Abstract
Introduction
Domestic violence and abuse (DVA) is prevalent, harmful and more dangerous among diaspora communities because of the difficulty accessing DVA services, language and migration issues. Consequently, migrant/refugee women are common among primary care populations, but evidence for culturally competent DVA primary care practice is negligible. This pragmatic cluster randomised controlled trial aims to increase DVA identification and referral (primary outcomes) threefold and safety planning (secondary outcome) among diverse women attending intervention vs comparison primary care clinics. Additionally, the study plans to improve recording of DVA, ethnicity, and conduct process and economic evaluations.
Methods and analysis
Recruitment of ≤28 primary care clinics in Melbourne, Australia with high migrant/refugee communities. Eligible clinics need ≥1 South Asian general practitioner (GP) and one of two common software programmes to enable aggregated routine data extraction by GrHanite. Intervention staff undertake three DVA training sessions from a GP educator and bilingual DVA advocate/educator. Following training, clinic staff and DVA affected women 18+ will be supported for 12 months by the advocate/educator. Comparison clinics are trained in ethnicity and DVA data entry and offer routine DVA care. Data extraction of DV identification, safety planning and referral from routine GP data in both arms. Adjusted regression analysis by intention-to-treat by staff blinded to arm. Economic evaluation will estimate cost-effectiveness and cost–utility. Process evaluation interviews and analysis with primary care staff and women will be framed by Normalisation Process Theory to maximise understanding of sustainability. Harmony will be the first primary care trial to test a culturally competent model for the care of diverse women experiencing DVA.
Ethics and dissemination
Ethical approval from La Trobe University Human Ethics Committee (HEC18413) and dissemination by policy briefs, journal articles and conference and community presentations.
Trial registration number
ANZCTR- ACTRN12618001845224; Pre-results.
Keywords: primary care, preventive medicine, public health
Strengths and limitations of this study.
First domestic violence and abuse (DVA) study specifically co-designed with ethno-specific DVA agencies and communities and piloted for culturally competent practice in primary care.
Based on three previous successful DVA trials in primary care, with one intervention (Identification and Response to Improve Safety) being scaled up across the UK, one intervention (WEAVE) being rolled out across Australia and MOSAIC (Mothers’ Advocates in the Community) planned for rollout in Peru.
All general practitioner clinics (in both arms) trained for improved and easier recording of domestic violence and ethnicity in routine computer software.
Currently, no rigorous way to accurately identify migrant/refugee patients in primary care.
Recruitment and practice is affected by the COVID-19 epidemic.
Introduction
Domestic violence and abuse (DVA), especially intimate partner violence (IPV) affects at least one in three women globally and one in six Australian women.1 2 It can be defined as behaviour by an intimate partner or ex-partner that causes physical, sexual or psychological harm, including aggression, sexual coercion and psychological abuse and controlling behaviours.3 While IPV is the most common form of DVA, other family members, for example, in-laws, can significantly contribute to the abuse. DVA has a particularly damaging effect on women’s mental as well as physical and reproductive health.1 Women victim survivors experience higher rates of health problems, compared with non-affected women, including: physical injuries, chronic pain, post-traumatic stress disorder (PTSD), depression and anxiety, unplanned pregnancies, gynaecological trauma and death.4 In 2014–2015, almost two Australian women a week were murdered by an intimate partner.5
Australia is a culturally and linguistically diverse society with 28% of the population born overseas and almost 50% from a migrant or refugee background.6 Migrant and refugee families are often impacted by a multitude of intersectional barriers that impact their experience, particularly of DVA.7 They can face significant hurdles to good mental health and safety—racism, lack of knowledge about Australian systems and services, and the broader challenges of acculturation. Furthermore, rigid cultural norms, stereotyped gender roles, visa limitations and fear of authorities can impact on migrant and refugee community’s ability to engage with service providers.8
In countries where war or social upheaval has recently taken place; few sanctions against DVA exist; and where women have no access to sanctuary, either as refuge or family support, rates of DVA are high.9 Such countries, including South Asia (SA) countries, represent significant diaspora communities, especially those with young families. Women in these countries report poorer mental health, obstetric and child health outcomes than the non-abused women in their countries.10 11
Risk factors and approaches to DVA among diaspora communities
Surveys of DVA among diaspora communities are few. While none have random samples and use differing samples and measurement tools, some have found similar DVA rates to those in countries of origin.8 12 Common risks for IPV include low education and employment status and perpetrator alcohol abuse, but migrant and refugee women experience additional risks with poor knowledge of rights and services.13 14 An effective and acknowledged strategy to reach victims and families is the use of bicultural workers.15
In Victoria, Australia, women from SA (India, Pakistan, Bangladesh, Nepal and Sri Lanka) comprise the largest group of migrants with young families and are disproportionately represented in DVA agency data.16 With the resulting social isolation, combined with little or no knowledge of available supports, language barriers and different cultural norms, migrant and refugee women experiencing DVA can be at great risk of serious harm and femicide.17 18
Domestic violence and interventions in primary care
Due to greater ill health, victims and their children are over-represented in clinical settings compared with the general community.19 There is a dearth of evidence for effective DVA interventions in primary care settings.20 No DVA intervention studies in primary care have specifically addressed the cultural competency of clinicians. Primary healthcare providers are often the only contact with a healthcare professional for a woman who is experiencing DVA.19 It is common for symptoms of abuse to go unrecognised by healthcare providers.20 Primary healthcare providers are uniquely placed to identify DVA and provide support.
