Summary
Background
Identifying and understanding reasons for being unsure or unwilling regarding intention to be vaccinated against coronavirus disease (COVID-19) may help to inform future public health messages aimed at increasing vaccination coverage. We analyzed a broad array of individual's psychological dispositions with regard to decision-making about COVID-19 vaccination in Japan.
Methods
A nationally representative cross-sectional web survey was conducted with 30053 Japanese adults aged 20 years or older at the end of February 2021. In addition to the question on the individual's intention to be vaccinated against COVID-19, respondents were asked about their sociodemographic, health-related, and psychological characteristics as well as information sources about COVID-19 and their levels of trust. Also, those who responded ‘not sure’ or ‘no’ regarding intention to take COVID-19 vaccine were asked why. Multinomial logistic regression with sparse group Lasso (Least Absolute Shrinkage and Selection Operator) penalty was used to compute adjusted odds ratios for factors associated with the intention (not sure/no versus yes).
Findings
The percentages of respondents who answered ‘not sure’ or ‘no’ regarding intention to be vaccinated against COVID-19 vaccine were 32.9% and 11.0%, respectively. After adjusting for covariates, the perceived risks of COVID-19, perceived risk of a COVID-19 vaccine, perceived benefits of a COVID-19 vaccine, trust in scientists and public authorities, and the belief that healthcare workers should be vaccinated were significantly associated with vaccination intention. Several sources of information about COVID-19 were also significantly associated with vaccination intention, including physicians, nurses, and television, medical information sites with lower odds of being unsure or unwilling, and internet news sites, YouTube, family members, and scientists and researchers with higher odds. The higher the level of trust in television as a source of COVID-19 information, the higher the odds of responding ‘not sure’ (odds ratio 1.11, 95% confidence interval 1.01–1.21). We also demonstrated that many respondents presented concerns about the side effects and safety of a COVID-19 vaccine as a major reason for being unsure or unwilling. To decide whether or not to get the vaccine, many respondents requested more information about the compatibilities between the vaccine and their personal health conditions, whether other people had been vaccinated, the effectiveness of vaccines against variants, and doctors’ recommendations.
Interpretation
Our findings suggest that public health messaging based on the sociodemographic and psychological characteristics of those who are unsure or unwilling regarding intention to be vaccinated against COVID-19 vaccine may help to increase vaccine uptake amongst this population.
Funding
The present work was supported in part by a grant from the Ministry of Health, Labour and Welfare of Japan (H29-Gantaisaku-ippan-009).
Keywords: Japan, COVID-19, attitudes towards vaccinations, psychological dispositions, information source
Research in context.
Evidence before this study
We searched PubMed for articles published in English from 1 January 2020 to 16 June 2021 with the following keywords: (“COVID-19” OR “SARS-CoV-2”) AND (“vaccine”[title] OR “vaccines”[title] OR “vaccination”[title]) AND (“intention” OR “hesitant” OR “resistant”) AND (“survey” OR “poll”). Our search found 475 titles. Several previous studies have examined possible determinants of intent to be vaccinated against COVID-19 when it becomes available. The main reasons for not wanting to receive COVID-19 even if it became available were concerns about its safety, potential side effects, efficacy, as well as trust in the government, the medical industry, and pharmaceutical companies involved in the vaccine development. Sociodemographic determinants of unsureness and unwillingness to be vaccinated that have been identified so far include age, gender, and socioeconomic status. However, most studies have been conducted in Europe and the United States, and there is little evidence for other regions, such as Asia, including Japan. There are also fewer reports on psychological than socioeconomic factors, and little discussion of the relationship between sources of information about the new coronas and the level of trust in them and vaccination intentions.
Added value of this study
This survey collected data on COVID-19 vaccination intentions in a nationally representative sample of more than 30,000 individuals aged 20 years and older in Japan, an East Asian country where vaccine confidence is among the lowest in the world. This large number of participants allowed for stratified analysis according to population groups, based on age and the presence of underlying diseases; these conditions were the same as those set by the government for the priority vaccination population, allowing for a more policy-oriented analysis. In addition to sociodemographic determinants, we have assessed the psychological profile of people who are unsure or unwilling to be vaccinated against COVID-19. Also, the association of the intention with information sources about COVID-19 and the levels of trust in them were investigated. For the topics related to vaccine complacency and confidence issues, the survey also asked about the reasons for being unsure or unwilling to be vaccinated against COVID-19. As of February-March 2021, the percentages of respondents responding ‘yes’, ‘not sure’, or ‘no’ regarding the intention to be vaccinated against COVID-19 were 56.1%, 32.9%, and 11.0%, respectively. This suggests that the proportions of respondents who are accepting the COVID-19 vaccine may be comparatively similar, as estimated by the latest systematic review (Robinson et al. (2021).
Implications of all the available evidence
Like other countries, Japan has a significant challenge in achieving the vaccination coverage required for population immunity. As has already been recognized in other countries, in Japan, younger groups less vulnerable to falling ill of COVID-19 are less willing to vaccinate against COVID-19. In the present study, in Japan, the trust in public authorities and scientists involved in COVID-19 vaccines was strongly correlated with COVID-19 vaccine intention, which reaffirm the importance of ensuring trust in those who represent these authorities. Many respondents presented concerns about the side effects and safety of the vaccine as a major reason for being unsure or unwilling to be vaccinated. They also requested more information about the compatibilities between the vaccine and their personal health conditions, whether other people had been vaccinated, the effectiveness of vaccines against variants, and doctors’ recommendations. Proactive messaging of these information from public authorities and scientists, especially those in positions of high trust, may result in those who had previously been unsure or unwilling to be vaccinated against COVIS-19 to be more receptive to a COVID-19 vaccine.
Alt-text: Unlabelled box
Introduction
Hesitancy about the coronavirus disease (COVID-19) vaccines is a major challenge in improving vaccination coverage, and studies to understand the situation are being conducted extensively around the world.[1,2] Identifying, understanding, and addressing the reasons for being unsure or unwilling regarding intention to be vaccinated against COVID-19 vaccine are important steps in ensuring the rapid and requisite uptake of the vaccination.[3,4] Past experience in routine immunization and crisis contexts demonstrated that acceptance of vaccination results from a complex decision-making process influenced by a variety of factors, including confidence issues (not trusting vaccine or provider), complacency issues (not feeling the need for or the value of the vaccine), and convenience issues (access).[5,6] In addition to the issue of complacency, which has been fueled by misinformation spread through multiple channels[7], the recent literature has identified explicit concerns about vaccine confidence—such as safety, potential side effects, efficacy, and trust in the government, the medical industry and pharmaceutical companies—as particular reasons that individuals provide for their uncertainty or unwillingness regarding the COVID-19 vaccination.[1,2,[8], [9], [10], [11]]
While this information is useful, it is insufficient to explain why individuals have come to these epistemological positions.[12] The literature on individual's intention to receive a vaccine indicates that there are likely several psychological characteristics that traverse individuals’ perceptions and attitudes which distinguish those who are unsure or unwilling about COVID-19 vaccination from those who are accepting.[3,5,13,14] Thus, it is important to identify the psychological determinants of people's unsureness and unwillingness to be vaccinated against COVID-19.[3] This is an approach that reflects the ‘attitude roots’ model of science rejection,[15] which may help not only to reach and maintain high vaccine coverage, but also to better inform public health messaging efforts aimed at increasing COVID-19 vaccine uptake.[14] To date, some studies have explored psychological determinants in relation to COVID-19 vaccine intention.[3,13,14,[16], [17], [18], [19]] For example, in addition to general attitudes towards vaccines,[13] perceived risks of COVID-19, perceived risks and benefits of the COVID-19 vaccine, perceived norms about the COVID-19 vaccine, trust in authoritative members of society about the COVID-19 vaccine, and beliefs about the COVID-19 vaccine, have each been demonstrated, in some way, to influence COVID-19 vaccine intention.[16,17]
Improving individual acceptance of the COVID-19 vaccine is especially important in Japan, which has ranked among the countries with the lowest vaccine confidence in the world.[20] This may be related to the fact that the Ministry of Health, Labor and Welfare of Japan (MHLW) suspended proactive recommendation of the human papillomavirus (HPV) vaccine in 2013 after unconfirmed reports of adverse events following vaccination, which were extensively covered in the media.[21] HPV vaccination coverage in Japan decreased from 68.4–74.0% among the 1994–98 birth cohort to 0.6% in the 2000 birth cohort.[22]
In Japan, at the time this study was conducted, the COVID-19 vaccination campaign were scheduled to begin for the elderly after April, followed by people with underlying diseases, and then the rest of the general population. In the present study, we conducted a nationwide web survey with over 30,000 participants in Japan, the largest of its kind in the country to the best of our knowledge, to analyze a broad array of individual's psychological dispositions with regard to decision-making about COVID-19 vaccination. The objectives of this study were as follows: first, to determine what proportions of the general adult population in Japan were accepting, unsure, or unwilling to take a vaccine for COVID-19; second, to determine the information sources used by individuals who are unsure or unwilling to take a COVID-19 vaccine, as well as the level of trust they place in these sources; third, to profile individuals who are unsure or unwilling regarding intention to be vaccinated against COVID-19 by identifying the key sociodemographic, health-related, and psychological characteristics as well as information sources about COVID-19 and the levels of trust in them that distinguish these individuals from those who are accepting of a COVID-19 vaccine; and finally, to determine key reasons for being unsure or unwilling regarding intention to take the COVID-19 vaccine.
Methods
Study population
Study participants were registered with a panel of a web survey company (Cross Marketing Inc.).[23] The panel included those aged 20 years or older who were able to complete surveys in Japanese. Panel membership was provided on a voluntary basis, and the incentives to join the panel were that those who responded to questionnaires administered by the company were provided with 'points' based on the survey volume. Points could be used to purchase products and services from partner companies.[23] As of 2021, this survey company had access to approximately 4.65 million panel members with diverse demographic, socioeconomic and geographic characteristics.[23]
In this study, the target number of study participants was set at approximately 30,000. In order to ensure national representation, a quota sampling method based on age (at the time of the survey), gender, and prefecture population ratios obtained from the 2015 National Census was used to finally set 30053 participants as the fixed number.[24] Participation was on a first-come-first-served basis and the survey was closed when the number of respondents reached the pre-determined target population according to age, gender, and prefecture. The survey began on 26 February 2021 and the target was reached on 4 March 2021. The respondents were required to respond to each question so that there were no missing values. In order to avoid unmotivated or dishonest responses, we tried to improve the quality of the questionnaire responses by asking respondents to take an oath (TO) that they would be serious before they started answering the questionnaire.[25] Masuda et al. (2019) found that respondents who took an oath to answer seriously chose fewer straight-line responses (i.e. answering ‘yes’ or ‘no’ to all items all the way through the item in a straight line) and midpoint responses than the control group, suggesting that respondents behaved consistently with their initial commitment to their oath.[25] It was also suggested that the TO method is superior to the instructional manipulation check method (i.e. a question testing respondents’ attention) in that it does not reduce the sample size. We have adopted the Japanese wording of the oath proposed in this study as is.
Measures
The survey questionnaire was developed based on a thorough review of past literature on similar topics,[16,17] and was supervised by the Japan Epidemiological Association and the Japanese Society of Infectious Diseases as well as experts involved in the COVID-19 Information Value Improvement and Link project (CIVIL project). In addition to the question on the individual's intention to be vaccinated against COVID-19, the questionnaire consisted of five parts. The first part asked questions about the sociodemographic characteristics of participants; the second part asked questions about health-related topics, including health literacy; the third part asked questions about psychological characteristics; the fourth part asked questions about information sources used to gather information about the COVID-19 pandemic and the level of trust in them; and in the last part, those who were unsure or unwilling to take a COVID-19 vaccine were asked why. All questions were closed-ended questions and had single-answer or multiple-answer formats, including binary, ‘yes/no’ scales, nominal and ordinal scales, and Likert scale questions; and are outlined in the resulting tables (Table 1 for sociodemographic questions; Supplementary Tables 1 for health-related and psychological questions; Supplementary Tables 3 and 4 for questions about information sources and trust levels; and Table 3 for questions about the reasons for being unsure or unwilling). Unless otherwise stated, respondents provided information as of the time of the survey response.
