Abstract
Objective:
To evaluate potential differences in therapeutic outcomes between youths who completed a full course of treatment as planned compared to youths who terminated treatment prematurely.
Method:
Using longitudinal data from the National Child Traumatic Stress Network (NCTSN) Core Data Set, the present study examined demographic characteristics, trauma history, scores on standardized measures, and ratings of functional impairment and behavior problems in a large clinical sample of children and adolescents exposed to trauma who received treatment at NCTSN centers across the United States. Baseline and follow-up data were used to compare treatment completers (n = 3,108) and noncompleters (n = 4,029).
Results:
Both treatment completers and noncompleters received benefits from treatment by NCTSN mental health providers in that both groups showed significant decreases in mean scores from baseline to follow-up on all standardized measures. However, compared to noncompleters, treatment completers showed three types of significantly greater benefit at follow-up. These included: (a) greater rates of decline (i.e., steeper slopes) on all outcome measures; (b) greater reductions in the odds of falling within the clinical range on standardized measures; and (c) greater reductions in the odds of exhibiting functional impairment and behavior problems at follow-up. In contrast, compared to treatment completers, noncompleters reported significantly higher rates of lifetime exposure to community violence, psychological maltreatment, physical abuse, neglect, sexual abuse, and sexual assault.
Conclusion:
These findings underscore the value of incorporating engagement and retention strategies in treatments for traumatized youths to maximize therapeutic benefit and raise the standard of care.
Over the past three decades, the field of child traumatic stress has witnessed a proliferation of trauma-focused, evidence-based treatments (EBTs) designed to effectively address the diverse clinical needs of children and families exposed to an array of traumatic events (Dorsey et al., 2017; Silverman & Hinshaw, 2008). However, these advances have not been matched with commensurate advances in treatment engagement and retention strategies that facilitate adherence and completion of treatment (Ofonedu, Belcher, Budhathoki, & Gross, 2017). Indeed, premature dropout and early termination of services—factors that have long concerned child mental health practitioners and researchers alike—continue to hinder youths and families from reaping the full benefits of treatment (Yasinskia et al., 2018). Rates of premature dropout in child mental health services vary considerably, ranging from 28% to 75% (De Haan, Boon, de Jong, Hoeve, & Vermeiren, 2013; Kazdin, 1996; Kazdin & Mazurick, 1994). Dropout and early termination have also been linked to functional impairment, symptoms, psychiatric conditions, and comorbidities (Murphy et al., 2014; Sprang et al., 2013; Yasinskia et al., 2018).
Social determinants of health and other disparities have exacerbated these trends for low-income and historically underrepresented racial and ethnic populations seeking mental health services (Ofonedu et al., 2017; Satcher, 2001). The sequelae of trauma exposure have been well documented; however, many gaps remain regarding how dropout and risk factors for early termination influence child outcomes. Major initiatives such as the National Child Traumatic Stress Network (NCTSN) play a critical role in addressing public health concerns by raising the standard of care for traumatized children and their families, including improving treatment retention to maximize therapeutic benefit.
Soon after the inception of the NCTSN, and as a result of the Children’s Health Act (106th Congress, 2000), the United States General Accounting Office issued a report describing the effectiveness of federally funded programs for traumatized children as “largely unknown” (U.S. General Accounting Office, 2002). The GAO report specifically noted that:
Moreover, little is known about the effectiveness of federal programs that can help children who have experienced trauma to obtain mental health services or about gaps in access to needed services. SAMHSA’s National Child Traumatic Stress Initiative, which is specifically designed to take a coordinated approach to improving mental health care for children who have experienced various kinds of trauma, plans to evaluate both its overall program and individual components. If carefully implemented, the SAMHSA evaluations have the potential to provide information on ways to effectively provide mental health services to children who have experienced trauma. (p. 4)
In response to this expectation, the UCLA/Duke University National Center for Child Traumatic Stress (NCCTS) implemented an electronic data capture system to monitor and evaluate NCTSN activities, including examining clinical outcomes among youths receiving services at NCTSN sites. The current study builds on prior investigations that have utilized the Core Data Set (CDS) (see Steinberg et al., 2014 for review). These studies characterize the youths served by NCTSN sites, including youths’ trauma history profiles, distress reactions, and functional impairment.
The rationale for the present study arose from five related lines of inquiry, including: (a) evidence from the psychotherapy literature of a general dose-response relation between therapy sessions completed and therapeutic benefit (Lambert, 2010); (b) calls to define and measure therapeutic benefit in ways that are relevant and transparent to stakeholders—that is, to augment emphasis on statistically significant change by incorporating indicators of clinically significant change (Kazdin, 2006); (c) an increasing focus within the traumatic stress field on characteristics of attrition and premature treatment termination among youths receiving trauma-focused treatment (Wamser-Nanney & Steinzor, 2016); (d) efforts to support parents/caregivers in promoting youths’ completion of trauma-focused treatment (Dorsey et al., 2014); and (e) efforts to integrate evidence-based engagement strategies to minimize premature treatment termination (McKay et al., 2004).
The aim of the present study was to evaluate potential differences in therapeutic outcomes between youths who completed a full course of treatment as planned (treatment completers) compared to youths who terminated prematurely (treatment noncompleters). We hypothesized that treatment completers would manifest greater therapeutic benefit than noncompleters by exhibiting at follow-up: (a) significantly larger change scores on distress measures; (b) significantly lower rates of falling in the clinical range on standardized clinical measures; and (c) significantly reduced odds of manifesting behavioral and functional problems. We also explored whether the baseline demographic and trauma history variables differed between completers versus noncompleters.
METHOD
The NCTSN Core Data Set (CDS)
The CDS is the first national web-based data collection tool designed to answer key questions relevant to researchers, practitioners, and policy makers in the field of child traumatic stress (Briggs et al., 2013; Steinberg et al., 2014). It contains detailed information on 19,073 children seen between 2004 and 2012 in 74 NCTSN-affiliated academic, hospital, and community service sites across the United States. Congressional appropriations to the NCCTS included funds to support CDS analytic reports addressing issues central to the NCTSN mission of raising the standard of care and increasing access to services for traumatized children and their families. The CDS includes assessment measures collected at baseline and every three months thereafter (or pre and post for shorter-term interventions). CDS data collection procedures complied with the Institutional Review Board of Duke University Health System and all federal regulations for human subject protection. Each participating NCTSN center complied with the regulatory guidelines of their respective institutions.
Study Groups
The present study examined treatment outcomes among children and adolescents (N = 7,137) who received services from NCTSN centers. The sample included youths who (a) reported a history of at least one trauma; or (b) had a traumatic experience designated as a primary focus of treatment; or (c) received a trauma-related treatment. Youths were excluded from the analyses if they were missing date of birth. Two mutually exclusive groups were formed: those who completed treatment as planned (treatment completers) and those who did not (treatment noncompleters) for various reasons (e.g., case transferred to another clinic; child dropped out prior to completion; lost to follow-up for other reasons). Of these 7,137 youths, approximately 44% (N = 3,108) completed treatment as planned, whereas approximately 56% (N = 4,029) did not. Length of follow-up was defined as the total number of months elapsed between date of follow-up assessment indicating treatment completed as planned (for treatment completers) or the last available follow-up assessment (for noncompleters) minus date of baseline assessment (for both groups). The average number of months between baseline and follow-up for all study participants was 8.3 ± 6.8 months (median = 6.4, range: 0.03–96 months); the median length of followup for treatment completers was 6.2 months and 6.5 months for noncompleters.
