Abstract
Objectives
The SARS-CoV-2 pandemic greatly influenced the overall quality of healthcare. The purpose of this study was to compare the time variables for acute stroke treatment and evaluate differences in the pre-hospital and in-hospital care before and during the SARS-CoV-2 pandemic, as well as between the first and second waves.
Materials and methods
Observational and retrospective study from an Italian hospital, including patients who underwent thrombectomy between January 1st 2019 and December 31st 2020.
Results
Out of a total of 594 patients, 301 were treated in 2019 and 293 in 2020. The majority observed in 2019 came from spoke centers (67,1%), while in 2020 more than half (52%, p < 0.01) were evaluated at the hospital's emergency room directly (ER-NCGH). When compared to 2019, time metrics were globally increased in 2020, particularly in the ER-NCGH groups during the period of the first wave (N = 24 and N = 56, respectively): “Onset-to-door”:50,5 vs 88,5, p < 0,01; “Arrival in Neuroradiology – groin”:13 vs 25, p < 0,01; “Door-to-groin”:118 vs 143,5, p = 0,02; “Onset-to-groin”:180 vs 244,5, p < 0,01; “Groin-to-recanalization”: 41 vs 49,5, p = 0,03. When comparing ER-NCGH groups between the first (N = 56) and second (N = 49) waves, there was an overall improvement in times, namely in the “Door-to-CT” (47,5 vs 37, p < 0,01), “Arrival in Neuroradiology – groin” (25 vs 20, p = 0,03) and “Onset-to-groin” (244,5 vs 227,5, p = 0,02).
Conclusions
During the SARS-CoV-2 pandemic, treatment for stroke patients was delayed, particularly during the first wave. Reallocation of resources and the shutting down of spoke centers may have played a determinant role.
Key Words: SARS-CoV-2, Pandemic, Italy, Stroke, Endovascular, Thrombectomy
Abbreviations: ASPECTS, Alberta Stroke Programme Early CT Score; ER, Emergency Room; ER-NCGH, Emergency Room of Niguarda Ca’ Granda Hospital; IQR, Interquartile range; NCGH, Niguarda Ca’ Granda Hospital; NIHSS, National Institutes of Health Stroke Scale; SC, Spoke center
Introduction
Under the banner of “time is brain”,1 the race towards achieving the fastest treatment in acute stroke is ongoing. Metrics such as “Onset-to-door”, “Door-to-groin” and “Groin-to-recanalization” are used to assess the results and ultimately allow to achieve a better quality of care.
The SARS-CoV-2 infection first appeared in late 2019 in Wuhan, China, and quickly evolved into a global pandemic in 2020. Last year, more than 82 million people worldwide contracted the infection and more than 1.8 million died.2 This reality had an inevitable impact in healthcare, namely in the management of acute ischaemic stroke. The very basis of social distancing and the isolation measures that slow down the viral spread, in turn work against stroke detection, which relies on someone else to quickly detect a given patient's symptoms.3
Italy was the first western country to suffer with the viral spread,4 , 5 and as early as February 2020, professionals were dealing with an unknown threat before every other country in Europe. This pandemic brought about a paradigm shift, prompting not only changes in hospital care, but also social challenges, and Italy was at the forefront of the battle.5 The initial attempts to contain the spread of the virus were insufficient and hospital capacity, as well as resources and personnel were lacking due to reallocation to COVID-wards, with measures going as far as closing down strategic departments,5 , 6 such as stroke units.
Lombardy was the region in Italy with the highest number of SARS-CoV-2 infections during the first wave.5 In the specific case of the Niguarda Ca’ Granda Hospital (NCGH), the initial plan was for it to remain a mostly SARS-CoV-2 free hospital, given its status as a referral center, particularly for neurointensive care.5 However, on February 22nd the first thrombectomy on a SARS-CoV-2 positive patient took place, and by then NCGH was already at the center of the epidemic in Milan, Lombardy. Amidst the chaos ensued by the rapid viral spread, most spoke centers (SC) were shut down and the majority of cases of suspected stroke were now coming directly to the emergency room (ER) of NCGH.
