Abstract
The purpose of this report is to develop a theoretical model based on empirical evidence that can serve as a foundation for the science of peer-support factors that facilitate engagement in digital health interventions for people with serious mental illness (SMI). A review of the literature on how peer-support specialist interaction with consumers with SMI in digital health behavior change interventions enhances engagement. Unlike relationships with other health providers, peer-to-consumer relationships are based on reciprocal accountability —meaning that peer-support specialists and consumer mutually help and learn from each other. Under the recovery model of mental illness, reciprocal accountability suggests autonomy, flexible expectations, shared lived experience, and bonding influence engagement in digital interventions. Separate yet related components of reciprocal accountability in the context of digital health intervention engagement include (1) goal setting, (2) task agreement, and (3) bonding. Hope and sense of belonging are hypothesized moderators of peer-support factors in digital health interventions. Peer-support factors help people with SMI learn to live sucessfully both in the clinic and community. Peer-support specialists add value and complement traditional mental health treatment through their professional training and lived experience with a mental illness. The proposed model is a pioneering step towards understanding how peer-support factors impact engagement in digital health behavior change interventions among people with a lived experience of SMI. The model presents proposed factors underlying the reciprocal accountability processes in the context of digital health intervention engagement. This model and related support factors can be used to examine or identify research questions and hypotheses.
Keywords: Peer support, Digital health, Human factors, Science of behavior change
As the landscape of digital health interventions is transforming the way mental health services are provided—one constant remains the same—engaging in digital health behavior change interventions is difficult (Eysenbach 2005), especially among people with serious mental illness (SMI; i.e., schizophrenia spectrum disorder, bipolar disorder, and persistent, refractory major depressive disorder) (Christensen et al. 2009). Digital health behavior change interventions are behaviorally based interventions delivered via the Internet and mobile technologies. For people living with SMI, there are multiple challenges to engagement, including the individual and interactive effects of poverty (El-Mallakh 2007), internalized stigma (Corrigan and Watson 2002), low motivation caused by mental health conditions (Kukla et al. 2013), and/or lack of social support (Badcock et al. 2015; Beebe 2010; Cacioppo et al. 2006; Linz and Sturm 2013). Engagement is known to be key in producing clinically meaningful outcomes (Darkins et al. 2015; Hales et al. 2014). As such, an understanding of the factors that promote engagement in health digital interventions can guide the scientific community in developing health digital intervention components for people with SMI.
Engagement has been defined as a “multi-dimensional psychosocial process resulting from the conjoint cognitive, emotional, and behavioral enactment of individuals toward their health condition and management” in traditional face-to-face intervention settings (Graffigna et al. 2013). We define engagement in digital health interventions similar to former conceptualizations, with the addition of information about specific processes that contribute to goal attainment in the digital health context for people with SMI. A wide range of people with a lived experience of SMI receiving digital health interventions have been found to drop out of treatment early (i.e., approximately 1% to 72%) (Firth et al. 2015; Hidalgo-Mazzei et al. 2018; Palmier-Claus et al. 2012; Torous et al. 2015). Even in randomized controlled trials with precision participant selection processes and research staff support, attrition is common (Christensen et al. 2009; Christensen et al. 2002). Participants have been found to terminate early, often due to poor therapeutic alliance (Frank and Gunderson 1990; Horvath et al. 2011; Melau et al. 2015) and characteristics of people with a lived experience of SMI such as lack of afford-ability, lack of interest, lack of necessity, safety and privacy concerns (Anttila et al. 2012; Barnes et al. 2012; de Leeuw et al. 2012; Poole et al. 2012), technical issues (Anttila et al. 2012; de Leeuw et al. 2012; Poole et al. 2012; Todd et al. 2013), and limited digital health literacy (Anttila et al. 2012; Poole et al. 2012). Importantly, peer-supported digital health interventions for SMI may address several of these challenges, by increasing motivation and assisting with day-to-day intervention engagement. Peer-supported digital health interventions are digital interventions that include live or automated consumer interactions with a peer-support specialist as the “interventionists” or “coach.”
Support from a human in digital health interventions can improve engagement and reduce attrition (Ritterband et al. 2009). Human support from trained clinicians has shown to enhance in engagement in digital health behavior change interventions, via telephone, e-mail, and chat rooms (Naslund et al. 2015). By contrast, peer-support specialists (e.g., “peers,” certified peer specialists, recovery coaches) are individuals who have a mental health diagnosis, are in recovery, and who provide peer-support services (Solomon 2004). Peer-support specialists, an emerging workforce of digital health service providers, have also shown to enhance in engagement in digital health interventions, via text messaging (Fortuna et al. 2018b), web-based shared decision-making programs (Finnerty et al. 2018; Salyers et al. 2016), and social media chat rooms (Naslund et al. 2014). Peer-support specialists and digital health interventions for people with SMI are emerging as an important priority area for the World Health Organization (World Health Organization 2018). Further, people with a lived experience of SMI are also calling for digital interventions in mental health programs to include peer-support specialists (Fortuna et al. 2018c).
The impact of human support on digital health engagement in SMI populations is informed by the Supportive Accountability model, which theorizes that human support from health providers (e.g., lay, traditional mental health, and/or medical providers) enhances engagement in digital health interventions (Mohr et al. 2011). In this model, providers promote intervention engagement with people with a lived experience of SMI, in part, through common factors such as bonding (the degree of alliance and attachment between providers and people with a lived experience of SMI), legitimacy (perception of providers grounded in expertise, reciprocity, and caring), and accountability (implicit or explicit expectations that individuals justify their actions) (Mohr et al. 2011). However, peer-support specialists are different from other types of human support due to their shared experience of living with SMI, which contributes to the personal insights they gain from recovery and their unique commitment to helping others with a mental health condition. Peer-support specialists, therefore, can offer a level and quality of acceptance, understanding, and validation that is distinctive from the human support provided by other health providers (Mead and MacNeil 2006); however, to date, it is not known how support from peer-support specialists enhances engagement in digital health interventions.
This report proposes a theoretical model that can serve as a foundation for the science of human factors, or what we call “peer-support factors,” in digital health interventions within the context of SMI. An understanding of human factors in peer-supported digital interventions can guide researchers, peer-support specialists, and providers in developing peer-supported intervention components for digital health interventions for SMI. It is important to note that in this report, we focus on non-usage and dropout attrition due to modifiable factors of the intervention (Christensen et al. 2009; Christensen et al. 2002)—not those individuals that drop out prematurely from interventions whom have received enough benefit.
