Fifteen years ago, the term multimorbidity rarely appeared in chronic disease health care policies. Today, research has revealed very high rates of multimorbidity, leading to it being labeled the number one challenge in developed countries.1-5 Paradoxically, chronic disease prevention and management (CDPM) programs of integrated care have popped up in all health care systems but they mainly follow a single-disease approach in their interventions. In this article, we define CDPM programs broadly as any interventions intended to improve care for patients with chronic diseases and risk factors; these are added to usual care and are typically delivered by a team.
Even though the number of publications on multimorbidity has increased substantially in the past 10 years,6 intervention studies have, so far, been scarce and demonstrated inconsistent results.7 In general, naturally occurring CDPM programs of integrated care for multimorbidity do not produce evidence strong enough to support their scaling up. A consensus has, however, emerged among researchers on the need for more integrated and patient-centred approaches.4,8 Some evidence supporting the effectiveness of patient-centred care has been generated9 but, until recently, it has been limited. Various experts have made suggestions for the care of patients with multimorbidity but these take the form of general guiding principles for addressing priorities and interactions or for avoiding harm and polypharmacy.10-12 The chronic care model (CCM) is the most inspiring organizational framework for guiding care for people with chronic disease, but it lacks detail on how to create “productive interactions” with patients and how to be a “prepared, proactive practice team.”13
The implementation of new models of patient-centred care for persons with multimorbidity in primary health care faces additional challenges mostly related to a lack of readiness or competing demands. Change management theory and models14 might help circumvent some challenges but these lack specificity for the implementation of integrated care for persons with multimorbidity at the clinical level. We propose a new framework that specifies effective, evidence-informed components of interventions in patient-centred integrated care that can improve outcomes for patients with multimorbidity.
Methods
This work was part of research program called Patient-Centred Innovations for Persons with Multimorbidity (PACE in MM). The team was funded by the Canadian Institutes of Health Research as part of their Community-Based Primary Health Care Signature Initiative under the leadership of the 2 authors.15 The main goal of PACE in MM was to reorient care from a single-disease focus to a multimorbidity focus, and to realign the health care system from separate disease silos to coordinated and patient-centred collaborations in care.16 Concretely, the team committed to partner with existing CDPM programs and accompany them in a transformation process to enhance a patient-centred approach and multimorbidity focus and to formally assess the effectiveness of the programs. As an important step to inform program enhancement, the team reviewed the available evidence coming mainly from 2 sources: a scoping review of the available literature and a realist synthesis of natural experiments with robust evaluations. This article summarizes the key findings from these 2 sources to create an overarching framework of effective, evidence-informed components of interventions in patient-centred integrated care for multimorbidity.
Building on 4 high-quality systematic reviews,7,17-19 the scoping review identified 53 publications on interventions for patient-centred care and multimorbidity. The main findings are 7 high-level components of interventions associated with positive health-related outcomes, which were divided into 37 single operational elements. An example of a high-level component would be “providing a patient-oriented approach,” while the corresponding operational elements would be “creating an individualized and adapted care intervention,” “performing regular contacts and assessment,” and “sharing the care plan with team members.”20
Following an environmental scan of all CDPM programs considered as natural experiments in the 2 most populated Canadian provinces, Quebec and Ontario, the 12 programs with the most robust evaluations were included in a realist synthesis.21 This realist synthesis identified 8 main mechanisms that are associated with positive outcomes. Two examples of mechanisms would be “creating co-located interdisciplinary teams” and “providing educational resources and skills.”
Both the scoping review and the realist synthesis were conducted by the PACE in MM team as part of the first year of the research program.
The PACE in MM framework
Figure 1 displays the PACE in MM framework for effective integrated care. Five overarching components were divided into several smaller elements or pieces, as will be explained in the following sections. Central to the framework is the underpinning of evidence for effective interventions in terms of health outcomes and health care use.
Figure 1.
