Abstract
BACKGROUND AND PURPOSE:
The Woven EndoBridge has proved to be a safe and effective treatment, especially for wide-neck intracranial aneurysms. The recent fifth-generation Woven EndoBridge came with smaller devices. The purpose of this study was to assess the safety and efficiency of Woven EndoBridge treatment of small and very small aneurysms.
MATERIALS AND METHODS:
Between September 2017 and March 2020, all consecutive patients treated with a 3- or 3.5 mm-width Woven EndoBridge device were included in this retrospective intention-to-treat study. Clinical and radiologic findings were evaluated at immediate and last-available follow-up. Angiographic outcome was assessed by an external expert reader.
RESULTS:
One hundred twenty-eight aneurysms were treated with a fifth-generation Woven EndoBridge device including 29 with a width of ≤3.5 mm. Ten aneurysms were ruptured (34%). In 3 cases (10%), Woven EndoBridge treatment could not be performed because the aneurysm was still too small for the smallest available Woven EndoBridge device and another endovascular strategy was chosen. The median follow-up time was 11.2 months. Complete and adequate occlusion was obtained in 71% and 90% of the treated aneurysms, respectively. Retreatment was needed in 2 cases (10%). Symptomatic ischemic complications leading to transient neurologic deficits occurred in 2 cases (7%) (1 procedure-related and 1 device-related) but with full spontaneous recovery at discharge.
CONCLUSIONS:
The fifth-generation Woven EndoBridge device seems to be a safe and technically feasible treatment for both ruptured and unruptured small and very small intracranial aneurysms, with satisfactory occlusion rates on midterm follow-up. However, further study is needed to evaluate longer-term efficiency.
Since the publications of the results of the International Subarachnoid Aneurysm Trial (ISAT), in many centers, endovascular therapy has become the first-line treatment for intracranial aneurysms.1,2 With an annual rupture rate of 0.36% per year, the treatment of small, unruptured, intracranial aneurysms remains disputable.3 However, independent predictors of rupture such as a history of subarachnoid hemorrhage, active smoking, location on the anterior communicating artery, and aneurysm multiplicity were identified, providing selection criteria for potential treatment. 4-7
The treatment of small and very small aneurysms is often challenging, especially for ruptured cases, in which therapeutic options are limited.8-10 Conceived as an intrasaccular flow-disruption device, the Woven EndoBridge aneurysm embolization system (WEB; MicroVention) has proved to be a safe and effective treatment for bifurcation aneurysms.11-14 The absence of systematic use of antiplatelet therapy in a hemorrhagic context makes the WEB therapy particularly interesting for ruptured wide-neck aneurysms.15-17
Since 2010, the device progressively evolved from an initial double-layer version to single-layer (SL-WEB) and single-layer spherical versions. Recently, the fifth-generation WEBs became available outside the United States,18 compatible with a new and smaller delivery catheter (VIA 17; MicroVention), facilitating the treatment of smaller and more distal aneurysms. The changes in the braiding design allowed the development of smaller devices (3- and 3.5-mm width).
The WEB device has been evaluated in many Good clinical practice (GCP) studies, but the smaller fifth-generation devices were not included at that time. 11,19,20 The purpose of this study was to report the follow-up results of ruptured and unruptured small and very small intracranial aneurysms treated using the new, smaller fifth-generation WEB devices.
MATERIALS AND METHODS
Between September 2017 and March 2020, all patients treated for an intracranial aneurysm in Department of Interventional Neuroradiology (NEURI Brain Vascular Center, Bicêtre Hospital, Le Kremlin Bicêtre, France) neurovascular center were retrospectively reviewed. All cases that had the intention to treat with a WEB as a first-line strategy were included. The collected data base was notified to the French Data Protection Authority. All patients gave informed consent before inclusion.
Inclusion Criteria
Every patient in whom an SL 3 or SL 3.5 WEB was used to attempt to treat an intracranial aneurysm was included. Patients with both ruptured or unruptured aneurysms were included. No exclusion criteria were defined. Technical failures were included but were not considered for follow-up evaluations.