Theories of Peer Support
Peer support is a paid type of social service delivered by individuals living with mental illnesses who are trained to offer support services for mind-body recovery and overall health (Cabassa et al. 2017). Peer support is broadly defined as “giving and receiving help founded on key principles of respect, shared responsibility, and mutual agreement of what is helpful” (Mead and MacNeil 2006). Peer-support services have been recognized as a key component of the mental health system transformation to a recovery-oriented, person-centered model of care (Solomon 2004). Although peer-support services depend on various funding sources and are applied in a range of roles, job titles, and settings, peer-delivered programs share overarching philosophies, values, and goals relevant to the recovery and self-determination movement (Myrick and del Vecchio 2016).
Evidence indicates that peer support improves a multitude of outcomes among individuals with SMI diagnoses—including increasing levels of hope, empowerment, and self-care and decreasing depressive symptoms and psychosis (Davidson et al. 2012). Peer support is based on six social and behavioral theories including social support (Sarason et al. 1983), experiential knowledge (Borkman 1999), helper-therapy principle (Skovholt 1974), social learning theory (Bandura and Ramachaudran 1994), social comparison theory (Festinger 1954), and self-determination theory (Ryan and Deci 2000). We, including scientific researchers and certified peer specialists, have constructed a model based on these theories that explain how peer-support specialists might influence engagement in digital health behavior change interventions for individuals with SMI. This model details human factors or “peer-support factors” in digital health engagement (see Fig. 1). Below, we briefly describe each of these theories and the factors that delineate how peers influence engagement in digital health behavior change interventions.
Fig. 1.
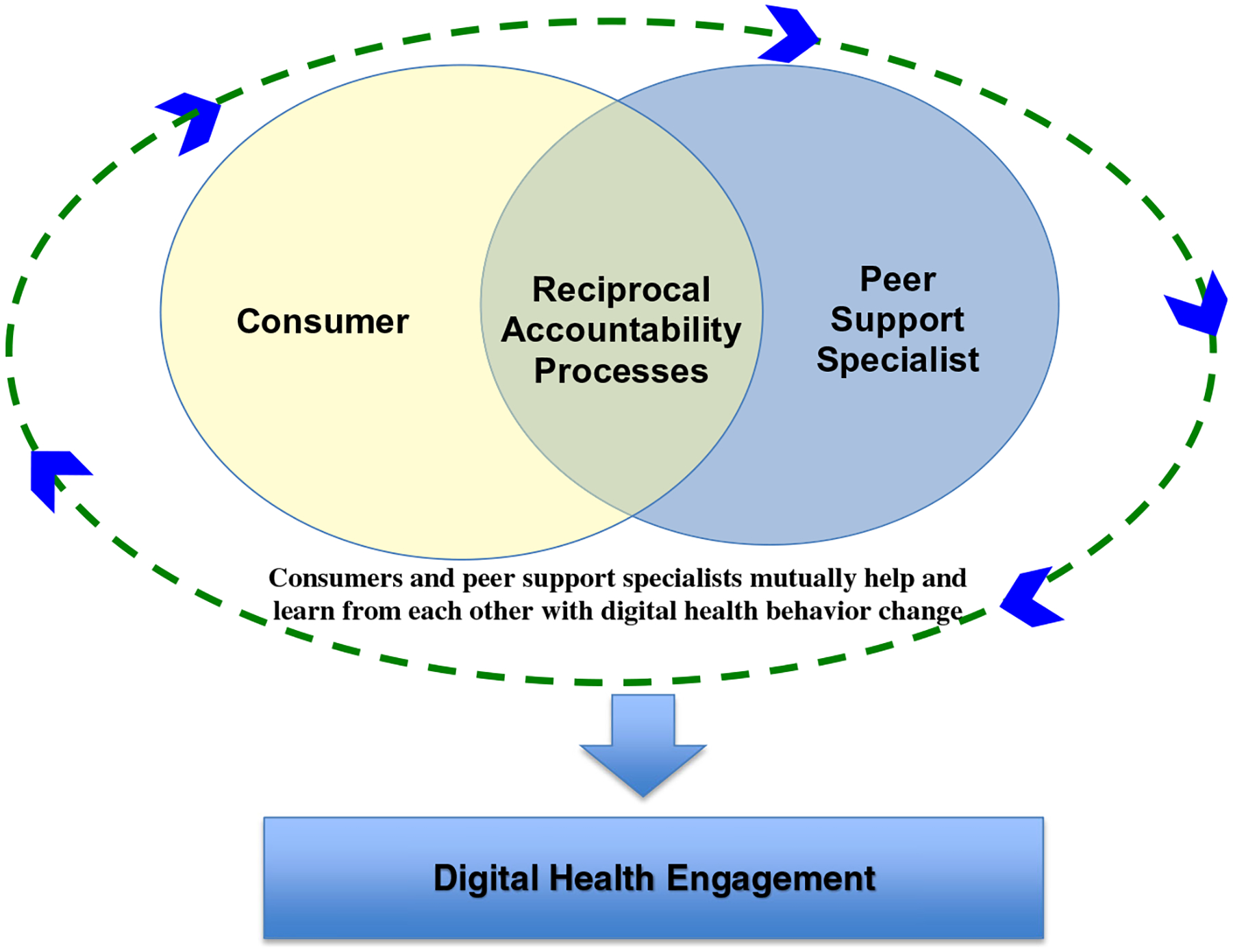
The model of reciprocal accountability of engagement in digital health behavior change interventions
Peer-to-Consumer Alliance
The strength of the peer-to-consumer relationship may act as a necessary peer-support function for improving engagement in digital health interventions. Alliance is a critical component to successful mental health outcomes (Wampold 2015) as it is directly related to engagement in mental health intervention (Eliacin et al. 2018). Alliance is defined as “the combination of (1) client and therapist agreement on goals, (2) client and therapist agreement on how to achieve the goals (task agreement), and (3) the development of a personal bond between the participants” (Tracey and Kokotovic 1989).