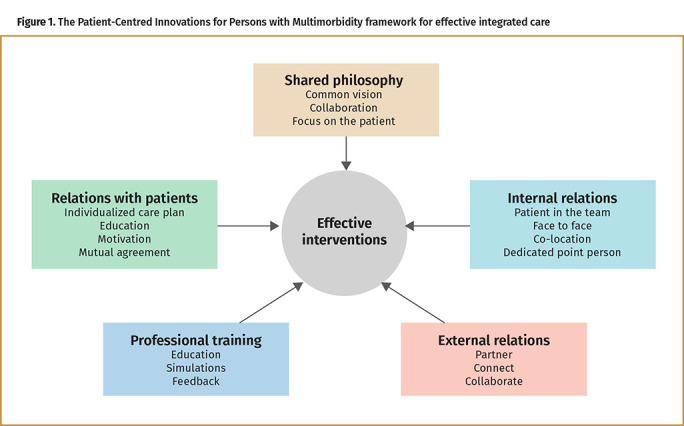
The Patient-Centred Innovations for Persons with Multimorbidity framework for effective integrated care
Shared philosophy. This component refers to the team’s shared vision of the program or intervention.21 Team members need to have a common vision in order to provide integrated chronic care, and this need is even greater when treating patients with multimorbidity. The team’s shared vision is the key to their successful collaboration. For all members, the focus has to be on the patient rather than on a single disease. Achieving this focus is especially challenging for unstable or very large clinical teams. Written vision statements and terms of reference can assist in the team’s adoption of the shared philosophy, perhaps especially if they are supported by a strong leadership. Integrated care for patients with multimorbidity requires a change of the care paradigm. All members of the team have to act on it.
Shared philosophy or vision is a key element in several frameworks related to change management.14 It is also included in the “plan” step of the plan-do-study-act framework for quality improvement.22
Internal relations. This second component refers to how the different team members cooperate and communicate.20,21 First, consistent with the patient-centred approach, the team has to consider the patient as a full member of the team. As well, a dedicated point person has to be identified. This person is the main bridge between the patient and the other professionals. Face-to-face meetings are ideal to facilitate exchanges among professionals. To make these meetings effective, participants can present, review, and discuss one or more cases together. Also ideal, although it is not always possible, is to have professionals co-located within the same clinical environment, so that they can develop good internal relationships and foster team functioning; coordination among team members who are not co-located is a realistic alternative option to consider.
Including this component in the framework is consistent with the literature’s findings that interprofessional collaboration is associated both qualitatively and quantitatively with successful outcomes in primary health care.23
External relations. Following on from the importance of internal relations, the third component in the framework highlights the attention that must be paid to the team’s relations with the rest of the health care system and the community.21 Members of the governance structure, such as local or regional managers or decision makers, have to partner to avoid duplication of their efforts or counter-productive concurrent initiatives. The team has to connect with the local hospital to ensure good transitions in care. Collaboration with community organizations can offer more opportunities for the patients to be empowered. The team can also cooperate with other available primary health care programs, such as home care or specialized support services.
This finding aligns with the literature on integrated care and coordination.24 It comes as no surprise, given the number of people that have to be involved in the care of patients with multimorbidity, but has not been explicitly considered in the implementation on the front lines of primary care.
Professional training. This component addresses the need for integrated care skills, which might not be part of the regular training of all professionals involved in primary care. Therefore, additional or specific training might need to be provided.21 The intensity of the training depends on the scope of the transformation. Training might be specific to the most common chronic conditions but also has to include the new processes of care involved in the transformation. It might include practice with simulated patients or role-playing, feedback from peers, or other educational strategies. This component is essential to enable the transformation.25 The passage from usual care to integrated care involving patient-centred teams cannot be successfully traveled without adequate training.
Relations with patients. This is a very important component of integrated care.20,21 It is also a key aspect of the classic patient-centred clinical method.26 Providing a unique and individualized care plan for each patient in response to the patient’s own objectives is respectful of patient values. Similarly, the team can provide patients with education in response to their specific requests and unique needs. Education might not be effective in the long run if attention is not also paid to sustaining the patient’s motivation. This point is especially true regarding health behaviour changes, which are frequently required. Face-to-face contacts with patients are essential, as is sufficient appointment time to allow patients and providers to achieve agreement on their shared objectives.
