Abstract
The COVID-19 pandemic has caused millions of deaths and massive societal distress worldwide. Therapeutic solutions are urgently needed, but de novo drug development remains a lengthy process. One promising alternative is computational drug repurposing, which enables the prioritization of existing compounds through fast in silico analyses. Recent efforts based on molecular docking, machine learning, and network analysis have produced actionable predictions. Some predicted drugs, targeting viral proteins and pathological host pathways are undergoing clinical trials. Here, we review this work, highlight drugs with high predicted efficacy and classify their mechanisms of action. We discuss the strengths and limitations of the published methodologies and outline possible future directions. Finally, we curate a list of COVID-19 data portals and other repositories that could be used to accelerate future research.
Keywords: Computational drug repurposing, COVID-19, SARS-CoV-2, Docking and molecular dynamics, Structure-guided machine learning, Virus–host interaction network analysis
Introduction
The emergence of the novel coronavirus, known as SARS-CoV-2, became a defining event for 2019. The virus was first discovered in Wuhan, China. Transmitted via respiratory secretions, it quickly spread to neighboring countries and the rest of the world, causing COVID-19 (Coronavirus Disease 2019). To date, the COVID-19 pandemic has resulted in over four million deaths. The relatively high mortality, alongside the massive societal distress caused by the virus, stimulated intensive research on its biology, associated disease, and the development of vaccines and therapeutics.
SARS-CoV-2 is an enveloped, non-segmented, positive-sense RNA virus. It is part of the Coronaviridae family of viruses, which are known to cause respiratory infections in human hosts. SARS-CoV-2 is a beta coronavirus most closely related to SARS-CoV-1, with which it shares 79% genetic similarity, and more distally related to MERS-CoV, with which it shares approximately 50% of its genomic sequence.1, 2 Several proteins encoded by the SARS-CoV-2 viral genome have been implicated in its pathogenesis. The spike protein, responsible for viral entry, binds to the angiotensin converting enzyme 2 (ACE2) receptor, which is broadly expressed in human tissues.3, 4 Other viral proteins have key roles in the viral transcriptase–replicase complex (RdRp, Mpro/3CL, PLPro, helicase).5, 6, 7
The defining features of COVID-19 are a high rate of asymptomatic spread and high incidence of life-threatening complications.1, 8, 9, 10, 11 Owing to these complications and the lack of immunity in the population, the scientific and medical communities launched a large-scale research response that led to the development of multiple vaccines.12 Despite the proven efficacy of these vaccines, there is an urgent need for COVID-19 therapeutics due to vaccine distribution delays, failed immunity, vaccine hesitancy, and the possible emergence of resistant strains.13, 14
De novo development of therapeutics is a lengthy process, and is not a practical way to address the current pandemic.15 Drug repurposing is an emerging strategy in which existing therapeutics, that have already tested safe in humans, are repositioned to treat other diseases.16, 17 For example, clinical trials showed that remdesivir, an antiviral known for its effectiveness against the Ebola virus, was superior to placebo in shortening the time to recovery in COVID-19 patients.17, 18 Nevertheless, a systematic experimental screening of the potentially very large pool of drugs to be considered for repurposing is not feasible, due to both lengthy time-scales and prohibitive cost. To overcome this limitation, one promising alternative is computational drug repurposing.
Computational drug repurposing, broadly speaking, uses algorithms and massive database information to prioritize drugs for repositioning.19, 20, 21, 22, 23, 24, 25 One major advantage of computational approaches is the potential for fast large-scale screenings. Another major advantage is the potential to identify previously unknown benefits of existing drugs in disease contexts that are radically different from the original intended target conditions. By contrast, experimental drug repurposing is typically restricted to closely related disease contexts.
Multiple reviews in the area of computational repurposing of drugs have focused on drugs and mechanisms of action with potential for use against COVID-19, regardless of the specific computational methods used for prediction.26, 27, 28, 29 Other works have reviewed progress and perspectives relating to artificial intelligence-based methods.30, 31 Additional, more comprehensive, reviews have extended the methodological classes further to include network-, structure-, and signature-based drug repurposing methods.32, 33, 34
Our review, like that of Galindez et al.,33 is positioned to include both a careful curation of the many published methods and the identification of the most promising drug predictions. While Galindez et al.33 focused on generalized workflows in each method class, we provide a more in-depth review of selected works, aiming to illustrate the details of drug repurposing strategies that have resulted in experimentally validated drug predictions. In addition, a novel aspect of our review is the introduction of early progress in the category of text mining for COVID-19 drug repurposing.
The objectives of this review are: (1) the identification of published works that produce drug predictions that have been validated either in vitro or in vivo; (2) classification of the corresponding computational techniques, with a detailed presentation of selected works; (3) summarization of drug candidates and the mechanisms of pathogenesis that would be modulated; and (4) curation of the main data sources and COVID-19-specific portals. Finally, this review aims to guide future work in the field.
Classification of computational approaches for the repurposing of drugs against COVID-19
For a global view of efforts on computational drug repurposing, we conducted a manual curation of the literature and analyzed the COVID-19 Drug and Gene Set Library.35 This resource includes both computationally predicted and experimentally validated drug candidates along with the associated publications. The COVID-19 Drug and Gene Set Library is one of the most comprehensive crowdsourcing initiatives to integrate drug and gene sets related to COVID-19 research.
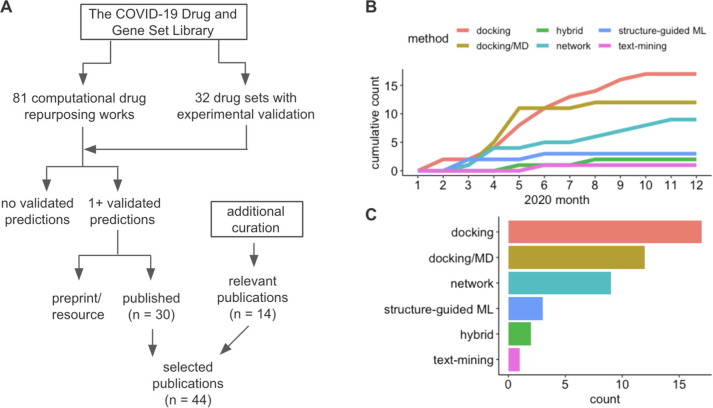
We defined selection criteria for inclusion in this review to identify the most methodologically sound manuscripts that have undergone rigorous peer review, sufficient methodological diversity and the most promising drug candidate predictions (Fig. 1 A). First, we applied two selection criteria to the COVID-19 Drug and Gene Set Library: the presence of a computational prediction for at least one experimentally validated compound; and publication of the associated paper in a peer-reviewed journal (excluding preprints, technical reports or other resources). Second, we manually curated relevant published works that are not yet in the COVID-19 Drug and Gene Set Library to increase coverage of the different methodological areas and to incorporate other major publications. In all, we include 44 peer-reviewed manuscripts (Fig. 1A). Consistent with previous reviews in the field of computational drug repurposing,19, 20, 21, 22, 23, 24, 25 we group the selected works into the following categories: molecular docking, molecular docking with follow-up molecular dynamics simulations, structure-guided machine learning, network-based methods, hybrid methods, and text mining.
Figure 1.
Selection and classification of works on computational drug repurposing for COVID-19. A. To identify the most effective computational drug repurposing works, we used the COVID-19 Drug and Gene Set Library,35 complemented by manual curation of the literature. The selection criteria aimed to identify methods that resulted in at least one predicted compound that was validated with further experiments. B. We classified the selected works into six groups: docking, docking/MD (molecular dynamics), network, structure-guided machine-learning (ML), hybrid and text mining. The publication trends for these groups in 2020 are shown. C. The final numbers of publications in each category included in our review.
Our review of the literature required the manual curation of manuscripts and drug predictions that, given the urgency of the pandemic, are being published at an exceptionally rapid rate. Thus, we restricted our curation to a time frame between the onset of the pandemic and January 2021. Analysis of publication trends during this time showed a very early production of works on molecular docking, with and without molecular dynamics simulations, followed by the publication of works on network-based approaches, structure-guided machine learning, and hybrid methods (Fig. 1B). Currently, the majority of the published works are in the docking category (39%), docking with follow-up molecular dynamics simulations (27%), network-based approaches (20%), structure-guided machine learning (7%), and hybrid methods (5%) (Fig. 1C). To date, the text-mining category has received relatively little attention, with only one published manuscript.36 Text-mining approaches may be underrepresented in the context of COVID-19 because they look for previously unrecognized connections between drug targets and diseases, but the genes involved in COVID-19 pathogenesis are still largely unknown.
Molecular docking
In the context of drug repurposing for the development of therapeutics against viral infections, docking techniques assess the fitness of an interaction between small molecules and viral proteins with a known 3D structure.22 The fitness (or binding affinity) is commonly computed as a potential energy, which is a function of force fields acting on the interacting molecular particles. Lower potential energy values (higher binding affinity) correspond to more stable conformations for complexes involving the small molecule and the viral protein, and are more likely to be associated with neutralization of the viral protein function by the ligand. Thus, small molecules that have high binding affinity for viral proteins are prioritized as potentially repurposable drugs. The well-established methods and software packages for docking approaches include GLIDE,37 AutoDock Vina,38 and SwissDock.39 The packages differ from one another in terms of the employed algorithms, scoring methods, docking type (flexible or rigid), and docking elements (for example, protein–protein, protein–ligand, protein–peptide). Parks and Smith40 provided a recent perspective on the potential advantages of molecular docking for quick repurposing of drugs for use against SARS-CoV-2.
The earliest studies faced the challenge of the lack of a solved structure for SARS-CoV-2 viral proteins. One way to circumvent this problem is to rely on the conservation of sequence and assume 3D structure conservation between SARS-CoV-2 and other coronaviruses, particularly SARS-CoV-1. For example, some early works predicted drug candidates targeting SARS-CoV-2 Mpro/3CL by leveraging the sequence and structure conservation of key protein residues in SARS-CoV-1 and SARS-CoV-2 inhibitor-binding pockets.41
A more principled way to overcome the challenge of unsolved viral protein structure is homology modelling.42 Homology modeling refers to the construction of an atomic-resolution model of the protein of interest (e.g. SARS-CoV-2 Mpro/3CL) based on its amino acid sequence and an experimental three-dimensional structure of a homologous protein (e.g. SARS-CoV-1 Mpro/3CL).43 For example, Wu et al.44 systematically applied homology modeling to all of the proteins encoded by SARS-CoV-2 genes, predicting 19 structures. The authors then used these predicted structures to perform molecular docking against compound libraries such as the ZINC drug database45 and a database of natural products. The study identified 78 commonly used antiviral drugs, including those currently on the market and undergoing clinical trials, as potential targets for SARS-CoV-2 Mpro/3CL (almitrine, carvedilol, telmisartan, conivaptan), RdRp (idarubicin), and PLpro (ribavirin). Additional studies have followed a similar strategy, leveraging homology modeling of the SARS-CoV-2 proteins RdRp,46, 47 Mpro/3CL,48 Plpro,49 helicase,50 and the spike protein,51 as well as the human protein TMPRSS252, 53 in their docking studies. After the crystal structures of SARS-CoV-2 viral proteins were resolved, a second wave of papers applied docking methods directly to these solved structures to predict additional drug targets.54, 55, 56, 57, 58, 59, 60 Interestingly, the predictions made by docking methods that used solved structures largely differed from those made using methods that leveraged homology modeling, with ribavirin being the most notable prediction made by methods in both categories.
Next, we illustrate how homology modeling, molecular docking and experimental techniques can be successfully combined by looking in depth at the study by Jin et al.61 In an effort to develop drugs against human coronaviruses, an earlier study by Yang et al.62 had found an MPro/3CL substrate recognition pocket that is highly conserved in the genus Coronavirus.62 On the basis of this finding, Yang et al.62 designed a wide-spectrum inhibitor of Mpro/3CL, named N3, that showed antiviral activity against SARS-CoV-1 and MERS. Jin et al.61 started by constructing a homology model for SARS-CoV-2 Mpro/3CL, and used molecular docking to ascertain that N3 can target the modeled Mpro/3CL. Next, Jin et al.61 experimentally assessed the efficacy of N3 for SARS-CoV-2 Mpro/3CL through analysis of binding kinetics, showing potent inhibition. In addition, the study determined the crystal structure of SARS-CoV-2 Mpro/3CL in complex with N3. The determined structure helped reveal a substrate-binding pocket highly conserved among Mpro/3CL in all coronaviruses. This served as a model for in silico screening of candidate inhibitors to target SARS-CoV-2 Mpro/3CL. Using the GLIDE docking software package, the analysis identified cinanserin, a well-characterized serotonin antagonist previously shown to inhibit SARS-CoV-1 Mpro/3CL,63 as a potential inhibitor of SARS-CoV-2 Mpro/3CL. To discover other potential Mpro/3CL inhibitors, Jin et al.61 used a fluorescence resonance energy transfer assay to screen a library of about 10,000 compounds consisting of approved drugs, clinical-trial drug candidates and natural products. The primary candidates included the approved drug disulfiram, as well as the clinical-trial drug candidate ebselen, which had shown efficacy against other viruses.64, 65, 66 Further in vitro experiments measuring viral replication in cell-based assays confirmed strong antiviral activity for N3 and ebselen.
