Abstract
Glucocorticoid-induced osteoporosis (GIOP) is the most common form of secondary osteoporosis, accounting for 20% of osteoporosis diagnoses. Using glucocorticoids for >6 months leads to osteoporosis in 50% of patients, resulting in an increased risk of fracture and death. Osteoblasts, osteocytes, and osteoclasts work together to maintain bone homeostasis. When bone formation and resorption are out of balance, abnormalities in bone structure or function may occur. Excess glucocorticoids disrupt the bone homeostasis by promoting osteoclast formation and prolonging osteoclasts' lifespan, leading to an increase in bone resorption. On the other hand, glucocorticoids inhibit osteoblasts' formation and facilitate apoptosis of osteoblasts and osteocytes, resulting in a reduction of bone formation. Several signaling pathways, signaling modulators, endocrines, and cytokines are involved in the molecular etiology of GIOP. Clinically, adults ≥40 years of age using glucocorticoids chronically with a high fracture risk are considered to have medical intervention. In addition to vitamin D and calcium tablet supplementations, the major therapeutic options approved for GIOP treatment include antiresorption drug bisphosphonates, parathyroid hormone N-terminal fragment teriparatide, and the monoclonal antibody denosumab. The selective estrogen receptor modulator can only be used under specific condition for postmenopausal women who have GIOP but fail to the regular GIOP treatment or have specific therapeutic contraindications. In this review, we focus on the molecular etiology of GIOP and the molecular pharmacology of the therapeutic drugs used for GIOP treatment.
KEYWORDS: Bone remodeling, Glucocorticoid, Osteoblast, Osteoclast, Secondary osteoporosis
INTRODUCTION
There are >49 million patients with osteoporosis in developed countries, such as the United States, European Union, Australia, and Japan [1]. Patients with osteoporosis tend to develop vertebrae and hip fractures. Vertebrae fractures and fragility fractures at other sites of the body have increased by millions with the population of osteoporosis [2,3,4,5], which causes a heavy financial burden on the country [2,6]. Moreover, complications may arise in addition to pain and limited mobility, which increases the risk of death in fracture patients and imposes financial burdens on the family and society [7,8]. Therefore, several countries recognize osteoporosis as a major public health issue, and the World Health Organization has ranked osteoporosis as the second most crucial health care issue worldwide. Osteoporosis can be divided into (1) primary osteoporosis (including postmenopausal osteoporosis and senile osteoporosis) and (2) secondary osteoporosis. Primary osteoporosis is most common in postmenopausal women [9,10,11] and elderly persons [12]. Secondary osteoporosis has been associated with various congenital diseases and endocrine disharmony, as well as nutritional status and some medications [13]. The most common form of secondary osteoporosis is glucocorticoid-induced osteoporosis (GIOP) [14], accounting for 20% of all forms of osteoporosis [15]. The majority of these patients have autoimmune diseases (e.g., rheumatoid arthritis and lupus erythematosus), allergic diseases (e.g., asthma and atopic dermatitis), or have undergone organ transplantation. GIOP occurs in two phases: an early phase in which bone mineral density (BMD) declines due to rapid bone resorption and a slow and progressive phase in which BMD declines due to the impaired bone formation [16]. The underlying mechanism of GIOP could be complicated and multifactorial. In this review, we provide an overview of the molecular etiology, assessment, and treatment options in the aspect of molecular pharmacology for GIOP.
ENDOGENOUS GLUCOCORTICOID IS REQUIRED FOR BONE HOMEOSTASIS
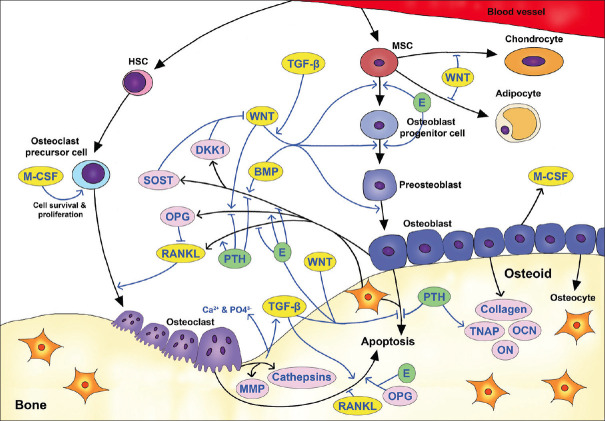
Bone remodeling is a normal physiological process that involves bone resorption and bone synthesis. Under normal physiological conditions, bone resorption and bone formation are in balance, and many cytokines, hormones, and signaling pathways are involved [17] [Figure 1]. The bone remodeling process undergoes continuously during which osteoclasts absorb aged or damaged bones, whereas osteoblasts and osteocytes are responsible for new bone formation. However, if an imbalance arises, abnormalities in the bone structure or function may occur, resulting in osteometabolic disorders, such as osteopetrosis or osteoporosis [18]. Osteoblasts, osteocytes, and osteoclasts interplay with each other to maintain bone microstructure and homeostasis. Osteoblasts and osteocytes secrete receptor activator of NF-κB ligand (RANKL) and osteoprotegerin (OPG) to regulate osteoclasts proliferation and differentiation [16]. On the other way, the activated transforming growth factor-beta (TGF-β) and bone morphogenetic protein (BMP) released from the bone matrix after bone resorption also regulate osteoblasts formation [19,20]. Moreover, osteoblasts and osteocytes negatively feedback the differentiation of osteoblasts by inhibiting Wingless-related integration site (WNT) signaling through the secretion of WNT antagonists, Sclerostin (SOST), and Dickkopf 1 (DKK1) [21].
Figure 1.
Schematic representation of signaling pathways involved in bone remodeling and the formation of osteoblast and osteoclast. WNT, transforming growth factor-beta, bone morphogenetic protein, parathyroid hormone, and estrogen (e) are essential modulators of osteoblast and osteoclast formation. WNT and bone morphogenetic protein enhance the differentiation of osteoblasts. Bone morphogenetic protein, estrogen, and parathyroid hormone could indirectly regulate WNT activity by controlling the expression of Sost, and Dkk1 from osteoblasts and osteocytes. Transforming growth factor-beta enhances bone formation by suppressing the apoptosis of osteoblasts and osteocytes and enhancing the apoptosis of osteoclasts. Moreover, estrogen and WNT also suppress the apoptosis of osteoblasts and osteocytes. Blue lines indicate the effects of signaling molecules or the secreted proteins on the regulation of bone remodeling. Ligands are marked as yellow ovals. Signal modulators or the extracellular matrix proteins are marked as pink ovals. Endocrines are marked as green ovals
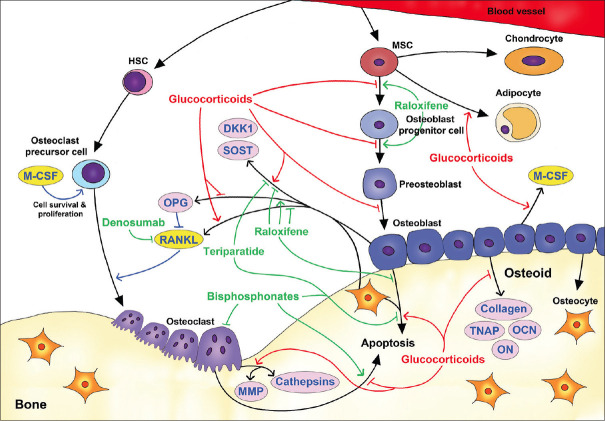
Endogenous glucocorticoid at physiologic concentrations is necessary for osteoblasts to maintain bone homeostasis [22,23]. The physiological activity of glucocorticoids is regulated by two enzymes, namely 11β-hydroxysteroid dehydrogenase type 1 (11β-HSD1) and type 2 (11β-HSD2), among which 11β-HSD1 activates glucocorticoid, whereas 11β-HSD2 inactivates glucocorticoid [24]. Studies using mouse models elucidate the significance of endogenous glucocorticoids in bone homeostasis. The decrease of glucocorticoid sensitivity in osteoblasts by transgenic expressing of glucocorticoid inactivating enzyme 11β-HSD2 causes a reduction of the bone mass [25,26]. Mice with conditional knockout of the glucocorticoid receptor in osteoblast lineage also reveal a significant reduction of vertebral bone density and osteoblast activity [27]. These results suggest that endogenous glucocorticoid is necessary for osteoblast activity and bone mineralization. In another way, human diseases causing an imbalance of endogenous glucocorticoid secretion also impair bone metabolism. Cushing's disease, causing an elevation of serum level of endogenous glucocorticoids, is correlated with osteoporosis [28,29,30]. Patients with Addison's disease who have a reduced serum level of endogenous glucocorticoids are also associated with a higher risk of hip fracture [31]. In conclusion, evidence from animal models and clinical observations suggests an essential role of endogenous glucocorticoid in maintaining bone remodeling. While the proper regulation of glucocorticoids' physiological concentration is essential for bone homeostasis, excessive glucocorticoids cause bone loss through the dysregulation of osteoblastogenesis and osteoclastogenesis [Figure 2].
Figure 2.
Schematic representation of the molecular etiology of glucocorticoid-induced osteoporosis and the effect of anti-osteoporotic drugs. Glucocorticoids (red) induce osteoporosis by inhibiting the differentiation of osteoblasts from mesenchymal stem cell, inducing apoptosis of osteoblasts and osteocytes, increasing the formation of osteoclasts, and prolonging the lifespan of osteoclasts. The effects of anti-osteoporotic drugs (green lines) such as bisphosphonates, teriparatide, denosumab, and raloxifene are indicated. Bisphosphonates inhibit the activity of osteoclast and induce its apoptosis. Bisphosphonates and the intermittent administration of teriparatide decrease the apoptosis of osteoblasts and osteocytes. Raloxifene, only used for postmenopausal women with glucocorticoid-induced osteoporosis, promotes bone formation by stimulating osteogenesis and suppressing osteoblast apoptosis and indirectly inhibits osteoclastogenesis by decreasing the expression of receptor activator of NF-κB ligand and increasing the expression of receptor activator of NF-κB ligand inhibitor osteoprotegerin. Denosumab inhibits osteoclastogenesis by neutralizing receptor activator of NF-κB ligand. Blue lines indicate the signaling affecting osteoclastogenesis
THE NEGATIVE IMPACT OF EXCESSIVE GLUCOCORTICOIDS ON OSTEOBLAST AND OSTEOCYTE
The therapeutic concentration of glucocorticoids reduces the formation and survival of osteoblast and osteocyte. Osteoblasts are differentiated from mesenchymal stem cells (MSCs) which travel through the blood vessel to reach the bone surface [32]. At the bone surface, the WNT signaling promotes the differentiation of MSC into osteoblast progenitor cell [33] and inhibits the differentiation of MSC into chondrocyte or adipocyte [34,35]. In the modulation of osteogenesis, glucocorticoids facilitate the differentiation of MSCs into adipocytes instead of osteoblast progenitor cells [36,37,38].
The differentiation of osteoblast progenitor cells into preosteoblasts and then osteoblasts requires the action of WNT and BMP signaling [39,40,41] by which activate the expression of Runt-related transcription factor 2 (Runx2) and Osterix (SP7) transcription factors [42,43]. Accordingly, excess glucocorticoids exposure suppresses WNT signaling by decreasing Wnt expression [44], bolstering the expression of WNT antagonists, such as Dkk1 [22,45,46,47], Sost [46,48], and Secreted frizzled-related protein-1 (sFRP-1) [22,49], and increasing the expression of negative WNT signaling regulator Axin-2 [49]. It is to be noted that the serum concentration of SOST is reduced in humans, which might reflect a compensatory mechanism that remains elucidated [50,51]. Glucocorticoids also suppress the BMP signaling by inhibiting BMP-2 expression [46,52] and enhancing the expression of BMP antagonists – Follistatin and Dan [49]. Besides, glucocorticoids suppress both the expression of Runx2 and RUNX2 activity and thus inhibit osteoblast maturation [53,54].
