Abstract
In the context of a chronic illness such as type 1 diabetes (T1D), managing general stressors may be linked to diabetes-specific stressors for persons with T1D, an intraindividual contagion phenomenon (i.e., spillover). Among those with romantic partners, stress may also be associated with the partner’s stress (i.e., crossover). These intraindividual and interpersonal processes may be further strengthened or weakened in the presence of individual (e.g., sleep satisfaction) and interpersonal (e.g., relationship satisfaction) factors. This study examined spillover and crossover effects between daily general and diabetes-specific stressors and whether sleep satisfaction and relationship satisfaction moderated spillover and crossover effects among couples in which one person had T1D. Persons with T1D (n = 199; Mage = 46.82, 52.3% female) and their romantic partners (n = 199; Mage = 46.41, 47.2% female) reported general stressors and sleep satisfaction, and persons with T1D reported diabetes-specific stressors on 14 consecutive days. Both couple members completed a survey that assessed relationship satisfaction. Multi-level models revealed significant within-person and between-person stress spillover and crossover effects. When examining the moderating role of sleep satisfaction, however, persons with T1D with better sleep satisfaction did not experience spillover between one domain and the other. Furthermore, partners with higher relationship satisfaction did not experience crossover between the persons with T1D diabetes-specific stressors and their general stressors. These findings support the conceptualization of the link between general and diabetes-specific stressors as both an intraindividual and a dyadic process among couples coping with T1D. In addition, better sleep satisfaction can prevent spillover effects, and relationship satisfaction can prevent stress crossover effects.
Keywords: diabetes, sleep satisfaction, stress crossover, stress spillover, relationship satisfaction
Type 1 diabetes (T1D) is an autoimmune disease resulting from the immune destruction of insulin-producing beta-cells in the pancreas that requires daily self-management to mimic a functioning pancreas. Everyday life with T1D involves checking blood glucose levels, monitoring blood glucose levels, injecting insulin, and monitoring diet and exercise (Chiang, Kirkman, Laffel, & Peters, 2014). Persons with T1D experience daily stress related to their diabetes management (e.g., frustration with a low blood glucose) and more general stress, including routine challenges of day-to-day living unrelated to diabetes management, such as stressors at work and interpersonal conflicts. These daily general stressors have proximal and long-term effects on well-being (Charles, Piazza, Mogle, Sljwinski, & Almeida, 2013). Moreover, for persons with diabetes, daily general stressors may compete with time and energy to manage diabetes effectively. This transmission between general stressors and diabetes-specific stressors in the daily life of a person with T1D is an intraindividual phenomenon referred to as stress spillover (Bolger, DeLongis, Kessler, & Wethington, 1989).
Managing stress is not only an individual phenomenon but is also an interpersonal process (Helgeson et al., 2019). In the context of a romantic relationship, the stress experiences of the person with an illness and those of the romantic partner may be associated with one another. This is referred to as stress crossover (Bolger et al., 1989). For couples coping with T1D, the types of stressors that crossover may include both general stressors and more diabetes-specific stressors. Despite the potential for spillover and crossover stress processes, little is known about whether spillover stress processes occur between general stressors and diabetes-specific stressors or whether these diabetes and general stressors transmit between the person with T1D and the romantic partner.
Previous stress spillover and crossover literature has mainly focused on work-life stressors (e.g., Carlson, Thompson, & Kacmar, 2019; Lawson, Sun, & McHale, 2019; Zhang, Foley, & Yang, 2013), with relatively few studies focused on couples or families coping with chronic illnesses (e.g., Yorgason, Roper, Sandberg, & Berg, 2012). In addition, most studies on stress spillover and crossover have examined individual differences (between-person associations) in stress spillover and crossover processes (e.g., Wang, Jex, Peng, Liu, & Wang, 2019; Zemp, Nussbeck, Cummings, & Bodenmann, 2017). For example, one cross-sectional study examined individual differences in work-life spillover and crossover effects into family life and found that individuals with higher workaholism were less likely than those with lower workaholism to report that they provided support to their partners due to work-life conflict (Bakker, Demerouti, & Burke, 2009). Few studies have focused on intraindividual variability (within-person associations). One such study found that relationship quality was best on days when female partners in Chinese dual-earning couples reported a high level of external stress and a high level of partner support (e.g., Hilpert et al., 2018).
Stress spillover and crossover in daily life are likely to vary over time in the context of couples coping with T1D, given the daily nature of the tasks required for successful diabetes management. Daily diary approaches can capture this fluctuation by examining the link between general and diabetes-specific stressors on the same day by measuring both over a series of consecutive days. In addition, daily diary approaches allow for differentiating within-person and between-person effects of daily stressors (Boker & Nesselroade, 2002). In examining spillover, we can determine whether one experiences a greater number of diabetes-specific stressors when one also has more general stressors on a given day (within-person [WP] effect). We can also examine whether individuals who experience more general stressors than the average person also have a greater number of diabetes-specific stressors than the average person (between-person [BP] effect). Distinguishing within- and between-person effects can provide a more precise and complete understanding of how couples with T1D experience stress spillover and crossover processes (Hilpert et al., 2018).
General stressors of persons with T1D may be associated with their diabetes-specific stressors in everyday life. Among persons with T1D, the added effects of general life stressors and diabetes-specific stressors may place high demands on their daily management (Chao et al., 2016). Experiencing more stressors has been linked with physiological processes (e.g., Marcovecchio & Chiarelli, 2012), which may be linked with diabetes-specific stressors, like a high blood glucose reading. In addition, greater stress is associated with lower engagement in self-care behaviors (Hilliard et al., 2016). For example, persons with T1D who are busy at work or parenting children may struggle to find the time required for timely and proper diabetes management. As such, they might experience hypo- or hyperglycemia. However, we know little about how general stressors are associated with diabetes-specific stressors or stress spillover.
Furthermore, little is known about how adults manage their disease in the context of couple relationships, one of the main sources of support in adulthood (e.g., Helgeson et al., 2019). An extensive literature demonstrates the importance of the social context in childhood and adolescence (Berg et al., 2017; Sparud-Lundin & Hallström, 2016), but less is known about the effects of the social context among adults with T1D. When managing diabetes in the context of a romantic relationship, T1D participants’ general stressors may be associated with their partner’s general stressors. In addition, T1D participants’ diabetes-specific stressors may also be contagious to the partner’s general stressors. Utilizing dyadic data from both persons with T1D and partners allows for examining stress crossover processes.