Although docking methods can assess the fitness of an interaction between a drug and its intended target, they typically predict a large number of potential drug candidates. An effective way to restrict this pool of candidates is provided by Molecular Dynamics (MD) simulations. Docking methods are based on a static description of the interactions between drugs and targets, whereas MD gives a view of their dynamic interactions by analyzing the motion of atoms and molecules over time. Because molecular systems typically consist of a vast number of particles, the computational cost of MD simulations can be considerable. Therefore, it is computationally prohibitive to employ MD simulations to screen systematically against large drug databases, and MD simulations are typically applied to the most promising targets preselected through docking. MD and docking methods complement each other, leading to more reliable predictions and to less follow-up experimental work. Multiple software packages for MD simulations are available, including GROMACS,67 and AMBER.68 MD simulations, in combination with molecular docking, have been used to identify drug candidates against SARS-CoV-2 Mpro/3CL,53, 69, 70, 71, 72, 73, 74 RdRp,75 nsp16 and nsp10,76 against the human protein ACE2,77 and against the complex between the SARS-CoV-2 spike protein and ACE2.51, 78
Structure-guided machine-learning approaches
The recent rapid growth of drug-related data sets, as well as of open data initiatives, has led to new developments in machine-learning methods, especially in deep-learning techniques. Docking methods compute binding affinity using the detailed molecular structures of drugs and their targets, whereas machine-learning models use simplified vector representations of these structures. In the simplest case, for example, the so-called ‘fingerprint’ representation of a molecule is a vector of the structural fragments in the molecule. Machine-learning models require a training set that pairs up input features, that is molecular descriptors of drugs and their targets (such as their molecular fingerprints), and outputs such as binding affinities. Like docking methods, trained machine-learning models produce a prediction that is an estimate of the binding affinity between a drug candidate and its target proteins, either viral or host. When compared to docking, machine-learning models have additional advantages in that (1) they can be applied in the absence of a solved 3D protein structure, which was the case for some early papers using this approach and (2) the calculation of the binding affinity is more computationally efficient.
Focusing on the SARS-CoV-2 Mpro/3CL, Gao et al.79 proposed a machine-learning-based approach in which they compiled a carefully selected training set of 314 SARS-CoV-1 or SARS-CoV-2 Mpro/3CL protease inhibitors and their binding affinities collected from single protein experiments. The input variables for each inhibitor were constructed by encoding its high-dimensional biomolecular interactions with Mpro/3CL in a low-dimensional representation. A gradient boosting decision tree model showed good performance (Pearson correlation between predicted and true binding affinities of 0.79). Gao et al.79 then used the model to predict the binding affinities between the SARS-CoV-2 Mpro/3CL protease and 1553 US Food and Drug Administration (FDA)-approved drugs as well as 7012 investigational or off-market drugs. Among the FDA-approved drugs with predicted high-affinity scores were chloroxine (an antibacterial drug that belongs to the same family as chloroquine, but with a different predicted mechanism of action), demexiptiline (a tricyclic antidepressant) and fluorouracil (an antineoplastic). Among investigational compounds, the top result was debio-1347 (a fibroblast growth factor receptor (FGFR) inhibitor under investigation for the treatment of solid tumors). Interestingly, the predicted binding affinity of debio-1347 for SARS-CoV-2 Mpro/3CL was higher than that of any of the FDA-approved drugs, indicating the potential of debio-1347 for COVID-19 repurposing.
Batra et al.80 trained a structure-based machine-learning model to repurpose drug candidates against the spike protein and the spike–human ACE2 interface complex. The model used as input a set of structural and physicochemical features that capture the interactions between the drug molecule and the target proteins at various spatial scales. As output, the model predicted the corresponding AutoDock Vina score. Predictions were based on a random forest model trained on docking-generated binding affinities. Top-scoring ligands, including FDA-approved antivirals (such as valaciclovir) and antibacterials (such as sulfamethoxazole), were further validated in silico by all-atom docking studies.
Studies by Beck et al.81 and by Ton et al.82 employed deep-learning-based models, called Molecule Transformer–Drug Target Interaction (MT–DTI) and Deep Docking, respectively, to predict drug–target interactions. MT-DTI was trained with a database of approximately a billion compounds combining data from the BindingDB database83 and the Drug Target Common database,84 and was used to predict the binding affinity between SARS-CoV-2 proteins and 3411 FDA-approved drugs. Interestingly, the predictions included drug candidates that are able to target multiple viral proteins simultaneously. For example, atazanavir was predicted to bind SARS-CoV-2 Mpro/3CL, RdRp, and helicase. Similarly, ganciclovir was predicted to bind to three subunits of the replication complex. Deep Docking, a recently developed deep-learning platform shown to provide accurate and fast approximations of docking outcomes, enabled a virtual screening of the entire ZINC library of over 109 compounds against Mpro/3CL.45 Analysis of the top 1000 candidate inhibitors showed good chemical diversity and superior docking scores relative to those of known Mpro/3CL inhibitors. This method demonstrates the plausibility of performing exhaustive virtual screening, although the large number of predictions make it difficult to evaluate the success rate and the overall clinical applicability.
Network-based approaches
During the viral life cycle, the virus interacts with multiple components of the host cell. Previously described approaches have aimed to identify inhibitory molecules that directly target viral proteins. An alternative therapeutic option is to target the host or the virus–host interactome, typically using techniques from network pharmacology. The host interactome consists of human proteins as nodes and their interactions as edges, drawing upon various repositories of protein–protein interactions (PPI). The virus–host interactome extends this network by including viral proteins and their interactions with host proteins, typically leveraging high-throughput experiments. Additional data, such as transcriptomics, are used to derive subnetworks that are relevant to the disease under study, in this case COVID-19. Finally, databases of drug targets are utilized to predict druggable nodes in these subnetworks, identifying potential therapeutics that can perturb key processes of COVID-19 pathology.
Early papers that aimed to identify COVID-19 disease-relevant subnetworks needed to overcome the lack of data on interactions between SARS-CoV-2 and human proteins. Alakwaa85 and Cava et al.86 focused solely on host networks centered around ACE2, which is broadly expressed and is critical for SARS-CoV-2 cellular entry. They identified ACE2-associated networks derived from the analysis of gene expression in lung tissue transcriptomes in the public domain (e.g. GTEx87), and mapped databases of drug perturbations onto these gene sets. The work of Zhou et al.88 built upon a similar strategy and constructed a broader pan Coronavirus–host interactome network, which included a set of 119 host proteins associated with previously characterized human, mouse, and avian Coronaviruses. The drug repurposing methodology rested on the idea that for a drug to be effective, its targets should be either in the Coronavirus–host interactome or in close proximity to the interactome within the global human PPI network. Guided by this idea, alongside additional information such as transcriptomics data, literature-reported antiviral evidence and known side effects, the authors prioritized four classes of drugs. These included estrogen receptor modulators, angiotensin receptor blockers, immunosuppressant or antineoplastic agents, and anti-inflammatory agents. Finally, Zhou et al.88 predicted three potentially synergistic drug combinations for COVID-19: sirolimus (immunosuppressor) + dactinomycin (RNA synthesis inhibitor), toremifene (estrogen receptor modulator) + emodin (antiviral agent), and mercaptopurine (antineoplastic agent) + melatonin (anti-inflammatory agent).
Network-based repurposing strategies require high-confidence information on interactions between viral and human proteins. In contrast to the computationally derived interactome in the Zhou et al.88 study, Gordon et al. 89 experimentally identified 332 interactions between SARS-CoV-2 and human proteins. For each viral protein, a set of interacting host proteins was determined using affinity purification mass spectrometry, and assessed via immunological pathway analysis. This analysis revealed that the interacting host proteins participate in major cellular processes including DNA replication, epigenetic and transcriptional regulation, multiple innate immune pathways, and host translational machinery. Next, the authors predicted 69 agents, including FDA-approved drugs, that would disrupt host proteins and cellular processes potentially hijacked during SARS-CoV-2 infection. Further experiments revealed the antiviral activity of two broad classes of active compounds: those impinging on the translational machinery of the host needed for viral biogenesis, and those modulating the sigma1 and sigma2 receptors (chaperone proteins at the endoplasmic reticulum). Translation inhibitors (such as zotatifin and aplidin/plitidepsin) and sigma receptor ligands that have antiviral activity (such as haloperidol and clemastine/cloperastine) were identified as potential candidates for repurposing of drugs against COVID-19.
Bouhaddou et al.90 performed the first proteomics and phosphoproteomics analysis to explore how host pathways rewire upon SARS-CoV-2 infection. The study revealed a prominent role of phosphorylation events in modulating the cell cycle and cytoskeletal organization of infected cells. The strategy for drug repurposing hinged on detecting changes in phosphorylation states between SARS-CoV-2-infected and control cells. These identified changes were then mapped to changes in the activity of 97 kinases linked by database knowledge with their substrates.91 Of note, several inferred kinases were members of the virus–host PPI map generated by Gordon et al.89 Finally, Bouhaddou et al.90 looked for drugs that were able to inhibit the identified kinases, producing 87 drug candidates. In vitro assays involving 68 out of these 87 kinase inhibitors, including silmitasertib (an inhibitor of CK2), gilteritinib (an inhibitor of AXL), and ARRY-797 (an inhibitor of p38) demonstrated strong antiviral activity.
More recent studies took advantage of the increasing availability of transcriptomics data, which make it possible to identify SARS-CoV-2-regulated genes and pathways, and their overlap with drug-modulated genes.92, 93 By applying network proximity measures to multi-omics data from diverse tissues, Zhou et al.94 revealed similarities between COVID-19 and other pathologies, including inflammatory bowel disease and asthma. The shared pathological processes could suggest candidates for repurposing in COVID-19.
Hybrid methodologies
An important study of Bojkova et al., 95 which makes and validates multiple predictions, does not fit the standard computational drug repurposing classification. We place this study in the ‘Hybrid’ category because it integrates diverse computational techniques as well as experimental work.
To identify host pathways that are modulated by SARS-CoV-2 infection, Bojkova et al.95 established a novel cell culture model using a human epithelial carcinoma cell line. The SARS-CoV-2 infection profile, comprising both viral and host proteins, was quantified through translatome and proteome analysis at multiple time points within 2–24 hours after infection. First, the authors identified host proteins whose translation kinetics showed high correlation with those of viral proteins. Network and enrichment analyses of these proteins showed a strong increase in the host translation machinery, suggesting that translation inhibitors may reduce SARS-CoV-2 replication. This hypothesis was validated using two translation inhibitors, cycloheximide and emetine. To gain further insight into host proteome changes after infection, Bojkova et al. 95 performed hierarchical clustering of the host proteins’ expression profiles over time. This revealed an upregulated cluster of proteins that was enriched in spliceosome components and carbon metabolism, suggesting that targeting these two pathways may prevent SARS-CoV-2 replication. Both hypotheses were validated using, respectively, pladienolide B (a spliceosome inhibitor) and 2-deoxy-D-glucose (an inhibitor of hexokinase implicated in carbon metabolism). Additional correlation analysis of the kinetics of host and viral proteins showed that SARS-CoV-2 replication can be also inhibited using ribavirin and NMS-873 (a compound targeting the protein homeostasis machinery). Altogether, this work revealed that SARS-CoV-2 infection modulates critical host functions such as splicing, diverse metabolism sub-pathways, and proteostasis. Drugs that interfere with these pathways can be successfully repurposed to prevent SARS-CoV-2 replication in a human cell line and are good candidates for further testing in clinical settings for COVID-19.
Mining of text and healthcare records
The compilation of knowledge on COVID-19 has grown exponentially since the beginning of the pandemic. Several initiatives, such as the COVID-19 Open Research Dataset (CORD-19) and LitCovid, have made the published work more easily accessible.96, 97 This opens up great opportunities for analysis based on text mining and natural language processing. A recent publication by Wang et al.97 provides a review of the different text-mining systems and their applications to COVID-19 research, including information retrieval, automated annotation, and drug repurposing.98 The COVID-19 Drug Repository is the first significant work on computational drug repurposing based on text mining.36 The goal of this repository, which integrates data from PubMed, clinical trials and drug databases, is to centralize information on drugs against COVID-19 in a structured framework. The available information includes drug descriptions, side effects, pharmacology-oriented data, and drug–gene interactions. The resource makes it possible to identify putative repurposing candidates by analyzing omics data in conjunction with mined drug–target interactions.
More generally, text mining can be used to derive ‘knowledge graphs’. These are models of entities and relationships in a particular domain (for example, COVID-19 research) that can support the inference of novel relationships. In our context, a novel relationship could represent the potential efficacy of an existing drug against COVID-19.98 Finally, another promising research direction is the mining of electronic health records, prescription records and medical insurance claims.99 As these data types accumulate in the context of COVID-19, frameworks that identify new uses for on-market prescription drugs by systematically analyzing healthcare databases can be applied.100 Although still in their early stages, the mining of text and healthcare records will become an increasingly important tool in addressing the information overload, and in generating new hypotheses for drug repurposing.
