Abstract
Few healthcare provider organizations systematically track their healthcare equity, and fewer enable direct interaction with such data by their employees. From May to August 2019, we enhanced the data architecture and reporting functionality of our existing institutional quality scorecard to allow direct comparisons of quality measure performance by gender, age, race, ethnicity, language, zip code, and payor. The Equity Lens was made available to over 4000 staff in September 2019 for 82 institutional quality measures. During the first 11 months, 235 unique individuals used the tool; users were most commonly from the quality and equity departments. Two early use cases evaluated hypertension control and readmissions by race, identifying potential inequities. This is the first description of an interactive equity lens integrated into an institutional quality scorecard made available to healthcare system employees. Early evidence suggests the tool is used and can inform quality improvement initiatives.
Keywords: quality, equity, disparities, scorecard, dashboard, healthcare systems
INTRODUCTION
In their seminal report Crossing the Quality Chasm,1 the National Academy of Medicine included healthcare equity as 1 of 6 domains of healthcare quality, and most recently elevated equity to a cross-cutting dimension across all domains of quality.2 Yet, despite this recognition of the importance of equity to the quality of healthcare delivery, inequities in healthcare persist3,4 and have received renewed attention this past year in the wake of the COVID-19 pandemic and the global reckoning with racial injustice sparked by the killing of George Floyd.4–6
The first step to addressing healthcare inequities is to identify them,7 but measurement of healthcare equity has lagged behind other measures of quality.8 One approach used to assess healthcare equity has been to stratify existing quality measures by key patient characteristics such as race. This method has been used by the National Healthcare Quality and Disparities Report over the last 15 years to document inequities in healthcare quality across the US,9 fueling national calls to advance high quality healthcare for all by requiring a focus on equity as a key component of quality.10,11
In principle, such an approach could be used at the level of a local healthcare system as well.8,12 Over the last decade, our own healthcare system has developed an institutional quality scorecard to track our system’s performance on the quality domains defined by the National Academy of Medicine, including measures of safety, timeliness, effectiveness, efficiency, and patient-centeredness (often referred to as the “STEEEP” domains).1 These scorecards have been used to set quality goals and targets for the institution and are leveraged by leaders, teams, and individuals to drive improvement. However, equity was the 1 domain of quality defined by the National Academy of Medicine that we struggled to analyze historically.
OBJECTIVE
In this article, we describe the development, implementation, and use of an Equity Lens integrated into our institutional quality scorecard to enable the examination of quality measure performance by patient sociodemographic characteristics. The goal of this work was to facilitate the identification of inequities in quality measure performance, such that those inequities could be examined and addressed, ultimately leading to improved clinical outcomes for all.
MATERIALS AND METHODS
Setting
The University of Chicago Medical Center (UCMC) includes an adult and freestanding children’s hospital with a total of 811 beds, and 5 multispecialty faculty ambulatory practice sites in the Chicago metropolitan area, with over 30 000 admissions, 100 000 emergency department visits, and over 600 000 outpatient encounters annually. UCMC employs over 900 attending physicians, 2800 nurses, and 1100 house staff.
UCMC has an institutional quality committee, which meets monthly and includes physician quality chiefs from all clinical departments and service lines, as well as chairs and cochairs of relevant quality subcommittees, directors of departments within the chief medical officer’s (CMO’s) office, select house staff, a board member, administrative and clinical leaders of inpatient, emergency, and ambulatory services and, most recently, leaders from our diversity, equity and inclusion department. The institutional quality scorecard serves as the committee’s “North Star,” and performance on “priority” quality measures is reviewed monthly.
The data science team reports to the CMO and collaborates closely with quality and information technology (IT). The work described here required 3 full-time equivalents (FTEs) from data science, and partnership with 2 data architects in IT to help structure data appropriately and automate monthly updates.