The alliance between peers and consumers is different than that of lay and traditional providers, as it is developed through reciprocal accountability. Reciprocal accountability is derived from social work literature and includes a “system wherein all persons involved hold one another accountable for specific commitments and activities in order to achieve the goals and objectives, which bring them together” (Borrero et al. 1979). Unlike relationships with other health providers, peer-to-consumer relationships are based on reciprocal accountability—meaning that peer-support specialists and consumer mutually help and learn from each other (helper-therapy principle) (Solomon 2004) and hold each other accountable in their personal recovery. This is contrasted with relationships in traditional face-to-face therapy, whereby therapists directly influence consumers’ recovery but are not expected to receive personal benefit from the relationship. For example, reciprocal accountability can challenge peer-support specialists and consumers to keep encouraging each other to meet their personalized goals. While people with a lived experience of SMI benefit from the feedback and experience of peers, peers benefit from mentoring others that are earlier in the recovery process. Frequent interactions lead to increased motivation to engage and maintain behaviors from both parties. Reciprocal accountability enables individuals to experience benefits from helping others through increased competence, receiving positive feedback, and self-affirmation (Skovholt 1974). Not surprisingly, many peer-support programs have shown benefits to the peer-support specialists who are delivering services to people with a lived experience of SMI (Salzer et al. 2013). This type of reciprocity accountability between consumers and other types of health providers (e.g., counselors, therapists) would not be appropriate or ethical. In traditional mental health and medical models, therapists and counselors are generally cautioned against sharing details of their personal lives with consumers.
By contrast, “traditional” accountability is defined as consumers’ expectation that they have to defend their actions or inactions (Lerner and Tetlock 1999). Rather, within a model of reciprocal accountability, peers and consumers view each other as equals and expect each other to focus on their personalized recovery goals. Reciprocal accountability requires a focus on the “whole person”—their values, their views, their beliefs, and their wants—not just mental health symptoms (Borrero et al. 1979). This focus on the recovery model of mental illness underscores that every person has strengths and even though they may not have control over psychiatric symptoms, people can still strive to live meaningful lives (Borrero et al. 1979).
Under the recovery model of mental illness, reciprocal accountability suggests autonomy, flexible expectations, shared lived experience, and bonding influence engagement in digital interventions. Below, we describe separate yet related components of reciprocal accountability in the context of digital health intervention engagement, including (1) goal setting, (2) task agreement, and (3) bonding. Then, we discuss hypothesized moderators of peer-support factors in digital health interventions.
Goal Setting
Autonomy
An essential aspect of peer support is its focus on promoting autonomy for people with a lived experience of SMI. Self-determination theory suggests that individuals are more likely to act on decisions they make for themselves, relative to decisions they feel are made through pressure or coercion (Deci and Ryan 1985). People with a lived experience of SMI typically have a long history of not being given a choice in defining their life goals or in treatment options (Wright 1997). If people with a lived experience of SMI perceive their goals as being largely determined by health providers, they may be less likely to work towards those goals (Brehm and Brehm 1981; Ordóñez et al. 2009). Often informed by their own experiences that have inhibited autonomy, a goal of peer-support specialists is to promote autonomy among people with a lived experience of SMI (Fortuna et al. 2018a). Based on self-determination theory, peer-supported digital health interventions that enable users to choose their own goals freely are likely to result in greater engagement (Brehm and Brehm 1981). Thus, creating a context that enables choice in peer-supported digital health interventions is important (e.g., choice in what goal they want to achieve or choice their actions of integrating the intervention into their daily life). Digital health interventions that employ software specifications that require consumers to engage with features such as setting medication reminders may violate a consumers’ sense of autonomy. By contrast, peer-developed smartphone applications such as PeerTECH offer a means for people with SMI to choose their own goal and the algorithms of the smartphone application changes to highlight relevant content based on their personalized goals (Fortuna et al. 2018c).
Flexible Expectations
Goal setting should include flexible expectations in how and when people with a lived experience of SMI achieve their goals. Recovery is a non-linear process with potential daily fluctuations in direction and course. Due to the severity of symptoms, people with a lived experience of SMI are likely to experience ups and downs as they make their way through a digital health behavior change intervention. A sense of flexibility is important in developing a realistic understanding of the recovery process. Unrealistic expectations lead to frustration and disengagement (Polivy 2001)—realistic expectations can have the opposite effect. As people have a higher likelihood of achieving these realistic goals—as they achieve them, this produces rewards, which has enhanced intrinsic motivation towards goal-directed behavior (Deci and Ryan 1985). Within the recovery model, peer-support specialists and consumers set clear goals but also accept that recovery does not always mean people with a lived experience of SMI will return to premorbid level of functioning. Peer-support specialists’ lived experience of flexible expectations helps them transpose those lessons for others.
Performance Monitoring
Performance monitoring is an important aspect of working towards personalized goals (Mohr et al. 2011). However, researchers should be thoughtful about the methods they employ to monitor progress. Performance monitoring through mobile sensors, social media data (i.e., Instagram, Facebook), motion mapping, and Bluetooth technology are commonly used as benchmarks in behavioral interventions for exercise and mental health. However, in the context of SMI, these methods may violate a consumers’ sense of autonomy and lead to disengagement. Performance monitoring without permission, input, and understanding may be seen as coercive and reminiscent of forced treatments.
Task Agreement
Shared Lived Experience
Peer-support specialists might influence task agreement (i.e., consumers and peer-support specialists agree on how to achieve goals) through their shared lived experience. Peer-support specialists have experiential knowledge of living with a serious mental illness (Borkman 1999). People with a lived experience of SMI are, therefore, more likely to view peer-support specialists as highly credible and trustworthy, increasing motivation to attain the goals they set (Tyler 1997). Peers are viewed as more credible than lay providers and traditional providers (Solomon 2004), in part, because of their personal experience of interacting with the mental health system. By contrast, knowledge of the mental health system among therapists and counselors is often derived from professional education and training, rather than direct experience of being a consumer of mental health services (Salzer 2002).
