EXECUTIVE SUMMARY
The U.S. healthcare system continues to experience high costs and suboptimal health outcomes that are largely influenced by social determinants of health. National policies such as the Affordable Care Act and value-based payment reforms incentivize healthcare systems to engage in strategies to improve population health. Healthcare systems are increasingly expanding or developing new partnerships with community-based organizations to support these efforts. We conducted a systematic review of peer-reviewed literature in the United States to identify examples of hospital–community partnerships; the main purposes or goals of partnerships; study designs used to assess partnerships; and potential outcomes (e.g., process- or health-related) associated with partnerships. Using robust keyword searches and a thorough reference review, we identified 37 articles published between January 2008 and December 2019 for inclusion. Most studies employed descriptive study designs (n = 21); health needs assessments were the most common partnership focus (n = 15); and community/social service (n = 21) and public health organizations (n = 15) were the most common partner types. Qualitative findings suggest hospital–community partnerships hold promise for breaking down silos, improving communication across sectors, and ensuring appropriate interventions for specific populations. Few studies in this review reported quantitative findings. In those that did, results were mixed, with the strongest support for improvements in measures of hospitalizations. This review provides an initial synthesis of hospital partnerships to address population health and presents valuable insights to hospital administrators, particularly those leading population health efforts.
INTRODUCTION
The U.S. healthcare system continues to experience high costs and suboptimal health outcomes. There is growing recognition that social determinants of health contribute significantly to these poor outcomes (Bradley et al., 2017; Institute for Healthcare Improvement, 2018; Kindig & Stoddart, 2003; Schettler, 2006; Stoto, 2013). In response to these growing concerns, national policies such as the Affordable Care Act (ACA) and Internal Revenue Service (IRS) community health needs assessment (CHNA) requirements for not-for-profit hospitals are incentivizing healthcare systems to address the health of populations they serve (Berwick et al., 2008; Institute for Healthcare Improvement, 2018; Koh & Sebelius, 2010; Stoto, 2013). Not surprisingly, recent surveys have found strong support for population health management among health system leaders in the United States (Deloitte United States, 2017; Health Research & Educational Trust, n.d.). However, these organizations historically have put less emphasis on prevention and the upstream social determinants of health as compared to clinical initiatives (Schettler, 2006). Recognizing a need to supplement their capabilities in these areas, many health systems have begun to develop or expand existing partnerships with community-based organizations to help them better address population health (Kindig & Isham, 2014).
Hospitals have partnered with other healthcare delivery organizations to address market pressures arising from managed care, global capitation, and other risk-sharing arrangements (Gaynor & Haas-Wilson, 1999; Lake et al., 2003). While there were early models of hospital partnerships with community-based organizations (Bucks County Health Improvement Partnership, n.d.; Prybil et al., 2014) to address community health, these efforts have more recently been embraced as a strategy to support health systems’ population health management activities (Berwick et al., 2008; Institute for Healthcare Improvement, 2018). Some examples of these types of partnerships include hospital–public health partnerships for CHNAs (Hogg et al., 2015; Laymon et al., 2015; Singh & Carlton, 2017; Wilson et al., 2014), multisector collaborative networks (Hogg & Varda, 2016; Mays et al., 2016; Towe et al., 2016), and partnerships with community-based organizations to improve access to community resources (Lindau et al., 2016; Morgan et al., 2016).
The purpose of this study was to discern patterns in how hospitals address population health outside of the clinical setting through partnerships with nonhospital organizations, as described in peer-reviewed literature. We conducted a systematic literature review to identify examples of hospital–community partnerships and the main purposes of these partnerships; classify study designs used to assess partnerships; and determine potential outcomes (e.g., process or health-related) associated with partnerships. Results of this review can support a better understanding of how health systems engage with community partners for population health and should be of interest to hospital administrators focused on population health management, organizations interested in collaborating with health systems, and researchers who want to assess the impact and quality of these types of partnerships.
METHODS
Search Strategy
We conducted initial searches for relevant articles via the PubMed, EMBASE, and CINAHL databases. We used keyword searches to identify articles related to hospital-based partnerships for population or community health improvement that were published between January 1, 2008, and December 31, 2019. Keywords included collaboration, cooperation, partnership, hospital, tax exempt, nonprofit, not-for-profit, community health services, and population health. We conducted and reported this systematic review in accordance with the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement (Moher et al., 2009).
Inclusion and Exclusion Criteria
We used the following inclusion and exclusion criteria to assess the eligibility of articles: (1) partnership was the focus of study, (2) hospital was included as a main partner, (3) there was at least one other nonhospital-based partner, and (4) the partnership focused on efforts occurring outside of the clinical setting to address specific health conditions or risk factors related to poor health outcomes (Auerbach, 2016). We excluded articles from outside the United States and/or those that were not peer reviewed.
Screening
We conducted initial title and abstract reviews to remove articles that did not meet our inclusion criteria. Two authors (KEH and NM) assessed a random subset of articles to check for consensus on inclusion. Once agreement was reached, KEH assessed the remaining articles. Following the abstract review, we assessed full articles to confirm eligibility for inclusion. After initial screening, we used a snowball technique to identify additional eligible articles in the reference lists of included articles that may not have been indexed in one of the databases we drew from or that were not identified based on our search criteria.
Analysis
We extracted the following information from each article: (1) hospital type, (2) purpose of partnership, (3) partner type(s), (4) study design, (5) purpose of study, (6) outcome measures, and (7) whether the study reported quantitative outcomes. We computed descriptive statistics (frequencies) of study attributes (Table 1). In addition, we summarized attributes and synthesized findings of included studies by partnership purpose (Table 2). We broadly grouped partnership purposes according to four areas: (1) community health needs assessment, (2) care coordination/transitions, (3) health and wellness programs, and (4) other population/public health activities.
TABLE 1.
Description of Study Attributes (n = 37 studies)
| Study Characteristics | Number | Percentage |
|---|---|---|
| Purpose of partnership | ||
| Community health needs assessment | 15 | 40.5 |
| Care coordination/transitions | 11 | 29.7 |
| Health/wellness program | 7 | 18.9 |
| Other population/public health activities | 4 | 10.8 |
| Hospital classification | ||
| Not-for-profit, general | 17 | 45.9 |
| Academic medical center | 6 | 13.5 |
| Specialty | 2 | 5.4 |
| Critical access | 3 | 8.1 |
| Unspecified/multiple | 10 | 27.0 |
| Non-hospital partner | ||
| Community or social service organization (including not-for-profits) | 21 | 56.8 |
| Public health organization | 15 | 40.5 |
| Healthcare delivery organization | 10 | 27.0 |
| Educational organization (e.g., university, school) | 7 | 18.9 |
| Community members | 3 | 8.1 |
| Religious organization | 3 | 8.1 |
| Business | 2 | 5.4 |
| Housing and transportation services | 2 | 5.4 |
| Payer | 2 | 5.4 |
| Other | 2 | 5.4 |
| Publication year | ||
| 2008–2010 | 2 | 5.4 |
| 2011–2013 | 3 | 8.1 |
| 2014–2016 | 15 | 40.5 |
| 2017–2019 | 17 | 45.9 |
| Study type/design | ||
| Case study | 21 | 56.8 |
| Cross-sectional | 9 | 24.3 |
| Quasi-experimental (difference-in-difference) | 2 | 5.4 |
| Experimental (randomized controlled trial) | 3 | 5.4 |
| Other (content analysis/cluster analysis) | 2 | 8.1 |
| Quantitative measures included | 14 | 37.8 |
TABLE 2.