Data structure
Our organization transitioned to providing our institutional quality scorecard in a new business intelligence platform (Tableau Server) in 2016. In order to ease this transition for users, the initial version of the report looked similar to the legacy report (Crystal Reports, SAP, Germany) and did not utilize the interactivity features available. As users became more comfortable with the new tool over time, we began to develop a more interactive report. Starting in May 2019, the data architecture supporting the institutional quality scorecard was further enhanced by including additional patient variables, providing the ability for direct comparisons of quality measure performance between patient populations. We utilized Tableau (Tableau Software, Seattle, WA) and Microsoft SQL Server (Microsoft, Redmond, WA) to accomplish this work.
Data quality
The resulting Equity Lens and available institutional quality scorecard use the same underlying data and approach for monthly updates. The approach leverages an extract transform and load process to migrate and curate data for reporting from various sources including our electronic health record (EHR, Epic Systems, Verona, WI), Press Ganey, and Vizient. The data transformation and refresh happens monthly and begins with several automated checks by IT. Prior to the data being pushed to the production report, the data science team performs several data quality checks as well to ensure data have updated as expected.
Implementation
The Equity Lens report was released on Tableau Server as a new second tab accompanying the previously released institutional quality scorecard. It was made available to all with access to the institutional quality scorecard, including faculty and house staff clinicians; key leaders of all service lines, diversity, equity, and inclusion, and population health; and staff on the quality improvement team. The report release was communicated through e-mail and relevant committee meetings. All data within the report were protected by firewalls and could not be accessed outside the healthcare system’s internal network. The ability to download underlying data was also restricted to keep all analyses within the application.
Evaluation
Utilization of the report was tracked (using Tableau Server’s PostgreSQL database) from September 2019 through July 2020 by evaluating the number of total views and distinct viewers of the report. A view was defined as an individual user opening the report within the Tableau Server for any duration of time. Utilization was compared against that of the existing institutional quality scorecard. Super users of both the institutional quality scorecard and Equity Lens were defined using thresholds of at least 5, 10, and 20 views over the study period. Last, we describe 2 early use cases of the Equity Lens, including the measure examined, team involved, inequity identified, and planned next steps.
RESULTS
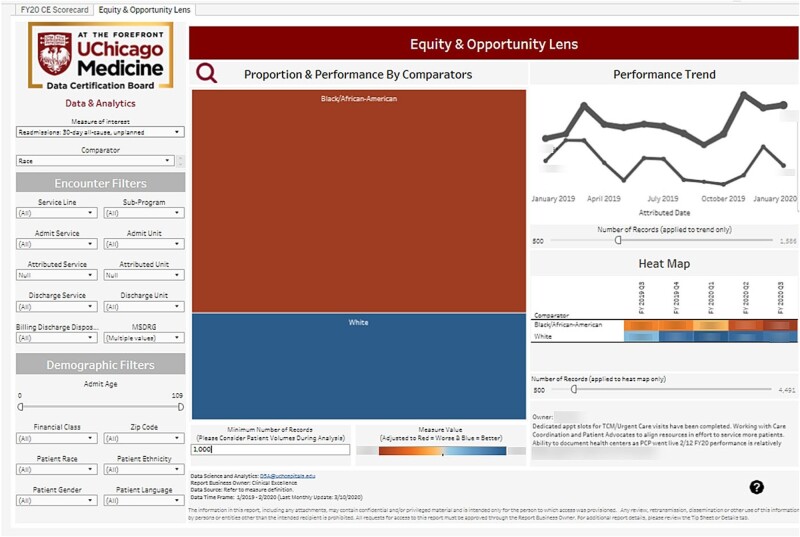
The Equity Lens (Figure 1) was released as an addition to the existing institutional quality scorecard (Figure 2), and requires user interaction to identify potential inequities in different patient populations. On the left side of the dashboard, a user must choose a single measure of interest, a sociodemographic variable on which to stratify performance of the selected measure, and various encounter and demographic filters to further refine the population for analysis. For example, if a user sought to examine readmission rates by race, they would choose the readmission measure and then race as the comparator option. Users can choose to filter their patient population by encounter variables such as service lines, discharge units, discharge dispositions, and Medicare Severity Diagnosis Related Groups, as well as by additional demographic variables such as age, payor, zip code, race, ethnicity, gender, and language. After choosing their measure, comparator, and filter(s) of interest, they can then analyze data within the report. The far left visual provides the various comparator groups where the size of the box represents the volume of patients in that comparator group with color indicating performance for that quality measure (eg, red reflects worse performance, blue reflects better performance). The top right visual provides the historical monthly performance for the selected measure of interest, stratified by comparator group. The heat map in the bottom right is a visual representation of quarter-to-quarter performance with color indicating performance for each comparator grouping. Users can hover directly on any data point to get additional content such as numerator and denominator totals.
