longitudinal study. Knee Surg Sports Traumatol Arthrosc 2018;26:3636–44. 10.1007/s00167-018-4916-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 1998;52:377–84. 10.1136/jech.52.6.377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hooper P, Jutai JW, Strong G, et al. Age-related macular degeneration and low-vision rehabilitation: a systematic review. Can J Ophthalmol 2008;43:180–7. 10.3129/i08-001 [DOI] [PubMed] [Google Scholar]
- 25.Irving DB, Cook JL, Menz HB. Factors associated with chronic plantar heel pain: a systematic review. J Sci Med Sport 2006;9:11–22. 10.1016/j.jsams.2006.02.004 [DOI] [PubMed] [Google Scholar]
- 26.Mosler AB, Agricola R, Weir A, et al. Which factors differentiate athletes with hip/groin pain from those without? A systematic review with meta-analysis. Br J Sports Med 2015;49:810. 10.1136/bjsports-2015-094602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Munn J, Sullivan SJ, Schneiders AG. Evidence of sensorimotor deficits in functional ankle instability: a systematic review with meta-analysis. J Sci Med Sport 2010;13:2–12. 10.1016/j.jsams.2009.03.004 [DOI] [PubMed] [Google Scholar]
- 28.Fukuda TY, Fingerhut D, Moreira VC, et al. Open kinetic chain exercises in a restricted range of motion after anterior cruciate ligament reconstruction: a randomized controlled clinical trial. Am J Sports Med 2013;41:788–94. 10.1177/0363546513476482 [DOI] [PubMed] [Google Scholar]
- 29.Berschin G, Sommer B, Behrens A, et al. Whole body vibration exercise protocol versus a standard exercise protocol after ACL reconstruction: a clinical randomized controlled trial with short term follow-up. J Sports Sci Med 2014;13:580–9. [PMC free article] [PubMed] [Google Scholar]
- 30.Bieler T, Sobol NA, Andersen LL, et al. The effects of high-intensity versus low-intensity resistance training on leg extensor power and recovery of knee function after ACL-reconstruction. Biomed Res Int 2014;2014:1–11. 10.1155/2014/278512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Perry MC, Morrissey MC, King JB, et al. Effects of closed versus open kinetic chain knee extensor resistance training on knee laxity and leg function in patients during the 8- to 14-week post-operative period after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2005;13:357–69. 10.1007/s00167-004-0568-7 [DOI] [PubMed] [Google Scholar]
- 32.Risberg MA, Holm I, Myklebust G, et al. Neuromuscular training versus strength training during first 6 months after anterior cruciate ligament reconstruction: a randomized clinical trial. Phys Ther 2007;87:737–50. 10.2522/ptj.20060041 [DOI] [PubMed] [Google Scholar]
- 33.Kang H, Jung J, Yu J. Comparison of strength and endurance between open and closed kinematic chain exercises after anterior cruciate ligament reconstruction: randomized control trial. J. Phys. Ther 2012;24:1055–7. [Google Scholar]
- 34.Kınıklı GI, Yüksel I, Baltacı G, et al. The effect of progressive eccentric and concentric training on functional performance after autogenous hamstring anterior cruciate ligament reconstruction: a randomized controlled study. Acta Orthop Traumatol Turc 2014;48:283–9. 10.3944/AOTT.2014.13.0111 [DOI] [PubMed] [Google Scholar]
- 35.Lepley LK, Wojtys EM, Palmieri-Smith RM. Combination of eccentric exercise and neuromuscular electrical stimulation to improve quadriceps function post-ACL reconstruction. Knee 2015;22:270–7. 10.1016/j.knee.2014.11.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Welling W, Benjaminse A, Lemmink K, et al. Progressive strength training restores quadriceps and hamstring muscle strength within 7 months after ACL reconstruction in amateur male soccer players. Phys Ther Sport 2019;40:10–18. 10.1016/j.ptsp.2019.08.004 [DOI] [PubMed] [Google Scholar]
- 37.Friedmann-Bette B, Profit F, Gwechenberger T, et al. Strength training effects on muscular regeneration after ACL reconstruction. Med Sci Sports Exerc 2018;50:1152–61. 10.1249/MSS.0000000000001564 [DOI] [PubMed] [Google Scholar]
- 38.Santos HH, Sousa CdeO, Medeiros CLP, et al. Correlation between eccentric training and functional tests in subjects with reconstructed ACL. Revista Brasileira de Medicina do Esporte 2018;24:471–6. 10.1590/1517-869220182406184218 [DOI] [Google Scholar]
- 39.González-Badillo JJ, Izquierdo M, Gorostiaga EM. Moderate volume of high relative training intensity produces greater strength gains compared with low and high volumes in competitive weightlifters. J Strength Cond Res 2006;20:73–81. 10.1519/R-16284.1 [DOI] [PubMed] [Google Scholar]
- 40.Fry AC. The role of resistance exercise intensity on muscle fibre adaptations. Sports Med 2004;34:663–79. 10.2165/00007256-200434100-00004 [DOI] [PubMed] [Google Scholar]
- 41.Toigo M, Boutellier U. New fundamental resistance exercise determinants of molecular and cellular muscle adaptations. Eur J Appl Physiol 2006;97:643–63. 10.1007/s00421-006-0238-1 [DOI] [PubMed] [Google Scholar]
- 42.Schoenfeld BJ. Is there a minimum intensity threshold for resistance training-induced hypertrophic adaptations? Sports Med 2013;43:1279–88. 10.1007/s40279-013-0088-z [DOI] [PubMed] [Google Scholar]