Table 1.
Sociodemographic characteristics of the study participants by three COVID-19 vaccine intention groups.
| Yes | Not sure | No | P-value | Total | |
|---|---|---|---|---|---|
| N = 16869 | N = 9874 | N = 3310 | N = 30053 | ||
| Sociodemographic characteristics | |||||
| Gender (SA) | <0.001 | ||||
| Women | 8133 (48.2) | 5777 (58.5) | 1680 (50.8) | 15590 (51.9) | |
| Men | 8719 (51.7) | 4074 (41.3) | 1617 (48.9) | 14410 (47.9) | |
| Other | 17 (0.1) | 23 (0.2) | 13 (0.4) | 53 (0.2) | |
| Prefecture (SA) | 0.011 | ||||
| Hokkaido | 915 (5.4) | 554 (5.6) | 167 (5.0) | 1636 (5.4) | |
| Aomori | 146 (0.9) | 80 (0.8) | 38 (1.1) | 264 (0.9) | |
| Iwate | 146 (0.9) | 85 (0.9) | 27 (0.8) | 258 (0.9) | |
| Miyagi | 348 (2.1) | 188 (1.9) | 59 (1.8) | 595 (2.0) | |
| Akita | 115 (0.7) | 67 (0.7) | 20 (0.6) | 202 (0.7) | |
| Yamagata | 129 (0.8) | 64 (0.6) | 19 (0.6) | 212 (0.7) | |
| Fukushima | 196 (1.2) | 103 (1.0) | 34 (1.0) | 333 (1.1) | |
| Ibaraki | 289 (1.7) | 156 (1.6) | 52 (1.6) | 497 (1.7) | |
| Tochigi | 172 (1.0) | 107 (1.1) | 29 (0.9) | 308 (1.0) | |
| Gunma | 168 (1.0) | 87 (0.9) | 31 (0.9) | 286 (1.0) | |
| Saitama | 858 (5.1) | 546 (5.5) | 177 (5.3) | 1581 (5.3) | |
| Chiba | 804 (4.8) | 462 (4.7) | 127 (3.8) | 1393 (4.6) | |
| Tokyo | 2084 (12.4) | 1112 (11.3) | 465 (14.0) | 3661 (12.2) | |
| Kanagawa | 1358 (8.1) | 802 (8.1) | 256 (7.7) | 2416 (8.0) | |
| Niigata | 365 (2.2) | 191 (1.9) | 39 (1.2) | 595 (2.0) | |
| Toyama | 157 (0.9) | 75 (0.8) | 29 (0.9) | 261 (0.9) | |
| Ishikawa | 168 (1.0) | 80 (0.8) | 26 (0.8) | 274 (0.9) | |
| Fukui | 83 (0.5) | 61 (0.6) | 12 (0.4) | 156 (0.5) | |
| Yamanashi | 104 (0.6) | 54 (0.5) | 26 (0.8) | 184 (0.6) | |
| Nagano | 267 (1.6) | 186 (1.9) | 54 (1.6) | 507 (1.7) | |
| Gifu | 217 (1.3) | 132 (1.3) | 51 (1.5) | 400 (1.3) | |
| Shizuoka | 403 (2.4) | 241 (2.4) | 66 (2.0) | 710 (2.4) | |
| Aichi | 1147 (6.8) | 621 (6.3) | 225 (6.8) | 1993 (6.6) | |
| Mie | 237 (1.4) | 134 (1.4) | 35 (1.1) | 406 (1.4) | |
| Shiga | 139 (0.8) | 81 (0.8) | 33 (1.0) | 253 (0.8) | |
| Kyoto | 325 (1.9) | 200 (2.0) | 77 (2.3) | 602 (2.0) | |
| Osaka | 1174 (7.0) | 760 (7.7) | 243 (7.3) | 2177 (7.2) | |
| Hyogo | 747 (4.4) | 455 (4.6) | 161 (4.9) | 1363 (4.5) | |
| Nara | 177 (1.0) | 105 (1.1) | 37 (1.1) | 319 (1.1) | |
| Wakayama | 78 (0.5) | 40 (0.4) | 14 (0.4) | 132 (0.4) | |
| Tottori | 67 (0.4) | 40 (0.4) | 13 (0.4) | 120 (0.4) | |
| Shimane | 88 (0.5) | 41 (0.4) | 6 (0.2) | 135 (0.4) | |
| Okayama | 278 (1.6) | 182 (1.8) | 59 (1.8) | 519 (1.7) | |
| Hiroshima | 397 (2.4) | 241 (2.4) | 83 (2.5) | 721 (2.4) | |
| Yamaguchi | 151 (0.9) | 92 (0.9) | 25 (0.8) | 268 (0.9) | |
| Tokushima | 98 (0.6) | 54 (30.5) | 19 (0.6) | 171 (0.6) | |
| Kagawa | 150 (0.9) | 88 (0.9) | 30 (0.9) | 268 (0.9) | |
| Ehime | 192 (1.1) | 122 (1.2) | 41 (1.2) | 355 (1.2) | |
| Kochi | 74 (0.4) | 35 (0.4) | 19 (0.6) | 128 (0.4) | |
| Fukuoka | 864 (5.1) | 550 (5.6) | 192 (5.8) | 1606 (5.3) | |
| Saga | 94 (0.6) | 61 (0.6) | 15 (0.5) | 170 (0.6) | |
| Nagasaki | 161 (1.0) | 102 (1.0) | 29 (0.9) | 292 (1.0) | |
| Kumamoto | 223 (1.3) | 115 (1.2) | 38 (1.1) | 376 (1.3) | |
| Oita | 129 (0.8) | 73 (0.7) | 23 (0.7) | 225 (0.7) | |
| Miyazaki | 109 (0.6) | 71 (0.7) | 20 (0.6) | 200 (0.7) | |
| Kagoshima | 172 (1.0) | 76 (0.8) | 38 (1.1) | 286 (1.0) | |
| Okinawa | 106 (0.6) | 102 (1.0) | 31 (0.9) | 239 (0.8) | |
| Highest educational level (SA) | <0.001 | ||||
| Middle school | 344 (2.0) | 376 (3.8) | 124 (3.7) | 844 (2.8) | |
| High school | 5503 (32.6) | 3575 (36.2) | 1096 (33.1) | 10174 (33.9) | |
| Junior college | 3130 (18.6) | 2075 (21.0) | 628 (19.0) | 5833 (19.4) | |
| University | 7099 (42.1) | 3500 (35.4) | 1281 (38.7) | 11880 (39.5) | |
| Graduate school (master's course) | 611 (3.6) | 279 (2.8) | 149 (4.5) | 1039 (3.5) | |
| Graduate school (doctoral course) | 182 (1.1) | 69 (0.7) | 32 (1.0) | 283 (0.9) | |
| Occupation type (SA) | <0.001 | ||||
| Agriculture, forestry and fisheries | 110 (0.7) | 71 (0.7) | 21 (0.6) | 202 (0.7) | |
| Construction | 495 (2.9) | 269 (2.7) | 116 (3.5) | 880 (2.9) | |
| Manufacturing | 1665 (9.9) | 1037 (10.5) | 368 (11.1) | 3070 (10.2) | |
| Information and communications | 454 (2.7) | 325 (3.3) | 125 (3.8) | 904 (3.0) | |
| Transportation and postal services | 397 (2.4) | 307 (3.1) | 117 (3.5) | 821 (2.7) | |
| Wholesale and retail trade | 1015 (6.0) | 764 (7.7) | 212 (6.4) | 1991 (6.6) | |
| Finance and insurance | 355 (2.1) | 243 (2.5) | 86 (2.6) | 684 (2.3) | |
| Real estate and goods rental and leasing | 250 (1.5) | 140 (1.4) | 48 (1.5) | 438 (1.5) | |
| Scientific research, professional and technical services | 247 (1.5) | 117 (1.2) | 46 (1.4) | 410 (1.4) | |
| Accommodations, food and beverage services | 309 (1.8) | 275 (2.8) | 76 (2.3) | 660 (2.2) | |
| Living-related and personal services and amusement services | 231 (1.4) | 186 (1.9) | 66 (2.0) | 483 (1.6) | |
| Education and learning support | 598 (3.5) | 320 (3.2) | 117 (3.5) | 1035 (3.4) | |
| Healthcare and welfare | 1240 (7.4) | 445 (4.5) | 204 (6.2) | 1889 (6.3) | |
| Combined services | 137 (0.8) | 63 (0.6) | 39 (1.2) | 239 (0.8) | |
| Services (not elsewhere classified) | 1321 (7.8) | 889 (9.0) | 343 (10.4) | 2553 (8.5) | |
| Public service (not elsewhere classified) | 550 (3.3) | 257 (2.6) | 125 (3.8) | 932 (3.1) | |
| Students | 277 (1.6) | 257 (2.6) | 107 (3.2) | 641 (2.1) | |
| Homemaker | 3993 (23.7) | 2209 (22.4) | 512 (15.5) | 6714 (22.3) | |
| Others | 3225 (19.1) | 1700 (17.2) | 582 (17.6) | 5507 (18.3) | |
| Annual household income in 2020 – million JPY (SA) | <0.001 | ||||
| –1) | 878 (5.2) | 916 (9.3) | 315 (9.5) | 2109 (7.0) | |
| [1–2) | 1335 (7.9) | 977 (9.9) | 403 (12.2) | 2715 (9.0) | |
| [2–3) | 2240 (13.3) | 1492 (15.1) | 433 (13.1) | 4165 (13.9) | |
| [3–4) | 2663 (15.8) | 1533 (15.5) | 446 (13.5) | 4642 (15.4) | |
| [4–5) | 2278 (13.5) | 1184 (12.0) | 387 (11.7) | 3849 (12.8) | |
| [5–6) | 1723 (10.2) | 982 (9.9) | 318 (9.6) | 3023 (10.1) | |
| [6–7) | 1295 (7.7) | 716 (7.3) | 258 (7.8) | 2269 (7.5) | |
| [7–8) | 1149 (6.8) | 611 (6.2) | 218 (6.6) | 1978 (6.6) | |
| [8–9) | 823 (4.9) | 364 (3.7) | 130 (3.9) | 1317 (4.4) | |
| [9–10) | 759 (4.5) | 348 (3.5) | 122 (3.7) | 1229 (4.1) | |
| [10– or | 1726 (10.2) | 751 (7.6) | 280 (8.5) | 2757 (9.2) | |
| Household size including respondent (SA) | <0.001 | ||||
| 1 | 2778 (16.5) | 2029 (20.5) | 851 (25.7) | 5658 (18.8) | |
| 2 | 6902 (40.9) | 3229 (32.7) | 992 (30.0) | 11123 (37.0) | |
| 3 | 3843 (22.8) | 2369 (24.0) | 804 (24.3) | 7016 (23.3) | |
| 4 | 2310 (13.7) | 1584 (16.0) | 458 (13.8) | 4352 (14.5) | |
| 5 | 715 (4.2) | 447 (4.5) | 146 (4.4) | 1308 (4.4) | |
| More than 6 | 321 (1.9) | 216 (2.2) | 59 (1.8) | 596 (2.0) | |
| Marital size (SA) | <0.001 | ||||
| Married (including de facto marriage) | 11328 (67.2) | 5244 (53.1) | 1493 (45.1) | 18065 (60.1) | |
| Not married (without partner) | 3020 (17.9) | 2903 (29.4) | 1198 (36.2) | 7121 (23.7) | |
| Not married (with a partner) | 797 (4.7) | 632 (6.4) | 304 (9.2) | 1733 (5.8) | |
| Widowed | 713 (4.2) | 381 (3.9) | 84 (2.5) | 1178 (3.9) | |
| Divorced | 1011 (6.0) | 714 (7.2) | 231 (7.0) | 1956 (6.5) | |
| To what extent did the COVID-19 pandemic affect your life, within the past year? (SA) | <0.001 | ||||
| Not at all | 787 (4.7) | 580 (5.9) | 528 (16.0) | 1895 (6.3) | |
| Not much | 4293 (25.4) | 2644 (26.8) | 977 (29.5) | 7914 (26.3) | |
| Somewhat | 8961 (53.1) | 5053 (51.2) | 1313 (39.7) | 15327 (51.0) | |
| Quite a lot | 2828 (16.8) | 1597 (16.2) | 492 (14.9) | 4917 (16.4) |
SA: single-answer questions; MA: multiple-answer question
Table 3.