Individuals may be more or less susceptible to stress spillover and crossover effects because of other factors. Sleep is an especially important factor that may affect how resilient an individual is to stress spillover and crossover. Sleep is a complex and dynamic process that is essential for good health and well-being (e.g., Barber & Munz, 2011). Sleep researchers have extensively examined the link between sleep and stress and found that sleep quality has either positive or negative effects on stressful experiences by affecting emotional, cognitive, and physiological responses to stressors (e.g., Chambers, 2017; Poryazova, Werth, Bassetti, & Khatami, 2009; Prehn-Kristensen et al., 2018; Xie et al., 2013). For example, Tracy et al (2019) found in the present sample that individuals experience a lower number of both general and diabetes-specific stressors when they have better sleep satisfaction. Therefore, higher sleep satisfaction, defined in this study as an individual’s overall perceived satisfaction with sleep (Hall, 2010), may buffer stress spillover and crossover effects, and lower sleep satisfaction may exacerbate those effects.
Furthermore, individuals may be more or less influenced by stress spillover and crossover effects, particularly in the context of coping with T1D health stressors, because of interpersonal factors such as relationship satisfaction. Because relationship satisfaction has been associated with the management of marital conflicts and dyadic coping strategies (Bodenmann, Pihet, & Kayser, 2006; Li et al., 2018), relationship satisfaction may play a role in the stress process. Previous research has shown that the crossover effects of stressors between romantic partners are associated with poorer relationship satisfaction (Buck & Neff, 2012; Neff & Karney, 2007, 2009). In addition, previous research found that high relationship satisfaction buffered the negative effects of various types of emotional strain among young pregnant couples (Røsand, Slinning, Eberhard-Gran, Røysamb, & Tambs, 2012). Alternatively, previous research based on older individuals suggests that those with better relationship satisfaction might be more vulnerable to stress crossover effects between two romantic partners (Monin, Levy, & Kane, 2017). The explanation for this finding has to do with emotional contagion or interdependence (Hatfiled, Cacioppo, & Rapson, 1994); that is, happier couples may be more in tune with their partners’ stressors and feel stressed as a result. That is, good relationship satisfaction may exacerbate stress crossover effects among couples coping with T1D. Thus, further research is required to examine the role of relationship satisfaction, particularly in the context of couples coping with T1D.
In the current study, we examined daily stress spillover between general and diabetes-specific stressors and stress crossover between persons with T1D and their partners (for both general stressors and diabetes-specific stressors from persons with T1D and partners’ general stressors). Persons with T1D and their partners completed a 14-day diary where they reported their experiences of general stressors and daily sleep satisfaction, and persons with T1D reported diabetes-specific stressors. Persons with T1D and their partners also completed a survey that assessed relationship satisfaction. For spillover effects, we hypothesized that when persons with T1D reported a greater number of general stressors, they also would report a greater number of diabetes-specific stressors at WP and BP levels. For crossover effects, we hypothesized that when persons with T1D reported a greater number of daily general stressors, partners would also report a greater number of daily general stressors at both WP and BP levels. We also hypothesized that when persons with T1D reported a greater number of daily diabetes-specific stressors, partners would also report a greater number of daily general stressors at WP and BP levels. For the moderating role of sleep satisfaction, we hypothesized that better average daily sleep satisfaction would buffer spillover and crossover effects of daily stressors. For the role of relationship satisfaction, we did not specifically hypothesize whether relationship satisfaction would exacerbate or buffer spillover and crossover effects of daily stressors, as couples with higher relationship satisfaction could resolve the stressors and conflict better or be more influenced by their partner’s stressors due to emotional contagion.
In all analyses, we first examined concurrent (same-day) associations. Then we examined lagged associations by controlling for the previous day’s dependent variable. In the lagged analyses, we were able to examine bidirectional associations for stress spillover and crossover; that is, for example, whether previous day’s general stressors of persons with T1D is linked to spouses’ general stressors the following day and whether previous day’s general stressors of spouses is linked to general stressors of persons with T1D the following day.
Method
Participants
All study procedures were approved by each of the two university’s institutional review boards. Persons with T1D and their partners provided written informed consent. Persons with T1D were recruited from participating endocrinology clinics at the University of Utah Diabetes & Endocrinology Center (UDC) and St. Mark’s Hospital in Salt Lake City and University of Pittsburgh Medical Center (UPMC) and the University of Pittsburgh Pitt+Me research registry in Pittsburgh. Individuals were eligible if they had a diagnosis of T1D for at least one year, were taking insulin for T1D within one year of diagnosis, spoke English as their primary language (necessary for cognitive testing as part of the larger study), and were married or in a cohabiting relationship for at least one year. At the Utah sites, of the 319 persons with T1D approached, 66 were ineligible, and 118 declined to participate. Of the remaining 135 couples, 107 were scheduled and included in the study. At the Pittsburgh sites, of the 202 contacted by the project director, 47 were ineligible (including two found ineligible after they started study procedures), 57 declined participation, and six could not be reached, resulting in 92 couples included in the study. The final sample included 199 couples (398 individuals) who were eligible, enrolled, and completed study measures across both sites. Couples were primarily heterosexual (n = 193), with three female same-sex and three male same-sex couples. The average length of diagnosis was 26.97 years old (SD = 13.88, range from 3.10 to 60.63 years). Around 71% of persons with T1D and around 78% of partners worked full or part-time. Demographic data for persons with T1D and partners are shown in Table 1.
Table 1.
Demographic information for persons with T1D and partners
| Persons with T1D | Partners | |||
|---|---|---|---|---|
| M (SD) | Range | M (SD.) | Range | |
| Age | 46.82(13.95) | 25.85–74.89 | 46.40(14.17) | 23.92–76.70 |
| Gender (% Women) | 52.3% | -- | 47.2% | -- |
| Race (%White) | 92.5% | -- | 94% | -- |
| Ethnicity (% Hispanic) | 6% | -- | 3% | -- |
| Daily Sleep Satisfaction | 3.17(.60) | 1.75–4.93 | 3.09(4.85) | 1–4.85 |
| Length of Diagnosis | 26.97(13.88) | 3.10–60.63 | -- | -- |
| Pump Use (%) | 68.7% | -- | -- | -- |
| CGM Use (%) | 43.4% | -- | -- | -- |
| HbA1c | 7.57(1.06) | 4.9–11.20 | -- | -- |
Procedure
At Site 1, trained recruiters approached persons with T1D who were at least 25 years of age in the clinic. Interested participants were provided information about the study (verbally and with a brochure) and were asked to provide their preferred contact information to discuss eligibility and enrollment. At Site two, persons with T1D were approached by their regular diabetes care provider because the recruiter at Site two was not affiliated with that clinic and, thus, could not obtain permission to release their name and contact information to the project coordinator. The diabetes care provider simply told persons with T1D that there was a research study and asked whether the recruiter could contact them to describe the study. The recruiter then contacted persons with T1D who agreed to be contacted and provided them with more information about the study, assessed interest in the study, and discussed eligibility and enrollment. If persons with T1D were eligible and interested in the study, the study team then obtained permission to independently contact their romantic partner for eligibility screening. If both members of a couple met study criteria and agreed to participate, the couple was enrolled in the study and scheduled for a laboratory visit.