Indications
Embolization indications for unruptured small aneurysms were all discussed in a local multidisciplinary meeting with neuroradiologists and neurosurgeons.
Among the 19 small and very small unruptured aneurysms, 7 were treated due to a personal or familial history of aneurysm rupture; 5 were treated due to multiple aneurysms locations; 2 due to both personal history of aneurysm rupture and multiple aneurysm locations, 4 due to irregular aneurysm shape combined with patient anxiety; and 1, due to aneurysm modifications with time.
In most cases, the WEB was selected as a first-line strategy because of wide-neck lesions. Wide-neck aneurysms were defined as aneurysms with an aspect ratio inferior or equal to 1.2.21 Treatment was performed on a biplane angiographic system (Azurion; Philips Healthcare).
Antiplatelet Therapy
Patients with unruptured aneurysms were administered a dual-antiplatelet therapy (acetylsalicylic acid, 160 mg, and ticagrelor, 90 mg) 24 hours before the intervention in case an additional stent placement would be required. No antiplatelet therapy was administered for patients with ruptured aneurysms. Postoperative antiplatelet therapy was specifically prescribed only in cases of major protrusion (generally aspirin for 1 month).
Procedures
All procedures were performed with the patient under general anesthesia and systemic heparinization. After puncture, a long delivery catheter and a guiding catheter were positioned in the internal carotid artery or the vertebral artery according to the case. A 3D rotational angiography was then systematically performed for WEB sizing. The WEB device was usually slightly oversized in width.
Aneurysm catheterization was then performed using the VIA 17 microcatheter, and the selected WEB was deployed. Prior to detachment, a control VasoCT (Philips Healthcare)22 was performed to evaluate the WEB positioning (Fig 1). If needed, the device could then be repositioned or replaced (Supplemental Online Video).
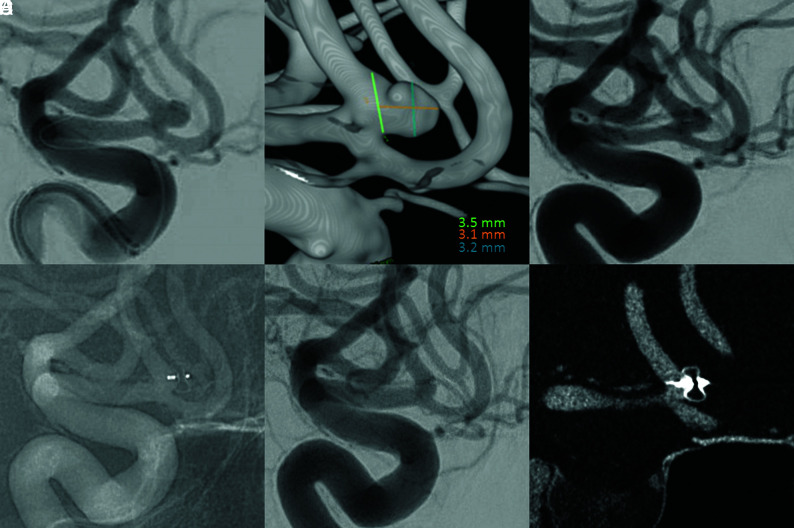
FIG 1.
Ruptured anterior communicating artery aneurysm treatment using an SL 3.5 × 2 mm WEB. A, Left internal carotid angiogram shows the aneurysm. B, 3D rotational angiography with aneurysm measurement. C, A postdeployment angiogram shows a good filling of the aneurysmal sac with persistent opacification inside the WEB. D and E, Three-month follow-up angiogram shows complete exclusion of the aneurysm. F, Three-month follow-up VasoCT confirms the aneurysm exclusion, with slight WEB compaction.
Follow-up Evaluation
Clinical evaluation was based on the mRS and evaluated before every follow-up angiography, which were routinely scheduled at 6, 18, and 42 months or 3, 15, and 39 months after treatment for unruptured and ruptured aneurysms, respectively.