In addition to WNT and BMP, TGF-β is also involved in regulating osteoblast formation. TGF-β could promote the differentiation of osteoblast progenitor cells from MSCs [55] by enhancing the WNT signaling [56]. On the other hand, TGF-β inhibits osteoblasts and osteocytes' differentiation by decreasing the expression of Runx2 [57,58,59,60,61,62]. However, the essentiality of TGF-β in the regulation of osteoblastogenesis can be evident by the study showing that Tgfb1-null mice exhibit a significant loss of trabecular bone density and the reduction of osteoblasts [63]. Even limited literature addresses glucocorticoids' effect on TGF-β signaling; it has been reported that glucocorticoid treatment decreases the mRNA level of TGF-β [64].
Excess glucocorticoids also lead to apoptosis of osteoblasts and osteocytes. The undifferentiated osteoblast usually goes through apoptosis a few months after its formation. WNT [65], TGF-β [66,67], interleukin-6 (IL-6) [67], and estrogen [68,69,70] are reported to suppress the apoptosis of osteoblast. By contrast to osteoblasts' 3-month lifespan, osteocytes are long-lived bone cells that can survive for more than decades [71,72]. Osteocytes are mechanosensory cells that can sense the microdamage on the bone through their dendritic processes [73] and trigger their apoptosis [73,74,75]. While osteocytes undergo apoptosis, the neighboring nonapoptotic osteocytes attract osteoclast precursor cells to the microdamage site by releasing IL-6 and soluble IL-6 receptor [76] and secret RANKL to stimulate the osteoclastogenesis [77]. In the regulation of lifespan of cultured osteoblasts and osteocytes, excess glucocorticoids (≥10−6 M) induced apoptosis [78,79,80]. This observation is consistent with the in vivo experiment showing that excess glucocorticoids increase the apoptosis of osteoblasts and osteocytes [81]. Mechanistically, glucocorticoids could induce the apoptosis of osteoblasts by inhibiting the WNT, TGF-β, and IL-6 signaling [64,65,82].
THE EXCESSIVE GLUCOCORTICOIDS PROMOTE THE DIFFERENTIATION AND SURVIVAL OF OSTEOCLAST
The excessive amount of glucocorticoids promote the proliferation and survival of osteoclast precursor cells. Osteoclasts are originated from hematopoietic stem cells which differentiate into osteoclast precursor cells and then fuse to form multinucleated osteoclasts [83]. During osteoclastogenesis, both macrophage colony-stimulating factor (M-CSF) and RANKL play vital roles [84]. M-CSF is required for the cell survival and proliferation of osteoclast precursor cells, whereas RANK is required for the differentiation of osteoclast precursor cells [85,86,87]. When M-CSF binds to its receptor, colony-stimulating factor 1 receptor (c-Fms), on osteoclast precursor cells, the cell survival and proliferation of osteoclast precursor cells are promoted through the extracellular signal-regulated kinases and Serine/threonine kinase (Akt) signaling pathways [88]. Evidence has shown that glucocorticoids promote the proliferation and survival of osteoclast precursor cells by increasing the expression and half-life of M-CSF produced by osteoblast [89,90].
Glucocorticoids also promote osteoclast differentiation. RANKL secreted by both osteocytes and osteoblasts binds to the RANK receptor on osteoclast precursor cells and subsequently activates the mitogen-activated protein kinase, Akt, and nuclear factor of activated T-cells, cytoplasmic 1 signaling, which stimulate the differentiation and fusion of osteoclast precursor cells into multinuclear osteoclasts [91,92,93]. The activity of RANKL can be neutralized by its decoy receptor OPG secreted by both osteoblasts and osteocytes [94,95,96]. When Opg is expressed in large amounts, it hinders the formation of osteoclasts, resulting in osteopetrosis [94]; conversely, osteoporosis can be observed in Opg knockout mice [97,98]. Therefore, the ratio of RANKL/OPG is recognized as an indicator for the trend of osteoclast differentiation. For example, IL-6 enhances osteoclastogenesis by increasing the Rankl/Opg ratio [99]. Glucocorticoids promote the differentiation of osteoclast precursor cells toward osteoclast by enhancing the expression of Rankl from osteoclasts [100,101]. In the other way, glucocorticoids indirectly increase the RANKL activity by reducing the expression of its decoy receptor Opg. Glucocorticoids reduce the expression of Opg by directly regulating its expression in osteoblasts [100] or indirectly reduce the expression of Opg through the suppression of WNT signaling, which promotes the secretion of OPG from osteoblasts and osteocytes [102]. It has also been reported that glucocorticoids stimulate osteoclast formation through the activation of IL-6 signaling in osteoblasts [103], although the detailed mechanism is unclear.
The average lifespan of osteoclasts is around 2 weeks in humans [104]. Glucocorticoids act directly on osteoclasts to suppress their apoptosis and thus prolong the lifespan of osteoclasts [105,106]. On the other hand, glucocorticoids also suppress apoptosis of osteoclast precursor cells by decreasing the expression of Opg [107] and increasing the expression of Rankl [108]. Although glucocorticoids prolonged osteoclasts' lifespan, it was reported that glucocorticoids reduce osteoclast activity by disrupting M-CSF-stimulated cytoskeletal organization in vitro [109].
THE IMPACT OF THERAPEUTIC GLUCOCORTICOIDS ON BONE MATRIX
During the process of bone formation, osteoblasts secrete osteoid, the premineralized bone matrix, to prompt bone formation [110] and differentiate into osteocytes embedded in the bone matrix [111]. In osteoid, hydroxyapatite, a complex of calcium and phosphate, is formed within the matrix vesicles that bud from the plasma membrane of osteoblasts [112]. The hydroxyapatite further deposits into the extracellular matrix (ECM) of the bone and interacts with the main fibrous protein, type I Collagen, to form the mineralized collagen essential for maintaining the bone strength [113]. In GIOP patients, glucocorticoids lessen bone mineralization by inhibiting the expression of type I Collagen and increasing the expression of interstitial Collagenase [114,115,116].
Osteoblasts also secrete noncollagenous proteins, such as tissue nonspecific alkaline phosphatase (TNAP), osteocalcin (OCN), and osteonectin (ON)/secreted protein acidic and rich in cysteine [117]. These noncollagenous proteins play crucial roles in the bone matrix's mineralization and could be affected by glucocorticoids. TNAP is a membrane-bound enzyme that is localized on the plasma membrane of osteoblasts and the matrix vesicles [118,119]. TNAP can hydrolyze inorganic pyrophosphate (PPi) to phosphate (Pi) for the formation of hydroxyapatite [120]. OCN is a γ-carboxy glutamic acid-containing protein and has a dual function on bone development. In one way, OCN functions as an inhibitor of bone mineralization by binding to calcium, mediating its association with hydroxyapatite; in the other way, OCN and osteopontin enhance the mechanical properties of the bone [121]. Besides, exogenous supplementation of OCN enhances the differentiation of osteoblasts and increases extracellular calcium levels and TNAP activity [122]. As a calcium-binding matricellular protein, ON triggers the release of the calcium ion by binding to both collagen and hydroxyapatite [123], thereby promoting mineralization of the collagen matrix during bone formation. In addition, ON-null mice have fewer osteoblasts and osteoclasts, leading to a decrease in bone remodeling [124]. As for osteoclast, it also secrets proteolytic enzymes, such as matrix metalloproteinases (MMP) [125] and cathepsins [126,127], for the degradation of the matrix protein of the ECM during bone resorption. The treatment of glucocorticoids negatively impacts the mineralization of bone matrix by reducing the TNAP activity [128], expression of Ocn [129,130,131], and expression of On [132] in osteoblasts. Moreover, glucocorticoids increase the expression of Mmp9, Mmp13, and Cathepsin K by osteoclasts and thus promote the bone reabsorption [78,132,133].
FRACTURE RISK ASSESSMENT FOR GLUCOCORTICOID-INDUCED OSTEOPOROSIS
For adults ≥40 years of age using glucocorticoids chronically, the fracture risk can be assessed based on BMD and the fragility fracture history. As defined by the World Health Organization in 2008, a BMD T score of <-2.5 standard deviation is considered as osteoporosis. In addition to BMD, the 2017 American College Rheumatology Guideline for the Prevention and Treatment of GIOP recommends using Fracture Risk Assessment Tool (FRAX®, https://www.sheffield.ac.uk/FRAX/) for fracture risk assessment, which is a tool that integrates the information derived from both clinical risk factors and BMD. In the guideline, adults with low FRAX® fracture probability are recommended to take only calcium and Vitamin D, whereas adults with moderate-to-high FRAX® fracture probability (10-year probability of major osteoporotic fracture >10%) are suggested to be treated with additional anti-osteoporosis medication. However, the International Osteoporosis Foundation and the European Calcified Tissue Society suggested that an intervention threshold, instead of the categorization of FRAX® fracture probability, should be determined for clinical practice [134]. Besides, FRAX® fracture probability does not consider the dose of glucocorticoids; therefore, it needs to be adjusted according to the condition of glucocorticoid usage. For example, FRAX® calculations for the 10-year probability of major osteoporotic fracture and hip fracture should be uplifted by 15% and 20%, respectively, when patients take glucocorticoids at doses >7.5 mg/day [135]. In Taiwan, although there is no specific intervention threshold set for GIOP, the 2019 Taiwanese Consensus and Guidelines for the Prevention and Treatment of Adult Osteoporosis suggests using a presumed individual intervention threshold [136]. The presumed individual intervention threshold is defined as the 10-year probability of FRAX®-derived fracture risks for an individual who does not have rheumatoid arthritis, glucocorticoid usage, and other osteoporotic risk factors but has a previous fracture history [136,137]. By comparing it with the adjusted-FRAX® 10-year probability according to the glucocorticoid dosages, the timing of medical interventions could be determined. Besides, a novel hybrid intervention threshold was established to identify high-risk populations of fragility fractures in Taiwan by considering the FRAX®-derived fracture risks probability, BMD, and presumed individual intervention threshold [138]. However, the intervention threshold for GIOP could vary from country to country, depending on the health policy, economic status, and reimbursement issues.
It is to be noted that the FRAX® calculation is not applicable to determine the fracture risk probability for patients <40 years of age. Although young patients quickly regain bone mass when glucocorticoids are discontinued, the use of glucocorticoids at a dose of >7.5 mg/day for 6 months could still lead to a rapid decrease in bone density in hip or vertebrae (a decrease of >10% in one year) [139]. Therefore, both BMD and prior osteoporotic fracture history should be considered when physicians judge medical intervention for individuals <40 years of age.
TREATMENT OPTIONS FOR GLUCOCORTICOID-INDUCED OSTEOPOROSIS
Calcium and Vitamin D supplements
The evaluation indicators of drug therapy include the dosage and duration of glucocorticoid usage, fragility fracture history, BMD, age, and whether the patient is a postmenopausal woman [140]. In general, prophylaxis and treatment should be initiated in patients using glucocorticoids at a daily dose of 5–7.5 mg for >3 months [139]. Patients treated with glucocorticoids have faced systematic calcium loss caused by reduced gastrointestinal absorption and renal tubular reabsorption [141,142]. Therefore, it is suggested that adult patients should take adequate calcium (1000–1200 mg/day) and Vitamin D (600–800 IU/day) supplements to reduce calcium loss from bone and increase calcium absorption in the gastrointestinal tract [139]; for adults >50 years of age, a daily intake of 1200 mg calcium with 800–1000 IU Vitamin D is suggested [136].