Evidence for effective primary healthcare interventions and expert DVA advocacy
HARMONY has been adapted from three cluster randomised controlled trials of DVA in general practices19 21 22 but drew most heavily in design from the IRIS (Identification and Response to Improve Safety) study, the approach of which is described in detail below. We enhanced the IRIS model with understanding about primary care cultural competency23 and with parts of the WEAVE intervention model.19 The WEAVE trial incorporated brief motivational counselling for women at different levels of readiness that reduced depression and increased general practitioner (GP) safety discussions.19 We felt that migrant/refugee women would require GP support to build confidence and discuss safety before they are ready to act on a referral.
We built on GP DVA training from all three trials.18, 20,22
The IRIS general practice systems model
IRIS is a system-level GP DVA intervention in the UK.21 IRIS aimed to improve DVA identification, documentation and management in primary care and referral rates to specialist DVA agencies. It consisted of joint training for all clinicians by GP trainers and advocates, and sustained support from an advocate. Advocates supported women who experienced DVA and aimed to empower them, increase their safety and link them and their children to community support services. The trial showed a threefold increase for documented disclosures risk ratio (RR) 3.1 (95% CI 2.2 to 4.3) and sixfold for referrals RR 6.43 (95% CI 4.15 to 9.97) documented by specialist agencies compared with clinics offering usual care.
Patient and public involvement
No patient involved.
Feasibility study
HARMONY was developed in consultation with migrant/refugee non-government organisations (NGOs) and communities.
It was piloted in 2015 for 4 months with two intervention and two comparison clinics in north-west metropolitan Melbourne. The feasibility study successfully trialled recruitment, DVA culturally competent training and the use of GrHanite, a specially designed GP data software programme. To date, there has been no way to routinely monitor trends in identification nor any form of DVA GP management in Australia. The University of Melbourne has developed GrHanite, a software tool designed to extract data ethically for research with a specific capability to interface with the majority of GP computer systems in use in Australia. HARMONY has developed and is further testing GrHanite for routine DVA and ethnicity data collection.
Pilot study results (unpublished) demonstrated HARMONY effectiveness, with 13 referrals to In Touch (Multicultural agency against family violence (FV)) from the intervention clinics compared with 0 in the comparison clinics. These results were sufficiently encouraging to lead to this more rigorous study.
Study design, aims and objectives
HARMONY is designed as a pragmatic (parallel group) cluster-randomised controlled trial with GP clinics as the units of cluster and no stopping rules. HARMONY will test a GP clinic system intervention (IRIS) for effectiveness in Australian primary care.
Specifically, HARMONY aims primarily to (1) Increase (A) GP identification and (B) referral of DVA among all women aged 18+ in intervention versus comparison clinics.
This will be measured (A) by extracting routine GP data on identification and referrals, and (B) compared with referrals received by InTouch Multicultural Centre for Family Violence in both arms. We will explore the rate among migrant/refugee (especially South Asian women).
HARMONY’s secondary aims are to (2) Increase GP safety planning for DVA among women aged 18+ in intervention compared with comparison clinics. This will be measured by extracting routine GP data. We will explore the rate among migrant/refugee (especially South Asian women); (3) Determine the cost-effectiveness of the intervention relative to usual care and (4) Investigate the factors that enable practice change and sustainability.
Methods and analysis
Study setting
The HARMONY study is located in GP clinics located in the North West and South Eastern suburbs of Melbourne, Australia where the highest proportions of South Asian communities are located.