Figure 1.
Equity lens. The left side of the dashboard provides users the options to choose a measure of interest, a sociodemographic variable on which to stratify performance of the selected measure, and various encounter and demographic filters to further refine the population for analysis. The left-most visual represents the various comparator groups. The size of the box represents number of patients and color indicates performance on the measure, with red representing worse performance and blue representing better performance. The far-right visuals provide historical performance month-by-month (top) and quarter-by-quarter (bottom). The image details an example of how 30-day all-cause unplanned readmission rates can be analyzed by race. Portions of the image were blurred intentionally for publication.
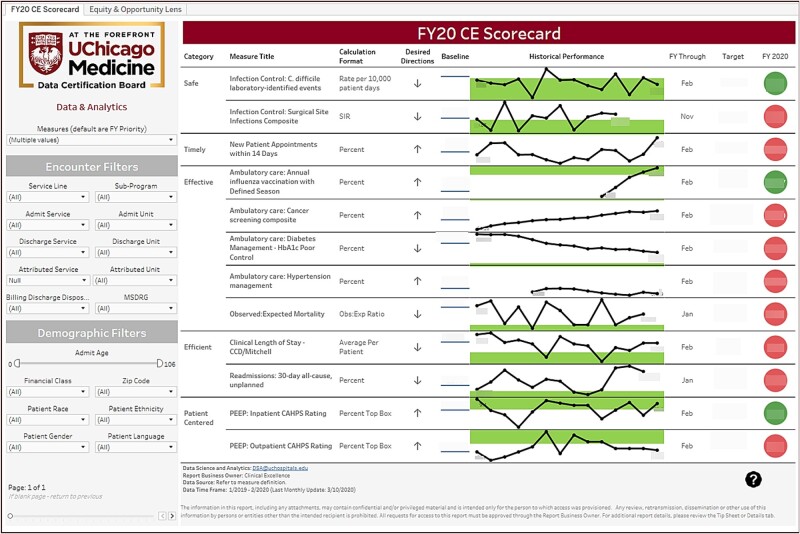
Figure 2.
Quality scorecard. By default, the institutional quality scorecard displays the institutional priority quality measures, organized into the domains of Safe, Timely, Effective, Efficient, and Patient-Centered. The left side of the scorecard provides users the option to examine other available quality measures of interest and leverage encounter and demographic filters to further refine the population of interest. The scorecard displays performance for those selected measures, as well as units of measurement for each measure, month-to-month trends, and fiscal year-to-date performance relative to institutional targets. Portions of the image were blurred intentionally for publication.
Approximately 4000 faculty and staff have access to the report. In the first 11 months, there have been 1273 views of the Equity Lens compared to 6634 views of the institutional quality scorecard, with 235 and 544 unique users of each, respectively (Table 1). Of the unique viewers of the Equity Lens and the institutional quality scorecard, there were 35 and 169 unique users, respectively, who viewed it more than 5 times. UCMC’s quality improvement and diversity, equity and inclusion departments are the 2 groups not involved in the report development with the greatest use of the report (Supplementary Appendix Table 1). A wider range of groups with repeat engagement was identified for the institutional quality scorecard (Supplementary Appendix Table 1).
Table 1.
Institutional use of the Equity Lens and quality scorecard (September 2019–July 2020)
| Measure of utilization | N |
|---|---|
| Equity Lens total views | 1273 |
| Equity Lens distinct users | 235 |
| Equity Lens super users | |
| >20 Views | 12 |
| >10 Views | 21 |
| >5 Views | 35 |
| Quality scorecard total views | 6634 |
| Quality scorecard distinct users | 544 |
| Quality scorecard super users | |
| >20 Views | 61 |
| >10 Views | 106 |
| >5 Views | 169 |
Two early use cases evaluated hypertension control and readmissions by race and identified potential inequities (Table 2).