Bisphosphonates
Bisphosphonates have a nonhydrolyzable P-C-P structure and are analogs of pyrophosphate. Structurally, the bisphosphonates with a nitrogen-containing side chain on the central carbon exhibit substantial therapeutic effects (e.g., alendronate, risedronate, and zoledronate). Bisphosphonates have a high affinity to hydroxyapatite, and thus they could accumulate on surfaces undergoing active resorption. Upon entry into osteoclasts through endocytosis, nitrogen-containing bisphosphonates inhibit the mevalonate pathway's farnesyl pyrophosphate synthase, thereby blocking protein prenylation, inhibiting the function of osteoclasts [143,144], and inducing osteoclast apoptosis [145,146]. Apart from the major therapeutic effect of bisphosphonates on inhibiting osteoclasts, bisphosphonates can also increase the lifespan of osteoblasts and osteocytes by inhibiting their apoptosis [147]. In the other way, bisphosphonates decrease the expression of the BMP antagonists Follistatin and Dan, the WNT signaling inhibitors sFRP-1 and axin-2 [49], thus facilitating WNT and BMP signaling and eventually increasing osteoblast formation.
Side effects of bisphosphonates may comprise erosive esophagitis, ulcer bleeding, hypocalcemia, renal function decline, osteonecrosis of the jaw, and atypical femoral fracture [148]. The failure of oral bisphosphonate treatment can be defined as GIOP patients who have new fractures after >18 months of oral bisphosphonates or experienced a significant decrease in BMD (>10% per year) after 1 year of treatment. In such a scenario, follow-up treatment with other osteoporotic drugs, such as denosumab or teriparatide, is suggested [139]. If the failure of oral bisphosphonate treatment is due to poor medical compliance or drug absorption issue caused by gastrointestinal side effects, intravenous bisphosphonates can be considered because of its long dosing interval and infrequent gastrointestinal side effects [149]. Accordingly, a decrease in BMD, new fractures, and other rare side effects, such as osteonecrosis of the jaw and atypical femoral fractures, should be carefully evaluated. For patients who stop using glucocorticoids and have a low risk of fracture, bisphosphonates can be discontinued; however, this is not recommended in patients who have discontinued glucocorticoids but remain at high risk of fracture [139]. It is to be noted that bisphosphonates have a relatively long half-life and tend to be trapped in bones, potentially affecting fetal bones; therefore, they are not recommended for pregnant women [150].
Therapeutic monoclonal antibody
Another commonly used drug in clinical practice is RANKL inhibitor (Denosumab). It is a human monoclonal antibody that binds and neutralizes RANKL, limiting the formation of osteoclasts, thereby inhibiting bone resorption [151]. The clinical trial indicates that GIOP patients take denosumab (60 mg subcutaneously once every six months) has a better therapeutic effect than those take risedronate (5 mg oral per day) in terms of BMD increases in spine and hip after one year of the treatment [152].The side effects for patients taking denosumab include hypocalcemia, osteonecrosis of the jaw, and a high risk of infection [153,154]. In addition, the incidence of vertebrae compression fracture also increases rapidly after discontinuation of denosumab [155]. Moreover, there may be a risk of fetal teratogenesis when used in pregnant women [156]. An advantage of denosumab is that no dose adjustment is necessary for patients with renal impairment; however, patients with creatinine clearance <30 mL/min or receiving dialysis are at risk for hypocalcemia. A clinical study has shown that denosumab therapy is well tolerated and improves BMD for patients with solid organ transplant, especially in those with renal function impairment or bisphosphonate intolerance [157]. However, a significant decrease of BMD at the lumbar spine and hip was reported when denosumab was discontinued in renal transplant recipients [158]. Therefore, if denosumab treatment is to be discontinued, an alternative anti-osteoporotic therapy should be considered.
Parathyroid hormone N-terminal active fragment
Teriparatide is an active form of parathyroid hormone (PTH) consisting of the N-terminal 34 amino acids. In the clinical survey, teriparatide significantly increases the expression of bone formation markers and bone mass density of GIOP patients [159,160,161]. Intermittent use of teriparatide facilitates osteoblast production, increases TNAP activity [162], and promotes WNT signaling by reducing WNT signaling inhibitors, such as Sost, Dkk1, sFRP-1, and axin-2 [49,163,164,165]. Intermittent administration of teriparatide also inhibits apoptosis of osteoblasts and osteocytes [166,167], thereby promoting bone formation and increasing bone mass. In addition, teriparatide and WNT can synergistically increase the nuclear translocation of β-catenin by PKA-mediated phosphorylation, thus facilitating WNT signaling [165]. In the absence of WNT binding, PTH-PTH1R complex can also bind to WNT coreceptor LRP6 and trigger WNT signaling in osteoblasts [168]. Teriparatide also decreases the expression of BMP antagonists Follistatin and Dan to facilitate BMP signaling [49]. Besides, PTH exerts an insulin-like growth factor I-mediated anabolic effect on bone formation [169,170].
However, long-term use of teriparatide may increase Rankl expression and inhibit Opg expression, causing osteoclast differentiation and increasing the number of osteoclasts, leading to bone resorption and bone loss [171,172]. Furthermore, bone loss and fractures may rapidly occur after teriparatide is discontinued [173]. Accordingly, after teriparatide discontinuation, other osteoporotic drugs should be used. After long-term use of teriparatide, the side effects include a possible cause of osteosarcoma, hypercalcemia, nausea, leg cramps, and dizziness [174].
Selective estrogen receptor modulator
The selective estrogen receptor modulator (SERM), such as raloxifene, lasofoxifene, and bazedoxifene, acts as a tissue-specific agonist and antagonist as it activates estrogen receptors in bone and inhibits estrogen receptors in the uterus and breast [175]. Estrogen facilitates the differentiation of MSCs into osteoblastic lineage [176]. Correspondingly, raloxifene stimulates Runx2 expression to promote the differentiation and proliferation of osteoblasts and suppresses the production of osteoclasts by inhibiting the expression of IL-6 [177]. Estrogen inhibits the expression of Sost by osteocytes and bolsters WNT signaling, leading to increased osteoblast formation [178,179]. Raloxifene also attenuates the expression of Sost and Dkk1 in mice [180]. In the other way, estrogen could suppress the differentiation of osteoclast precursor cells by decreasing Rankl expression and increasing Opg expression in osteoblasts and osteocytes [181,182]. Similarly, raloxifene increased the expression of Opg and decreased the expression of Rankl and IL-6 in human osteoblastic MG-63 cells [183]. However, different from the effect of estrogen on the regulation of apoptosis [38,69,184], clinical and cell culture studies indicate that raloxifene neither enhances the osteoclast apoptosis [185] nor suppress osteocyte apoptosis [186], except that raloxifene could protect osteoblast from apoptosis induced by sodium nitroprusside [187].
Clinical trials with postmenopausal osteoporotic women indicate that raloxifene [188], lasofoxifene [189], and bazedoxifene [190] are effective for reducing the incidence of vertebral fractures, but not nonvertebral fractures. Among SERMs for the osteoporosis treatment in postmenopausal women, raloxifene is the only SERM approved by the United States Food and Drug Administration (US FDA); the Taiwan FDA approves raloxifene and bazedoxifene. Although the US FDA does not approve the use of raloxifene for GIOP patients, the 2017 American College Rheumatology Guideline for the Prevention and Treatment of GIOP suggests that raloxifene could be used to treat postmenopausal women who have GIOP but fail to respond to regular GIOP treatment or have specific therapeutic contraindications [139]. It is to be noted that women receiving raloxifene might have an increased risk of venous thromboembolism [191].
TREATMENT OF GLUCOCORTICOID-INDUCED OSTEOPOROSIS IN PREGNANT WOMEN AND CHILDREN
Because of the lack of comprehensive medication safety assessments for osteoporotic drugs used in pregnant women, there is no treatment recommendation for pregnant GIOP patients. According to the 2017 American College Rheumatology guidelines, oral bisphosphonates are recommended only when female GIOP patients are not planning to become pregnant and have moderate to high risk of fracture; otherwise, only calcium tablets and vitamin D should be used. However, when the female GIOP patients experience side effects from oral bisphosphonates, teriparatide is recommended. Because of safety concerns, denosumab and intravenous injection of high-potency bisphosphonates are only applicable to the female GIOP patients having a high risk of fracture and avoiding pregnancy when other anti-osteoporotic drugs are not applicable [139].
Glucocorticoids are extensively used in children with various indications because of their significant anti-inflammatory and immunomodulatory activity. A study conducted in the United Kingdom found that 1.2% of children received at least one kind of oral glucocorticoid within a year to treat asthma attacks. Asthma is a chronic, obstructive, and inflammatory lung disease requiring long-term treatment with glucocorticoids adjusted according to each child's response to treatment [192]. Other chronic inflammatory diseases in children requiring long-term treatment with glucocorticoid for >3 months include juvenile idiopathic arthritis, systemic lupus erythematosus, juvenile dermatomyositis, Crohn's disease, and nephrotic syndrome. The glucocorticoids used to control these inflammatory diseases have an additive effect on reducing bone formation and severely compromising children's bone health [193].
An epidemiologic study conducted on the British population (including those aged 4–17 years) showed that oral glucocorticoids used for >4 cycles per year significantly increased fracture risk, with humerus fracture being the most common [194]. Therefore, the treatment of osteoporosis in children (between 4 and 17 years of age) who use glucocorticoids chronically requires a multifaceted approach: (1) Nutritional intake should be actively tracked to prevent obesity and ensure adequate intake of calcium (1000 mg/day), Vitamin D (at least 600 IU/day and exposure to sunlight for approximately 20 min/day), and protein. Furthermore, track the serum concentration of 1, 25-dihydroxyvitamin D every 3–6 months to determine whether the intake dose needs to be adjusted. (2) Regularly perform supervised physical exercises. In addition to controlling ideal body weight, it is also beneficial to maintaining bone and muscle strength. (3) For spontaneous fractures, especially vertebrae fractures (confirmed by pain or height loss), regular radiological examinations are required to rule out the possibility of occult fractures. For patients who have suffered GIOP fractures and continue to use glucocorticoids for >3 months (0.1 mg/kg/day), medical intervention is required [139].
CONCLUSION
GIOP is the most common type of secondary osteoporosis. It often occurs in patients who used glucocorticoids for a long time, such as those with autoimmune diseases, allergic diseases (e.g., asthma and atopic dermatitis), or organ transplantation. It is an iatrogenic disease in which osteogenesis and osteoclastogenesis are out of balance. Excess glucocorticoids cause rapid bone loss by downregulating bone formation and upregulating bone resorption during the 1st year of glucocorticoid treatment. In addition to direct effects on bone cells, such as osteoblasts, osteoclasts, and osteocytes, glucocorticoids also indirectly cause calcium loss, hypocalcemia, and secondary hyperparathyroidism. Therefore, the dosage and duration of treatment with glucocorticoids should be minimized. Moreover, nonpharmacological treatments, such as appropriate nutrition and exercise, should be combined with pharmacological treatments. For GIOP patients at high risk of fracture, medical intervention is recommended. In the future, more definitive safety studies have to be conducted for the medication of pregnant women and children with GIOP. Due to the limited choices and side effects of the drugs used for GIOP, it is eager to invent more effective and safer therapeutic drugs to meet the best interest of GIOP patients and society.
Financial support and sponsorship
This study was supported by grants from Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation (TCRD109-53) to C.H.P. and Tzu Chi University (610400239-11) to M.D.L.