Prior to attending the in-person laboratory session, persons with T1D and romantic partners provided informed consent for completing a brief at-home online questionnaire and provided informed consent for completing all other study procedures in oral and written form at the laboratory visit. During the laboratory visit, participants were instructed in how to complete a daily diary every evening before going to bed for 14 days as part of a larger study. The present study primarily uses measures from the daily diary. On average, persons with T1D completed 13.82 days (SD = .56), and partners completed an average 13.71 days of the diary (SD = .86).
Participants were compensated individually for their participation and for mileage for traveling to the laboratory. Persons with T1D were compensated up to $225 for completing all of the parts of the study ($100 for the initial survey and lab-assessment, $7.14 per diary day completed up to $100, and $25 for returning a study-owned glucometer in a pre-paid/pre-addressed envelope), with partners compensated similarly with the exception of the glucometer data.
Measures
Daily diabetes-specific stressors.
Persons with T1D completed a brief checklist (1 = yes, 0 = no) where they indicated the presence of six or seven common daily diabetes-specific stressors: problem with high blood sugar, low blood sugar, forget or skip a blood glucose test, take the wrong amount of insulin, feel bad (upset, angry, sad) because of your diabetes, difficulties with your diet, and, problem with your equipment used to monitor diabetes (if they were using a pump or continuous glucose monitor). This measure has been used previously in adolescents and emerging adult samples with T1D (Berg et al., 2013) and is based on empirically-derived coding of T1D participants’ descriptions of diabetes-specific stressors (Beveridge, Berg, Wiebe, & Palmer, 2006). Because individuals utilizing pumps or CGMs were presented with an additional stressor, the daily measure of diabetes-specific stressors reflected a proportional count of daily stressors endorsed per day (out of 6 or 7, depending on whether they used equipment). Persons with T1D, on average, reported .25 diabetes-specific stressors each day (SD = .22). For approximately 27 % of the days, participants reported no diabetes-specific stressors.
Daily general stressors.
Both persons with T1D and partners indicated the presence of four general daily stressors (1 = yes, 0 = no; e.g., argument or disagreement with someone, stressors at work, stressors at home, have something bad happen to a relative or close friend) which were drawn from the Daily Inventory of Stressful Events in a U.S. national sample of adults, aged 25 to 74. These are four of the most common general stressors from this U.S. national sample of adults (Almeida, Wethington, & Kessler, 2002). Qualitative analyses of the stressors by adults in this study also support these four types of stressors (Kelly et al., under review). This daily measure of general stressors reflected a proportional count of stressors endorsed. Persons with T1D reported an average of .15 (SD = .21) general stressors, and partners reported an average of .15 (SD = .20) general stressors. For approximately 57% of the days, persons with T1D and partners reported no general stressors.
Spouse as a source of general stressors.
Some of the general stressors, in particular argument or conflict could have occurred with the spouse, thereby confounding a spillover effect with general stressors. To address this issue, we included a covariate (“spouse was a source of general stressors”) from a qualitative item in the larger study. This covariate comes from data where participants were asked to briefly describe stressful events that occurred throughout the day (diabetes specific or general) and open-ended responses were coded for the presence or absence of specific qualitative codes (e.g., whether an event occurred; if the event involved diabetes; if a person or persons was the source of the stress; and the specific characteristics of the event). We created a variable from this coding to determine if the spouse, in particular, was mentioned as the source of a general stressor event on that day (1 = spouse was the source of stress; 0 = no spousal involvement in stressful event). This variable was then included as a covariate in our analyses to more definitively understand whether any effects observed were crossover, compared to simply being an artifact of interpersonal stress.
Sleep satisfaction.
To capture daily sleep satisfaction, participants rated the prior night’s sleep using the following item: “How satisfied/dissatisfied were you with your sleep last night?” on a 1 (not at all satisfied) to 5 (completely satisfied) scale (Williams, Cribbet, Rau, Gunn, & Czajkowski, 2013). This item was modeled after a similar item on the Pittsburgh Sleep Quality Index (a longer, validated global self-report of sleep quality; Buysse, Reynolds, Monk, Berman, & Kupfer, 1989), with the wording changed to reflect the daily level. To create an individual difference variable, we aggregated daily sleep satisfaction to examine average sleep satisfaction over 14 days. On average, across the days of the diary, persons with T1D and partners reported they were somewhat satisfied with their sleep (M Persons with T1D = 3.17, SD = .98; M Partners = 3.09, SD = .98).
Relationship satisfaction.
Persons with T1D and partners completed a 16-item version of the Couples Satisfaction Index (CSI-16; Funk & Rogge, 2007), a measure of relationship satisfaction with excellent internal consistency (persons with T1D: α = .97; partners: α = .98) and convergent validity with other measures of relationship satisfaction. A sample item is, “How rewarding is your relationship with your partner?” CSI-16 scores can range from 0 to 81, with higher scores indicating higher levels of relationship satisfaction. CSI-16 scores falling below 51.5 indicate significant relationship dissatisfaction. In our sample, the average satisfaction score was 65.74 (SD = 14.27) for persons with T1D and 63.93 (SD = 15.06) for partners with 15.6 % of persons with type 1 diabetes scoring below 51.5 and 18.1% of partners scoring below 51.5.
Analytic Strategy
The present study utilized multi-level models (Raudenbush & Bryk, 2001) in IBM SPSS Mixed (version 25; 2017) to account for the fact that diary days were nested within individuals and individuals were nested within couples. We employed a two-level multi-level model to address the study’s central questions. We separated the within-person, and between-person variability by group (person) means centering at Level 1 and grand mean centering at Level 2 (Hoffman, 2015; Hoffman & Stawski, 2009). Modeling within- and between-person variability decomposes the effect of individuals’ and their partners’ day-to-day fluctuations in the constructs of interest while accounting for between-person (individual) differences in these constructs (Bolger & Laurenceau, 2013). For instance, the models that examined the effect of T1D participants’ daily diabetes-specific stressors on partners’ daily general stressors allowed for the separation of the effect of T1D participants’ day-to-day fluctuations in daily diabetes-specific stressors while accounting for between-person differences in daily diabetes-specific stressors (i.e., average levels of T1D participants’ diabetes-specific stressors across the 14 days) on the intercept of partners’ daily general stressors. Day of the daily diary was included in all models. Random effects were allowed on the intercept.
