Abstract
The Home Health Value-based Purchasing (HHVBP) demonstration, incorporating a payment formula designed to incentivize both high quality care and quality improvement, is expected to become a national program after 2022, when the demonstration ends. This study investigated the relationship between costs and several quality dimensions, to inform HHVBP policy. Using Medicare cost reports, OASIS and Home Health Compare data for 7,673 home health agencies nationally, we estimated cost functions with instrumental variables for quality. The estimated net marginal costs varied by composite quality measure, baseline quality, and agency size. For four of the five composite quality measures the net marginal cost was negative for low quality agencies, suggesting that quality improvement was cost saving for this agency type. As the magnitude of the net marginal cost is commensurate with the payment incentive planned for HHVBP it should be considered when designing the incentives for HHVBP, to maximize their effectiveness.
INTRODUCTION
The Centers for Medicare and Medicaid Services (CMS) is currently implementing a pilot Home Health Value-Based Purchasing (HHVBP) program (CMS.gov, 2016), which is expected to become a national program after the pilot ends in 2022. As CMS did with other value-based purchasing programs in other sectors of the health care system, HHVBP aims to move home health from a volume based model to a model that promotes delivery of higher quality care for Medicare beneficiaries while enhancing efficiency.
HHVBP was introduced in 2016 as a demonstration in nine states: Massachusetts, Maryland, North Carolina, Florida, Washington, Arizona, Iowa, Nebraska, and Tennessee. Payment to all Medicare certified home health agencies (HHAs) in these states has been adjusted based on their quality performance, starting with 3% in 2018, and will increase annually up to 8% by 2022 (CMS.gov, 2016). The payment adjustment is based on improvement quality measures (QMs), process QMs and one hospitalizations QM, all measured with a two year lag (e.g. the 2018 payment is based on 2016 data). The payment adjustment is a composite of two components, one providing incentives for the agency to improve relative to its own prior performance, and the other incentivizing improvement relative to other HHAs.
The CMS has evaluated the first two years of the demonstration (2016 and 2017). The evaluation used mixed methods, comparing performance measures in demonstration and non-demonstration states and to the prior period (2014–2015), in a difference in difference approach, complemented by surveys of HHAs (Arbor Research Collaborative for Health & L&M Policy Research, 2019). The findings showed a modest increase in the improvement QMs and process QMs reported in OASIS (Home Health Outcome and Assessment Information Set), no change in the patient experience measures, and reduction in the hospitalization measure reported in Home Health Compare (HHC) (Medicare.gov, a). However, the hospitalization measure had also exhibited this reduction in 2015, prior to the beginning of the HHVBP demonstration, and thus is likely attributable to other factors, such as the rehospitalization penalty program (CMS.gov, 2012). Of particular interest is the fact that the surveys did not identify any differences in operational activities between demonstration and non-demonstration HHAs and the evaluators concluded that “…Based on our interviews with HHAs … we did not find evidence of an impact of HHVBP on agency quality improvement activities…”(Arbor Research Collaborative for Health & L&M Policy Research, 2019).
NEW CONTRIBUTION
It should be noted that the CMS evaluation only assessed the first two years of the demonstration, in which the financial impact was limited to 3% in year 1 and 5% in year 2. Perhaps as the rewards and penalties increase up to 8% by 2022, HHAs will become more responsive to the incentives. A recent study of HHAs found an increase in the supply of agencies in response to payment add-ons in rural areas only when the add-on was substantial, at 10%, compared to lower add-ons below 5% (Mroz, Patterson, & Frogner, 2020). However, if effective quality improvement initiatives in home care are more expensive than the amounts placed at risk by the HHVBP, then HHAs may find it more cost effective to continue their current practices despite the potential financial rewards promised by the HHVBP.
In this paper we present an analysis that might inform this issue and guide CMS restructuring of the HHVBP program to make it more attractive to HHAs and hence more effective. We present an analysis of the relationship between costs and quality of care in home health. To our knowledge, there have been only three studies of HHA costs in the last two decades.1 Valdmanis, (Valdmanis, Rosko, Leleu, & Mukamel, 2017) studied the overall, technical and scale efficiency of HHAs using a national, 2010 sample. Using Data Envelopment Analysis techniques they found that efficiency could be substantially improved, and that for-profit HHAs were more efficient than non-profit agencies. This study did not address the cost/quality relationship. Cabin et al. (Cabin, Himmelstein, Siman, & Woolhandler, 2014) analyzed costs and quality for 5,808 large HHAs in 2010–2011, employing simple correlation, without controlling for confounders. They found that total costs per patient were negatively correlated with four of five aggregate quality indicators: overall mean quality, improvement in seven functional care outcomes, avoided hospitalization, and avoided increased bed sores. Mukamel at al. (Mukamel et al., 2014) estimated cost functions of a 2010 national sample of large HHAs, but did not account for potential endogenity between costs and quality. The cost functions included four composite quality measures developed from the QMs reported in HHC. Higher quality was associated with lower costs for two measures: hospitalizations and the assessment composite measure. For the treatment composite a significant relationship was found only among the non-profit HHAs, and it was associated with higher costs. These mixed findings of the relationships between cost and quality might be related to the endogeneity.
The study presented here improves on previous studies by estimating cost functions for more recent data, 2014–2017, accounting explicitly for endogeneity using instrumental variables, and including an extensive set of control variables. It offers important policy guidance via an analysis of the incentives provided by the structure exhibited by the estimated cost functions. It links baseline quality of the HHA, the specific quality measure under consideration, the size of the agency in terms of its annual expenditures, and the magnitude of the financial incentive of the HHVBP program.
CONCEPTUAL FRAMEWORK
HHAs faced with HHVBP financial incentives will be deciding whether or not to improve quality of care, and which QM(s) to improve. They will consider the cost of quality improvement associated with any given QM versus the benefits, and choose to improve those QMs for which they anticipate that the combination of the financial incentive provided by HHVBP and the savings from quality improvement will at least equal, if not exceed, the expected costs, i.e. the net costs.
Both costs and savings from improvement are likely to vary across QMs. The QMs measure quality by the percent of patients who experience either better processes of care or better health outcomes. Depending on the processes and health outcomes, as well as the starting (baseline) level of quality, the cost of improvement is likely to vary. For example, educating patients with diabetes on how to care for their feet requires fewer resources than helping a stroke patient regain mobility which may requires extensive physical therapy. Similarly, the savings to be had from quality improvement are due to the fact that the percent of patients who are “healthier” is larger after the HHA has improved its processes. Continuing the example above, patients with diabetes who care for their feet because of the improvement in their education would require fewer foot checks by a visiting nurse to prevent sores. Stroke patients who progress faster in regaining their mobility require less assistance in activities of daily living and require this assistance for shorter periods of time. As a result they are less likely to develop pressure sores, hence requiring less nursing interventions and possibly fewer hospitalization. As with costs, the degree of savings will depend on the QM and the baseline level of quality of the agency.