Reasons for responding ‘not sure’ or ‘no’ regarding intention to be vaccinated against COVID-19
| Not sure | No | P-value | Total | |
|---|---|---|---|---|
| N = 9874 | N = 3310 | N = 30053 | ||
| What are reasons for refusing or being unsure to receive a COVID-19 vaccine? (MA) | ||||
| Specific anxiety about the COVID-19 vaccine | ||||
| Adverse reactions and safety | 7809 (79.1) | 2258 (68.2) | <0.001 | 10067 (76.4) |
| Effectiveness | 3109 (31.5) | 989 (29.9) | 0.088 | 4098 (31.1) |
| Not wanting to be the first to get a new vaccine | 2275 (23.0) | 954 (28.8) | <0.001 | 3229 (24.5) |
| Rigor of clinical trials | 1683 (17.0) | 656 (19.8) | <0.001 | 2339 (17.7) |
| Contents of the vaccine | 1099 (11.1) | 594 (17.9) | <0.001 | 1693 (12.8) |
| Others | 131 (1.3) | 94 (2.8) | <0.001 | 225 (1.7) |
| More information is needed to decide whether or not to get a COVID-19 vaccine | ||||
| Compatibility with personal health conditions (e.g., allergies, comorbidities) | 4342 (44.0) | 1077 (32.5) | <0.001 | 5419 (41.1) |
| Doctor's recommendation | 2092 (21.2) | 331 (10.0) | <0.001 | 2423 (18.4) |
| Depends on the pandemic situation | 1546 (15.7) | 443 (13.4) | 0.002 | 1989 (15.1) |
| Whether other people have been vaccinated or not | 1899 (19.2) | 350 (10.6) | <0.001 | 2249 (17.1) |
| Others | 60 (0.6) | 40 (1.2) | 0.001 | 100 (0.8) |
| Attitude toward vaccination in general, not limited to the new coronavirus vaccine | ||||
| Religious beliefs | 49 (0.5) | 29 (0.9) | 0.020* | 78 (0.6) |
| Vaccines are not necessary | 238 (2.4) | 321 (9.7) | <0.001 | 559 (4.2) |
| I don't think the vaccine is effective | 523 (5.3) | 579 (17.5) | <0.001 | 1102 (8.4) |
| I am anxious about adverse reactions and safety of vaccines | 4575 (46.3) | 1357 (41.0) | <0.001 | 5932 (45.0) |
| I have a fear of vaccines | 1428 (14.5) | 548 (16.6) | 0.004 | 1976 (15.0) |
| Others | 80 (0.8) | 37 (1.1) | 0.127 | 117 (0.9) |
| Lack of trust | ||||
| Vaccines in general | 2166 (21.9) | 953 (28.8) | <0.001 | 3119 (23.7) |
| Government | 2340 (23.7) | 896 (27.1) | <0.001 | 3236 (24.5) |
| Pharmaceutical companies | 1060 (10.7) | 596 (18.0) | <0.001 | 1656 (12.6) |
| Medical care in general | 529 (5.4) | 335 (10.1) | <0.001 | 864 (6.6) |
| Vaccine development or testing process | 1911 (19.4) | 732 (22.1) | 0.001 | 2643 (20.0) |
| Others | 63 (0.6) | 20 (0.6) | 0.932 | 83 (0.6) |
| Other reasons | ||||
| I want high-risk people to be vaccinated first | 2216 (22.4) | 549 (16.6) | <0.001 | 2765 (21.0) |
| I am afraid to go to a medical institution for vaccination | 947 (9.6) | 283 (8.5) | 0.081 | 1230 (9.3) |
| It may not be effective for mutants | 2119 (21.5) | 684 (20.7) | 0.345 | 2803 (21.3) |
| I don't like needles. | 1087 (11.0) | 484 (14.6) | <0.001 | 1571 (11.9) |
| Others | 255 (2.6) | 151 (4.6) | <0.001 | 406 (3.1) |
MA: multiple-answer question. * Statistical significance disappeared after Bonferroni correction for multiple testing
Intent to be vaccinated against COVID-19 was measured with the question: ‘when a vaccine for COVID-19 becomes available, will you get vaccinated?” Response options were “yes,” “not sure,” and “no.” Based on the responses, individuals were classified into three vaccine intention groups: yes (accepting), not sure (unsure), and no (unwilling).
Sociodemographic variables considered in this study were informed by the existing evidence relating to vaccine intention. We asked respondents about age, gender, prefecture of residence, education level, occupation type, household income in 2020, household size, marital status, and to what extent their lives have been affected by the COVID-19 pandemic.
Health-related variables included self-reported health status, experience of any COVID-19 tests (polymerase chain reaction [PCR] test, antigen test, or antibody test), presence of underlying diseases (e.g. diabetes, heart failure, respiratory disease, and chronic obstructive pulmonary disease [COPD], among others, or if the respondent was on dialysis or using immunosuppressive or anticancer drugs), if a respondent was living with family members who are elderly or have underlying diseases, what preventive measures a respondent is taking against COVID-19, if there is anyone close to a respondent who was infected with COVID-19, and whether or not a respondent had ever refrained from visiting a medical institution.
Psychological characteristics were measured based on single items rather than validated scales for the purpose of both research and policy benefits, such as reduced respondent burden and ease of interpretation, while accounting for many variables.[26] Respondents were first asked about their perceived risk of COVID-19, how anxious they were about COVID-19, and to guess their own likelihood of infection. In addition, with regard to the perceived risks and benefits of vaccines against COVID-19, respondents were asked about the degree of disadvantages, benefits, and reassurance they felt about COVID-19 vaccines. To investigate the perceived norms of respondents, they were asked whether they should be vaccinated against COVID-19 if others are vaccinated. To investigate the trust of the respondents, they were asked about their level of trust in scientists who were involved in developing COVID-19 vaccines, the public agencies approving the vaccines, and the healthcare providers conducting vaccinations. To investigate the beliefs of respondents, they were asked whether healthcare workers and employees of elderly care facilities should be vaccinated against COVID-19. Finally, to evaluate the respondents’ general attitude toward vaccination, they were asked about their history of influenza and routine vaccinations.
Participants were given 30 options for which information sources they used to gather information about the COVID-19 pandemic: physicians; nurses; pharmacists; veterinarians; dentists; health fairs and events; newspapers; magazines; books; scientific literature; television; radio; internet news sites; search engines (e.g., Google, Yahoo); LINE (a ubiquitous Japanese SNS Service); Facebook; Twitter; Instagram; YouTube; TikTok; medical information sites; blogs or web pages of celebrities and famous people; local authorities such as prefectures and municipalities; the government; the medical task-force advising the government, known as the Novel Coronavirus Expert Meeting (re-established as Novel Coronavirus Infectious Disease Control Subcommittee in July 2020); friends; family members; scientists and researchers; pharmaceutical companies; and other companies. Respondents were also asked how much they trust the information from each of these sources.
Regarding variables relating to the reasons for being unsure or unwilling to take COVID-19 vaccine, there were five major themes related to vaccine complacency and confidence issues,[5,6] which were informed by previous studies with a similar scope in free-response questions and thematized as:[27] specific anxiety about the COVID-19 vaccine; need additional information; general attitude toward vaccination, not limited to the COVID-19 vaccine; lack of trust; and other reasons. Since the efficacy of vaccines against mutant strains has been attracting a lot of public attention,[28] we added one item of concern about the efficacy of vaccines against these strains. At the time this study was conducted, there was still little public information about vaccination locations, and the COVID-19 vaccination is free of charge as it is paid in full as a public expense, so we did not ask about convenience and access issues.
Data analysis
In Japan, as in many other countries, given the limited initial supply of COVID-19 vaccines, priority groups for vaccination are high-risk populations for COVID-19, such as the elderly and those with underlying diseases. Therefore, in order to make this study more policy relevant by providing estimation results for each of those groups, we employed a stratified analysis (in addition to a pooled, unstratified analysis) by age group (the elderly and younger adults) and by the presence or absence of underlying disease: Group (A) elderly with underlying diseases; Group (B) elderly without underlying diseases; Group (C) younger adults with underlying diseases; and Group (D) younger adults without underlying diseases. In this study, for analytical purposes, the elderly were defined as those over 65 years old, which is the same as the government definition in this context.[29] In addition, in the present study, a respondent who answered ‘yes’ to the following question was determined as having an underlying disease: “do you have an underlying disease (diabetes, heart failure, and respiratory disorders [COPD], etc.)? Or are you on dialysis, or using immunosuppressive or anticancer drugs?” For the purpose of avoiding technical terms in the questionnaire and using expressions that can be easily understood by the general public, this is a simplified version of the actual government definition.[29] It should be noted that in this study, instead of introducing these four groups into the model as a single categorical variable and adding interaction terms with other variables, stratification was chosen to avoid including a large number of variables into the model and making the estimation results unstable.[30]
The analytical strategy covered four elements linked to the study objectives. First, the proportion of respondents classified into the three vaccine intention groups (yes, not sure, and no) were calculated. These proportions were further stratified for each of the sociodemographic, health-related, and psychological variables, and compared between the three intention groups using Chi-squared test.
Second, the three vaccine intention groups were compared with respect to where they sourced their information about COVID-19 and the level of trust they had in the information sources. For the former, Chi-squared test was used to compare the proportion of respondents who used each information source between groups. For the latter, the Likert scale was treated as a continuous variable, ranging from zero (not at all) to three (extremely), which allowed for the calculation of the mean and standard errors of the scores for each source. The comparisons between the vaccine intention groups were made using Kruskal-Wallis rank-sum test.
Third, multinomial logistic regression models were fitted to the pooled data and each of Groups A–D to identify the important sociodemographic, health-related, and psychological characteristics as well as information sources about COVID-19 and their levels of trust, associated with being unsure or unwilling regarding intention to be vaccinated against COVID-19: the COVID-19 vaccine acceptance group was set as the reference group. To control the multicollinearity between covariates and select the optimal covariates sets simultaneously, we employed the sparse group Lasso (Least Absolute Shrinkage and Selection Operator) method with an L1 penalty and 10-fold negative log-likelihood-based cross validation.[31] In regression models with many covariates, or when there is multicollinearity among some variables, the penalization (or shrinkage-based) method is a common approach for handling complex constraints in optimization problems by adding the sum of the absolute values of the coefficients as the penalty term to the likelihood; this method induces the sparsity among the covariate set and thus is effective for controlling for multicollinearity.[32] After the variable selection, to reduce bias due to the Lasso penalization, the final models were re-fitted using the selected sets of covariates, which is called “de-biasing” procedure. Their associations with each covariate are presented as the adjusted odds ratio (OR) with the 95% confidence interval (CI). For non-binary categorical covariates from responses to single-answer questions, reference groups were chosen as follows: for bi-directional and uni-directional ordinal covariates, the middle and first/last category was chosen as the reference group for ease of interpretation, respectively; for other categorical covariates, the category with the largest number of responses was basically chosen as the reference category. Responses to multiple-answer questions were converted to binary dummy variables prior to the analysis. Likert scale questions were converted into categorical variables, except for the levels of trust in information sources about COVID-19, which were considered as continuous variables. Highest education levels and annual household income in 2020 (ordinal scale questions) were also treated as continuous variables. Age (continuous variable) and the presence or absence of underlying disease were considered only for the unstratified analysis. In addition, two continuous variables representing the COVID-19 infection status of each respondent's place of residence were also considered in the analyses: the total number of COVID-19 infection cases as of February 26, 2021, the survey start date, and the number of COVID-19 infection cases during the past month (January 27 to February 26, 2021).[33]
Fourth, for each reason for not being unsure or unwilling regarding intention to be vaccinated, the proportions of respondents who selected the reasons were compared between those who were unsure and unwilling using Chi-squared test.