The majority (75%) of youths received an evidence-based trauma-focused treatment (e.g., Trauma-Focused Cognitive-Behavioral Therapy) as their primary intervention. The remainder did not receive a trauma-focused intervention as their primary treatment but received other evidence-supported treatments. Some youths who received a primary trauma-focused intervention also received an ancillary intervention (e.g., psychoeducation, acute interventions, social skills training). Overall, 90% of study subjects received a trauma-informed intervention as either a primary or secondary mode of treatment.
Instruments
Trauma History
The Trauma History Profile (THP) was derived from the General Trauma and Trauma Detail Form and the Trauma History section of the UCLA Posttraumatic Stress Reaction Index for DSM-IV (PTSD-RI) (Steinberg et al., 2013). This form was completed by the provider at intake or early in the course of services and supplemented over the course of treatment as new traumas were revealed or occurred. Multiple informants, including the youths, caregivers, and other collaterals (e.g., case worker) contributed information about the child’s trauma history, noting whether experiences were confirmed or suspected. The THP covers 19 different trauma types and includes an option to report other traumas not specified. Clinicians were supplied with standardized definitions for each trauma type modeled after the National Child Abuse and Neglect Data System Glossary (U.S. Department of Health and Human Services, Administration for Children and Families, Children’s Bureau, 2000). The THP also collects data on the age(s) over which an endorsed trauma occurred, whether the child experienced or witnessed the trauma, and specific details about the traumatic experience.
The UCLA PTSD Reaction Index for DSM-IV (PTSD-RI) (Steinberg, Brymer, Decker, & Pynoos, 2004); Steinberg et al., 2013) was used in this study to assess PTSD symptoms in youths aged 7–21. The symptom scale maps directly onto DSM-IV criteria and assesses the number of days during the past month (0 = none of the time to 4 = most of the time) in which the symptom occurred. Scoring procedures permit tabulation of a PTSD-RI Total Score, as well as B (Intrusion), C (Avoidance), and D (Arousal) subscale scores. The PTSD-RI has previously shown strong psychometric properties with Cronbach’s α ranging from .88 to .90 across racial/ethnic groups and from .86 to .90 across age groups for boys and .89 to .90 across age groups for girls (Contractor et al., 2013; Elhai, Layne, & Steinberg et al., 2013). The present study produced a total-scale α of 0.97 and used a cutoff of ≥ 38 to classify youths whose scores fell in the clinical range (Steinberg et al., 2013).
The Trauma Symptom Checklist for Children-Alternate (TSCC-A) (Briere, 1996) assesses distress symptoms in children and adolescents aged 8–16. It contains five clinical subscales (Anxiety, Depression, Anger, Posttraumatic Stress, and Dissociation). The TSCC-A was normed on a large, racially and economically diverse youth sample, demonstrating robust psychometric properties (Sadowski & Friedrich, 2000). For the present study, we used the first four subscales (Cronbach’s α range = 0.94–0.95), and classified T-scores ≥ 65 as falling in the clinical range.
The Child Behavior Checklist (Achenbach & Rescorla, 2001) is completed by a parent or caregiver for youths aged 1½−5 and 6–18 years. The CBCL yields scores on two broad-spectrum scales for internalizing and externalizing problems and a total score created by summing internalizing and externalizing scores. In the present study, Cronbach’s α were .99 for both age groups. T-scores ≥64 (for ages < 6 years of age), and ≥70 (for 6–18 years of age) were classified as falling in the clinical range.
Indicators of Severity of Problems, a measure developed for the CDS, was used to rate the severity of a range of behavior problems and functional impairments. Domains included: academic problems; behavior problems in school or day care; problems with skipping school; behavior problems at home or in the community; suicidality; other self-injurious behaviors; developmentally inappropriate sexualized behaviors; alcohol use; substance use; attachment problems; criminal activity; running away from home; sexual exploitation experiences; and other medical problems or disabilities. Clinicians rated each problem on a 3-point scale consisting of not a problem, sometimes a problem, very much a problem. In the analyses, responses to each problem were collapsed into a dichotomous variable (0 = not a problem; 1 = sometimes or very much a problem).
Statistical Analyses
Descriptive statistics and frequencies for demographic and trauma history variables were generated for both groups. To account for clustering of youths within NCTSN centers, group comparisons were conducted using a random-effects model for continuous and the Cochran-Mantel-Haenszel (CMH) test for categorical variables. Descriptive statistics and frequencies for all continuous and binary outcomes were generated for baseline and follow-up within each study group. Generalized estimating equation (GEE) regression models (Molenberghs, Fitzmaurice, Kenward, Tsiatis, & Verbeke, 2014) with specified link functions (i.e., identity and logit for continuous measures and binary outcomes respectively) were used to compare changes in outcomes from baseline to follow-up between the two groups.
Model covariates included group (treatment completers vs. noncompleters), length of follow-up time (in months), and a group-by-time interaction term. Models also included a subject-level random effect to account for repeated measures within subjects. Cutoff values were used to calculate percentages of youths whose scores fell within the clinical range at both baseline and follow-up. Changes in the percentage of cases falling within the clinical range were compared between the two groups using the model described previously.
Multivariate imputation by fully conditional specification (FCS) was used to handle missing outcomes through a three-step approach (Molenberghs et al., 2014). Steps included (a) creating 10 imputed data sets, (b) using the GEE regression model described previously to analyze each imputed data set, and (c) combining the results to form multiple imputation estimates and inferential statistics. The improvement in continuous measures from baseline to follow-up within each study group and differences between groups were estimated through model contrasts and summarized using slopes (i.e., rate of decline from baseline to follow-up) and standard errors (SEs). The estimated yearly reductions in continuous measures from the aforementioned regressions were also plotted by group. Similarly, the reductions in proportions of binary outcomes (i.e., slope from baseline to follow-up) within each study group, and group differences in reductions, were estimated and summarized using odds ratios (OR) with 95% confidence intervals (95% CI). Last, sensitivity analyses were conducted for the clinical measures that differed at baseline between groups by adjusting for their baseline scores in the regression models.
RESULTS
Table 1 presents baseline demographic characteristics for youths by study group. Among the 7,137 youths who received treatment from NCTSN centers, the distributions of race/ethnicity between the two groups were similar. Approximately 40% in each group were White; a slightly higher percentage of Hispanic youths were treatment completers (39%) than noncompleters (35%) (p = .01), whereas a lower percentage of Black youths were treatment completers (18%) than noncompleters (21%) (p = .01). The median number of total trauma types was the same for both treatment groups (median = 3; range = 0–15).
TABLE 1.