First, we ran unconditional models to calculate intraclass correlation coefficients (ICCs) and examine within- and between-person variability in daily stressors across the 14 diary days. Second, for analyses of spillover, the predictor variable was general stressors of persons with T1D (both BP and WP), and the dependent variable was their diabetes-specific stressors. Third, for analyses of crossover, we first examined the predictor variable of persons with T1Ds’ general stressors (both WP and BP) and the dependent variable of partners’ general stressors. A similar analysis was examined for persons with T1Ds’ diabetes-specific stressors and the dependent variable of partners’ general stressors.
Finally, we were interested to know whether sleep satisfaction or relationship satisfaction in general (BP) moderated the association between self- and partner-stressors. Predictor variables included T1D participants’ daily stressors (both WP and BP), two moderators, sleep satisfaction and relationship satisfaction, and interaction effects between daily WP stressor and each of the two BP moderators (i.e., two cross-level interactions) in the same model. The length of diagnosis was included as a covariate for all analyses. To examine the moderating role of individual differences in sleep satisfaction, we aggregated daily sleep satisfaction over the 14 days. For the two moderating variables, sleep satisfaction and relationship satisfaction; we included the variable that was connected to those who are affected by spillover and crossover of stressors. For example, when examining spillover we used the person with T1D’s sleep satisfaction and relationship satisfaction, but when examining crossover from general stressors of persons with T1D to partners’ general stressors, we used the partner’s sleep satisfaction and relationship satisfaction. We also examined the sleep satisfaction at the daily level as a moderator. We found no significant within-person effects of sleep satisfaction and stressors; thus, we did not include within-person interaction between sleep satisfactionof stressor.
Furthermore, we examined bidirectional lagged associations in all analyses by controlling for the previous day’s dependent variable. For example, first, for analyses of spillover, we analyzed prior day’s general stressors of persons with T1D (both BP and WP) predicting their diabetes-specific stressors the following day, controlling for prior day’s diabetes-specific stressors. Then, in order to rule out the reverse direction of effects that daily diabetes-specific stressors affect general stressors the following day, we analyzed prior day’s diabetes-specific stressors predicting general stressors the following day, controlling for prior day’s general stressors.
Results
Variance Partitioning
To examine within- versus between-person variance in outcomes, we calculated intraclass correlation coefficients (ICCs) from variance estimates obtained from unconditional (empty) models. ICCs indicated that there was both within- and between-person variability in measures of daily diabetes-specific stressors (64.27% within; 35.73% between), and daily general stressors (84.92% within; 15.08% between for persons with T1D; 82.49% within; 17.51% between for partners).
Concurrent (Same-day) Spillover Effects of Daily Stressors in Persons with T1D
We found significant spillover effects of stressors between T1D participants’ general stressors and their diabetes-specific stressors. As shown in the top third of Table 2, on days when persons with T1D reported more general stressors than usual, they also reported more diabetes-specific stressors (WP). In addition, persons with T1D who reported more general stressors on average than others also reported more diabetes-specific stressors than others (BP).
Table 2.
Spillover effects and crossover effects of daily stressors
| 1. Spillover effects between T1D participants’ GS and their DS. | ||
|---|---|---|
| Dependent variable: T1D participants’ DS | b (SE) | t |
| Intercept | .29(.02) | 16.57*** |
| Day | −.002(.001) | −2.03* |
| Persons’ with T1D GS wp | .06(.02) | 3.40** |
| Persons’ with T1D GS bp | .77(.08) | 9.65*** |
| Length of Diagnosis bP | −.001(.001) | −2.40* |
| 2. Crossover effects between T1D participants’ GS and partners’ GS. | ||
| Dependent variable: Partners’ GS | b (SE) | t |
| Intercept | .13(.02) | 8.05*** |
| Day | −.01(.001) | −6.04*** |
| Persons’ with T1D GS wp | .19(.03) | 7.09*** |
| Persons’ with T1D GS bp | .01(.07) | .13 |
| Spouse as a source of stress wp | .07(.02) | 4.49*** |
| Length of Diagnosis bp | .001(.001) | 1.09 |
| 3. Crossover effects between T1D participants’ DS and partners’ GS | ||
| Dependent variable: Partners’ GS | b (SE) | t |
| Intercept | .13(.01) | 9.13*** |
| Day | −.01(.001) | −8.48*** |
| Persons’ with T1D DS wp | .01(.02) | .32 |
| Persons’ with TID DS bp | .11(.05) | 2.23* |
| Length of Diagnosis bp | .001(.0005) | 1.34 |
Note. wp = within-person. bp = between-person. DS= diabetes-specific stressors. GS= general stressors. Table reports unstandardized coefficients (b) with standard errors (SE) in parentheses.
p < .05,
p < .01,
p < .001
We found that sleep satisfaction moderated the spillover effects between daily general stressors and daily diabetes-specific stressors (see the top third of Table 3 for full model results). That is, persons with T1D with lower sleep satisfaction experienced spillover between their general stressors and their diabetes-specific stressors (b=.12, z=4.52, p < .001), but those with higher sleep satisfaction did not experience spillover of daily stressors (b=−.001, z=.02, p = .98) (see Figure 1a).
Table 3.
