Abstract
Background and Aims
The coronavirus disease 2019 (COVID-19) pandemic has limited the ability to perform endoscopy. The aim of this study was to quantify the impact of the pandemic on endoscopy volumes and indications in the United States.
Methods
We performed a retrospective analysis of data from the GI Quality Improvement Consortium (GIQuIC) registry. We compared volumes of colonoscopy and esophagogastroduodenoscopy (EGD) during the pandemic (March-September 2020) to before the pandemic (January 2019-February 2020). The primary outcome was change in monthly volumes. Secondary outcomes included changes in the distribution of procedure indications and in procedure volume by region of United States, patient characteristics, trainee involvement, and practice setting, as well as colorectal cancer diagnoses.
Results
Among 451 sites with 3514 endoscopists, the average monthly volume of colonoscopies and EGDs dropped by 38.5% and 33.4%, respectively. There was regional variation, with the greatest and least decline in procedures in the Northeast and South, respectively. There was a modest shift in procedure indications from prevention to diagnostic, an initial increase in performance in the hospital setting, and a decrease in procedures with trainees. The decline in volume of colonoscopy and EGD during the first 7 months of the pandemic was equivalent to approximately 2.7 and 2.4 months of prepandemic productivity, respectively. Thirty percent fewer colorectal cancers were diagnosed compared to expected.
Conclusion
These data on actual endoscopy utilization nationally during the pandemic can help in anticipating impact of delays in care on outcomes and planning for the recovery phase.
Keywords: Colonoscopy, Upper gastrointestinal endoscopy, Volume, COVID-19
What You Need to Know.
Background
The COVID-19 pandemic has limited the ability to perform endoscopy worldwide. We evaluated the impact on endoscopy volumes across the US, particularly among ambulatory surgical centers.
Findings
There was a 38.5% and 33.4% drop in colonoscopies and EGDs performed during the pandemic, equivalent to a loss of 2.7 and 2.4 months of prepandemic productivity. Compared to expected, 30% fewer colorectal cancers were diagnosed.
Implications for patient care
Postponement of endoscopy is likely to result in delayed diagnosis of cancer and other conditions. Prioritizing diagnostic procedures, while also increasing capacity for deferred screening and surveillance procedures is necessary.
Alt-text: Unlabelled box
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has affected the ability to perform endoscopy due to concerns for spreading infection to staff and patients, rationing of personal protective equipment, and diversion of endoscopy personnel and facilities for more acute care needs.1, 2, 3, 4, 5 While professional societies have provided guidance regarding the performance of endoscopy during this pandemic6, 7, 8, 9, 10 and several surveys have assessed self-reported impact of COVID-19 on endoscopy care and plans for triaging,11 , 12 the full impact on endoscopy utilization, particularly in the United States (US), is unknown.13
A survey of endoscopy units in 48 different countries found that nearly all centers had to reduce endoscopy volumes, with the majority reducing >50%.14 A different survey of 252 endoscopy units across 6 continents also showed massive reductions (83%) in endoscopy procedures.15 This magnitude in reduction was mirrored in an analysis of United Kingdom data.16 Reports on changes in endoscopy volumes in the US have been limited to primarily large, academic teaching hospitals.17 , 18 The aim of this study was to quantify the impact of the pandemic on endoscopy volumes and indications in the US among geographically diverse practices, including ambulatory centers.
Materials and Methods
We performed a retrospective analysis of the GI Quality Improvement Consortium (GIQuIC), a large, national clinical data registry of colonoscopy and esophagogastroduodenoscopy (EGD) from endoscopy facilities across the US. GIQuIC captures patient demographics, indication, findings, pathology, and follow-up recommendations, with most participating facilities utilizing endoscopic reporting software to transfer data. GIQuIC data from adults age ≥18 was analyzed from January 1, 2019 through September 30, 2020.
We defined 2 phases for our analysis: (1) “pre-pandemic” (January 2019-February 2020), and (2) “pandemic” (March 2020 through September 2020), based on the time course of COVID-19 in the US. The first US COVID-19 case was on January 20, 2020,19 and the first death on February 6, 2020.20 Mandates regarding social distancing (defined as school closing; available at https://covid19.healthdata.org/united-states-of-america) began in March 2020, and on March 18, 2020, the Centers for Medicare & Medicaid Services issued guidance that all non-urgent surgeries and medical procedures be delayed. Data was extracted from GIQuIC on February 10, 2021 and we limited our evaluation to procedures dated through September 2020 because of the lag time of data upload from sites into GIQuIC, which can take up to several months. Only sites with continuous data input at baseline (defined as ≥1 procedure/each month) were included.