For every patient, the last available follow-up angiography was retrospectively reviewed by an external expert neurointerventional radiologist. Angiographic results were classified according to the Bicêtre Occlusion Scale Score.23 Complete occlusion was defined as grades 0 or 0′; adequate occlusion was defined as grades 0, 0′, 1, or 2; and other grades were considered to be aneurysm remnants. Aneurysms that required retreatment were systematically considered to be aneurysm remnants, irrespective of Core Lab evaluation.
RESULTS
Patients
Between September 2017 and March 2020, one hundred twenty-eight aneurysms were embolized in our center with a fifth-generation WEB device. Twenty-seven patients with 29 aneurysms were treated using an SL 3 or a SL 3.5 WEB. Two patients were treated for 2 distinct aneurysms. Ten (34%) of the 29 aneurysms were ruptured aneurysms. The mean age was 54 years (median, 55 years; range, 32–90 years of age), and 18 (67%) patients were women. A history of hypertension and dyslipidemia was found in 7 (26%) and 4 (15%) patients, respectively. Eight (30%) patients were active smokers, and 6 (22%) had a history of smoking.
Aneurysm locations were the following: middle cerebral artery (15 aneurysms, 52%), anterior communicating artery (8 aneurysms, 28%), basilar tip (3 aneurysms, 11%), carotid tip (1 aneurysm, 3%), anterior cerebral artery (1 aneurysm, 3%), and posterior communicating artery (1 aneurysm, 3%). The overall mean width and height were 2.8 mm (range, 1.7–4.8 mm) and 2.9 mm (range, 2.1–4.4 mm), respectively. Eighteen aneurysms (62%) were considered wide-neck. The mean aspect ratio was 1.2 (range, 0.7–2.0) (Table).
Baseline characteristics and angiographic outcomesa
| Treated Intracranial Aneurysms | All (n = 29) |
|---|---|
| Baseline demographic characteristics | All (n = 27) |
| Age (mean) (yr) | 54 (SD, 11.5) |
| Female | 18 (67) |
| Hypertension | 7 (26) |
| Dyslipidemia | 4 (15) |
| Smoking | |
| Global | 14 (52) |
| Active | 8 (30) |
| History | 6 (22) |
| Baseline aneurysm characteristics | All (n = 29) |
| Aneurysm location | |
| Middle cerebral artery | 15 (52) |
| Anterior communicating artery | 8 (28) |
| Basilar tip | 3 (11) |
| Carotid tip | 1 (3) |
| Anterior cerebral artery | 1 (3) |
| Posterior communicating artery | 1 (3) |
| Acutely ruptured | 10 (34) |
| Maximum diameter (mean) (mm) | 3.8 (SD, 0.9) |
| Aneurysm height (mean) (mm) | 2.9 (SD, 0.6) |
| Aneurysm width (mean) (mm) | 2.8 (SD, 0.6) |
| Aneurysm neck (mean) (mm) | 2.6 (SD, 0.5) |
| Aspect ratio (height/neck) (mean) | 1.2 (SD, 0.4) |
| Width/neck ratio (mean) | 1.1 (SD, 0.2) |
| Wide neck | 18 (62) |
| Baseline treatment characteristics | All (n = 29) |
| WEB | |
| SL 3 | 17 (59) |
| SL 3.5 | 9 (31) |
| Technical failure | 3 (10) |
| Angiographic outcomes | All (n = 21) |
| Adequate occlusion | 19 (90) |
| Complete occlusion | 15 (71) |
| Aneurysm remnant | 2 (10) |
Data are number of subjects (and percentage) for qualitative variables, and mean (and standard deviation) for quantitative variables.
Technical Results and Adverse Events
Technical success with satisfactory WEB deployment was achieved in 26 aneurysms (90%). In 2 cases, even the SL 3 WEB (the smallest existing WEB) was considered too large on the control VasoCT before detachment, with device protrusion inside the parent artery. In 1 anterior communicating artery aneurysm, the angulation did not allow proper deployment of the WEB. These 3 patients were successfully treated using coils.