Demographic and Trauma Characteristics by Treatment Completion Group
| Study Group (N = 7,137) |
|||
|---|---|---|---|
| Characteristics | Total (N = 7,137) | Treatment Noncompleters (N = 4,029) | Treatment Completers (N = 3,108) |
| Agea,*, mean (SD) | 11.0 (4.4) | 10.9 (4.4) | 11.1 (4.4) |
| Malesb,c N (%) | 3,270 (45.8) | 1,842 (45.7) | 1,428 (46.0) |
| Race/ethnicityb, N (%) | |||
| White | 2,775 (38.9) | 1,559 (38.7) | 1,216 (39.1) |
| Black | 1,402 (19.6) | 856 (21.3) | 546 (17.6) |
| Hispanic | 2,601 (36.4) | 1,399 (34.7) | 1,202 (38.7) |
| Other | 227 (3.18) | 137 (3.40) | 90 (2.90) |
| Unknown/missing | 132 (1.85) | 78 (1.94) | 54 (1.74) |
| Number of trauma typesb,*, N (%) | |||
| Mean (SD); median | 3.6 (2.6); 3 | 3.6 (2.7); 3 | 3.6 (2.6); 3 |
| None | 106 (1.49) | 64 (1.59) | 42 (1.35) |
| Fewer than 4 | 3,209 (45.0) | 1,757 (43.6) | 1,452 (46.7) |
| 4 or more total types | 3,268 (45.8) | 1,853 (46.0) | 1,415 (45.5) |
| Unknown/missing | 554 (7.76) | 355 (8.81) | 199 (6.40) |
| Trauma Typeb,d | |||
| Domestic violence | 3,469 (48.6) | 1,969 (48.9) | 1,500 (48.3) |
| Impaired caregiver | 3,357 (47.0) | 1,864 (46.3) | 1,493 (48.0) |
| Community violence* | 2,823 (39.6) | 1,655 (41.1) | 1,168 (37.6) |
| Psychological maltreatment* | 2,651 (37.1) | 1,558 (38.7) | 1,093 (35.2) |
| Physical maltreatment/abuse** | 2,166 (30.4) | 1,294 (32.1) | 872 (28.1) |
| Neglect *** | 1,802 (25.3) | 1,095 (27.2) | 707 (22.8) |
| Sexual maltreatment/abuse** | 1,633 (22.9) | 1,022 (25.4) | 611 (19.7) |
| War/Terrorism/Political violence inside the U.S. | 1,321 (18.5) | 657 (16.3) | 664 (21.4) |
| Sexual assault/rape* | 1,080 (15.1) | 642 (15.9) | 438 (14.1) |
| War/terrorism/political violence outside U.S. | 958 (13.4) | 485 (12.0) | 473 (15.2) |
| Kidnapping | 880 (12.3) | 429 (10.7) | 451 (14.5) |
| Physical assault* | 831 (11.6) | 466 (11.6) | 365 (11.7) |
| Natural disaster | 695 (9.74) | 360 (8.94) | 335 (10.8) |
| Traumatic loss or bereavement | 550 (7.71) | 248 (6.16) | 302 (9.72) |
| School violence | 461 (6.46) | 238 (5.91) | 223 (7.18) |
| Forced displacement | 181 (2.54) | 97 (2.41) | 84 (2.70) |
| Extreme interpersonal violence | 159 (2.23) | 88 (2.18) | 71 (2.28) |
| Serious injury/accident | 100 (1.40) | 43 (1.07) | 57 (1.83) |
| Illness/medical trauma | 61 (0.85) | 35 (0.87) | 26 (0.84) |
Random-effects model was used.
Cochran-Mantel-Haenszel test was used.
One subject with missing gender.
Includes confirmed and suspected trauma.
p < .05
p < .001
p < .0001.
Table 1 also presents frequency distributions of each trauma type at baseline by study group. The percentages of 6 out of the 19 trauma types reported by treatment noncompleters were significantly higher than those reported by completers. These included sexual assault/rape (16% vs. 14%), sexual maltreatment/abuse (25% vs. 20%), neglect (27% vs. 23%), physical maltreatment/abuse (32% vs. 28%), psychological maltreatment (39% vs. 35%), and community violence (41% vs. 38%).
The upper section of Table 2 presents the mean standardized T-scores for the CBCL and TSCC-A and the mean scores for the B, C, D, and total PTSD-RI at baseline and follow-up by study group. GEE regression revealed that youths from both groups exhibited significant decreases from baseline on all outcome measures. Further, the estimated mean reduction was significanly greater for treatment completers than treatment noncompleters on all outcome measures (all ps < .01). For example, the mean decrease of 11.2 (a drop from 27.5 to 16.3) in total PTSD-RI score reported by treatment completers was significantly greater than that reported by treatment noncompleters (mean decrease = 7.2; a reduction from 27.6 to 20.4; p < .0001). Given that CBCL Externalizing Behavior and CBCL Total Score differed significantly between groups at baseline, sensitivity analyses adjusting for baseline scores revealed that the mean change scores of both CBCL outcome measures was significantly greater for treatment completers than for noncompleters (p < .0001).
TABLE 2.