It is reasonable to hypothesize that HHAs faced with a menu of quality improvement options would first take advantage of those associated with net savings, to which we refer as the “low-hanging fruit” strategies. We, therefore, expect that HHAs at low baseline quality levels are the ones taking advantage of these strategies and hence experience net savings. Taking these actions allow HHAs to incrementally “climb up” the quality ladder, until they eventually exhaust the “low-hanging fruit” options. Any additional improvement will require adoption of strategies that are no longer net cost saving. Hence, we expect to observe declining savings and eventually net costs associated with marginal quality improvement as baseline quality increases. The financial incentive that HHVBP offers changes the calculus for the HHA. It associates quality improvement with higher Medicare payment, thus extending the quality range over which the HHA experiences net savings rather than net costs.
In this paper we estimate cost functions for HHAs. We obtain net costs as a function of composite measures of the QMs, compare them to the HHVBP incentives, and discuss the implications.
METHODS
This study was approved by the Institutional Review Board of the University of California, Irvine (HS# 2016-3012).
Sample and Data
This study included all 8,176 Medicare and Medicaid certified HHAs in operation during 2014–2017 that were large enough to be required to submit full Medicare cost reports, had OASIS data and published QMs in HHC. These are 68% of the 12,000 HHA nationally. Data for each agency were merged using the Medicare provider number for the agency.
The cost reports include information about ownership, number of unique patients by payer, outside contracts for employees by type, and annual expenditures. OASIS includes socio-demographic information for all Medicare and Medicaid patients, patient zip-code, physical and mental health status, services received, and the CMS case-mix index (the Home Health Resource Groups (HHRGs)) which is used in the Home Health Prospective Payment System (HHPPS) (Medicare.gov, b). QMs were obtained from the HHC web site (Medicare.gov, a). The QMs include measures based on OASIS data, Medicare claims, and the patient experience survey, HHCAHPS. We obtained the wage index data used by CMS in setting the HHPPS payments (Medicare.gov, b). It is calculated annually and is used to adjust HHAs’ Prospective Payment rates to reflect annual and regional variations in wages (Centers for Medicare & Medicaid Services, 2018a). HHA Certificate of Need status by state was obtained from the National Conference of State Legislatures (National Conference of State Legislatures, 2019). Household income data by zip-code was obtained from the American Community Survey 5-year Census (United States Census Bureau, 2019) estimates for 2014–2017.
The initial sample included 26,406 HHA-year observations during the 2014–2017 period, corresponding to 8,176 unique HHAs. We excluded HHAs with less than a complete year of cost data, those with missing number of unique patients and those with fewer than 5 competitors in their market. Following the cost reports’ methodology (Federal Register, 2013), we excluded observations in the top and bottom 1% of the total costs distribution. Finally, we excluded observations if the difference of within-agency median cost or the percent annual change within-agency were in the top or bottom 5% of their respective distributions. The final analytic sample included 20,571 (78 %) observations, corresponding to 7,673 (94%) unique agencies. To determine if our findings are sensitive to the exclusion of cost outliers, analyses were repeated without these exclusions. The findings were similar to those reported here.
Variables
Total expenditures, number of unique patients, percent Medicare patients, percent low utilization episodes (LUPA)2, percent partial episodes (PEP)3, a dichotomous variable indicating if the HHA contracted out for temporary employees by type (e.g. RNs, CNAs, therapists), years in operation, chain ownership, and non-profit or government ownership were created for each calendar year between 2014–2017 for each HHA from the cost reports. For HHAs whose fiscal years did not coincide with calendar years, variables were created as a weighted average from two cost reports with weights corresponding to the number of days in the relevant calendar year. Costs were inflated to 2017 dollars using the Consumer Price Index for the Care of Invalids and Elderly at Home (Bureau of Labor Statistics, 2019).
We created five Super QMs (SQMs) as composite measures from the QMs reported in HHC between 2014 and 2017. We were guided by several considerations in creating the SQMs. Because our objective was to make the analysis relevant to HHAs and home health policy we first reviewed all 21 QMs reported during the period and eliminated those that were either topped out (defined as those whose value averaged over 95% during the period) and thus were likely candidates for elimination by CMS in the near future, or those that were already known to be slated for elimination. We then reviewed factor analyses information of clinical groupings of the remaining QMs: The ADLs and pain improvement QMs all loaded on one factor with factor loading ranging above 0.8 for all. The oral medication QM and the breathing improvement QM both involve education of the patient to take care of themselves. These loaded also on one factor with loading factors above 0.8. The HHCAHPS QMs loaded on one factor with weights exceeding 0.8 except for medication safety which loaded at 0.67. Hospitalization and care initiated in a timely care did not group with any remaining QMs. Table 1 lists individual QMs making up each SQM.
Table 1:
Definitions of Super Quality Measures (SQMs)
| Super Quality Measures (SQMs) and Data Sources | Quality Measure in Home Health Compare |
|---|---|
| Patient Improvement in Managing Daily Activities and Pain – OASIS | How often patients got better at walking or moving around? |
| How often patients got better at getting in and out of bed? | |
| How often patients got better at bathing? | |
| How often patients had less pain when moving around? | |
| Timely Care - OASIS | How often the home health team began their patients’ care in a timely manner? |
| Patient Improvement in Self Treatment - OASIS | How often patients’ breathing improved? |
| How often patients got better at taking their drugs correctly by mouth? | |
| Hospitalizations - Claims | How often home health patients had to be admitted to the hospital? |
| Patient Experience – HHCAHPS | Percent of patients who reported that their home health team gave care in a professional way. |
| Percent of patients who reported that their home health team communicated well with them. | |
| Percent of patients who reported that their home health team discussed medicines, pain, and home safety with them. | |
| Percent of patients who gave their home health agency a rating of 9 or 10 on a scale from 0 (lowest) to 10 (highest). | |
| Percent of patients who reported YES, they would definitely recommend the home health agency to friends and family. |
To calculate the SQMs from the individual QMs we standardized each QM using its sample mean and standard deviation. For ADLs/pain, self-care, and patient experience, the standardized QMs were averaged to create the SQMs. The ADLs/Pain SQM was based on an average of 3 non-missing HHC QMs if one of the 4 was missing. The 5 SQMs were re-scaled by multiplying by 10. The hospitalization SQM was redefined such that higher values indicated better quality for all SQMs. Table 2 provides means and ranges for all SQMs.