Summary and conclusions
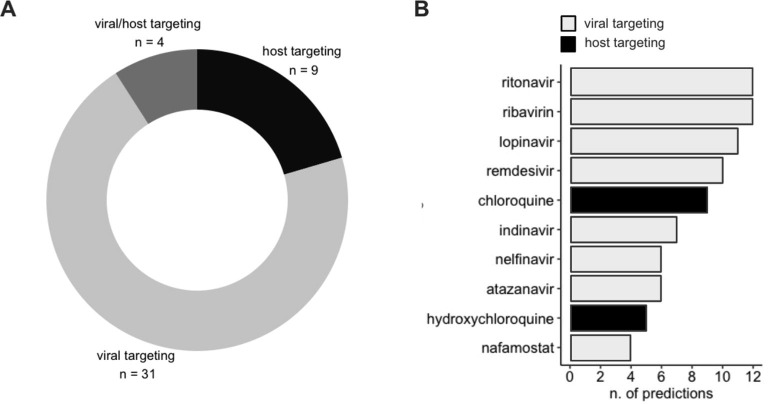
Computational drug repurposing for SARS-CoV-2 has homed in on two main mechanisms of action (Table 1 ). The most frequent mechanism is the direct inhibition of SARS-CoV-2 viral proteins (Fig. 2 A, seen in 31 of 44 reviewed works). The criterion for repurposing is the high binding affinity of the drugs to viral proteins, which is estimated using molecular docking or machine learning. This strategy has previously led to successful repurposing of antimicrobial drugs, including inhibitors of the Zika Virus.17 In the context of SARS-CoV-2, potentially repurposable drugs include multiple inhibitors of RdRp, Mpro/3CL protease, and other viral proteins. We found extensive overlap between the drug compounds predicted by the reviewed works. Many commonly used antivirals that have garnered international attention and have been used clinically in the treatment of COVID-19,101, 102 such as ritonavir and ribavirin, were predicted by up to 12 different computational approaches (Fig. 2B).
Table 1.
List of FDA-approved and investigational compounds predicted by computational drug repurposing methods to be effective against COVID-19. The predicted mechanism of action and current indication is included where available. Hyperlinks are provided for compounds in clinical trials. *Compound failing experimental validation or clinical trial.
| Drug Name | Predicted MOA | Predicted Class | Current indication | Reference | Validation |
|---|---|---|---|---|---|
| Bedaquiline | inhibitor of MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | Antibacterial | 101 | In vitro (cell culture) |
| Carmofur | inhibitor of MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | Antineoplastic | 61 | In vitro (cell culture & FRET assay) |
| Cinanserin | inhibitor of MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | No current pharmaceutical use | 63 | In vitro (tissue culture) |
| Disulfiram | inhibitor of MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | Alcoholism medication | 61 | In vitro (cell culture & FRET assay) |
| Ebselen | inhibitor of MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | Potential diabetes medication | 61 | In vitro (cell culture & FRET assay) |
| N3 | inhibitor of MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | No current pharmaceutical use | 61 | In vitro (cell based assays) |
| PX-12 | inhibitor of MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | Potential antineoplastic medication | 61 | In vitro (cell culture & FRET assay) |
| Shikonin | inhibitor of MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | Homeopathic medication | 61 | In vitro (cell culture & FRET assay), |
| TDZD-8 | inhibitor of MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | Potential Alzheimer's medication | 61 | In vitro (cell culture & FRET assay) |
| Tideglusib | inhibitor of MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | Potential Alzheimer's medication | 61 | In vitro (cell culture & FRET assay) |
| Baloxavir marboxil | inhibitor of MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | Antiviral for influenza | 102 | In vivo (clinical trial) |
| Mefloquine | inhibitor of MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | Antimalarial agent | 103 | In vitro (cell culture) |
| Almitrine | inhibitor of MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | Potential agent for the treatment of COPD | 104 | In vivo |
| Ritonavir | inhibitor of MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | Antiviral for HIV | 105 | In vivo (clinical trial)* |
| Indinavir | inhibitor of MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | Antiviral for HIV | 106 | In vitro (cell culture)* |
| Telmisartan | inhibitor of MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | Anti-hypertensive | clinical trial | In vivo (clinical trial) |
| Atazanavir | inhibitor of MPro/3CL, RdRp, Helicase | inhibitor of SARS-CoV-2 protein(s) | Antiviral for HIV | 107 | In vitro (cell culture) |
| Remdesivir | inhibitor of MPro/3CL, RdRp | inhibitor of SARS-CoV-2 protein(s) | Antiviral for Ebola, approved for use for SARS CoV-2 | 18 | In vivo (clinical trial) |
| Ciclesonide | inhibitor of MPro/3CL, NSP15 | inhibitor of SARS-CoV-2 protein(s) | Agent for the treatment of Asthma (anti-inflammatory) | 108 | In vitro (cell culture) |
| Sofosbuvir | inhibitor of RdRp | inhibitor of SARS-CoV-2 protein(s) | Antiviral for HepC | clinical trial | In vivo (clinical trial) |
| Hydroxychloroquine (HCQ) | inhibitor of RdRp | inhibitor of SARS-CoV-2 protein(s) | Antimalarial agent | 109 | In vivo (clinical trial)* |
| Favipiravir | inhibitor of RdRp | inhibitor of SARS-CoV-2 protein(s) | Antiviral agent | clinical trial | In vivo (clinical trial) |
| Ribavirin | inhibitor of PLpro | inhibitor of SARS-CoV-2 protein(s) | Antiviral, broad-spectrum | 110 | In vivo (clinical trial)* |
| Amodiaquine | based on similarity to HCQ | inhibitor of SARS-CoV-2 protein(s) | Anti-malarial | 111 | In vitro (cell culture) |
| Cycloheximide | protein translation inhibitor | inhibitor of host protein(s)/pathway(s) | No current pharmaceutical use | 95 | In vitro (cell culture) |
| Emetine | protein translation inhibitor | inhibitor of host protein(s)/pathway(s) | Antiprotozoal | 112 | In vitro (cell culture) |
| Rapamycin | mTOR inhibitor | inhibitor of host protein(s)/pathway(s) | Immunosuppressant with antifungal and antineoplastic properties | clinical trial | In vivo (clinical trial) |
| Toremifene | estrogen receptor modulators | inhibitor of host protein(s)/pathway(s) | Selective estrogen receptor modulator | 113 | In vitro (cell culture) |
| Tamoxifen | estrogen receptor modulators | inhibitor of host protein(s)/pathway(s) | Selective estrogen receptor modulator | 114 | In vitro (cell culture) |
| Chloroquine | sigma1 receptor of Endoplasmic Reticulum | inhibitor of host protein(s)/pathway(s) | Antiparasitic | 115 | In vitro (cell culture) |
| Merimepodib | inhibitor of host proteins interacting with SARS-CoV-2 Nsp14 | inhibitor of host protein(s)/pathway(s) | IMPDH inhibitor | clinical trial | In vivo (clinical trial) |
| Mycophenolic acid | inhibitor of host proteins interacting with SARS-CoV-2 Nsp14 | inhibitor of host protein(s)/pathway(s) | Immunosuppressant | 116 | In vitro (cell culture) |
| Silmitasertib | Kinase inhibitor | inhibitor of host protein(s)/pathway(s) | Potential antineoplastic | 90 | In vitro (cell culture) |
| Gilteritinib | Kinase inhibitor | inhibitor of host protein(s)/pathway(s) | Antineoplastic | 90 | In vitro (cell culture) |
| ARRY-797 | Kinase inhibitor | inhibitor of host protein(s)/pathway(s) | Potential cardiovascular agent | 90 | In vitro (cell culture) |
| MAPK13-IN-1 | Kinase inhibitor | inhibitor of host protein(s)/pathway(s) | Potential antineoplastic | 90 | In vitro (cell culture) |
| SB203580 | Kinase inhibitor | inhibitor of host protein(s)/pathway(s) | Potential antineoplastic | 90 | In vitro (cell culture) |
| Ralimetinib | Kinase inhibitor | inhibitor of host protein(s)/pathway(s) | Potential antineoplastic | 90 | In vitro (cell culture) |
| Apilimod | Kinase inhibitor | inhibitor of host protein(s)/pathway(s) | Antiviral and antineoplastic | 90 | In vitro (cell culture) |
| Imatinib | Kinase inhibitor | inhibitor of host protein(s)/pathway(s) | Antineoplastic | 116 | In vitro (cell culture) |
| Dinaciclib | Kinase inhibitor | inhibitor of host protein(s)/pathway(s) | Potential antineoplastic | 90 | In vitro (cell culture) |
| Camostat mesylate | TMPRSS2 inhibitor | inhibitor of host protein(s)/pathway(s) | Agent for treatment of pancreatitis | 117 | In vitro (cell culture) |
| Nafamostat mesylate | TMPRSS2 inhibitor | inhibitor of host protein(s)/pathway(s) | Anticoagulant | clinical trial | In vivo (clinical trial) |
| Lopinavir | Protease inhibitor | inhibitor of host protein(s)/pathway(s) | Antiretroviral | 112 | In vitro (cell culture) |
| Zotatifin | translation inhibitor | inhibitor of host protein(s)/pathway(s) | Potential antineoplastic | clinical trial | in vivo (clinical trial) |
| Colchicine | Anti-inflammatory | inhibitor of host protein(s)/pathway(s) | Anti-inflammatory | clinical trial | In vivo (clinical trial) |
| Melatonin | Anti-inflammatory | inhibitor of host protein(s)/pathway(s) | Anti-inflammatory | clinical trial | In vivo (clinical trial) |
| Siltuximab | IL6 inhibitor | inhibitor of host protein(s)/pathway(s) | Anti-inflammatory agent | 118 | In vivo |
| Tetrandrine | Calcium channel blocker | inhibitor of host protein(s)/pathway(s) | Agent for the treatment of hypertension | 119 | In vitro (cell culture) |
| Lacking validation | |||||
| Carvedilol | inhibitor of SARS-CoV-2 protein(s), MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | Treatment of high blood pressure, congestive heart failure | ||
| Conivaptan | inhibitor of MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | Treatment for hyponatremia | ||
| Chloroxine | inhibitor of MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | Antibacterial | ||
| Demexiptiline | inhibitor of MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | Antidepressant | ||
| Fluorouracil | inhibitor of MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | Antineoplastic | ||
| Debio-1347 | inhibitor of MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | Antineoplastic | ||
| Mercaptopurine | inhibitor of MPro/3CL | inhibitor of SARS-CoV-2 protein(s) | Antineoplastic agent with immunosuppressant properties | ||
| Emodin | inhibitor of MPro/3CL, Spike protein | inhibitor of SARS-CoV-2 protein(s) | Treatment of Polycystic kidney | ||
| Ganciclovir | inhibitor of MPro/3CL, RdRp, Helicase | inhibitor of SARS-CoV-2 protein(s) | Antiviral | ||
| Idarubicin | inhibitor of RdRp | inhibitor of SARS-CoV-2 protein(s) | Antineoplastic | ||
| Valaciclovir | inhibitor of Spike protein & Spike protein - ACE2 interface complex | inhibitor of SARS-CoV-2 protein(s) | Antiviral | ||
| Sulfamethoxazole | inhibitor of Spike protein & Spike protein - ACE2 interface complex | inhibitor of SARS-CoV-2 protein(s) | Antibacterial | ||
| Dactinomycin | RNA synthesis inhibitor | inhibitor of host protein(s)/pathway(s) | Antineoplastic | ||
| Plitidepsin | translation inhibitor | inhibitor of host protein(s)/pathway(s) | Antineoplastic | ||
| Haloperidol | sigma1/2 receptor of Endoplasmic Reticulum | inhibitor of host protein(s)/pathway(s) | Antipsychotic | ||
| Clemastine | sigma1/2 receptor of Endoplasmic Reticulum | inhibitor of host protein(s)/pathway(s) | Anti allergy | ||
| Cloperastine | sigma1/2 receptor of Endoplasmic Reticulum | inhibitor of host protein(s)/pathway(s) | Cough suppressant | ||
| Pladienolide B | spliceosome inhibitor | inhibitor of host protein(s)/pathway(s) | Potential antineoplastic | ||
| 2-deoxy-D-glucose | carbon metabolism | inhibitor of host protein(s)/pathway(s) | Potential antineoplastic and antiviral | ||
| NMS-873 | protein homeostasis machinery | inhibitor of host protein(s)/pathway(s) | No current pharmaceutical use | ||
Table 2.