Baseline and Follow-Up Means and Standard Deviations for Clinical Measures and Percent of Cases Falling in the Clinical Range by Treatment Completion Group and Comparisons Between Treatment Groups
| Study Group (N = 7,137) |
||||||
|---|---|---|---|---|---|---|
| Not Completed as Planned (N = 4,029) |
Completed as Planned (N = 3,108) |
Comparison Between Study Groups |
||||
| Standardized T-Score, Mean Score (SD) | Baseline | Follow-up | Baseline | Follow-up | Difference in Slopes (SE) | P |
| CBCL | N = 3,317 | N = 1,705 | N = 2,385 | N = 1,717 | ||
| Externalizing behavior* | 62.3 (11.5) | 58.6 (11.8) | 61.4 (11.6) | 53.9 (12.0) | −0.26 (0.05) | <.0001 |
| Internalizing behavior | 61.7 (11.2) | 57.8 (11.6) | 61.7 (11.3) | 53.1 (12.0) | −0.25 (0.05) | <.0001 |
| Total Score* | 63.0 (10.9) | 58.8 (11.9) | 62.4 (11.0) | 53.6 (12.4) | −0.28 (0.05) | <.0001 |
| TSCC-A | N = 2,309 | N = 1,184 | N = 1,949 | N = 1,739 | ||
| Anger | 50.6 (11.1) | 47.1 (10.7) | 50.1 (11.5) | 44.8 (9.92) | −0.16 (0.04) | <.0001 |
| Anxiety | 52.9 (13.4) | 47.6 (12.0) | 52.6 (13.0) | 45.7 (10.9) | −0.12 (0.05) | 0.0086 |
| Depression | 51.8 (12.7) | 46.4 (11.1) | 51.2 (12.1) | 44.1 (10.1) | −0.16 (0.04) | 0.0006 |
| Posttraumatic Stress | 53.0 (11.9) | 47.2 (10.9) | 52.9 (11.7) | 45.3 (9.87) | −0.14 (0.04) | 0.0010 |
| PTSD–RI | N = 2,528 | N = 1,484 | N = 1,985 | N = 1,885 | ||
| Criteria B | 7.80 (5.51) | 5.27 (4.90) | 7.95 (5.47) | 4.18 (4.29) | −0.07 (0.02) | 0.0010 |
| Criteria C | 10.1 (6.63) | 7.20 (6.14) | 10.1 (6.76) | 5.70 (5.66) | −0.08 (0.02) | 0.0007 |
| Criteria D | 9.71 (4.80) | 7.88 (4.69) | 9.48 (4.79) | 6.38 (4.48) | −0.07 (0.02) | 0.0002 |
| Total Score | 27.6 (15.0) | 20.4 (14.1) | 27.5 (15.1) | 1. (12.9) | −0.21 (0.05) | 0.0001 |
| % Cases in Clinical Range§, N (%) | Slope Comparison (OR)a (95% CI) | P | ||||
| CBCLb | ||||||
| Externalizing behavior* | 1,026 (30.9) | 363 (21.3) | 679 (28.5) | 222 (12.9) | 0.59 (0.44, 0.79) | 0.0004 |
| Internalizing behavior | 1,016 (30.6) | 343 (20.1) | 731 (30.7) | 198 (11.5) | 0.53 (0.39, 0.73) | 0.0001 |
| Total Score* | 1,191 (35.9) | 416 (24.4) | 784 (32.9) | 247 (14.4) | 0.58 (0.43, 0.78) | 0.0005 |
| TSCC-Ac | ||||||
| Anger | 295 (12.8) | 101 (8.53) | 259 (13.3) | 107 (6.15) | 0.57 (0.37, 0.87) | 0.0089 |
| Anxiety | 436 (18.9) | 128 (10.8) | 346 (17.8) | 119 (6.84) | 0.55 (0.34, 0.88) | 0.0153 |
| Depression | 388 (16.8) | 93 (7.85) | 290 (14.9) | 96 (5.52) | 0.51 (0.27, 0.98) | 0.0423 |
| Post-Traumatic Stress | 416 (18.0) | 97 (8.19) | 345 (17.7) | 93 (5.35) | 0.49 (0.29, 0.82) | 0.0075 |
| Total PTSD-RId | 710 (28.1) | 203 (13.7) | 522 (26.3) | 150 (7.96) | 0.51 (0.33, 0.81) | 0.0045 |
Note. CBCL = Child Behavior Checklist; TSCC-A = Trauma Symptom Checklist for Children–Alternate; PTSD-RI = PTSD Reaction Index.
Significant difference in baseline scores between the two groups (p < .05).
Missing category not included in percentage calculation.
Comparison (binary) of difference in odds ratios of falling within the clinical range from baseline to follow-up between study groups.
T-scores ≥ 64 (for < 6 years of age) and ≥ 70 (for ≥ 6 years of age) were interpreted as in the clinical range.
T-scores ≥ 65 interpreted as in the clinical range on all TSCC-A clinical subscales.
Total PTSD-RI scores ≥ 38 interpreted as in the clinical range.
Compared to treatment noncompleters, treatment completers showed a significantly steeper rate of decline per month in CBCL total scale scores (slopes: −0.51 vs. −0.23 [not shown]); difference in slopes: −0.28, p < .0001; CBCL externalizing behaviors (difference in slopes: −.26, p < .0001); and CBCL internalizing behaviors (difference in slopes: −0.25, p < .0001) after accounting for length of follow-up. Similar findings emerged in relation to TSCC-A subscale scores, including Anger (difference in slopes: −0.16, p = 0.0001), Anxiety (difference in slopes: −0.12, p = 0.0086), Depression (difference in slopes: −0.16, p = 0.0006), and Posttraumatic Stress (difference in slopes: −0.14, p = 0.001). Similar findings also emerged for the PTSD-RI subscale scores including Criterion B (p = 0.001), Criterion C (p = 0.0007), Criterion D (p = 0.0002), and the total PTSD-RI score (p = 0.0001).
As also shown in the lower portion of Table 2, percentages of youths whose baseline scores fell in the clinical range were comparable across the two groups for all measures, except CBCL Externalizing Behavior (31% for treatment noncompleters, 29% for completers, p = 0.045) and CBCL Total Scores (36% for treatment noncompleters, 33% for completers, p = 0.018). The percentages of youths who scored above the clinical range on all measures decreased significantly from baseline to follow-up for both groups. However, treatment completers had significantly greater reductions in the percentage of youths who fell within the clinical range at follow-up compared to treatment noncompleters on all measures (all ps < 0.05).
Moreover, the estimated odds that CBCL total scores would fall within the clinical range at follow-up (compared to baseline) significantly decreased for both treatment noncompleters (OR = 0.71, 95% CI: 0.63–0.81, not shown) and treatment completers (OR = 0.41, 95% CI: 0.31–0.55, not shown). Comparing the rate of change for treatment completers and noncompleters, treatment completers showed significantly steeper reductions in the odds of falling within the clinical range per year than noncompleters (OR = 0.58, 95% CI: 0.43–0.78). Similarly, the estimated odds that total PTSD-RI scores would fall within the clinical range at follow-up (compared to baseline) significantly decreased for both treatment noncompleters and treatment completers (OR: 0.38 vs. 0.19 respectively, not shown). Comparing treatment completers and noncompleters, the estimated reduction in the odds for falling within the clinical range for total PTSD-RI score decreased more steeply from baseline to follow-up for treatment completers (OR = 0.51, 95% CI: 0.33–0.81).
Figure 1 depicts the estimated mean reduction per year from baseline to follow-up for each measure by study group. Treatment completers exhibited a significantly greater average decrease on all study measures. For example, the estimated decreases in CBCL total scores for youths who did, versus did not, complete treatment as planned were 6.1 versus 2.7 respectively. Similarly, the estimated mean reduction per year in PTSD-RI total score for youths who did versus did not complete treatment as planned was 8.4 and 5.9 respectively.
FIGURE 1.