Objectives
The aim of this study is to characterize the impact of the SARS-CoV-2 pandemic on the medical system's responsiveness regarding endovascular treatment for ischaemic stroke. As secondary objectives, the authors intended to compare differences between the first and second waves and to evaluate how changes in the pre-hospital organization might have influenced the results.
Materials and methods
Population
This is an observational and retrospective study based on the prospectively managed internal database of the Neuroradiology Department of NCGH in Milan, Italy. The clinical sample was retrieved by searching for patients who underwent endovascular treatment for ischemic stroke between January 1st 2019 and December 31st 2020, and it included those whose first medical evaluation took place directly at the ER of NCGH or elsewhere in the hospital in case of inpatients (intra-hospital), and those that were redirected from one of the SC.
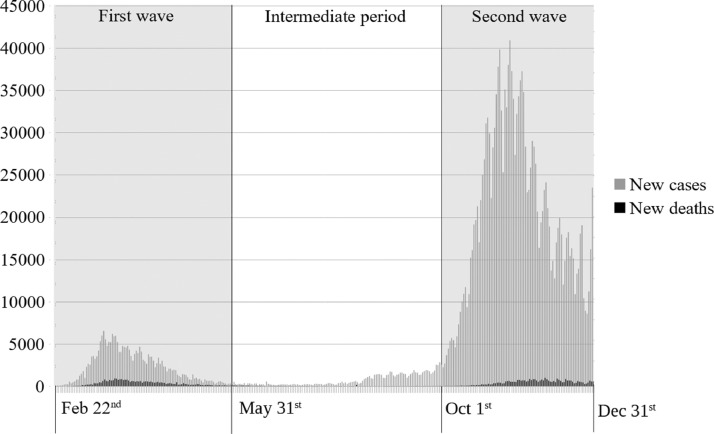
The starting date of the pandemic was based on the day on which the first SARS-CoV-2 positive mechanical thrombectomy was performed, i.e., February 22nd, 2020. Patients treated after this date (pandemic phase) were subsequently divided into 3 subgroups based on the day of the treatment (Fig. 1 ):
-
1.
First wave: the period between February 22nd and May 31st 2020, in which the first peak of incidence occurred.7 The lack of knowledge of the disease led to the adoption of extremely restrictive measures, which were nonetheless unsuccessful at reducing the burden on the healthcare system. This was the time during which healthcare was most vulnerable.
-
2.
Intermediate period: between May 31st and October 1st 2020. This time window between both waves was characterized by the lowest incidence of infections7 and, consequently, a partial recovery of the healthcare system.
-
3.
Second wave: from October 1st to December 31st 2020, the incidence of infections began to rise exponentially, with its peak around November 2020.7 Even though the number of infections far exceeded that of the first wave, the experience and knowledge gained made it possible to avoid the collapse of the healthcare system.
Fig. 1.
Incidences of new cases and new deaths by SARS-CoV-2 in Italy from February 22nd to December 31st. For the purpose of this study, the pandemic phase was divided in First wave, Intermediate period and Second wave. Adapted from the publicly available database by Our World in Data at: https://github.com/owid/covid-19-data/tree/master/public/data and https://www.ourworldindata.org.
Metrics and data
For each patient, the following time metrics were evaluated in minutes:
-
•
Onset-to-door: time interval between onset of symptoms and arrival at any ER (NCGH or other);
-
•
Door-to-CT: time interval between arrival at any ER (NCGH or other) and the first image of the CT scan (NCGH or other);
-
•
Agreement for sending – arrival in Neuroradiology: time interval between discussion with the neurologist in the ER (NCGH or other) and arrival at the NCGH neuroradiology department;
-
•
Arrival in Neuroradiology – groin: time interval between arrival at the NCGH neuroradiology department and femoral artery puncture;
-
•
Door-to-groin: time interval between arrival at the ER (NCGH or other) and femoral artery puncture;
-
•
Onset-to-groin: time interval from onset of symptoms to femoral artery puncture;
-
•
Groin-to-recanalization: time interval from femoral artery puncture to recanalization.