Conflicts of interest
Dr. Ing-Ho Chen, an editorial board member at Tzu Chi Medical Journal, had no roles in the peer review process of or decision to publish this article. The other authors declared that they have no conflicts of interest.
REFERENCES
- 1.Wade SW, Strader C, Fitzpatrick LA, Anthony MS, O'Malley CD. Estimating prevalence of osteoporosis: Examples from industrialized countries. Arch Osteoporos. 2014;9:182. doi: 10.1007/s11657-014-0182-3. [DOI] [PubMed] [Google Scholar]
- 2.Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, et al. Osteoporosis in the European Union: Medical management, epidemiology and economic burden.A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA) Arch Osteoporos. 2013;8:136. doi: 10.1007/s11657-013-0136-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Odén A, McCloskey EV, Johansson H, Kanis JA. Assessing the impact of osteoporosis on the burden of hip fractures. Calcif Tissue Int. 2013;92:42–9. doi: 10.1007/s00223-012-9666-6. [DOI] [PubMed] [Google Scholar]
- 4.Watts NB GLOW investigators. Insights from the Global Longitudinal Study of Osteoporosis in Women (GLOW) Nat Rev Endocrinol. 2014;10:412–22. doi: 10.1038/nrendo.2014.55. [DOI] [PubMed] [Google Scholar]
- 5.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17:1726–33. doi: 10.1007/s00198-006-0172-4. [DOI] [PubMed] [Google Scholar]
- 6.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465–75. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 7.Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573–9. doi: 10.1001/jama.2009.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Svedbom A, Hernlund E, Ivergård M, Compston J, Cooper C, Stenmark J, et al. Osteoporosis in the European Union: A compendium of country-specific reports. Arch Osteoporos. 2013;8:137. doi: 10.1007/s11657-013-0137-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Melton LJ., 3rd How many women have osteoporosis now? J Bone Miner Res. 1995;10:175–7. doi: 10.1002/jbmr.5650100202. [DOI] [PubMed] [Google Scholar]
- 10.Vestergaard P, Rejnmark L, Mosekilde L. Osteoporosis is markedly underdiagnosed: A nationwide study from Denmark. Osteoporos Int. 2005;16:134–41. doi: 10.1007/s00198-004-1680-8. [DOI] [PubMed] [Google Scholar]
- 11.Weitzmann MN, Pacifici R. Estrogen deficiency and bone loss: An inflammatory tale. J Clin Invest. 2006;116:1186–94. doi: 10.1172/JCI28550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Veldurthy V, Wei R, Oz L, Dhawan P, Jeon YH, Christakos S. Vitamin D, calcium homeostasis and aging. Bone Res. 2016;4:16041. doi: 10.1038/boneres.2016.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walker-Bone K. Recognizing and treating secondary osteoporosis. Nat Rev Rheumatol. 2012;8:480–92. doi: 10.1038/nrrheum.2012.93. [DOI] [PubMed] [Google Scholar]
- 14.Compston J. Glucocorticoid-induced osteoporosis: An update. Endocrine. 2018;61:7–16. doi: 10.1007/s12020-018-1588-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Overman RA, Toliver JC, Yeh JY, Gourlay ML, Deal CL. United States adults meeting 2010 American College of Rheumatology criteria for treatment and prevention of glucocorticoid-induced osteoporosis. Arthritis Care Res (Hoboken) 2014;66:1644–52. doi: 10.1002/acr.22346. [DOI] [PubMed] [Google Scholar]
- 16.Chotiyarnwong P, McCloskey EV. Pathogenesis of glucocorticoid-induced osteoporosis and options for treatment. Nat Rev Endocrinol. 2020;16:437–47. doi: 10.1038/s41574-020-0341-0. [DOI] [PubMed] [Google Scholar]
- 17.Matsuo K, Irie N. Osteoclast-osteoblast communication. Arch Biochem Biophys. 2008;473:201–9. doi: 10.1016/j.abb.2008.03.027. [DOI] [PubMed] [Google Scholar]
- 18.Zaidi M. Skeletal remodeling in health and disease. Nat Med. 2007;13:791–801. doi: 10.1038/nm1593. [DOI] [PubMed] [Google Scholar]
- 19.Oreffo RO, Mundy GR, Seyedin SM, Bonewald LF. Activation of the bone-derived latent TGF beta complex by isolated osteoclasts. Biochem Biophys Res Commun. 1989;158:817–23. doi: 10.1016/0006-291x(89)92795-2. [DOI] [PubMed] [Google Scholar]
- 20.Huntley R, Jensen E, Gopalakrishnan R, Mansky KC. Bone morphogenetic proteins: Their role in regulating osteoclast differentiation. Bone Rep. 2019;10:100207. doi: 10.1016/j.bonr.2019.100207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ramli FF, Chin KY. A review of the potential application of osteocyte-related biomarkers, fibroblast growth factor-23, sclerostin, and dickkopf-1 in predicting osteoporosis and fractures. Diagnostics (Basel) 2020;10:145. doi: 10.3390/diagnostics10030145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mak W, Shao X, Dunstan CR, Seibel MJ, Zhou H. Biphasic glucocorticoid-dependent regulation of Wnt expression and its inhibitors in mature osteoblastic cells. Calcif Tissue Int. 2009;85:538–45. doi: 10.1007/s00223-009-9303-1. [DOI] [PubMed] [Google Scholar]
- 23.Kalak R, Zhou H, Street J, Day RE, Modzelewski JR, Spies CM, et al. Endogenous glucocorticoid signalling in osteoblasts is necessary to maintain normal bone structure in mice. Bone. 2009;45:61–7. doi: 10.1016/j.bone.2009.03.673. [DOI] [PubMed] [Google Scholar]
- 24.Weinstein RS. Glucocorticoids, osteocytes, and skeletal fragility: The role of bone vascularity. Bone. 2010;46:564–70. doi: 10.1016/j.bone.2009.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang M, Trettel LB, Adams DJ, Harrison JR, Canalis E, Kream BE. Col3.6-HSD2 transgenic mice: A glucocorticoid loss-of-function model spanning early and late osteoblast differentiation. Bone. 2010;47:573–82. doi: 10.1016/j.bone.2010.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sher LB, Woitge HW, Adams DJ, Gronowicz GA, Krozowski Z, Harrison JR, et al. Transgenic expression of 11beta-hydroxysteroid dehydrogenase type 2 in osteoblasts reveals an anabolic role for endogenous glucocorticoids in bone. Endocrinology. 2004;145:922–9. doi: 10.1210/en.2003-0655. [DOI] [PubMed] [Google Scholar]
- 27.Rauch A, Seitz S, Baschant U, Schilling AF, Illing A, Stride B, et al. Glucocorticoids suppress bone formation by attenuating osteoblast differentiation via the monomeric glucocorticoid receptor. Cell Metab. 2010;11:517–31. doi: 10.1016/j.cmet.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 28.Kaltsas G, Makras P. Skeletal diseases in Cushing's syndrome: Osteoporosis versus arthropathy. Neuroendocrinology. 2010;92(Suppl 1):60–4. doi: 10.1159/000314298. [DOI] [PubMed] [Google Scholar]
- 29.Lonser RR, Nieman L, Oldfield EH. Cushing's disease: Pathobiology, diagnosis, and management. J Neurosurg. 2017;126:404–17. doi: 10.3171/2016.1.JNS152119. [DOI] [PubMed] [Google Scholar]
- 30.Belaya ZE, Grebennikova TA, Melnichenko GA, Nikitin AG, Solodovnikov AG, Brovkina OI, et al. Effects of endogenous hypercortisolism on bone mRNA and microRNA expression in humans. Osteoporos Int. 2018;29:211–21. doi: 10.1007/s00198-017-4241-7. [DOI] [PubMed] [Google Scholar]
- 31.Björnsdottir S, Sääf M, Bensing S, Kämpe O, Michaëlsson K, Ludvigsson JF. Risk of hip fracture in Addison's disease: A population-based cohort study. J Intern Med. 2011;270:187–95. doi: 10.1111/j.1365-2796.2011.02352.x. [DOI] [PubMed] [Google Scholar]
- 32.Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, et al. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284:143–7. doi: 10.1126/science.284.5411.143. [DOI] [PubMed] [Google Scholar]
- 33.Hu H, Hilton MJ, Tu X, Yu K, Ornitz DM, Long F. Sequential roles of hedgehog and Wnt signaling in osteoblast development. Development. 2005;132:49–60. doi: 10.1242/dev.01564. [DOI] [PubMed] [Google Scholar]
- 34.Hill TP, Später D, Taketo MM, Birchmeier W, Hartmann C. Canonical Wnt/beta-catenin signaling prevents osteoblasts from differentiating into chondrocytes. Dev Cell. 2005;8:727–38. doi: 10.1016/j.devcel.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 35.Kennell JA, MacDougald OA. Wnt signaling inhibits adipogenesis through beta-catenin-dependent and -independent mechanisms. J Biol Chem. 2005;280:24004–10. doi: 10.1074/jbc.M501080200. [DOI] [PubMed] [Google Scholar]
- 36.Lecka-Czernik B, Gubrij I, Moerman EJ, Kajkenova O, Lipschitz DA, Manolagas SC, et al. Inhibition of Osf2/Cbfa1 expression and terminal osteoblast differentiation by PPARgamma2. J Cell Biochem. 1999;74:357–71. [PubMed] [Google Scholar]
- 37.Wu Z, Bucher NL, Farmer SR. Induction of peroxisome proliferator-activated receptor gamma during the conversion of 3T3 fibroblasts into adipocytes is mediated by C/EBPbeta, C/EBPdelta, and glucocorticoids. Mol Cell Biol. 1996;16:4128–36. doi: 10.1128/mcb.16.8.4128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yang YJ, Zhu Z, Wang DT, Zhang XL, Liu YY, Lai WX, et al. Tanshinol alleviates impaired bone formation by inhibiting adipogenesis via KLF15/PPARγ2 signaling in GIO rats. Acta Pharmacol Sin. 2018;39:633–41. doi: 10.1038/aps.2017.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang M, Yan Y, Lim YB, Tang D, Xie R, Chen A, et al. BMP-2 modulates beta-catenin signaling through stimulation of Lrp5 expression and inhibition of beta-TrCP expression in osteoblasts. J Cell Biochem. 2009;108:896–905. doi: 10.1002/jcb.22319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rawadi G, Vayssière B, Dunn F, Baron R, Roman-Roman S. BMP-2 controls alkaline phosphatase expression and osteoblast mineralization by a Wnt autocrine loop. J Bone Miner Res. 2003;18:1842–53. doi: 10.1359/jbmr.2003.18.10.1842. [DOI] [PubMed] [Google Scholar]
- 41.Zhang R, Oyajobi BO, Harris SE, Chen D, Tsao C, Deng HW, et al. Wnt/β-catenin signaling activates bone morphogenetic protein 2 expression in osteoblasts. Bone. 2013;52:145–56. doi: 10.1016/j.bone.2012.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gu K, Zhang L, Jin T, Rutherford RB. Identification of potential modifiers of Runx2/Cbfa1 activity in C2C12 cells in response to bone morphogenetic protein-7. Cells Tissues Organs. 2004;176:28–40. doi: 10.1159/000075025. [DOI] [PubMed] [Google Scholar]