Eligibility criteria
Inclusion criteria: To be eligible, GP clinics must (A) have ≥1 South Asian bilingual/bicultural GPs and (B) use either of the two most common GP medical software programmes in Australia (Medical Director or Best Practice) and agree to have anonymised data extraction by the GrHanite software program from computerised medical records.
Exclusion criteria: clinics outside these regions, those without any South Asian GPs, and whose medical software is neither of the two most common programmes.
Interventions
Clinics randomised into the HARMONY intervention arm will receive:
Clinic training with an emphasis on cultural competency
We are providing culturally competent DVA training, whose original adult learning programme components were tested through our previous trials in general practice.19 21 22 Together with migrant/refugee agencies, we adapted these to emphasise culturally safe practice. Content also drew on recommendations from the WHO guidelines,3 and Canadian trauma informed care guidelines.24 This manualised programme includes offering clinicians culturally competent training to: identify DVA symptoms; ask and respond sensitively to all, but especially migrant/refugee women; motivational interviewing; develop women-centred goals appropriate to women’s readiness to make change; trauma-informed care; discuss safety strategies; document both ethnicity and DVA accurately on GP routine software; and to warmly refer women to support services. Training also includes how to refer affected children (and abusive partners) to available services. All intervention administrative staff will be trained about patient safety and confidentiality, supportive responses and culturally safe clinic environments.
An important aspect of the training is the co-facilitation by a GP educator and a bilingual/bicultural South Asian DVA advocate/educator, based with and managed by an immigrant women’s domestic violence service.16 The programme is now delivered fully online (See protocol amendment below altered because of COVID-19) with one 90 min session for all staff focused on whole clinic practice and two 90 min clinical sessions, delivered four to 8 weeks apart. Key features of the educational programme include: clinical audit with feedback, online modules and prereading; interactive reflective exercises on active listening and attitudes; role play simulation and case discussions; use of survivor voices in videosand a practice readiness checklist. This programme, (accruing quality assurance points for the clinician) will be further reinforced by opportunities over the intervention year for two teleconference/webinar case discussions. One clinician per practice, self-selecting or chosen by staff during training to be the formal ‘practice champion’ will maintain discussion about DVA in the clinic and liaise with the DVA advocate. The intervention commences after the first training session.
HARMONY bilingual bicultural DVA advocate/educator
A South Asian advocate/educator is recruited, employed by and located with our partner agency InTouch, Multicultural Centre Against Family Violence. The advocate/educator will continue to provide support throughout the year long intervention (commencing immediately after the first training and for twelve months) through:
Fortnightly visits or zoom calls with intervention GP clinics for secondary consultations and to provide feedback at clinic meetings.
Providing standard DVA casework for all migrant/refugee women 18+ referred to In Touch from Harmony intervention clinics and referral on to other services for those not migrant/refugee women.
Provide ad hoc secondary phone consultation with intervention clinicians about patient cases and referral.
Accurately record and feedback casework data on referral rates to intervention practices.
Comparison
Comparison clinics will receive half an hour of online training and reminder newsletters to better document ethnicity and DVA outcomes in routine software. They will continue to offer routine GP care for any DVA patients they see. At the end of the 12-month intervention, comparison clinics will be offered the full training programme. They will not receive the specialised advocate/educator support.
Outcomes
Primary outcomes
(1) Recorded identification of DVA among active female patients aged ≥18 years on routine GP software in intervention versus comparison clinics. The denominator for this outcome and the one below will be the number of all active female patients ≥18 in the same time period.
(2) Number of referrals of all affected active female patients 18≥recorded on routine GP software and those recorded as received by InTouch from intervention clinics versus comparison clinics. N.B. We have also asked clinicians to record referrals to other FV agencies and expect that while women will be referred elsewhere, this will either be randomly spread or in greater proportions in intervention clinics as the Harmony training manual lists other FV agencies.
We do not plan an adjustment for multiple outcomes.
Secondary outcomes
(3) Recorded safety planning of all affected active female patients by GPs in intervention clinics compared with comparison clinics among active female patients ≥18 experiencing DVA. Anonymised routine data for DVSP will be collected from medical records using the GrHanite software tool.
Currently, there is no way to record Safety planning in routine GP software. Consequently, we have designed and specified that GPs record DVSP as a safety planning code in the Diagnosis or Reason for visit in Today’s notes sections. GPs in both arms of the study have been asked to do this.