The following demographic, clinical and neuroimaging variables were also registered:
-
•
Age and gender;
-
•
Where the patient was first evaluated by a stroke professional (ER or elsewhere intra-hospital in NCGH, or in one of the SC);
-
•
SARS-CoV-2 infection (antigen test result or, in initial cases, based on chest CT findings);
-
•
National Institutes of Health Stroke Scale (NIHSS) score at presentation (initial) and at 24 h (dichotomized as high if > 6 and low if ≤ 6);
-
•
Alberta Stroke Programme Early CT Score (ASPECTS) at presentation (dichotomized as high if > 6 and low if ≤ 6);
-
•
Quality of collateral circulation (good, intermediate or poor, following Tan Scoring system8 grades 3, 2 and 1, respectively);
-
•
Presence of tandem occlusion;
-
•
Administration of intravenous fibrinolytic;
-
•
Modified treatment in cerebral ischemia (mTICI) score (dichotomized as good if ≥ 2b and bad if < 2b);
-
•
Deployment of intracranial or cervical stent.
Statistical analysis
For the statistical analysis, the 4.0.2 version of the R software (The R Foundation)9 was used. To check whether the continuous variables were normally distributed, a Shapiro-Wilk test was performed; considering that the distribution was never normal, the different groups were compared using the Wilcoxon test. Fisher's exact test was used for discrete variables. The time metrics registered, displayed as medians and interquartile range (IQR), were compared by repeating the statistical analysis among subgroups in three different ways:
-
1.Patients treated in 2020 vs patients treated in 2019; both globally and considering only patients from the ER of NCGH (ER-NCGH).
-
2.Patients treated in the period of the first wave of the pandemic vs patients treated in the same period of the year of 2019, considering all patients regardless of their origin, as well as specifically those from ER-NCGH and from SC.
-
3.Patients treated during the first wave of the pandemic vs patients treated during the second wave of the pandemic, in both cases considering only ER-NCGH patients.
-
1.
Results
A total of 594 patients were included: 348 from the pre-pandemic phase (301 from 2019 and 47 from 2020, before February 22nd) and 246 from the pandemic phase (76 during the first wave, 89 in the intermediate period and 81 during the second wave). Only 11 (1,8%) of the total sample were considered positive for SARS-CoV-2 infection at the time of the ischaemic event - 9 had a positive reverse-transcription polymerase chain reaction swab test, and in two of the earliest cases, the diagnosis was done by presumption based on thoracic CT findings. This was according to the best available evidence at the time and considering swab tests were not as available, nor as sensitive, back then.10 , 11
2019. vs 2020 (all patients)
Table 1.1 discriminates the demographic, clinical and neuroimaging variables and Table 1.2 shows the differences in time metrics.
Table 1.1.
Demographic, clinical and neuroimaging variables between the 2019 and the 2020 groups.
| Variables | 2019 (N=301) | 2020 (N=293) | P Value |
|---|---|---|---|
| Age (average ± SD) | 72 ± 15.5 | 70 ± 14.6 | .4 |
| Gender (% female) | 51.2% | 46.1% | .2 |
| First evaluation (%): Spoke Intra-hospital ER |
202 (67,1%) 9 90 |
132 8 153 (52,2%) |
<.01 |
| ASPECTS* (%): High (>6) Low (≤6) |
245 (95,3%) 12 (4,7%) |
225 (90%) 25 (10%) |
.02 |
| Collateral circulation: Good Intermediate Poor |
82 153 21 |
85 138 25 |
.5 |
| Initial NIHSS†: High (>6) Low (≤6) |
215 57 |
210 51 |
.74 |
| Change in NIHSS†: Improvement Stable Worsening |
110 18 21 |
91 19 19 |
.79 |
| Stent deployment(%) | 46 (15.3%) | 53 (18.1%) | .37 |
| Tandem occlusion (%) | 37 (12.4%) | 39 (13.5%) | .73 |
| mTICI‡: good–bad (%) | 260 (87,5%)-37 | 258 (89,6%)-30 | .5 |
| Intravenous fibrinolysis (%) | 111 (36.9%) | 90 (31%) | .14 |
ASPECTS: Alberta Stroke Programme Early CT Score
NIHSS: National Institutes of Health Stroke Scale
mTICI: modified treatment in cerebral ischemia.
Table 1.2.