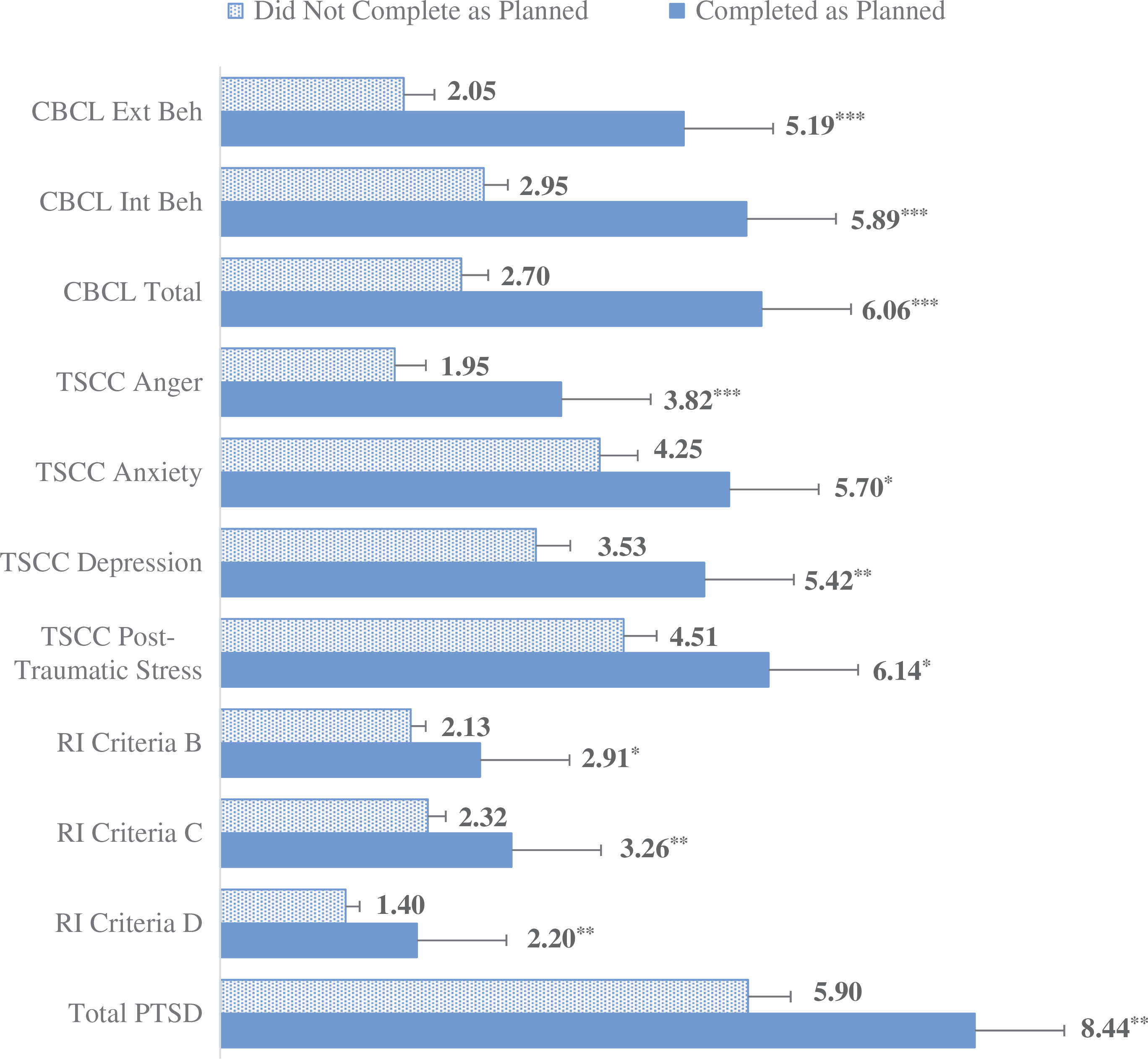
Estimated Decline (With Standard Error) in Clinical Measures From Baseline by Study Group.
*A significant difference in yearly decline between the two study groups was observed.
*P < .05; **P < .001; ***P < .0001.
Table 3 presents the frequencies of problems in behavior and functioning for treatment completers versus noncompleters at both baseline and follow-up, as well as regression summaries. At baseline, more than 40% of youths reported the following problems for treatment completers versus noncompleters: academic problems (52% vs. 50%), behavior problems at home/community (61% vs. 57%) or in school/daycare (47% vs. 45%), and attachment problems (45% vs. 42%). Also at baseline, between 10% and 20% of youths reported the following problems for completers versus noncompleters: sucidality (17% vs. 13%), developmentally inappropriate sexual behaviors (17% vs. 13%), other self-injury (14% vs. 12%), and skipping school (13% vs. 14%). Last, 10% or fewer reported the following problems at baseline: alcohol and substance use, criminal activity, and running away from home. At follow-up, youths from both groups reported a lower prevalence of all types of problems. For example, academic problems decreased from 52% to 31% for noncompleters and from 50% to 32% for completers. Additionally, behavior problems at home/community dropped from 61% to 36% for noncompleters and from 57% to 31% for completers.
TABLE 3.
Frequencies and Between-Groups Odd Ratios for Problems with Behavior and Functioning at Baseline and Follow-up
| Not Completed as Planned (N = 4,029) | Completed as Planned (N = 3,108) | Odds Ratio Comparison Between Study Groups | ||||
|---|---|---|---|---|---|---|
| Type of Problem, N (%) | Baseline | Follow-up | Baseline | Follow-up | Odds Ratio (95% CI) | p |
| Academic problems* | 2,092 (51.9) | 1,235 (30.7) | 1,563 (50.3) | 1,006 (32.4) | 0.69 (0.59, 0.81) | <.0001 |
| Problem in school or day care* | 1,884 (46.8) | 1,118 (27.8) | 1,403 (45.2) | 791 (25.5) | 0.58 (0.49, 0.70) | <.0001 |
| Skipping school | 523 (13.0) | 315 (7.82) | 419 (13.5) | 161 (5.18) | 0.37 (0.26, 0.52) | <.0001 |
| Problems at home or community* | 2,466 (61.2) | 1,455 (36.1) | 1,754 (56.5) | 969 (31.2) | 0.61 (0.51, 0.73) | <.0001 |
| Suicidality* | 677 (16.8) | 249 (6.18) | 413 (13.3) | 114 (3.67) | 0.37 (0.21, 0.66) | 0.0007 |
| Other self-injurious behavior* | 571 (14.2) | 242 (6.01) | 384 (12.4) | 126 (4.06) | 0.42 (0.28, 0.65) | <.0001 |
| Inappropriate sexual behavior* | 678 (16.8) | 287 (7.13) | 397 (12.8) | 119 (3.83) | 0.42 (0.26, 0.68) | 0.0004 |
| Alcohol use | 265 (6.58) | 130 (3.23) | 234 (7.53) | 66 (2.12) | 0.27 (0.13, 0.58) | 0.0010 |
| Substance abuse | 365 (9.06) | 190 (4.72) | 318 (10.2) | 91 (2.93) | 0.26 (0.16, 0.42) | <.0001 |
| Attachment problems* | 1,800 (44.7) | 1,082 (26.9) | 1,310 (42.2) | 707 (22.8) | 0.52 (0.43, 0.63) | <.0001 |
| Criminal activity | 318 (7.89) | 129 (3.20) | 279 (8.98) | 62 (2.00) | 0.22 (0.09, 0.51) | 0.0007 |
| Running away from home | 274 (6.80) | 153 (3.80) | 208 (6.69) | 47 (1.51) | 0.15 (0.07, 0.34) | <.0001 |
A significant group difference at baseline was observed (p < .001).
Table 3 also presents differences in the reduction of behavior and functional problems between the two groups. For example, there was a significantly greater reduction in the odds of having academic problems from baseline to follow-up among treatment completers compared to noncompleters (OR = 0.69, 95% CI: 0.59, 0.81; p < .0001). Further, there was a significantly greater reduction in the odds of having attachment problems from baseline to follow-up among treatment completers than among noncompleters (OR = 0.52, 95% CI: 0.43, 0.63; p < .0001).