Among patients successfully treated with a WEB, no perioperative rupture was reported. Thromboembolic complications occurred in 4 cases, of which 3 were intraoperative thromboembolism. Of those 3, complete recanalization was achieved during the final angiography in 2 patients after intra-arterial abciximab injection. In the third case, owing to the excellent leptomeningeal collateral circulation, we decided not to perform any endovascular treatment and no deficit was observed after the intervention.
A postoperative neurologic deficit was depicted in 2 cases, and DWI revealed small punctiform ischemic spots. The first patient was treated with abciximab, and DWI spots were located in the territory of the branch where the clot had been seen. In the second case, no intraoperative thromboembolic complications were depicted, and MR imaging revealed 4 DWI spots in the middle cerebral artery territory. Deficits were all completely regressive at the patients’ discharge.
Clinical Outcome
Clinical worsening defined as a higher mRS score at the final control than before treatment was observed in 3 patients (10%). These patients were treated for ruptured aneurysms. In 2 of these patients, initial subarachnoid hemorrhage was associated with intraparenchymal hematoma, resulting in a persistent neurologic deficit in 1 patient and a persistent psychomotor slowdown in the other. In the latter case, clinical worsening was due to persistent asthenia and headache at 11 months after the initial rupture. At discharge, no procedure-related morbidity or mortality was reported. During the follow-up period, none of the ruptured aneurysms treated with a WEB rebled.
Angiographic Outcome
Twenty-one aneurysms (72%) had at least 1 angiographic evaluation at the time of this study. Mean follow-up was 10.9 months (range, 3.1–22.3 months). Complete occlusion was obtained in 15 aneurysms (71%), and adequate occlusion, in 19 aneurysms (90%). Retreatment was needed in 2 patients (Table).
DISCUSSION
Twenty-nine individual aneurysms were treated using 3- and 3.5-mm SL WEBs in this retrospective study. The median follow-up was 11.2 months. Technical success was achieved in 90% of the cases, with complete and adequate occlusion rates in 71% and 90% of aneurysms, respectively. Four patients experienced periprocedural thrombotic events, with 2 ischemic complications leading to full recovery at discharge. No perioperative rupture was reported.
Treatment Feasibility and Angiographic Efficiency
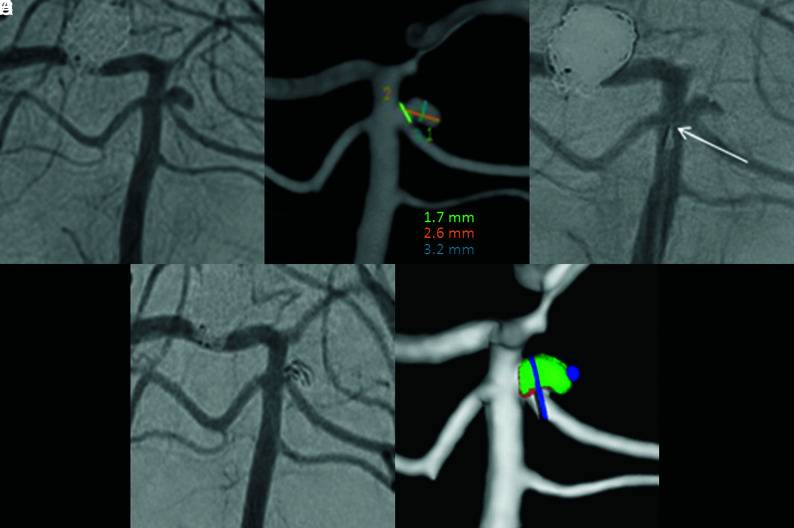
Technical success was achieved in 90% of the treatments. However, the WEB could not be deployed in 3 cases. In 2 of the 3 technical failures, successful treatment could not be achieved owing to the WEB size. With an average aneurysm width of 1.7 and 2.2 mm and an average height of 2.3 and 2.1 mm, respectively, the SL 3 size was chosen. In each case, the WEB was protruding into the parent artery and had to be removed. Indeed, in some cases and especially in small, irregular aneurysms, the choice of the device size can be challenging. A postoperative evaluation using the IDsize software (Sim&Cure) showed that this situation could have been predicted (Fig 2). In the future, a systematic preoperative software simulation might improve device selection and success rates.