Time variables between the 2019 and the 2020 groups (total patients).
| Variables (min)* | 2019 (N=301) | 2020 (N=293) | P Value |
|---|---|---|---|
| Onset-to-door | 67.5 (50–95.25) | 72 (53–113) | .06 |
| Door-to-CT | 32 (23.75–45) | 37.5 (28–54) | <.01 |
| Agreement - Arrival in NR† | 66 (48–88) | 64 (40–87) | .97 |
| Arrival in NR† - groin | 16 (13–23) | 20 (16–26) | <.01 |
| Door-to-groin | 159 (120.5–222.5) | 150 (121–203) | .78 |
| Onset-to-groin | 240 (193–295) | 240 (186.75–310) | .37 |
| Groin-to-recanalization | 43 (25–66) | 43 (27–68) | .26 |
minutes shown as medians (IQR)
NR: neuroradiology.
Of the 301 patients from 2019, 90 came directly from the ER-NCGH, 202 were redirected from SC and 9 were intra-hospital NCGH cases. Out of the total 293 cases from 2020 (pre-pandemic and pandemic phases), 153 came from the ER-NCGH, 132 from SC and 8 were intra-hospital. The total number of patients from each year did not differ significantly, but their distribution across the sites of first medical evaluation did (ER-NCGH: 29,9% vs 52%; SC: 67,1% vs 45%, p>0.01). The 2020 sample had more patients in the low ASPECTS score group (4,7% vs 10%, p<0,01).
The “Onset-to-door”, “Door-to-CT” and the “Arrival in NR – groin” times showed a tendency for increase in 2020, with a difference in medians of around 4 (67,5 vs 72 min, p=0.06), 5 (32 min vs 37,5 min, p>0.01) and 4 min (16 vs 20 min p<0.01), respectively.
2019. vs 2020 (ER-NCGH patients)
Table 2 compares the same time metrics between 2019 and 2020, but looking only at the ER-NCGH groups (N= 90 and N=153, respectively). Not only the “Door-to-CT” (34 vs 40, p<0,01) and the “Arrival in NR – groin” (15 vs 20, p<0.01), but also the “Door-to-groin” (115 vs 134. p<0,01) and “onset-to-groin” (194 vs 227. p<0,01) times were notably increased. The “Groin-to-recanalization” time also showed a tendency for increase (41 vs 48. p=0,08).
Table 2.
Time variables between the ER-NCGH groups of 2019 and 2020.
| Variables (min)* | 2019 (N=90) | 2020 (N=153) | P Value |
|---|---|---|---|
| Onset-to-door | 77 (50–119) | 83 (56.5–133.75) | .24 |
| Door-to-CT | 34 (26–45.5) | 40 (31–55) | <.1 |
| Agreement - Arrival in NR† | 42 (30–54) | 44 (30–65) | .27 |
| Arrival in NR† - groin | 15 (12–20) | 20 (16.5–25) | <.01 |
| Door-to-groin | 115 (94–142) | 134 (110.5–162) | <.01 |
| Onset-to-groin | 194 (159.25–232.5) | 227 (179–274) | <.01 |
| Groin-to-recanalization | 41 (25–61) | 48 (29–69.5) | .08 |
minutes shown as medians (IQR)
NR: neuroradiology.
Among the remaining variables, there was a tendency for the 2020 ER group to have a bigger proportion of patients with good collateral circulation (20% vs 33%, p=0,06).
First wave
Between February 22nd 2019 and May 31st 2019, a total of 78 patients with ischaemic stroke were submitted to endovascular treatment (52 from SC, 24 from ER-NCGH and 2 intra-hospital). In the same period in 2020 (“first wave”), the total number was 76 (18 from SC, 56 from the ER of NCGH and 2 intra-hospital). Three SARS-CoV-2 positive patients from the first wave did not have available beds in the intensive care unit after thrombectomy and suffered a bad outcome. Four patients that were initially accepted, did not undergo treatment due to late arrival or lack of staff or hospital beds.