Description of Study Attributes and Main Findings by Focus Area
| Authors and Year | Hospital Type | Partners | Article/Study Type | Outcomes | Findings |
|---|---|---|---|---|---|
| Focus Area 1: Community Health Needs Assessment | |||||
| Ainsworth et al. (2013) | Not-for-profit | Community-based/social service organizations | Case study | Description of process, perceptions of partnership/process and how approach influenced collaboration | Participants from four health systems felt that this approach to a CHNA led to expanded partnerships across the systems and with other community organizations. They also reported that their professional knowledge had improved. |
| Cain et al. (2017) | Not-for-profit | Community members | Case study | Description of a model for incorporating community members into a CHNA and community members’ perspectives on the hospital’s role in the community | Community members said health systems need to include culture as a health resource, do more to foster connections within their communities, and be more present in their communities. These partnerships help hospitals better act on CHNA data collected. |
| Kirk et al. (2017) | Not-for-profit | Public health organizations, community-based/social service organizations, and businesses | Case study | Description of process and lessons learned | The CBPR approach for CHNA helped generate diverse partnerships, define priority needs co-owned by partners, and set the stage for partners to work together for maximum impact. |
| Oppenheim et al. (2019) | Not-for-profit | Religious organizations and community members | Case study | Description of partnership and process used to develop and implement the assessment | The CBPR ensured that CHNA questions were relevant to the community, facilitated the recruitment of participants, and helped translate data to practice and improved care. |
| Krumwiede et al. (2015) | Not-for-profit | Educational organization, community-based/social service organizations | Case study | Description of process and outcomes related to nursing student educational objectives | Nursing students were able to apply the CBCAR framework to help the hospital and its partners conduct a CHNA and core competencies. |
| Van Gelderen et al. (2018) | Not-for-profit | Public health organization, educational organization, community members | Case study | Description of process and outcomes related to six phases of CBCAR framework: partnership, dialogue, pattern recognition, meaning of pattern, insight into action, and reflection on evolving pattern | The CBCAR framework ensured that all voices were heard in the CHNA process, aligned partners, improved communication, and diminished power struggles. It also helped to establish a sustainable community-based collaborative and increase the capacity of the critical access hospital to conduct a CHNA. |
| Beatty et al. (2015) | Not-for-profit | Public health organizations | Content analysis | Level of joint action for CHNAs and hospital characteristics associated with collaboration for CHNAs | 38.2% of the hospitals were “cooperating” with a local health department for a CHNA, with 20.6% “networking,” 20.6% “coordinating,” and only 2.9% “collaborating”; 18% had no identifiable level of joint action. There were no significant differences in hospital characteristics related to a joint action for a CHNA. |
| Carlton & Singh (2015) | Not-for-profit | Public health organizations | Cross-sectional | Degrees of health department-hospital partnership for CHNA and characteristics of LHDs involved in partnerships, association between LHD engagement in accreditation activities and collaboration with hospitals | LHDs partnered with hospitals for CHNA tended to be larger, have higher total and per capita expenditures, be more likely to be locally governed, and have a local board of health. Accreditation activities significantly correlated with LHD-hospital collaboration included completion of a CHNA, completion of a health improvement plan, and completion of an strategic plan. |
| Ellis Hilts et al. (2018) | Not-for-profit | Public health organizations | Cross-sectional | Use of resource dependence theory to assess external market characteristics associated with the likelihood of a health department conducting a CHNA and whether it did so in partnership with a hospital | There was partial support for a resource dependence theory to assess the association between external market characteristics and the likelihood of a LHD to conduct CHNA alone or in partnership with a hospital. Two of three variables measuring munificence were positively associated with a CHNA, and one was associated with a CHNA with a hospital. |
| Laymon et al. (2015) | Not-for-profit | Public health organizations | Cross-sectional | Trends in collaborative CHNAs and associations between CHNA characteristics (i.e., methods used and lead organization) and health department characteristics | Collaborative CHNA activity was positively associated with population size, health department governance type (local or shared vs. state), and local health department and coalition-led efforts. |
| Wilson et al. (2014) | Not-for-profit | Public health organizations | Cross-sectional | Differences in LHD characteristics by degrees of hospital-LHD collaboration for CHNAs | LHDs collaborating with hospitals for CHNAs were more likely to serve a younger population (aged <65) with a higher median income, have higher total expenditures, be interested in voluntary accreditation, and have an administrator with a bachelor’s degree or higher. |
| Kuehnert et al. (2014) | Unspecified | Public health organization and community-based/social service organizations | Cross-sectional | User perceptions of content, format, and impact utility of the assessment | Respondents had positive views of all aspects of the CHNA, with an average score of 3.17 out of 4 for content, 3.19 for format, and 3.21 for impact. Those not involved in the CHNA had significantly less agreement about its usefulness than those who were involved. |
| Franz et al. (2017) | Not-for-profit | Public health organizations, other-unspecified | Cross-sectional | Assessment of how the ACA and IRS CHNA requirements affected not-for-profit hospitals’ approach to these assessments | The ACA requirements have resulted in hospitals formalizing health assessments, using assessments to develop an evidence base, developing local partnerships, and reflecting about their role in the larger public health system. |
| Mathews et al. (2015) | Not-for-profit | Educational organization | Case study | Description of partnership | Academic partners’ research expertise can assist with CHNAs and have a vested interest in implementation strategies to improve health. |
| Sampson et al. (2015) | Not-for-profit | Public health organization | Case study | Description of partnership and successes and challenges experienced during CHNA process | The partnership built on experience and long-standing relationships to overcome barriers related to market competition, limited health department resources, and varying organizational cultures and expectations. New regulations such as the ACA CHNA requirements for hospitals and voluntary accreditation for public health departments also influenced the success of the partnership. |
| Focus Area 2: Care Coordination/Transitions | |||||
| Berkowitz et al. (2016) | Academic medical center | Community-based/social service organizations and other healthcare delivery organization | Case study | Description of partnership, burden and social barriers population faces in obtaining care, lessons learned | Success requires integration of teams across the continuum of care, development of common workflows, and efficient use of IT and other resources. A team that includes clinic and community-based care, collaboration with community-based organizations, integration of behavioral health, and linkages to social services reduces barriers to patients. |
| Everett et al. (2014) | Academic medical center | Community-based/social service organizations and other healthcare delivery organization | Case study | Description of program, progress and challenges in developing the program | The program integrated behavioral interventionists into primary care teams, leading to reports of significant patient and primary care staff satisfaction. |
| Hsiao et al. (2018) | Academic medical center | Community-based/social service organizations and other healthcare delivery organization | Case study | Description of partnership, perceptions of programs impact | The biggest barrier was the siloed health system. Findings emphasized the need to engage patients, get buy-in from healthcare workers, connect with the community, and improve communication across sites—notably with better data and information sharing. |
| Malseptic et al. (2018) | Not-for-profit | Community-based/social service organizations other healthcare delivery organization, other, housing services, educational organizations | Case study | Description of partnership and early lessons learned | Locally derived data help hospitals design interventions for their communities. Also, investment in technologies can expedite patient engagement, nonmedical providers add cost-effective value to complex care teams, and collaboration with community partners improves care continuity and promotes stability outside of the hospital. |