- 43.Shen B, Wei A, Whittaker S, Williams LA, Tao H, Ma DD, et al. The role of BMP-7 in chondrogenic and osteogenic differentiation of human bone marrow multipotent mesenchymal stromal cells in vitro. J Cell Biochem. 2010;109:406–16. doi: 10.1002/jcb.22412. [DOI] [PubMed] [Google Scholar]
- 44.Hildebrandt S, Baschant U, Thiele S, Tuckermann J, Hofbauer LC, Rauner M. Glucocorticoids suppress Wnt16 expression in osteoblasts in vitro and in vivo. Sci Rep. 2018;8:8711. doi: 10.1038/s41598-018-26300-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ohnaka K, Taniguchi H, Kawate H, Nawata H, Takayanagi R. Glucocorticoid enhances the expression of dickkopf-1 in human osteoblasts: Novel mechanism of glucocorticoid-induced osteoporosis. Biochem Biophys Res Commun. 2004;318:259–64. doi: 10.1016/j.bbrc.2004.04.025. [DOI] [PubMed] [Google Scholar]
- 46.Yao W, Cheng Z, Busse C, Pham A, Nakamura MC, Lane NE. Glucocorticoid excess in mice results in early activation of osteoclastogenesis and adipogenesis and prolonged suppression of osteogenesis: A longitudinal study of gene expression in bone tissue from glucocorticoid-treated mice. Arthritis Rheum. 2008;58:1674–86. doi: 10.1002/art.23454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhou M, Wu J, Yu Y, Yang Y, Li J, Cui L, et al. Polygonum multiflorm alleviates glucocorticoid-induced osteoporosis and Wnt signaling pathway. Mol Med Rep. 2018;17:970–8. doi: 10.3892/mmr.2017.7997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kawano Y, Kypta R. Secreted antagonists of the Wnt signalling pathway. J Cell Sci. 2003;116:2627–34. doi: 10.1242/jcs.00623. [DOI] [PubMed] [Google Scholar]
- 49.Hayashi K, Yamaguchi T, Yano S, Kanazawa I, Yamauchi M, Yamamoto M, et al. BMP/Wnt antagonists are upregulated by dexamethasone in osteoblasts and reversed by alendronate and PTH: Potential therapeutic targets for glucocorticoid-induced osteoporosis. Biochem Biophys Res Commun. 2009;379:261–6. doi: 10.1016/j.bbrc.2008.12.035. [DOI] [PubMed] [Google Scholar]
- 50.Thiele S, Hannemann A, Winzer M, Baschant U, Weidner H, Nauck M, et al. Regulation of sclerostin in glucocorticoid-induced osteoporosis (GIO) in mice and humans. Endocr Connect. 2019;8:923–34. doi: 10.1530/EC-19-0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jacobsson M, van Raalte DH, Heijboer AC, den Heijer M, de Jongh RT. Short-term glucocorticoid treatment reduces circulating sclerostin concentrations in healthy young Men: A randomized, placebo-controlled, double-blind study. JBMR Plus. 2020;4:e10341. doi: 10.1002/jbm4.10341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Luppen CA, Chandler RL, Noh T, Mortlock DP, Frenkel B. BMP-2 vs.BMP-4 expression and activity in glucocorticoid-arrested MC3T3-E1 osteoblasts: Smad signaling, not alkaline phosphatase activity, predicts rescue of mineralization. Growth Factors. 2008;26:226–37. doi: 10.1080/08977190802277880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pereira RC, Delany AM, Canalis E. Effects of cortisol and bone morphogenetic protein-2 on stromal cell differentiation: Correlation with CCAAT-enhancer binding protein expression. Bone. 2002;30:685–91. doi: 10.1016/s8756-3282(02)00687-7. [DOI] [PubMed] [Google Scholar]
- 54.Koromila T, Baniwal SK, Song YS, Martin A, Xiong J, Frenkel B. Glucocorticoids antagonize RUNX2 during osteoblast differentiation in cultures of ST2 pluripotent mesenchymal cells. J Cell Biochem. 2014;115:27–33. doi: 10.1002/jcb.24646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lee KS, Hong SH, Bae SC. Both the Smad and p38 MAPK pathways play a crucial role in Runx2 expression following induction by transforming growth factor-beta and bone morphogenetic protein. Oncogene. 2002;21:7156–63. doi: 10.1038/sj.onc.1205937. [DOI] [PubMed] [Google Scholar]
- 56.Zhou S, Eid K, Glowacki J. Cooperation between TGF-beta and Wnt pathways during chondrocyte and adipocyte differentiation of human marrow stromal cells. J Bone Miner Res. 2004;19:463–70. doi: 10.1359/JBMR.0301239. [DOI] [PubMed] [Google Scholar]
- 57.Li J, Tsuji K, Komori T, Miyazono K, Wrana JL, Ito Y, et al. Smad2 overexpression enhances Smad4 gene expression and suppresses CBFA1 gene expression in osteoblastic osteosarcoma ROS17/2.8 cells and primary rat calvaria cells. J Biol Chem. 1998;273:31009–15. doi: 10.1074/jbc.273.47.31009. [DOI] [PubMed] [Google Scholar]
- 58.Alliston T, Choy L, Ducy P, Karsenty G, Derynck R. TGF-beta-induced repression of CBFA1 by Smad3 decreases cbfa1 and osteocalcin expression and inhibits osteoblast differentiation. EMBO J. 2001;20:2254–72. doi: 10.1093/emboj/20.9.2254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kang JS, Alliston T, Delston R, Derynck R. Repression of Runx2 function by TGF-beta through recruitment of class II histone deacetylases by Smad3. EMBO J. 2005;24:2543–55. doi: 10.1038/sj.emboj.7600729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hjelmeland AB, Schilling SH, Guo X, Quarles D, Wang XF. Loss of Smad3-mediated negative regulation of Runx2 activity leads to an alteration in cell fate determination. Mol Cell Biol. 2005;25:9460–8. doi: 10.1128/MCB.25.21.9460-9468.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Breen EC, Ignotz RA, McCabe L, Stein JL, Stein GS, Lian JB. TGF beta alters growth and differentiation related gene expression in proliferating osteoblasts in vitro, preventing development of the mature bone phenotype. J Cell Physiol. 1994;160:323–35. doi: 10.1002/jcp.1041600214. [DOI] [PubMed] [Google Scholar]
- 62.Borton AJ, Frederick JP, Datto MB, Wang XF, Weinstein RS. The loss of Smad3 results in a lower rate of bone formation and osteopenia through dysregulation of osteoblast differentiation and apoptosis. J Bone Miner Res. 2001;16:1754–64. doi: 10.1359/jbmr.2001.16.10.1754. [DOI] [PubMed] [Google Scholar]
- 63.Tang Y, Wu X, Lei W, Pang L, Wan C, Shi Z, et al. TGF-beta1-induced migration of bone mesenchymal stem cells couples bone resorption with formation. Nat Med. 2009;15:757–65. doi: 10.1038/nm.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Li Y, Jie L, Tian AY, Zhong S, Tian MY, Zhong Y, et al. Transforming Growth Factor Beta is regulated by a Glucocorticoid-Dependent Mechanism in Denervation Mouse Bone. Sci Rep. 2017;7:9925. doi: 10.1038/s41598-017-09793-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Almeida M, Han L, Bellido T, Manolagas SC, Kousteni S. Wnt proteins prevent apoptosis of both uncommitted osteoblast progenitors and differentiated osteoblasts by beta-catenin-dependent and -independent signaling cascades involving Src/ERK and phosphatidylinositol 3-kinase/AKT. J Biol Chem. 2005;280:41342–51. doi: 10.1074/jbc.M502168200. [DOI] [PubMed] [Google Scholar]
- 66.Karsdal MA, Larsen L, Engsig MT, Lou H, Ferreras M, Lochter A, et al. Matrix metalloproteinase-dependent activation of latent transforming growth factor-beta controls the conversion of osteoblasts into osteocytes by blocking osteoblast apoptosis. J Biol Chem. 2002;277:44061–7. doi: 10.1074/jbc.M207205200. [DOI] [PubMed] [Google Scholar]
- 67.Jilka RL, Weinstein RS, Bellido T, Parfitt AM, Manolagas SC. Osteoblast programmed cell death (apoptosis): Modulation by growth factors and cytokines. J Bone Miner Res. 1998;13:793–802. doi: 10.1359/jbmr.1998.13.5.793. [DOI] [PubMed] [Google Scholar]
- 68.Tomkinson A, Gevers EF, Wit JM, Reeve J, Noble BS. The role of estrogen in the control of rat osteocyte apoptosis. J Bone Miner Res. 1998;13:1243–50. doi: 10.1359/jbmr.1998.13.8.1243. [DOI] [PubMed] [Google Scholar]
- 69.Bradford PG, Gerace KV, Roland RL, Chrzan BG. Estrogen regulation of apoptosis in osteoblasts. Physiol Behav. 2010;99:181–5. doi: 10.1016/j.physbeh.2009.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gavali S, Gupta MK, Daswani B, Wani MR, Sirdeshmukh R, Khatkhatay MI. Estrogen enhances human osteoblast survival and function via promotion of autophagy. Biochim Biophys Acta Mol Cell Res. 2019;1866:1498–507. doi: 10.1016/j.bbamcr.2019.06.014. [DOI] [PubMed] [Google Scholar]
- 71.Manolagas SC. Birth and death of bone cells: Basic regulatory mechanisms and implications for the pathogenesis and treatment of osteoporosis. Endocr Rev. 2000;21:115–37. doi: 10.1210/edrv.21.2.0395. [DOI] [PubMed] [Google Scholar]
- 72.Bonewald LF. The amazing osteocyte. J Bone Miner Res. 2011;26:229–38. doi: 10.1002/jbmr.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tresguerres FG, Torres J, López-Quiles J, Hernández G, Vega JA, Tresguerres IF. The osteocyte: A multifunctional cell within the bone. Ann Anat. 2020;227:151422. doi: 10.1016/j.aanat.2019.151422. [DOI] [PubMed] [Google Scholar]
- 74.Noble BS, Stevens H, Loveridge N, Reeve J. Identification of apoptotic changes in osteocytes in normal and pathological human bone. Bone. 1997;20:273–82. doi: 10.1016/s8756-3282(96)00365-1. [DOI] [PubMed] [Google Scholar]
- 75.Verborgt O, Gibson GJ, Schaffler MB. Loss of osteocyte integrity in association with microdamage and bone remodeling after fatigue in vivo. J Bone Miner Res. 2000;15:60–7. doi: 10.1359/jbmr.2000.15.1.60. [DOI] [PubMed] [Google Scholar]
- 76.Cheung WY, Simmons CA, You L. Osteocyte apoptosis regulates osteoclast precursor adhesion via osteocytic IL-6 secretion and endothelial ICAM-1 expression. Bone. 2012;50:104–10. doi: 10.1016/j.bone.2011.09.052. [DOI] [PubMed] [Google Scholar]