For statistical two-side tests for single-answer questions, a p-value that is less than 0.05 was considered statistically significant. To control type 1 error inflation due to the multiple testing procedure, the Bonferroni multiple testing correction was applied if necessary (for variables for multiple-answer questions). R version 3.6.3 was used for all statistical analyses.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
Intention to be vaccinated against COVID-19
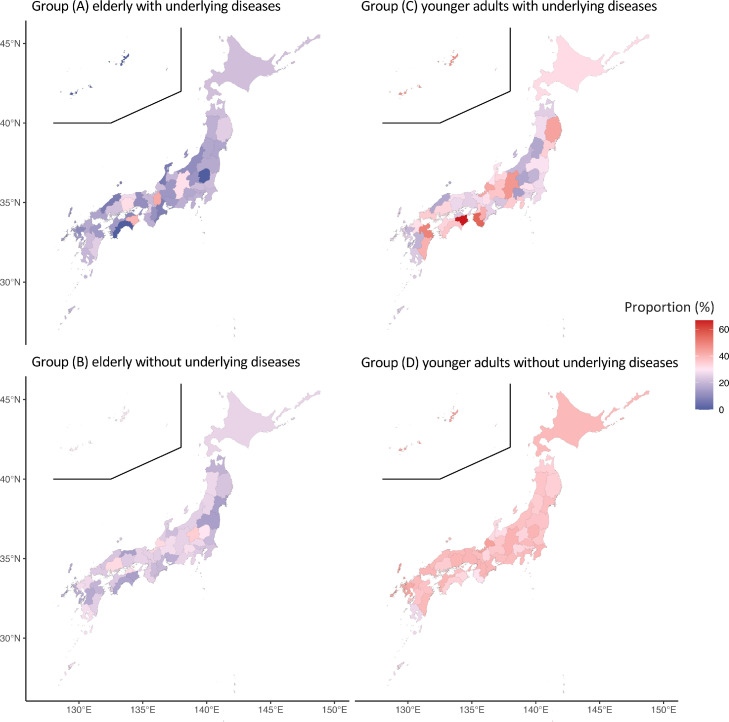
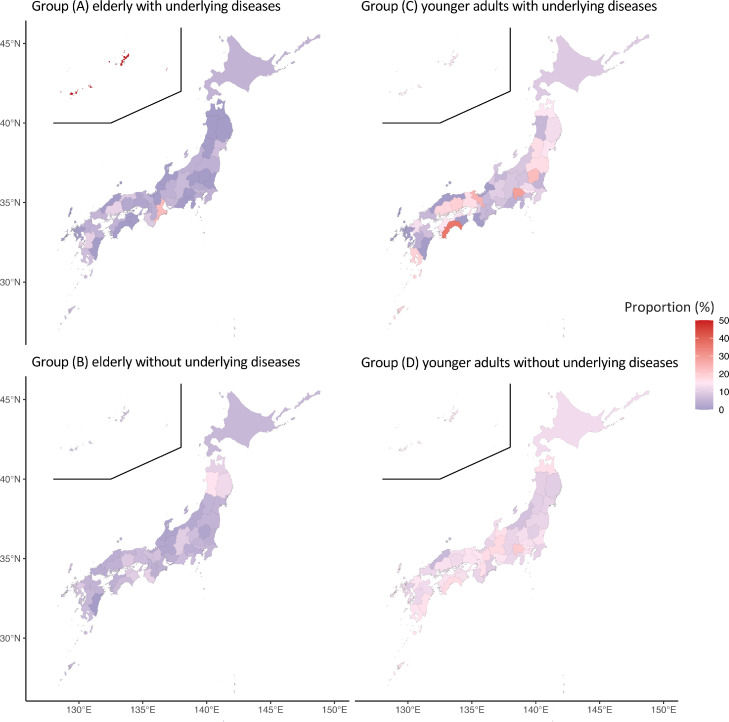
For the pooled analysis, 56.1% of respondents were accepting of a COVID-19 vaccine, 32.9% were unsure about such a vaccine, and 11.0% were unwilling to be vaccinated. Demographic characteristics as well as health-related and psychological characteristics of the study participants are presented in Table 1 and the Supplementary Table 1, respectively. The intention to vaccinate against COVID-19 differed clearly depending on age and the presence of underlying diseases, with younger respondents and those without underlying diseases more likely to be unsure and unwilling to take a COVID-19 vaccine (Supplementary Table 2). Statistically significant prefectural differences were observed in the proportions (p<0.05). Prefecture-level statistical differences were only found in Group D (p<0.05) (Figure 1, Figure 2 and Supplementary Table 2).
Figure 1.
Proportions of those responding ‘not sure’ regarding intention to be vaccinated against COVID-19 by Groups (A–D).
Figure 2.
Proportions of those responding ‘no’ regarding intention to be vaccinated against COVID-19 by Groups (A–D).
Information sources about COVID-19 and trust levels
For all sources of information, consumption was statistically significantly different amongst the three vaccine intention groups, except for veterinarians, search engines, and TikTok (Supplementary Table 3). Television (accepting 86.8%, unsure 80.2%, unwilling 59.2%) and internet news sites (54.7%, 53.6%, 44.9%) were the primary sources of information for all response groups. Compared to the vaccine accepting group, the unsure and unwilling groups were more likely to use information from Twitter (6.9%, 8.3%, 11.9%). A similar trend was observed for each of the Groups (A–D), and furthermore, younger respondents consumed more information from Twitter and search engines.
For all sources of information, the level of trust was statistically significantly different among the three vaccine intention groups (Supplementary Figure 1). The most trusted sources of information were physicians (mean level of trust 1.85, 95% CI 1.84–1.86 for accepting; 1.64, 1.63–1.66 for unsure; 1.41, 1.38–1.44 for unwilling) and nurses (mean trust 1.69, 1.68–1.70; 1.53, 1.52–1.54; 1.34, 1.32–1.37) in all three vaccine intention groups. In addition, local authorities, the government, newspapers, and television were also relatively trusted. However, the level of trust in these sources was lower in the unsure and unwilling groups than in the vaccine accepting group. Other exact values are presented in Supplementary Table 4. As shown in Supplementary Figure 1, a similar trend was observed for each of the risk Groups (A–D). Younger respondents tended to have higher trust scores for SNS.
Factors associated with the COVID-19 vaccine intention
Age, gender, and occupation types were identified as factors related to responding ‘not sure’ regarding the COVID-19 vaccine intention (Table 2): older age had lower odds (OR 0.98, 95% CI 0.98–0.99), women had higher odds than men (1.53, 1.41–1.66), and compared to healthcare and welfare, most occupation types had higher odds. In addition, those without underlying diseases had higher odds than those with underlying diseases (1.22, 1.09–1.37). There was no statistical significance of regional differences in the proportion of those responding ‘not sure’ about their intention to be vaccinated with COVID-19, except in a few prefectures after adjusting for covariates. Two variables representing the COVID-19 infection status of each respondent's place of residence were not statistically significant and did not remain in the final regression models.
Table 2.
Odds ratios (95% confidence intervals) for responding ‘not sure’ or ‘no’ regarding intention to be vaccinated
| Not sure, N = 9874 | P value | No, N = 3310 | P value | |
|---|---|---|---|---|
| COVID-19 pandemic situation | ||||
| Total number of COVID-19 infected cases in residential prefectures as of February 16, 2021 | 1.00 (1.00–1.00) | 0.779 | 1.00 (1.00–1.00) | 0.291 |
| Number of COVID-19 infected cases in residential prefectures between 16 January and February 16, 2021 | 1.00 (1.00–1.00) | 0.421 | 1.00 (1.00–1.00) | 0.268 |
| Sociodemographic characteristics | ||||
| Age (SA) | 0.98 (0.98–0.99) | <0.001 | 0.97 (0.96–0.97) | <0.001 |
| Gender (SA) | ||||
| Women | 1.53 (1.41–1.66) | <0.001 | 1.56 (1.37–1.78) | <0.001 |
| Men | 1.00 (reference) | NA | 1.00 (reference) | NA |
| Other | 1.92 (0.81–4.57) | 0.141 | 1.41 (0.44–4.45) | 0.563 |
| Prefecture (SA) | ||||
| Hokkaido | 1.08 (0.93–1.26) | 0.296 | 0.99 (0.77–1.27) | 0.937 |
| Aomori | 0.88 (0.61–1.27) | 0.497 | 1.39 (0.82–2.36) | 0.217 |
| Iwate | 1.09 (0.77–1.54) | 0.641 | 1.09 (0.61–1.97) | 0.764 |
| Miyagi | 0.93 (0.73–1.18) | 0.554 | 1.02 (0.69–1.52) | 0.909 |
| Akita | 1.05 (0.71–1.55) | 0.818 | 1.38 (0.71–2.68) | 0.346 |
| Yamagata | 1.05 (0.71–1.55) | 0.814 | 1.07 (0.57–2.01) | 0.838 |
| Fukushima | 0.88 (0.64–1.22) | 0.450 | 0.80 (0.48–1.34) | 0.397 |
| Ibaraki | 1.02 (0.79–1.32) | 0.867 | 0.97 (0.64–1.47) | 0.885 |
| Tochigi | 1.12 (0.81–1.55) | 0.495 | 0.80 (0.45–1.40) | 0.429 |
| Gunma | 0.70 (0.50–0.99) | 0.047 | 0.69 (0.39–1.20) | 0.187 |
| Saitama | 1.20 (1.05–1.37) | 0.007 | 1.25 (1.01–1.56) | 0.043 |
| Chiba | 1.02 (0.90–1.16) | 0.775 | 0.97 (0.79–1.21) | 0.813 |
| Tokyo | 1.00 (reference) | NA | 1.00 (reference) | NA |
| Kanagawa | 1.05 (0.92–1.19) | 0.483 | 0.98 (0.80–1.21) | 0.876 |
| Niigata | 1.04 (0.82–1.31) | 0.745 | 0.80 (0.52–1.25) | 0.330 |
| Toyama | 0.77 (0.55–1.09) | 0.143 | 1.16 (0.66–2.03) | 0.599 |
| Ishikawa | 0.77 (0.54–1.10) | 0.155 | 0.75 (0.41–1.36) | 0.344 |
| Fukui | 1.58 (1.00–2.49) | 0.050 | 0.75 (0.31–1.83) | 0.527 |
| Yamanashi | 0.78 (0.51–1.19) | 0.246 | 1.62 (0.86–3.05) | 0.135 |
| Nagano | 1.08 (0.84–1.38) | 0.565 | 1.10 (0.73–1.66) | 0.654 |
| Gifu | 1.04 (0.78–1.39) | 0.779 | 1.37 (0.87–2.14) | 0.170 |
| Shizuoka | 0.99 (0.80–1.23) | 0.931 | 0.83 (0.57–1.20) | 0.320 |
| Aichi | 0.95 (0.83–1.09) | 0.446 | 0.98 (0.79–1.23) | 0.893 |
| Mie | 0.83 (0.63–1.10) | 0.206 | 0.87 (0.53–1.44) | 0.599 |
| Shiga | 0.99 (0.69–1.44) | 0.966 | 1.23 (0.70–2.15) | 0.478 |
| Kyoto | 0.93 (0.74–1.17) | 0.532 | 1.06 (0.73–1.52) | 0.770 |
| Osaka | 1.16 (1.02–1.32) | 0.026 | 1.01 (0.82–1.25) | 0.896 |
| Hyogo | 1.01 (0.86–1.18) | 0.936 | 1.23 (0.96–1.58) | 0.102 |
| Nara | 1.21 (0.88–1.68) | 0.240 | 1.42 (0.86–2.36) | 0.171 |
| Wakayama | 0.54 (0.33–0.89) | 0.016 | 0.42 (0.19–0.94) | 0.035 |
| Tottori | 0.99 (0.59–1.64) | 0.954 | 1.24 (0.56–2.76) | 0.601 |
| Shimane | 0.81 (0.51–1.30) | 0.386 | 0.11 (0.03–0.38) | <0.001 |
| Okayama | 1.26 (0.98–1.61) | 0.073 | 1.75 (1.17–2.60) | 0.006 |
| Hiroshima | 1.11 (0.90–1.38) | 0.331 | 1.37 (0.97–1.94) | 0.070 |
| Yamaguchi | 0.95 (0.67–1.35) | 0.772 | 0.62 (0.34–1.15) | 0.129 |
| Tokushima | 0.99 (0.64–1.52) | 0.958 | 1.68 (0.86–3.30) | 0.132 |
| Kagawa | 1.26 (0.89–1.80) | 0.196 | 1.09 (0.60–1.98) | 0.786 |
| Ehime | 0.91 (0.68–1.22) | 0.541 | 1.21 (0.76–1.94) | 0.415 |
| Kochi | 1.26 (0.73–2.19) | 0.402 | 1.78 (0.77–4.12) | 0.179 |
| Fukuoka | 1.06 (0.92–1.23) | 0.425 | 1.14 (0.90–1.44) | 0.290 |
| Saga | 1.14 (0.75–1.73) | 0.546 | 1.36 (0.65–2.86) | 0.416 |
| Nagasaki | 1.10 (0.79–1.53) | 0.577 | 0.93 (0.53–1.64) | 0.807 |
| Kumamoto | 0.86 (0.64–1.16) | 0.324 | 0.86 (0.53–1.40) | 0.535 |