| Sandberg et al. (2014) | Not-for-profit | Public health organization, other healthcare delivery organization, and payer organization | Case study | Description of partnership/program and preliminary patient outcomes: ED visits, hospitalizations, outpatient visits, quality of care for patients with chronic conditions, patient satisfaction | First-year results showed a 9.1% decrease in ED visits and a 3.3% increase in outpatient visits. There was also an increase in the percentage of patients receiving optimal care for chronic conditions: diabetes (8.6% to 10%), vascular (25.0% to 36.1%), and asthma care (10.6% to 13.8%); 87% of patients were satisfied with their care. |
| Sadowski et al. (2009) | Academic medical center | Housing services and community-based/social service organizations | Experimental | Hospitalizations, hospital days, ED visits | Housing and case management services supported a 29% reduction in hospitalizations and hospital days and a 24% reduction in ED visits. |
| Gaskin et al. (2018) | Unspecified | Public health organization, community-based/social service organizations | Quasi-experimental | Adult inpatient stays, readmissions, ED visits per 1,000 residents, and charges per 1,000 residents for inpatient stays and ED visits; participant perceptions of how initiative affected access to care and health behaviors | The initiative was associated with decreases in inpatient stays (13.73 per 1,000 in 2013, 18.03 per 1,000 in 2014, 16.76 per 1,000 in 2015, 17.47 in 2016) but increases in ED visits (32.4 per 1,000 in 2013, 41.01 per 1,000 in 2014, 38.78 per 1,000 in 2015, 38.75 in 2016). The initiative was associated with decreases in annual costs per 1,000 residents for inpatient stays ($125,308-$166,764) and increases in annual costs per 1,000 residents for ED visits ($46,301-$63,553). |
| Warren et al. (2019) | Unspecified | Community-based/social service organizations and other healthcare delivery organization | Case study | Description of initiative and preliminary results for enrollment and readmission rates | 4,978 participants enrolled in the initial 2 years of the program, surpassing the goal of 4,800. There was an 11% decline in the readmission rate for participants from the inception of the program. |
| Sherry et al. (2016) | Unspecified | Community-based/social service organizations payer, educational organizations, other healthcare delivery organizations, and public health organizations | Case study | Description of cross-sector partnerships, identification of factors that promote or inhibit cross-sector collaboration | Factors that facilitated community-oriented collaboration included flexible financing, shared leadership, shared data, and shared vision. |
| Baxter et al. (2018) | Not-for-profit | Other healthcare delivery organizations and community-based/social service organizations | Case study | Description of program and preliminary results for 30-day readmission rates | In the first year, readmission rates for all palliative care patients decreased from 22% to 16%. |
| Murphy et al. (2018) | Academic medical center | Community-based/social service organizations and other healthcare delivery organization | Quasi-experimental | Paid costs and counts of ED visits, admissions; readmissions per member per year for a cohort of high-risk Medicaid and Medicare beneficiaries | The program was associated with nonsignificant cost savings of $1,171 for Medicaid participants and $476 for Medicare participants. For ED visits, there was a small, nonsignificant decrease for Medicaid (ratio = 0.97) and a slight, nonsignificant increase in ED visits for Medicare (ratio = 1.02). The rate of admissions for the Medicaid cohort was relatively unchanged (rate = 1.01), and there was a nonsignificant increase in admissions for the Medicare cohort (rate = 1.08). There was a slight, nonsignificant increase in the readmission rate for the Medicaid cohort (ratio = 1.03), and a larger but still nonsignificant increase in the readmission rate for the Medicare cohort (ratio = 1.29). |
| Focus Area 3: Health and Wellness Programs | |||||
| Buys et al. (2017) | Academic medical center | Community-based/social service organizations | Experimental | Nutritional intake, readmission rate, and patient acceptability and satisfaction | There was no effect related to hospital readmissions. There was a significant effect related to nutritional intake, and participants reported satisfaction with the program. |
| Cho et al. (2015) | Unspecified | Community-based/social service organizations | Cross-sectional | Self-reported rates of hospitalizations, resolution of medication alerts | Self-report of hospitalization was lower than expected; a high percentage of medication alerts were resolved within 30 days. |
| Martin et al. (2018) | Not-for-profit | Community-based/social service organizations | Cross-sectional | Readmissions rates and cost measurements | The program was associated with a 38.0% improvement in the 30-day all-cause readmission rate from baseline and $212,160 in costs savings for the program related to decreased readmissions. |
| Haas & Kimmel (2011) | Unspecified | Religious organization, other healthcare delivery organization, and community-based/social service organizations | Case study | Counts of referrals, dropout rate, staff response to adverse events | Referrals to the program increased from 168 to 2,456 between 2001 and 2010; however, there was a high dropout rate (50%). |
| Hoke et al. (2015) | Not-for-profit | Educational organization and community-based/social service organizations | Case study | Provision of screenings, follow-up to parents | Annual screenings were completed for 67% of students in the district; letters were sent to all parents of students who were screened. |
| Mendelson et al. (2008) | Not-for-profit | Religious organization | Experimental | Measure of maternal health behaviors, measures of glycemic control, rates of neonatal and maternal hospitalizations | There were no significant differences between groups for measures of glycemic control or days of maternal or neonatal hospitalizations. There were significant improvements in a measure of healthful behaviors. |
| Woods-Jaeger et al. (2018) | Children’s hospital | Educational organization | Case study | Feasibility of interventions | “Theraplay” intervention benefited children and improved teacher-child interactions. Therapists’ and teachers’ perceptions of benefits related to children’s developmental needs and benefits differed, which could be addressed through better therapist-teacher collaboration. Participants in parental behavioral therapy and skills training intervention reported satisfaction with the program and improved relationships with children, discipline, and other personal or family problems. |
| Focus Area 4: Other Public/Population Health Activities | |||||
| Ferrer et al. (2013) | Not-for-profit | Public health organization, community-based/social service organizations, and businesses | Case study | Hospitalizations, ED and urgent care visits, and associated costs | Found a 24% decrease in hospitalizations, 12% increase in ED visits, and 9% decrease in total charges among high-use patients in the first year. Second-year preliminary results indicated a trend toward decreased hospitalizations and ED visits. |
| Franz et al. (2018) | Children’s hospital | Community-based/social service organizations | Case-study | Strategies hospitals use to communicate with residents and how efforts are perceived by residents | Respondents valued the hospital as a provider of medical care but did not know about its involvement in community improvement (ineffective communication). |
| Hogg et al. (2015) | Unspecified | Public health organizations | Cross-sectional | Hospital participation in public health activities from 1998–2006 and 2006–2012 | Hospital participation in public health activities increased between 1998 and 2006 (37% to 41%) and decreased between 2006 and 2012 (41% to 39%). Hospital participation in public health activities was positively associated with availability of public health services. |
| Noh et al. (2018) | Unspecified | Other | Cluster analysis | Taxonomy of hospital partnerships for community or population health | Categorized partnerships as: exploratory (26.1%; developed partnerships outside medical sector), exploitative (18.3%; developed partnerships with traditional medical sector partners), ambidextrous (27%; developed partnerships both inside and outside of the traditional medical sector), and independent (28.6%; developed no partnerships). |
Note. ACA = Affordable Care Act; CBCAR = Community-based Collaborative Action Research; CBPR = community-based participatory research; CHNA = community health needs assessment; ED = emergency department; IRS = Internal Revenue Service; LHD = local health department.
RESULTS
Our keyword searches identified 557 articles for review. After removing duplicates and applying our title, abstract, and full-text selection criteria, 26 articles remained. We identified an additional 11 articles through our reference lists review for a final set of 37 articles for inclusion in our analyses (see Figure 1 for our PRISMA flow diagram). The 37 articles were all published between 2008 and 2019, with more than three fourths published between 2015 and 2019. The most common study design among the included articles was case study (n = 21), followed by cross-sectional (n = 9). Five studies applied a more rigorous design (three experimental; two quasi-experimental). A little more than one-third (n = 14) reported quantitative measures to assess the impact or potential impact of studied initiatives.
FIGURE 1. PRISMA Diagram.