(4) Economic evaluation will estimate cost-effectiveness and cost–utility. Cost-effectiveness will be computed from a provider perspective (cost of the intervention per case of DVA identified, and the cost per woman referred to a DVA advocate). Data on the number of consultations, length and type of consultation will be imputed through extraction via the GrHanite tool. Following the approach taken in the economic evaluation of IRIS, we will then extend the cost-effectiveness analysis to report a cost–utility analysis. This will require a Markov model, estimating longer term impacts of the intervention on both service use and health outcomes. Probabilistic sensitivity analysis will be used to explore the impact of uncertainty on the results. These costs will predominantly be collected using our own study-specific forms.
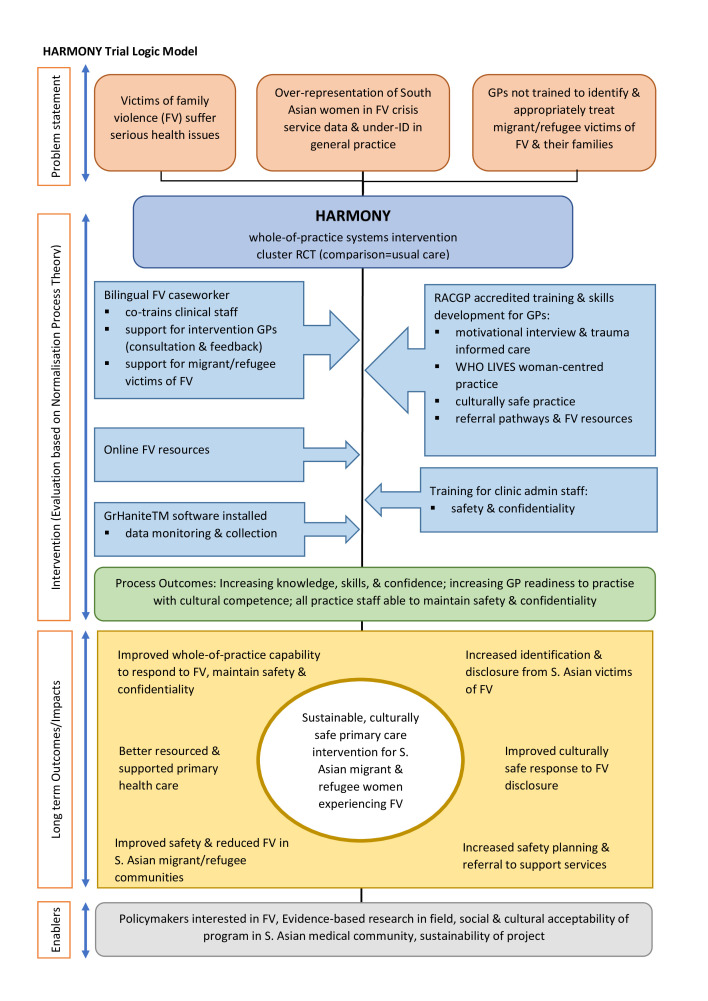
The programme logic of the study and its hypotheses are represented below in figure 1.
Figure 1.
HARMONY programme logic model (see attachment). GP, general practitioner.
Timelines
Recruitment was completed at the end of October 2020. All first training sessions and all comparison clinic training sessions were completed by the end of April 2021.
Primary outcomes of identification, referrals and safety planning will be extracted from routine data from December 2018 to December 2019 for baseline (prior to any training and to COVID-19), 6 months from each clinic’s commencement date (following session 1), 12 months (intervention completion) and 15 months following completion of each clinic’s first training session. Intervention in the majority of clinics will be completed by the end of 2021.
Sample size
Unfortunately, because of unreliable routine GP data collection on ethnicity, language or culture, there is no accurate way to sample only South Asian patients. We have, therefore, powered the study on all women and recruited only among clinics in areas of high South Asian patient populations and with one or more South Asian GPs. We outline below, how we are estimating the South Asian patient populations among each clinic and what the limitations of these estimates will be.
Based on our own feasibility study and IRIS outcomes,21 we estimate that the rate of DVA identification among all female patients will be five women per 1000 female patients in the comparison arm. To detect an increase in the identification or referral rate to 20 women per 1000 with 80% power and a significance level of 5%, 873 person-years per arm is required for individual randomisation. This sample size was inflated to account for the cluster design; assuming an intracluster coefficient of 0.01, and any cluster size from 2000 to 3000 person-years per clinic (based on conservative mean size of the GP female populations in our feasibility study). With these estimations, we require 28 clinics (allowing for a 21% drop-out to 22 clusters).