Table 2:
Summary Statistics
| Study Sample | Excluded Observations** | ||||
|---|---|---|---|---|---|
| Number of Unique HHAs | 7,673 | 503 | |||
| Number of HHA-Year Observations | 20,571 | 5,835 | |||
| Mean (Median) |
Standard Deviation | Mean (Median) |
Standard Deviation | P-value* | |
| Total Cost (in 2017 $) | 3,024,014 (1,796,973) |
3,463,212 | 4,759,854 (1,466,700) |
12,520,117 | <0.001 |
| SQM: Improved Daily Activities/Pain (range −35 to +22) | 0.862 | 7.649 | 1.398 | 7.461 | <0.001 |
| SQM: Timely Care (range −94 to +10) | 1.349 | 8.215 | 1.061 | 8.703 | 0.020 |
| SQM: Improve Self-Treatment (range −34 to +24) | 0.903 | 8.146 | 1.508 | 7.879 | <0.001 |
| SQM: Hospital Admissions (range −62 to +37) | −0.501 | 8.763 | −0.394 | 9.310 | 0.413 |
| SQM: HHCAHPS (range −79 to +21) | 0.387 | 7.312 | −0.057 | 7.692 | <0.001 |
| Number of Unique Patients | 877 (442) |
1,218 | 1588 (356) |
6,946 | <0.001 |
| % Medicare Patients | 70.692 | 24.238 | 67.765 | 27.182 | <0.001 |
| % LUPA Episodes | 7.841 | 5.016 | 8.211 | 5.924 | <0.001 |
| % PEP Episodes | 2.030 | 1.944 | 2.174 | 2.468 | <0.001 |
| Average Case-Mix Index (HHRG) | 0.989 | 0.175 | 0.974 | 0.175 | <0.001 |
| Skilled Nursing Contract (0;1) | 0.357 | 0.473 | 0.358 | 0.475 | 0.851 |
| Home Health Aide Contract (0;1) | 0.184 | 0.383 | 0.212 | 0.406 | <0.001 |
| Occupational Therapy Contract (0;1) | 0.685 | 0.459 | 0.660 | 0.470 | 0.001 |
| Physical Therapy Contract (0;1) | 0.805 | 0.390 | 0.782 | 0.409 | <0.001 |
| Speech Therapy Contract (0;1) | 0.607 | 0.483 | 0.567 | 0.491 | <0.001 |
| Years in Operation | 16.698 | 11.872 | 18.673 | 12.821 | <0.001 |
| Chain Affiliation (0;1) | 0.331 | 0.469 | 0.267 | 0.441 | <0.001 |
| Hospital-based (0;1) | 0.097 | 0.295 | 0.189 | 0.391 | <0.001 |
| For-profit (0;1) | 0.817 | 0.386 | 0.792 | 0.405 | <0.001 |
| Non-profit (0;1) | 0.137 | 0.343 | 0.158 | 0.364 | <0.001 |
| Government (0;1) | 0.046 | 0.209 | 0.050 | 0.217 | 0.289 |
| Standardized Wage Index | 0.000 | 1.011 | 0.000 | 0.960 | 0.990 |
| HHI (Range 0 – 1) | 0.191 | 0.170 | 0.242 | 0.226 | <0.001 |
| State has HH CON (0;1) | 0.179 | 0.384 | 0.183 | 0.387 | 0.510 |
| Average % of households with annual income >= $60K | 41.428 | 9.971 | 41.778 | 10.048 | 0.018 |
| Instrument: Daily Activities/Pain | 0.421 | 4.152 | 1.550 | 4.476 | <0.001 |
| Instrument: Self Care | 0.562 | 4.436 | 1.757 | 4.722 | <0.001 |
| Instrument: Timely Care | 0.559 | 3.519 | 0.919 | 3.998 | <0.001 |
| Instrument: Hospital Admissions | −0.233 | 3.171 | −0.081 | 3.393 | 0.001 |
| Instrument: HHCAHPS | −0.689 | 3.407 | −0.746 | 3.667 | 0.272 |
| Number of Unique Competitors | 221 | 262 | 185 | 244 | <0.001 |
P-value for a two sample t-test comparing the means of the included agency-year observations to the means of the excluded. P-value for the proportion of HH CON for the included agency-year observations to the excluded proportion based on a two-sample z-test.
Means and standard deviations calculated from sample sizes varying from 4,006 for the number of patients and percent of patients that are Medicare, 4,195 for the percent of episodes that PEP/LUPA, 4,271 for total cost, and 4,281 for ownership and contract variables.
HHA: Home Health Agency; SQM: Super Quality Meaure; LUPA: Loq Utilization Payment Adjustment; PEP: Partial Episode Payment;
To define HHAs’ markets, identify their competitors, and measure competition, we used patient zip-code residence data in OASIS. Because HHAs are not brick-and-mortar organizations they can easily adjust their service area. We assumed that even a small number of patients in a zip-code indicates that HHAs view such zip-codes as part of their market. We defined the Herfindahl-Hirschman Index (HHI) for agency i as the weighted average of the HHIs of all zip- codes in which the HHA competed, where the weights equaled the share of admissions of HHAi in the zip-code out of its total admissions. We similarly calculated an admission weighted wage index from zip-code level HHPPS wage indices published by CMS. A variable measuring the admission weighted average percentages of households in each HHA market with annual income equal to or exceeding $60,000 was also calculated in a similar manner.
Analyses
Cost Functions Estimation
We pooled HHA-year observations over the 2014–2017 period and estimated separately three hybrid cost functions, one for the OASIS SQMs, one for the hospitalization SQM, and one for the HHCAHPS SQM, in which the log of total annual costs of an agency are specified as a function of exogenous wages and outputs, (Grannemann, Brown, & Pauly, 1986; Mukamel & Spector, 2000) controlling for cost shifters, as follows:
| (1) |
where Ci,t is total annual cost of HHA i in year t for SQMK (where K=1…3 in the OASIS model, and K=1 in the Claims and HHCAHPS models). P denotes number of unique patients, and W is wage index. X is a vector of cost shifters, such as ownership, case mix index and competition. To allow for non-linear relationship between quality and costs and diminishing returns to scale in the production of quality we included squared terms of SQMs in the cost equation. Studies of nursing home cost functions have found such relationships (Mukamel & Spector, 2000). The model was estimated with robust standard errors with clustering at the agency level.
The correlation amongst the three OASIS based SQMs ranged from 0.19 to 0.82, while the correlations between them and the hospitalization and the HHCAHPS SQMs and the correlations between the latter two ranged from only 0.01 to 0.05. This allowed us to estimate three separate equations, one for the three SQMs based on the OASIS measures, one for the hospitalization SQM, and one for the HHCAHPS SQM. This approach minimizes the number of IVs used in any one model without raising concerns about missing variables bias.
