Dear Editor,
We read with great interest the article by Chopra et al. recently published on Respiratory Medicine [1].
In their multicenter study, the Authors present incidence, clinical characteristics and outcome of pneumothorax in critically ill patients with coronavirus disease 2019 (COVID-19). They found that pneumothorax rate among invasively ventilated COVID-19 patients is 80/594 (13 %), and mortality rate for patients who developed pneumothorax is 50/80 (62 %). On the contrary, among 160 randomly selected invasively ventilated COVID-19 patients without pneumothorax, mortality was 78/160 (49 %).
We recently published a systematic review on rate of barotrauma among invasively ventilated COVID-19 patients [2]. Our pooled analysis included data from 13 studies and 1814 patients [[3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15]] and we found that pooled estimate of pneumothorax rate was 10.7 % (95 % confidence interval [CI] = 6.7 %–14.7 %), while overall rate of barotrauma event was 16.1 % (95 % CI = 11.8 %–20.4 %). In addition, we found an overall mortality rate for COVID-19 patients who developed barotrauma of 61.6 % (95 % CI = 50.2 %–73.0 %), as compared with a mortality of 49.5 % (95 % CI = 41.1 %–58.0 %) for COVID-19 patients who did not develop barotrauma.
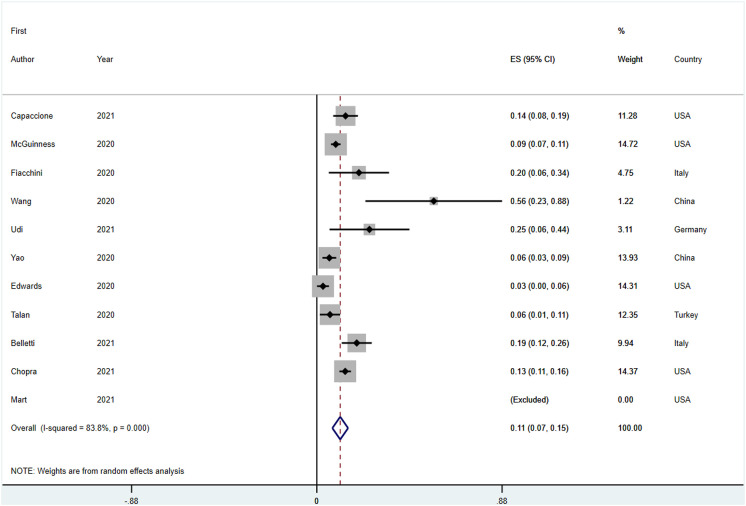