According to social learning theory, people with a lived experience of SMI may adopt healthy behaviors by observing and trying to replicate the actions of peer-support specialists that led to a successful road to recovery (Bandura 1994). Thus, consumer interactions with peer-support specialists who are successful in their recovery may stimulate agreement on how to achieve the goals. Thus, encouraging peer-support specialists to share their unique experience is important to inform the steps needed for people with a lived experience of SMI to engage in their own recovery. As such, asynchronous digital health technology such as peer-led videos or peer avatars, which are increasingly being used in digital health interventions, should not have a script written by traditional providers; rather, they allow peer-support specialists to share their experiences of recovery. It is important to train peer-support specialists to disclose their recovery stories using rehearsal and practice. Rehearsal can help peer-support specialists tell their stories in ways that are positive and beneficial to individuals, and not potentially triggering or harmful (i.e., unnecessary detail on topics regarding substance misuse, traumatic, or suicidal experiences). Additionally, to enhance the impact of social learning theory in asynchronous digital health technology and to promote task agreement, it may be useful to match peer-support specialists to consumers based on sociodemographic factors such as age or race.
Bond
Bonding
The therapeutic bond is an affective construct that is a significant predictor of goals and outcomes in digital health interventions (Beckner et al. 2007). Bonding is defined as the degree of platonic liking between a provider and consumer through emotional attachment. People with a lived experience of SMI, particularly minorities and those that live in underserved regions, are often distrustful of traditional providers (Fortuna et al. 2017; Sue and Sue 1990). Intervention engagement promotes bonding between peers and consumers through social support (Schutt and Rogers 2009). Although peer-support specialists are not trained therapists or counselors, they can be particularly effective in developing a bond with people with a lived experience of SMI (Davidson et al. 2006) through familiarity, perceived similarity, and trust (Zhao et al. 2012). Text messaging interactions between peer-support specialists and consumers have shown to facilitate bonding and digital health engagement (Fortuna et al. 2018b). It is not known if a bond can be facilitated between people with a lived experience of SMI and digital health technologies such as artificial intelligence (e.g., via digital avatars) or if such technologies are acceptable to people with a lived experience of SMI.
Moderators of Peer-support Factors
Sense of Belonging
Humans, whether experiencing a mental illness or not, have an innate need to belong (Baumeister and Leary 1995; Maslow 1954). Peer specialists and traditional providers can offer a sense of belonging. However, sense of belonging is defined as having an emotional attachment, a sense of identity, and group membership based on shared experiences (Hagborg 1998)—all of which may come faster for peer-support specialists compared to traditional providers, given that consumers with SMI often have difficulties trusting, connecting, and building relationships with lay providers/traditional providers due to feelings of stigmatization (Dixon et al. 2016). Unfortunately, many individuals diagnosed with SMI report the need to connect with others (Fortuna et al. 2019; Fortuna et al., Unmet need of people with serious mental illness, under review; Fortuna et al, Certified peer specialists’ perspective of the barriers and facilitators to mobile health engagement, under review.). A significantly higher proportion of people with SMI experience social isolation compared to the general population (Badcock et al. 2015)—commonly due to stigma, alienation, and loneliness (Linz and Sturm 2013). Social isolation reduces quality of life and also exacerbates physical health conditions (Linz and Sturm 2013). Emerging evidence indicates that digital health interventions that do not include human support may increase isolation (Fortuna et al. 2019; Fortuna et al., Unmet need of people with serious mental illness, under review; Fortuna et al, Certified peer specialists’ perspective of the barriers and facilitators to mobile health engagement, under review.). By increasing a sense of belonging, peer-support specialists may increase motivation and engagement in digital health interventions (Teo et al. 2003). For people with SMI who have fewer social supports, peer-supported digital health interventions may increase intervention engagement given people with a lived experience of SMI desire for social connection (Dixon et al. 2016).
Hope
Hope is defined as “a positive motivational state that is based on an interactively derived sense of successful agency (goal-directed energy) and pathways (planning to meet goals)” (Snyder et al. 1991). Hope is a protective emotion against despair (Lazarus 1999) and increases wellbeing (Peh et al. 2016). Thus, experiencing hope can be a catalyst for action. People with a lived experience of SMI might respond more positively to engaging in behavior change activities when they have a strong sense of hope (Corrigan et al. 2001) that they will be able to effectively manage their illness. Hopeful thoughts and related hopeful beliefs increase motivation to work towards planned goals (Shorey et al. 2002).
Because peer-support specialists have been able to successfully navigate the difficulties brought forth by a SMI diagnosis, they offer not only tangible assistance to people with a lived experience of SMI but embody the notion that meaningful change is possible. Unlike other service providers, peer specialists may increase hope in people simply through their positive interactions and self-disclosures (Davidson et al. 2006), allowing people with a lived experience of SMI to feel understood and validated.
According to social comparison theory (Festinger 1954), peer-support specialists-to-consumer interactions encourage an upward comparison, motivating them to engage in activities to meet their goals (Salzer et al. 2013). By interacting with peer-support specialists in recovery, people with a lived experience of SMI have hope in their future prognosis (Solomon 2004). These comparisons may not be possible with lay providers and traditional providers if they do not have experiences with mental illness or do not disclose their experiences as a person with a lived experience of SMI. To enhance the impact of social comparison theory in asynchronous digital health technology and encourage an upward comparison, hiring a peer-support specialist for videos or developing avatars that physically appear to be in recovery is ideal.
Summary of Peer-support Factors
Peer-support specialists complement traditional mental health treatment through their professional training and their lived experience of a mental illness. As such, reciprocal accountability overlaps with other models (e.g., supportive accountability) and provides a platform from which to understand peer-involved digital technology interventions for individuals with SMI. Peer-support factors suggest that engagement in digital health interventions will be enhanced when peer-support specialists are embedded within the recovery model of mental health and (1) the relationship is framed on reciprocal accountability in which peers and consumers view each other as equals and motivate each other to work towards their individual goals, (2) have similar lived experiences as consumers and are willing to share these experiences, (3) are in recovery and are perceived as credible experts; (4) peer-support specialists and consumers are matched together based on similarities such as medical or psychiatric conditions to promote optimal task agreement; (5) involve consumers as equal partners in defining personalized goals; (6) goal attainment is viewed as a non-linear process, and expectations to achieve goals are flexible and clear; (7) peer-support factor may be especially effective towards treatment engagement in people with experiencing a high level of stigma and (8) offer a sense of belonging and hope for the future.