Curated list of COVID-19-specific resources and repositories relevant to computational drug repurposing.
| Resource/ data type | Resource name | Website | Description | Reference | |
|---|---|---|---|---|---|
| COVID-19 platform | CORD-19 | https://www.kaggle.com/allen-institute-for-ai/CORD-19-research-challenge | Scholarly articles on COVID-19, SARS-CoV-2, and other related coronaviruses, with a focus on natural language processing and other AI techniques | 97 | |
| COVID-19 portfolio | https://icite.od.nih.gov/covid19/search/ | Publications and preprints on COVID-19 and SARS-CoV-2 | – | ||
| COVIDScholar | https://covidscholar.org/ | Search engine that utilizes natural language processing to aid in the search for COVID-19 articles | – | ||
| COVID-19 research explorer | https://covid19-research-explorer.appspot.com/ | Search engine for COVID-19 that operates on question-based searches | – | ||
| SPIKE-CORD | https://spike.covid-19.apps.allenai.org/search/covid19 | Search engine for CORD-19 which operates on query modes to perform extractive searches | – | ||
| Virus-CKB | https://www.cbligand.org/g/virus-ckb | Knowledgebase for research on COVID-19 and similar viral infections | 123 | ||
| SciSight | https://scisight.apps.allenai.org/ | Tool used to visualize the directions of the emerging literature network related to COVID-19 | – | ||
| KnetMiner | https://knetminer.org/COVID-19/ | Search engine that aids in COVID-19 related search queries based on keywords, gene lists, and genomic regions | – | ||
| COVID-19 Primer | https://covid19primer.com/dashboard | Tool that uses natural language processing (NLP) to summarize research trends, news coverage, and social media discussions on the topic of COVID-19 and SARS-CoV-2 | – | ||
| COVID-19 drug and gene set library | https://maayanlab.cloud/covid19/ | A collection of drug and gene sets related to COVID-19 research contributed by the community | 35 | ||
| CDC COVID-19 Databases and Journals | https://www.cdc.gov/library/researchguides/2019novelcoronavirus/databasesjournals.html | Compilation of selected databases and journals that can help researchers to find scholarly articles and data relating to COVID-19 | – | ||
| LitCovid | https://www.ncbi.nlm.nih.gov/research/coronavirus/ | A curated literature hub for tracking up-to-date scientific information about SARS-CoV-2 | 124 | ||
| iSearch COVID-19 portfolio | https://icite.od.nih.gov/covid19/search/ | An expert-curated database containing published papers and preprints | – | ||
| WHO COVID-19 research article database | https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov | A database gathering the latest international multilingual scientific findings and knowledge on COVID-19 | – | ||
| COVID-KOP | https://covidkop.renci.org/ | Biomedical reasoning system for data collected about the COVID-19 pandemic, including information on drugs, literature co-occurrences and phenotypes | 125 | ||
| HIT-COVID | https://akuko.io/post/covid-intervention-tracking | Quantification of the effectiveness of public health measures on SARS-CoV-2 transmission | 126 | ||
| COVID Moonshot | https://covid.postera.ai/covid | Crowdsourced initiative to accelerate the development of a COVID-19 antiviral | 127 | ||
| CIDO | http://www.ontobee.org/ontology/CIDO | Community-based ontology that supports COVID-19 knowledge and data standardization, integration, sharing, and analysis | 128 | ||
| COVEX | https://exbio.wzw.tum.de/covex/about | Online network and systems medicine platform for data analysis that integrates virus–human interactions for SARS-CoV-2 and SARS-CoV-1 | 129 | ||
| The COVIDome Project | https://www.ncbi.nlm.nih.gov/sars-cov-2/ | Collaborative effort to generate multidimensional datasets from biospecimens from COVID-19 patients and controls | – | ||
| NCBI SARS-CoV-2 Resource | https://www.ncbi.nlm.nih.gov/sars-cov-2/ | An expert-curated database which was developed to increase the useability of existing resources | – | ||
| PDBe COVID-19 | https://www.ebi.ac.uk/pdbe/covid-19 | 3D-structure data for large biological molecules, such as proteins and nucleic acids, that are specific to SARS-CoV-2 | 130 | ||
| Compound database | ZINC15 | https://zinc15.docking.org/ | 3D formats of purchasable compounds and their different properties, such as rings, substances, tranches, and patterns | 45 | |
| Drug response | PharmGKB | https://www.pharmgkb.org/ | Data on the impact of genetic variations on drug response and annotated information on drugs | 131 | |
| Drugs and drug targets | IUPHAR/BPS guide to pharmacology | https://www.guidetopharmacology.org/ | Information on drug targets, and on prescription and experimental medications that act on them | – | |
| DrugBank | https://www.drugbank.ca/ | Information on drugs and their chemical and pharmacological properties; this resource also contains information on drug targets and their sequences, structures, and pathways | 132 | ||
| Drug Target Commons Database | https://drugtargetcommons.fimm.fi/ | Bioactivity data for drugs and their targets | 84 | ||
| Drugs | Drug repurposing for COVID-19 | http://covid19.md.biu.ac.il/ | Database of existing drugs that have potential or proven efficacy against SARS-CoV-2 | – | |
| Binding affinities | BindingDB | https://www.bindingdb.org/bind/index.jsp | Information on the binding affinities between molecular entities and protein targets | 83 | |
| Gene | GenBank | https://www.ncbi.nlm.nih.gov/genbank/ | Publicly available DNA sequences | 133 | |
| EMBL-ENA | https://www.ebi.ac.uk/ena | Nucleotide sequencing information | 134 | ||
| GeneCards | https://www.genecards.org/ | Annotated and predicted human genes | 135 | ||
| CMAP | https://www.broadinstitute.org/connectivity-map-cmap | Gene expression profiles and disease-associated genes | 136 | ||
| MSigDB | https://www.gsea-msigdb.org/gsea/msigdb/index.jsp | Annotated gene sets that can be utilized with Gene Set Enrichment Analysis (GSEA) software | 137 | ||
| Protein | UniProt | https://covid-19.uniprot.org/uniprotkb?query=* | Information on protein sequence and annotation of SARS-CoV-2 | 138 | |
| Swiss-Prot | https://www.uniprot.org/statistics/Swiss-Prot | Part of UniProt, this resource includes protein sequences and their functional information | 139 | ||
| PDB | https://www.rcsb.org/ | 3D structure data for large biological molecules, such as proteins and nucleic acids | 130 | ||
| PRIDE | https://www.ebi.ac.uk/pride/ | Mass spectrometry proteomics and genomic data | 140 | ||
| CORUM | http://mips.helmholtz-muenchen.de/corum/ | Protein complexes, protein subunits, literature references, and experimental reports | 141 | ||
| Multi type | KEGG | https://www.genome.jp/kegg | Information on drugs, genes, proteins and pathways | 142 |
Figure 2.
Classification of predictions based on the mechanism of action. A. Proportions of reviewed works predicting drugs that target viral proteins, host proteins, or both. B. The most commonly predicted drugs, classified as either virus or host targeting. Several drugs have been predicted by multiple works.
The second mechanism is the inhibition of host pathways predicted by network-based and hybrid approaches (Fig. 2A, seen in 9 of 44 reviewed works). These methods identified host targets involved in virus life cycle, particularly entry and RNA synthesis. Progress in identifying inhibitors of host pathways that contribute to pathogenesis is critical, particularly for a virus that has already mutated enough to render some previously effective therapeutics significantly less potent. Of note, current methods are less effective in identifying drugs that target other key host pathways that contribute to pathology, such as aberrant immune responses and thrombosis, whose therapeutic manipulation showed promising results.103, 104, 105, 106 This may be due to a poor molecular understanding of the systems-level effects of SARS-CoV-2 infection. Finally, a few studies have identified both viral and host proteins as potential targets (Fig. 2A, seen in 4 of 44 reviewed works). These predictions were produced by docking and structure-based machine learning, which are not intrinsically limited to the identification of viral proteins as targets.
The overall strengths, limitations, and successful applications of the methodologies included in this review have been discussed previously.19, 20, 21, 22, 23, 24, 25 In the context of COVID-19, an additional challenge is the lack of solid prior biological knowledge. The knowledge required for each of the different method classes is being accumulated at different rates. For example, the SARS-CoV-2 protein structure, which is required for docking, was quickly solved for several viral proteins. On the other hand, the mapping of the virus–host interactome, which is needed for network approaches, is a research objective that will require longer-term effort. Therefore, efforts to assess the success rates of the different methods for COVID-19 drug repurposing are still premature. Regardless of the specific method being used, the preconditions for success go beyond target activity to encompass other key pharmacological aspects, such as safety, toxicity and drug–drug interactions. Furthermore, as noted by Edwards,107 the success rate of hypothesis-driven repurposing research far exceeds that of large-scale, hypothesis-free screenings. This concept is also evident in works of Gordon et al.,89 Jin et al.61 and Bojkova et al.95 reviewed here, which first produced data specifically for hypothesis generation, before validating the predictions in vitro. Going forward, the increasing accumulation of data, as well as improved knowledge of COVID-19 pathology, should enhance our ability to strike the right balance between hypothesis-driven screenings and the predominantly data-driven repurposing strategies reviewed here.
With this objective in mind, we have curated a list of COVID-19-specific data portals. We also include a list of other relevant resources typically employed by computational repurposing methods, both for COVID-19 and more broadly (Table 2 ). These repositories contain data describing gene and protein sequences and structures; drugs and drug targets; properties of chemical compounds; and biological networks and pathways. Furthermore, several -omics datasets, profiling SAR-CoV-2 infection in various tissues, have been published.108, 109, 110, 111, 112, 113 Although not exhaustive, our curated lists include the most commonly utilized repositories and provides a basis for future work.
Effective treatment of complex diseases, such as viral infections, may require the targeting of multiple host and viral processes. Severity and mortality of COVID-19 are highly dependent upon biological factors, such as older age, and upon pre-existing conditions, such as hypertension, diabetes, cardiovascular disease, or chronic obstructive pulmonary disease (COPD).114, 115, 116, 117 The optimal treatment is likely to depend on a specific patient’s characteristics, so future repurposing methods may account for variation in risk factors, leading to personalized treatments.
Combination therapies increase the spectrum of disease modulation, improving drug efficacy/toxicity ratios and combating drug resistance.118 A synergistic effect can be created by using several drugs that target different disease pathways.119 For example, combination drug therapy has become the gold standard in the treatment of cancer120 and in the treatment of several virus infections, notably HIV.121 The principle of ‘complementary exposure’,122 which optimizes drug effects over a large portion of the disease network, has predicted several synergistic drug combinations for the treatment of COVID-19. One example is sirolimus and dactinomycin, which inhibit mTOR signaling and RNA synthesis pathways, respectively. An important challenge and a promising objective for future computational drug repurposing is the ability to design effective drug combinations that target multiple COVID-19 pathological pathways.
Computational drug repurposing has led to remarkable success stories in several disease areas, including cancer, autoimmune diseases, and viral infections. Despite the many challenges, our review lays out the early promising steps towards successful computational repurposing for COVID-19.
Funding
This work was supported by the US National Institutes of Health (NIH) grant 5U19AI117873.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Biographies

Illya Aronskyy is a medical student at the Icahn School of Medicine at Mount Sinai, New York, NY. He graduated with a Bachelors in Science from Baruch College, where he conducted research on mitochondrial pathogenesis in familial amyotrophic lateral sclerosis (ALS) for which he received the Jonas E. Salk Scholarship.

Yosef Masoudi-Sobhanzadeh PhD is an Assistant Professor at Tabriz University of Medical Sciences (TUOMS) Research Center for Pharmaceutical Nanotechnology, Tabriz, Iran. His expertise is in the development of algorithms and data resources for biological applications.