To allow for potential endogeneity between the QMs and costs, we used instrumental variables (IVs) with 2 stage least squares (2SLS). We chose IVs that are often used in industrial organization studies of health care organizations’ behavior (Werner, Norton, Konetzka, & Polsky, 2012) defining IVs for each SQMi,k and each HHAi as the average of SQMj,k of all its competitors (j≠i) in all the markets in which HHAi competes. We first calculated the average quality of all competitors in each zip-code included in the market for the index agency, and then averaged the zip-code-level average quality of the competitors across all the zip-codes comprising the market for the index agency. Each of the three models, OASIS, Claims and HHCAHPS, included different IVs, each constructed from the k SQMs relevant to that model.
A proper IV should be highly correlated with the endogenous variable (non-zero average causal effect). We expect a priori that an HHA’s SQMs will be highly correlated with its competitors’ SQMs. Competing HHAs are expected to compete on quality, especially on publicly reported, and hence observed, SQMs, because price competition is limited when most patients are insured. A similar phenomenon has been observed for nursing homes where publication of QMs in Nursing Home Compare influenced referrals, and led nursing homes to bring their QMs in line with those of their competitors (Kim, 2016; Mukamel, Ye, Glance, & Li, 2015). Table 3 shows that all incremental F statistics in the first stage models (included in the appendix) range from 18.3 to 441.1, exceeding the critical value of F>10 required for rejection of the weak IV hypothesis (Staiger & Stock, 1997). The first stage equations are included in the appendix.
Table 3:
Incremental F Statistics for the 1st Stage Equations for Each Cost Function
| Incremental F | |
|---|---|
| Cost Function with OASIS SQMs | |
| SQM: Improve Daily Activities/Pain | 118.7 |
| SQM2: Improve Daily Activities/Pain | 62.3 |
| SQM: Timely Care | 99.7 |
| SQM2: Timely Care | 18.3 |
| SQM: Improve Self Treatment | 139.6 |
| SQM2: Improve Self Treatment | 69.3 |
| Cost Function with Claims SQMs | |
| SQM: Hospital Admissions | 381.9 |
| SQM2: Hospital Admissions | 21.0 |
| Cost Function with HHCAHPS SQMs | |
| SQM: Patient Experience | 441.1 |
| SQM2: Patient Experience | 62.3 |
A proper IV should also be correlated with the dependent variable only indirectly. This property cannot be tested statistically when the model is exactly identified, as it is in our case. Instead, it should be argued from first principles. In our context, the most likely concern is that this criterion is not met if high average quality among HHAs in a market creates demand for highly skilled labor and bids up wages, which in turn increase costs. However, HHAs do not dominate their labor market. They recruit nurses as well as therapists in a market that is dominated primarily by hospitals, and also includes clinics, nursing homes, and other medical providers (Medicare.gov, b), (Personal Communication, 2016). Hence, it is unlikely that the marginal demand created by HHAs as they improve quality would impact market wages. Nonetheless, to address this concern, we control for wages directly by including them in the regression specification.
Predicted Marginal Costs of Quality
Because we included both linear and squared SQM terms in the estimated cost function, the marginal cost of SQMs cannot be determined directly from the estimated equations. We calculated it as follows from each of the three cost equations:
| (2) |
where ∂Ci,t / ∂SQMi,t,k is the marginal cost for SQMi,t,k , δ1 and δ2 are the estimated coefficients from the second 2SLS equation, and the BaserAdj is the Baser Adjustment (Baser, 2007) to retransform the log cost estimates under heteroscedasticity and normality, both of which were found to apply in our case.
RESULTS
Table 2 presents descriptive statistics. Most variables are significantly different (p<0.05) between the included and excluded observations, however, the mean values are very close and the significance of the difference is likely due to the large sample sizes.
Table 4 presents the 2SLS estimates of the 3 cost functions, as well as the OLS estimates. The R2 ranged from 0.52 to 0.85. The Wooldridge Robust Score (J.M. Wooldridge, 1995) statistics reject the hypotheses that the SQMs are exogenous for all 3 models. All other variables generally behave as one would expect in a cost function. Costs increase with number of patients, wages, case-mix, home health Certificate of Need in the state, and higher average percentage household market income, and decrease with higher percentages of low utilization, higher percentages of partial episodes, and less competitive markets.
Table 4:
Ordinary Least Squares (OLS) and 2 Stage Least Squares (2SLS) Estimates of Three Cost Functions (p values in parentheses)
| OASIS SQM Model Coefficients | Claims (Hospitalizations) SQM Model Coefficients | HHCAHPS SQM Model Coefficients | ||||