FIG 2.
Technical failure in a left superior cerebellar artery with an SL 3 × 2 WEB. A, A left vertebral angiogram shows the left cerebellar aneurysm. B, 3D rotational angiography with aneurysm measurement. C, WEB deployment attempt, with the proximal marker (white arrow) protruding into the basilar trunk. D, Final angiogram after coiling. E, Retrospective Sim&Cure simulation showing SL 3 WEB protrusion into the superior cerebellar artery and basilar trunk.
Previous studies reported increased difficulties for endovascular treatment of smaller aneurysms using only coils. With less space in the aneurysmal sac for a proper placement of the microcatheter, coil deployment is indeed more challenging with an increased risk of protrusion into the parent artery and aneurysmal rupture. Thus, in the prospective Analysis of Treatment by Endovascular Approach of Nonruptured Aneurysms (ATENA) multicenter study, the rate of technical failure was significantly different in 1- to 6-mm aneurysms (5.7%) and in 7- to 15-mm aneurysms (2.3%).8 In a 2016 meta-analysis evaluating endovascular treatment with coils for ≤3 mm aneurysms, technical success was obtained in 92% of the coiled intracranial aneurysms, fairly close to the results obtained in this study.24 The 91% rate of “complete and near-complete” occlusion reported in this meta-analysis was also quite similar to the adequate occlusion rate of 90% described in this study. The technical success and angiographic efficiency of coil treatment in the 2016 meta-analysis were improved using stent-assisted techniques in 8% of the aneurysms, particularly in wide-neck lesions.25 However, with mandatory postoperative antiplatelet therapy, stent-assisted techniques are limited by hemorrhage risk in ruptured cases. Applicable in both wide-neck and ruptured small aneurysms, WEBs seem to be a viable alternative treatment.
Treatment Safety
Small and very small ruptured aneurysms have been associated with higher procedure-related rupture when treated by coils.26 The 2016 meta-analysis24 of endovascular treatment for ≤3-mm aneurysms found intraprocedural rupture rates of 7% of the coiling procedures, while thromboembolic events occurred in 4%. No perioperative rupture was reported in this study. Ischemic complications occurred in 2 patients (7%) (1 device-related and 1 procedure-related); however, neurologic deficits were spontaneously completely regressive at discharge, and no clinical worsening was attributed to WEB embolization on long-term follow-up. However, considering the risk associated with endovascular treatment and the 0.36% annual rupture rate in unruptured intracranial small aneurysms, treatment should be performed only in selected cases, taking into account the history of SAH, age, hypertension, or location of the aneurysm.3,6
Limitations
We decided not to perform a case-control study comparing WEB treatments with coiling because of potential biases. Indeed, most of the aneurysms treated here were wide-neck and ruptured so that endovascular coiling might not have been a feasible option. Also, since 2017, the WEB device is our favored first-line strategy so that our physician team has grown in experience since older coiling was performed.
This study is limited by its retrospective design and the small number of patients included, but until now, only a few articles have reported the use of the fifth-generation WEB device, including very few of the smallest WEBs.18,27
CONCLUSIONS
The fifth-generation WEB seems to be a technically feasible treatment for both ruptured and unruptured small and very small intracranial aneurysms, with satisfactory occlusion rates on midterm follow-up and acceptable complication rates. However, further study is needed to evaluate longer-term efficiency.
Supplementary Material
ABBREVIATIONS:
- SL
single-layer
- WEB
Woven EndoBridge
Footnotes
Disclosures: Jacques Moret—UNRELATED: Consultancy: Medtronic, MicroVention, Stryker, Balt. Laurent Spelle—UNRELATED: Consultancy: Medtronic, MicroVention, Stryker, Balt.