From the CCM to the PACE in MM framework
The CCM identified the most important structural elements a health care system must put in place to improve care for people with chronic diseases13: the community, the health system, self-management support, delivery system design, decision support, and clinical information systems. The strict application of evidence-based practice inspired by those 6 elements is meant to foster productive interactions between practice teams and activated patients. The PACE in MM framework complements the CCM by identifying the conditions under which those productive interactions could be implemented for patients with multimorbidity. In other words, the CCM offers the structure, while the PACE in MM framework offers the processes essential to creating productive interactions between the team and the patient, thus enabling the desired improved outcomes. This complementarity between the CCM and the PACE in MM framework is perhaps not surprising, because the latter largely derived from interventions that were concrete applications of either the CCM or some adaptation of it.
What the PACE in MM framework really adds
The PACE in MM framework is flexible and therefore easily adaptable to almost any new or ongoing CDPM programs. Its principles are universal and not specific to any given jurisdiction. It is largely inspired by the perspectives of the patients who have been included and consulted in the different studies selected by the sources. By including studies from around the world, the scoping review presents strong evidence of effectiveness. By including naturally occurring and pragmatic experiments as sources, the realist synthesis reflects feasible examples from the real world of actual primary health care providers, in addition to patients and caregivers. The framework could be applicable to any chronic disease program or, more specifically, to those programs for multimorbidity. Some might find commonalities between this framework and the Consolidated Framework for Implementation Research, with its 5 domains and 26 constructs used mostly for evaluation.27 However, the PACE in MM framework is rooted in a more specific literature about interventions based on patient-centred care; it is intended for care of patients with multimorbidity and meant to guide the interventions. The Consolidated Framework for Implementation Research can still guide the evaluation of any intervention inspired by the PACE in MM framework.
This framework is useful for many audiences. For decision makers, it provides direction for aligning the health care system to respond to the needs of most patients, ie, those affected by multimorbidity. For researchers, it guides the next generation of interventions to be implemented, trialed, and scaled up. For clinicians, it is an incentive and a guidance to work collaboratively to create innovative practices. And for patients with chronic diseases and multimorbidity, it is the basis of a new partnership in care.
The PACE in MM framework makes no pretense of dictating precisely, or in detail, the organization of care in any intervention built on its 5 components. It has to be seen as an inspiration arising from good evidence and robust synthesis processes. Its components, listed in Figure 1, come from a variety of sources and all are informed by evidence. At this stage, we cannot judge how they will interact to create effective interventions. However, applying the framework in clinical trials with robust evaluation will help to answer this question.
Conclusion
The PACE in MM framework complements the CCM by identifying the conditions under which productive interactions between practice teams and engaged, activated patients could be implemented for patients with multimorbidity. Implementing this framework extensively within the health care system will help to reorient care from a single-disease focus to a multimorbidity focus, and to move the health care system away from separate disease silos and toward coordinated patient-centred collaborations in care.
Footnotes
Competing interests
None declared
The opinions expressed in commentaries are those of the authors. Publication does not imply endorsement by the College of Family Physicians of Canada.
This article has been peer reviewed.
Cet article se trouve aussi en français à la page 242.
References
- 1.Global Burden of Disease Study 2013 Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386(9995):743-800. Epub 2015 Jun 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Starfield B. Threads and yarns: weaving the tapestry of comorbidity. Ann Fam Med 2006;4(2):101-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW.. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA 2005;294(6):716-24. [DOI] [PubMed] [Google Scholar]