Brief Overview of Technology-Based Models of Peer Support
Consumer-Run Organizations and Mobile Technologies
While informal peer-support services such as self-help groups and advocacy organizations have been an integral part of the mental health system since the 1960s and earlier, formally hiring or collaborating with peer-support specialists has occurred more recently over the past several decades (Davidson et al. 2006). In the 1980s and 1990s, formal peer support in mental health programs started to expand through the use of consumer-run organizations, and outreach and case management programs (Gagne et al. 2018). Mobile technologies, such as smartphone apps, show promise for extending psychiatric rehabilitation services in modern consumer-run community-based organizations (Mueller et al. 2018).
Peer-Supported Asynchronous Technology
Peer-supported asynchronous technology is defined as an intervention model that includes peer-support specialists in conjunction with technology that has communication features that do not occur in real time (e.g., consumer and peer-support specialists access a video side-by-side). For example, CommonGround is a peer-supported asynchronous technology intervention that promotes identifying personalized goals and strategies to enhance recovery (Campbell et al. 2014; Salyers et al. 2016). The CommonGround approach involves consumers completing a health report on a computer kiosk with assistance from peer-support specialists, which documents topics and focus areas for their discussion with the psychiatrist (Campbell et al. 2014; Salyers et al. 2016). CommonGround has shown improved consumer-provider communication, shared treatment decisions, focus on recovery-oriented goals (Campbell et al. 2014), self-reported symptoms, and recovery attitudes (Salyers et al. 2016).
Certified Peer Specialists-Delivered and Technology-Assisted Interventions
In 2007, the Centers for Medicare & Medicaid Services authorized state Medicaid programs to bill for peer-support services, which included the launch of statewide peer training, supervision, and certification (Chapman et al. 2018). Certified peer specialists are now a rapidly evolving, growing mental health profession with a total of 42 states adopting peer certification, supervision, and training programs (Kaufman et al. 2016). Certified peer specialists own and utilize smartphones, and the majority are willing to deliver technology-enhanced interventions using these devices to promote health behavior change (Fortuna et al. 2017). Promising evidence suggests the feasibility, acceptability, and preliminary effectiveness of peer-developed and delivered integrated self-management interventions that use mobile technologies for guided intervention delivery to support fidelity (Fortuna et al. 2018c).
Informal Peer Support, Social Media, and Virtual Reality
Informal peer support, similar to formal peer support is a non-hierarchical, reciprocal relationship between individuals with similar lived experience. For example, informal peer support can naturally occur between people who attend a support meeting. Social media platforms offer a means for people with SMI to share their personal lived experiences with a mental illness (Vance et al. 2009). There are support groups on Facebook for people with SMI (Aschbrenner et al. 2018; Naslund et al. 2018) and personal videos posted by people with a lived experience of SMI onto YouTube (Naslund et al. 2014). Informal peer support has shown to increase levels of social support (Castelein et al. 2008), self-esteem, and self-efficacy (Bracke and Verhaeghe 2006). Social media websites like Facebook, YouTube, and Twitter seem to be particularly useful as informal peer support outlets among people with a lived experience of SMI (Aschbrenner et al. 2018; Naslund et al. 2016; Naslund et al. 2018).
Virtual reality may also offer a means for informal peer support for people with SMI to share their personal lived experiences with a mental illness. Through virtual reality, support groups for people with SMI can potentially interact with one another on a personal level in a virtual environment. The feasibility, acceptability, and effectiveness of this type of technology for people that experience delusions and hallucinations are not known and a potentially meaningful technology is needed to explore with caution.
Conclusions
Most health providers are trained to understand serious mental illnesses as chronic deteriorating illnesses and to provide traditional treatments. Digital health using human factors has improved medication adherence and psychotherapy attendance rates. While these traditional mental health services combined with digital health can assist with treatment compliance, peer-support factors help people with SMI to learn to live successfully both in the clinic and community. Peer-support specialists add value and complement traditional mental health treatment through their professional training and lived experience with a mental illness (Cook et al. 2010). The proposed model is a pioneering step towards understanding how peer-support factors impact engagement in digital health behavior change interventions among people with a lived experience of SMI. The model proposed factors underlying the reciprocal accountability processes in the context of digital health intervention engagement. This model and related support factors can be used to examine or identify research questions and hypotheses.
Footnotes
Conflict of interest The authors declare that there is no conflict of interest.
References
- Anttila M, Välimäki M, Hätönen H, Luukkaala T, & Kaila M (2012). Use of web-based patient education sessions on psychiatric wards. International Journal of Medical Informatics, 81(6), 424–433. 10.1016/j.ijmedinf.2012.02.004. [DOI] [PubMed] [Google Scholar]
- Aschbrenner KA, Naslund JA, Gorin AA, Mueser KT, Scherer EA, Viron M, Kinney A, & Bartels SJ (2018). Peer support and mobile health technology targeting obesity-related cardiovascular risk in young adults with serious mental illness: protocol for a randomized controlled trial. Contemporary Clinical Trials, 74, 97–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badcock JC, Shah S, Mackinnon A, Stain HJ, Galletly C, Jablensky A, & Morgan VA (2015). Loneliness in psychotic disorders and its association with cognitive function and symptom profile. Schizophrenia Research, 169(1–3), 268–273. [DOI] [PubMed] [Google Scholar]
- Bandura A (1994). Self-efficacy. In Corsini RJ. Encyclopedia of psychology 2 (3),368–369. New York: Wiley. [Google Scholar]