- 43.Cormie P, McGuigan MR, Newton RU. Adaptations in athletic performance after ballistic power versus strength training. Med Sci Sports Exerc 2010;42:1582–98. 10.1249/MSS.0b013e3181d2013a [DOI] [PubMed] [Google Scholar]
- 44.Gonzalo-Skok O, Tous-Fajardo J, Arjol-Serrano JL, et al. Improvement of repeated-sprint ability and horizontal-jumping performance in elite young basketball players with low-volume repeated-maximal-power training. Int J Sports Physiol Perform 2016;11:464–73. 10.1123/ijspp.2014-0612 [DOI] [PubMed] [Google Scholar]
- 45.Jensen R, Ebben W. Knee function, strength and resumption of preinjury sports participation in young athletes following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 2007;49:145–53. [DOI] [PubMed] [Google Scholar]
- 46.Lamont HS, Cramer JT, Bemben DA, et al. Effects of 6 weeks of periodized squat training with or without whole-body vibration on short-term adaptations in jump performance within recreationally resistance trained men. J Strength Cond Res 2008;22:1882–93. 10.1519/JSC.0b013e3181821a1a [DOI] [PubMed] [Google Scholar]
- 47.Tramel W, Lockie RG, Lindsay KG, et al. Associations between absolute and relative lower body strength to measures of power and change of direction speed in division II female Volleyball players. Sports 2019;7:160. 10.3390/sports7070160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cormie P, McGuigan MR, Newton RU. Developing maximal neuromuscular power: part 2 - training considerations for improving maximal power production. Sports Med 2011;41:125–46. 10.2165/11538500-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 49.DeWeese BH, Hornsby G, Stone M. The training process: planning for strength–power training in track and field. Part 2: practical and applied aspects. J Sport Health Sci 2015;4:318–24. [Google Scholar]
- 50.Stone M, O’Bryant H, Garhammer J. A theoretical model of strength training. Natl Strength Condit Assoc J 1982;4:36–9. [Google Scholar]
- 51.Strohacker K, Fazzino D, Breslin WL, et al. The use of periodization in exercise prescriptions for inactive adults: a systematic review. Prev Med Rep 2015;2:385–96. 10.1016/j.pmedr.2015.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Beynnon BD, Johnson RJ, Naud S, et al. Accelerated versus nonaccelerated rehabilitation after anterior cruciate ligament reconstruction: a prospective, randomized, double-blind investigation evaluating knee joint laxity using roentgen stereophotogrammetric analysis. Am J Sports Med 2011;39:2536–48. 10.1177/0363546511422349 [DOI] [PubMed] [Google Scholar]
- 53.Cormie P, McGuigan MR, Newton RU. Developing maximal neuromuscular power: Part 1--biological basis of maximal power production. Sports Med 2011;41:17–38. 10.2165/11537690-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 54.Wetters N, Weber AE, Wuerz TH. Mechanism of injury and risk factors for anterior cruciate ligament injury. Oper Tech Sports Med 2016;24:2–6. [Google Scholar]
- 55.Ohta H, Kurosawa H, Ikeda H, et al. Low-load resistance muscular training with moderate restriction of blood flow after anterior cruciate ligament reconstruction. Acta Orthop Scand 2003;74:62–8. 10.1080/00016470310013680 [DOI] [PubMed] [Google Scholar]
- 56.van Melick N, van Cingel REH, Brooijmans F, et al. Evidence-Based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med 2016;50:1506–15. 10.1136/bjsports-2015-095898 [DOI] [PubMed] [Google Scholar]
- 57.Ardern CL, Taylor NF, Feller JA, et al. Sports participation 2 years after anterior cruciate ligament reconstruction in athletes who had not returned to sport at 1 year: a prospective follow-up of physical function and psychological factors in 122 athletes. Am J Sports Med 2015;43:848–56. 10.1177/0363546514563282 [DOI] [PubMed] [Google Scholar]
- 58.Webster KE, Feller JA, Leigh WB, et al. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med 2014;42:641–7. 10.1177/0363546513517540 [DOI] [PubMed] [Google Scholar]
- 59.Ebert JR, Edwards P, Yi L, et al. Strength and functional symmetry is associated with post-operative rehabilitation in patients following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2018;26:2353–61. 10.1007/s00167-017-4712-6 [DOI] [PubMed] [Google Scholar]
- 60.Scheffler SU, Unterhauser FN, Weiler A. Graft remodeling and ligamentization after cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2008;16:834–42. 10.1007/s00167-008-0560-8 [DOI] [PubMed] [Google Scholar]
- 61.Noehren B, Snyder-Mackler L. Who's afraid of the big bad wolf? open-chain exercises after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 2020;50:473–5. 10.2519/jospt.2020.0609 [DOI] [PubMed] [Google Scholar]
- 62.Ardern CL, Glasgow P, Schneiders A, et al. 2016 consensus statement on return to sport from the first world Congress in sports physical therapy, Bern. Br J Sports Med 2016;50:853–64. 10.1136/bjsports-2016-096278 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjsem-2021-001144supp001.pdf (58.6KB, pdf)
bmjsem-2021-001144supp002.pdf (69KB, pdf)