J.-B. Girot and J. Caroff contributed equally to this work.
References
- 1.Molyneux AJ, Kerr RSC, Yu LM, et al. International Subarachnoid Aneurysm Trial (ISAT) Collaborative Group. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet 2005;366:809–17 10.1016/S0140-6736(05)67214-5 [DOI] [PubMed] [Google Scholar]
- 2.Abecassis IJ, Zeeshan Q, Ghodke BV, et al. Surgical versus endovascular management of ruptured and unruptured intracranial aneurysms: emergent issues and future directions. World Neurosurg 2020;136:17–27 10.1016/j.wneu.2019.12.127 [DOI] [PubMed] [Google Scholar]
- 3.UCAS Japan Investigators, Morita A, Kirino T, et al. The natural course of unruptured cerebral aneurysms in a Japanese cohort. N Engl J Med 2012;366:2474–82 10.1056/NEJMoa1113260 [DOI] [PubMed] [Google Scholar]
- 4.Korja M, Lehto H, Juvela S. Lifelong rupture risk of intracranial aneurysms depends on risk factors: a prospective Finnish cohort study. Stroke 2014;45:1958–63 10.1161/STROKEAHA.114.005318 [DOI] [PubMed] [Google Scholar]
- 5.Salih M, Harris D, Moore J, et al. Current management of small unruptured intracranial aneurysms in the United States: results of a national survey. World Neurosurg 2021;146:e631–38 10.1016/j.wneu.2020.10.149 [DOI] [PubMed] [Google Scholar]
- 6.Ikawa F, Morita A, Tominari S, et al. Japan Neurosurgical Society for UCAS Japan Investigators. Rupture risk of small unruptured cerebral aneurysms. J Neurosurg 2019. January 25. [Epub ahead of print] 10.3171/2018.9.JNS181736 [DOI] [PubMed] [Google Scholar]
- 7.Choi JH, Park HS. The incidence and characteristics of patients with small ruptured aneurysms (<5 mm) in subarachnoid hemorrhage. J Korean Neurosurg Soc 2017;60:424–32 10.3340/jkns.2016.0910.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pierot L, Spelle L, Vitry F; ATENA Investigators. Immediate clinical outcome of patients harboring unruptured intracranial aneurysms treated by endovascular approach: results of the ATENA study. Stroke 2008;39:2497–504 10.1161/STROKEAHA.107.512756 [DOI] [PubMed] [Google Scholar]
- 9.Cognard C, Pierot L, Anxionnat R, et al. Clarity Study Group. Results of embolization used as the first treatment choice in a consecutive nonselected population of ruptured aneurysms: clinical results of the Clarity GDC study. Neurosurgery 2011;69:837–41; discussion 842 10.1227/NEU.0b013e3182257b30 [DOI] [PubMed] [Google Scholar]
- 10.Malhotra A, Wu X, Forman HP, et al. Management of tiny unruptured intracranial aneurysms: a comparative effectiveness analysis. JAMA Neurol 2018;75:27–34 10.1001/jamaneurol.2017.3232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pierot L, Gubucz I, Buhk JH, et al. Safety and efficacy of aneurysm treatment with the WEB: results of the WEBCAST 2 study. AJNR Am J Neuroradiol 2017;38:1151–55 10.3174/ajnr.A5178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pierot L, Costalat V, Moret J, et al. Safety and efficacy of aneurysm treatment with WEB: results of the WEBCAST study. J Neurosurg 2016;124:1250–56 10.3171/2015.2.JNS142634 [DOI] [PubMed] [Google Scholar]
- 13.Pierot L, Moret J, Turjman F, et al. WEB treatment .of intracranial aneurysms: clinical and anatomic results in the French Observatory. AJNR Am J Neuroradiol 2016;37:655–59 10.3174/ajnr.A4578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sivan-Hoffmann R, Gory B, Riva R, et al. One-year angiographic follow-up after WEB-SL endovascular treatment of wide-neck bifurcation intracranial aneurysms. AJNR Am J Neuroradiol 2015;36:2320–24 10.3174/ajnr.A4457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Da Ros V, Bozzi A, Comelli C, et al. Ruptured intracranial aneurysms treated with Woven Endobridge intrasaccular flow disruptor: a multicenter experience. World Neurosurg 2019;122:e498–505 10.1016/j.wneu.2018.10.088 [DOI] [PubMed] [Google Scholar]