Individual Differences of sleep satisfaction and relationship satisfaction as moderators for spillover and crossover effects of daily stressors
| 1. Sleep satisfaction and relationship satisfaction as moderators for spillover effects between T1D participants’ GS and their DS. | ||
|---|---|---|
| Dependent variable: T1D participants’ DS | b (SE) | t |
| Intercept | .29(.02) | 16.36*** |
| Day | −.002(.001) | −1.99* |
| T1D participants’ GS wp | .06(.02) | 3.09** |
| T1D participants’ GS wp x T1D participants’ sleep satisfaction bp | −.10(.03) | −2.87** |
| T1D participants’ GS wp x T1D participants’ relationship satisfaction bP | .001(.001) | .51 |
| T1D participants’ GS bp | .77(.08) | 9.32*** |
| T1D participants’ sleep satisfaction bp | −.02(.01) | −1.29 |
| T1D participants’ relationship satisfaction bp | .0005(.001) | .87 |
| Length of Diagnosis bp | −.001(.001) | −2.19* |
| 2. Sleep satisfaction and relationship satisfaction as moderators for crossover effects between T1D participants’ GS and partners’ GS. | ||
| Dependent variable: Partners’ GS | b (SE) | t |
| Intercept | .14(.02) | 8.64*** |
| Day | −.01(.001) | −5.96*** |
| T1D participants’ GS wp | .19(.03) | 7.01*** |
| Spouse as a source of stress wp | .06(.02) | 4.13*** |
| Length of Diagnosis bp | .0004(.001) | .75 |
| T1D participants’ GS wp x Partners’ sleep satisfaction bp | −.06(.04) | −1.42 |
| T1D participants’GS wp x Partners’relationship satisfaction bp | .0003(.002) | .15 |
| T1D participants’ GS bp | −.01(.07) | −.12 |
| Partners’ sleep satisfaction bp | −.02(.01) | −1.32 |
| Partners’ relationship satisfaction bp | −.001(.0005) | −2.76** |
| 3. Sleep satisfaction and relationship satisfaction as moderators for crossover effects between T1D participants’ DS and partners’ GS. | ||
| Dependent variable: Partners’ GS | b (SE) | t |
| Intercept | .14(.01) | 9.84*** |
| Day | −.01(.001) | −8.56*** |
| T1D participants’ DS wp | .01(.02) | .38 |
| T1D participants’ DS wp x Partners’ sleep satisfaction bp | .03(.04) | .73 |
| T1D participants’ DS wp x Partners’ relationship satisfaction bp | −.004(.002) | −2.59* |
| T1D participants’ DS bp | .09(.05) | 1.99* |
| Partners’ sleep satisfaction bp | −.03(.01) | −2.82** |
| Partners’ relationship satisfaction bp | −.001(.0004) | −3.06** |
| Length of Diagnosis | .001 (.0005) | 1.08 |
Note. wp = within-person. bp = between-person. DS.: diabetes-specific stressors. GS.: general stressors. Table reports unstandardized coefficients (b) with standard errors (SE) in parentheses.
p < .05,
p < .01,
p < .001
Figure 1a.
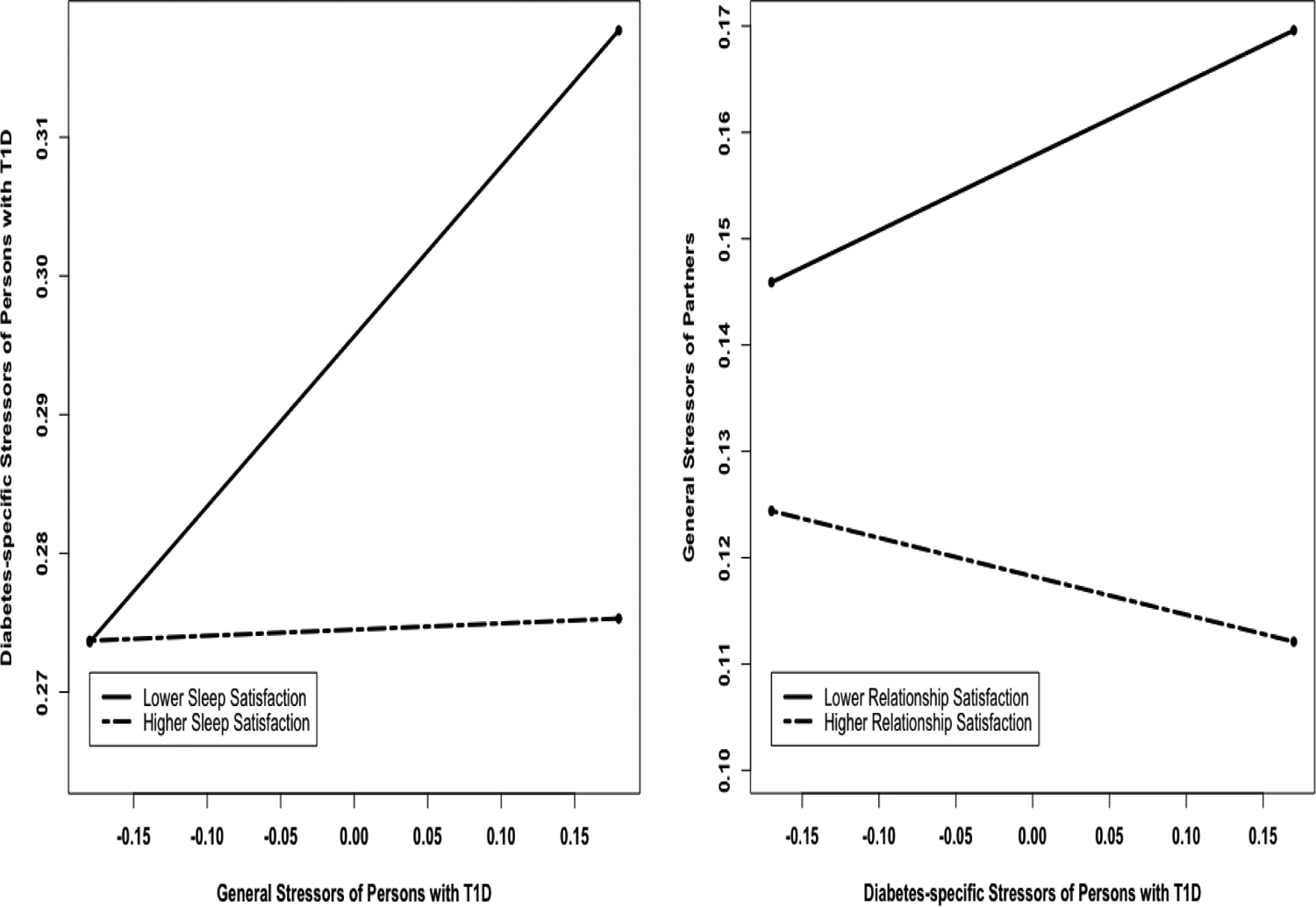
Spillover effects of T1D participants’ daily general stressors on T1D participants’ daily diabetes-specific stressors moderated by T1D participants’ sleep satisfaction (left). Figure 1b. Crossover effect of T1D participants’ daily diabetes-specific stressors on partners’ daily general stressors moderated by partners’ relationship satisfaction (right).
We did not find that relationship satisfaction moderated the spillover effects between daily general stressors and daily diabetes-specific stressors.
Concurrent (Same-Day) Crossover Effects of Daily General Stressors
We found significant crossover effects of stressors in the context of general stressors between persons with T1D and partners. On days when persons with T1D reported more general stressors than average, partners also reported more general stressors (WP). However, the BP effect was not significant. (See middle third of Table 2 for full model results). Neither sleep satisfaction nor relationship satisfaction moderated the crossover effects of persons with T1D general stressors and partners general stressors. (See middle third of Table 3 for full model results.)
Concurrent (Same-Day) Crossover Effects of Daily Diabetes- Specific Stressors to General Stressors
We found a significant crossover effect such that persons with T1D who reported more diabetes-specific stressors than others on average had partners who also reported more general stressors (BP). However, the WP effect was not significant. (See bottom third of Table 3 for full model results.)