- Bandura A, & Ramachaudran VS (1994). Encyclopedia of human behavior. New York: Academic Press. [Google Scholar]
- Barnes AL, Murphy ME, Fowler CA, & Rempfer MV (2012). Health-related quality of life and overall life satisfaction in people with serious mental illness. Schizophrenia Research and Treatment, 2012, 1–6. 10.1155/2012/245103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumeister RF, & Leary MR (1995). The need to belong: desire for interpersonal attachments as a fundamental human motivation. Psychological Bulletin, 117(3), 497–529. [PubMed] [Google Scholar]
- Beckner V, Vella L, Howard I, & Mohr DC (2007). Alliance in two telephone-administered treatments: relationship with depression and health outcomes. Journal of Consulting and Clinical Psychology, 75(3), 508–512. [DOI] [PubMed] [Google Scholar]
- Beebe LH (2010). What community living problems do persons with schizophrenia report during periods of stability? Perspectives in Psychiatric Care, 46(1), 48–55. [DOI] [PubMed] [Google Scholar]
- Borkman TJ (1999). Understanding self-help/mutual aid: experiential learning in the commons. New Brunswick, NJ: Rutgers University Press. [Google Scholar]
- Borrero M, Martens P, & Gubelman Borrero G (1979). Toward a theory of accountability. Journal of Sociology & Social Welfare, 6, 876–894. [Google Scholar]
- Bracke P, & Verhaeghe M (2006). The balance of peer support among persons with chronic mental health problems: consequences and antecedents. Paper presented at The 11th international congress of the European Society for Health and Medical Sociology. [Google Scholar]
- Brehm S, & Brehm JW (1981). Psychological reactance: a theory of freedom and control. New York, NY: Academic Press. [Google Scholar]
- Cabassa LJ, Camacho D, Vélez-Grau CM, & Stefancic A (2017). Peer-based health interventions for people with serious mental illness: a systematic literature review. Journal of Psychiatric Research, 84, 80–89. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, & Thisted RA (2006). Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychology and Aging, 21(1), 140–151. [DOI] [PubMed] [Google Scholar]
- Campbell SR, Holter MC, Manthey TJ, & Rapp CA (2014). The effect of CommonGround software and decision support center. American Journal of Psychiatric Rehabilitation, 17(2), 166–180. [Google Scholar]
- Castelein S, Bruggeman R, Van Busschbach JT, Van Der Gaag M, Stant A, Knegtering H, & Wiersma D (2008). The effectiveness of peer support groups in psychosis: a randomized controlled trial. Acta Psychiatrica Scandinavica, 118(1), 64–72. [DOI] [PubMed] [Google Scholar]
- Chapman SA, Blash LK, Mayer K, & Spetz J (2018). Emerging roles for peer providers in mental health and substance use disorders. American Journal of Preventive Medicine, 54(6), S267–S274. [DOI] [PubMed] [Google Scholar]
- Christensen H, Griffiths KM, & Korten A (2002). Web-based cognitive behavior therapy: analysis of site usage and changes in depression and anxiety scores. Journal of Medical Internet Research, 4(1), e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen H, Griffiths KM, & Farrer L (2009). Adherence in internet interventions for anxiety and depression: systematic review. Journal of Medical Internet Research, 11(2), e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook JA, Copeland ME, Corey L, Buffington E, Jonikas JA, Curtis LC, Grey DD, & Nichols WH (2010). Developing the evidence base for peer-led services: changes among participants following wellness recovery action planning (WRAP) education in two statewide initiatives. Psychiatric Rehabilitation Journal, 34(2), 113–120. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, & Watson AC (2002). Understanding the impact of stigma on people with mental illness. World Psychiatry, 1(1), 16–20. [PMC free article] [PubMed] [Google Scholar]
- Corrigan PW, McCracken SG, & Holmes EP (2001). Motivational interviews as goal assessment for persons with psychiatric disability. Community Mental Health Journal, 37(2), 113–122. [DOI] [PubMed] [Google Scholar]
- Darkins A, Kendall S, Edmonson E, Young M, & Stressel P (2015). Reduced cost and mortality using home telehealth to promote self-management of complex chronic conditions: a retrospective matched cohort study of 4,999 veteran patients. Telemedicine and e-Health, 21(1), 70–76. [DOI] [PubMed] [Google Scholar]
- Davidson L, Chinman M, Sells D, & Rowe M (2006). Peer support among adults with serious mental illness: a report from the field. Schizophrenia Bulletin, 32(3), 443–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson L, Bellamy C, Guy K, & Miller R (2012). Peer support among persons with severe mental illnesses: a review of evidence and experience. World Psychiatry, 11(2), 123–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Leeuw JRJ, van Splunteren P, & Boerema I (2012). Personal control in rehabilitation: an internet platform for patients with schizophrenia and their caregivers. Open Journal of Psychiatry, 2(04), 355–361. [Google Scholar]
- Deci EL, & Ryan RM (1985). The general causality orientations scale: self-determination in personality. Journal of Research in Personality, 19(2), 109–134. [Google Scholar]
- Dixon LB, Holoshitz Y, & Nossel I (2016). Treatment engagement of individuals experiencing mental illness: review and update. World Psychiatry, 15(1), 13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eliacin J, Coffing JM, Matthias MS, Burgess DJ, Bair MJ, & Rollins AL (2018). The relationship between race, patient activation, and working alliance: implications for patient engagement in mental health care. Administration and Policy in Mental Health and Mental Health Services Research, 45(1), 186–192. [DOI] [PubMed] [Google Scholar]
- El-Mallakh P (2007). Doing my best: poverty and self-care among individuals with schizophrenia and diabetes mellitus. Archives of Psychiatric Nursing, 21(1), 49–60. [DOI] [PubMed] [Google Scholar]
- Eysenbach G (2005). The law of attrition. Journal of Medical and Internet Research, 7(1), e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Festinger L (1954). A theory of social comparison processes. Human Relations, 7,117–140. 10.1177/001872675400700202. [DOI] [Google Scholar]