References
- 1.Tay M.Z., Poh C.M., Rénia L., MacAry P.A., Ng L.F.P. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020;20(6):363–374. doi: 10.1038/s41577-020-0311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang H., Li X., Li T., Zhang S., Wang L., Wu X., Liu J. The genetic sequence, origin, and diagnosis of SARS-CoV-2. Eur J Clin Microbiol Infect Dis. 2020;39(9):1629–1635. doi: 10.1007/s10096-020-03899-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nitulescu G., Paunescu H., Moschos S., Petrakis D., Nitulescu G., Ion G., Spandidos D., Nikolouzakis T., Drakoulis N., Tsatsakis A. Comprehensive analysis of drugs to treat SARS-CoV-2 infection: mechanistic insights into current COVID-19 therapies (Review) Int J Mol Med. 2020;46(2):467–488. doi: 10.3892/ijmm10.3892/ijmm.2020.4608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lechien J.R., Radulesco T., Calvo-Henriquez C., Chiesa-Estomba C.M., Hans S., Barillari M.R., et al. ACE2 & TMPRSS2 expressions in head & neck tissues: a systematic review. Head Neck Pathol. 2021;15:225–235. doi: 10.1007/s12105-020-01212-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mousavizadeh L., Ghasemi S. Genotype and phenotype of COVID-19: their roles in pathogenesis. J Microbiol Immunol Infect. 2021;54(2):159–163. doi: 10.1016/j.jmii.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dai W., Zhang B., Jiang X.-M., Su H., Li J., Zhao Y., Xie X., Jin Z., Peng J., Liu F., Li C., Li Y., Bai F., Wang H., Cheng X.i., Cen X., Hu S., Yang X., Wang J., Liu X., Xiao G., Jiang H., Rao Z., Zhang L.-K., Xu Y., Yang H., Liu H. Structure-based design of antiviral drug candidates targeting the SARS-CoV-2 main protease. Science. 2020;368(6497):1331–1335. doi: 10.1126/science:abb4489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mittal A., Manjunath K., Ranjan R.K., Kaushik S., Kumar S., Verma V., Hobman T.C. COVID-19 pandemic: insights into structure, function, and hACE2 receptor recognition by SARS-CoV-2. PLoS Pathog. 2020;16(8):e1008762. doi: 10.1371/journal.ppat.1008762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perico L, Benigni A, Casiraghi F, Ng LFP, Renia L, Remuzzi G. Immunity, endothelial injury and complement-induced coagulopathy in COVID-19. Nat Rev Nephrol 17: 46–64. doi:10.1038/s41581-020-00357-4 [DOI] [PMC free article] [PubMed]
- 9.Yuki K., Fujiogi M., Koutsogiannaki S. COVID-19 pathophysiology: a review. Clin Immunol. 2020;215:108427. doi: 10.1016/j.clim.2020.108427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahmed M.U., Hanif M., Ali M.J., Haider M.A., Kherani D., Memon G.M., Karim A.H., Sattar A. Neurological manifestations of COVID-19 (SARS-CoV-2): a review. Front Neurol. 2020;11 doi: 10.3389/fneur.2020.00518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kochi A.N., Tagliari A.P., Forleo G.B., Fassini G.M., Tondo C. Cardiac and arrhythmic complications in patients with COVID-19. J Cardiovasc Electrophysiol. 2020;31(5):1003–1008. doi: 10.1111/jce:v31.510.1111/jce:14479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Amanat F., Krammer F. SARS-CoV-2 vaccines: status report. Immunity. 2020;52(4):583–589. doi: 10.1016/j.immuni.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou D., Dejnirattisai W., Supasa P., Liu C., Mentzer A.J., Ginn H.M., Zhao Y., Duyvesteyn H.M.E., Tuekprakhon A., Nutalai R., Wang B., Paesen G.C., Lopez-Camacho C., Slon-Campos J., Hallis B., Coombes N., Bewley K., Charlton S., Walter T.S., Skelly D., Lumley S.F., Dold C., Levin R., Dong T., Pollard A.J., Knight J.C., Crook D., Lambe T., Clutterbuck E., Bibi S., Flaxman A., Bittaye M., Belij-Rammerstorfer S., Gilbert S., James W., Carroll M.W., Klenerman P., Barnes E., Dunachie S.J., Fry E.E., Mongkolsapaya J., Ren J., Stuart D.I., Screaton G.R. Evidence of escape of SARS-CoV-2 variant B.1.351 from natural and vaccine-induced sera. Cell. 2021;184(9):2348–2361.e6. doi: 10.1016/j.cell.2021.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paltiel A.D., Schwartz J.L., Zheng A., Walensky R.P. Clinical outcomes of a COVID-19 vaccine: implementation over efficacy. Health Aff (Millwood) 2021;40(1):42–52. doi: 10.1377/hlthaff.2020.02054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DiMasi J.A., Florez M.I., Stergiopoulos S., Peña Y., Smith Z., Wilkinson M., Getz K.A. Development times and approval success rates for drugs to treat infectious diseases. Clin Pharmacol Ther. 2020;107(2):324–332. doi: 10.1002/cpt.v107.210.1002/cpt.1627. [DOI] [PubMed] [Google Scholar]
- 16.Pushpakom S., Iorio F., Eyers P.A., Escott K.J., Hopper S., Wells A., Doig A., Guilliams T., Latimer J., McNamee C., Norris A., Sanseau P., Cavalla D., Pirmohamed M. Drug repurposing: progress, challenges and recommendations. Nat Rev Drug Discov. 2019;18(1):41–58. doi: 10.1038/nrd.2018.168. [DOI] [PubMed] [Google Scholar]
- 17.Mercorelli B., Palù G., Loregian A. Drug repurposing for viral infectious diseases: how far are we? Trends Microbiol. 2018;26(10):865–876. doi: 10.1016/j.tim.2018.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beigel J.H., Tomashek K.M., Dodd L.E., Mehta A.K., Zingman B.S., Kalil A.C., Hohmann E., Chu H.Y., Luetkemeyer A., Kline S., Lopez de Castilla D., Finberg R.W., Dierberg K., Tapson V., Hsieh L., Patterson T.F., Paredes R., Sweeney D.A., Short W.R., Touloumi G., Lye D.C., Ohmagari N., Oh M.-D., Ruiz-Palacios G.M., Benfield T., Fätkenheuer G., Kortepeter M.G., Atmar R.L., Creech C.B., Lundgren J., Babiker A.G., Pett S., Neaton J.D., Burgess T.H., Bonnett T., Green M., Makowski M., Osinusi A., Nayak S., Lane H.C. Remdesivir for the treatment of Covid-19 – final report. N Engl J Med. 2020;383(19):1813–1826. doi: 10.1056/NEJMoa2007764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.D’Souza S., Prema K.V., Balaji S. Machine learning models for drug-target interactions: current knowledge and future directions. Drug Discov Today. 2020;25(4):748–756. doi: 10.1016/j.drudis.2020.03.003. [DOI] [PubMed] [Google Scholar]
- 20.Masoudi-Sobhanzadeh Y., Omidi Y., Amanlou M., Masoudi-Nejad A. Drug databases and their contributions to drug repurposing. Genomics. 2020;112(2):1087–1095. doi: 10.1016/j.ygeno.2019.06.021. [DOI] [PubMed] [Google Scholar]
- 21.Lotfi Shahreza M., Ghadiri N., Mousavi S.R., Varshosaz J., Green J.R. A review of network-based approaches to drug repositioning. Brief Bioinformatics. 2018;19:878–892. doi: 10.1093/bib/bbx017. [DOI] [PubMed] [Google Scholar]
- 22.Vanhaelen Q., Mamoshina P., Aliper A.M., Artemov A., Lezhnina K., Ozerov I., Labat I., Zhavoronkov A. Design of efficient computational workflows for in silico drug repurposing. Drug Discov Today. 2017;22(2):210–222. doi: 10.1016/j.drudis.2016.09.019. [DOI] [PubMed] [Google Scholar]
- 23.Tari L.B., Patel J.H. Systematic drug repurposing through text mining. Methods Mol Biol. 2014;1159:253–267. doi: 10.1007/978-1-4939-0709-0_14. [DOI] [PubMed] [Google Scholar]
- 24.Sliwoski G., Kothiwale S., Meiler J., Lowe E.W., Barker E.L. Computational methods in drug discovery. Pharmacol Rev. 2014;66(1):334–395. doi: 10.1124/pr.112.007336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Paranjpe M.D., Taubes A., Sirota M. Insights into computational drug repurposing for neurodegenerative disease. Trends Pharmacol Sci. 2019;40(8):565–576. doi: 10.1016/j.tips.2019.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Singh T.U., Parida S., Lingaraju M.C., Kesavan M., Kumar D., Singh R.K. Drug repurposing approach to fight COVID-19. Pharmacol Rep. 2020;72(6):1479–1508. doi: 10.1007/s43440-020-00155-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parvathaneni V., Gupta V. Utilizing drug repurposing against COVID-19 – efficacy, limitations, and challenges. Life Sci. 2020;259:118275. doi: 10.1016/j.lfs.2020.118275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Naveja JJ, Madariaga-Mazón A, Flores-Murrieta F, Granados-Montiel J, Maradiaga-Ceceña M, Alaniz VD, et al. Union is strength: antiviral and anti-inflammatory drugs for COVID-19. Drug Discov Today 26: 229–39. doi:10.1016/j.drudis.2020.10.018 [DOI] [PMC free article] [PubMed]
- 29.Mohamed K., Yazdanpanah N., Saghazadeh A., Rezaei N. Computational drug discovery and repurposing for the treatment of COVID-19: a systematic review. Bioorg Chem. 2021;106:104490. doi: 10.1016/j.bioorg.2020.104490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Keshavarzi Arshadi A., Webb J., Salem M., Cruz E., Calad-Thomson S., Ghadirian N., Collins J., Diez-Cecilia E., Kelly B., Goodarzi H., Yuan J.S. Artificial Intelligence for COVID-19 drug discovery and vaccine development. Front Artif Intell. 2020;3 doi: 10.3389/frai.2020.00065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhou Y., Wang F., Tang J., Nussinov R., Cheng F. Artificial intelligence in COVID-19 drug repurposing. Lancet Digit Health. 2020;2(12):e667–e676. doi: 10.1016/S2589-7500(20)30192-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dotolo S., Marabotti A., Facchiano A., Tagliaferri R. A review on drug repurposing applicable to COVID-19. Brief Bioinformatics. 2021;22:726–741. doi: 10.1093/bib/bbaa288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Galindez G., Matschinske J., Rose T.D., Sadegh S., Salgado-Albarrán M., Späth J., Baumbach J., Pauling J.K. Lessons from the COVID-19 pandemic for advancing computational drug repurposing strategies. Nat Comput Sci. 2021;1(1):33–41. doi: 10.1038/s43588-020-00007-6. [DOI] [PubMed] [Google Scholar]
- 34.Wang X., Guan Y. COVID-19 drug repurposing: a review of computational screening methods, clinical trials, and protein interaction assays. Med Res Rev. 2021;41(1):5–28. doi: 10.1002/med.v41.110.1002/med.21728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kuleshov M.V., Stein D.J., Clarke D.J.B., Kropiwnicki E., Jagodnik K.M., Bartal A., Evangelista J.E., Hom J., Cheng M., Bailey A., Zhou A., Ferguson L.B., Lachmann A., Ma'ayan A. The COVID-19 Drug and Gene Set Library. Patterns (N Y) 2020;1(6):100090. doi: 10.1016/j.patter.2020.100090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tworowski D, Gorohovski A, Mukherjee S, Carmi G, Levy E, Detroja R, et al. COVID19 Drug Repository: text-mining the literature in search of putative COVID19 therapeutics. Nucleic Acids Res 2021; 49: D1113–21. doi:10.1093/nar/gkaa969 [DOI] [PMC free article] [PubMed]
- 37.Friesner R.A., Banks J.L., Murphy R.B., Halgren T.A., Klicic J.J., Mainz D.T., et al. Glide: a new approach for rapid, accurate docking and scoring. 1. Method and assessment of docking accuracy. J Med Chem. 2004;47:1739–1749. doi: 10.1021/jm0306430. [DOI] [PubMed] [Google Scholar]
- 38.Trott O., Olson A.J. AutoDock Vina: improving the speed and accuracy of docking with a new scoring function, efficient optimization, and multithreading. J Comput Chem. 2010;31:455–461. doi: 10.1002/jcc.21334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Grosdidier A., Zoete V., Michielin O. SwissDock, a protein-small molecule docking web service based on EADock DSS. Nucleic Acids Res. 2011;39(suppl):W270–W277. doi: 10.1093/nar/gkr366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Phimister E.G., Parks J.M., Smith J.C. How to discover antiviral drugs quickly. N Engl J Med. 2020;382(23):2261–2264. doi: 10.1056/NEJMcibr2007042. [DOI] [PubMed] [Google Scholar]
- 41.Liu X., Wang X.-J. Potential inhibitors against 2019-nCoV coronavirus M protease from clinically approved medicines. J Genet Genomics. 2020;47(2):119–121. doi: 10.1016/j.jgg.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cavasotto C.N., Phatak S.S. Homology modeling in drug discovery: current trends and applications. Drug Discov Today. 2009;14(13-14):676–683. doi: 10.1016/j.drudis.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 43.Waterhouse A, Bertoni M, Bienert S, Studer G, Tauriello G, Gumienny R, et al. SWISS-MODEL: homology modelling of protein structures and complexes. Nucleic Acids Res 2018; 46: W296–303. doi:10.1093/nar/gky427 [DOI] [PMC free article] [PubMed]