Recruitment
To identify eligible clinics in communities with high South Asian populations, we first asked the state government partner to identify postcodes with the highest Indian populations and also consulted SA community organisations. HARMONY staff examined online website clinic data to identify GPs with SA names in relevant regions, and from the Melbourne and Monash Universities’ GP research networks and Primary Health Networks. We then faxed or emailed letters of invitation to all identified practices, followed by a phone call and an in person visit to further explain the study. Clinics that agreed to participate completed a Memorandum of Understanding (online supplemental file 1) and permission to install GrHanite. Following the GrHanite agreement, the software was installed. Data from GPs will be collected, but those from nurses, psychologists and other allied health clinicians will not be extracted but may be among clinicians referring to InTouch.
bmjopen-2020-046431supp001.pdf (400.7KB, pdf)
Randomisation and allocation concealment
On recruitment of ≥10 clinics and GrHanite installation, a statistician (blind to assigned group) enters the list into a computer minimisation programme including a random component and allocates clinics to group A or B. Recruitment continues in blocks of 4 or more. Clinics are incrementally randomised in the same way until ≤28 are randomised. Clinics are randomised stratified1: for size of practice—small ≤5 doctors and large six or more and2 SEIFA index for clinic postcode (1–5 classified as ‘lower’ and six or more as ‘higher’) and3 by location, where an equal number and size of clinic are assigned to the intervention (≤7 each for NW and SE) and comparison arms (≤7 each for NW and SE). Clinics are allocated and informed of their status by unblinded staff.
Blinding
HARMONY investigators, GrHanite staff and statisticians are blinded to the randomisation outcome of clinics. Harmony administration staff cannot be blinded to clinic status, as they are required to coordinate training in both arms of the study. Clinic staff are therefore not blinded either.
Data collection
GrHanite has been designed by University of Melbourne to help manage data acquisition for audit, research and health surveillance conforming to the highest standards of ethics, confidentiality and security. Prior to training, information technology technical staff will install GrHanite within the clinic. GPs and all staff in both arms of the study are taught to enter country of birth and language spoken at home. GPs will record when DVA is disclosed (DV), when they discussed safety (DVSP) and whether they have made a referral (DVREF) and to whom.
GrHanite identifies all active female patients (three or more visits in the last 2 years) to identify eligible patients for the denominator.25 GrHanite will extract deidentified anonymised data at regular intervals to the statistician throughout the intervention period and for 3 months after the intervention finishes. At installation, GrHanite will extract historical data (from December 2018 to December 2019) from all recruited GP clinics, excluding patient identifiers (anonymised). These will be baseline data (to exclude any impact of pre-Covid training) when compared with data collected during and after the intervention. Data on recorded referrals, DVA identification, patient sex, age, ethnicity, country of birth and language spoken at home will be extracted from clinic records in both study arms and forwarded to a confidential database managed by a statistician blinded to trial arm status, for cleaning and monitoring purposes.
Identification of SA women
South Asia (SA) comprises a diverse range of populations with a plethora of naming practices. We collected the surnames/family names used in India, Nepal, Afghanistan, Sri-Lanka, Pakistan, and Bangladesh. Staff began with a list of South Asian names provided from the InTouch database. BP (who is Nepalese) compiled an extensive list of Nepalese surnames, then using a range of web-based and informal approaches developed an extensive list of other SA surnames. They also sourced extensive lists from Forebears, an online database of surnames and genealogy information. They then consulted formal organisations (consulates, embassies and ethnic community organisations across Australia) who provided feedback on their validity. They finalised a list of 7690 verified surnames from the SA countries above. There could be other naming practices that were not picked up by us during this process. Some ethnic groups may not be accessible through this method and we will not pick up SA women married to men of other countries. Many names were classified on more than one list and some names are not limited to SA countries. However, we took the decision to be more inclusive rather than less.
These surnames are flagged in the GrHanite software, so that we can estimate the overall SA patient population and SA women in each clinic. These data will be used to compare the ethnicity data recorded by clinic staff and to estimate intervention effectiveness in these patient populations.