|---|---|---|---|---|---|---|
| 2SLS | OLS | 2SLS | OLS | 2SLS | OLS | |
| SQM: Improved Daily Activities/Pain | −0.018 (0.037) |
0.000 (0.789) |
||||
| SQM2: Improved Daily Activities/Pain | 0.001 (0.059) |
0.000 (<0.001) |
||||
| SQM: Timely Care | 0.033 (0.001) |
−0.001 (0.018) |
||||
| SQM2: Timely Care | 0.002 (0.002) |
−0.000 (0.001) |
||||
| SQM: Improve Self-Treatment | −0.026 (<0.001) |
−0.006 (<0.001) |
||||
| SQM2: Improve Self-Treatment | −0.001 (0.003) |
−0.000 (0.296) |
||||
| SQM: Hospital Admissions | 0.020 (<0.001) |
0.000 (0.729) |
||||
| SQM2: Hospital Admissions | 0.004 (<0.001) |
0.000 (<0.001) |
||||
| SQM: HHCAHPS | 0.006 (0.009) |
0.002 (0.004) |
||||
| SQM2: HHCAHPS | 0.001 (<0.001) |
−0.000 (0.690) |
||||
| Log (# of unduplicated patients) | 0.871 (<0.001) |
0.844 (<0.001) |
1.021 (<0.001) |
0.840 (<0.001) |
0.855 (<0.001) |
0.835 (<0.001) |
| % Medicare patients | 0.006 (<0.001) |
0.006 (<0.001) |
0.009 (<0.001) |
0.006 (<0.001) |
0.006 (<0.001) |
0.006 (<0.001) |
| % LUPA episodes | −0.012 (<0.001) |
−0.013 (<0.001) |
−0.012 (<0.001) |
−0.013 (<0.001) |
−0.012 (<0.001) |
−0.013 (<0.001) |
| % PEP episodes | −0.019 (<0.001) |
−0.018 (<0.001) |
−0.023 (<0.001) |
−0.019 (<0.001) |
−0.020 (<0.001) |
−0.018 (<0.001) |
| Average Case-Mix Index | 0.267 (<0.001) |
0.031 (0.281) |
0.127 (0.014) |
−0.030 (0.295) |
−0.040 (0.154) |
−0.031 (0.285) |
| Skilled Nursing Contract yes = 1; no=0 | 0.003 (0.763) |
0.010 (0.229) |
−0.013 (0.296) |
0.014 (0.076) |
0.012 (0.139) |
0.016 (0.048) |
| Home Health Aide Contract yes =1; no=0 | 0.047 (0.001) |
0.050 (<0.001) |
0.041 (0.004) |
0.050 (<0.001) |
0.040 (<0.001) |
0.051 (<0.001) |
| Occupational Therapy Contract yes = 1; no=0 | 0.015 (0.265) |
0.023 (0.020) |
0.025 (0.105) |
0.028 (0.006) |
0.029 (0.006) |
0.028 (0.005) |
| Physical Therapy Contract yes = 1; no=0 | −0.014 (0.345) |
−0.013 (0.245) |
−0.039 (0.019) |
−0.013 (0.251) |
−0.014 (0.230) |
−0.012 (0.308) |
| Speech Therapy Contract yes = 1; no=0 | 0.008 (0.525) |
0.006 (0.493) |
0.063 (<0.001) |
0.008 (0.365) |
0.024 (0.014) |
0.008 (0.337) |
| Years in Operation | 0.002 (0.001) |
0.002 (<0.001) |
0.002 (<0.001) |
0.002 (<0.001) |
0.002 (<0.001) |
0.002 (<0.001) |
| Part of a Chain yes = 1; no=0 |
0.115 (<0.001) |
0.054 (<0.001) |
0.070 (<0.001) |
0.044 (<0.001) |
0.052 (<0.001) |
0.043 (<0.001) |
| Hospital-Based yes = 1; no=0 |
0.147 (<0.001) |
0.159 (<0.001) |
0.181 (<0.001) |
0.152 (<0.001) |
0.134 (<0.001) |
0.148 (<0.001) |
| Non-Profit yes = 1; no=0 |
0.016 (0.399) |
0.019 (0.193) |
−0.010 (0.652) |
0.021 (0.159) |
0.026 (0.100) |
0.020 (0.183) |
| Government yes = 1; no=0 |
−0.062 (0.044) |
−0.041 (0.108) |
−0.020 (0.570) |
−0.038 (0.141) |
−0.051 (0.057) |
−0.042 (0.103) |
| Standardized Wage Index | 0.055 (<0.001) |
0.024 (<0.001) |
0.016 (0.020) |
0.020 (<0.001) |
0.015 (0.024) |
0.022 (<0.001) |
| State has HH CON = 1 | 0.081 (<0.001) |
0.030 (0.007) |
0.037 (0.012) |
0.025 (0.025) |
0.000 (0.973) |
0.024 (0.038) |
| HHI (Range 0 – 1) | −0.094 (0.015) |
−−0.126 (<0.001) |
−0.011 (0.813) |
−0.151 (<0.001) |
−0.134 (<0.001) |
−0.160 (<0.001) |
| % Households with income >= $60K | 0.003 (<0.001) |
0.003 (<0.001) |
0.004 (<0.001) |
0.002 (<0.001) |
0.003 (<0.001) |
0.002 (<0.001) |
| Year | 0.080 (<0.001) |
0.015 (<0.001) |
0.007 (0.073) |
0.003 (0.138) |
0.003 (0.196) |
0.003 (0.143) |
| Constant | −152.0 (<0.001) |
−21.8 (<0.001) |
−7.1 (0.370) |
2.9 (0.478) |
3.2 (0.455) |
3.0 (0.454) |
| Number of Observations | 20,571 | 20,571 | 20,571 | 20,571 | 20,571 | 20,571 |
| Number of HHAs | 7,673 | 7,673 | 7,673 | 7,673 | 7,673 | 7,673 |
| R2 | 0.704 | 0.854 | 0.517 | 0.851 | 0.835 | 0.851 |
| H0: SQM is Exogenous (Wooldridge’s Robust Score Test) | 37.11 (<0.001) |
47.43 (<0.001) |
11.21 (<0.001) |
|||
HHCAPS:Home Health ConsumerAssassment of Healthcare Providers & Systems;OASIS:Outcomes & Assessment Information set
Figure 1 presents the net marginal costs due to a 1 unit increase in an SQM from its baseline level for HHAs at the 25th, 50th and 75th percentiles of the predicted annual cost distribution. Quality, as measured by the SQMs, increases from left to right, with the range of values shown being the range observed in our sample of HHAs. Net marginal costs can be negative, indicating net savings, or positive, indicating net costs. For example, for the median annual cost HHA, the net marginal cost for the hospitalization SQM starts at a savings of close to $200,000 for HHA of very low quality and SQM of around −15. Savings decline (net marginal costs become less negative) as quality increases and reaches $0 when quality is at about SQM=−3, and continues to increase to positive values for net marginal costs, indicating that further quality improvement for this SQM and this HHA will entail net costs rather than savings. For the median annual cost HHA at very high levels of quality, further improvement will be quite expensive at the margin, more than $500,000.