- 44.Wu C., Liu Y., Yang Y., Zhang P., Zhong W.u., Wang Y., Wang Q., Xu Y., Li M., Li X., Zheng M., Chen L., Li H. Analysis of therapeutic targets for SARS-CoV-2 and discovery of potential drugs by computational methods. Acta Pharm Sin B. 2020;10(5):766–788. doi: 10.1016/j.apsb:2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sterling T., Irwin J.J. ZINC 15 – ligand discovery for everyone. J Chem Inf Model. 2015;55(11):2324–2337. doi: 10.1021/acs.jcim.5b00559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Elfiky A.A. Anti-HCV, nucleotide inhibitors, repurposing against COVID-19. Life Sci. 2020;248:117477. doi: 10.1016/j.lfs.2020.117477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Elfiky A.A. Ribavirin, Remdesivir, Sofosbuvir, Galidesivir, and Tenofovir against SARS-CoV-2 RNA dependent RNA polymerase (RdRp): a molecular docking study. Life Sci. 2020;253:117592. doi: 10.1016/j.lfs.2020.117592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen YW, Yiu C-PB, Wong K-Y. Prediction of the SARS-CoV-2 (2019-nCoV) 3C-like protease (3CL pro) structure: virtual screening reveals velpatasvir, ledipasvir, and other drug repurposing candidates. F1000Res 2020; 9: 129. doi:10.12688/f1000research.22457.2 [DOI] [PMC free article] [PubMed]
- 49.Cavasotto C.N., Di Filippo J.I. In silico drug repurposing for COVID-19: targeting SARS-CoV-2 proteins through docking and consensus ranking. Mol Inform. 2021;40(1):2000115. doi: 10.1002/minf.v40.110.1002/minf.202000115. [DOI] [PubMed] [Google Scholar]
- 50.Borgio J.F., Alsuwat H.S., Al Otaibi W.M., Ibrahim A.M., Almandil N., Al Asoom L.I., Salahuddin M., Kamaraj B., AbdulAzeez S. State-of-the-art tools unveil potent drug targets amongst clinically approved drugs to inhibit helicase in SARS-CoV-2. Arch Med Sci. 2020;16(3):508–518. doi: 10.5114/aoms.2020.94567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Basu A., Sarkar A., Maulik U. Molecular docking study of potential phytochemicals and their effects on the complex of SARS-CoV2 spike protein and human ACE2. Sci Rep. 2020;10:17699. doi: 10.1038/s41598-020-74715-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rahman N., Basharat Z., Yousuf M., Castaldo G., Rastrelli L., Khan H. Virtual screening of natural products against type II transmembrane serine protease (TMPRSS2), the priming agent of Coronavirus 2 (SARS-CoV-2) Molecules. 2020;25:2271. doi: 10.3390/molecules25102271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Elmezayen A.D., Al-Obaidi A., Şahin A.T., Yelekçi K. Drug repurposing for coronavirus (COVID-19): in silico screening of known drugs against coronavirus 3CL hydrolase and protease enzymes. J Biomol Struct Dyn. 2021;39(8):2980–2992. doi: 10.1080/07391102.2020.1758791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yu R., Chen L., Lan R., Shen R., Li P. Computational screening of antagonists against the SARS-CoV-2 (COVID-19) coronavirus by molecular docking. Int J Antimicrob Agents. 2020;56(2):106012. doi: 10.1016/j.ijantimicag.2020.106012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sencanski M., Perovic V., Pajovic S.B., Adzic M., Paessler S., Glisic S. Drug repurposing for candidate SARS-CoV-2 main protease inhibitors by a novel in silico method. Molecules. 2020;25:3830. doi: 10.3390/molecules25173830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shah B., Modi P., Sagar S.R. In silico studies on therapeutic agents for COVID-19: drug repurposing approach. Life Sci. 2020;252:117652. doi: 10.1016/j.lfs.2020.117652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gimeno A., Mestres-Truyol J., Ojeda-Montes M.J., Macip G., Saldivar-Espinoza B., Cereto-Massagué A., Pujadas G., Garcia-Vallvé S. Prediction of novel inhibitors of the main protease (M-pro) of SARS-CoV-2 through consensus docking and drug reposition. Int J Mol Sci. 2020;21(11):3793. doi: 10.3390/ijms21113793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Liu S, Zheng Q, Wang Z. Potential covalent drugs targeting the main protease of the SARS-CoV-2 coronavirus. Bioinformatics 2020; 36: 3295–8. doi:10.1093/bioinformatics/btaa224 [DOI] [PMC free article] [PubMed]
- 59.Kandeel M., Al-Nazawi M. Virtual screening and repurposing of FDA approved drugs against COVID-19 main protease. Life Sci. 2020;251:117627. doi: 10.1016/j.lfs.2020.117627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kouznetsova VL, Zhang A, Tatineni M, Miller MA, Tsigelny IF. Potential COVID-19 papain-like protease PLpro inhibitors: repurposing FDA-approved drugs. Peer J 2020; 8: e9965. doi:10.7717/peerj.9965 [DOI] [PMC free article] [PubMed]
- 61.Jin Z., Du X., Xu Y., Deng Y., Liu M., Zhao Y., Zhang B., Li X., Zhang L., Peng C., Duan Y., Yu J., Wang L., Yang K., Liu F., Jiang R., Yang X., You T., Liu X., Yang X., Bai F., Liu H., Liu X., Guddat L.W., Xu W., Xiao G., Qin C., Shi Z., Jiang H., Rao Z., Yang H. Structure of Mpro from SARS-CoV-2 and discovery of its inhibitors. Nature. 2020;582(7811):289–293. doi: 10.1038/s41586-020-2223-y. [DOI] [PubMed] [Google Scholar]
- 62.Yang H., Xie W., Xue X., Yang K., Ma J., Liang W., Zhao Q.i., Zhou Z., Pei D., Ziebuhr J., Hilgenfeld R., Yuen K.Y., Wong L., Gao G., Chen S., Chen Z., Ma D., Bartlam M., Rao Z., Bjorkman P. Design of wide-spectrum inhibitors targeting coronavirus main proteases. PLoS Biol. 2005;3(10):e324. doi: 10.1371/journal.pbio.0030324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chen L., Gui C., Luo X., Yang Q., Günther S., Scandella E., Drosten C., Bai D., He X., Ludewig B., Chen J., Luo H., Yang Y., Yang Y., Zou J., Thiel V., Chen K., Shen J., Shen X.u., Jiang H. Cinanserin is an inhibitor of the 3C-like proteinase of severe acute respiratory syndrome coronavirus and strongly reduces virus replication in vitro. J Virol. 2005;79(11):7095–7103. doi: 10.1128/JVI.79.11.7095-7103.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhang D.-W., Yan H.-L., Xu X.-S., Xu L., Yin Z.-H., Chang S., Luo H. The selenium-containing drug ebselen potently disrupts LEDGF/p75-HIV-1 integrase interaction by targeting LEDGF/p75. J Enzyme Inhib Med Chem. 2020;35(1):906–912. doi: 10.1080/14756366.2020.1743282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mukherjee S., Weiner W.S., Schroeder C.E., Simpson D.S., Hanson A.M., Sweeney N.L., Marvin R.K., Ndjomou J., Kolli R., Isailovic D., Schoenen F.J., Frick D.N. Ebselen inhibits hepatitis C virus NS3 helicase binding to nucleic acid and prevents viral replication. ACS Chem Biol. 2014;9(10):2393–2403. doi: 10.1021/cb500512z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Simanjuntak Y., Liang J.-J., Chen S.-Y., Li J.-K., Lee Y.-L., Wu H.-C., Lin Y.-L., Pierson T.C. Ebselen alleviates testicular pathology in mice with Zika virus infection and prevents its sexual transmission. PLoS Pathog. 2018;14(2):e1006854. doi: 10.1371/journal.ppat.1006854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Van Der Spoel D., Lindahl E., Hess B., Groenhof G., Mark A.E., Berendsen H.J.C. GROMACS: fast, flexible, and free. J Comput Chem. 2005;26(16):1701–1718. doi: 10.1002/(ISSN)1096-987X10.1002/jcc.v26:1610.1002/jcc.20291. [DOI] [PubMed] [Google Scholar]
- 68.Case D.A., Cheatham T.E., Darden T., Gohlke H., Luo R., Merz K.M., Onufriev A., Simmerling C., Wang B., Woods R.J. The Amber biomolecular simulation programs. J Comput Chem. 2005;26(16):1668–1688. doi: 10.1002/(ISSN)1096-987X10.1002/jcc.v26:1610.1002/jcc.20290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mittal L., Kumari A., Srivastava M., Singh M., Asthana S. Identification of potential molecules against COVID-19 main protease through structure-guided virtual screening approach. J Biomol Struct Dyn. 2021;39(10):3662–3680. doi: 10.1080/07391102.2020.1768151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Al-Khafaji K., Al-Duhaidahawi D., Taskin T.T. Using integrated computational approaches to identify safe and rapid treatment for SARS-CoV-2. J Biomol Struct Dyn. 2021;39:3387–3395. doi: 10.1080/07391102.2020.1764392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pant S., Singh M., Ravichandiran V., Murty U.S.N., Srivastava H.K. Peptide-like and small-molecule inhibitors against Covid-19. J Biomol Struct Dyn. 2021;39(8):2904–2913. doi: 10.1080/07391102.2020.1757510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Muralidharan N., Sakthivel R., Velmurugan D., Gromiha M.M. Computational studies of drug repurposing and synergism of lopinavir, oseltamivir and ritonavir binding with SARS-CoV-2 protease against COVID-19. J Biomol Struct Dyn. 2021;39(7):2673–2678. doi: 10.1080/07391102.2020.1752802. [DOI] [PubMed] [Google Scholar]
- 73.Odhar H.A., Ahjel S.W., Albeer A.A.M.A., Hashim A.F., Rayshan A.M., Humadi S.S. Molecular docking and dynamics simulation of FDA approved drugs with the main protease from 2019 novel coronavirus. Bioinformation. 2020;16:236–244. doi: 10.6026/97320630016236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Khan S.A., Zia K., Ashraf S., Uddin R., Ul-Haq Z. Identification of chymotrypsin-like protease inhibitors of SARS-CoV-2 via integrated computational approach. J Biomol Struct Dyn. 2021;39(7):2607–2616. doi: 10.1080/07391102.2020.1751298. [DOI] [PubMed] [Google Scholar]
- 75.Elfiky A.A. SARS-CoV-2 RNA dependent RNA polymerase (RdRp) targeting: an in silico perspective. J Biomol Struct Dyn. 2021;39:3204–3212. doi: 10.1080/07391102.2020.1761882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Encinar J.A., Menendez J.A. Potential drugs targeting early innate immune evasion of SARS-Coronavirus 2 via 2’-O-methylation of viral RNA. Viruses. 2020;12:525. doi: 10.3390/v12050525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Abdelli I., Hassani F., Bekkel Brikci S., Ghalem S. In silico study the inhibition of angiotensin converting enzyme 2 receptor of COVID-19 by Ammoides verticillata components harvested from Western Algeria. J Biomol Struct Dyn. 2021;39:3263–3276. doi: 10.1080/07391102.2020.1763199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Trezza A., Iovinelli D., Santucci A., Prischi F., Spiga O. An integrated drug repurposing strategy for the rapid identification of potential SARS-CoV-2 viral inhibitors. Sci Rep. 2020;10:13866. doi: 10.1038/s41598-020-70863-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gao K, Nguyen DD, Chen J, Wang R, Wei G. Repositioning of 8565 existing drugs for COVID-19. J Phys Chem Lett June 2020; 11: 5373–82. doi:10.1021/acs.jpclett.0c01579 [DOI] [PMC free article] [PubMed]
- 80.Batra R., Chan H., Kamath G., Ramprasad R., Cherukara M.J., Sankaranarayanan S.K.R.S. Screening of therapeutic agents for COVID-19 using machine learning and ensemble docking studies. J Phys Chem Lett. 2020;11(17):7058–7065. doi: 10.1021/acs.jpclett.0c0227810.1021/acs.jpclett.0c02278.s00110.1021/acs.jpclett.0c02278.s002. [DOI] [PubMed] [Google Scholar]