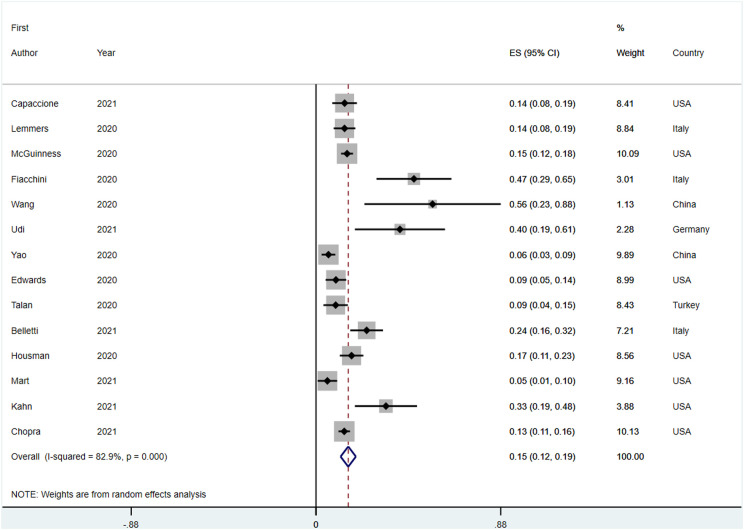
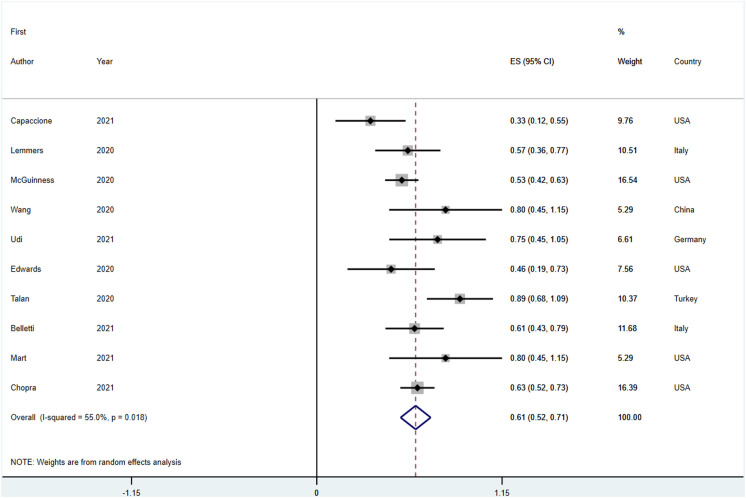
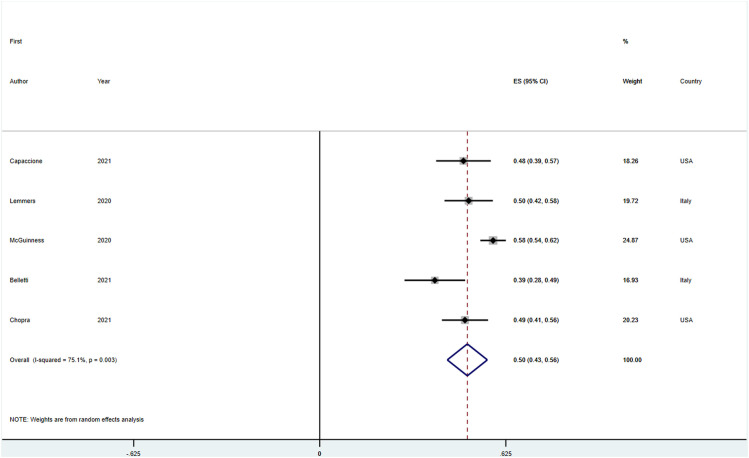
We are pleased to read that our findings are further reinforced by another study, that confirms that pneumothorax rate among mechanically ventilated COVID-19 patients is between 10 and 15 %. Indeed, after including the study by Chopra et al. in an updated meta-analysis, the pooled pneumothorax rate is 11.1 % (95 % CI = 7.4 %–14.8 %) (Fig. 1 ), while the overall barotrauma rate is 15.4 % (95 % CI = 11.7 %–19 %) (Fig. 2 ). Furthermore, the study by Chopra et al. also confirms a mortality rate above 60 % for COVID-19 patients with barotrauma (updated pooled estimate = 61.4 %; 95 % CI = 52.1 %–70.7 %) (Fig. 3 ), as compared with a mortality lower than 50 % for patients who did not develop barotrauma (updated pooled estimate = 49.5 %; 95 % CI = 42.8 %–52.3 %) (Fig. 4 ).
Fig. 1.
Forest plot for pneumothorax development in invasively ventilated COVID-19 patients.
Fig. 2.
Forest plot for barotrauma development in invasively ventilated COVID-19 patients.
Fig. 3.
Forest plot for longest follow-up mortality in invasively ventilated COVID-19 patients who developed barotrauma.
Fig. 4.
Forest plot for longest follow-up mortality in invasively ventilated COVID-19 patients who did not developed barotrauma.