Figure 1:
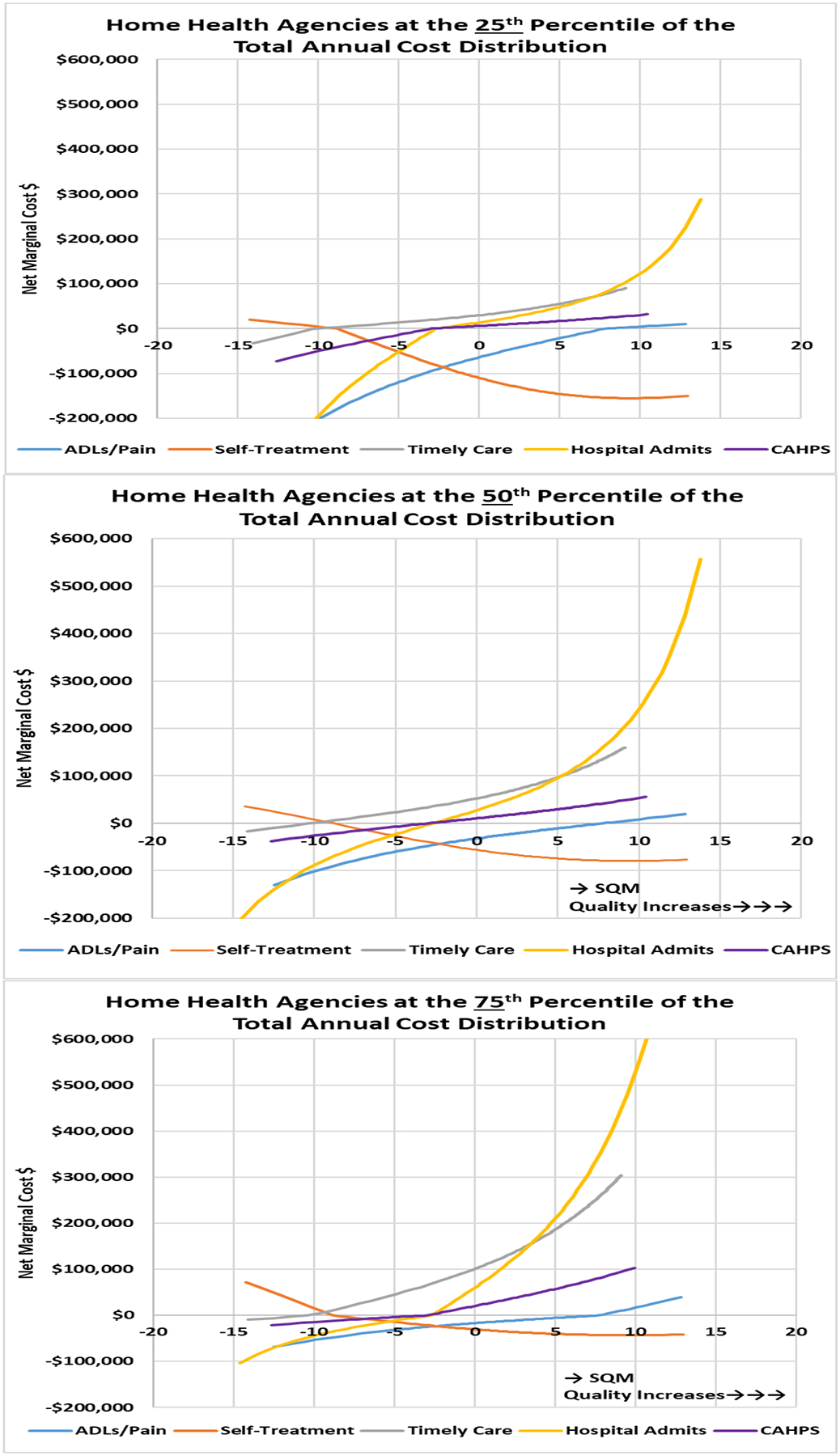
Net Marginal Cost for a 1 Unit Increase as the SQM increases from Baseline for Agencies at the 25th, 50th and 75th Percentiles of the Total Cost Distribution (Source: Author’s contribution)
All SQMs, except for the self-treatment SQM, exhibit net savings when baseline quality is low. The net savings decrease and eventually turn into net costs as baseline quality increases. In other words, as baseline quality increases the marginal costs seem to increase faster than the marginal savings. HHAs that start with higher levels of quality seem to gain less savings and incur more costs when implementing quality improvement strategies that increase their quality by 1 SQM unit compared with HHAs that are starting from a lower baseline quality level. Both the level of the net marginal costs and the rate at which it changes with baseline quality are different across SQMs and for HHAs of different sizes. In general, the smaller HHAs, at the lowest 25th percentile of the cost distribution, HHAs that also tend to treat fewer patients, are more likely to experience net savings, and the larger HHAs, at the 75th percentile and above, that also tend to treat more patients, are more likely to experience net costs.
Self-treatment is the one SQM that exhibits a different behavior. Rather than diminishing net savings as baseline quality increases it shows net costs at low baseline quality, which declines and turns into net saving when baseline quality increases.
Table 5 presents the predicted net marginal costs for the median SQMs for different size agencies, the percentage of net marginal costs within total agency annual costs, and the predicted net marginal cost per patient. Table 5 demonstrates that predicted net total costs increase in absolute value with agency size, but decrease as the number of unique patients increase. It also shows that as percent of total cost, net marginal costs vary from less than 1% to close to 7%.
Table 5:
Net Marginal Costs for a 1 Unit Increase in the SQM At Different Levels of the Total Costs Distributions for the Median SQMs (Predicted total net marginal costs as percent of total agency annual costs are shown in parentheses)
| Predicted Total Net Marginal Costs (in Thousands 2017 $) | Predicted Net Marginal Cost per Unique Patient (2017 $) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HHAs Cost Ranges in Percentiles | 0 – 10th | 10th – 25th | 25th – 50th | 50th – 75th | 75th – 90th | 90th – 100th | 0 – 10th | 10th – 25th | 25th – 50th | 50th – 75th | 75th – 90th | 90th – 100th |
| Sample Size | N=2,058 | N=3,085 | N=5,143 | N=5,143 | N=3,085 | N=2,057 | N=2,058 | N=3,085 | N=5,143 | N=5,143 | N=3,085 | N=2,057 |
| OASIS SQM Model | ||||||||||||
| Daily activity / pain | ||||||||||||
| 50th percentile SQM = 1.19 |
−8,079 (−2.6%) |
−12,174 (−1.3%) |
−19,835 (−1.6%) |
−35,860 (−1.2%) |
−66,726 (−1.5%) |
−134,404 (−1.5%) |
−70 | −67 | −63 | −56 | −51 | −43 |
| Self-treatment | ||||||||||||
| 50th percentile SQM = 1.69 |
−20,200 (−5.0%) |
−29,765 (−3.2%) |
−47,078 (−3.3%) |
−84,415 (−2.9%) |
−155,610 (−2.5%) |
−304,501 (−3.0%) |
−176 | −160 | −150 | −132 | −118 | −99 |
| Timely Care | ||||||||||||
| 50th percentile SQM = 3.68 |
+28,034 (+6.7%) |
+41,667 (+4.9%) |
+64,907 (+5.0%) |
+108,893 (+3.3%) |
+202,745 (+5.1%) |
+413,228 (+4.2%) |
+237 | +225 | +201 | +169 | +151 | +134 |
| Claims SQM Model | ||||||||||||
| Hospital Admits | ||||||||||||
| 50th percentile SQM = −0.54 |
+5,734 (+1.2%) |
+9,085 (+1.4%) |
+15,660 (+1.0%) |
+30,631 (+1.5%) |
+65,429 (+1.3%) |
+145,267 (+1.3%) |
+54 | +54 | +52 | +49 | +49 | +48 |
| Survey SQM Model | ||||||||||||
| Patient Experience | ||||||||||||
| 50th percentile SQM = 1.33 |
+5,055 (+1.2%) |
+7,452 (+0.9%) |
+11,656 (+0.7%) |
+20,354 (+0.9%) |
+38,132 (+0.6%) |
+76,569 (+0.7%) |
+47 | +43 | +38 | +32 | +29 | +25 |
We repeated these analyses to test the sensitivity of our findings to the exclusion of the nine demonstration states, as these states might have behaved differently starting in 2016, given the expectation of the implementation of HHVBP payment adjustment in 2018 based on 2016 data. The findings, however, are similar, with no significant differences between the marginal net costs for the full sample and the sample excluding the nine demonstration states.4
DISCUSSION
This study estimates cost functions for the 68% largest HHAs nationally. We find that the estimated net marginal costs varies by SQM, baseline quality, and agency’s annual expenditures level. For four of the five (SQMs): ADLs/pain, timely care, hospitalizations and patient experience, the net marginal cost is negative for low baseline quality agencies, suggesting that quality improvement is cost saving for these agency types. The net marginal cost increases as baseline quality increases. It becomes positive for agencies with high baseline quality. Self-treatment exhibits the opposite pattern, with a positive net marginal cost at low levels of baseline quality, which declines as baseline quality increases. These findings support the “low-hanging fruit” hypothesis we posit in the conceptual framework section for the ADLs/pain, timely care, hospitalizations and patient experience SQMs. These findings also raise the question of why we observe the opposite behavior for the self treatment SQM.