DISCUSSION
There is abundant evidence of a dose-response relation in the mainstream psychotherapy outcome literature between therapy sessions attended and derived therapeutic benefit (Lambert, 2010). The failure of a significant percentage of youths to complete treatment has been a longstanding concern in the child and adolescent mental health field (Dorsey et al., 2014; McKay et al., 2004). Results from this study underscore the value of this line of research by documenting both the general benefits of mental health treatment for traumatized youths and the added benefits associated with completing a full course of treatment. The present study, based on over 7,000 youths served by 74 NCTSN sites, provides evidence that treatment produces significant therapeutic benefits, even in the absence of completing a full course of treatment. Moreover, treatment completion produces incrementally greater benefits: Treatment completers had significantly steeper rates of decline from baseline to follow-up on a range of clinical measures, significantly increased odds of falling below the clinical range at follow-up on norm-referenced clinical measures, and significantly reduced odds of exhibiting behavioral and functional problems.
Throughout its 15-year history, the NCTSN has witnessed advances in practice parameters for treating traumatized children and adolescents (Cohen, 2010; Cook & Newman, 2014). The NCTSN has utilized these guidelines to promote evidence-based practice, including the use of validated measures and evidence-based trauma-focused interventions. The present findings inform these parameters by underscoring the importance of treatment engagement and retention strategies to maximize therapeutic benefit and improve the standard of care.
To date, treatment engagement and retention approaches have focused primarily on supplementing interventions with other strategies (e.g., motivational interviewing, reminder calls, bilingual therapists, evening appointments) designed to enhance client motivation, parent involvement, cultural understanding, and address barriers to care (Dorsey et al., 2014). In addition to these steps, the NCTSN is promoting the use of elements that can enhance trauma-focused treatment engagement and retention. Examples include addressing safety concerns early in treatment (DeRosa, Habib, & Pelcovitz et al., 2006), strengthening coping skills to modulate extreme negative emotions (Cloitre, Koenen, Coen, & Han, 2002), helping youths to manage trauma reminders and prioritize their most distressing experiences (Saltzman et al., 2017). Other efforts include adapting interventions for such high-risk populations as refugee families (Isakson, Legerski, & Layne, 2015), homeless youths (Burt et al., 1999), military families (Cozza, 2015), and American Indians (Gone & Alcantara, 2007).
Results from this study highlight the utility of assessing youths’ trauma histories. Such profiles can support risk screening and referral to trauma-focused treatment, the identification of potential markers for premature dropout, and signal a need for treatment retention strategies (Gopelan et al., 2010). Underscoring this utility, noncompleters had significantly higher percentages of exposure to psychological maltreatment, physical maltreatment/abuse, neglect, sexual abuse, sexual assault/rape, and community violence. In this regard, the present study design did not rule out the possibility that higher rates of preexisting trauma exposure among noncompleters contributed to the lower degree of clinical improvement. A lower degree of clinical improvement may have also been associated with less satisfaction with the rate or amount of therapeutic gain and a decrease in client engagement and motivation to continue in treatment.
Study Limitations and Strengths
The present findings emerged from a mixture of clinic-referred subgroups with different demographic and trauma history profiles, limiting generalizability of the results. The analyses accounted for the clustering of observations within subjects across NCTSN centers, but other sources of heterogeneity (e.g., demographic characteristics, urban vs. rural, SES, treatment protocol and modality used, provider characteristics) remain. Further, given the role of the CDS as a quality improvement initiative, no randomized control group was available, and varying degrees of compliance with data collection procedures across NCTSN sites resulted in missing data that required data imputation. In addition, although clinicians were trained in the administration and use of the Indicators of Severity of Problems, this measure requires further investigation of its clinical utility. Nevertheless, these indicators have proven useful across a range of studies in clarifying relations between trauma exposure and adolescent risk-taking behavior (Layne et al., 2014), relations between sexual abuse and functional impairment (Kisiel et al., 2014), behavioral and functional profiles of war-exposed refugee youths (Betancourt et al., 2012), and functional impairments in psychologically maltreated youths (Spinazzola et al., 2014).
Strengths of the present study include a large and diverse national sample of youths presenting for evaluation and treatment of trauma-related problems across a broad range of geographic regions and NCTSN settings. These settings include community mental health centers, residential programs, juvenile justice programs, child welfare agencies, community-based mental health clinics, and school-based mental health programs. Although not nationally representative, the current study is to our knowledge the largest trauma treatment outcome study of its kind.
There has been a steadily growing discussion in the treatment outcome literature regarding whether statistically significant change in scores on standardized outcome measures also constitutes “real-world” clinically significant change that is directly relevant to clinicians, clients, caregivers, insurers, policy makers, and other stakeholders (Becker, Chorpita, & Daleiden, 2011; Ferguson, Robinson, & Splaine, 2002; Jacobson & Truax, 1991; Kazdin, 2006; Lambert, 2010; Nietzel & Trull, 1988). This distinction has spawned the increasing use of metrics intended to demonstrate clinically significant change. Such metrics have included reducing test scores from a nonnormative to a normative range and evaluating whether indicators of functional impairment and behavior problems have improved by the end of treatment. The present study incorporated a broad range of assessment tools, including standardized and normed tests, validated clinical instruments, and clinician-rated indicators of behavior and functioning. Used in tandem, these study features revealed that treatment completion as planned was associated with higher odds of reductions in standardized test scores from an elevated to a normative range and with reduced odds of exhibiting functional impairment and behavior problems at the end of treatment.
Future Directions
Given the rich body of treatment information and clinical ratings in the NCTSN Core Data Set, planned future treatment outcome studies will include analyses taking into account: (a) client demographics; (b) trauma history and trauma-specific details; (c) comorbid conditions; (d) treatment provided; (e) length of treatment; (f) provider agency or organization type and region; (g) therapist type and level of training; and (h) client service use history.
ACKNOWLEDGMENTS
We would like to acknowledge the 74 centers within the NCTSN that have contributed data to the Core Data Set, as well as the staff, children, youths, and families at NCTSN centers throughout the United States (U.S.) who made this collaborative network possible. We also thank our colleagues and partners at the Center for Mental Health Services (CMHS)/Substance Abuse and Mental Health Services Administration (SAMHSA) for their leadership and guidance. The views, policies, and opinions expressed are those of the authors and do not necessarily reflect those of CMHS, SAMHSA or USDHHS. We also thank Carrie Purbeck Trunzo, MHA; Robert Lee, M. S., Courtney Smith, and Tracy Bethel, MPH. for their assistance with this study.
FUNDING
This work was supported by the Substance Abuse and Mental Health Services Administration [1U79SM062976–01].
Footnotes
DISCLOSURE STATEMENT
No potential conflict of interest was reported by the authors.
Contributor Information
Alan M. Steinberg, UCLA/Duke University National Center for Child Traumatic Stress in the UCLA Department of Psychiatry and Biobehavioral Sciences.
Christopher M. Layne, UCLA/Duke University National Center for Child Traumatic Stress in the UCLA Department of Psychiatry and Biobehavioral Sciences.
Ernestine C. Briggs, UCLA/Duke University National Center for Child Traumatic Stress in the Department of Psychiatry at Duke University.