Table 2.
Early use cases of the Equity Lens
| MeasureStratification variableTeam | Analysis/Findings | Next steps |
|---|---|---|
|
|
|
|
|
Reconnecting with relevant section chiefs to share identified priorities and draft a proposal to address those priorities |
DISCUSSION
The first step to addressing healthcare inequities is identification. Performance across multiple STEEP domain measures can now be analyzed at our institution across different patient populations as defined by their sociodemographic characteristics. This can be done in a fraction of the time of previous analytic requests supported by the data science team. Through this approach, we have begun to democratize our data to users across our healthcare system to further aid efforts in identifying and addressing potential inequities in healthcare quality.
Our analysis suggests that, when such a tool is available, it will be used, especially by staff in the quality and diversity, equity, and inclusion departments and can be a resource in the identification of healthcare disparities that clinical teams can address. As users began to access the tool, the importance of data quality was a consistent point of discussion. We chose to display all relevant patient demographics as identified within our EHR and did not filter out smaller patient populations or records with null values. This emphasized both the completeness of our data and the importance of consistent documentation of sociodemographic variables, in the context of clinical practice,13,14 to aid in equity analysis.
While the initial organizational response to the release of the report has been positive, the greatest challenge has been expanding the use of the tool to other hospital groups to drive performance improvement and reduce inequities. In addition, identifying disparities in quality metrics is only the first step to advancing healthcare equity. Eliminating identified disparities requires additional steps, including diagnosing the reasons for identified inequities that are unique to the patient population and healthcare organization in which they occur; and designing and implementing tailored health care interventions with ongoing monitoring of results following implementation, to inform intervention adjustments to ensure effectiveness.7,15 Future institutional efforts will focus on providing expectations that owners of quality measures as well as quality chiefs use the Equity Lens when examining performance on their measures of interest and report on identified inequities and plans to further evaluate and mitigate these inequities when providing updates at section, departmental, service line, and institutional meetings. We aim to change our culture, to go beyond improvement on our institutional quality measures in aggregate to improvement that is equitable across our diverse patient populations.
Our analysis has limitations. For our measurement of utilization, we were unable to accurately track session duration—as well as use of the report in larger group meetings, where there may have been multiple individuals viewing the report. In addition, we did not assess the accuracy of the sociodemographic variables in the report.13
CONCLUSION
To our knowledge, this is the first description of an interactive equity lens integrated into an institutional quality scorecard disseminated to all healthcare system faculty, staff, and trainees. Early evidence suggests the tool is used by quality and equity leaders and staff and can inform quality improvement initiatives. Our next step is to foster further engagement and use of the Equity Lens across a broader audience of healthcare providers and leaders, to ensure inequities are identified, where they exist, and addressed.
FUNDING
Drs. Chin and Cook were supported in part by the Robert Wood Johnson Foundation Advancing Health Equity: Leading Care, Payment, and Systems Transformation Program Office. Dr. Chin was also supported by the Merck foundation Bridging the Gap: Reducing Disparities in Diabetes Care National Program Office and the Chicago Center for Diabetes Translation Research (NIDDK P30 DK092949).
AUTHOR CONTRIBUTIONS
All listed authors were significant contributors to the design and interpretation of the work detailed, helped draft and revise the manuscript, and provided a final review and approval of submission. All authors listed are worthy of authorship per the ICMJE guidelines.
SUPPLEMENTARY MATERIAL
Supplementary material is available at the Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGMENTS
We would like to acknowledge Lisa Vinci, MD and Danielle Jungst, MPH for their efforts with the Hypertension Management Use Case, and Michael Wall, PharmD for his input and guidance of the development of the Equity Lens.