The primary outcome was the change in the monthly number of colonoscopies and EGDs performed during the pandemic compared to baseline. Secondary outcomes included changes in the distribution of procedure indications, and changes in procedure volume by region (Midwest, West, South, Northeast), patient age, sex, comorbidities as measured by American Society of Anesthesiologists (ASA) classification (ASA I/II vs ASA ≥III), fellow trainee involvement, practice setting (office, ambulatory surgery center (ASC), or hospital), and endoscopist specialty (gastroenterology (GI) vs non-GI, as determined by national provider identification (NPI) number). Colonoscopy indications were categorized as screening (no prior history of colon polyps or colorectal cancer), surveillance (prior history of colon polyps or colon colorectal cancer), or diagnostic (eg, diarrhea, anemia, bleeding, etc.). EGD indications were categorized as symptom-driven (eg, gastroesophageal reflux disease (GERD), dysphagia, abdominal pain, diarrhea), surveillance (eg, Barrett's esophagus), bleeding, treatment/intervention (eg, dilation, stent placement), or “other.” We also compared nadirs and peaks in specific months to the corresponding month during the prior year. Finally, we looked at colorectal cancer detected during colonoscopy (defined as a diagnosis of adenocarcinoma on pathology) in terms of absolute numbers per month and as a percentage of colonoscopies performed. GIQuIC did not have reliable data on upper GI cancer diagnoses (ie, esophageal, gastric) over this time period.
We performed descriptive statistics, calculating means and proportions. Categorical variables were compared using a chi-square test. A sensitivity analysis was performed, excluding sites that reported no procedures during the pandemic phase, in order to account for uncertainty in whether these sites were not performing endoscopy or did perform some endoscopy but perhaps lacked staff for reporting due to the pandemic.
This study (#02000526) was considered non-human subjects research and exempt from review by the Dartmouth-Hitchcock Institutional Review Board due to exemption category 4 (secondary research on data) on 6/8/2020.
Results
Description of Practices
Overall, data from 451 practices with 3,514 contributing endoscopists were available for analysis. Among the endoscopists, 2,975 (84.7%) were GI and 539 (15.3%) were non-GI. The practices were located across 46 states and 2 US territories, with 44.6% in the South, 20.6% in the West, 18.2% in the Northeast, and 16.6% in the Midwest. In terms of practice setting, 66.1% were ASCs, 24.4% hospitals, and 3.3% offices, with 6.2% mixed or unknown setting. Since the start of the pandemic, 4 (0.89%) sites did not submit any endoscopy data to GIQuIC.
Overall Change in Volumes of Procedures
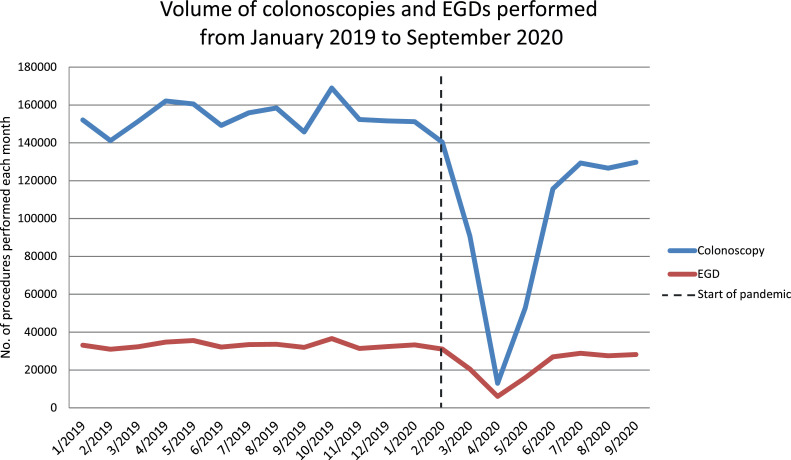
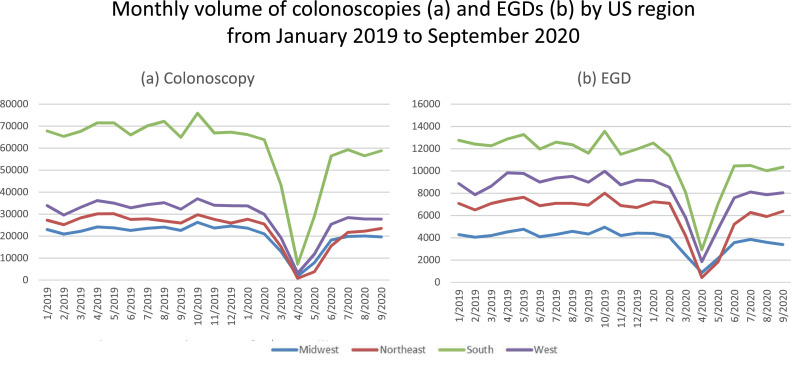
The average monthly volume of colonoscopies dropped from 152,909 in the baseline phase to 93,993 in the pandemic phase, a decline of 38.5% (Figure 1 ). The sharpest decline (92.0%) was in April 2020 compared to April 2019. The average monthly volume of EGDs dropped from 33,025 in the baseline period to 21,989 in the pandemic phase, a decline of 33.4%. Similar to colonoscopy, the sharpest decline in EGD (82.6%) was in April 2020 compared to April 2019. These patterns were seen across the US, with the greatest proportional decline in the Northeast (46.7% for colonoscopy; 39.4% for EGD) compared to the South (35.1% for colonoscopy; 31.4% for EGD) (P< 0.00001; Figure 2 ).