- 77.Kennedy OD, Herman BC, Laudier DM, Majeska RJ, Sun HB, Schaffler MB. Activation of resorption in fatigue-loaded bone involves both apoptosis and active pro-osteoclastogenic signaling by distinct osteocyte populations. Bone. 2012;50:1115–22. doi: 10.1016/j.bone.2012.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Jia J, Yao W, Guan M, Dai W, Shahnazari M, Kar R, et al. Glucocorticoid dose determines osteocyte cell fate. FASEB J. 2011;25:3366–76. doi: 10.1096/fj.11-182519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Li H, Qian W, Weng X, Wu Z, Li H, Zhuang Q, et al. Glucocorticoid receptor and sequential P53 activation by dexamethasone mediates apoptosis and cell cycle arrest of osteoblastic MC3T3-E1 cells. PLoS One. 2012;7:e37030. doi: 10.1371/journal.pone.0037030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhang S, Liu Y, Liang Q. Low-dose dexamethasone affects osteoblast viability by inducing autophagy via intracellular ROS. Mol Med Rep. 2018;17:4307–16. doi: 10.3892/mmr.2018.8461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.O'Brien CA, Jia D, Plotkin LI, Bellido T, Powers CC, Stewart SA, et al. Glucocorticoids act directly on osteoblasts and osteocytes to induce their apoptosis and reduce bone formation and strength. Endocrinology. 2004;145:1835–41. doi: 10.1210/en.2003-0990. [DOI] [PubMed] [Google Scholar]
- 82.Swolin-Eide D, Ohlsson C. Effects of cortisol on the expression of interleukin-6 and interleukin-1 beta in human osteoblast-like cells. J Endocrinol. 1998;156:107–14. doi: 10.1677/joe.0.1560107. [DOI] [PubMed] [Google Scholar]
- 83.Rodan GA, Martin TJ. Therapeutic approaches to bone diseases. Science. 2000;289:1508–14. doi: 10.1126/science.289.5484.1508. [DOI] [PubMed] [Google Scholar]
- 84.Boyce BF. Advances in the regulation of osteoclasts and osteoclast functions. J Dent Res. 2013;92:860–7. doi: 10.1177/0022034513500306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kim JH, Kim N. Signaling Pathways in Osteoclast Differentiation. Chonnam Med J. 2016;52:12–7. doi: 10.4068/cmj.2016.52.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Fata JE, Kong YY, Li J, Sasaki T, Irie-Sasaki J, Moorehead RA, et al. The osteoclast differentiation factor osteoprotegerin-ligand is essential for mammary gland development. Cell. 2000;103:41–50. doi: 10.1016/s0092-8674(00)00103-3. [DOI] [PubMed] [Google Scholar]
- 87.Asagiri M, Sato K, Usami T, Ochi S, Nishina H, Yoshida H, et al. Autoamplification of NFATc1 expression determines its essential role in bone homeostasis. J Exp Med. 2005;202:1261–9. doi: 10.1084/jem.20051150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lee AW, States DJ. Both src-dependent and -independent mechanisms mediate phosphatidylinositol 3-kinase regulation of colony-stimulating factor 1-activated mitogen-activated protein kinases in myeloid progenitors. Mol Cell Biol. 2000;20:6779–98. doi: 10.1128/mcb.20.18.6779-6798.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Rubin J, Biskobing DM, Jadhav L, Fan D, Nanes MS, Perkins S, et al. Dexamethasone promotes expression of membrane-bound macrophage colony-stimulating factor in murine osteoblast-like cells. Endocrinology. 1998;139:1006–12. doi: 10.1210/endo.139.3.5778. [DOI] [PubMed] [Google Scholar]
- 90.Glantschnig H, Fisher JE, Wesolowski G, Rodan GA, Reszka AA. M-CSF, TNFalpha and RANK ligand promote osteoclast survival by signaling through mTOR/S6 kinase. Cell Death Differ. 2003;10:1165–77. doi: 10.1038/sj.cdd.4401285. [DOI] [PubMed] [Google Scholar]
- 91.Nakashima T, Hayashi M, Fukunaga T, Kurata K, Oh-Hora M, Feng JQ, et al. Evidence for osteocyte regulation of bone homeostasis through RANKL expression. Nat Med. 2011;17:1231–4. doi: 10.1038/nm.2452. [DOI] [PubMed] [Google Scholar]
- 92.Suda T, Takahashi N, Udagawa N, Jimi E, Gillespie MT, Martin TJ. Modulation of osteoclast differentiation and function by the new members of the tumor necrosis factor receptor and ligand families. Endocr Rev. 1999;20:345–57. doi: 10.1210/edrv.20.3.0367. [DOI] [PubMed] [Google Scholar]
- 93.Xiong J, Onal M, Jilka RL, Weinstein RS, Manolagas SC, O'Brien CA. Matrix-embedded cells control osteoclast formation. Nat Med. 2011;17:1235–41. doi: 10.1038/nm.2448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Simonet WS, Lacey DL, Dunstan CR, Kelley M, Chang MS, Lüthy R, et al. Osteoprotegerin: A novel secreted protein involved in the regulation of bone density. Cell. 1997;89:309–19. doi: 10.1016/s0092-8674(00)80209-3. [DOI] [PubMed] [Google Scholar]
- 95.Fei Q, Guo C, Xu X, Gao J, Zhang J, Chen T, et al. Osteogenic growth peptide enhances the proliferation of bone marrow mesenchymal stem cells from osteoprotegerin-deficient mice by CDK2/cyclin A. Acta Biochim Biophys Sin (Shanghai) 2010;42:801–6. doi: 10.1093/abbs/gmq086. [DOI] [PubMed] [Google Scholar]
- 96.Boyle WJ, Simonet WS, Lacey DL. Osteoclast differentiation and activation. Nature. 2003;423:337–42. doi: 10.1038/nature01658. [DOI] [PubMed] [Google Scholar]
- 97.Wagner EF, Karsenty G. Genetic control of skeletal development. Curr Opin Genet Dev. 2001;11:527–32. doi: 10.1016/s0959-437x(00)00228-8. [DOI] [PubMed] [Google Scholar]
- 98.Bucay N, Sarosi I, Dunstan CR, Morony S, Tarpley J, Capparelli C, et al. osteoprotegerin-deficient mice develop early onset osteoporosis and arterial calcification. Genes Dev. 1998;12:1260–8. doi: 10.1101/gad.12.9.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Palmqvist P, Persson E, Conaway HH, Lerner UH. IL-6, leukemia inhibitory factor, and oncostatin M stimulate bone resorption and regulate the expression of receptor activator of NF-kappa B ligand, osteoprotegerin, and receptor activator of NF-kappa B in mouse calvariae. J Immunol. 2002;169:3353–62. doi: 10.4049/jimmunol.169.6.3353. [DOI] [PubMed] [Google Scholar]
- 100.Hofbauer LC, Gori F, Riggs BL, Lacey DL, Dunstan CR, Spelsberg TC, et al. Stimulation of osteoprotegerin ligand and inhibition of osteoprotegerin production by glucocorticoids in human osteoblastic lineage cells: Potential paracrine mechanisms of glucocorticoid-induced osteoporosis. Endocrinology. 1999;140:4382–9. doi: 10.1210/endo.140.10.7034. [DOI] [PubMed] [Google Scholar]
- 101.Sivagurunathan S, Muir MM, Brennan TC, Seale JP, Mason RS. Influence of glucocorticoids on human osteoclast generation and activity. J Bone Miner Res. 2005;20:390–8. doi: 10.1359/JBMR.041233. [DOI] [PubMed] [Google Scholar]
- 102.Glass DA, 2nd, Bialek P, Ahn JD, Starbuck M, Patel MS, Clevers H, et al. Canonical Wnt signaling in differentiated osteoblasts controls osteoclast differentiation. Dev Cell. 2005;8:751–64. doi: 10.1016/j.devcel.2005.02.017. [DOI] [PubMed] [Google Scholar]
- 103.Udagawa N, Takahashi N, Katagiri T, Tamura T, Wada S, Findlay DM, et al. Interleukin (IL)-6 induction of osteoclast differentiation depends on IL-6 receptors expressed on osteoblastic cells but not on osteoclast progenitors. J Exp Med. 1995;182:1461–8. doi: 10.1084/jem.182.5.1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Baserga R. The Biology of Cell Reproduction. Cambridge, Mass: Harvard University Press; 1985. [Google Scholar]
- 105.Jia D, O'Brien CA, Stewart SA, Manolagas SC, Weinstein RS. Glucocorticoids act directly on osteoclasts to increase their life span and reduce bone density. Endocrinology. 2006;147:5592–9. doi: 10.1210/en.2006-0459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Weinstein RS, Chen JR, Powers CC, Stewart SA, Landes RD, Bellido T, et al. Promotion of osteoclast survival and antagonism of bisphosphonate-induced osteoclast apoptosis by glucocorticoids. J Clin Invest. 2002;109:1041–8. doi: 10.1172/JCI14538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Liu W, Xu C, Zhao H, Xia P, Song R, Gu J, et al. Osteoprotegerin Induces Apoptosis of Osteoclasts and Osteoclast Precursor Cells via the Fas/Fas Ligand Pathway. PLoS One. 2015;10:e0142519. doi: 10.1371/journal.pone.0142519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wu X, Pan G, McKenna MA, Zayzafoon M, Xiong WC, McDonald JM. RANKL regulates Fas expression and Fas-mediated apoptosis in osteoclasts. J Bone Miner Res. 2005;20:107–16. doi: 10.1359/JBMR.041022. [DOI] [PubMed] [Google Scholar]
- 109.Kim HJ, Zhao H, Kitaura H, Bhattacharyya S, Brewer JA, Muglia LJ, et al. Glucocorticoids suppress bone formation via the osteoclast. J Clin Invest. 2006;116:2152–60. doi: 10.1172/JCI28084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Florencio-Silva R, Sasso GR, Sasso-Cerri E, Simões MJ, Cerri PS. Biology of Bone Tissue: Structure, Function, and Factors That Influence Bone Cells. Biomed Res Int. 2015;2015:421746. doi: 10.1155/2015/421746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Baron R, Kneissel M. WNT signaling in bone homeostasis and disease: From human mutations to treatments. Nat Med. 2013;19:179–92. doi: 10.1038/nm.3074. [DOI] [PubMed] [Google Scholar]
- 112.Hasegawa T, Yamamoto T, Tsuchiya E, Hongo H, Tsuboi K, Kudo A, et al. Ultrastructural and biochemical aspects of matrix vesicle-mediated mineralization. Jpn Dent Sci Rev. 2017;53:34–45. doi: 10.1016/j.jdsr.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Weiner S, Traub W. Organization of hydroxyapatite crystals within collagen fibrils. FEBS Lett. 1986;206:262–6. doi: 10.1016/0014-5793(86)80993-0. [DOI] [PubMed] [Google Scholar]
- 114.Canalis E. Mechanisms of glucocorticoid action in bone. Curr Osteoporos Rep. 2005;3:98–102. doi: 10.1007/s11914-005-0017-7. [DOI] [PubMed] [Google Scholar]
- 115.Delany AM, Gabbitas BY, Canalis E. Cortisol downregulates osteoblast alpha 1 (I) procollagen mRNA by transcriptional and posttranscriptional mechanisms. J Cell Biochem. 1995;57:488–94. doi: 10.1002/jcb.240570314. [DOI] [PubMed] [Google Scholar]
- 116.Delany AM, Jeffrey JJ, Rydziel S, Canalis E. Cortisol increases interstitial collagenase expression in osteoblasts by post-transcriptional mechanisms. J Biol Chem. 1995;270:26607–12. doi: 10.1074/jbc.270.44.26607. [DOI] [PubMed] [Google Scholar]
- 117.Lin X, Patil S, Gao YG, Qian A. The bone extracellular matrix in bone formation and regeneration. Front Pharmacol. 2020;11:757. doi: 10.3389/fphar.2020.00757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Hoshi K, Amizuka N, Oda K, Ikehara Y, Ozawa H. Immunolocalization of tissue non-specific alkaline phosphatase in mice. Histochem Cell Biol. 1997;107:183–91. doi: 10.1007/s004180050103. [DOI] [PubMed] [Google Scholar]
- 119.Miao D, Scutt A. Histochemical localization of alkaline phosphatase activity in decalcified bone and cartilage. J Histochem Cytochem. 2002;50:333–40. doi: 10.1177/002215540205000305. [DOI] [PubMed] [Google Scholar]