- 81.Beck B.R., Shin B., Choi Y., Park S., Kang K. Predicting commercially available antiviral drugs that may act on the novel coronavirus (SARS-CoV-2) through a drug-target interaction deep learning model. Comput Struct Biotechnol J. 2020;18:784–790. doi: 10.1016/j.csbj.2020.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ton A.-T., Gentile F., Hsing M., Ban F., Cherkasov A. Rapid identification of potential inhibitors of SARS-CoV-2 main protease by deep docking of 1.3 billion compounds. Mol. Inform. 2020;39(8):2000028. doi: 10.1002/minf.v39.810.1002/minf.202000028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Liu T., Lin Y., Wen X., Jorissen R.N., Gilson M.K. BindingDB: a web-accessible database of experimentally determined protein-ligand binding affinities. Nucleic Acids Res. 2007;35(Database):D198–D201. doi: 10.1093/nar/gkl999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tanoli Z., Alam Z., Vähä-Koskela M., Ravikumar B., Malyutina A., Jaiswal A., et al. Drug Target Commons 2.0: a community platform for systematic analysis of drug-target interaction profiles. Database (Oxford) 2018;2018:1–13. doi: 10.1093/database/bay083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Alakwaa F.M. Repurposing didanosine as a potential treatment for COVID-19 using single-cell RNA sequencing data. mSystems. 2020;5:e00297–e320. doi: 10.1128/mSystems.00297-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cava C., Bertoli G., Castiglioni I. In silico discovery of candidate drugs against Covid-19. Viruses. 2020;12:404. doi: 10.3390/v12040404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mele M., Ferreira P.G., Reverter F., DeLuca D.S., Monlong J., Sammeth M., Young T.R., Goldmann J.M., Pervouchine D.D., Sullivan T.J., Johnson R., Segre A.V., Djebali S., Niarchou A., Consortium T.G., Wright F.A., Lappalainen T., Calvo M., Getz G., Dermitzakis E.T., Ardlie K.G., Guigo R. The human transcriptome across tissues and individuals. Science. 2015;348(6235):660–665. doi: 10.1126/science:aaa0355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zhou Y., Hou Y., Shen J., Huang Y., Martin W., Cheng F. Network-based drug repurposing for novel coronavirus 2019-nCoV/SARS-CoV-2. Cell Discov. 2020;6:14. doi: 10.1038/s41421-020-0153-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gordon D.E., Jang G.M., Bouhaddou M., Xu J., Obernier K., White K.M., O’Meara M.J., Rezelj V.V., Guo J.Z., Swaney D.L., Tummino T.A., Hüttenhain R., Kaake R.M., Richards A.L., Tutuncuoglu B., Foussard H., Batra J., Haas K., Modak M., Kim M., Haas P., Polacco B.J., Braberg H., Fabius J.M., Eckhardt M., Soucheray M., Bennett M.J., Cakir M., McGregor M.J., Li Q., Meyer B., Roesch F., Vallet T., Mac Kain A., Miorin L., Moreno E., Naing Z.Z.C., Zhou Y., Peng S., Shi Y., Zhang Z., Shen W., Kirby I.T., Melnyk J.E., Chorba J.S., Lou K., Dai S.A., Barrio-Hernandez I., Memon D., Hernandez-Armenta C., Lyu J., Mathy C.J.P., Perica T., Pilla K.B., Ganesan S.J., Saltzberg D.J., Rakesh R., Liu X.i., Rosenthal S.B., Calviello L., Venkataramanan S., Liboy-Lugo J., Lin Y., Huang X.-P., Liu YongFeng, Wankowicz S.A., Bohn M., Safari M., Ugur F.S., Koh C., Savar N.S., Tran Q.D., Shengjuler D., Fletcher S.J., O’Neal M.C., Cai Y., Chang J.C.J., Broadhurst D.J., Klippsten S., Sharp P.P., Wenzell N.A., Kuzuoglu-Ozturk D., Wang H.-Y., Trenker R., Young J.M., Cavero D.A., Hiatt J., Roth T.L., Rathore U., Subramanian A., Noack J., Hubert M., Stroud R.M., Frankel A.D., Rosenberg O.S., Verba K.A., Agard D.A., Ott M., Emerman M., Jura N., von Zastrow M., Verdin E., Ashworth A., Schwartz O., d’Enfert C., Mukherjee S., Jacobson M., Malik H.S., Fujimori D.G., Ideker T., Craik C.S., Floor S.N., Fraser J.S., Gross J.D., Sali A., Roth B.L., Ruggero D., Taunton J., Kortemme T., Beltrao P., Vignuzzi M., García-Sastre A., Shokat K.M., Shoichet B.K., Krogan N.J. A SARS-CoV-2 protein interaction map reveals targets for drug repurposing. Nature. 2020;583(7816):459–468. doi: 10.1038/s41586-020-2286-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Bouhaddou M., Memon D., Meyer B., White K.M., Rezelj V.V., Correa Marrero M., Polacco B.J., Melnyk J.E., Ulferts S., Kaake R.M., Batra J., Richards A.L., Stevenson E., Gordon D.E., Rojc A., Obernier K., Fabius J.M., Soucheray M., Miorin L., Moreno E., Koh C., Tran Q.D., Hardy A., Robinot R., Vallet T., Nilsson-Payant B.E., Hernandez-Armenta C., Dunham A., Weigang S., Knerr J., Modak M., Quintero D., Zhou Y., Dugourd A., Valdeolivas A., Patil T., Li Q., Hüttenhain R., Cakir M., Muralidharan M., Kim M., Jang G., Tutuncuoglu B., Hiatt J., Guo J.Z., Xu J., Bouhaddou S., Mathy C.J.P., Gaulton A., Manners E.J., Félix E., Shi Y., Goff M., Lim J.K., McBride T., O’Neal M.C., Cai Y., Chang J.C.J., Broadhurst D.J., Klippsten S., De wit E., Leach A.R., Kortemme T., Shoichet B., Ott M., Saez-Rodriguez J., tenOever B.R., Mullins R.D., Fischer E.R., Kochs G., Grosse R., García-Sastre A., Vignuzzi M., Johnson J.R., Shokat K.M., Swaney D.L., Beltrao P., Krogan N.J. The global phosphorylation landscape of SARS-CoV-2 infection. Cell. 2020;182(3):685–712.e19. doi: 10.1016/j.cell.2020.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ochoa D., Jarnuczak A.F., Viéitez C., Gehre M., Soucheray M., Mateus A., Kleefeldt A.A., Hill A., Garcia-Alonso L., Stein F., Krogan N.J., Savitski M.M., Swaney D.L., Vizcaíno J.A., Noh K.-M., Beltrao P. The functional landscape of the human phosphoproteome. Nat Biotechnol. 2020;38(3):365–373. doi: 10.1038/s41587-019-0344-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Jia Z., Song X., Shi J., Wang W., He K. Transcriptome-based drug repositioning for coronavirus disease 2019 (COVID-19) Pathog Dis. 2020;78:ftaa036. doi: 10.1093/femspd/ftaa036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Taguchi Y.-h., Turki T., Li Q. A new advanced in silico drug discovery method for novel coronavirus (SARS-CoV-2) with tensor decomposition-based unsupervised feature extraction. PLoS ONE. 2020;15(9):e0238907. doi: 10.1371/journal.pone.0238907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zhou Y., Hou Y., Shen J., Mehra R., Kallianpur A., Culver D.A., Gack M.U., Farha S., Zein J., Comhair S., Fiocchi C., Stappenbeck T., Chan T., Eng C., Jung J.U., Jehi L., Erzurum S., Cheng F., Soranzo N. A network medicine approach to investigation and population-based validation of disease manifestations and drug repurposing for COVID-19. PLoS Biol. 2020;18(11):e3000970. doi: 10.1371/journal.pbio.3000970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bojkova D., Klann K., Koch B., Widera M., Krause D., Ciesek S., Cinatl J., Münch C. Proteomics of SARS-CoV-2-infected host cells reveals therapy targets. Nature. 2020;583(7816):469–472. doi: 10.1038/s41586-020-2332-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Chen Q., Allot A., Lu Z. Keep up with the latest coronavirus research. Nature. 2020;579:193. doi: 10.1038/d41586-020-00694-1. [DOI] [PubMed] [Google Scholar]
- 97.Lu Wang L, Lo K, Chandrasekhar Y, Reas R, Yang J, Eide D, et al. CORD-19: The Covid-19 Open Research Dataset. ArXiv 2020; 2004.10706v2.
- 98.Wang L.L., Lo K. Text mining approaches for dealing with the rapidly expanding literature on COVID-19. Brief Bioinform. 2021;22:781–799. doi: 10.1093/bib/bbaa296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Gurwitz D. Repurposing current therapeutics for treating COVID-19: a vital role of prescription records data mining. Drug Dev Res. 2020;81:777–781. doi: 10.1002/ddr.21689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Ozery-Flato M., Goldschmidt Y., Shaham O., Ravid S., Yanover C. Framework for identifying drug repurposing candidates from observational healthcare data. JAMIA Open. 2020;3:536–544. doi: 10.1093/jamiaopen/ooaa048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Cao B., Wang Y., Wen D., Liu W., Wang J., Fan G., Ruan L., Song B., Cai Y., Wei M., Li X., Xia J., Chen N., Xiang J., Yu T., Bai T., Xie X., Zhang L.i., Li C., Yuan Y.e., Chen H., Li H., Huang H., Tu S., Gong F., Liu Y., Wei Y., Dong C., Zhou F., Gu X., Xu J., Liu Z., Zhang Y.i., Li H., Shang L., Wang K.e., Li K., Zhou X., Dong X., Qu Z., Lu S., Hu X., Ruan S., Luo S., Wu J., Peng L.u., Cheng F., Pan L., Zou J., Jia C., Wang J., Liu X., Wang S., Wu X., Ge Q., He J., Zhan H., Qiu F., Guo L.i., Huang C., Jaki T., Hayden F.G., Horby P.W., Zhang D., Wang C. A trial of lopinavir-ritonavir in adults hospitalized with severe Covid-19. N Engl J Med. 2020;382(19):1787–1799. doi: 10.1056/NEJMoa2001282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Tong S., Su Y., Yu Y., Wu C., Chen J., Wang S., Jiang J. Ribavirin therapy for severe COVID-19: a retrospective cohort study. Int J Antimicrob Agents. 2020;56(3):106114. doi: 10.1016/j.ijantimicag.2020.106114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lo M.W., Kemper C., Woodruff T.M. COVID-19: complement, coagulation, and collateral damage. J Immunol. 2020;205(6):1488–1495. doi: 10.4049/jimmunol.2000644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Villar J., Ferrando C., Martínez D., Ambrós A., Muñoz T., Soler J.A., Aguilar G., Alba F., González-Higueras E., Conesa L.A., Martín-Rodríguez C., Díaz-Domínguez F.J., Serna-Grande P., Rivas R., Ferreres J., Belda J., Capilla L., Tallet A., Añón J.M., Fernández R.L., González-Martín J.M., Aguilar G., Alba F., Álvarez J., Ambrós A., Añón J.M., Asensio M.J., Belda J., Blanco J., Blasco M., Cachafeiro L., del Campo R., Capilla L., Carbonell J.A., Carbonell N., Cariñena A., Carriedo D., Chico M., Conesa L.A., Corpas R., Cuervo J., Díaz-Domínguez F.J., Domínguez-Antelo C., Fernández L., Fernández R.L., Ferrando C., Ferreres J., Gamboa E., González-Higueras E., González-Luengo R.I., González-Martín J.M., Martínez D., Martín-Rodríguez C., Muñoz T., Ortiz Díaz-Miguel R., Pérez-González R., Prieto A.M., Prieto I., Rivas R., Rojas-Viguera L., Romera M.A., Sánchez-Ballesteros J., Segura J.M., Serna-Grande P., Serrano A., Solano R., Soler J.A., Soro M., Tallet A., Villar J. Dexamethasone treatment for the acute respiratory distress syndrome: a multicentre, randomised controlled trial. Lancet Respir Med. 2020;8(3):267–276. doi: 10.1016/S2213-2600(19)30417-5. [DOI] [PubMed] [Google Scholar]
- 105.Farne H., Kumar K., Ritchie A.I., Finney L.J., Johnston S.L., Singanayagam A. Repurposing existing drugs for the treatment of COVID-19. Ann Am Thorac Soc. 2020;17(10):1186–1194. doi: 10.1513/AnnalsATS.202005-566FR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.DiNicolantonio J.J., Barroso-Aranda J. Harnessing adenosine A2A receptors as a strategy for suppressing the lung inflammation and thrombotic complications of COVID-19: potential of pentoxifylline and dipyridamole. Med Hypotheses. 2020;143:110051. doi: 10.1016/j.mehy.2020.110051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Edwards A. What are the odds of finding a COVID-19 frug from a lab repurposing screen? J Chem Inf Model. 2020;60:5727–5729. doi: 10.1021/acs.jcim.0c00861. [DOI] [PubMed] [Google Scholar]
- 108.Han Y., Duan X., Yang L., Nilsson-Payant B.E., Wang P., Duan F., Tang X., Yaron T.M., Zhang T., Uhl S., Bram Y., Richardson C., Zhu J., Zhao Z., Redmond D., Houghton S., Nguyen D.-H., Xu D., Wang X., Jessurun J., Borczuk A., Huang Y., Johnson J.L., Liu Y., Xiang J., Wang H., Cantley L.C., tenOever B.R., Ho D.D., Pan F.C., Evans T., Chen H.J., Schwartz R.E., Chen S. Identification of SARS-CoV-2 inhibitors using lung and colonic organoids. Nature. 2021;589(7841):270–275. doi: 10.1038/s41586-020-2901-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Pérez-Bermejo J.A., Kang S., Rockwood S.J., Simoneau C.R., Joy D.A., Ramadoss G.N., et al. SARS-CoV-2 infection of human iPSC-derived cardiac cells predicts novel cytopathic features in hearts of COVID-19 patients. BioRxiv. 2020 doi: 10.1101/2020.08.25.265561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Desai N., Neyaz A., Szabolcs A., Shih A.R., Chen J.H., Thapar V., Nieman L.T., Solovyov A., Mehta A., Lieb D.J., Kulkarni A.S., Jaicks C., Xu K.H., Raabe M.J., Pinto C.J., Juric D., Chebib I., Colvin R.B., Kim A.Y., Monroe R., Warren S.E., Danaher P., Reeves J.W., Gong J., Rueckert E.H., Greenbaum B.D., Hacohen N., Lagana S.M., Rivera M.N., Sholl L.M., Stone J.R., Ting D.T., Deshpande V. Temporal and spatial heterogeneity of host response to SARS-CoV-2 pulmonary infection. Nat Commun. 2020;11(1) doi: 10.1038/s41467-020-20139-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Nienhold R., Ciani Y., Koelzer V.H., Tzankov A., Haslbauer J.D., Menter T., Schwab N., Henkel M., Frank A., Zsikla V., Willi N., Kempf W., Hoyler T., Barbareschi M., Moch H., Tolnay M., Cathomas G., Demichelis F., Junt T., Mertz K.D. Two distinct immunopathological profiles in autopsy lungs of COVID-19. Nat Commun. 2020;11(1) doi: 10.1038/s41467-020-18854-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zhang J.-Y., Wang X.-M., Xing X., Xu Z., Zhang C., Song J.-W., Fan X., Xia P., Fu J.-L., Wang S.-Y., Xu R.-N., Dai X.-P., Shi L., Huang L., Jiang T.-J., Shi M., Zhang Y., Zumla A., Maeurer M., Bai F., Wang F.-S. Single-cell landscape of immunological responses in patients with COVID-19. Nat Immunol. 2020;21(9):1107–1118. doi: 10.1038/s41590-020-0762-x. [DOI] [PubMed] [Google Scholar]
- 113.Wilk A.J., Rustagi A., Zhao N.Q., Roque J., Martínez-Colón G.J., McKechnie J.L., Ivison G.T., Ranganath T., Vergara R., Hollis T., Simpson L.J., Grant P., Subramanian A., Rogers A.J., Blish C.A. A single-cell atlas of the peripheral immune response in patients with severe COVID-19. Nat Med. 2020;26(7):1070–1076. doi: 10.1038/s41591-020-0944-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Li X., Xu S., Yu M., Wang K.e., Tao Y.u., Zhou Y., Shi J., Zhou M., Wu B.o., Yang Z., Zhang C., Yue J., Zhang Z., Renz H., Liu X., Xie J., Xie M., Zhao J. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. 2020;146(1):110–118. doi: 10.1016/j.jaci.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Pascarella G., Strumia A., Piliego C., Bruno F., Del Buono R., Costa F., Scarlata S., Agrò F.E. COVID-19 diagnosis and management: a comprehensive review. J Intern Med. 2020;288(2):192–206. doi: 10.1111/joim.v288.210.1111/joim.13091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Jain V., Yuan J.-M. Predictive symptoms and comorbidities for severe COVID-19 and intensive care unit admission: a systematic review and meta-analysis. Int J Public Health. 2020;65(5):533–546. doi: 10.1007/s00038-020-01390-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Miller R., Englund K. Transmission and risk factors of OF COVID-19. Cleve Clin J Med. 2020 doi: 10.3949/ccjm.87a.ccc029. [DOI] [PubMed] [Google Scholar]