Figure 1.
Monthly volume of colonoscopies and EGDs from January 2019 to September 2020.
Figure 2.
Monthly volume of colonoscopies (a) and EGDs (b) by US region from January 2019 to September 2020.
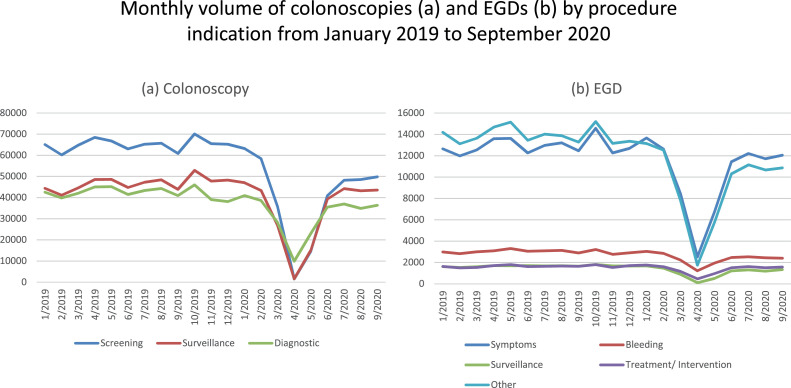
There was a modest shift in the indication for colonoscopy from 72.6% screening and surveillance and 27.4% diagnostic at baseline to 68.9% screening and surveillance and 31.1% diagnostic during the pandemic (Figure 3 a, P < 0.0001). The proportion of diagnostic colonoscopies peaked at 76.1% in April 2020, when the monthly volume of colonoscopies nadired at 12,992, compared to 27.8% in April 2019, when the monthly volume of colonoscopies was 162,065. The proportion of EGDs performed for bleeding and treatment/intervention peaked at 39.2% in April 2020, when the monthly volume of EGDs nadired at 6,066, compared to 23.9% in April 2019, when the monthly volume of EGDs was 34,771 (Figure 3b, P ≤ 0.0001).
Figure 3.
Monthly volume of colonoscopies (a) and EGDs (b) by procedure indication from January 2019 to September 2020.
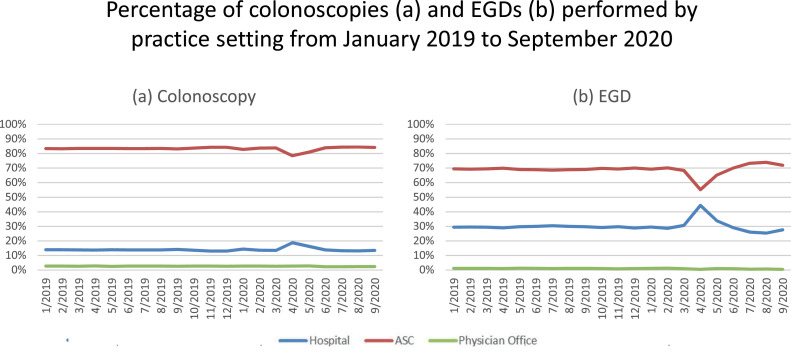
Comparing the baseline to pandemic periods, there was no clinically significant change in the mean age of patients undergoing colonoscopy (59.4-59.3 years, P < 0.0001) or EGD (56.8-56.4 years, P < 0.0001) or the distribution by sex (colonoscopy: 53.9% to 54.2% female, P < 0.0001; EGD: 58.8% to 59.3% female, P= 0.002). During the pandemic, there was a small increase in the proportion of patients with ASA III or higher undergoing colonoscopy (+2.2%, P < 0.0001) and EGD (+1.5%, P < 0.0001). The proportion of patients with ASA III or higher peaked in April 2020 at 28.9% and 44.4% for colonoscopy and EGD, respectively, compared to 20.4% and 31.5%, respectively in April 2019 (both P’s < 0.0001). There was an initial increase in the proportion of colonoscopies (18.8%) and EGDs (44.4%) performed in hospitals compared to ASCs and offices in April and May 2020 that reverted back to pre-pandemic proportions by June 2020 (Figure 4 ).