| Oita | 0.96 (0.65–1.40) | 0.823 | 1.40 (0.75–2.61) | 0.291 |
| Miyazaki | 0.94 (0.62–1.43) | 0.781 | 0.98 (0.50–1.93) | 0.950 |
| Kagoshima | 0.73 (0.51–1.03) | 0.074 | 1.48 (0.88–2.51) | 0.142 |
| Okinawa | 1.40 (0.97–2.03) | 0.069 | 1.07 (0.60–1.91) | 0.824 |
| Highest educational level (SA) | 0.97 (0.93–1.00) | 0.066 | 1.00 (0.94–1.06) | 0.936 |
| Occupation type (SA) | ||||
| Agriculture, forestry and fisheries | 2.23 (1.43–3.49) | <0.001 | 0.54 (0.26–1.13) | 0.102 |
| Construction | 1.55 (1.22–1.99) | <0.001 | 1.22 (0.84–1.76) | 0.291 |
| Manufacturing | 1.74 (1.45–2.09) | <0.001 | 0.97 (0.73–1.30) | 0.860 |
| Information and communications | 1.90 (1.47–2.44) | <0.001 | 1.00 (0.68–1.47) | 0.999 |
| Transportation and postal services | 2.33 (1.81–3.01) | <0.001 | 1.37 (0.93–2.02) | 0.113 |
| Wholesale and retail trade | 1.98 (1.63–2.41) | <0.001 | 0.99 (0.72–1.35) | 0.926 |
| Finance and insurance | 2.12 (1.63–2.77) | <0.001 | 1.67 (1.12–2.50) | 0.012 |
| Real estate and goods rental and leasing | 1.94 (1.41–2.67) | <0.001 | 1.02 (0.61–1.69) | 0.945 |
| Scientific research, professional and technical services | 1.69 (1.22–2.34) | 0.002 | 1.01 (0.60–1.69) | 0.981 |
| Accommodations, food and beverage services | 1.65 (1.27–2.15) | <0.001 | 0.82 (0.54–1.26) | 0.370 |
| Living-related and personal services and amusement services | 2.03 (1.50–2.73) | <0.001 | 1.47 (0.93–2.33) | 0.100 |
| Education and learning support | 1.72 (1.36–2.18) | <0.001 | 1.19 (0.82–1.71) | 0.362 |
| Healthcare and welfare | 1.00 (reference) | NA | 1.00 (reference) | NA |
| Combined services | 1.33 (0.87–2.03) | 0.186 | 1.57 (0.88–2.80) | 0.123 |
| Services (not elsewhere classified) | 1.63 (1.35–1.97) | <0.001 | 1.13 (0.84–1.50) | 0.423 |
| Public service (not elsewhere classified) | 1.69 (1.32–2.16) | <0.001 | 1.43 (0.99–2.09) | 0.060 |
| Students | 2.32 (1.76–3.06) | <0.001 | 1.06 (0.70–1.58) | 0.794 |
| Homemaker | 1.83 (1.55–2.17) | <0.001 | 1.14 (0.87–1.50) | 0.325 |
| Others | 2.06 (1.72–2.46) | <0.001 | 1.30 (0.99–1.72) | 0.059 |
| Annual household income in 2020 (SA) | 0.99 (0.98–1.00) | 0.217 | 1.01 (0.99–1.03) | 0.548 |
| Healthcare-related characteristics, including health literacy | ||||
| Absence of underlying diseases (e.g. diabetes, heart failure, respiratory disease, COPD, etc., or on dialysis, or using immunosuppressive or anticancer drugs) (SA) | 1.22 (1.09–1.37) | <0.001 | 1.20 (0.99–1.45) | 0.068 |
| Psychological characteristics | ||||
| What is your best guess as to whether you will get COVID-19 within the next 6 months? (SA) – perceived risks of COVID-19 | ||||
| I don't think I will get COVID-19 | 1.20 (1.07–1.35) | 0.002 | 1.35 (1.12–1.64) | 0.002 |
| I think I will get a mild case of COVID-19 | 0.97 (0.87–1.10) | 0.672 | 0.91 (0.74–1.11) | 0.340 |
| I think I will get seriously ill from COVID-19 | 1.00 (reference) | NA | 1.00 (reference) | NA |
| I have already had COVID-19 | 4.25 (2.79–6.47) | <0.001 | 2.62 (1.55–4.42) | <0.001 |
| How do you think the disadvantages of the COVID-19 vaccine are? (SA) – perceived risks of a COVID-19 vaccine | ||||
| Very small | 0.24 (0.20–0.29) | <0.001 | 0.15 (0.10–0.21) | <0.001 |
| Small | 0.45 (0.41–0.49) | <0.001 | 0.44 (0.37–0.52) | <0.001 |
| Medium | 1.00 (reference) | NA | 1.00 (reference) | NA |
| Large | 1.21 (1.08–1.36) | <0.001 | 1.91 (1.63–2.24) | <0.001 |
| Very large | 2.53 (1.84–3.49) | <0.001 | 3.90 (2.66–5.72) | <0.001 |
| Do you think getting a COVID-19 vaccine will ease your anxiety? (SA) – perceived benefits of a COVID-19 vaccine | ||||
| Strongly disagree | 1.55 (1.18–2.03) | 0.002 | 2.81 (2.07–3.81) | <0.001 |
| Disagree | 1.24 (1.12–1.38) | <0.001 | 1.77 (1.52–2.06) | <0.001 |
| Neither agree nor disagree | 1.00 (reference) | NA | 1.00 (reference) | NA |
| Agree | 0.57 (0.53–0.62) | <0.001 | 0.61 (0.52–0.73) | <0.001 |
| Strongly agree | 0.74 (0.54–1.00) | 0.050 | 1.09 (0.63–1.89) | 0.761 |
| If others have been vaccinated against COVID-19, do you think you should be vaccinated as well? (SA) – perceived norms about a COVID-19 vaccine | ||||
| Strongly disagree | 0.40 (0.29–0.54) | <0.001 | 5.67 (4.16–7.73) | <0.001 |
| Disagree | 0.80 (0.70–0.91) | <0.001 | 3.55 (3.03–4.16) | <0.001 |
| Neither agree nor disagree | 1.00 (reference) | NA | 1.00 (reference) | NA |
| Agree | 0.27 (0.25–0.29) | <0.001 | 0.14 (0.12–0.17) | <0.001 |
| Strongly agree | 0.03 (0.02–0.04) | <0.001 | 0.03 (0.02–0.05) | <0.001 |
| Do you trust scientists in the field of vaccine development for COVID-19? (SA) – trusts about COVID-19 vaccine | ||||
| Strongly distrust | 0.71 (0.44–1.16) | 0.177 | 0.76 (0.44–1.30) | 0.315 |
| Distrust | 0.89 (0.74–1.07) | 0.196 | 1.01 (0.80–1.27) | 0.945 |
| Neutral | 1.00 (reference) | NA | 1.00 (reference) | NA |
| Trust | 0.71 (0.64–0.78) | <0.001 | 0.89 (0.74–1.06) | 0.178 |
| Strongly trust | 0.71 (0.51–0.99) | 0.047 | 0.55 (0.31–0.99) | 0.048 |
| Do you trust the public authorities to approve vaccines for COVID-19? (SA) – trusts about COVID-19 vaccine | ||||
| Strongly distrust | 2.19 (1.54–3.13) | <0.001 | 3.54 (2.36–5.29) | <0.001 |
| Distrust | 1.44 (1.26–1.65) | <0.001 | 1.79 (1.48–2.16) | <0.001 |
| Neutral | 1.00 (reference) | NA | 1.00 (reference) | NA |
| Trust | 0.64 (0.58–0.70) | <0.001 | 0.77 (0.64–0.92) | 0.006 |
| Strongly trust | 0.82 (0.56–1.19) | 0.291 | 0.74 (0.39–1.40) | 0.353 |
| Do you think that healthcare workers and employees of elderly care facilities should be vaccinated? (SA) – belief about COVID-19 vaccine | ||||
| Yes | 0.78 (0.62–0.99) | 0.037 | 0.17 (0.13–0.21) | <0.001 |
| No | 1.00 (reference) | NA | 1.00 (reference) | NA |
| Can't say either | 2.67 (2.11–3.38) | <0.001 | 0.66 (0.51–0.84) | <0.001 |
| Do you receive an influenza vaccine? (SA) | ||||
| Every year | 1.00 (reference) | NA | 1.00 (reference) | NA |
| Every few years | 1.46 (1.33–1.61) | <0.001 | 1.83 (1.52–2.21) | <0.001 |
| Rarely or never | 2.83 (2.61–3.07) | <0.001 | 5.73 (4.93–6.67) | <0.001 |
| Information sources about COVID-19 (MA) | ||||
| Physicians | 0.82 (0.72–0.92) | 0.001 | 0.70 (0.56–0.87) | 0.001 |
| Nurses | 0.79 (0.65–0.96) | 0.018 | 0.66 (0.48–0.91) | 0.010 |
| Television | 1.06 (0.96–1.18) | 0.244 | 0.81 (0.70–0.93) | 0.004 |
| Internet news sites | 1.21 (1.12–1.31) | <0.001 | 1.07 (0.94–1.21) | 0.290 |
| YouTube | 1.36 (1.14–1.61) | <0.001 | 1.09 (0.84–1.41) | 0.525 |
| Medical information sites | 0.64 (0.50–0.83) | <0.001 | 0.63 (0.42–0.95) | 0.026 |
| Family members | 1.13 (1.02–1.26) | 0.021 | 1.11 (0.92–1.34) | 0.288 |
| Scientists and researchers | 1.19 (0.93–1.52) | 0.168 | 1.80 (1.24–2.63) | 0.002 |
| Trust levels in information sources (MA) | ||||
| Physicians | 1.08 (0.98–1.18) | 0.103 | 0.99 (0.86–1.14) | 0.919 |
| Nurses | 1.02 (0.92–1.13) | 0.743 | 1.02 (0.86–1.19) | 0.854 |
| Television | 1.11 (1.01–1.21) | 0.022 | 1.02 (0.90–1.16) | 0.755 |
| Internet news sites | 1.06 (0.97–1.16) | 0.190 | 0.98 (0.84–1.13) | 0.733 |
| YouTube | 1.03 (0.93–1.14) | 0.527 | 1.21 (1.04–1.41) | 0.015 |
| Medical information sites | 0.97 (0.91–1.04) | 0.350 | 0.97 (0.87–1.08) | 0.575 |
| Family members | 1.02 (0.95–1.10) | 0.618 | 1.02 (0.91–1.15) | 0.727 |
| Scientists and researchers | 1.04 (0.96–1.13) | 0.320 | 0.98 (0.86–1.12) | 0.768 |
The estimates were derived from the multinomial logistic regression, in reference to the COVID-19 vaccine acceptance group. SA: single-answer questions; MA: multiple-answer question. Highest education levels and annual household income in 2020 (ordinal scale questions) were also treated as continuous variables. Age (continuous variable) and the presence or absence of underlying disease were considered only for the unstratified analysis. Only variables that are important for interpretation are left in this table; the complete table containing all variables left in the final model can be found in Supplementary Table 5.