Collectively, these data confirm that barotrauma occur frequently in COVID-19 patients requiring mechanical ventilation, and is associated with a worse outcome and a very high mortality risk. Interestingly, the study by Chopra et al. is one of the few studies that identified worse lung mechanics at start of mechanical ventilation as a risk factor for development of barotrauma [2]. Most of previously published studies reported no significant differences among mechanical ventilation settings/parameters between patients who developed barotrauma and those who did not. They also found a trend towards lower age and higher use of steroids in pneumothorax patients, which were also suggested by other Authors [2,16].
Interestingly, in a recent study by our group, we identified Macklin-like radiological sign [17,18] detected on chest computed tomography (CT) scan as potential predictor of subsequent development of barotrauma about 12 days in advance [3].
Considering the high mortality rate associated with development of barotrauma in COVID-19 patients, and the ongoing debate on optimal timing of intubation in these patients [[19], [20], [21]], we believe that it might be justified to avoid intubation in patients with Macklin-like radiological sign on chest CT, and prefer early support with alternative techniques including awake prone positioning and extracorporeal membrane oxygenation [[22], [23], [24], [25]].
Funding
None.
Declaration of competing interest
None.
Acknowledgements
None.
References
- 1.Chopra A., Al-Tarbsheh A.H., Shah N.J., et al. Pneumothorax in critically ill patients with COVID-19 infection: incidence, clinical characteristics and outcomes in a case control multicenter study. Respir Med. 2021;184 doi: 10.1016/j.rmed.2021.106464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Belletti A., Todaro G., Valsecchi G., et al. Barotrauma in COVID-19 patients undergoing invasive mechanical ventilation: a systematic literature review. Crit Care Med. 2021 doi: 10.1097/CCM.0000000000005283. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Belletti A., Palumbo D., Zangrillo A., et al. Predictors of pneumothorax/pneumomediastinum in mechanically ventilated COVID-19 patients. J Cardiothorac Vasc Anesth. 2021 doi: 10.1053/j.jvca.2021.02.008. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Capaccione K.M., D’souza B., Leb J., et al. Pneumothorax rate in intubated patients with COVID-19. Acute Crit Care. 2021;36(1):81–84. doi: 10.4266/acc.2020.00689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lemmers D.H.L., Abu Hilal M., Bnà C., et al. Pneumomediastinum and subcutaneous emphysema in COVID-19: barotrauma or lung frailty? ERJ Open Res. 2020;6(4) doi: 10.1183/23120541.00385-2020. 00385-02020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fiacchini G., Tricò D., Ribechini A., et al. Evaluation of the incidence and potential mechanisms of tracheal complications in patients with COVID-19. JAMA Otolaryngol Neck Surg. 2021;147(1):70–76. doi: 10.1001/jamaoto.2020.4148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Talan L., Şaşal Solmaz F.G., Ercan U., et al. COVID-19 pneumonia and pneumothorax: case series. Tuberk Toraks. 2020;68(4):437–443. doi: 10.5578/tt.70355. [DOI] [PubMed] [Google Scholar]
- 8.Udi J., Lang C.N., Zotzmann V., et al. Incidence of barotrauma in patients with COVID-19 pneumonia during prolonged invasive mechanical ventilation – a case-control study. J Intensive Care Med. 2021;36(4):477–483. doi: 10.1177/0885066620954364. [DOI] [PubMed] [Google Scholar]