Figure 4.
Percentage of colonoscopies (a) and EGDs (b) performed by practice setting from January 2019 to September 2020.
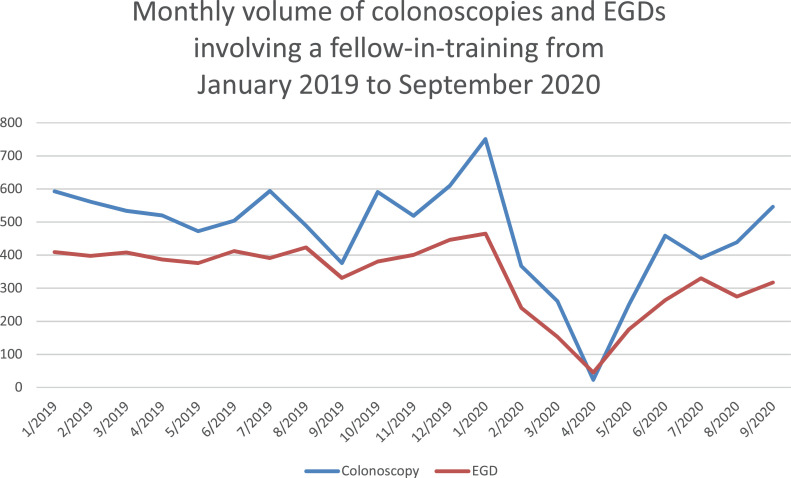
Compared to the pre-pandemic period, cases involving fellows nadired in April 2020, with an overall decrease of 36.6% (p=0.004) and 42.9% (P < 0.0001) in the average monthly number of colonoscopies and EGDs, respectively, in which fellows were involved (Figure 5 ). The change in volume of colonoscopy and EGD during the pandemic did not differ meaningfully by endoscopist specialty (Supplemental data).
Figure 5.
Monthly volume of colonoscopies and EGDs involving fellows-in-training from January 2019 to September 2020.
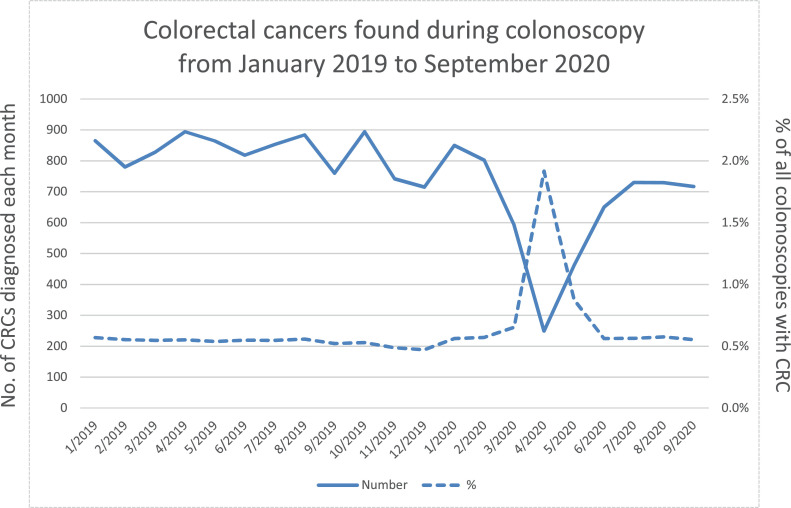
Diagnosis of Colorectal Cancer
From March to September 2020, a total of 4129 colorectal cancers were detected during colonoscopy. This was 1772 cancers (30%) fewer than what would have been expected based on a comparison to the same months in the prior year (March to September 2019) in which 5901 colorectal cancers were detected (Figure 6 ). The percentage of colonoscopies performed in which colorectal cancer was diagnosed was more than twice as high in April and May 2020 compared to April and May 2019 pre-pandemic (1.1% vs 0.5%, P < 0.0001; Figure 6).
Figure 6.
Colorectal cancers found during colonoscopy in absolute numbers and as a percentage of colonoscopies performed from January 2019 to September 2020.
Sensitivity Analysis
The sensitivity analysis, excluding sites with no procedures reported during the pandemic, did not show any meaningful differences in results.