- 118.Li X., Qin G., Yang Q., Chen L., Xie L. Biomolecular network-based synergistics drug combination discovery. Biomed Res Int. 2016;2016:8518945. doi: 10.1155/2016/8518945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Sun W., Sanderson P.E., Zheng W. Drug combination therapy increases successful drug repositioning. Drug Discov Today. 2016;21(7):1189–1195. doi: 10.1016/j.drudis.2016.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Mokhtari R.B., Homayouni T.S., Baluch N., Morgatskaya E., Kumar S., Das B., Yeger H. Combination therapy in combating cancer. Oncotarget. 2017;8(23):38022–38043. doi: 10.18632/oncotarget.v8i2310.18632/oncotarget.16723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Cihlar T., Fordyce M. Current status and prospects of HIV treatment. Curr Opin Virol. 2016;18:50–56. doi: 10.1016/j.coviro.2016.03.004. [DOI] [PubMed] [Google Scholar]
- 122.Cheng F., Kovács I.A., Barabási A.-L. Network-based prediction of drug combinations. Nat Commun. 2019;10:1197. doi: 10.1038/s41467-019-09186-x123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Feng Z., Chen M., Liang T., Shen M., Chen H., Xie X.-Q. Virus-CKB: an integrated bioinformatics platform and analysis resource for COVID-19 research. Brief Bioinformatics. 2021;22:882–895. doi: 10.1093/bib/bbaa155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Chen Q., Allot A., Lu Z. LitCovid: an open database of COVID-19 literature. Nucleic Acids Res. 2021;49:D1534–D1540. doi: 10.1093/nar/gkaa952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Korn D., Bobrowski T., Li M., Kebede Y., Wang P., Owen P., et al. COVID-KOP: integrating emerging COVID-19 data with the ROBOKOP database. Bioinformatics. 2021;37:586–587. doi: 10.1093/bioinformatics/btaa718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Zheng Q., Jones F.K., Leavitt S.V., Ung L., Labrique A.B., Peters D.H., Lee E.C., Azman A.S. HIT-COVID, a global database tracking public health interventions to COVID-19. Sci Data. 2020;7(1) doi: 10.1038/s41597-020-00610-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Chodera J., Lee A.A., London N., von Delft F. Crowdsourcing drug discovery for pandemics. Nat Chem. 2020;12:581. doi: 10.1038/s41557-020-0496-2. [DOI] [PubMed] [Google Scholar]
- 128.He Y., Yu H., Ong E., Wang Y., Liu Y., Huffman A., Huang H.-H., Beverley J., Hur J., Yang X., Chen L., Omenn G.S., Athey B., Smith B. CIDO, a community-based ontology for coronavirus disease knowledge and data integration, sharing, and analysis. Sci Data. 2020;7(1) doi: 10.1038/s41597-020-0523-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Sadegh S., Matschinske J., Blumenthal D.B., Galindez G., Kacprowski T., List M., Nasirigerdeh R., Oubounyt M., Pichlmair A., Rose T.D., Salgado-Albarrán M., Späth J., Stukalov A., Wenke N.K., Yuan K., Pauling J.K., Baumbach J. Exploring the SARS-CoV-2 virus-host-drug interactome for drug repurposing. Nat Commun. 2020;11(1) doi: 10.1038/s41467-020-17189-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Berman H.M., Battistuz T., Bhat T.N., Bluhm W.F., Bourne P.E., Burkhardt K., Feng Z., Gilliland G.L., Iype L., Jain S., Fagan P., Marvin J., Padilla D., Ravichandran V., Schneider B., Thanki N., Weissig H., Westbrook J.D., Zardecki C. The protein data bank. Acta Crystallogr D Biol Crystallogr. 2002;58(6):899–907. doi: 10.1107/S0907444902003451. [DOI] [PubMed] [Google Scholar]
- 131.Hewett M., Oliver D.E., Rubin D.L., Easton K.L., Stuart J.M., Altman R.B., Klein T.E. Pharmgkb: the Pharmacogenetics Knowledge Base. Nucleic Acids Res. 2002;30:163–165. doi: 10.1093/nar/30.1.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Wishart D.S., Feunang Y.D., Guo A.C., Lo E.J., Marcu A., Grant J.R., et al. DrugBank 5.0: a major update to the DrugBank database for 2018. Nucleic Acids Res. 2018;46 doi: 10.1093/nar/gkx1037. D1074–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Benson D.A., Cavanaugh M., Clark K., Karsch-Mizrachi I., Lipman D.J., Ostell J., Sayers E.W. GenBank. Nucleic Acids Res. 2017;45(D1):D37–D42. doi: 10.1093/nar/gkw1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Harrison P.W., Alako B., Amid C., Cerdeño-Tárraga A., Cleland I., Holt S., et al. The European nucleotide archive in 2018. Nucleic Acids Res. 2019;47 doi: 10.1093/nar/gky1078. D84–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Safran M, Dalah I, Alexander J, Rosen N, Stein TI, Shmoish M, et al. GeneCards Version 3: the human gene integrator. Database (Oxford) 2010; 2010: baq020. doi:10.1093/database/baq020 [DOI] [PMC free article] [PubMed]
- 136.Yang K., Dinasarapu A.R., Reis E.S., Deangelis R.A., Ricklin D., Subramaniam S., Lambris J.D. CMAP: Complement Map Database. Bioinformatics. 2013;29:1832–1833. doi: 10.1093/bioinformatics/btt269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Liberzon A., Subramanian A., Pinchback R., Thorvaldsdottir H., Tamayo P., Mesirov J.P. Molecular signatures database (MSigDB) 3.0. Bioinformatics. 2011;27(12):1739–1740. doi: 10.1093/bioinformatics/btr260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.UniProt Consortium UniProt: a hub for protein information. Nucleic Acids Res. 2015;43:D204–D212. doi: 10.1093/nar/gku989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Bairoch A., Boeckmann B. The SWISS-PROT protein sequence data bank. Nucleic Acids Res. 1992;20(Suppl):2019–2022. doi: 10.1093/nar/20.suppl.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Martens L., Hermjakob H., Jones P., Adamski M., Taylor C., States D., Gevaert K., Vandekerckhove J., Apweiler R. PRIDE: the proteomics identifications database. Proteomics. 2005;5(13):3537–3545. doi: 10.1002/(ISSN)1615-986110.1002/pmic.v5:1310.1002/pmic.200401303. [DOI] [PubMed] [Google Scholar]
- 141.Ruepp A., Brauner B., Dunger-Kaltenbach I., Frishman G., Montrone C., Stransky M., Waegele B., Schmidt T., Doudieu O.N., Stumpflen V., Mewes H.W. CORUM: the comprehensive resource of mammalian protein complexes. Nucleic Acids Res. 2008;36(Database):D646–D650. doi: 10.1093/nar/gkm936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Ogata H., Goto S., Sato K., Fujibuchi W., Bono H., Kanehisa M. KEGG: Kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 1999;27(1):29–34. doi: 10.1093/nar/27.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
References
Further reading
- 143.Ke Y.-Y., Peng T.-T., Yeh T.-K., Huang W.-Z., Chang S.-E., Wu S.-H., Hung H.-C., Hsu T.-A., Lee S.-J., Song J.-S., Lin W.-H., Chiang T.-J., Lin J.-H., Sytwu H.-K., Chen C.-T. Artificial intelligence approach fighting COVID-19 with repurposing drugs. Biomed J. 2020;43(4):355–362. doi: 10.1016/j.bj.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Murugan N.A., Kumar S., Jeyakanthan J., Srivastava V. Searching for target-specific and multi-targeting organics for Covid-19 in the Drugbank database with a double scoring approach. Sci Rep. 2020;10:19125. doi: 10.1038/s41598-020-75762-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Gendrot M., Andreani J., Boxberger M., Jardot P., Fonta I., Le Bideau M., Duflot I., Mosnier J., Rolland C., Bogreau H., Hutter S., La Scola B., Pradines B. Antimalarial drugs inhibit the replication of SARS-CoV-2: an in vitro evaluation. Travel Med Infect Dis. 2020;37:101873. doi: 10.1016/j.tmaid.2020.101873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Barthélémy R., Blot P.-L., Tiepolo A., Le Gall A., Mayeur C., Gaugain S., Morisson L., Gayat E., Mebazaa A., Chousterman B.G. Efficacy of almitrine in the treatment of hypoxemia in SARS-Cov-2 acute respiratory distress syndrome. Chest. 2020;158(5):2003–2006. doi: 10.1016/j.chest.2020.05.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Mahdi M., Mótyán J.A., Szojka Z.I., Golda M., Miczi M., Tőzsér J. Analysis of the efficacy of HIV protease inhibitors against SARS-CoV-2’s main protease. Virol J. 2020;17:190. doi: 10.1186/s12985-020-01457-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Fintelman-Rodrigues N., Sacramento C.Q., Ribeiro Lima C., Souza da Silva F., Ferreira A.C., Mattos M., de Freitas C.S., Cardoso Soares V., da Silva Gomes Dias S., Temerozo J.R., Miranda M.D., Matos A.R., Bozza F.A., Carels N., Alves C.R., Siqueira M.M., Bozza P.T., Souza T.M.L. Atazanavir, alone or in combination with ritonavir, inhibits SARS-CoV-2 replication and proinflammatory cytokine production. Antimicrob Agents Chemother. 2020;64(10) doi: 10.1128/AAC.00825-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Matsuyama S., Kawase M., Nao N., Shirato K., Ujike M., Kamitani W., Shimojima M., Fukushi S., Gallagher T. The inhaled steroid ciclesonide blocks SARS-CoV-2 RNA replication by targeting the viral replication-transcription complex in cultured cells. J Virol. 2020;95(1) doi: 10.1128/JVI.01648-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Skipper C.P., Pastick K.A., Engen N.W., Bangdiwala A.S., Abassi M., Lofgren S.M., Williams D.A., Okafor E.C., Pullen M.F., Nicol M.R., Nascene A.A., Hullsiek K.H., Cheng M.P., Luke D., Lother S.A., MacKenzie L.J., Drobot G., Kelly L.E., Schwartz I.S., Zarychanski R., McDonald E.G., Lee T.C., Rajasingham R., Boulware D.R. Hydroxychloroquine in nonhospitalized adults with early COVID-19: a randomized trial. Ann Intern Med. 2020;173(8):623–631. doi: 10.7326/M20-4207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Bocci G., Bradfute S.B., Ye C., Garcia M.J., Parvathareddy J., Reichard W., Surendranathan S., Bansal S., Bologa C.G., Perkins D.J., Jonsson C.B., Sklar L.A., Oprea T.I. Virtual and in vitro antiviral screening revive therapeutic drugs for COVID-19. ACS Pharmacol Transl Sci. 2020;3(6):1278–1292. doi: 10.1021/acsptsci.0c00131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Choy K.-T., Wong A.-L., Kaewpreedee P., Sia S.F., Chen D., Hui K.P.Y., Chu D.K.W., Chan M.C.W., Cheung P.-H., Huang X., Peiris M., Yen H.-L. Remdesivir, lopinavir, emetine, and homoharringtonine inhibit SARS-CoV-2 replication in vitro. Antiviral Res. 2020;178:104786. doi: 10.1016/j.antiviral.2020.104786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Watashi K. Identifying and repurposing antiviral drugs against severe acute respiratory syndrome coronavirus 2 with in silico and in vitro approaches. Biochem Biophys Res Commun. 2021;538:137–144. doi: 10.1016/j.bbrc.2020.10.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Yuan S., Chan J.F.W., Chik K.K.H., Chan C.C.Y., Tsang J.O.L., Liang R., Cao J., Tang K., Chen L.-L., Wen K., Cai J.-P., Ye Z.-W., Lu G., Chu H., Jin D.-Y., Yuen K.-Y. Discovery of the FDA-approved drugs bexarotene, cetilistat, diiodohydroxyquinoline, and abiraterone as potential COVID-19 treatments with a robust two-tier screening system. Pharmacol Res. 2020;159:104960. doi: 10.1016/j.phrs.2020.104960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Wang M., Cao R., Zhang L., Yang X., Liu J., Xu M., Shi Z., Hu Z., Zhong W.u., Xiao G. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30(3):269–271. doi: 10.1038/s41422-020-0282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Hoffmann M., Kleine-Weber H., Schroeder S., Krüger N., Herrler T., Erichsen S., Schiergens T.S., Herrler G., Wu N.-H., Nitsche A., Müller M.A., Drosten C., Pöhlmann S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181(2):271–280.e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Song Y., Zhang M., Yin L., Wang K., Zhou Y., Zhou M.i., Lu Y. COVID-19 treatment: close to a cure? A rapid review of pharmacotherapies for the novel coronavirus (SARS-CoV-2) Int J Antimicrob Agents. 2020;56(2):106080. doi: 10.1016/j.ijantimicag.2020.106080. [DOI] [PMC free article] [PubMed] [Google Scholar]