- 4.Fortin M, Soubhi H, Hudon C, Bayliss EA, van den Akker M.. Multimorbidity’s many challenges. BMJ 2007;334(7602):1016-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fortin M, Stewart M, Poitras ME, Almirall J, Maddocks H.. A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Ann Fam Med 2012;10(2):142-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramond-Roquin A, Fortin M.. Towards increased visibility of multimorbidity research. J Comorb 2016;6(2):42-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith SM, Wallace E, O’Dowd T, Fortin M.. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev 2016;(3):CD006560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Navickas R, Petric VK, Feigl AB, Seychell M.. Multimorbidity: what do we know? What should we do? J Comorb 2016;6(1):4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lewin SA, Skea ZC, Entwistle V, Zwarenstein M, Dick J.. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev 2001;(4):CD003267. [DOI] [PubMed] [Google Scholar]
- 10.Kernick D, Chew-Graham CA, O’Flynn N.. Clinical assessment and management of multimorbidity: NICE guideline. Br J Gen Pract 2017;67(658):235-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Muth C, van den Akker M, Blom JW, Mallen CD, Rochon J, Schellevis FG, et al. . The Ariadne principles: how to handle multimorbidity in primary care consultations. BMC Med 2014;12:223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wallace E, Salisbury C, Guthrie B, Lewis C, Fahey T, Smith SM.. Managing patients with multimorbidity in primary care. BMJ 2015;350:h176. [DOI] [PubMed] [Google Scholar]
- 13.Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract 1998;1(1):2-4. [PubMed] [Google Scholar]
- 14.Kotter JP, Schlesinger LA.. Choosing strategies for change. Harv Bus Rev 1979;57(2):106-14. [PubMed] [Google Scholar]
- 15.Stewart M, Fortin M; Patient-Centred Innovations for Persons with Multimorbidity Team . Patient-Centred Innovations for Persons with Multimorbidity: funded evaluation protocol. CMAJ Open 2017;5(2):E365-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.University of Sherbrooke [website] . PACE in MM. Sherbrooke, QC: University of Sherbrooke; 2017. Available from: http://www.paceinmm.recherche.usherbrooke.ca/. Accessed 2020 Jan 31. [Google Scholar]
- 17.Dwamena F, Holmes-Rovner M, Gaulden CM, Jorgenson S, Sadigh G, Sikorskii A, et al. . Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev 2012;(12):CD003267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Bruin SR, Versnel N, Lemmens LC, Molema CCM, Schellevis FG, Nijpels G, et al. . Comprehensive care programs for patients with multiple chronic conditions: a systematic literature review. Health Policy 2012;107(2-3):108-45. Epub 2012 Aug 9. [DOI] [PubMed] [Google Scholar]
- 19.Smith SM, Soubhi H, Fortin M, Hudon C, O’Dowd T.. Managing patients with multimorbidity: systematic review of interventions in primary care and community settings. BMJ 2012;345:e5205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Poitras ME, Maltais ME, Bestard-Denommé L, Stewart M, Fortin M.. What are the effective elements in patient-centered and multimorbidity care? A scoping review. BMC Health Serv Res 2018;18(1):446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brown J, Ryan B, Chouinard MC, Januzi L, Diallo BB, Stewart M, et al. . Facets of interventions associated with outcomes of chronic disease prevention and management programs in two Canadian provinces: a realist synthesis. Presented at: 43rd North American Primary Care Research Group Annual Meeting; 2015. October 24-28; Cancun, Mexico. [Google Scholar]
- 22.Langley GL, Moen RD, Nolan KM, Nolan TW, Norman CL, Provost LP.. The improvement guide: a practical approach to enhancing organizational performance. 2nd ed. San Francisco, CA: Jossey-Bass Publishers; 2009. [Google Scholar]
- 23.Jacobson PM, HDR Inc; Canadian Nurses Association . Evidence synthesis for the effectiveness of interprofessional teams in primary care. Ottawa, ON: Canadian Health Services Research Foundation; 2012. Available from: https://www.cna-aiic.ca/~/media/cna/files/en/synthesisinterprofteams_jacobson-en-web.pdf. Accessed 2021 Mar 2. [Google Scholar]
- 24.Government of British Columbia, Ministry of Health . Integrated models of primary care and mental health & substance use care in the community: literature review and guiding document. Victoria, BC: Government of British Columbia, Ministry of Health; 2012. Available from: http://www.health.gov.bc.ca/library/publications/year/2012/integrated-models-lit-review.pdf. Accessed 2021 Mar 2. [Google Scholar]
- 25.Varkey P, Antonio K.. Change management for effective quality improvement: a primer. Am J Med Qual 2010;25(4):268-73. Epub 2010 May 5. [DOI] [PubMed] [Google Scholar]
- 26.Stewart M, Brown JB, Weston WW, McWhinney IR, McWilliam CL, Freeman TR.. Patient-centered medicine: transforming the clinical method. 3rd ed. London, Engl: Radcliffe Publishing Ltd; 2014. [Google Scholar]
- 27.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC.. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation Sci 2009;4:50. [DOI] [PMC free article] [PubMed] [Google Scholar]