Discussion
In this report of the impact of the pandemic on endoscopy utilization from 443 gastrointestinal endoscopy facilities across the US, we found that colonoscopy and EGD volumes decreased significantly throughout all regions. These trends are consistent with those reported in the Veterans Health systems13 and overall professional consensus to postpone non-urgent procedures.13 , 21 The shift away from routine screening or surveillance toward diagnostic and therapeutic indications is in line with available guidance.6 , 7 , 21 , 22 ASCs and offices showed greater decline in volume compared to hospitals, as may be expected, as hospitals tend to perform procedures on sicker patients with more urgent indications.
A retrospective evaluation of US insurance data covering 41 health care organizations, predominantly large academic health centers and their affiliates found a decrease in colonoscopy and EGD utilization of 85% and 72% during the pandemic.18 The greater decline in that study compared to the current study is likely due to the difference in the duration of data capture since the start of the pandemic (March to July 2020 vs March to September 2020). That study also noted a 73% decrease in endoscopic ultrasound (EUS) and 49% decrease in endoscopic retrograde cholangiopancreatography (ERCP). Our study adds important information on pandemic-related change in endoscopy utilization in ambulatory surgical centers.
Rates of decline in our study at the onset of the pandemic are similar to that seen internationally. In the United Kingdom, where a national endoscopic database captures all endoscopies performed in the country, there was an 89% and 86% decline in performance of colonoscopy and EGD, respectively in March to May 2020.16 Worldwide web-based survey data echo this magnitude of decline.14 , 15 A survey in April 2020 of 48 countries including the US, with >94% hospital-based, teaching facilities, found that the majority of the centers (85%) reported greater than 50% reduction in endoscopy volumes, with 61% and 31% centers reporting over 75% and 90% reduction, respectively.14 Based on self-report, the most common indications for endoscopy were upper GI bleeding, lower GI bleeding, cholangitis, and suspected cancer. A survey conducted by the World Endoscopy Organization in late April-May 2020 of 252 endoscopy units across 55 countries and 6 continents found average reductions of 85% and 82% for colonoscopy and EGD, respectively.15 The reductions in endoscopy volumes were consistent across all continents except for Australia/New Zealand, which performed 41% of their baseline volumes, likely reflecting a lower COVID-19 case burden in these countries (1500 cases by May 25, 2020).15
Fellows-in-training performed fewer procedures since the start of the pandemic. This has implications for skill development and overall training, particularly if volumes remain low over a sustained period.23 The data herein resonates with the decreased involvement of fellows during endoscopy as captured in a web-based survey in the US conducted in March and April 2020. Among the 63 teaching facilities included, 41% had limited involvement of fellows to select endoscopy cases and 49% had eliminated fellows involvement altogether.24 Among the 47 interventional endoscopy training programs, 45% had stopped endoscopy training. Restriction of trainee participation in endoscopy has been met with varying levels of acceptance from fellows.25 An international survey found high rates of anxiety among fellows, in part related to concerns that the reduction in procedure volumes during the pandemic will prolong their training.26 Being a trainee increased the risk for pandemic-related burnout.27
During the first 7 months of the pandemic, over 400,000 fewer colonoscopies and nearly 80,000 fewer EGDs were reported than would be expected from pre-pandemic levels, representing approximately 2.7 and 2.4 months of lost colonoscopy and EGD productivity, respectively. We would expect this loss of productivity to result in a backlog of patients awaiting procedures. In addition, there will likely be patients who will choose to further delay endoscopy while the pandemic continues due to a desire to avoid medical facilities. A single-center survey study found that patients who are older, non-white and undergoing the procedure for screening purposes are more likely to be more concerned with the risk of COVID-19 exposure.28 As vaccinations increase and patient case counts decline, patient wiliness to come for endoscopy may improve. It is unclear what proportion of these apparently deferred procedures will ultimately be performed and when, and the extent to which postponement of endoscopy may result in adverse patient outcomes. A retrospective study at a safety-net teaching hospital found that among 480 patients whose procedures were delayed, colorectal cancer screening was the most common indication.17 In that study, 46% of delayed cases were eventually completed, with a median of 88 days to completion. Colorectal cancers were diagnosed in 9 of 223 patients with delays (4.0%).