- 16.Caroff J, Mihalea C, Dargento F, et al. Woven Endobridge (WEB) device for endovascular treatment of ruptured intracranial wide-neck aneurysms: a single-center experience. Neuroradiology 2014;56:755–61 10.1007/s00234-014-1390-7 [DOI] [PubMed] [Google Scholar]
- 17.Lubicz B, Mine B, Collignon L, et al. WEB device for endovascular treatment of wide-neck bifurcation aneurysms. AJNR Am J Neuroradiol 2013;34:1209–14 10.3174/ajnr.A3387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mihalea C, Caroff J, Pagiola I, et al. Safety and efficiency of the fifth generation Woven EndoBridge device: technical note. J Neurointerv Surg 2019;11:511–55 10.1136/neurintsurg-2018-014343 [DOI] [PubMed] [Google Scholar]
- 19.Pierot L, Moret J, Barreau X, et al. Aneurysm treatment with Woven EndoBridge in the cumulative population of three prospective, multicenter series: 2-year follow-up. Neurosurgery 2020;87:357–67 10.1093/neuros/nyz557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arthur AS, Molyneux A, Coon AL, et al. WEB-IT Study investigators. The safety and effectiveness of the Woven EndoBridge (WEB) system for the treatment of wide-necked bifurcation aneurysms: final 12-month results of the pivotal WEB Intrasaccular Therapy (WEB-IT) study. J Neurointerv Surg 2019;11:924–30 10.1136/neurintsurg-2019-014815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brinjikji W, Cloft HJ, Kallmes DF. Difficult aneurysms for endovascular treatment: overwide or undertall? AJNR Am J Neuroradiol 2009;30:1513–17 10.3174/ajnr.A1633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Caroff J, Mihalea C, Neki H, et al. Role of C-arm VasoCT in the use of endovascular WEB flow disruption in intracranial aneurysm treatment. AJNR Am J Neuroradiol 2014;35:1353–57 10.3174/ajnr.A3860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Caroff J, Mihalea C, Tuilier T, et al. Occlusion assessment of intracranial aneurysms treated with the WEB device. Neuroradiology 2016;58:887–91 10.1007/s00234-016-1715-9 [DOI] [PubMed] [Google Scholar]
- 24.Yamaki VN, Brinjikji W, Murad MH, et al. Endovascular treatment of very small intracranial aneurysms: meta-analysis. AJNR Am J Neuroradiol 2016;37:862–67 10.3174/ajnr.A4651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zheng Y, Song Y, Liu D, et al. Stent-assisted coiling embolization of tiny, wide-necked intracranial aneurysms. Acta Neurochir (Wien) 2017;159:93–100 10.1007/s00701-016-3022-y [DOI] [PubMed] [Google Scholar]
- 26.Nguyen TN, Raymond J, Guilbert F, et al. Association of endovascular therapy of very small ruptured aneurysms with higher rates of procedure-related rupture. J Neurosurg 2008;108:1088–92 10.3171/JNS/2008/108/6/1088 [DOI] [PubMed] [Google Scholar]
- 27.Goertz L, Liebig T, Siebert E, et al. Low-profile intra-aneurysmal flow disruptor WEB 17 versus WEB predecessor systems for treatment of small intracranial aneurysms: comparative analysis of procedural safety and feasibility. AJNR Am J Neuroradiol 2019;40:1766–72 10.3174/ajnr.A6183 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.