- Finnerty M, Austin E, Chen Q, Layman D, Kealey E, Ng-Mak D, Rajagopalan K, & Hoagwood K (2018). Implementation and use of a client-facing web-based shared decision-making system (MyCHOIS-CommonGround) in two specialty mental health clinics. Community Mental Health Journal, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firth J, Cotter J, Torous J, Bucci S, Firth JA, & Yung AR (2015). Mobile phone ownership and endorsement of “mHealth” among people with psychosis: a meta-analysis of cross-sectional studies. Schizophrenia Bulletin, 42(2), 448–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortuna KL, Lohman MC, Batsis JA, DiNapoli EA, DiMilia PR, Bruce ML, & Bartels SJ (2017). Patient experience with healthcare services among older adults with serious mental illness compared to the general older population. The International Journal of Psychiatry in Medicine, 52(4–6), 381–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortuna K, Aschbrenner K, & Bartels S (2018a). Integration of peer philosophy in clinical workflow. Psychiatric Quarterly, 89(4), 795–800. 10.1007/s11126-018-9578-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortuna K, Aschbrenner K, Lohman M, Salzer M, & Bartels S (2018b). Text message exchanges between older adults with serious mental illness and older certified peer specialists in a smartphone-supported self-management intervention. Psychiatric Rehabilitation Journal, 42, 57–63. 10.1037/prj0000305. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortuna KL, DiMilia PR, Lohman MC, Bruce ML, Zubritsky CD, Halaby MR, Walker RM, Brooks JM, & Bartels SJ (2018c). Feasibility, acceptability, and preliminary effectiveness of a peer-delivered and technology supported self-management intervention for older adults with serious mental illness. Psychiatric Quarterly, 89(2), 293–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortuna K, Barr P, Goldstein C, Walker R, Brewer L, Zagaria A, Bartels S (2019). Application of Community-engaged research to inform the development and implementation of a peer-delivered mobile health intervention for adults with serious mental illness. Journal of Participatory Medicine, 11(1), e12380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank AF, & Gunderson JG (1990). The role of the therapeutic alliance in the treatment of schizophrenia: relationship to course and outcome. Archives of General Psychiatry, 47(3), 228–236. [DOI] [PubMed] [Google Scholar]
- Gagne CA, Finch WL, Myrick KJ, & Davis LM (2018). Peer workers in the behavioral and integrated health workforce: opportunities and future directions. American Journal of Preventive Medicine, 54(6), S258–S266. [DOI] [PubMed] [Google Scholar]
- Graffigna G, Barello S, & Riva G (2013). How to make health information technology effective: the challenge of patient engagement. Archives of Physical Medicine and Rehabilitation, 94, 2034–2035. 10.1016/j.apmr.2013.04.024. [DOI] [PubMed] [Google Scholar]
- Hagborg WJ (1998). An investigation of a brief measure of school membership. Adolescence, 33(130), 461–468. [PubMed] [Google Scholar]
- Hales SB, Davidson C, & Turner-McGrievy GM (2014). Varying social media post types differentially impacts engagement in a behavioral weight loss intervention. Translational Behavioral Medicine, 4(4), 355–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hidalgo-Mazzei D, Reinares M, Mateu A, Nikolova VL, del Mar Bonnin C, Samalin L, Garcia-Estela A, Perez-Sola V, Young AH, Strejilevich S, & Vieta E (2018). OpenSIMPLe: a realworld implementation feasibility study of a smartphone-based psychoeducation programme for bipolar disorder. Journal of Affective Disorders, 241, 436–445. [DOI] [PubMed] [Google Scholar]
- Horvath AO, Del Re A, Flückiger C, & Symonds D (2011). Alliance in individual psychotherapy. Psychotherapy, 48(1), 9–16. [DOI] [PubMed] [Google Scholar]
- Kaufman L, Kuhn W, & Stevens Manser S (2016). Peer specialist training and certification programs: a National Overview. Texas Institute for Excellence in Mental Health, School of Social Work, University of Texas at Austin. [Google Scholar]
- Kukla M, Salyers MP, & Lysaker PH (2013). Levels of patient activation among adults with schizophrenia: associations with hope, symptoms, medication adherence, and recovery attitudes. The Journal of Nervous and Mental Disease, 201(4), 339–344. [DOI] [PubMed] [Google Scholar]
- Lazarus RS (1999). Hope: an emotion and a vital coping resource against despair. Social Research, 66(2), 653–678. [Google Scholar]
- Lerner JS, & Tetlock PE (1999). Accounting for the effects of accountability. Psychological Bulletin, 125(2), 255–275. [DOI] [PubMed] [Google Scholar]
- Linz SJ, & Sturm BA (2013). The phenomenon of social isolation in the severely mentally ill. Perspectives in Psychiatric Care, 49(4), 243–254. [DOI] [PubMed] [Google Scholar]
- Maslow AH (1954). The instinctoid nature of basic needs. Journal of Personality, 22, 326–347. [DOI] [PubMed] [Google Scholar]
- Mead S, & MacNeil C (2006). Peer support: what makes it unique. International Journal of Psychosocial Rehabilitation, 10(2), 29–37. [Google Scholar]
- Melau M, Harder S, Jeppesen P, Hjorthøj C, Jepsen J, Thorup A, & Nordentoft M (2015). The association between working alliance and clinical and functional outcome in a cohort of 400 patients with first-episode psychosis: a cross-sectional study. The Journal of Clinical Psychiatry, 76(1), 83–90. [DOI] [PubMed] [Google Scholar]
- Mohr DC, Cuijpers P, & Lehman K (2011). Supportive accountability: a model for providing human support to enhance adherence to eHealth interventions. Journal of Medical Internet Research, 13(1). 10.2196/2Fjmir.1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller NE, Panch T, Macias C, Cohen BM, Ongur D, & Baker JT (2018). Using smartphone apps to promote psychiatric rehabilitation in a peer-led community support program: pilot study. JMIR Mental Health, 5(3), e10092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myrick K, & del Vecchio P (2016). Peer support services in the behavioral healthcare workforce: state of the field. Psychiatric Rehabilitation Journal, 39(3), 197–206. [DOI] [PubMed] [Google Scholar]
- Naslund JA, Grande SW, Aschbrenner KA, & Elwyn G (2014). Naturally occurring peer support through social media: the experiences of individuals with severe mental illness using YouTube. PLoS One, 9(10), e110171. 10.1371/journal.pone.0110171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund JA, Marsch LA, McHugo GJ, & Bartels SJ (2015). Emerging mHealth and eHealth interventions for serious mental illness: a review of the literature. Journal of Mental Health, 24(5), 321–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund J, Aschbrenner K, Marsch L, & Bartels S (2016). The future of mental health care: peer-to-peer support and social media. Epidemiology and Psychiatric Sciences, 25(2), 113–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund JA, Aschbrenner KA, Marsch LA, McHugo GJ, & Bartels SJ (2018). Facebook for supporting a lifestyle intervention for people with major depressive disorder, bipolar disorder, and schizophrenia: an exploratory study. Psychiatric Quarterly, 89(1), 81–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ordóñez LD, Schweitzer ME, Galinsky AD, & Bazerman MH (2009). Goals gone wild: the systematic side effects of overprescribing goal setting. Academy of Management Perspectives, 23(1), 6–16. [Google Scholar]