The decline in colorectal cancer diagnoses of 30% during the pandemic seen in this study is within the range (12% to 72%) of decline in colorectal cancer diagnosis from other studies in the US18 and from other countries.16 , 31 , 32 When patients with as of yet undiagnosed colorectal cancer come to medical attention, they may present at more advanced stage, with associated negative implications for prognosis, morbidity, and mortality.33 In the setting of abnormal fecal immunochemical testing (FIT), performance of colonoscopy more than 9 months after the abnormal FIT result is associated with adverse colorectal cancer outcomes, including higher incidence of colorectal cancer and advanced stage colorectal cancer.29 Another question is whether and how our systems can continue to prioritize diagnostic colonoscopy for evaluation of symptoms suggestive of a higher likelihood of colorectal cancer,34 while also resuming screening and surveillance exams for colorectal cancer prevention.35 , 36 FIT will likely have an important role in expanding colorectal cancer screening to account for pandemic-related lags in performance of screening colonoscopy and could help risk-stratify those who would most benefit from colonoscopy,30 , 33 , 36
A strength of this study is the inclusion of a large number of sites throughout the US. The change in volume of endoscopic procedures performed across these sites may be useful in models predicting delays in care and the impact on outcomes and resources needed in an eventual recovery phase. Limitations include the inability to account for variable lag time in procedure performance to data upload, which may be prolonged during the pandemic. For this reason, the last month of our analysis was over 4 months prior to the date of data extraction. In addition, a large proportion of EGDs had an unknown “other” indication, which may bias analyses. The change in volume of EGDs with an indication of “other” closely mirrored that of EGDs that were symptom-driven, a pattern that should be further evaluated within GIQuIC. GIQuIC does not capture data on other endoscopic procedures, and thus we cannot comment on changes in their utilization. Information about individual practices was limited to the available variables in GIQuIC. Therefore, we cannot comment on staff schedules and procedure duration before and during the pandemic, nor local availability of personal protective equipment, all of which may have influenced change in procedure volume. While we were able to capture the diagnoses of colorectal cancer, further details such as a stage at diagnosis and mortality were not available. We did not have data on local case counts so cannot comment on correlation between local pandemic surges and endoscopy volumes. Finally, practices in GIQuIC may not be completely representative of endoscopy practice across the US since sites self-select into participation in a quality-focused registry and there is a greater proportion of ASCs.
In summary, this study provides real-world evaluation of endoscopic utilization among a large number of geographically diverse endoscopy practices throughout the US. The decrease in endoscopy performance and shift in indications and locations of care validate prior survey studies among single and multi-centers across the US and provide tangible numbers upon which modeling and triaging may be based, if needed. As endoscopic procedures resume in US healthcare facilities, it will be important to identify those who have missed opportunities for early detection and treatment and address potential disparities in the prioritization of scheduling the backlog of procedures.30 , 37 Future studies should evaluate endoscopy utilization across the US during an eventual recovery phase, including the effect of vaccination, and the impact of delays in care on patient outcomes, such as colorectal cancer stage of diagnosis and mortality.
Footnotes
Conflicts of Interest The authors have no relevant disclosures or conflicts of interest. The contents of this work do not represent the views of the Department of Veterans Affairs or the United States Government.
Funding Dr. Audrey Calderwood is supported by 1R21CA227776-01A1, The Dartmouth-Hitchcock Cancer Research Fellows Program, and by the NCI Cancer Center support grant 5P30CA023108 to the Dartmouth-Hitchcock Norris Cotton Cancer Center as well as The Dartmouth Clinical and Translational Science Institute, under award number UL1TR001086 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH). This material is the result of work supported with resources of the VA Puget Sound Health Care System. The funding agencies played no role in the design, conduct or interpretation of this study.
Author Contributions Conception and design of the study (AHC, JAD); acquisition of data (AHC, MSC, JLW); analysis and interpretation of data (AHC, MSC, JLW, JAD); statistical analysis (JLW); drafting of the manuscript (AHC); critical revision of the manuscript (AHC, MSC, JLW, JAD); study supervision (AHC); approval of the final version of the manuscript (AHC, MSC, JLW, JAD).
Ethical Statement The corresponding author, on behalf of all authors, jointly and severally, certifies that their institution has approved the protocol for any investigation involving humans or animals and that all experimentation was conducted in conformity with ethical and humane principles of research.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.tige.2021.07.003.