Data analysis
A full statistical analysis plan is currently in draft. Analysis of the primary outcomes before (baseline), during (6 months) at the 12-month period and 3 months after will be conducted by a statistician blinded to allocation status using an intention-to-treat analysis. The denominators for the analysis (ie, number of active female patients per clinic) are also extracted over the same period. Poisson regression will be used to compare the intervention and comparison arms, with the number of documented identifications and referrals within the 12-month intervention period for every cluster as the independent variables. The same will be undertaken for safety planning. The Poisson regression models will include the number of active women ≥18 per clinic as the exposure variable and GP clinic as the random effect to take account of clustering. Models will adjust for any randomisation imbalance in key factors or confounders, such as South Asian population per clinic. This subgroup analysis for estimated proportions of South Asian women will not be generalisable or accurate, as we have not powered the study for SA status and identification methods are not rigorous. We will also analyse 15-month outcome data to test sustainability of the training.
Process evaluation
There is a large gap in evidence for effective DVA education curricula.26 We will evaluate the clinic training with a pretest and post-test assessment of GP training using the GRIPS instrument24 and explore its impact in process evaluation outlined below. In order to explore critical factors affecting sustainability, we will embed the process evaluation methods in normalisation process theory (NPT)27 http://wwwnormalizationprocessorg/npt-toolkit/.
Interviews, semistructured around NPT concepts in DVA primary care work, will be conducted with clinicians, practice managers and administrative staff during and after the end of the intervention to assess intervention process and impact. Bilingual interviews (translated and back-translated) will include: a subset of South Asian women referred to DVA agencies from both arms of the study; and a sample of GPs and reception staff in both arms to explore the experiences of the intervention and what was achieved; and key stakeholders including DVA advocates, In Touch managers and DVA community-based agencies, to explore factors influencing success or limitations of the model and the value to clinics. Qualitative data will be transcribed, entered into NVivo and coded and analysed according to NPT.
Ethical issues and dissemination
Harmony has an obligation to mitigate any harms from this study.28 We will establish a data safety monitoring committee (DSMC) whose role is defined as:
Monitor implementation of trial protocol, safety and any reported harms.28
Monitor clinics withdrawals and lost to follow-up.
Monitor evidence for differences between the intervention and comparison clinics in the main efficacy outcome measures and advise if discontinuation of the trial is necessary.
Monitor continuing appropriateness of data collected in relation to patient information.
Advise on protocol modifications, suggested by investigators (eg, to trial endpoints or sample size).
Monitor sample size assumptions.
Monitor compliance with previous DSMC recommendations.
We will be teaching clinicians self-care and how to manage vicarious trauma. We will also provide two GP teleconferences for an opportunity to discuss current practice with GPs and bilingual caseworkers. Additionally, all participating GPs will be provided with contact information of the Doctor’s Health Advisory Service http://www.dhas.org.au/) and the Regional Mental Health Service. Our hypothesis is that affected patients in intervention clinics will receive enhanced GP care and patients in comparison clinics will receive usual care until after the intervention.
Data privacy
Data from electronic medical records will be extracted using GrHanite. This deidentifies and encrypts the data. Although deidentified, GrHanite employs privacy protecting record linkage techniques that will involve the extraction of limited clinical information relating to females aged ≥18 identified as experiencing DVA. Data collected from referrals received by In Touch will be anonymised.
Consent and confidentiality
We are obtaining consent at GP practice level. Given the nature of the data collected, that is, patient identifiers removed (deidentified), and the privacy protecting techniques used by GrHanite to protect individual identity, consent to query the patient electronic medical records is sought only from the general practices, and not individual patients. As data are deidentified, we believe the risk of harm to patients is negligible.
Dissemination policy
We will create summaries for participating clinics, short accessible policy briefs for governments, offer community media summaries, write peer-reviewed journal articles and present results to relevant national and international conferences.
The HARMONY study has received ethical approval from the La Trobe University Human Ethics Committee (HEC18413).
Protocol amendment
The Harmony study commenced recruitment late in 2019, and one clinic received two sessions of face-to-face DVA training but had not received any advocate intervention, three received one session only and some comparison clinics the half hour training face to face until the COVID-19 pandemic hit Melbourne and was worst in recruiting areas. The study was suspended March to September 2020 and recommenced recruitment in September 2020. All training is now online and the one fully trained clinic was given a brief refresher course. Current and future amendments made in ANZCTR.