- Palmier-Claus JE, Ainsworth J, Machin M, Barrowclough C, Dunn G, Barkus E, Rogers A, Wykes T, Kapur S, Buchan I, & Salter E (2012). The feasibility and validity of ambulatory self-report of psychotic symptoms using a smartphone software application. BMC Psychiatry, 12(1), 1–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peh CX, Kua EH, & Mahendran R (2016). Hope, emotion regulation, and psychosocial well-being in patients newly diagnosed with cancer. Supportive Care in Cancer, 24(5), 1955–1962. [DOI] [PubMed] [Google Scholar]
- Polivy J (2001). The false hope syndrome: unrealistic expectations of self-change. International Journal of Obesity, 25(S1), 80–84. [DOI] [PubMed] [Google Scholar]
- Poole R, Simpson SA, & Smith DJ (2012). Internet-based psychoeducation for bipolar disorder: a qualitative analysis of feasibility, acceptability and impact. BMC Psychiatry, 12(1), 139. 10.1186/1471-244X-12-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritterband LM, Thorndike FP, Cox DJ, Kovatchev BP, & Gonder-Frederick LA (2009). A behavior change model for internet interventions. Annals of Behavioral Medicine, 38(1), 18–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan RM, & Deci EL (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist, 55(1), 68–78. [DOI] [PubMed] [Google Scholar]
- Salyers MP, Fukui S, Bonfils KA, Firmin RL, Luther L, Goscha R, Rapp CA, & Holter MC (2016). Consumer outcomes after implementing CommonGround as an approach to shared decision making. Psychiatric Services, 68(3), 299–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salzer MS (2002). Consumer-delivered services as a best practice in mental health care delivery and the development of practice guidelines. Psychiatric Rehabilitation Skills, 6(3), 355–382. 10.1080/10973430208408443. [DOI] [Google Scholar]
- Salzer MS, Darr N, Calhoun G, Boyer W, Loss RE, Goessel J, Schwenk E, & Brusilovskiy E (2013). Benefits of working as a certified peer specialist: results from a statewide survey. Psychiatric Rehabilitation Journal, 36(3), 219–221. 10.1037/prj0000016. [DOI] [PubMed] [Google Scholar]
- Sarason IG, Levine HM, Basham RB, & Sarason BR (1983). Assessing social support: the social support questionnaire. Journal of Personality and Social Psychology, 44(1), 127–139. 10.1037/0022-3514.44.1.127. [DOI] [Google Scholar]
- Schutt RK, & Rogers ES (2009). Empowerment and peer support: structure and process of self-help in a consumer-run center for individuals with mental illness. Journal of Community Psychology, 37(6), 697–710. [Google Scholar]
- Shorey HS, Snyder CR, Rand KL, Hockemeyer JR, & Feldman DB (2002). Authors’ response: somewhere over the rainbow: hope theory weathers its first decade. Psychological Inquiry, 13(4), 322–331. 10.1207/S15327965PLI1304_03. [DOI] [Google Scholar]
- Skovholt TM (1974). The client as helper: a means to promote psychological growth. The Counseling Psychologist, 4(3), 58–64. 10.1177/001100007400400308 [DOI] [Google Scholar]
- Snyder CR, Harris C, Anderson JR, Holleran SA, Irving LM, Sigmon ST, Yoshinobu L, Gibb J, Langelle C, & Harney P (1991). The will and the ways: development and validation of an individual-differences measure of hope. Journal of Personality and Social Psychology, 60(4), 570–585. 10.1037/0022-3514.60.4.570. [DOI] [PubMed] [Google Scholar]
- Solomon P (2004). Peer support/peer provided services underlying processes, benefits, and critical ingredients. Psychiatric Rehabilitation Journal, 27(4), 392–401. [DOI] [PubMed] [Google Scholar]
- Sue DW, & Sue D (1990). Counseling the culturally different: theory and practice. Oxford, England: John Wiley & Sons. [Google Scholar]
- Teo H-H, Chan H-C, Wei K-K, & Zhang Z (2003). Evaluating information accessibility and community adaptivity features for sustaining virtual learning communities. International Journal of Human-Computer Studies, 59(5), 671–697. 10.1016/S1071-5819(03)00087-9. [DOI] [Google Scholar]
- Todd NJ, Jones SH, & Lobban FA (2013). What do service users with bipolar disorder want from a web-based self-management intervention? A qualitative focus group study. Clinical Psychology & Psychotherapy, 20(6), 531–543. 10.1002/cpp.1804. [DOI] [PubMed] [Google Scholar]
- Torous J, Staples P, Shanahan M, Lin C, Peck P, Keshavan M, & Onnela J-P (2015). Utilizing a personal smartphone custom app to assess the Patient Health Questionnaire-9 (PHQ-9) depressive symptoms in patients with major depressive disorder. JMIR mental health, 2(1), e8. 10.2196/mental.3889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tracey TJ, & Kokotovic AM (1989). Factor structure of the Working Alliance Inventory. Psychological Assessment: A Journal of Consulting and Clinical Psychology, 1(3), 207–210. 10.1037/1040-3590.1.3.207. [DOI] [Google Scholar]
- Tyler TR (1997). The psychology of legitimacy: a relational perspective on voluntary deference to authorities. Personality and Social Psychology Review, 1(4), 323–345. 10.1207/s15327957pspr0104_4. [DOI] [PubMed] [Google Scholar]
- Vance K, Howe W, & Dellavalle RP (2009). Social internet sites as a source of public health information. Dermatologic Clinics, 27(2), 133–136. 10.1016/j.det.2008.11.010. [DOI] [PubMed] [Google Scholar]
- Wampold BE (2015). How important are the common factors in psychotherapy? An update. World Psychiatry, 14(3), 270–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2018). Guidelines for the management of physical health conditions in adults with severe mental disorders. Geneva: World Health Organization. [PubMed] [Google Scholar]
- Wright D (1997). Getting out of the asylum: understanding the confinement of the insane in the nineteenth century. Social History of Medicine, 10(1), 137–155. [DOI] [PubMed] [Google Scholar]
- Zhao L, Lu Y, Wang B, Chau PYK, & Zhang L (2012). Cultivating the sense of belonging and motivating user participation in virtual communities: a social capital perspective. International Journal of Information Management, 32(6), 574–588. 10.1016/j.ijinfomgt.2012.02.006. [DOI] [Google Scholar]