Appendix. Supplementary materials
References
- 1.Gralnek IM, Hassan C, Beilenhoff U, et al. ESGE and ESGENA position statement on gastrointestinal endoscopy and the COVID-19 pandemic. Endoscopy. 2020 doi: 10.1055/a-1155-6229. doi: 10.1055/a-1155-6229 [published Online First: 2020/04/18] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Repici A, Maselli R, Colombo M, et al. Coronavirus (COVID-19) outbreak: what the department of endoscopy should know. Gastrointest Endosc. 2020 doi: 10.1016/j.gie.2020.03.019. [published Online First: 2020/03/18] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sultan S, Lim JK, Altayar O, et al. AGA Institute Rapid recommendations for gastrointestinal procedures during the COVID-19 pandemic. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.03.072. [published Online First: 2020/04/05] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gross SA, Robbins DH, Greenwald DA, et al. Preparation in the Big Apple: New York City, a new epicenter of the COVID-19 pandemic. Am J Gastroenterol. 2020;115(6):801–804. doi: 10.14309/ajg.0000000000000636. [published Online First: 2020/05/20] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Repici A, Pace F, Gabbiadini R, et al. Endoscopy units and the COVID-19 outbreak: a multi-center experience from Italy. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.04.003. [published Online First: 2020/04/14] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Soetikno R, Teoh AY, Kaltenbach T, et al. Considerations in performing endoscopy during the COVID-19 pandemic. Gastrointest Endosc. 2020 doi: 10.1016/j.gie.2020.03.3758. [published Online First: 2020/04/02] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Castro Filho EC, Castro R, Fernandes FF, et al. Gastrointestinal endoscopy during COVID-19 pandemic: an updated review of guidelines and statements from international and national societies. Gastrointest Endosc. 2020 doi: 10.1016/j.gie.2020.03.3854. [published Online First: 2020/04/09] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang X, Tang C, Tian D, et al. Management of digestive disorders and procedures associated with COVID-19. Am J Gastroenterol. 2020;115:1153–1155. doi: 10.14309/ajg.0000000000000728. [published Online First: 2020/06/05] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chiu PWY, Ng SC, Inoue H, et al. Practice of endoscopy during COVID-19 pandemic: position statements of the Asian Pacific Society for Digestive Endoscopy (APSDE-COVID statements) Gut. 2020 doi: 10.1136/gutjnl-2020-321185. [published Online First: 2020/04/04] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ang TL. Gastrointestinal endoscopy during COVID-19 pandemic. J Gastroenterol Hepatol. 2020 doi: 10.1111/jgh.15048. [published Online First: 2020/03/28] [DOI] [PubMed] [Google Scholar]
- 11.Mahadev S, Aroniadis OC, Barraza LH, et al. Gastrointestinal endoscopy during the coronavirus pandemic in the New York area: results from a multi-institutional survey. Endosc Int Open. 2020;8:E1865–E1E71. doi: 10.1055/a-1264-7599. [published Online First: 2020/11/27] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kushnir VM, Berzin TM, Elmunzer BJ, et al. Plans to reactivate gastroenterology practices following the COVID-19 pandemic: a survey of North American centers. Clin Gastroenterol Hepatol. 2020;18:2287–2294. doi: 10.1016/j.cgh.2020.05.030. e1[published Online First: 2020/05/25] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gawron AJ, Kaltenbach T, Dominitz JA. The impact of the COVID-19 pandemic on access to endoscopy procedures in the VA healthcare system. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.07.033. [published Online First: 2020/07/28] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alboraie M, Piscoya A, Tran QT, et al. The global impact of COVID-19 on gastrointestinal endoscopy units: an international survey of endoscopists. Arab J Gastroenterol. 2020;21(3):156–161. doi: 10.1016/j.ajg.2020.08.008. [published Online First: 2020/09/12] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parasa S, Reddy N, Faigel DO, et al. Global impact of the COVID-19 pandemic on endoscopy: an international survey of 252 centers from 55 countries. Gastroenterology. 2020;159:1579–1581. doi: 10.1053/j.gastro.2020.06.009. e5[published Online First: 2020/06/15] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rutter MD, Brookes M, Lee TJ, et al. Impact of the COVID-19 pandemic on UK endoscopic activity and cancer detection: a National Endoscopy Database Analysis. Gut. 2021;70:537–543. doi: 10.1136/gutjnl-2020-322179. [published Online First: 2020/07/22] [DOI] [PubMed] [Google Scholar]
- 17.Issaka RB, Feld LD, Kao J, et al. Real-world data on the impact of COVID-19 on endoscopic procedural delays. Clin Transl Gastroenterol. 2021;12:e00365. doi: 10.14309/ctg.0000000000000365. [published Online First: 2021/06/02] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khan A, Bilal M, Morrow V, et al. Impact of the coronavirus disease 2019 pandemic on gastrointestinal procedures and cancers in the United States: a multicenter research network study. Gastroenterology. 2021;160:2602–2604. doi: 10.1053/j.gastro.2021.02.055. e5[published Online First: 2021/03/01] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Team IC-F. Modeling COVID-19 scenarios for the United States. Nat Med. 2021;27:94–105. doi: 10.1038/s41591-020-1132-9. [published Online First: 2020/10/23] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Santa Clara County Public Health. County of Santa Clara identifies three additional early COVID-19 deaths. Secondary Santa Clara Couty Public Health. County of Santa Clara identifies three additional early COVID-19 deaths, 2020. https://covid19.sccgov.org/news-releases/pr-04-21-2020-scc-identifies-three-additional-early-covid-19-deaths.