We found that relationship satisfaction moderated the crossover effects between diabetes-specific stressors of persons with T1D and general stressors of partners (see bottom third of Table 3 for full model results.) Partners with lower relationship satisfaction experienced crossover between T1D participants’ diabetes-specific stressors and partners’ general stressors (b=.07, z=2,13, p = .03), but those with higher relationship satisfaction did not experience crossover (b=−.05, z=−1.65, p = .10) (see Figure 1b). We did not find that sleep satisfaction moderated crossover effects between T1D participants’ daily diabetes-specific stressors and partners’ general stressors.
Lagged Associations of Spillover and Crossover
There were no significant lagged effects for stress spillover (i.e., positive association between diabetes stressors of persons with T1D and their general stressors) or stress crossover (i.e., positive association between stressors for both diabetes stressors and general stressors). There also were not significant lagged effects for spillover or crossover when moderating variables were included in the models. See Supplemental Tables S1 and S2 for full model results.
Discussion
This study contributes to the stress spillover and crossover literature by examining both within-person and between-person associations using a daily diary method. Consistent with previous research on work-family spillover (Hilpert et al., 2018; van Steenbergen, Kluwer, & Karney, 2011; Wang et al., 2019; Zemp et al., 2017), we found spillover and crossover effects of stressors among couples with T1D. These findings support the conceptualization of the link of T1D participants’ general stressors and diabetes-specific stressors to partners’ general stressors as both an intraindividual process and interpersonal process among couples coping with T1D.
We found both significant intraindividual variability and individual differences in stress spillover among persons with T1D by focusing on general stressors and diabetes-specific stressors in the context of managing chronic illness. Given that personal resources, such as time and energy are limited (Greenhaus, Collins, & Shaw, 2003), dealing with one domain of stressors may compete with the time and energy that it takes to cope with the other domain of stressors. Persons with T1D can benefit from reducing their stress in other domains of life in order to deal with their diabetes-specific stressors. For example, when a person with T1D experiences more stressors at work than usual, the person may miss the opportunity to manage their diabetes or may be overwhelmed and less motivated to manage diabetes, resulting in the experience of more diabetes-specific stressors on that day. Regarding individual differences in stress spillover, persons with T1D who have higher caregiving or parenting responsibilities than other people, for example, might experience more interference with diabetes management on average because caregiving or parenting responsibilities and diabetes may need to be handled simultaneously. Qualitative analyses of the stressors experienced by adults in this study indicate that other domains of life frequently interfere with the management of diabetes stressors (Kelly et al., under review).
This study also points to the important dyadic nature of daily stressors among couples coping with T1D. In particular, the current research extends the limited body of research on stress spillover and crossover in the context of managing chronic illnesses (Yorgason et al., 2012) between persons with T1D and partners. We revealed daily crossover effects in the general stressors between persons with T1D and partners. That is, when persons with diabetes experienced general stressors, their partners also experienced general stressors.
We predicted stress would exhibit both within- and between-person spillover and crossover effects. We found both within-person and between-person effects for stress spillover, but only within-person effects for crossover effects of general stressors of persons with T1D to their spouses’ general stressors It is possible that controlling for “spouses as a source of stressors” accounted for between-person variance of the crossover between the general stressors of persons with T1D and those of spouses. That is, spouses as a source of stressors could be operating as an individual difference variable in these analyses. Furthermore, we only found between-person effects for crossover effects of diabetes stressors of persons with T1D to spouses’ general stressors. It is possible that spouses are only aware at a general level of the diabetes stressors that persons with T1D are experiencing and may be less aware of the daily variation in diabetes stressors.
A significant contribution of the present study was to explore potential protective or risk factors of stress spillover and crossover effects. First, as we expected, sleep satisfaction moderated the spillover effects such that spillover effects within persons with T1D, an intraindividual process, may be prevented by better sleep satisfaction. The present finding is consistent with earlier work demonstrating that higher sleep satisfaction has been linked to better emotion regulation, which may, in turn, be associated with stress management directly (Tavernier & Willoughby, 2015).
In addition, as we mentioned above, relationship satisfaction moderated the crossover effects between diabetes-specific stressors of persons with T1D and partners’ general stressors. This finding implies that relationship satisfaction is more critical than sleep satisfaction to moderate crossover effects, potentially due to the interpersonal nature of the crossover. Furthermore, our results suggest higher relationship satisfaction can be a protective factor against transmitting stressors between persons with T1D and partner. Couples with higher relationship satisfaction may have better individual and dyadic coping strategies and resources as well as better marital conflict resolution skills so that they are not vulnerable to the stress crossover effects (Bodenmann et al., 2006; Li et al., 2018). This finding is consistent with Røsand et al. (2012), who found that relationship satisfaction can play a protective role in crossover effects for young pregnant couples. All in all, relationship satisfaction may be an important consideration for couples in which one partner is managing a chronic illness such as T1D.
We found both concurrent (same-day) within-person and between-person spillover and crossover effects, but we did not find any lagged associations of spillover and crossover. Several potential explanations exist for why fluctuations of the prior day’s stressors did not affect stressors the following day. Daily diary data were collected at the end of each day for 14 consecutive days. The effects of stressful events may have been resolved across the day so that they did not last until the following day, and therefore did not affect daily stressful events the following day. Future research would benefit from measuring daily stress multiple times per day to obtain a more fine-grained level of stress spillover and crossover effects. Furthermore, future research should consider measuring the intensity of daily stressors and coping strategies of stressors and resources to obtain a more complete understanding of stress spillover and crossover effects.
The results should be interpreted in the context of some limitations. First, we cannot make any causal claims. Our spillover and crossover effects are same-day associations, thus we do not know whether general stressors lead to diabetes stressors or diabetes stressors lead to general stressors. Furthermore, our lagged analyses did little to clarify directionality. Second, the generalizability of our sample is limited to individuals from more advantaged populations. Though type 1 diabetes is more prevalent among non-Hispanic Whites, our sample did not reflect national distributions of individuals of different ethnicities. Additionally, our sample comprised individuals with higher socioeconomic status who were near recommended target levels of HbA1c. We did not specifically recruit for heterosexual couples, but most of our participants were in heterosexual relationships. Our results also may not generalize to populations who are experiencing more significant stress or are in lower quality relationships. Finally, regarding our measure of general stressors, one of the stressors included work stressors. This category of stressor was likely not equally relevant across individuals as not all participants worked, especially older participants. In the future, researchers may need to account for whether stressors are developmentally appropriate to the time of the life-span.