- 120.Hessle L, Johnson KA, Anderson HC, Narisawa S, Sali A, Goding JW, et al. Tissue-nonspecific alkaline phosphatase and plasma cell membrane glycoprotein-1 are central antagonistic regulators of bone mineralization. Proc Natl Acad Sci U S A. 2002;99:9445–9. doi: 10.1073/pnas.142063399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zoch ML, Clemens TL, Riddle RC. New insights into the biology of osteocalcin. Bone. 2016;82:42–9. doi: 10.1016/j.bone.2015.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Carvalho MS, Cabral JM, da Silva CL, Vashishth D. Synergistic effect of extracellularly supplemented osteopontin and osteocalcin on stem cell proliferation, osteogenic differentiation, and angiogenic properties. J Cell Biochem. 2019;120:6555–69. doi: 10.1002/jcb.27948. [DOI] [PubMed] [Google Scholar]
- 123.Termine JD, Kleinman HK, Whitson SW, Conn KM, McGarvey ML, Martin GR. Osteonectin, a bone-specific protein linking mineral to collagen. Cell. 1981;26:99–105. doi: 10.1016/0092-8674(81)90037-4. [DOI] [PubMed] [Google Scholar]
- 124.Delany AM, Amling M, Priemel M, Howe C, Baron R, Canalis E. Osteopenia and decreased bone formation in osteonectin-deficient mice. J Clin Invest. 2000;105:1325. doi: 10.1172/JCI7039C1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Andersen TL, del Carmen Ovejero M, Kirkegaard T, Lenhard T, Foged NT, Delaissé JM. A scrutiny of matrix metalloproteinases in osteoclasts: Evidence for heterogeneity and for the presence of MMPs synthesized by other cells. Bone. 2004;35:1107–19. doi: 10.1016/j.bone.2004.06.019. [DOI] [PubMed] [Google Scholar]
- 126.Drake FH, Dodds RA, James IE, Connor JR, Debouck C, Richardson S, et al. Cathepsin K, but not cathepsins B, L, or S, is abundantly expressed in human osteoclasts. J Biol Chem. 1996;271:12511–6. doi: 10.1074/jbc.271.21.12511. [DOI] [PubMed] [Google Scholar]
- 127.Vizovišek M, Fonović M, Turk B. Cysteine cathepsins in extracellular matrix remodeling: Extracellular matrix degradation and beyond. Matrix Biol. 2019;75-76:141–59. doi: 10.1016/j.matbio.2018.01.024. [DOI] [PubMed] [Google Scholar]
- 128.Iu MF, Kaji H, Naito J, Sowa H, Sugimoto T, Chihara K. Low-dose parathyroid hormone and estrogen reverse alkaline phosphatase activity suppressed by dexamethasone in mouse osteoblastic cells. J Bone Miner Metab. 2005;23:450–5. doi: 10.1007/s00774-005-0627-2. [DOI] [PubMed] [Google Scholar]
- 129.Strömstedt PE, Poellinger L, Gustafsson JA, Carlstedt-Duke J. The glucocorticoid receptor binds to a sequence overlapping the TATA box of the human osteocalcin promoter: A potential mechanism for negative regulation. Mol Cell Biol. 1991;11:3379–83. doi: 10.1128/mcb.11.6.3379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ikeda T, Kohno H, Yamamuro T, Kasai R, Ohta S, Okumura H, et al. The effect of active vitamin D3 analogs and dexamethasone on the expression of osteocalcin gene in rat tibiae in vivo. Biochem Biophys Res Commun. 1992;189:1231–5. doi: 10.1016/0006-291x(92)92336-v. [DOI] [PubMed] [Google Scholar]
- 131.Morrison N, Eisman J. Role of the negative glucocorticoid regulatory element in glucocorticoid repression of the human osteocalcin promoter. J Bone Miner Res. 1993;8:969–75. doi: 10.1002/jbmr.5650080810. [DOI] [PubMed] [Google Scholar]
- 132.He H, Wang C, Tang Q, Yang F, Xu Y. Possible mechanisms of prednisolone-induced osteoporosis in zebrafish larva. Biomed Pharmacother. 2018;101:981–7. doi: 10.1016/j.biopha.2018.02.082. [DOI] [PubMed] [Google Scholar]
- 133.Stoch SA, Wagner JA. Cathepsin K inhibitors: A novel target for osteoporosis therapy. Clin Pharmacol Ther. 2008;83:172–6. doi: 10.1038/sj.clpt.6100450. [DOI] [PubMed] [Google Scholar]
- 134.Lekamwasam S, Adachi JD, Agnusdei D, Bilezikian J, Boonen S, Borgström F, et al. A framework for the development of guidelines for the management of glucocorticoid-induced osteoporosis. Osteoporos Int. 2012;23:2257–76. doi: 10.1007/s00198-012-1958-1. [DOI] [PubMed] [Google Scholar]
- 135.Kanis JA, Johansson H, Oden A, McCloskey EV. Guidance for the adjustment of FRAX according to the dose of glucocorticoids. Osteoporos Int. 2011;22:809–16. doi: 10.1007/s00198-010-1524-7. [DOI] [PubMed] [Google Scholar]
- 136.Hwang JS. 2019 Taiwanese Consensus and Guidelines for the Prevention and Treatment of Adult Osteoporosis. Taipei, Taiwan: The Taiwanese Osteoporosis Association; 2019. pp. 37–41. [Google Scholar]
- 137.Yu SF, Chen JF, Chen YC, Lai HM, Ko CH, Chiu WC, et al. Beyond bone mineral density, FRAX-based tailor-made intervention thresholds for therapeutic decision in subjects on glucocorticoid: A nationwide osteoporosis survey. Medicine (Baltimore) 2017;96:e5959. doi: 10.1097/MD.0000000000005959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Hsu CY, Wu CH, Yu SF, Su YJ, Chiu WC, Chen YC, et al. Novel algorithm generating strategy to identify high fracture risk population using a hybrid intervention threshold. J Bone Miner Metab. 2020;38:213–21. doi: 10.1007/s00774-019-01046-4. [DOI] [PubMed] [Google Scholar]
- 139.Buckley L, Guyatt G, Fink HA, Cannon M, Grossman J, Hansen KE, et al. 2017 American College of Rheumatology Guideline for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Care Res (Hoboken) 2017;69:1095–110. doi: 10.1002/acr.23279. [DOI] [PubMed] [Google Scholar]
- 140.Rizzoli R, Biver E. Glucocorticoid-induced osteoporosis: Who to treat with what agent? Nat Rev Rheumatol. 2015;11:98–109. doi: 10.1038/nrrheum.2014.188. [DOI] [PubMed] [Google Scholar]
- 141.Huybers S, Naber TH, Bindels RJ, Hoenderop JG. Prednisolone-induced Ca2+malabsorption is caused by diminished expression of the epithelial Ca2+channel TRPV6. Am J Physiol Gastrointest Liver Physiol. 2007;292:G92–7. doi: 10.1152/ajpgi.00317.2006. [DOI] [PubMed] [Google Scholar]
- 142.Reid IR, Ibbertson HK. Evidence for decreased tubular reabsorption of calcium in glucocorticoid-treated asthmatics. Horm Res. 1987;27:200–4. doi: 10.1159/000180820. [DOI] [PubMed] [Google Scholar]
- 143.Rogers MJ. New insights into the molecular mechanisms of action of bisphosphonates. Curr Pharm Des. 2003;9:2643–58. doi: 10.2174/1381612033453640. [DOI] [PubMed] [Google Scholar]
- 144.Kavanagh KL, Guo K, Dunford JE, Wu X, Knapp S, Ebetino FH, et al. The molecular mechanism of nitrogen-containing bisphosphonates as antiosteoporosis drugs. Proc Natl Acad Sci U S A. 2006;103:7829–34. doi: 10.1073/pnas.0601643103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Hughes DE, Wright KR, Uy HL, Sasaki A, Yoneda T, Roodman GD, et al. Bisphosphonates promote apoptosis in murine osteoclasts in vitro and in vivo. J Bone Miner Res. 1995;10:1478–87. doi: 10.1002/jbmr.5650101008. [DOI] [PubMed] [Google Scholar]
- 146.Ito M, Amizuka N, Nakajima T, Ozawa H. Ultrastructural and cytochemical studies on cell death of osteoclasts induced by bisphosphonate treatment. Bone. 1999;25:447–52. doi: 10.1016/s8756-3282(99)00197-0. [DOI] [PubMed] [Google Scholar]
- 147.Plotkin LI, Weinstein RS, Parfitt AM, Roberson PK, Manolagas SC, Bellido T. Prevention of osteocyte and osteoblast apoptosis by bisphosphonates and calcitonin. J Clin Invest. 1999;104:1363–74. doi: 10.1172/JCI6800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Favus MJ. Bisphosphonates for osteoporosis. N Engl J Med. 2010;363:2027–35. doi: 10.1056/NEJMct1004903. [DOI] [PubMed] [Google Scholar]
- 149.Mottaghi P. Intravenous bisphosphonates for postmenopausal osteoporosis. J Res Med Sci. 2010;15:175–84. [PMC free article] [PubMed] [Google Scholar]
- 150.Marini JC. Do bisphosphonates make children's bones better or brittle? N Engl J Med. 2003;349:423–6. doi: 10.1056/NEJMp038103. [DOI] [PubMed] [Google Scholar]
- 151.Lewiecki EM, Bilezikian JP. Denosumab for the treatment of osteoporosis and cancer-related conditions. Clin Pharmacol Ther. 2012;91:123–33. doi: 10.1038/clpt.2011.268. [DOI] [PubMed] [Google Scholar]
- 152.Saag KG, Pannacciulli N, Geusens P, Adachi JD, Messina OD, Morales-Torres J, et al. Denosumab Versus Risedronate in Glucocorticoid-Induced Osteoporosis: Final Results of a Twenty-Four-Month Randomized, Double-Blind, Double-Dummy Trial. Arthritis Rheumatol. 2019;71:1174–84. doi: 10.1002/art.40874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Curtis JR, Xie F, Yun H, Saag KG, Chen L, Delzell E. Risk of hospitalized infection among rheumatoid arthritis patients concurrently treated with a biologic agent and denosumab. Arthritis Rheumatol. 2015;67:1456–64. doi: 10.1002/art.39075. [DOI] [PubMed] [Google Scholar]
- 154.Khan AA, Morrison A, Kendler DL, Rizzoli R, Hanley DA, Felsenberg D, et al. Case-Based Review of Osteonecrosis of the Jaw (ONJ) and Application of the International Recommendations for Management From the International Task Force on ONJ. J Clin Densitom. 2017;20:8–24. doi: 10.1016/j.jocd.2016.09.005. [DOI] [PubMed] [Google Scholar]
- 155.Cummings SR, Ferrari S, Eastell R, Gilchrist N, Jensen JB, McClung M, et al. Vertebral Fractures After Discontinuation of Denosumab: A Post hoc Analysis of the Randomized Placebo-Controlled FREEDOM Trial and Its Extension. J Bone Miner Res. 2018;33:190–8. doi: 10.1002/jbmr.3337. [DOI] [PubMed] [Google Scholar]
- 156.Boyce RW, Varela A, Chouinard L, Bussiere JL, Chellman GJ, Ominsky MS, et al. Infant cynomolgus monkeys exposed to denosumab in utero exhibit an osteoclast-poor osteopetrotic-like skeletal phenotype at birth and in the early postnatal period. Bone. 2014;64:314–25. doi: 10.1016/j.bone.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 157.Brunova J, Kratochvilova S, Stepankova J. Osteoporosis Therapy With Denosumab in Organ Transplant Recipients. Front Endocrinol (Lausanne) 2018;9:162. doi: 10.3389/fendo.2018.00162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Kobel C, Frey D, Graf N, Wuthrich RP, Bonani M. Follow-p of bone mineral density changes in de novo kidney transplant recipients treated with two doses of the receprtor activator of nuclear factor kappaB ligand inhibitor denosumab. Kidney Blood Press Res. 2019;44:1285–93. doi: 10.1159/000503066. [DOI] [PubMed] [Google Scholar]