Li-Jung Liang, UCLA Department of Medicine..
Melissa J. Brymer, UCLA/Duke University National Center for Child Traumatic Stress in the UCLA Department of Psychiatry and Biobehavioral Sciences.
Thomas R. Belin, UCLA Department of Biostatics and the UCLA Department of Psychiatry and Biobehavioral Sciences.
John A. Fairbank, UCLA/Duke University National Center for Child Traumatic Stress in the Department of Psychiatry at Duke University.
Robert S. Pynoos, UCLA/Duke University National Center for Child Traumatic Stress in the UCLA Department of Psychiatry and Biobehavioral Sciences.
REFERENCES
- 106th Congress. (2000). H. R. 4365 - Children’s Health Act of 2000. Public Law 106–310. 114 STAT. 1101. Published October 17, 2000. Retrieved July 3, 2018, from https://www.gpo.gov/fdsys/pkg/PLAW-106publ310/pdf/PLAW-106publ310.pdf [Google Scholar]
- Achenbach TM, & Rescorla LA (2001). Manual for the ASEBA school-age forms & profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- Becker KD, Chorpita BF, & Daleiden EL (2011). Improvement in symptoms versus functioning: How do our best treatments measure up? Administration and Policy in Mental Health and Mental Health Services Research, 38, 440–458. doi: 10.1007/s10488-010-0332-x [DOI] [PubMed] [Google Scholar]
- Betancourt TS, Newnham EA, Layne CM, Kim S, Steinberg AM, Ellis H, & Birman D (2012). Trauma history and psychopathology in war-affected refugee children referred for trauma-related mental health services in the United States. Journal of Traumatic Stress, 25(6), 682–690. doi: 10.1002/jts.21749 [DOI] [PubMed] [Google Scholar]
- Briere J (1996). Trauma symptom checklist for children. professional manual. Odessa, FL: Psychological Assessment Resources. [Google Scholar]
- Briggs EC, Fairbank JA, Greeson JKP, Layne CM, Steinberg AM, Amaya-Jackson LM, … Pynoos RS (2013). Links between child and adolescent trauma exposure and service use histories in a national clinic-referred sample. Psychological Trauma: Theory, Research, Practice and Policy, 5(2), 101–109. doi: 10.1037/a0027312 [DOI] [Google Scholar]
- Burt MR, Laudan YA, Douglas T, Valente J, Lee E, & Iwen B (1999). Homelessness: Programs and the people they serve: Findings of the national survey of homeless assistance providers and clients: Technical report prepared for the interagency council on the homeless. Washington, DC: The Council. [Google Scholar]
- Cloitre M, Koenen KC, Coen LR, & Han H (2002). Skills training in affective and interpersonal regulation followed by exposure: A phase-based treatment for PTSD related to childhood abuse. Journal of Consulting and Clinical Psychology, 70(5), 1067–1074. doi:10/1037//0022-006X.70.5.1067 [DOI] [PubMed] [Google Scholar]
- Cohen JA; The Work Group on Quality Issues; and the AACAP Work Group on Quality Issues. (2010). Practice parameter for the assessment and treatment of children and adolescents with posttraumatic stress disorder. Journal of Child and Adolescent Psychiatry, 49(4), 414–430. [PubMed] [Google Scholar]
- Contractor AA, Layne CM, Steinberg AM, Ostrowski SA, Ford JD, & Elhai JD (2013). Do gender and age moderate the symptom structure of PTSD? Findings from a national clinical sample of children and adolescents. Psychiatry Research, 210(3), 1056–1064. doi: 10.1016/j.psychres.2013.09.012 [DOI] [PubMed] [Google Scholar]
- Cook JM, & Newman E; New Haven Trauma Competency Group. (2014).A consensus statement on trauma mental health: The New Haven Competency conference process and major findings. Psychological Trauma: Theory, Research, Practice and Policy, 6(4), 300–307. [Google Scholar]
- Cozza SJ (2015). Meeting the intervention needs of military children and families. Journal of the American Academy of Child and Adolescent Psychiatry, 54(4), 247–248. doi: 10.1016/j.jaac.2015.01.012 [DOI] [PubMed] [Google Scholar]
- De Haan AM, Boon AE, de Jong JT, Hoeve M, & Vermeiren RR (2013). A metaanalytic review on treatment dropout in child and adolescent outpatient mental health care. Clinical Psychology Review, 33(5), 698–711. doi: 10.1016/j.cpr.2013.04.005 [DOI] [PubMed] [Google Scholar]
- DeRosa R, Habib M, Pelcovitz D, Rathus J, Sonnenklar J, & Ford J (2006). Structured Psychotherapy for Adolescents Responding to Chronic Stress (SPARCS). Unpublished treatment manual. Manhasset, NY: North Shore North Shore-Long Island Jewish Health System. [Google Scholar]
- Dorsey S, McLaughlin KA, Kerns SEU, Harrison JP, Lambert HK, Briggs EC, … Amaya-Jackson L (2017). Evidence base update for psychosocial treatments for children and adolescents exposed to traumatic events. Journal of Clinical Child and Adolescent Psychology, 46, 303–330. doi: 10.1080/15374416.2016.1220309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorsey S, Pullmann MD, Berliner L, Koschmann D, McKay M, & Deblinger E (2014). Engaging foster parents in treatment: A randomized trial of supplementing trauma-focused cognitive behavioral therapy with evidence-based engagement strategies. Child Abuse and Neglect, 38(9), 1508–1520. doi: 10.1016/j.chiabu.2014.03.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhai JD, Layne CM, Steinberg AS, Brymer MJ, Briggs MJ, Ostrowski SA, & Pynoos RS (2013). Psychometric properties of the UCLA PTSD reaction index. Part II: Investigating factor structure findings in a national clinic-referred youth sample. Journal of Traumatic Stress, 26, 10–18. doi: 10.1002/jts.21755 [DOI] [PubMed] [Google Scholar]
- Ferguson RJ, Robinson AB, & Splaine M (2002). Use of the reliable change index to evaluate clinical significance in SF-36 outcomes. Quality of Life Research, 11, 509–516. [DOI] [PubMed] [Google Scholar]
- Gone JP, & Alcantara CP (2007). Identifying effective mental health interventions for American Indians and Alaska Natives: A review of the literature. Cultural Diversity & Ethnic Minority Psychology, 13(4), 356–363. doi: 10.1037/1099-9809.13.4.356 [DOI] [PubMed] [Google Scholar]
- Gopelan G, Goldstein L, Klingenstein K, Sicher C, Blake C, & McKay M (2010). Engaging families into child mental health treatment: Updates and special considerations. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 19(3), 182–196. [PMC free article] [PubMed] [Google Scholar]
- Isakson BL, Legerski JP, & Layne CM (2015). Adapting and implementing evidence-based interventions for trauma-exposed refugee youth and families. Journal of Contemporary Psychotherapy, 45(4), 245–253. doi: 10.1007/s10879-015-9304-5 [DOI] [Google Scholar]