These findings hold some useful clinical implications. First, findings highlight that couples in which one partner has a chronic illness may benefit from interventions targeting stress reduction, to prevent spillover between general stressors and diabetes-specific stressors. In addition, the results also suggest that persons with T1D may benefit from interventions to improve sleep satisfaction and stress in order to prevent spillover between one domain and the other. Currently, there are no recommendations for screening for sleep problems in persons with T1D. Routine sleep screening would identify specific types of sleep diagnosis, and factors that can influence sleep satisfaction, such as nocturnal hypoglycemia, sleep apnea, anxiety, and depression, and subsequently, a treatment plan could be identified. It is also recommended that family members are involved in this assessment (Young-Hyman et al., 2016). To prevent crossover between persons with T1D and partners, healthcare providers caring for partners can use these findings to increase their awareness of the fact that good relationship satisfaction can prevent crossover between diabetes-specific stressors of persons with T1D and general stressors of partners and involve partners in the intervention. Family counseling may be necessary when stress crossover to the persons with T1D partner is present (American Diabetes Association, 2017).
This study showed that when persons with T1D experience daily general stressors, they also experience more diabetes stressors, a process we referred to as stress spillover. This study also suggested that the general and diabetes-specific stressors that persons with T1D face may be transmitted to partners’ experience of daily stressors, a process referred to as stress crossover. The current study addressed limitations from previous research, by capturing both intraindividual variability in spillover and crossover effects and individual differences in spillover and crossover effects. These results indicated that sleep satisfaction and relationship satisfaction might be important factors in preventing stress spillover and crossover processes, respectively. This study provides a foundation for future longitudinal research on couples coping with T1D to understand the long-term consequences of health and well-being of daily stress spillover and crossover effects.
Supplementary Material
Acknowledgements:
The study was funded by the National Institutes of Health DP3 DK103999
Footnotes
Author’s note: Part of this study was presented at the Society of Behavioral Medicine in 2019.
Contributor Information
Eunjin Lee Tracy, University of Pittsburgh School of Medicine, Department of Psychiatry
Cynthia A. Berg, University of Utah, Department of Psychology
Caitlin S. Kelly, University of Utah, Department of Psychology
Robert G. Kent de Grey, University of Utah, Department of Psychology
Michelle L. Litchman, University of Utah, College of Nursing
Nancy A. Allen, University of Utah, College of Nursing
Vicki S. Helgeson, Carnegie Mellon University, Department of Psychology
References
- Almeida DM, Wethington E, & Kessler RC (2002). The daily inventory of stressful events: an interview-based approach for measuring daily stressors. Assessment, 9, 41–55. [DOI] [PubMed] [Google Scholar]
- American Diabetes Association. (2017). Lifestyle management. Sec. 4. In Standards of Medical Care in Diabetes. Diabetes Care, 40(Suppl. 1):S33–S43 [DOI] [PubMed] [Google Scholar]
- Bakker AB, Demerouti E, & Burke R (2009). Workaholism and relationship quality: a spillover-crossover perspective. Journal of Occupational Health Psychology, 14, 23–33. [DOI] [PubMed] [Google Scholar]
- Barber LK, & Munz DC (2011). Consistent-sufficient sleep predicts improvements in self regulatory performance and psychological strain. Stress and Health: Journal of the International Society for the Investigation of Stress, 27, 314–324. [Google Scholar]
- Berg CA, Butner J, Butler JM, King PS, Hughes AE, & Wiebe DJ (2013). Parental persuasive strategies in the face of daily problems in adolescent T1D management. Health Psychology, 32, 719–728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg CA, Butner J, Wiebe DJ, Hughes AE, Osborn P, King PS, Palmer DL, & Butler JM (2017). Developmental model of parent-child coordination for selfregulation in type 1 diabetes management across childhood and into emerging adulthood. Developmental Review, 46, 1–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beveridge RM, Berg CA, Wiebe DJ, & Palmer DA (2006). Mother and Adolescent Representations of Illness Ownership and Stressful Events Surrounding Diabetes. Journal of Pediatric Psychology, 31, 818–827. [DOI] [PubMed] [Google Scholar]
- Bodenmann G, Pihet S, & Kayser K (2006). The relationship between dyadic coping and marital quality: A 2-year longitudinal study. Journal of Family Psychology, 20, 485–493. [DOI] [PubMed] [Google Scholar]
- Boker SM, & Nesselroade JR (2002). A method for modeling the intrinsic dynamics of intraindividual variability: Recovering the parameters of simulated oscillators in multi wave panel data. Multivariate Behavioral Research, 37, 127–160. [DOI] [PubMed] [Google Scholar]
- Bolger N, DeLongis A, Kessler RC, & Wethington E (1989). The contagion of stress across multiple roles. Journal of Marriage and the Family, 51, 175–183. [Google Scholar]
- Bolger N, & Laurenceau J-P (2013). Intensive longitudinal methods. New York, NY: Guilford Press. [Google Scholar]
- Buck AA, & Neff LA (2012). Stress spillover in early marriage: The role of self-regulatory depletion. Journal of Family Psychology, 26, 698–708. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds C 3., Monk TH, Berman SR, & Kupfer DJ (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 28, 193–213. [DOI] [PubMed] [Google Scholar]
- Carlson DS, Thompson MJ, & Kacmar KM (2019). Double crossed: The spillover and crossover effects of work demands on work outcomes through the family. Journal of Applied Psychology, 104, 214–228. [DOI] [PubMed] [Google Scholar]
- Chambers AM (2017). The role of sleep in cognitive processing: focusing on memory consolidation. Wiley Interdisciplinary Reviews. Cognitive Science, 8, 1–14. [DOI] [PubMed] [Google Scholar]
- Chao AM, Minges KE, Park C, Dumser S, Murphy KM, Grey M, & Whittemore R (2016). General life and diabetes-related stressors in early adolescents with type 1 diabetes. Journal of Pediatric Health Care, 30, 133–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles ST, Piazza JR, Mogle J, Sliwinski MJ, & Almeida DM (2013). The Wear and Tear of Daily Stressors on Mental Health. Psychological Science (0956–7976), 24, 733–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiang Kirkman, M. S., Laffel LMB, & Peters AL (2014). Type 1 diabetes through the life span: A position statement of the American Diabetes Association. Diabetes Care, 37, 2034–2054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funk JL, & Rogge RD (2007). Testing the ruler with item response theory: Increasing precision of measurement for relationship quality with the Couples Satisfaction Index. Journal of Family Psychology, 21, 572–583. [DOI] [PubMed] [Google Scholar]
- Greenhaus JH, Collins KM, & Shaw JD (2003). The relation between work-family balance and quality of life. Journal of Vocational Behavior, 63(3), 510–531. [Google Scholar]
- Hall MH (2010). Behavioral medicine and sleep: Concepts, measures, and methods. In Steptoe A (Ed.). Handbook of behavioral medicine: Methods and applications (pp. 749–765). New York: Springer. [Google Scholar]
- Hatfiled E, Cacioppo JT, & Rapson RL (1994).Emotional contagion. New York, NY:Cambridge University Press [Google Scholar]
- Helgeson VS, Berg CA, Kelly CS, Vleet M, Zajdel M, Tracy EL, & Litchman ML (2019). Patient and partner illness appraisals and health among adults with type 1 diabetes. Journal of Behavioral Medicine. 42. 480–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilliard ME, Yi-Frazier JP, Hessler D, Butler AM, Anderson BJ, & Jaser S (2016). Stress and A1c among People with Diabetes across the Lifespan. Current Diabetes Reports, 16, 67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilpert P, Xu F, Milek A, Atkins DC, Bodenmann G, & Bradbury TN (2018). Couples coping with stress: Between-person differences and within-person processes. Journal of Family Psychology, 32, 366–374. [DOI] [PubMed] [Google Scholar]
- Hoffman L, & Stawski RS (2009). Persons as contexts: Evaluating between-person and within-person effects in longitudinal analysis. Research in Human Development, 6(2–3), 97–120. [Google Scholar]
- Hoffman L (2015). Longitudinal analysis: Modeling within-person fluctuation and change. New York, NY: Routledge. [Google Scholar]
- IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp. [Google Scholar]
- Kelly CS, Berg CA, Tracy EL, Staylor K, Mahoney S, & Helgeson VS (under review). The daily experience of type 1 diabetes-related stress across adulthood.