- 159.Lane NE, Sanchez S, Modin GW, Genant HK, Pierini E, Arnaud CD. Parathyroid hormone treatment can reverse corticosteroid-induced osteoporosis.Results of a randomized controlled clinical trial. J Clin Invest. 1998;102:1627–33. doi: 10.1172/JCI3914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Saag KG, Shane E, Boonen S, Marín F, Donley DW, Taylor KA, et al. Teriparatide or alendronate in glucocorticoid-induced osteoporosis. N Engl J Med. 2007;357:2028–39. doi: 10.1056/NEJMoa071408. [DOI] [PubMed] [Google Scholar]
- 161.Hirooka Y, Nozaki Y, Inoue A, Li J, Shiga T, Kishimoto K, et al. Effects of denosumab versus teriparatide in glucocorticoid-induced osteoporosis patients with prior bisphosphonate treatment. Bone Rep. 2020;13:100293. doi: 10.1016/j.bonr.2020.100293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Nishida S, Yamaguchi A, Tanizawa T, Endo N, Mashiba T, Uchiyama Y, et al. Increased bone formation by intermittent parathyroid hormone administration is due to the stimulation of proliferation and differentiation of osteoprogenitor cells in bone marrow. Bone. 1994;15:717–23. doi: 10.1016/8756-3282(94)90322-0. [DOI] [PubMed] [Google Scholar]
- 163.Keller H, Kneissel M. SOST is a target gene for PTH in bone. Bone. 2005;37:148–58. doi: 10.1016/j.bone.2005.03.018. [DOI] [PubMed] [Google Scholar]
- 164.Bellido T, Ali AA, Gubrij I, Plotkin LI, Fu Q, O'Brien CA, et al. Chronic elevation of parathyroid hormone in mice reduces expression of sclerostin by osteocytes: A novel mechanism for hormonal control of osteoblastogenesis. Endocrinology. 2005;146:4577–83. doi: 10.1210/en.2005-0239. [DOI] [PubMed] [Google Scholar]
- 165.Guo J, Liu M, Yang D, Bouxsein ML, Saito H, Galvin RJ, et al. Suppression of Wnt signaling by Dkk1 attenuates PTH-mediated stromal cell response and new bone formation. Cell Metab. 2010;11:161–71. doi: 10.1016/j.cmet.2009.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Jilka RL, Weinstein RS, Bellido T, Roberson P, Parfitt AM, Manolagas SC. Increased bone formation by prevention of osteoblast apoptosis with parathyroid hormone. J Clin Invest. 1999;104:439–46. doi: 10.1172/JCI6610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Weinstein RS, Jilka RL, Almeida M, Roberson PK, Manolagas SC. Intermittent parathyroid hormone administration counteracts the adverse effects of glucocorticoids on osteoblast and osteocyte viability, bone formation, and strength in mice. Endocrinology. 2010;151:2641–9. doi: 10.1210/en.2009-1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Wan M, Yang C, Li J, Wu X, Yuan H, Ma H, et al. Parathyroid hormone signaling through low-density lipoprotein-related protein 6. Genes Dev. 2008;22:2968–79. doi: 10.1101/gad.1702708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Canalis E, Centrella M, Burch W, McCarthy TL. Insulin-like growth factor I mediates selective anabolic effects of parathyroid hormone in bone cultures. J Clin Invest. 1989;83:60–5. doi: 10.1172/JCI113885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Wang Y, Nishida S, Boudignon BM, Burghardt A, Elalieh HZ, Hamilton MM, et al. IGF-I receptor is required for the anabolic actions of parathyroid hormone on bone. J Bone Miner Res. 2007;22:1329–37. doi: 10.1359/jbmr.070517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Locklin RM, Khosla S, Turner RT, Riggs BL. Mediators of the biphasic responses of bone to intermittent and continuously administered parathyroid hormone. J Cell Biochem. 2003;89:180–90. doi: 10.1002/jcb.10490. [DOI] [PubMed] [Google Scholar]
- 172.Huang JC, Sakata T, Pfleger LL, Bencsik M, Halloran BP, Bikle DD, et al. PTH differentially regulates expression of RANKL and OPG. J Bone Miner Res. 2004;19:235–44. doi: 10.1359/JBMR.0301226. [DOI] [PubMed] [Google Scholar]
- 173.Glüer CC, Marin F, Ringe JD, Hawkins F, Möricke R, Papaioannu N, et al. Comparative effects of teriparatide and risedronate in glucocorticoid-induced osteoporosis in men: 18-month results of the EuroGIOPs trial. J Bone Miner Res. 2013;28:1355–68. doi: 10.1002/jbmr.1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Karatoprak C, Kayatas K, Kilicaslan H, Yolbas S, Yazimci NA, Gümüskemer T, et al. Severe hypercalcemia due to teriparatide. Indian J Pharmacol. 2012;44:270–1. doi: 10.4103/0253-7613.93869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Quintanilla Rodriguez BS, Correa R. Raloxifene. Treasure Island, FL: StatPearls; 2020. [Google Scholar]
- 176.Zhao JW, Gao ZL, Mei H, Li YL, Wang Y. Differentiation of human mesenchymal stem cells: The potential mechanism for estrogen-induced preferential osteoblast versus adipocyte differentiation. Am J Med Sci. 2011;341:460–8. doi: 10.1097/MAJ.0b013e31820865d5. [DOI] [PubMed] [Google Scholar]
- 177.Taranta A, Brama M, Teti A, De luca V, Scandurra R, Spera G, et al. The selective estrogen receptor modulator raloxifene regulates osteoclast and osteoblast activity in vitro. Bone. 2002;30:368–76. doi: 10.1016/s8756-3282(01)00685-8. [DOI] [PubMed] [Google Scholar]
- 178.Fujita K, Roforth MM, Demaray S, McGregor U, Kirmani S, McCready LK, et al. Effects of estrogen on bone mRNA levels of sclerostin and other genes relevant to bone metabolism in postmenopausal women. J Clin Endocrinol Metab. 2014;99:E81–8. doi: 10.1210/jc.2013-3249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Mödder UI, Clowes JA, Hoey K, Peterson JM, McCready L, Oursler MJ, et al. Regulation of circulating sclerostin levels by sex steroids in women and in men. J Bone Miner Res. 2011;26:27–34. doi: 10.1002/jbmr.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Kalam A, Talegaonkar S, Vohora D. Effects of raloxifene against letrozole-induced bone loss in chemically-induced model of menopause in mice. Mol Cell Endocrinol. 2017;440:34–43. doi: 10.1016/j.mce.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 181.Taxel P, Kaneko H, Lee SK, Aguila HL, Raisz LG, Lorenzo JA. Estradiol rapidly inhibits osteoclastogenesis and RANKL expression in bone marrow cultures in postmenopausal women: A pilot study. Osteoporos Int. 2008;19:193–9. doi: 10.1007/s00198-007-0452-7. [DOI] [PubMed] [Google Scholar]
- 182.Saika M, Inoue D, Kido S, Matsumoto T. 17beta-estradiol stimulates expression of osteoprotegerin by a mouse stromal cell line, ST-2, via estrogen receptor-alpha. Endocrinology. 2001;142:2205–12. doi: 10.1210/endo.142.6.8220. [DOI] [PubMed] [Google Scholar]
- 183.Sun J, Sun WJ, Li ZY, Li L, Wang Y, Zhao Y, et al. Daidzein increases OPG/RANKL ratio and suppresses IL-6 in MG-63 osteoblast cells. Int Immunopharmacol. 2016;40:32–40. doi: 10.1016/j.intimp.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 184.Hughes DE, Dai A, Tiffee JC, Li HH, Mundy GR, Boyce BF. Estrogen promotes apoptosis of murine osteoclasts mediated by TGF-beta. Nat Med. 1996;2:1132–6. doi: 10.1038/nm1096-1132. [DOI] [PubMed] [Google Scholar]
- 185.Michael H, Härkönen PL, Kangas L, Väänänen HK, Hentunen TA. Differential effects of selective oestrogen receptor modulators (SERMs) tamoxifen, ospemifene and raloxifene on human osteoclasts in vitro. Br J Pharmacol. 2007;151:384–95. doi: 10.1038/sj.bjp.0707232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.van Essen HW, Holzmann PJ, Blankenstein MA, Lips P, Bravenboer N. Effect of raloxifene treatment on osteocyte apoptosis in postmenopausal women. Calcif Tissue Int. 2007;81:183–90. doi: 10.1007/s00223-007-9050-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Polunin VS. The problems of developing a healthy life style and the treatment and rehabilitation of the population of the USSR from the viewpoints of the Ayurvedic approaches of the Maharishi. Vopr Kurortol Fizioter Lech Fiz Kult. 1992;1:57–8. [PubMed] [Google Scholar]
- 188.Ettinger B, Black DM, Mitlak BH, Knickerbocker RK, Nickelsen T, Genant HK, et al. Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: Results from a 3-year randomized clinical trial.Multiple Outcomes of Raloxifene Evaluation (MORE) Investigators. JAMA. 1999;282:637–45. doi: 10.1001/jama.282.7.637. [DOI] [PubMed] [Google Scholar]
- 189.Goldstein SR, Neven P, Cummings S, Colgan T, Runowicz CD, Krpan D, et al. Postmenopausal evaluation and risk reduction with lasofoxifene (PEARL) trial: 5-year gynecological outcomes. Menopause. 2011;18:17–22. doi: 10.1097/gme.0b013e3181e84bb4. [DOI] [PubMed] [Google Scholar]
- 190.Kaufman JM, Palacios S, Silverman S, Sutradhar S, Chines A. An evaluation of the Fracture Risk Assessment Tool (FRAX®) as an indicator of treatment efficacy: The effects of bazedoxifene and raloxifene on vertebral, nonvertebral, and all clinical fractures as a function of baseline fracture risk assessed by FRAX®. Osteoporos Int. 2013;24:2561–9. doi: 10.1007/s00198-013-2341-6. [DOI] [PubMed] [Google Scholar]
- 191.Kanis JA, Johnell O, Black DM, Downs RW, Jr, Sarkar S, Fuerst T. Effect of raloxifene on the risk of new vertebral fracture in postmenopausal women with osteopenia or osteoporosis: A reanalysis of the Multiple Outcomes of Raloxifene Evaluation trial. Bone. 2003;33:293–300. doi: 10.1016/s8756-3282(03)00200-x. [DOI] [PubMed] [Google Scholar]
- 192.Horak F, Doberer D, Eber E, Horak E, Pohl W, Riedler J, et al. Diagnosis and management of asthma-Statement on the 2015 GINA Guidelines. Wien Klin Wochenschr. 2016;128:541–54. doi: 10.1007/s00508-016-1019-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.von Scheven E, Corbin KJ, Stagi S, Cimaz R. Glucocorticoid-associated osteoporosis in chronic inflammatory diseases: Epidemiology, mechanisms, diagnosis, and treatment. Curr Osteoporos Rep. 2014;12:289–99. doi: 10.1007/s11914-014-0228-x. [DOI] [PubMed] [Google Scholar]
- 194.van Staa TP, Cooper C, Leufkens HG, Bishop N. Children and the risk of fractures caused by oral corticosteroids. J Bone Miner Res. 2003;18:913–8. doi: 10.1359/jbmr.2003.18.5.913. [DOI] [PubMed] [Google Scholar]