- 9.Yao W., Wang T., Jiang B., et al. Emergency tracheal intubation in 202 patients with COVID-19 in Wuhan, China: lessons learnt and international expert recommendations. Br J Anaesth. 2020;125(1):e28–e37. doi: 10.1016/j.bja.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang X., Duan J., Han X., et al. High incidence and mortality of pneumothorax in critically Ill patients with COVID-19. Heart Lung. 2021;50(1):37–43. doi: 10.1016/j.hrtlng.2020.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Housman B., Jacobi A., Carollo A., et al. COVID-19 ventilator barotrauma management: less is more. Ann Transl Med. 2020;8(23) doi: 10.21037/atm-20-3907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McGuinness G., Zhan C., Rosenberg N., et al. Increased incidence of barotrauma in patients with COVID-19 on invasive mechanical ventilation. Radiology. 2020;297(2):E252–E262. doi: 10.1148/RADIOL.2020202352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mart M.F., Norfolk S.G., Flemmons L.N., et al. Pneumomediastinum in acute respiratory distress syndrome from COVID-19. Am J Respir Crit Care Med. 2021;203(2):237–238. doi: 10.1164/rccm.202008-3376IM. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kahn M.R., Watson R.L., Thetford J.T., Wong J.I., Kamangar N. High incidence of barotrauma in patients with severe coronavirus disease 2019. J Intensive Care Med. 2021;36(6):646–654. doi: 10.1177/0885066621989959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Edwards J.A., Breitman I., Bienstock J., et al. Pulmonary barotrauma in mechanically ventilated coronavirus disease 2019 patients: a case series. Ann Med Surg. 2021;61:24–29. doi: 10.1016/j.amsu.2020.11.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Palumbo D., Campochiaro C., Belletti A., et al. Pneumothorax/pneumomediastinum in non-intubated COVID-19 patients: differences between first and second Italian pandemic wave. Eur J Intern Med. 2021;88:144–146. doi: 10.1016/j.ejim.2021.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Macklin C.C. Transport of air along sheaths of pulmonic blood vessels from alveoli to mediastinum: clinical implications. Arch Intern Med. 1939;64(5):913–926. doi: 10.1001/archinte.1939.00190050019003. [DOI] [Google Scholar]
- 18.Murayama S., Gibo S. Spontaneous pneumomediastinum and Macklin effect: overview and appearance on computed tomography. World J Radiol. 2014;6(11):850–854. doi: 10.4329/wjr.v6.i11.850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Siempos, Xourgia E., Ntaidou T.K., et al. Effect of early vs. Delayed or No intubation on clinical outcomes of patients with COVID-19: an observational study. Front Med. 2020;7 doi: 10.3389/fmed.2020.614152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cabrini L., Ghislanzoni L., Severgnini P., et al. Early versus late tracheal intubation in COVID-19 patients: a pro-con debate also considering heart-lung interactions. Minerva Cardioangiol. 2020 doi: 10.23736/S0026-4725.20.05356-6. In press. [DOI] [PubMed] [Google Scholar]
- 21.Lee Y.H., Choi K.-J., Choi S.H., et al. Clinical significance of timing of intubation in critically ill patients with COVID-19: a multi-center retrospective study. J Clin Med. 2020;9(9) doi: 10.3390/jcm9092847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sartini C., Tresoldi M., Scarpellini P., et al. Respiratory parameters in patients with COVID-19 after using noninvasive ventilation in the prone position outside the intensive care unit. JAMA. 2020;323(22):2338–2340. doi: 10.1001/jama.2020.7861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schmidt M., Pineton de Chambrun M., Lebreton G., et al. Extracorporeal membrane oxygenation instead of invasive mechanical ventilation in a patient with severe COVID-19-associated acute respiratory distress syndrome. Am J Respir Crit Care Med. April 2021 doi: 10.1164/rccm.202102-0259le. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Loyalka P., Cheema F.H., Rao H., Rame J.E., Rajagopal K. Early usage of extracorporeal membrane oxygenation in the absence of invasive mechanical ventilation to treat COVID-19-related hypoxemic respiratory failure. ASAIO J. 2021;67(4):392–394. doi: 10.1097/MAT.0000000000001393. [DOI] [PubMed] [Google Scholar]
- 25.Tang J., Li W., Jiang F., Wang T. Successfully treatment of application awake extracorporeal membrane oxygenation in critical COVID-19 patient: a case report. J. Cardiothorac. Surg. 2020;15(1) doi: 10.1186/s13019-020-01376-9. [DOI] [PMC free article] [PubMed] [Google Scholar]