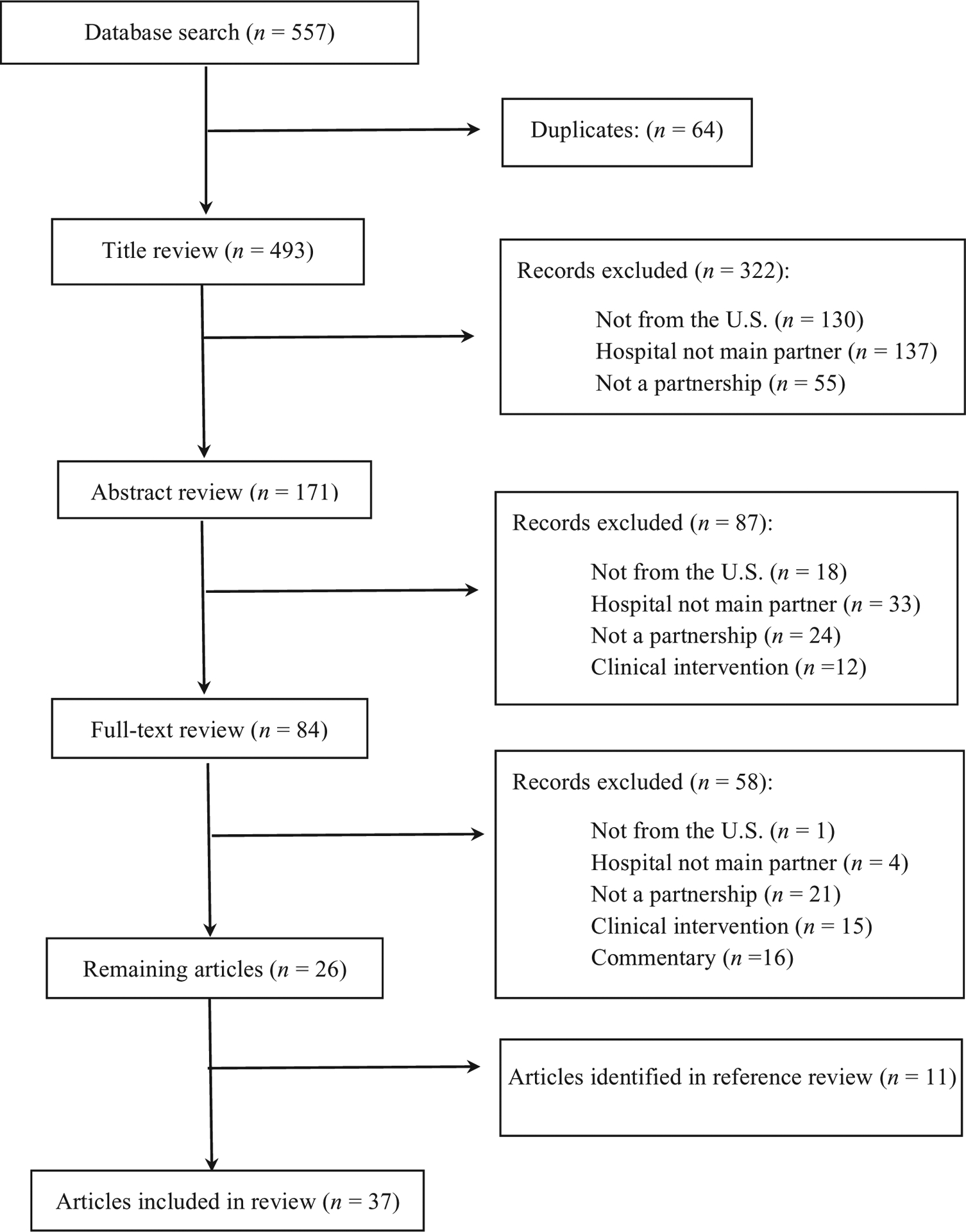
Note. PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses
The most common type of partnership purpose was to conduct health needs assessments (n = 15), followed by care coordination activities (n = 11; see Table 1). Not-for-profit hospitals were the most common subjects in included articles, with none of the partnerships in included articles focusing solely on for-profit hospitals. Some included multiple hospitals and/or did not specify hospital type in their studies (n = 10). Community organizations were the most common nonhospital partner (n = 18), followed by public health organizations (n = 15) and other healthcare delivery organizations (n = 10). In the following section, we synthesize attributes and results across all studies.
Community Health Needs Assessment
Table 2 presents the findings from the 15 articles that focused on partnerships for CHNAs. Six of the 15 applied case study designs describe processes that had been used to incorporate community voices into health needs assessments.(Ainsworth et al., 2013; Cain et al., 2017; Kirk et al., 2017; Krumwiede et al., 2015; Oppenheim et al., 2019; Van Gelderen et al., 2018). Overarching themes identified in these studies emphasized that conducting a CHNA in a way that engages and incorporates community perspectives helps to create diverse, collaborative partnerships that can last beyond the initial assessment (Ainsworth et al., 2013; Cain et al., 2017; Kirk et al., 2017; Krumwiede et al., 2015), helps health systems define priorities that are relevant to the communities they serve (Kirk et al., 2017; Oppenheim et al., 2019; Van Gelderen et al., 2018), and assists in better translating and acting on data gathered as part of these processes (Cain et al., 2017; Oppenheim et al., 2019).
An additional five studies that focused on CHNA activities looked specifically at partnerships between hospitals and public health agencies to conduct these assessments (Beatty et al., 2015; Carlton & Singh, 2015; Ellis Hilts et al., 2018; Laymon et al., 2015; Wilson et al., 2014). One of these studies looked at hospitals’ likelihood of engaging in these partnerships and found that a little more than 40% were “cooperating” or “networking” with a local health department for a CHNA, approximately 24% were “coordinating” or “collaborating” with a local health department for a CHNA, and about 20% had no identifiable level of engagement with a local health department for a CHNA (Beatty et al., 2015).
The other four studies looking at hospital–public health partnerships did so from the perspective of public health agencies (Carlton & Singh, 2015; Ellis Hilts et al., 2018; Laymon et al., 2015; Wilson et al., 2014). Ellis Hilts and colleagues (2018) looked for associations between measures of the external market environment and local health departments’ likelihood of conducting a CHNA in partnership with a hospital. They found that the number of primary care physicians per 1,000 capita was positively associated with local health department (LHD)–hospital partnerships for CHNAs, and a higher violent crime rate in a market was negatively associated with LHD–hospital partnerships for CHNAs. Three studies looked at associations between degrees of LHD–hospital collaboration and LHD characteristics related to joint action for CHNAs (Carlton & Singh, 2015; Laymon et al., 2015; Wilson et al., 2014). These studies found that LHDs partnering with hospitals for CHNAs were more likely to have higher total expenditures (Carlton & Singh, 2015; Wilson et al., 2014), serve a larger population (Carlton & Singh, 2015; Laymon et al., 2015), have a local governance structure as opposed to a state governance structure (Carlton & Singh, 2015; Laymon et al., 2015), and be interested and/or engaged in voluntary public health accreditation activities (Carlton & Singh, 2015; Wilson et al., 2014).
The final four studies looking at partnerships for CHNAs looked at a variety of aspects of hospital partnerships to support CHNAs, including user perceptions of these activities (Kuehnert et al., 2014), the value of specific partners (Mathews et al., 2015), and the influence of new regulations such as voluntary public health accreditation and IRS CHNA requirements on partnerships (Franz et al., 2017; Sampson et al., 2015). Findings from these studies included reports that new regulations had influenced the development and success of hospital partnerships with community-based organizations to support CHNA efforts (Franz et al., 2017; Sampson et al., 2015). In addition, qualitative findings emphasized the potential value that outside organizations such as academic institutions can bring to the CHNA process (e.g., research expertise; Mathews et al., 2015) and suggested that while users of CHNAs generally had positive views of the CHNA process and products, those not directly involved in the assessments were significantly less sure about its usefulness (Kuehnert et al. 2014).