Discussion
Women from migrant and refugee backgrounds experience a double jeopardy from their experience of abuse and their migration isolation. HARMONY builds on learning from three previous DVA randomised controlled trials and guidance developed by WHO.29 Harmony’s strengths are that it combines a system approach with clinic-wide strategies, DVA training for GPs and other clinical staff emphasising culturally competency and yearlong support from bilingual/bicultural advocates for clinicians and women to empower and support women from migrant/refugee backgrounds experiencing DVA. It may be limited by the fact that while the intervention is focused on migrant and refugee women, especially those from SA, the current under-recording of this in GP clinic data means that their proportions in clinic populations can only be a broad estimate. It is a goal of Harmony to improve these rates. Harmony will be a world-first primary care trial specifically designed to test culturally competent DVA primary care and improve routine monitoring of DVA among the diversity of diaspora patients.
Supplementary Material
Acknowledgments
The authors acknowledge with gratitude our partner organisation In Touch Multicultural Centre Against Family Violence, in particular Asha Padisetti, Naime Cevik and Ruth Fox, our excellent GP trainer Dr Jennifer Neil and GP clinic recruiting staff Jennie Raymond and Kitty Novy. We also acknowledge our funding bodies.
Footnotes
Contributors: AT, KH, JY and GF designed the study, DB: the GrHaniteprogram and software, RN: the economic evaluation and AT and JY the process evaluation. KH, AT and GF designed the training with WHO advice from CG-M, with inTouch staff. FY, BP and MA contributed to design logistics, training and cultural competency adaptations (BP). XL and CDN are statisticians and contributed to sampling and SAP design. AT drafted the protocol and all authors edited the protocol.
Funding: The HARMONY study is funded by the National Health and Medical Research Partnerships in Health Fund (NHMRC) APP1134477, with additional funding from the Commonwealth of Australia Department of Social Services and the Victorian government Department of Multicultural Affairs and Social Inclusion
Disclaimer: The views expressed are those of the authors and do not necessarily reflect policy of the WHO. The funding bodies have played no role in the study design; collection, management, analysis, and interpretation of these data; the writing of this protocol; and the decision to submit this protocol for publication.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not required.
References
- 1.World Health Organisation . Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence. Geneva: WHO, 2013. [Google Scholar]
- 2.Australian Bureau of Statistics . Personal safety, Australia: statistics for family, domestic, sexual violence, physical assault, partner emotional abuse, child abuse, sexual harassment, Stalking and safety. Canberra: ABS, 2017. https://www.abs.gov.au/statistics/people/crime-and-justice/personal-safety-australia/latest-release#data-download [Google Scholar]
- 3.The Violence Prevention Information System (Violence Info) WHO . Violence information Geneva, 2017. Available: https://apps.who.int/violence-info/intimate-partner-violence
- 4.Valpied J, Hegarty K. Intimate partner abuse: identifying, caring for and helping women in healthcare settings. Womens Health 2015;11:51–63. 10.2217/WHE.14.59 [DOI] [PubMed] [Google Scholar]
- 5.Australian Institute of Health and Welfare (AIHW) . Family, domestic and sexual violence in Australia: continuing the National story. Canberra: Australian Institute of Health and Welfare, 2019. [Google Scholar]
- 6.Australian Bureau of Statistics . 2071.0 - Reflecting a Nation: stories from the 2011 census, 2012-2013. Cultural Diversity in Australia [PDF]. Canberra: ABS, 2012. http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/2071.0main+features902012-2013 [Google Scholar]
- 7.El-Murr A. Intimate partner violence in Australian refugee communities: scoping review of issues and service responses. Melbourne: Australian Institute of Family Studies, 2018. [Google Scholar]
- 8.Vaughan C, Davis E, Murdolo A. Promoting community-led responses to violence against immigrant and refugee women in metropolitan and regional Australia: the ASPIRE project. Sydney: Australia’s National Research Organisation for Women’s Safety, 2015. [Google Scholar]
- 9.Sabri B, Renner LM, Stockman JK, et al. Risk factors for severe intimate partner violence and violence-related injuries among women in India. Women Health 2014;54:281–300. 10.1080/03630242.2014.896445 [DOI] [PubMed] [Google Scholar]