To address this question we first note that the marginal cost of quality we estimated is a net cost. It includes all investments associated with improving quality, such as increased number of visits per episode, enhanced training of staff to improve the “content” of a visit, providing staff with better equipment such as mobile monitors, or using tele-monitors in patients’ homes. It also includes all savings that might result from improvement in care and health outcomes, such as need for fewer follow-up visits or less intensive care as the patient’s condition improves (Mukamel & Spector, 2000). Hence, we need to consider all processes of care to understand the cost/quality relationship.
We reviewed our findings with HHA clinical and financial experts who suggested that the self treatment SQM may reflect fundamental differences in the way care is delivered when compared with the other SQMs. This SQM requires the HHA staff to educate patients on how to take care of themselves rather than have the HHA staff provide ongoing “hands-on care”. This implies an initial intensive staff effort to bring the patient to a level of self-treatment that allows the patient to maintain his/her health and avert future complications and deterioration, unlike the other SQMs that require ongoing, direct provision of care by the staff. Thus, the more successful the staff is at educating patients about self-care, the more patients will experience better outcomes without requiring a high level of ongoing staff care, and net savings are likely to increase as baseline quality increases.
Incentives and HHVBP
Our findings have behavioral implications that may influence the impact of the incentives in the HHVBP. First, we note that the magnitude of the net marginal costs are commensurate with the payment incentives under the HHVBP (see Table 5): Both are on the order of several percentage points of total annual costs or payment. HHAs likely will consider not only the incentives in the payment system when adopting a particular strategy, but also the net costs of improvement. As both are of similar magnitude, HHAs’ expectation of the net marginal costs may either enhance or detract from the impact of the payment incentives, depending on whether they are positive or negative.
Net marginal costs vary with the SQM, the baseline quality and the HHA size, but the variation has a different pattern from the variation in the financial incentives. The HHVBP system as set in the 2016 HH PPS final rule (Centers for Medicare & Medicaid Services, 2018b) included two components, an improvement component that was based on the degree of improvement in performance of the HHA relative to its baseline, and an achievement component based on its performance relative to the top decile in its state. Under this rule, both were given equal weight and the QMs contributing to each measure were given equal weight. The only factor that affected the size of the incentive differentially across QMs and HHAs was the degree to which an agency’s QMs deviated from their baselines and benchmarks. Our analysis of the marginal net costs, specifically the fact that net savings exceed costs at low baseline quality and then diminish (except for the self-treatment SQM) suggests that HHAs will have stronger incentives to improve when their baseline quality is low. This implies that the net marginal costs in general enhance the improvement component of the incentives in the HHVBP that targets the low baseline HHAs, and are less effective for the achievement component that targets the high baseline agencies. Furthermore, the hospitalization SQM has the largest net marginal cost values, and is thus the least likely to be chosen for improvement.
The CMS implemented changes in the rules for the HHVBP in calendar year 2019 (Centers for Medicare & Medicaid Services, 2018b) in a direction that tends to ameliorate both of the disincentives we identified in our analysis above. As we note, the achievement component of the HHVBP is less effective given the cost/quality structure we find. The 2019 changes made by CMS to the HHVBP methodology increase the relative weight of the achievement component relative to the improvement component, thus ameliorating this disincentive. Furthermore, the hospitalization SQM, which our findings suggest is the least likely to be chosen for improvement, receives an increased weight by the 2019 changes, counteracting the disincentive to choose the hospitalization QM for improvement due to the cost/quality relationship we find. It remains to be seen if the magnitude of the changes instituted by CMS will suffice to overcome the potential disincentives due to net marginal costs.
Limitations
We should note several limitations of our study. First, due to availability of cost and QM data only for sufficiently large HHAs, we were able to include only 8,176 HHAs (in our initial sample) out of the about 12,000 (68%) agencies nationally. Another limitation, necessitated by the complexity of the data and the methodology, is that we were unable to estimate costs of individual QMs directly and instead estimated the costs of SQMs. This makes our findings less directly relevant to policy makers and HHAs. However, the findings offer insights that can help decision makers. In particular, while they do not offer the granularity required for immediate action, they do provide information about general areas of quality and the QMs making up those areas, thus helping to prioritize and focus quality improvement initiatives.
Summary
In summary, to our knowledge this is the first study that estimates the relationship between costs and quality in home health, accounting for endogeneity and non-linearity in quality. The net marginal costs vary with the baseline level of quality of the agency, its annual expenditures level, and the specific area of quality. Agencies have incentives to adopt first those quality improvement efforts that are likely to generate net savings, namely the “low-hanging fruit” strategy. The insights provided by these analyses could inform design of value-based purchasing payment systems and their effectiveness.
Supplementary Material
Footnotes
There have been studies investigating home health “costs” where costs refer to the Medicare payment per beneficiary. Those are different from the annual expenditures of the agency, which we are referring to in this study.
HHAs are paid by the Medicare PPS system for a 60 day episode. A LUPA episode is defined as an episode with 4 or fewer home visits by the agency.
HHAs are paid by the Medicare PPS system for a 60 day episode. A PEP episode is an episode that is terminated prior to the 60th day.
The only exceptions were two levels of initial quality for the HHCAHPS model.