Several psychological variables were associated with responding ‘not sure’ regarding the COVID-19 vaccine intention. The odds of responding ‘not sure’ were higher for those who tended to not get vaccinated against influenza, and the odds were also higher for those with lower perceived risks of COVID-19, those with higher perceived risk of a COVID-19 vaccine, lower perceived benefits of a COVID-19 vaccine and those with lower trust in scientists and public authorities involved in COVID-19 vaccines. For the belief that healthcare workers and employees of elderly care facilities should be vaccinated against COVID-19, those who answered "can't say either" had a higher odds of responding ‘not sure’ regarding the COVID-19 vaccine intention than those who answered "no" (2.67, 2.11–3.38). Similarly, for the perceived norm regarding whether one should be vaccinated if others are vaccinated, the odds were higher for those who answered "neither agree nor disagree" than for the other responses. Several sources of information about COVID-19 remained in the final models with statistical significance, including physicians, nurses, and television, medical information sites with lower odds, and internet news sits, YouTube, family members, and scientists and researchers with higher odds. The higher the level of trust in television as a source of COVID-19 information, the higher the odds of responding ‘not sure’ (1.11, 1.01–1.21).
The stratified analyses showed similar trends; however, there were some differences from the pooled analysis in terms of the statistical significance of variables and whether or not they remained in the final model: in Group (B), education level remained a significant variable, with higher education having lower odds (0.91, 0.83–1.00) (Supplementary Table 6). In Groups (B) and (D), gender was significantly associated with the vaccine intension, with women being more like to be unsure to take a COVID-19 vaccine. As for Group (D), the relationship between income level and responding ‘not sure’ was statistically significant, with higher income levels having lower odds (0.98, 0.97–1.00). In Groups (A), none of the occupation types were statistically significant and did not remain in the final models. Similarly, as for psychological characteristics, the relationship with vaccination intention was basically similar among the four Groups, although the statistical significance was slightly different them. On the other hand, the variables remaining in the final model and their significance for information source and trust largely varied between the Groups.
A similar trend was observed in the unwilling group (Table 2 and Supplementary Table 7). For the perceived norm regarding whether one should be vaccinated if others are vaccinated, the odds of responding ‘no’ regarding the COVID-19 vaccine intention were highest for those who answered "strongly disagree" than for the other responses. In Group (A), regarding the risk perception of COVID-19, those who were not anxious about COVID-19 at all were less likely to respond 'no' regarding the COVID-19 vaccine intention, which was the opposite of the results of the pooled analysis and the other Groups (Supplementary Table 7).
Reasons for responding ‘not sure’ or ‘no’ regarding intention to be vaccinated against COVID-19
The most common reason for responding ‘not sure’ or ‘no’ regarding the COVID-19 vaccine intention was specific anxiety about the COVID-19 vaccine (Table 3), especially its side effects and safety (unsure 79.1%, unwilling 68.2%). The second most common reason was related to attitude towards a vaccine in general, not limited to the COVID-19 vaccine, especially side effects and the safety of vaccines (46.3%, 41.0%). The third most common reason was that more information was necessary to decide whether or not to be vaccinated, especially on comparability with personal health conditions (44.0%, 32.5%). The unsure group was more likely to request than the unwilling group more information to decide whether or not to be vaccinated regarding doctors’ recommendations (21.2%, 10.0%) and whether other people have been vaccinated (19.2%, 10.6%). In both groups, approximately 20% of respondents were unsure or unwilling to take a COVID-19 vaccine because they thought the vaccine might not be effective against COVID-19 variants.
Whereas the elderly or those with underlying diseases were more likely to need information about compatibility with personal health conditions, younger adults and those without underlying diseases were more likely to need information about whether other people have been vaccinated or not (Supplementary Table 8).
Discussion
Vaccination intention surveys have rarely been conducted in Asia,[1,16,17] and to our knowledge this study provides the largest survey results from Japan, an East Asian country where vaccine confidence is among the lowest in the world.[20] Among 30,000 nationally representative individuals aged 20 years and older, the percentages of respondents responding ‘yes’, ‘not sure’, or ‘no’ regarding the intention to be vaccinated against COVID-19 were 56.1%, 32.9%, and 11.0%, respectively. These findings are roughly consistent with the results of an online survey conducted just one month before our survey among the general public aged 20 to 79, which showed that 62.1% of respondents were willing to receive the vaccine, although the response format was different.[34] This previous study collected data from about 3,000 participants by quota sampling method based on age, gender, and residential area, similar to our study sampling method. The uniqueness of our study includes the fact that we did not set an upper age limit for the participants, and by collecting data from more than 30,000 participants, we were able to perform stratified analyses, by building regression models for four population groups based on age and the presence of underlying diseases; these conditions were the same as those set by the government for the priority vaccination population, allowing for a more pragmatic and policy-oriented analysis. In addition, the present study included questions about the sources of information about the COVID-19 and the level of confidence in them, providing useful information for the development of public health messaging to promote vaccination. Finally, we also asked about reasons for being unsure or unwilling to be vaccinated against COVID-19.
Our findings also suggest that the proportions of respondents who are accepting the COVID-19 vaccine may be comparatively similar to Western countries. In the latest systematic review and meta-analysis,[17] 58,656 participants from 28 large nationally representative survey samples in 13 countries, not including Japan (mostly from the United States, United Kingdom, and Canada, but also France, Australia, China, Denmark, Germany, Italy, Ireland, Netherlands, Poland, Portugal) were assessed for their COVID-19 vaccine intentions. The proportion of people with intention not to be vaccinated against COVID-19 has increased over time, with pooled data from surveys conducted between June and October 2020 showing that 60% (95% CI 49%–69%) had intention to vaccinate and 20% (13%–29%) had intention not to vaccinate, although intentions vary widely across samples and countries. Some Asian countries, had higher acceptance: 88.6–91.3% in China,[1,35] 79.8% in South Korea,[1] and 67.9% in Singapore during the early pandemic period (March–June 2020).[1] Similar vaccination intentions were obtained in the French survey at that time (76%),[36] but the latest estimate for France (September-October 2020) showed a decreasing trend to 52%.[37]
Sociodemographic and health-related profile of those being unsure or unwilling to be vaccinated against COVID-19
After adjusting for covariates, sociodemographic factors such as age, gender, education, and income level were statistically significantly associated with being unsure or unwilling to take the COVID-19 vaccine (although in some cases only in the stratified analyses). These results are consistent with a number of studies which have found that younger age is associated with being unsure or unwilling to be vaccinated against COVID-19.[27,34,[38], [39], [40]] Women more likely to be unsure or unwilling to take a COVID-19 vaccine; this was consistent with previous studies.[2,9,34,[39], [40], [41], [42], [43], [44]] Similar to previous studies,[9,34,39,40,[43], [44], [45], [46]] people with lower education levels and incomes were more likely to be unsure or unwilling to be vaccinated against COVID-19.
The statistical significance of the relationship between education, income, occupation as well as prefecture of residence and the COVID-19 vaccination intention slightly differed in the stratified analyses for the different populations. These suggest that strategies that explicitly target specific populations and address population-specific factors may be more effective. For example, we have identified gender as an important factor in vaccination intentions among elderly and younger adults without underlying diseases, suggesting that gender-based approaches may be effective.
Psychological profile of people who are unsure or unwilling to be vaccinated against COVID-19
To date, many psychological characteristics of individuals, such as perceived risks, perceived norms, and trust, have been confirmed to be associated with vaccine intention.[47], [48], [49], [50], [51], [52], [53], [54] Similar to these past findings, we found that in Japan, the perceived risks of COVID-19, perceived risk of a COVID-19 vaccine, perceived benefits of a COVID-19 vaccine, trust in scientists and public authorities, and the belief that healthcare workers should be vaccinated were significantly associated with responding ‘not sure’ or ‘no’ regarding the intention to be vaccinated against COVID-19.
These findings were in line with previous studies conducted in other countries attempting to understand the reasons behind uncertainty or unwillingness to be vaccinated against COVID-19. Barello et al (2020) and Dror et al. (2020) reported that people with lower levels of perceived severity of COVID-19 and personal vulnerability to the risk of infection were less likely to accept the COVID-19 vaccine.[18,19] Barello et al. (2021) and Lin et al. (2020) demonstrated that the perceived safety of the COVID-19 vaccine was a major determinant of vaccine uptake.[14,16] Murphy et al. (2021) demonstrated that COVID-19 vaccine-hesitant people were distinguished from vaccine-accepting people by being more distrustful of experts and authority figures (i.e. scientists, health care professionals), and more likely to hold conspiratorial and paranoid beliefs.[3] In our study, those with influenza vaccination experience were more likely to accept the COVID-19 vaccine, as shown in previous studies regarding vaccine intention generally,[38,39,45] as well as in the COVID-19 context.[13]
One of the major differences between the unsure and unwilling groups in this study was their relationship with the perceived norm regarding a COVID-19 vaccine that one should be vaccinated if others are vaccinated. In the unsure group, respondents who took the neutral position of "neither agree nor disagree" were more likely to be unsure to take a COVID-19 vaccine. However, in the unwilling group, respondents who answered "strongly disagree" were more likely to be unwilling to take a COVID-19 vaccine. These findings are consistent with psychological evidence that people who are unsure or non-professional (i.e. lay people) about a certain topic tend to choose neutral answers in a survey.[55] A similar result was observed in a study regarding the perceived effectiveness of preventive behaviors against COVID-19.[56] Furthermore, a previous study showed that the intention to wear a mask as a COVID-19 preventive measure was also associated with the perceived norm.[50] The relationship of psychological characteristics with COVID-19 vaccination intention was basically similar among the stratified four Groups, although their statistical significances were slight difference between them. In the pooled analysis, the more anxious about COVID-19 the respondents were, the less likely they were to answer 'no' regarding the intention to be vaccinated, while the opposite was true for Group (A), who were elderly with underlying diseases. This may be somewhat explained by the fact that there were more people in this group who were concerned about compatibility with personal health conditions and side effects and safety of the vaccine, but further investigation is required.