- Lawson KM, Sun X, & McHale SM (2019). Family-friendly for her, longer hours for him: Actor-partner model linking work-family environment to work-family interference. Journal of Family Psychology, 33, 444–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Cao H, Zhou N, Ju X, Lan J, Zhu Q, & Fang X (2018). Daily communication, conflict resolution, and marital quality in Chinese marriage: A three-wave, cross-lagged analysis. Journal of Family Psychology, 32, 733–742. [DOI] [PubMed] [Google Scholar]
- Marcovecchio ML, & Chiarelli F (2012). The effects of acute and chronic stress on diabetes control. Science Signaling, 5(247), pt10. [DOI] [PubMed] [Google Scholar]
- Monin JK, Levy BR, & Kane HS (2017). To Love is to Suffer: Older Adults’ Daily Emotional Contagion to Perceived Spousal Suffering. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 72(3), 383–387. 10.1093/geronb/gbv070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neff LA, & Karney BR (2007). Stress crossover in newlywed marriage: A longitudinal and dyadic perspective. Journal of Marriage and Family, 69, 594–607. [Google Scholar]
- Neff LA, & Karney BR (2009). Stress and reactivity to daily relationship experiences: How stress hinders adaptive processes in marriage. Journal of Personality and Social Psychology, 97, 435–450. [DOI] [PubMed] [Google Scholar]
- Poryazova R, Werth E, Bassetti CL, & Khatami R (2009). Hypersomnia, REM sleep fragmentation and loss of motivation in a patient with hypothalamic lesions. Sleep Medicine, 10, 812–813. [DOI] [PubMed] [Google Scholar]
- Prehn-Kristensen A, Böhmig A, Schult J, Pedersen A, Wiesner CD, & Baving L (2018). Does sleep help prevent forgetting rewarded memory representations in children and adults? Frontiers in Psychology, 9, 924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW & Bryk AS (2001). Hierarchical linear models: Applications and data analysis methods. Thousand Oaks, CA: Sage. [Google Scholar]
- Røsand G-MB, Slinning K, Eberhard-Gran M, Røysamb E, & Tambs K (2012). The buffering effect of relationship quality on emotional distress in couples. BMC Public Health, 12, 66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparud-Lundin C, & Hallström I (2016). Parents’ experiences of two different approaches to diabetes care in children newly diagnosed with T1D. Qualitative Health Research, 26, 1331–1340. [DOI] [PubMed] [Google Scholar]
- Tavernier R, & Willoughby T (2015). A longitudinal examination of the bidirectional association between sleep problems and social ties at university: The mediating role of emotion regulation. Journal of Youth and Adolescence, 44, 317–330. [DOI] [PubMed] [Google Scholar]
- Tracy EL, Berg CA, Baucom KJW, Turner SL, Kelly C, Van Vleet M, Butner J, & Helgeson VS (2019). Daily sleep quality and daily stressors in couples coping with Type 1 Diabetes. Health Psychology. 38, 75–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Steenbergen EF, Kluwer ES, & Karney BR (2011). Workload and the trajectory of marital satisfaction in newlyweds: Job satisfaction, gender, and parental status as moderators. Journal of Family Psychology, 25, 345–355. [DOI] [PubMed] [Google Scholar]
- Wang Z, Jex SM, Peng Y, Liu L, & Wang S (2019). Emotion regulation in supervisory interactions and marital well-being: A spillover–crossover perspective. Journal of Occupational Health Psychology. [DOI] [PubMed] [Google Scholar]
- Williams PG, Cribbet MR, Rau HK, Gunn HE, & Czajkowski LA (2013). The effects of poor sleep on cognitive, affective, and physiological responses to a laboratory stressor. Annals of Behavioral Medicine, 46, 40–51. [DOI] [PubMed] [Google Scholar]
- Xie L, Kang H, Xu Q, Chen MJ, Liao Y, Thiyagarajan M, O’Donnell J, Christensen DJ, Nicholson C, Iliff JJ, Takano T, Deane R, & Nedergaard M (2013). Sleep drives metabolite clearance from the adult brain. Science, 342(6156), 373–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yorgason JB, Roper SO, Sandberg JG, & Berg CA (2012). Stress spillover of health symptoms from healthy spouses to patient spouses in older married couples managing both diabetes and osteoarthritis. Families, Systems, & Health, 30, 330–343. [DOI] [PubMed] [Google Scholar]
- Young-Hyman D, de Groot M, Hill-Briggs F, Gonzalez JS, Hood K, & Peyrot M (2016). Psychosocial Care for People With Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care, 39, 2126–2140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemp M, Nussbeck FW, Cummings EM, & Bodenmann G (2017). The spillover of child-related stress into parents’ relationship mediated by couple communication. Family Relations: An Interdisciplinary Journal of Applied Family Studies, 66, 317–330. [Google Scholar]
- Zhang M, Foley S, & Yang B (2013). Work–family conflict among Chinese married couples: spillover and crossover effects. The International Journal of Human Resource Management, 24, 3213–3231. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