DATA AVAILABILITY STATEMENT
This project was formally determined to be quality improvement, not human subjects research, and was therefore not reviewed by the Institutional Review Board, which is consistent with institutional policy. Our institution authorizes presentation of aggregate data, but precludes sharing of individual study data with those outside the study team. Requests to learn more about the functionality and technical development of the dashboard can be directed to the corresponding or primary author.
CONFLICT OF INTEREST STATEMENT
Portions of this work were shared in oral presentations at the AMIA 2018 and 2020 Clinical Informatics conferences. Dr. Chin is a member of the Bristol-Myers Squibb Company Health Equity Advisory Board; Dr. Umscheid is a member of Press Ganey’s Diversity, Equity & Inclusion Advisory Council; and Mr. Williams is a member of Vizient’s Equity Committee and Chief Diversity Officer’s Network. None of these organizations had a role in the development, implementation, or evaluation of our institutional equity scorecard.
REFERENCES
- 1.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- 2.Institute of Medicine (US) Committee on Future Directions for the National Healthcare Quality and Disparities Reports; Ulmer C, Bruno M, Burke S, eds. Future Directions for the National Healthcare Quality and Disparities Reports. Washington DC: National Academies Press; 2010. 3, Updating the Framework for the NHQR and NHDR. https://www.ncbi.nlm.nih.gov/books/NBK220155/ Accessed April 28, 2021 [PubMed] [Google Scholar]
- 3.Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 4. Mackey K, Ayers CK, Kondo KK, et al. Racial and ethnic disparities in COVID-19-related infections, hospitalizations, and deaths: a systematic review. Ann Intern Med. 2021; 174 (3): 362–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chowkwanyun M, Reed AL.. Racial health disparities and Covid-19: caution and context. N Engl J Med 2020; 383 (3): 201–3. [DOI] [PubMed] [Google Scholar]
- 6. Evans MK, Rosenbaum L, Malina D, et al. Diagnosing and treating systemic racism. N Engl J Med 2020; 383 (3): 274–6. [DOI] [PubMed] [Google Scholar]
- 7. Chin MH, Clarke AR, Nocon RS, et al. A Roadmap and best practices for organizations to reduce racial and ethnic disparities in health care. J Gen Intern Med 2012; 27 (8): 992–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ramos R, Davis JL, Ross T, et al. Measuring health disparities and health inequities: do you have REGAL data? Qual Manag Health Care 2012; 21 (3): 176–87. [DOI] [PubMed] [Google Scholar]
- 9.Agency for Healthcare Research and Quality. National Healthcare Quality and Disparities Reports. 2020. https://www.ahrq.gov/research/findings/nhqrdr/index.html Accessed April 28, 2021
- 10.National Quality Forum. A roadmap for promoting health equity and eliminating disparities: the four I’s for health equity. 2017. https://www.qualityforum.org/Disparities_Project.aspx Accessed October 19, 2020
- 11.FamiliesUSA. Accelerating health equity by measuring and paying for results. 2019. https://familiesusa.org/wp-content/uploads/2019/03/HEV_Data-Stratification_-Issue-Brief.pdf Accessed October 19, 2020
- 12. Sivashanker K, Gandhi TK.. Advancing safety and equity together. N Engl J Med 2020; 382 (4): 301–3. [DOI] [PubMed] [Google Scholar]
- 13. Klinger EV, Carlini SV, Gonzalez I, et al. Accuracy of race, ethnicity, and language preference in an electronic health record. J Gen Intern Med 2015; 30 (6): 719–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cusick MM, Sholle ET, Davila MA, et al. A method to improve availability and quality of patient race data in an electronic health record system. Appl Clin Inform 2020; 11 (05): 785–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. DeMeester RH, Xu LJ, Nocon RS, et al. Solving disparities through payment and delivery system reform: a program to achieve health equity. Health Aff 2017, 36(6), 1133–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
This project was formally determined to be quality improvement, not human subjects research, and was therefore not reviewed by the Institutional Review Board, which is consistent with institutional policy. Our institution authorizes presentation of aggregate data, but precludes sharing of individual study data with those outside the study team. Requests to learn more about the functionality and technical development of the dashboard can be directed to the corresponding or primary author.