Care Coordination/Transitions
Table 2 summarizes the 11 articles that included partnerships focused on improving care coordination/transitions. Eight of these studies used case study designs to provide descriptions of partnerships with diverse organizations to support coordination of care for high-risk populations (e.g., Medicare, Medicaid; Baxter et al., 2018; Berkowitz et al., 2016; Everett et al., 2014; Hsiao et al., 2018; Malseptic et al., 2018; Sandberg et al., 2014; Sherry et al., 2016; Warren et al., 2019). Findings suggested that multisector partnerships are helpful in removing barriers to engagement with patients and connecting them to needed clinical, behavioral, and community-based services (Baxter et al., 2018; Berkowitz et al., 2016; Everett et al., 2014; Hsiao et al., 2018; Malseptic et al., 2018; Sandberg et al., 2014; Warren et al., 2019). Additional key takeaways documented across these studies included a need for better integration of providers across the continuum of care (Berkowitz et al., 2016; Everett et al., 2014; Hsiao et al., 2018; Malseptic et al., 2018; Sherry et al., 2016) and the use of available data and information technology to support better information sharing and design interventions tailored to communities of interest (Berkowitz et al., 2016; Hsiao et al., 2018; Malseptic et al., 2018; Sherry et al., 2016).
Also, three of the eight case studies included preliminary results of quantitative measures related to partnerships. Everett and colleagues (2014) and Sandberg and colleagues (2014) provided preliminary results suggesting high degrees of patient satisfaction with these collaborative models of care. Further preliminary results from these descriptive case studies noted improvements in measures of healthcare utilization. Specifically, Sandberg and colleagues (2014) reported a 9.1% decrease in emergency department (ED) visits and a corresponding 3.3% increase in outpatient visits among participants in the first year of the care coordination program; Warren and others (2019) reported an 11% decline in readmission rates for participants in their programs.
The remaining three studies focused on partnerships to support care coordination and applied quasi-experimental (Gaskin et al., 2018; Murphy et al., 2018) or experimental (Sadowski et al., 2009) designs to explore the potential impact of partnerships. Two of the three studies reported improvements in measures of hospitalizations. These improvements included a 29% relative reduction in hospitalizations for a housing and case management intervention group compared to control (Sadowski et al., 2009) and a significant reduction in inpatient stays for a multisector partnership-focused intervention, with an average of a 1.7% reduction in inpatient stays over a 4-year period in intervention zip codes as compared to control zip codes (Gaskin et al., 2018; Sadowski et al., 2009). The third reported no change for a cohort of Medicaid patients, and a slight, nonsignificant increase in hospital admissions among a cohort of Medicare patients (Murphy et al., 2018).
Results varied for measures of ED use across the studies using stronger study designs to assess partnerships to support care coordination. Sadowski and colleagues (2009) reported a 24% relative reduction in ED visits among its intervention group, and Murphy and colleagues (2018) reported a slight, nonsignificant decrease (incident rate ratio = 0.97) in ED visits among patients covered by Medicaid. However, Murphy and colleagues (2018) reported a slight, nonsignificant increase in ED visits for Medicare participants, and Gaskin and colleagues (2018) reported an average increase of 36 ED visits per 1,000 residents over the study period with significant differences in the number of ED visits per 1,000 residents between intervention and comparison groups. Two of these studies also measured outcomes related to costs of utilization and reported positive outcomes. Murphy and colleagues (2018) reported nonsignificant cost savings of $1,171 for Medicaid participants and $476 for Medicare participants. Gaskin and colleagues (2018) reported a total net savings in hospital charges compared to the cost of the initiative of $93.4 million over 4 years.
Health and Wellness Programs
Table 2 summarizes the seven articles that focused on partnerships related to health and wellness programs. Three of the seven were related to meal delivery programs for medically vulnerable populations (Buys et al., 2017; Cho et al., 2015; Martin et al., 2018). Two of these three applied cross-sectional study designs and reported significant improvements in rates of readmissions (Martin et al., 2018) and self-reported rates of hospitalizations as well as a positive return on investment for every dollar spent on the program (Cho et al., 2015). In the third article study, a randomized control trial did not find a significant change in hospital readmissions (Buys et al., 2017).
The other articles in this focus area included a gestational diabetes education program (Mendelson et al., 2008), a community-based exercise program for cancer patients (Haas & Kimmel, 2011), a behavioral health intervention to address toxic stress in early childhood (Woods-Jaeger et al., 2018), and a school-based health screening program (Hoke et al., 2015). Three of the articles used case study designs and reported positive programmatic outcomes such as the provision of state-mandated health screenings (Hoke et al., 2015), an increase in referrals to the community-based exercise program (Haas et al., 2011), and improved teacher–child interactions with the behavioral health intervention (Woods-Jaeger et al., 2018). Importantly, these observational studies indicated that partnerships facilitated positive programmatic outcomes. The last study, a randomized controlled trial assessing the effect of a partnership-based gestational diabetes education program on rates of hospitalizations and measures of glycemic control, did not find significant effects related to these measures (Mendelson et al., 2008).
Other Population/Public Health Activities
Table 2 summarizes the findings of four studies that used descriptive study designs to assess hospital partnerships with external organizations such as local health departments, social service organizations, and other businesses to support broad efforts to address population or community health needs (Ferrer et al., 2013; Franz et al., 2018; Hogg et al., 2015; Noh et al., 2018). Ferrer and colleagues (2013) used a case study design to explore the perceived value of this type of partnership and found that patients appreciated the extra time and assistance provided in the expanded services. The researchers also reported that the inclusion of nontraditional partners appeared to help provide holistic care to patients. Hogg and colleagues (2015) used a cross-sectional study design to assess trends in hospital participation in public health activities and reported that participation had increased between 1998 and 2006 (37% to 41%) but decreased slightly between 2006 and 2012 (41% to 39%). In addition, the authors reported a positive association between hospital engagement with public health agencies and the availability of public health services in communities. Noh and colleagues (2018) conducted a cluster analysis to describe hospital partnerships for community or population health. They found that 26.1% of hospitals had established partnerships with partners outside of the medical sector. Approximately 18.3% had partnerships with other medical sector partners, 27% had partnerships with organizations both within and outside of the medical sector, and 28.6% had not established strong partnerships with groups in either sector.
DISCUSSION
Results from our systematic review indicate that studies examining hospital partnerships for community or population health have been increasing, particularly in the past 5 years. This increase aligns with the implementation of several national policies and initiatives, including the ACA, the IRS CHNA requirements (U.S. Internal Revenue Service, n.d.), and the Public Health Accreditation Board’s voluntary national public health accreditation program (Public Health Accreditation Board, n.d.). Almost all studies in our review included some type of not-for-profit hospital, with for-profit hospitals only referenced as part of multiorganization collaborations that typically also involved not-for-profit hospitals. Therefore, we were not able to assess the differences between not-for-profit and for-profit hospitals related to partnerships for community or population health improvement.
CHNA was the most common partnership purpose across the studies we reviewed. Results from these studies suggest that partnerships to support CHNAs have led to hospitals engaging with a broader set of organizations. Notably, we found that public health agencies were one of the most common types of partners examined in these studies. This finding is promising, as both the strengthened IRS CHNA requirements for not-for-profit hospitals and the national voluntary public health accreditation program are encouraging partnerships between these two organization types (Abbott, 2011). However, all studies in this area used descriptive study designs, which made it difficult to form conclusions on the potential impact of these types of partnerships (Aggarwal & Ranganathan, 2019). Nevertheless, results identified several other beneficial outcomes such as the potential for partnerships to last beyond initial assessment processes, the ability to better define priorities that are co-owned by partners and relevant to the communities they serve, and the role of partners in assisting hospitals in translating and acting on data gathered as part of these CHNA processes (Ainsworth et al., 2013; Cain et al., 2017; Kirk et al., 2017; Krumwiede et al., 2015; Oppenheim et al., 2019; Van Gelderen et al., 2018).