Implications
The responsibility for disseminating public health messages tends to fall primarily on public authorities as well as scientists. People who are unsure or unwilling to take a COVID-19 vaccine may feel concern over the vaccination recommendations by public authorities and scientists if they have a high level of distrust of the messages sent by them.[52,57] In the present study, in Japan, the trust in public authorities and scientists involved in COVID-19 vaccines was strongly correlated with COVID-19 vaccine intention, which reaffirm the importance of ensuring trust in those who represent these authorities.[52,57]
We then demonstrated that many respondents presented concerns about the side effects and safety of a COVID-19 vaccine as a major reason for being unsure or unwilling to be vaccinated. In order to decide whether or not to get the vaccine, many respondents requested more information about the compatibilities between the vaccine and their personal health conditions, whether other people had been vaccinated, the effectiveness of vaccines against variants, and doctors’ recommendations. These reasons were also reported in Fisher et al.’s (2020) study conducted in the United States.[27] Proactive messaging of the above-mentioned information from public authorities and scientists, especially those in positions of high trust, may result in those who had previously been unsure or unwilling to be vaccinated against COVIS-19 to be more receptive to a COVID-19 vaccine.
The campaign against the HPV vaccination in Japan was based heavily on a discourse based around side-effects,[21] as was the now-discredited anti-MMR (measles, mumps, and rubella) campaign spearheaded by Wakefield et al.[58] This showed the importance of combating misinformation about side-effects, and acting early and decisively to dispute claims of the danger of vaccines, to prevent the possibility of debates about single vaccines cross-contaminating all information about vaccine safety, and swamping information about the health benefits of vaccination with exaggerated stories about the risks. Fortunately, this study also showed that trust in information from the government and local authorities as well as from medical professionals was relatively high, which indicates that an approach based on early and accurate dissemination of information countering exaggerated claims of side-effects may work as a practical solution. Note that the odds of being unsure or unwilling to be vaccinated against COVID-19 were higher for those who uses internet news sites, YouTube, family members, and scientists and researchers and lower for those who relied on physicians, nurses, television, and medical information sites as their sources of information of COVID-19. These results are also consistent with several previous studies, which suggested, for example, that people who use the internet may be less aware of the safety of vaccines and their benefits,[59] and that people who rely on informal sources of information, such as family members, may have less trust in health care.[60]
Meanwhile, in this study, the higher the level of trust in television as an information source, the more likely they were to be unsure to take the COVID-19 vaccine (although this was not statistically significant for the unwilling group). Given the higher levels of uncertainty and unwillingness seen in people who watch television as an information source of COVID-19, and the ubiquitous nature of television and print media in Japan, it is important that coverage in these media sources be balanced and properly objective.
Moreover, this study showed that the perceived benefit of a COVID-19 vaccine was associated with COVID-19 vaccine intention. It would be important for messages to those who are unsure or unwilling to take the vaccinate to emphasize the personal benefits of a COVID-19 vaccine. Furthermore, Murphy et al. (2021) reported that people who are hesitant about COVID-19 vaccination are likely less agreeable, less conscientious, and less emotionally stable.[3] Public health messages aimed at these populations need to be clear, direct, and repeated.[3]
We found that the unsure and unwilling groups (as well as those who are accepting of it) not only obtain information from traditional sources (television, newspapers, local authorities, and the government), but also from internet news sites, search engines, and especially from SNS. Similar observations were reported in the United Kingdom.[3] These results have implications for how to effectively communicate with these population. Globally, SNS is being used as a platform to disseminate messages to vaccine hesitant individuals.[61] Although caution is needed due to the fact that SNS have the potential to raise concerns about vaccine safety via the contemporary anti-vaccination movement and/or to spread misinformation, which in turn fuels vaccine hesitancy,[62] public authorities should disseminate information through multiple media channels (including SNS) to increase their chances of reaching the vaccine hesitant individuals. Combining knowledge of what sources of information those who are unsure or unwilling to be vaccinated access and which they trust most will help public authorities to effectively design and deliver public health messages, resulting in more people voluntarily accepting a COVID-19 vaccine.
Limitations
This study has some limitations. Self-selection bias may have affected the representativeness of the survey participants. For example, whether people participate in our survey may depend on their interest in the scope of the study. However, since our survey was conducted online, and respondents were given ‘points’, those who were not interested in the topic of this survey may have been motivated to participate. Therefore, it is thought to be more effective in reducing the effect of such bias than a survey that invites participants to a certain venue or that employed a mailing method with no other incentives provided. Other selection or sampling biases commonly linked to online surveys also need to be recognized.[63] The distribution of demographic characteristics of our study population was similar to that of the total population owing to a quota sampling method based on age, gender, and prefecture population ratios, according to the National Census 2015.[24] However, we were not able to adjust the sampling method with respect to education level. The percentage of respondents who attended university or have a higher level of education (43.9%) was larger than that of the total population (16.1%), reported by the 2010 National Census.[64] Given that several studies have suggested that lower education level is associated with being less likely to be vaccinated against COVID-19,[16,17] our survey data on vaccine unsureness and unwillingness might be underestimated. According to the Comprehensive Survey of Living Conditions (CSLC, a nationally representative cross-sectional annual survey conducted by the MHLW) in 2019, the year before our survey was conducted, 45.4% of households had an annual household income of 4 million yen or less.[65] This annual income level accounts for 45.3% of the households in this survey, which is very close to the results of the CSLC survey. It is important to recognize that the online collection of these data skews the participants towards more digitally experienced and skilled users, resulting in a bias towards representativeness, especially of the older population.[66] It is also important to note that online surveys may lead to lower levels of anxiety about certain social issues compared to interviews or other survey methods.[67] Additionally, as a cross-sectional design was used, a causal relationship was difficult to infer. Also, psychological characteristics were measured in this study based on a single item rather than a validated scale. The reason for this was to take into account a number of variables, but also for research and policy benefits such as reduced respondent burden and ease of interpretation.[26] The other limitations of our study include the timing of the survey in February–March, 2021. At this time, there was little information about vaccination locations, and people's vaccination intentions might have been influenced over time with new information regarding vaccination convenience.[5,6] In addition, we used three options for vaccination intentions in our study. However, in general, categorization of information means loss of within-category information; everyone above or below the cut-point is treated as equal. The level of willingness/unsureness/unwillingness to be vaccinated against COVID-19 may be likely to be very different among each category. Meanwhile, categorical variables can make the analysis and interpretation of results simple. Thus, we used categorical variables for the vaccine intention in this study because we believe it is important for the interpretation of results to be easily understandable to the public in order to build public health messaging that promotes vaccination, and to increase comparability with previous studies.[16,17]
Conclusions
Despite these limitations, our findings provide important evidence on the level of unsureness and unwillingness to be vaccinated against COVID-19 in Japan. Further, to the best of our knowledge, our findings were based on the largest survey to date, which allows for stratified analysis according to population groups. As previous studies in other countries have shown, a large proportion of the population is unsure or unwilling to take COVID-19 vaccine. This is especially true in Japan. In order for global vaccine development efforts to be successful, another effort must be strongly implemented in parallel: how to get these people to accept the vaccine. We believe that our findings underscore the importance of identifying, understanding, and addressing the various sociodemographic and psychological factors as well as the information sources and the trust levels in them that contribute to being unsure and unwilling to take the COVID-19 vaccine to better inform public health messages from public authorities.
Declaration of Competing Interest
The authors declare that they have no competing interests.
Acknowledgments
Contributors
Conception/design of the work: S.N., A.E., D.Y., T.K., Y.T., M.M., H.S., K.M.S., H.K., S.K., K.S., Y.Y., and H.M.; acquisition of data: S.N., H.S., K.M.S., H.K., S.K., K.S., and H.M.; analysis of data: S.N., A.E., D.Y., T.K., and Y.T.; interpretation of findings: all authors; drafting of the work: S.N.; substantially revised the work: S.N., A.E., D.Y., T.K., Y.T., M.M., S.G., S.S., M.A., K.S., and Y.Y.
Data sharing
The datasets generated during and/or analyzed during the current study are not publicly available due to ethical considerations but are available from the corresponding author on reasonable request.
Acknowledgment
We would like to thank the Japan Epidemiological Association and the Japanese Society of Infectious Diseases as well as those involved in the COVID-19 Information Value Improvement and Link project (CIVIL project) for supervising the questionnaires. This work was partly funded by research grants from the Ministry of Health, Labour and Welfare of Japan (H29-Gantaisaku-ippan-009). The funding source of this study had no role in the study design, data collection, data analysis, data interpretation, or writing of the report. The views expressed in this paper are solely those of the authors. The results of the survey were partially reported at Medical Note on March 26, 2021, in Japanese, including the proportions of COVID-19 vaccine acceptance, hesitance, and resistance in the pooled analysis: https://medicalnote.jp/nj_articles/210326-003-HG.
Funding
This work was partly funded by research grants from the Ministry of Health, Labour and Welfare of Japan (H29-Gantaisaku-ippan-009).
Ethics statement
Ethical approval was granted by the Ethics Committee of Keio University School of Medicine under authorization number 20200340. Respondents had to provide their consent before they proceeded to the questionnaire response page.
Editor note: The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.lanwpc.2021.100223.
Contributor Information
Shuhei Nomura, Email: nomura@keio.jp.
Hiroaki Miyata, Email: hm@keio.jp.
Appendix. Supplementary materials
References
- 1.Lazarus JV, Ratzan SC, Palayew A. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Neumann-Bohme S, Varghese NE, Sabat I. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J Health Econ. 2020;21(7):977–982. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murphy J, Vallieres F, Bentall RP. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021;12(1):29. doi: 10.1038/s41467-020-20226-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schoch-Spana M, Brunson EK, Long R. The public's role in COVID-19 vaccination: Human-centered recommendations to enhance pandemic vaccine awareness, access, and acceptance in the United States. Vaccine. 2020 doi: 10.1016/j.vaccine.2020.10.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.MacDonald NE, SWGoV Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 6.Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007-2012. Vaccine. 2014;32(19):2150–2159. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 7.Cornwall W. Officials gird for a war on vaccine misinformation. Science. 2020;369(6499):14–15. doi: 10.1126/science.369.6499.14. [DOI] [PubMed] [Google Scholar]
- 8.Lazarus JV, Wyka K, Rauh L. Hesitant or not? The association of age, gender, and education with potential acceptance of a COVID-19 vaccine: a country-level analysis. J Health Commun. 2020;25(10):799–807. doi: 10.1080/10810730.2020.1868630. [DOI] [PubMed] [Google Scholar]
- 9.Rhodes A, Hoq M, Measey MA, Danchin M. Intention to vaccinate against COVID-19 in Australia. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30724-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Williams L, Gallant AJ, Rasmussen S. Towards intervention development to increase the uptake of COVID-19 vaccination among those at high risk: Outlining evidence-based and theoretically informed future intervention content. Br J Health Psychol. 2020;25(4):1039–1054. doi: 10.1111/bjhp.12468. [DOI] [PubMed] [Google Scholar]
- 11.Lazarus JV, Binagwaho A, El-Mohandes AAE. Keeping governments accountable: the COVID-19 Assessment Scorecard (COVID-SCORE) Nat Med. 2020;26(7):1005–1008. doi: 10.1038/s41591-020-0950-0. [DOI] [PubMed] [Google Scholar]
- 12.Hornsey MJ, Harris EA, Fielding KS. The psychological roots of anti-vaccination attitudes: A 24-nation investigation. Health Psychol. 2018;37(4):307–315. doi: 10.1037/hea0000586. [DOI] [PubMed] [Google Scholar]
- 13.Graffigna G, Palamenghi L, Boccia S, Barello S. Relationship between citizens' health engagement and intention to take the COVID-19 vaccine in Italy: a mediation analysis. Vaccines (Basel) 2020;8(4) doi: 10.3390/vaccines8040576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barello S, Palamenghi L, Graffigna G. Looking inside the ‘black box’ of vaccine hesitancy: unlocking the effect of psychological attitudes and beliefs on COVID-19 vaccine acceptance and implications for public health communication. Psychological Medicine. 2021:1–2. doi: 10.1017/S003329172100101X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hornsey MJ, Fielding KS. Attitude roots and Jiu Jitsu persuasion: Understanding and overcoming the motivated rejection of science. Am Psychol. 2017;72(5):459–473. doi: 10.1037/a0040437. [DOI] [PubMed] [Google Scholar]
- 16.Lin C, Tu P, Beitsch LM. Confidence and receptivity for COVID-19 vaccines: a rapid systematic review. Vaccines (Basel) 2020;9(1) doi: 10.3390/vaccines9010016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Robinson E, Jones A, Lesser I, Daly M. International estimates of intended uptake and refusal of COVID-19 vaccines: A rapid systematic review and meta-analysis of large nationally representative samples. Vaccine. 2021;39(15):2024–2034. doi: 10.1016/j.vaccine.2021.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dror AA, Eisenbach N, Taiber S. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35(8):775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barello S, Nania T, Dellafiore F, Graffigna G, Caruso R. Vaccine hesitancy' among university students in Italy during the COVID-19 pandemic. Eur J Epidemiol. 2020;35(8):781–783. doi: 10.1007/s10654-020-00670-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Figueiredo A, Simas C, Karafillakis E, Paterson P, Larson HJ. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: a large-scale retrospective temporal modelling study. Lancet. 2020;396(10255):898–908. doi: 10.1016/S0140-6736(20)31558-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gilmour S, Kanda M, Kusumi E, Tanimoto T, Kami M, Shibuya K. HPV vaccination programme in Japan. Lancet. 2013;382(9894):768. doi: 10.1016/S0140-6736(13)61831-0. [DOI] [PubMed] [Google Scholar]
- 22.Hanley SJ, Yoshioka E, Ito Y, Kishi R. HPV vaccination crisis in Japan. Lancet. 2015;385(9987):2571. doi: 10.1016/S0140-6736(15)61152-7. [DOI] [PubMed] [Google Scholar]
- 23.Cross Marketing Inc. Web surveys [Japanese]. https://www.cross-m.co.jp/service/netresearch/(accessed July 6, 2021).