- 21.Rouillard S, Liu VX, Corley DA. COVID-19: long-term planning for procedure-based specialties during extended mitigation and suppression strategies. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.05.047. [published Online First: 2020/05/20] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Corley DA, Peek RM. COVID-19: what should clinicians and scientists do and when? Gastroenterology. 2020;158:2020–2023. doi: 10.1053/j.gastro.2020.03.026. [published Online First: 2020/05/23] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Soetikno R, Asokkumar R, McGill SK, et al. Simulation-based mastery learning for practicing gastroenterologists-renewed importance in the era of COVID-19. Am J Gastroenterol. 2020;115:1380–1383. doi: 10.14309/ajg.0000000000000788. [published Online First: 2020/08/11] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Forbes N, Smith ZL, Spitzer RL, et al. Changes in gastroenterology and endoscopy practices in response to the coronavirus disease 2019 pandemic: results from a North American survey. Gastroenterology. 2020;159:772–774. doi: 10.1053/j.gastro.2020.04.071. e13[published Online First: 2020/05/08] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clarke K, Bilal M, Sánchez-Luna SA, et al. Impact of COVID-19 pandemic on training: global perceptions of gastroenterology and hepatology fellows in the USA. Dig Dis Sci. 2020:1–5. doi: 10.1007/s10620-020-06655-y. [published Online First: 2020/10/20] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pawlak KM, Kral J, Khan R, et al. Impact of COVID-19 on endoscopy trainees: an international survey. Gastrointest Endosc. 2020;92:925–935. doi: 10.1016/j.gie.2020.06.010. [published Online First: 2020/06/15] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ong J, Ong AML, Ong S, et al. The impact of the coronavirus disease 2019 pandemic on gastroenterologists in Southeast Asia: a mixed-methods study. J Gastroenterol Hepatol. 2021 doi: 10.1111/jgh.15594. [published Online First: 2021/06/24] [DOI] [PubMed] [Google Scholar]
- 28.Taneja V, El-Dallal M, Bilal M, et al. Patient perspective on safety of elective gastrointestinal endoscopy during the COVID-19 pandemic. Tech Innov Gastrointest Endosc. 2021 doi: 10.1016/j.tige.2021.05.001. [published Online First: 2021/05/20] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Forbes N, Hilsden RJ, Martel M, et al. Association between time to colonoscopy after positive fecal testing and colorectal cancer outcomes: a systematic review. Clin Gastroenterol Hepatol. 2020 doi: 10.1016/j.cgh.2020.09.048. [published Online First: 2020/10/04] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Balzora S, Issaka RB, Anyane-Yeboa A, et al. Impact of COVID-19 on colorectal cancer disparities and the way forward. Gastrointest Endosc. 2020;92:946–950. doi: 10.1016/j.gie.2020.06.042. [published Online First: 2020/06/24] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gurney JK, Millar E, Dunn A, et al. The impact of the COVID-19 pandemic on cancer diagnosis and service access in New Zealand-a country pursuing COVID-19 elimination. Lancet Reg Health West Pac. 2021;10 doi: 10.1016/j.lanwpc.2021.100127. [published Online First: 2021/03/30] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Buscarini E, Benedetti A, Monica F, et al. Changes in digestive cancer diagnosis during the SARS-CoV-2 pandemic in Italy: a nationwide survey. Dig Liver Dis. 2021;53(6):682–688. doi: 10.1016/j.dld.2021.02.021. [published Online First: 2021/03/18] [DOI] [PubMed] [Google Scholar]
- 33.Alkatout I, Biebl M, Momenimovahed Z, et al. Has COVID-19 affected cancer screening programs? A systematic review. Front Oncol. 2021;11 doi: 10.3389/fonc.2021.675038. [published Online First: 2021/06/04] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Feuerstein JD, Bilal M, Berzin TM, et al. Triage of general gastrointestinal endoscopic procedures during the COVID-19 pandemic: results from a National Delphi Consensus Panel. Tech Innov Gastrointest Endosc. 2021;23:113–121. doi: 10.1016/j.tige.2020.12.005. [published Online First: 2021/02/02] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Issaka RB, Somsouk M. Colorectal cancer screening and prevention in the COVID-19 era. JAMA Health Forum. 2020;1 doi: 10.1001/jamahealthforum.2020.0588. e200588-e88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shaukat A, Church T. Colorectal cancer screening in the USA in the wake of COVID-19. Lancet Gastroenterol Hepatol. 2020;5:726–727. doi: 10.1016/s2468-1253(20)30191-6. [published Online First: 2020/06/23] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ponchon T, Chaussade S. COVID-19: how to select patients for endoscopy and how to reschedule the procedures? Endosc Int Open. 2020;08:E699–E700. doi: 10.1055/a-1154-8768. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.