Descriptive study designs were also the most-used design across all other partnership areas. Even with a limited ability to assess causality, results from descriptive studies suggest that hospital partnerships with other clinical and nonclinical partners may improve care coordination for patients, support community-based health and wellness programs, and increase hospital engagement in other population health or public health activities. Notably, these partnerships seem to hold promise for breaking down silos and improving communication between sectors and ensuring that interventions are evidence-based and appropriate to specific populations.
Only five studies in this review included study designs (experimental or quasi-experimental) that can reasonably support causal inference to assess the potential impact of hospital partnerships for population health activities. Among the studies using these designs, results were often mixed. The most consistent findings suggest these types of partnerships significantly and positively affect hospitalization rates. There was also support for the impact of these partnerships on utilization costs, with all three studies that included cost measures reporting positive effects, although one was nonsignificant. The greatest variability was for measures of ED utilization, with one of three studies reporting a significant positive effect, one reporting a significant negative effect, and the final study reporting no effect and a slight, nonsignificant increase in ED visits for a Medicaid and Medicare population, respectively. Only two studies looked at readmission rates; while one reported a significant positive effect, the other found no effect.
In general, there is a potential positive benefit associated with hospital–community partnerships for population or community health improvement, particularly for improving measures of healthcare utilization. However, given that most of the studies included in this review were limited to descriptive studies and that results from experimental and quasi-experimental studies were often mixed, there is an ongoing need for additional rigorous studies to better understand the impact of hospital partnerships on population health outcomes.
Further, articles in this review focused on partnerships to support programs and interventions at the individual level; very few looked at broader community efforts to address the underlying causes of poor health outcomes. Future studies should consider how hospitals can work with partners across various sectors to support initiatives aimed at broader system and policy changes to address key risk factors and social determinants of health. Public health organizations and other social and community-based organizations should be considered as partners in these efforts. These organizations have more experience with broader social determinants of health and can provide expertise and support for hospitals’ population health efforts (Koo et al., 2012).
Future research should examine how hospitals can engage with partners to implement strategies to support policies and practices to improve the underlying causes of preventable morbidity and mortality. Examples of such interventions could include partnerships to support systemic efforts to increase access to food, reduce hunger, and improve nutritional intake among high need populations; support community development efforts to improve living conditions in low-income communities; and efforts to reduce tobacco use among vulnerable populations (Braunstein & Lavizzo-Mourey, 2011; Castrucci & Auerbach, 2019; Gottlieb et al., 2019).
Study Limitations
This study has two important limitations. First, our review only included peer-reviewed, published articles and not gray literature. We have not captured all hospital partnerships focused on population or community health improvement. Second, although we used a robust keyword search and a snowball technique to identify articles for review, it is possible that we missed studies. Despite these limitations, this study presents a useful review of current peer-reviewed literature on hospital partnerships for population health and builds on the current knowledge base in this area.
CONCLUSION
National policies and initiatives, such as the ACA, IRS CHNA requirements, and emerging value-based payment models are incentivizing hospitals to adopt strategies to improve population health. Hospital administrators, especially those tasked with overseeing population health management activities, should identify the best partners to support these efforts, leverage these partnerships and sustain them beyond initial efforts to meet regulatory requirements, and use them to support the implementation of interventions focused on upstream social determinants of health. Importantly, our review provides an initial synthesis of hospital partnerships to address population health and can provide valuable insights for decision-makers. However, as much of the literature in this area is limited to descriptive findings, there is a need for more rigorous studies to better understand the potential short- and long-term effects of these partnerships.
Acknowledgments
Part of Dr. Ellis Hilts’s time while preparing this article was supported by the National Cancer Institute of the National Institutes of Health under award number T32 CA117865. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
The authors declare no conflicts of interest.
Contributor Information
Katy Ellis Hilts, IU Richard M. Fairbanks School of Public Health, Indianapolis, Indiana;.
Valerie A. Yeager, IU Richard M. Fairbanks School of Public Health;.
P. Joseph Gibson, Marion County Public Health Department, Indianapolis Indiana;.
REFERENCES
- Abbott AL (2011). Community benefits and health reform: Creating new links for public health and not-for-profit hospitals. Journal of Public Health Management and Practice, 17(6), 524–529. 10.1097/PHH.0b013e31822da124 [DOI] [PubMed] [Google Scholar]
- Aggarwal R, & Ranganathan P (2019). Study designs: Part 2—Descriptive studies. Perspectives in Clinical Research, 10(1), 34–36. 10.4103/picr.PICR_154_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ainsworth D, Diaz H, & Schmidtlein MC (2013). Getting more for your money: Designing community needs assessments to build collaboration and capacity in hospital system community benefit work. Health Promotion Practice, 14(6), 868–875. 10.1177/1524839912470445 [DOI] [PubMed] [Google Scholar]
- Auerbach J (2016). The 3 buckets of prevention. Journal of Public Health Management and Practice, 22(3), 215–218. 10.1097/PHH.0000000000000381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baxter KE, Rochon T, & Lally KM (2018). Providing palliative care across the continuum to reduce readmissions from community settings. Annals of Long Term Care, 26(1), 27–32. 10.25270/altc.2018.10.00019 [DOI] [Google Scholar]
- Beatty KE, Wilson KD, Ciecior A, & Stringer L (2015). Collaboration among Missouri nonprofit hospitals and local health departments: Content analysis of community health needs assessments. American Journal of Public Health, 105(Suppl 2), S337–S344. 10.2105/AJPH.2014.302488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkowitz SA, Brown P, Brotman DJ, Deutschendorf A, Dunbar L, Everett A, Hickman D, Howell E, Purnell L, Sylvester C, Zollinger R, Bellantoni M, Durso SC, Lyketsos C, Rothman P, & J-CHiP. (2016). Program Case study: Johns Hopkins Community Health Partnership: A model for transformation. Healthcare (Amsterdam, Netherlands), 4(4), 264–270. 10.1016/j.hjdsi.2016.09.001 [DOI] [PubMed] [Google Scholar]
- Berwick DM, Nolan TW, & Whittington J (2008). The Triple Aim: Care, health, and cost. Health Affairs, 27(3), 759–769. 10.1377/hlthaff.27.3.759 [DOI] [PubMed] [Google Scholar]