- 10.Silverman JG, Decker MR, Cheng DM, et al. Gender-Based disparities in infant and child mortality based on maternal exposure to spousal violence: the heavy burden borne by Indian girls. Arch Pediatr Adolesc Med 2011;165:22–7. 10.1001/archpediatrics.2010.261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kumar S, Jeyaseelan L, Suresh S, et al. Domestic violence and its mental health correlates in Indian women. Br J Psychiatry 2005;187:62–7. 10.1192/bjp.187.1.62 [DOI] [PubMed] [Google Scholar]
- 12.Raj A, Liu R, McCleary-Sills J, et al. South Asian victims of intimate partner violence more likely than non-victims to report sexual health concerns. J Immigr Health 2005;7:85–91. 10.1007/s10903-005-2641-9 [DOI] [PubMed] [Google Scholar]
- 13.Dasgupta SD, Warrier S. In the footsteps of "Arundhati": Asian Indian women's experience of domestic violence in the United States. Violence Against Women 1996;2:238–59. 10.1177/1077801296002003002 [DOI] [PubMed] [Google Scholar]
- 14.Raj A, Silverman JG, McCleary-Sills J. Immigration policies increase south Asian immigrant women’s vulnerability to intimate partner violence. J Am Med Womens Assoc 2005;60:26–32. [PubMed] [Google Scholar]
- 15.Taft AJ, Small R, Hoang KA. Intimate partner violence in Vietnam and among Vietnamese diaspora communities in Western societies: a comprehensive review. Journal of Family Studies 2008;14:167–82. 10.5172/jfs.327.14.2-3.167 [DOI] [Google Scholar]
- 16.inTouch . Changing lives: 2015 annual report. Melbourne, Australia: InTouch Multicultural Centre Against Family Violence, 2015. [Google Scholar]
- 17.Easteal P. Shattered dreams: marital violence against overseas born women in Australia. Melbourne, Australia: Australian Government Publishing Service, 1996: 201. [Google Scholar]
- 18.Ghafournia N. Battered at home, played down in policy: migrant women and domestic violence in Australia. Aggress Violent Behav 2011;16:207–13. 10.1016/j.avb.2011.02.009 [DOI] [Google Scholar]
- 19.Hegarty K, O'Doherty L, Taft AJ. Effect of screening and brief counselling for abused women on quality of life, safety planning and mental health: a primary care cluster randomised controlled trial (weave). The Lancet 2013;382:249–58. [DOI] [PubMed] [Google Scholar]
- 20.O'Doherty LJ, Taft A, Hegarty K, et al. Screening women for intimate partner violence in healthcare settings: abridged Cochrane systematic review and meta-analysis. BMJ 2014;348:g2913. 10.1136/bmj.g2913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Feder G, Davies RA, Baird K, et al. Identification and referral to improve safety (IRIS) of women experiencing domestic violence with a primary care training and support programme: a cluster randomised controlled trial. Lancet 2011;378:1788–95. 10.1016/S0140-6736(11)61179-3 [DOI] [PubMed] [Google Scholar]
- 22.Taft AJ, Small R, Hegarty KL, et al. Mothers' AdvocateS In the Community (MOSAIC)--non-professional mentor support to reduce intimate partner violence and depression in mothers: a cluster randomised trial in primary care. BMC Public Health 2011;11:178. 10.1186/1471-2458-11-178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pokharel B, Yelland J, Wilson A, Panthad S, et al. Culturally competent primary care response for women of immigrant and refugee backgrounds experiencing family violence: a systematic review protocol. Collegian 2021;28:333–40. 10.1016/j.colegn.2020.08.009 [DOI] [Google Scholar]
- 24.Browne A, Varcoe C, Ford-Gilboe M, et al. EQUIP healthcare: an overview of a multi-component intervention to enhance equity-oriented care in primary health care settings. Int J Equity Health 2016;14:443–54. 10.1186/s12939-015-0271-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.RACGP . The RACGP standards for general practices. 2015. 4th edition. Melbourne, Australia: Royal Australian College of General Practice (RACGP), 2015. [Google Scholar]
- 26.Kalra N, Di Tanna GL, García-Moreno C, et al. Training healthcare providers to respond to intimate partner violence against women. Cochrane Database Syst Rev 2017;7:CD012423. 10.1002/14651858.CD012423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.May CR, Mair FS, Dowrick CF, et al. Process evaluation for complex interventions in primary care: understanding trials using the normalization process model. BMC Fam Pract 2007;8:42. 10.1186/1471-2296-8-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bonell C, Jamal F, Melendez-Torres GJ, Cummins S, et al. 'Dark logic': theorising the harmful consequences of public health interventions. J Epidemiol Community Health 2015;69:95–8. 10.1136/jech-2014-204671 [DOI] [PubMed] [Google Scholar]
- 29.World Health Organisation . Caring for women subjected to violence:a WHO curriculum for training health care providers. Geneva: WHO, 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-046431supp001.pdf (400.7KB, pdf)