- Jacobson NS, & Truax P (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59, 12–19. [DOI] [PubMed] [Google Scholar]
- Kazdin AE (1996). Dropping out of child psychotherapy: Issues for research and implications for practice. Clinical Child Psychology and Psychiatry, 1(1), 133–156. doi: 10.1177/1359104596011012 [DOI] [Google Scholar]
- Kazdin AE (2006). Arbitrary metrics: Implications for identifying evidence-based treatments. American Psychologist, 61(1), 42–49. doi: 10.1037/0003-066X.61.1.42 [DOI] [PubMed] [Google Scholar]
- Kazdin AE, & Mazurick JL (1994). Dropping out of child psychotherapy: Distinguishing early and late dropouts over the course of treatment. Journal of Consulting and Clinical Psychology, 62(5), 1069–1074. doi: 10.1037/0022-006X.62.5.1069 [DOI] [PubMed] [Google Scholar]
- Kisiel C, Fehrenbach T, Liang L, Stolbach B, McClelland G, Griffin G, … Spinazzola J (2014). Examining child sexual abuse in relation to complex patterns of trauma exposure: Findings from the national child traumatic stress network. Psychological Trauma: Theory, Research, Practice and Policy, 6 (Suppl 1), S29–S39. doi: 10.1037/a0037812 [DOI] [Google Scholar]
- Lambert MJ (2010). Preventing treatment failure: The use of measuring, monitoring, and feedback in clinical practice. Washington, DC: American Psychological Association. [Google Scholar]
- Layne CM, Greeson JKP, Soeun K, Kim S, Reading S, Vivrette RL, … Pynoos RS (2014). Links between trauma exposure and adolescent high-risk health behaviors: Findings from the NCTSN core data set. Psychological Trauma: Theory, Research, Practice and Policy, 6(Suppl 1), S40–S49. doi: 10.1037/a0037799 [DOI] [Google Scholar]
- McKay MM, Hibbert R, Hoagwood K, Rodriguez J, Murray L, Legerski J, & Fernandez D (2004). Integrating evidence-based engagement interventions into “Real World” child mental health settings. Brief Treatment and Crisis Intervention, 4(2), 177–186. doi: 10.1093/brief-treatment/mhh014 [DOI] [Google Scholar]
- Molenberghs G, Fitzmaurice MG, Kenward MG, Tsiatis A, & Verbeke G (eds). (2014). Handbook of Missing Data Methodology. Boca Raton, FL: CRC Press. [Google Scholar]
- Murphy RA, Sink HE, GS A III, Carmody KA, Amaya-Jackson LM, & Briggs EC (2014). Predictors of treatment completion in a sample of youth who have experienced physical or sexual trauma. Journal of Interpersonal Violence, 29(1), 3–19. doi: 10.1177/0886260513504495 [DOI] [PubMed] [Google Scholar]
- Nietzel MT, & Trull TJ (1988). Meta-analytic approaches to social comparisons: A method for measuring clinical significance. Behavioral Assessment, 10(2), 159–169. [Google Scholar]
- Ofonedu ME, Belcher HE, Budhathoki C, & Gross DA (2017). Understanding barriers to initial treatment engagement among underserved families seeking mental health services. Journal of Child and Family Studies, 26(3), 863–876. doi: 10.1007/s10826-016-0603-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadowski CM, & Friedrich WN (2000). Psychometric properties of the Trauma Symptom Checklist for Children (TSCC) with psychiatrically hospitalized adolescents. Child Maltreatment, 5(4), 364–372. doi: 10.1177/1077559500005004008 [DOI] [PubMed] [Google Scholar]
- Saltzman WR, Layne CM, Pynoos RS, Olafson E, Kaplow JB, & Boat B (2017). Trauma and grief component therapy for adolescents: A modularized approach to assessing and treatment traumatized and bereaved youth. Cambridge, UK: Cambridge University Press. [Google Scholar]
- Department of Health and Human Services; Satcher D (2001). Mental health: Culture, race, and ethnicity – A supplement to mental health: A report of the surgeon general. Washington, DC: Author. [PubMed] [Google Scholar]
- Silverman WK, & Hinshaw SP (2008). The second special issue on evidence-based psychosocial treatments for children and adolescents: A 10-year update. Journal of Clinical Child and Adolescent Psychology, 37, 1–7. doi: 10.1080/15374410701817725 [DOI] [PubMed] [Google Scholar]
- Spinazzola J, Hodgdon H, Liang L, Ford JD, Layne CM, Pynoos R, … Kisiel C (2014). Unseen wounds: The contribution of psychological maltreatment to child and adolescent mental health and risk outcomes. Psychological Trauma: Theory, Research, Practice and Policy, 6(Suppl 1), S18–S28. doi: 10.1037/a0037766 [DOI] [Google Scholar]
- Sprang G, Craig CD, Clark JJ, Vergon K, Tindall MS, Cohen J, & Gurwitch R (2013). Factors impacting the completion of trauma-focused treatments: What can make a difference? Traumatology, 19, 28–40. doi: 10.1177/1534765612445931 [DOI] [Google Scholar]
- Steinberg AM, Brymer M, Decker K, & Pynoos RS (2004). The UCLA PTSD Reaction Index. Current Psychiatry Reports, 6, 96–100. [DOI] [PubMed] [Google Scholar]
- Steinberg AM, Brymer MJ, Kim S, Briggs EC, Ippen CG, Ostrowski SA, … Pynoos RS (2013). Psychometric properties of the UCLA PTSD Reaction Index: Part 1. Journal of Traumatic Stress, 26(1), 1–9. doi: 10.1002/jts.21780 [DOI] [PubMed] [Google Scholar]
- Steinberg AM, Pynoos RS, Gerrity ET, Gerrity ET, Layne CM, Vivrette RL, … Fairbank JA (2014). The NCTSN core data set: Emerging findings, future directions, and implications for theory, research, practice, and policy. Psychological Trauma: Theory, Research, Practice and Policy, 6(Suppl 1), S50–S57. doi: 10.1037/a0037798 [DOI] [Google Scholar]
- U.S. Department of Health and Human Services, Administration for Children and Families, Children’s Bureau. National child abuse and neglect data system glossary. Published March 2000. Retrieved July 3, 2018, from https://www.acf.hhs.gov/sites/default/files/cb/ncands_glossary.pdf
- U.S. General Accounting Office. (2002). Effectiveness of insurance coverage and federal programs for children who have experienced trauma largely unknown. Washington, DC: United States General Accounting Office. GAO-02–813. [Google Scholar]
- Wamser-Nanney R, & Steinzor CE (2016). Characteristics of attrition among children receiving trauma-focused treatment. Psychological Trauma, 8(6), 745–754. doi: 10.1037/tra0000143 [DOI] [PubMed] [Google Scholar]
- Yasinskia C, Hayesa AM, Alperta E, McCauley T, Ready CB, Webb C, & Deblinger E (2018). Treatment processes and demographic variables as predictors of dropout from trauma-focused cognitive behavioral therapy (TF-CBT) for youth. Journal of Behavioral Research and Therapy, 107, 10–18. doi: 10.1016/j.brat.2018.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]