- Bradley EH, Sipsma H, & Taylor LA (2017). American health care paradox: High spending on health care and poor health. QJM: Monthly Journal of the Association of Physicians, 110(2), 61–65. 10.1093/qjmed/hcw187 [DOI] [PubMed] [Google Scholar]
- Braunstein S, & Lavizzo-Mourey R (2011). How the health and community development sectors are combining forces to improve health and well-being. Health Affairs, 30(11), 2042–2051. 10.1377/hlthaff.2011.0838 [DOI] [PubMed] [Google Scholar]
- Bucks County Health Improvement Partnership. (n.d.). Bucks County Health Improvement Partnership. https://www.bchip.org/
- Buys DR, Campbell AD, Godfryd A, Flood K, Kitchin E, Kilgore ML, Allocca S, & Locher JL (2017). Meals enhancing nutrition after discharge: Findings from a pilot randomized controlled trial. Journal of the Academy of Nutrition and Dietetics, 117(4), 599–608. 10.1016/j.jand.2016.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cain CL, Orionzi D, O’Brien M, & Trahan L (2017). The power of community voices for enhancing community health needs assessments. Health Promotion Practice, 18(3), 437–443. 10.1177/1524839916634404 [DOI] [PubMed] [Google Scholar]
- Carlton EL, & Singh S (2015). Accreditation intent, community health assessments, and local health department–hospital collaboration. Frontiers in Public Health Services and Systems Research, 4(1), 1–6. 10.13023/FPHSSR.0401.01 [DOI] [Google Scholar]
- Castrucci B, & Auerbach J (2019, January 16). Meeting individual social needs falls short of addressing social determinants of health. Health Affairs. https://www.healthaffairs.org/do/10.1377/hblog20190115.234942/full/ [Google Scholar]
- Cho J, Thorud JL, Marishak-Simon S, Frawley L, & Stevens AB (2015). A model home-delivered meals program to support transitions from hospital to home. Journal of Nutrition in Gerontology and Geriatrics, 34(2), 207–217. 10.1080/21551197.2015.1031598 [DOI] [PubMed] [Google Scholar]
- Deloitte United States. (2017, July 24). 2017 Survey of US hospital CEOs. https://www2.deloitte.com/us/en/pages/life-sciences-and-health-care/articles/health-system-ceos.html
- Ellis Hilts K, Xia J, Yeager VA, Ferdinand AO, & Menachemi N (2018). Market characteristics associated with community health assessments by local health departments. Public Health, 162:118–125. 10.1016/j.puhe.2018.05.027 [DOI] [PubMed] [Google Scholar]
- Everett AS, Reese J, Coughlin J, Finan P, Smith M, Fingerhood M, Berkowitz S, Young JH, Johnston D, Dunbar L, Zollinger R, Ju J, Reuland M, Strain EC, & Lyketsos C (2014). Behavioural health interventions in the Johns Hopkins Community Health Partnership: Integrated care as a component of health systems transformation. International Review of Psychiatry, 26(6), 648–656. 10.3109/09540261.2014.979777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrer RL, Gonzalez Schlenker C, Lozano Romero R, Poursani R, Bazaldua O, Davidson D, Ann Gonzales M, Dehoyos J, Castilla M, Corona BA, Tysinger J, Alsip B, Trejo J, & Jaén CR (2013). Advanced primary care in San Antonio: Linking practice and community strategies to improve health. Journal of the American Board of Family Medicine, 26(3), 288–298. 10.3122/jabfm.2013.03.120238 [DOI] [PubMed] [Google Scholar]
- Franz B, Skinner D, & Kelleher K (2017). The impact of the Affordable Care Act on hospital-led community health evaluation in the U.S. Appalachian Ohio region. Journal of Evaluation in Clinical Practice, 23(4), 882–887. 10.1111/jep.12749 [DOI] [PubMed] [Google Scholar]
- Franz B, Skinner D, Kerr AM, Penfold R, & Kelleher K (2018). Hospital–community partnerships: Facilitating communication for population health on Columbus’ south side. Health Communication, 33(12), 1462–1474. 10.1080/10410236.2017.1359033 [DOI] [PubMed] [Google Scholar]
- Gaskin DJ, Vazin R, McCleary R, & Thorpe RJ Jr (2018). The Maryland Health Enterprise Zone initiative reduced hospital cost and utilization in underserved communities. Health Affairs, 37(10), 1546–1554. 10.1377/hlthaff.2018.0642 [DOI] [PubMed] [Google Scholar]
- Gaynor M, & Haas-Wilson D (1999). Change, consolidation, and competition in health care markets. The Journal of Economic Perspectives, 13(1), 141–164. 10.1257/jep.13.1.141 [DOI] [PubMed] [Google Scholar]
- Gottlieb L, Fichtenberg C, Alderwick H, & Adler N (2019). Social determinants of health: What’s a healthcare system to do? Journal of Healthcare Management, 64(4), 243–257. 10.1097/JHM-D-18-00160 [DOI] [PubMed] [Google Scholar]
- Haas BK, & Kimmel G (2011). Model for a community-based exercise program for cancer survivors: Taking patient care to the next level. Journal of Oncology Practice, 7(4), 252–256. 10.1200/JOP.2010.000194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Research & Educational Trust. (n.d.). Approaches to population health in 2015: A national survey of hospitals. http://www.hpoe.org/Reports-HPOE/2015/PopHealthSurvey_FINAL_picture.pdf
- Hogg RA, Mays GP, & Mamaril CB (2015). Hospital contributions to the delivery of public health activities in US metropolitan areas: National and longitudinal trends. American Journal of Public Health, 105(8), 1646–1652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogg RA, & Varda D (2016). Insights into collaborative networks of nonprofit, private, and public organizations that address complex health Issues. Health Affairs, 35(11), 2014–2019. 10.1377/hlthaff.2016.0725 [DOI] [PubMed] [Google Scholar]
- Hoke AM, Kephart DK, Dillon JF, McCullough JR, Blatt BJ, & Kraschnewski JL (2015). Improving community health while satisfying a critical community need: A case study for nonprofit hospitals. Preventing Chronic Disease, 12:E185. 10.5888/pcd12.150230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsiao YL, Bass EB, Wu AW, Richardson MB, Deutschendorf A, Brotman DJ, Bellantoni M, Howell EE, Everett A, Hickman D, Purnell L, Zollinger R, Sylvester C, Lyketsos CG, Dunbar L, & Berkowitz SA (2018). Implementation of a comprehensive program to improve coordination of care in an urban academic health care system. Journal of Health Organization and Management, 32(5), 638–657. 10.1108/JHOM-09-2017-0228 [DOI] [PubMed] [Google Scholar]
- Institute for Healthcare Improvement. (2018, April). Pathways to population health framework. http://pathways2pophealth.org/files/Pathways-to-Population-Health-Framework-April-2018.pdf
- Kindig DA, & Isham G (2014). Population health improvement: A community health business model that engages partners in all sectors. Frontiers of Health Services Management, 30(4), 3–20. [PubMed] [Google Scholar]
- Kindig D, & Stoddart G (2003). What is population health? American Journal of Public Health, 93(3), 380–383. 10.2105/AJPH.93.3.380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirk CM, Johnson-Hakim S, Anglin A, & Connelly C (2017). Putting the community back into community health needs assessments: Maximizing partnerships via community-based participatory research. Progress in Community Health Partnerships: Research, Education, and Action, 11(2), 167–173. 10.1353/cpr.2017.0021 [DOI] [PubMed] [Google Scholar]
- Koh HK, & Sebelius KG (2010). Promoting prevention through the Affordable Care Act. The New England Journal of Medicine, 363(14), 1296–1299. 10.1056/NEJMp1008560 [DOI] [PubMed] [Google Scholar]
- Koo D, Felix K, Dankwa-Mullan I, Miller T, & Waalen J (2012). A call for action on primary care and public health integration. American Journal of Public Health, 102(Suppl 3), S307–S309. 10.2105/AJPH.2012.300824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krumwiede KA, Van Gelderen SA, & Krumwiede NK (2015). Academic–hospital partnership: Conducting a community health needs assessment as a service learning project. Public Health Nursing, 32(4), 359–367. 10.1111/phn.12159 [DOI] [PubMed] [Google Scholar]
- Kuehnert P, Graber J, & Stone D (2014). Using a web-based tool to evaluate a collaborative community health needs assessment. Journal of Public Health Management and Practice, 20(2), 175–187. 10.1097/PHH.0b013e31829dc1e5 [DOI] [PubMed] [Google Scholar]