Contributor Information
Dana B. Mukamel, Department of Medicine, Division of General Internal Medicine; iTEQC Research Program; University of California, Irvine, CA.
Heather Ladd, Department of Medicine, Division of General Internal Medicine; iTEQC Research Program; University of California, Irvine.
Eugene Nuccio, School of Medicine; Division of Health Care Policy & Research; University of Colorado Anschutz Medical Campus.
Jacqueline S. Zinn, Fox School of Business; Temple University.
Dara H. Sorkin, Public Health, and Psychology and Social Behavior; Department of Medicine, Division of General Internal Medicine; University of California, Irvine.
Susan L. Ettner, Department of Medicine; Division of General Internal Medicine and Health Services Research; University of California, Los Angeles.
REFERENCES
- Arbor Research Collaborative for Health, & L&M Policy Research. (2019). Evaluation of the Home Health Value-Based Purchasing (HHVBP) Model - Second Annual Report - December Retrieved from https://innovation.cms.gov/files/reports/hhvbp-secann-rpt.pdf
- Baser O (2007). Modeling Transformed Health Care Cost with Unknown Heteroskedasticity. Applied Economics Research, 1, 1–6. [Google Scholar]
- Bureau of Labor Statistics. (2019). County Employment and Wages (QCEW) database now fully updated through 4th quarter 2018. Retrieved from https://www.bls.gov/home.htm
- Cabin W, Himmelstein DU, Siman ML, & Woolhandler S (2014). For-profit medicare home health agencies’ costs appear higher and quality appears lower compared to nonprofit agencies. Health Aff (Millwood), 33(8), 1460–1465. doi: 10.1377/hlthaff.2014.0307 [DOI] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services. (2018a). Medicare and Medicaid Programs; CY 2019 Home Health Prospective Payment System Rate Update and CY 2020 Case-Mix Adjustment Methodology Refinements; Home Health Value-Based Purchasing Model; Home Health Quality Reporting Requirements; Home Infusion Therapy Requirements; and Training Requirements for Surveyors of National Accrediting Organizations (CY 2019 HOME HEALTH WAGE INDEX). Retrieved from https://www.federalregister.gov/documents/2018/11/13/2018-24145/medicare-and-medicaid-programs-cy-2019-home-health-prospective-payment-system-rate-update-and-cy#h-43 [PubMed]
- Centers for Medicare & Medicaid Services. (2018b). Medicare and Medicaid Programs; CY 2019 Home Health Prospective Payment System Rate Update and CY 2020 Case-Mix Adjustment Methodology Refinements; Home Health Value-Based Purchasing Model; Home Health Quality Reporting Requirements; Home Infusion Therapy Requirements; and Training Requirements for Surveyors of National Accrediting Organizations. Retrieved from https://www.federalregister.gov/documents/2018/11/13/2018-24145/medicare-and-medicaid-programs-cy-2019-home-health-prospective-payment-system-rate-update-and-cy [PubMed]
- CMS.gov. (2012). Hospital Readmissions Reduction Program (HRRP). Retrieved from https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/HRRP/Hospital-Readmission-Reduction-Program
- CMS.gov. (2016). Home Health Value-Based Purchasing Model. Retrieved from https://innovation.cms.gov/initiatives/home-health-value-based-purchasing-model
- Federal Register. (2013). Proposed Rule 42 CFR Part 431 Vol 78, No 128. July 3, 2013 Retrieved from https://www.govinfo.gov/content/pkg/FR-2013-07-03/pdf/2013-15766.pdf
- Grannemann W, Brown S, & Pauly MV (1986). Estimating Hospital Costs: A Multiple Output Analysis. J Health Econ, 5(2), 107–127. [DOI] [PubMed] [Google Scholar]
- Wooldridge JM. (1995). Score diagnostics for linear models estimated by two stage least squares. In Advances in Econometrics and Quantitative Economics: Essays in Honor of Professor C.R. Rao by G. S. Maddala (Editor), T. N. Srinivasan (Editor), Peter C. B. Phillips (Editor) (pp. 66–87): Oxford: Blackwell. [Google Scholar]
- Kim AS (2016). Market Conditions and Performance in the Nursing Home Compare Five-Star Rating. J Health Polit Policy Law, 41(5), 939–968. doi: 10.1215/03616878-3632221 [DOI] [PubMed] [Google Scholar]
- Medicare.gov. (a). Home Health Compare - Find a home health agency. Retrieved from https://www.medicare.gov/homehealthcompare/search.html
- Medicare.gov. (b). Home Health Prospective Payment System Regulations and Notices. Retrieved from https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HomeHealthPPS/Home-Health-Prospective-Payment-System-Regulations-and-Notices.html
- Mroz TM, Patterson DG, & Frogner BK (2020). The Impact Of Medicare’s Rural Add-On Payments On Supply Of Home Health Agencies Serving Rural Counties. Health Aff (Millwood), 39(6), 949–957. doi: 10.1377/hlthaff.2019.00952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukamel DB, Fortinsky RH, White A, Harrington C, White LM, & Ngo-Metzger Q (2014). The policy implications of the cost structure of home health agencies. Medicare Medicaid Res Rev, 4(1). doi: 10.5600/mmrr2014-004-01-a03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukamel DB, & Spector WD (2000). Nursing home costs and risk adjusted outcome measures of quality. . Med Care, 38(1), 78–89. [DOI] [PubMed] [Google Scholar]
- Mukamel DB, Ye Z, Glance LG, & Li Y (2015). Does mandating nursing home participation in quality reporting make a difference? Evidence from Massachusetts. Med Care, 53(8), 713–719. doi: 10.1097/mlr.0000000000000390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Conference of State Legislatures. (2019). Certificate of Need State Laws. Retrieved from http://www.ncsl.org/research/health/con-certificate-of-need-state-laws.aspx
- Personal Communication (2016). [Home Health Agencies Director’s Interviews].
- Staiger D, & Stock JH (1997). Instrumental Variables Regression with Weak Instruments. Econometrica, 65(3), 557–586. [Google Scholar]
- United States Census Bureau. (2019). American Community Survey Data. Retrieved from https://www.census.gov/programs-surveys/acs/data.html
- Valdmanis VG, Rosko MD, Leleu H, & Mukamel DB (2017). Assessing overall, technical, and scale efficiency among home health care agencies. Health Care Manag Sci, 20(2), 265–275. doi: 10.1007/s10729-015-9351-1 [DOI] [PubMed] [Google Scholar]
- Werner RM, Norton EC, Konetzka RT, & Polsky D (2012). Do consumers respond to publicly reported quality information? Evidence from nursing homes. J Health Econ, 31(1), 50–61. doi: 10.1016/j.jhealeco.2012.01.001 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