- 24.Statistics Bureau of Japan. Population Census 2015 Statistical Maps of Japan. 2018. https://www.stat.go.jp/english/data/chiri/map/c_koku/2015.html (Accessed 13 March 2020).
- 25.Masuda S, Sakagami T, Morii M. Comparison among methods for improving response quality of surveys. Shinrigaku Kenkyu. 2019;90(5):463–472. [Google Scholar]
- 26.Bowling A. Just one question: If one question works, why ask several? Journal of Epidemiology and Community Health. 2005;59(5):342. doi: 10.1136/jech.2004.021204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 Vaccine: a survey of U.S. adults. Ann Intern Med. 2020;173(12):964–973. doi: 10.7326/M20-3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.The Asahi Shimbun. Japan has new virus variant that may reduce vaccines’ efficacy. 2021. http://www.asahi.com/ajw/articles/14204131 (Accessed 22 March 2021).
- 29.Ministry of Health, Labour and Welfare. Proposal for consideration of priority vaccination against COVID-19 [Japanese]. 2021. https://www.mhlw.go.jp/content/000739377.pdf (Accessed 6 April 2021).
- 30.Hastie T, Tibshirani R, Friedman J. Linear methods for regression. In: Hastie T, Tibshirani R, Friedman J, eds. The elements of statistical learning: data mining, inference, and prediction. New York, NY: Springer New York; 2009: 43-99.
- 31.Vincent M, Hansen NR. Sparse group lasso and high dimensional multinomial classification. Comput Stat Data An. 2014;71:771–786. [Google Scholar]
- 32.Tibshirani R. Regression shrinkage and selection via the Lasso. Journal of the Royal Statistical Society Series B (Methodological) 1996;58(1):267–288. [Google Scholar]
- 33.Toyo Keizai. Toyo Keizai Online "Coronavirus Disease (COVID-19) Situation Report in Japan". 2020. https://toyokeizai.net/sp/visual/tko/covid19/ (Accessed 6 April 2021).
- 34.Machida M, Nakamura I, Kojima T. Acceptance of a COVID-19 Vaccine in Japan during the COVID-19 Pandemic. Vaccines. 2021;9(3) doi: 10.3390/vaccines9030210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang J, Jing R, Lai X. Acceptance of COVID-19 Vaccination during the COVID-19 Pandemic in China. Vaccines (Basel) 2020;8(3) doi: 10.3390/vaccines8030482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ward JK, Alleaume C, Peretti-Watel P, Group C. The French public's attitudes to a future COVID-19 vaccine: The politicization of a public health issue. Soc Sci Med. 2020;265 doi: 10.1016/j.socscimed.2020.113414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hacquin A-S, Altay S, Ed Araujo, Chevallier C, Mercier H. Sharp rise in vaccine hesitancy in a large and representative sample of the French population: reasons for vaccine hesitancy. PsyArXiv. 2020 November 16. [Google Scholar]
- 38.Faasse K, Newby J. Public perceptions of COVID-19 in Australia: perceived risk, knowledge, health-protective behaviors, and vaccine intentions. Front Psychol. 2020;11 doi: 10.3389/fpsyg.2020.551004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Paul E, Steptoe A, Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. The Lancet Regional Health - Europe. 2021;1 doi: 10.1016/j.lanepe.2020.100012. 100012- [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Malik AA, McFadden SM, Elharake J, Omer SB. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26 doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pulcini C, Massin S, Launay O, Verger P. Factors associated with vaccination for hepatitis B, pertussis, seasonal and pandemic influenza among French general practitioners: a 2010 survey. Vaccine. 2013;31(37):3943–3949. doi: 10.1016/j.vaccine.2013.06.039. [DOI] [PubMed] [Google Scholar]
- 42.Flanagan KL, Fink AL, Plebanski M, Klein SL. Sex and gender differences in the outcomes of vaccination over the life course. Annu Rev Cell Dev Biol. 2017;33:577–599. doi: 10.1146/annurev-cellbio-100616-060718. [DOI] [PubMed] [Google Scholar]
- 43.The COCONEL Group A future vaccination campaign against COVID-19 at risk of vaccine hesitancy and politicisation. Lancet Infect Dis. 2020;20(7):769–770. doi: 10.1016/S1473-3099(20)30426-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Loomba S, de Figueiredo A, Piatek SJ, de Graaf K, Larson HJ. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat Hum Behav. 2021 doi: 10.1038/s41562-021-01056-1. [DOI] [PubMed] [Google Scholar]
- 45.Sherman SM, Smith LE, Sim J. COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Hum Vaccin Immunother. 2020:1–10. doi: 10.1080/21645515.2020.1846397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Klevens RM, Luman ET. U.S. children living in and near poverty: risk of vaccine-preventable diseases. Am J Prev Med. 2001;20(4):41–46. doi: 10.1016/s0749-3797(01)00281-1. Suppl. [DOI] [PubMed] [Google Scholar]
- 47.McHale P, Keenan A, Ghebrehewet S. Reasons for measles cases not being vaccinated with MMR: investigation into parents' and carers' views following a large measles outbreak. Epidemiol Infect. 2016;144(4):870–875. doi: 10.1017/S0950268815001909. [DOI] [PubMed] [Google Scholar]
- 48.Suk JE, Lopalco P, Celentano Pastore, Hesitancy L. trust and individualism in vaccination decision-making. PLoS Curr. 2015;7 doi: 10.1371/currents.outbreaks.49dba84ad4146de33706b1f131d7caa3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Murakami H, Kobayashi M, Hachiya M, Khan ZS, Hassan SQ, Sakurada S. Refusal of oral polio vaccine in northwestern Pakistan: a qualitative and quantitative study. Vaccine. 2014;32(12):1382–1387. doi: 10.1016/j.vaccine.2014.01.018. [DOI] [PubMed] [Google Scholar]
- 50.Nakayachi K, Ozaki T, Shibata Y, Yokoi R. Why do Japanese people use masks against COVID-19, even though masks are unlikely to offer protection from infection? Front Psychol. 2020;11:1918. doi: 10.3389/fpsyg.2020.01918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jamison AM, Quinn SC, Freimuth VS. You don't trust a government vaccine": Narratives of institutional trust and influenza vaccination among African American and white adults. Soc Sci Med. 2019;221:87–94. doi: 10.1016/j.socscimed.2018.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kennedy J. Populist politics and vaccine hesitancy in Western Europe: an analysis of national-level data. Eur J Public Health. 2019;29(3):512–516. doi: 10.1093/eurpub/ckz004. [DOI] [PubMed] [Google Scholar]
- 53.Mesch GS, Schwirian KP. Social and political determinants of vaccine hesitancy: Lessons learned from the H1N1 pandemic of 2009-2010. Am J Infect Control. 2015;43(11):1161–1165. doi: 10.1016/j.ajic.2015.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Karafillakis E, Larson HJ, consortium A The benefit of the doubt or doubts over benefits? A systematic literature review of perceived risks of vaccines in European populations. Vaccine. 2017;35(37):4840–4850. doi: 10.1016/j.vaccine.2017.07.061. [DOI] [PubMed] [Google Scholar]
- 55.Fischhoff B, Kadvany J. Oxford University Press; 2011. Risk: a very short introduction Oxford. [Google Scholar]
- 56.Nakayachi K, Ozaki T, Shibata Y, Yokoi R. A comparison of perceived effectiveness of preventive behaviors against COVID-19 between the public and medical experts: Not so different in means, but in distributions. J Health Psychol. 2021 doi: 10.1177/1359105321999701. [DOI] [PubMed] [Google Scholar]
- 57.McHale P, Keenan A, Ghebrehewet S. Reasons for measles cases not being vaccinated with MMR: investigation into parents' and carers' views following a large measles outbreak. Epidemiology and Infection. 2016;144(4):870–875. doi: 10.1017/S0950268815001909. [DOI] [PubMed] [Google Scholar]
- 58.The Editors of The Lancet Retraction—Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. The Lancet. 2010;375(9713):445. doi: 10.1016/S0140-6736(10)60175-4. [DOI] [PubMed] [Google Scholar]
- 59.Jones AM, Omer SB, Bednarczyk RA, Halsey NA, Moulton LH, Salmon DA. Parents' source of vaccine information and impact on vaccine attitudes, beliefs, and nonmedical exemptions. Adv Prev Med. 2012;2012 doi: 10.1155/2012/932741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Eller NM, Henrikson NB, Opel DJ. Vaccine information sources and parental trust in their child's health care provider. Health Educ Behav. 2019;46(3):445–453. doi: 10.1177/1090198118819716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Allen JD, Hollander J, Gualtieri L, Falconi TMA, Savir S, Agenor M. Feasibility of a twitter campaign to promote HPV vaccine uptake among racially/ethnically diverse young adult women living in public housing. Bmc Public Health. 2020;20(1) doi: 10.1186/s12889-020-08824-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Broadbent JJ. Vaccine hesitancy: misinformation on social media. BMJ. 2019;366:l4457. doi: 10.1136/bmj.l4457. [DOI] [PubMed] [Google Scholar]
- 63.Szolnoki G, Hoffmann D. Online, face-to-face and telephone surveys—Comparing different sampling methods in wine consumer research. Wine Economics and Policy. 2013;2(2):57–66. [Google Scholar]
- 64.Statistics Bureau of Japan. Population Census 2010 Statistical Maps of Japan. 2013. https://www.stat.go.jp/english/data/chiri/map/c_koku/2010.html (Accessed 5 June 2021).
- 65.Ministry of Health, Labour and Welfare. the 2019 Comprehensive Survey of Living Conditions [Japanese]. 2020. https://www.mhlw.go.jp/toukei/saikin/hw/k-tyosa/k-tyosa19/index.html (Accessed 5 June 2021).
- 66.Hargittai E, Piper AM, Morris MR. From internet access to internet skills: digital inequality among older adults. Universal Access in the Information Society. 2019;18(4):881–890. [Google Scholar]
- 67.Kishikawa Y, Murayama R, Fujinaga A, Uchiyama I. The validity of web survey on risk perception and environmental problem. Japanese Journal of Risk Analysis. 2018;28(1):3–11. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.