- Lake T, Devers K, Brewster L, & Casalino L (2003). Something old, something new: Recent developments in hospital–physician relationships. Health Services Research, 38(1 Pt 2), 471–488. 10.1111/1475-6773.00125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laymon B, Shah G, Leep CJ, Elligers JJ, & Kumar V (2015). The proof’s in the partnerships: Are Affordable Care Act and local health department accreditation practices influencing collaborative partnerships in community health assessment and improvement planning? Journal of Public Health Management and Practice, 21(1), 12–17. 10.1097/PHH.0000000000000087 [DOI] [PubMed] [Google Scholar]
- Lindau ST, Makelarski J, Abramsohn E, Beiser DG, Escamilla V, Jerome J, Johnson D, Kho AN, Lee KK, Long T, & Miller DC (2016). CommunityRx: A population health improvement innovation that connects clinics to communities. Health Affairs, 35(11), 2020–2029. 10.1377/hlthaff.2016.0694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malseptic GG, Melby LH, & Connolly KA (2018). Complex care models to achieve accountable care readiness: Lessons from two community hospitals. Healthcare (Amsterdam, Netherlands), 6(1), 74–78. 10.1016/j.hjdsi.2017.05.006 [DOI] [PubMed] [Google Scholar]
- Martin SL, Connelly N, Parsons C, & Blackstone K (2018). Simply delivered meals: A tale of collaboration. American Journal of Managed Care, 24(6), 301–304. https://www.ncbi.nlm.nih.gov/pubmed/29939505 [PubMed] [Google Scholar]
- Mathews AL, Coyle BS, & Deegan MM (2015). Building community while complying with the Affordable Care Act in the Lehigh Valley of Pennsylvania. Progress in Community Health Partnerships: Research, Education, and Action, 9(1), 101–112. 10.1353/cpr.2015.0000 [DOI] [PubMed] [Google Scholar]
- Mays GP, Mamaril CB, & Timsina LR (2016). Preventable death rates fell where communities expanded population health activities through multisector networks. Health Affairs, 35(11), 2005–2013. 10.1377/hlthaff.2016.0848 [DOI] [PubMed] [Google Scholar]
- Mendelson SG, McNeese-Smith D, Koniak-Griffin D, Nyamathi A, & Lu MC (2008). A community-based parish nurse intervention program for Mexican American women with gestational diabetes. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 37(4), 415–425. 10.1111/j.1552-6909.2008.00262.x [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, & PRISMA Group (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6(7), e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan AU, Dupuis R, D’Alonzo B, Johnson A, Graves A, Brooks KL, McClintock A, Klusaritz H, Bogner H, Long JA, Grande D, & Cannuscio CC (2016). Beyond books: Public libraries as partners for population health. Health Affairs, 35(11), 2030–2036. 10.1377/hlthaff.2016.0724 [DOI] [PubMed] [Google Scholar]
- Murphy SME, Hough DE, Sylvia ML, Sherry M, Dunbar LJ, Zollinger R, Richardson R, Berkowitz SA, & Frick KD (2018). Going beyond clinical care to reduce health care spending: Findings from the J-CHiP community-based population health management program evaluation. Medical Care, 56(7), 603–609. 10.1097/MLR.0000000000000934 [DOI] [PubMed] [Google Scholar]
- Noh E, Potthoff S, & Begun JW (2018). A taxonomy of hospitals based on partnerships for population health management. Health Care Management Review, 45(4), 321–331. 10.1097/HMR.0000000000000230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oppenheim CE, Axelrod K, Menyongai J, Chukwuezi B, Tam A, Henderson DC, & Borba CPC (2019). The HEAAL Project: Applying Community-Based Participatory Research (CBPR) methodology in a health and mental health needs assessment with an African immigrant and refugee faith community in Lowell, Massachusetts. Journal of Public Health Management and Practice, 25(1), E1–E6. 10.1097/PHH.0000000000000707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prybil L, Scutchfield FD, Killian R, Kelly A, Mays GP, Carman A, Levey S, McGeorge A, & Fardo DW (2014). Improving community health through hospital-public health collaboration: Insights and lessons learned from successful partnerships. UKnowledge, https://uknowledge.uky.edu/cgi/viewcontent.cgi?article=1001&context=hsm_book
- Public Health Accreditation Board. (n.d.). About PHAB. https://phaboard.org/about/
- Sadowski LS, Kee RA, VanderWeele TJ, & Buchanan D (2009). Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: A randomized trial. JAMA, 301(17), 1771–1778. 10.1001/jama.2009.561 [DOI] [PubMed] [Google Scholar]
- Sampson G, Miner Gearin KJ, & Boe M (2015). A rural local health department-hospital collaborative for a countywide community health assessment. Journal of Public Health Management and Practice, 21(1), 23–30. 10.1097/PHH.0000000000000088 [DOI] [PubMed] [Google Scholar]
- Sandberg SF, Erikson C, Owen R, Vickery KD, Shimotsu ST, Linzer M, Garrett NA, Johnsrud KA, Soderlund DM, & DeCubellis J (2014). Hennepin health: A safety-net accountable care organization for the expanded Medicaid population. Health Affairs, 33(11), 1975–1984. 10.1377/hlthaff.2014.0648 [DOI] [PubMed] [Google Scholar]
- Schettler T (2006). Toward an ecological view of health: An imperative for the twenty-first century. The center for health design and health care without harm. https://www.healthdesign.org/system/files/Toward%20an%20Ecological%20View%20of%20Health_0.pdf [Google Scholar]
- Sherry M, Wolff JL, Ballreich J, DuGoff E, Davis K, & Anderson G (2016). Bridging the silos of service delivery for high-need, high-cost individuals. Population Health Management, 19(6), 421–428. 10.1089/pop.2015.0147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh SR, & Carlton EL (2017). Exploring the link between completion of accreditation prerequisites and local health departments’ decision to collaborate with tax-exempt hospitals around the community health assessment. Journal of Public Health Management and Practice, 23(2), 138–147. 10.1097/PHH.0000000000000409 [DOI] [PubMed] [Google Scholar]
- Stoto MA (2013). Population health in the Affordable Care Act Era (Vol. 1). AcademyHealth. http://www.gih.org/files/FileDownloads/Population%20Health%20in%20the%20Affordable%20Care%20Act%20Era.pdf [Google Scholar]
- Towe VL, Leviton L, Chandra A, Sloan JC, Tait M, & Orleans T (2016). Cross-sector collaborations and partnerships: Essential ingredients to help shape health and well-being. Health Affairs, 35(11), 1964–1969. 10.1377/hlthaff.2016.0604 [DOI] [PubMed] [Google Scholar]
- U.S. Internal Revenue Service. (n.d.). Community health needs assessment for charitable hospital organizations, Section 501(r)(3). https://www.irs.gov/charities-non-profits/community-health-needs-assessment-for-charitable-hospital-organizations-section-501r3
- Van Gelderen SA, Krumwiede KA, Krumwiede NK, & Fenske C (2018). Trialing the community-based collaborative action research framework: Supporting rural health through a community health needs assessment. Health Promotion Practice, 19(5), 673–683. 10.1177/1524839917754043 [DOI] [PubMed] [Google Scholar]
- Warren C, Lemieux AA, & Phoenix Bittner N (2019). Excellence in population health: A successful community-based care transitions program model. Professional Case Management, 24(1), 39–45. 10.1097/NCM.0000000000000303 [DOI] [PubMed] [Google Scholar]
- Wilson KD, Mohr LB, Beatty KE, & Ciecior A (2014). Describing the continuum of collaboration among local health departments with hospitals around the community health assessments. Journal of Public Health Management and Practice, 20(6), 617–625. 10.1097/PHH.0000000000000030 [DOI] [PubMed] [Google Scholar]
- Woods-Jaeger BA, Sexton CC, Gardner B, Siedlik E, Slagel L, Tezza V, & O’Malley D (2018). Development, feasibility, and refinement of a toxic stress prevention research program. Journal of Child and Family Studies, 27(11), 3531–3543. 10.1007/s10826-018-1178-1 [DOI] [Google Scholar]