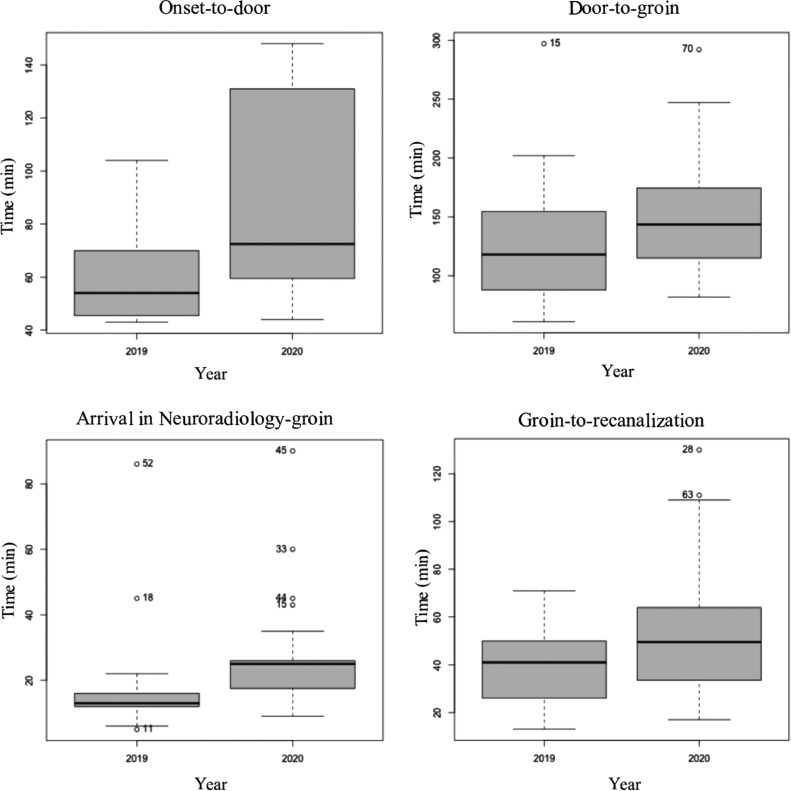
Comparisons between these subgroups are shown in Table 3 and Fig. 2 . Again, there was a remarkable difference in the percentage of patients coming directly to the ER of NCGH (30,8% vs 74%, p <0,01). There was also an increase in the “Onset-to-door” (50,5 vs 88,5, p<0,01), “Door-to-CT” (39 vs 47, p=0,06), “Arrival in Neuroradiology – groin” (13 vs 25, p<0,01), “Door-to-groin” (118 vs 143,5, p=0,02), “Onset-to-groin” (180 vs 244,5, p<0,01) and “Groin-to-recanalization” (41 vs 49,5, p=0,03) times during the first wave of the pandemic.
Table 3.
Time variables between the ER-NCGH groups of 2019 and 2020 during the first wave.
| Variables (min)* | 2019 (N=24) | 2020 (N=56) | P Value |
|---|---|---|---|
| Onset-to-door | 50.5 (45.75–64.25) | 88.5 (63–135.5) | <.01 |
| Door-to-CT | 39 (25–54.5) | 47 (35–58.5) | .06 |
| Agreement - Arrival in NR† | 37 (33–48) | 53 (35–66) | .8 |
| Arrival in NR† - groin | 13 (12–16) | 25(17.75–26) | <.01 |
| Door-to-groin | 118 (88–154.5) | 143.5 (115–173.75) | .02 |
| Onset-to-groin | 180 (138–200) | 244.5 (211–351.5) | <.01 |
| Groin-to-recanalization | 41 (26–50) | 49.5 (33.75–63) | .03 |
minutes shown as medians (IQR)
NR: neuroradiology.
Fig. 2.
Boxplot of the time variables between the ER-NCGH groups of 2019 and 2020 during each year's period of the first wave.
Analysis of the global and the SC samples during the periods of the first wave (not shown in table), revealed that the “Onset-to-door” time was also increased in the 2020 global sample (62 [48,78] vs 83 [61,134], p=0,01), but tended towards a decrease in the SC group (66 [55,89] vs 55 [27,79], p=0.2).
Patients from the first wave were younger than those from the same period in 2019 (70.5 vs 77, p=0,02), but there were no other notable differences between the groups.
First wave vs second wave (ER-NCGH)
Table 4 compares the time metrics between patients that came directly to the ER of NCGH during the first (N=56) and second (N=49) waves of the SARS-CoV-2 pandemic, in 2020. There was a global tendency for these to be reduced in the second wave, particularly the “Door-to-CT” (47,5 vs 37, p<0,01), “Arrival in Neuroradiology – groin” (25 vs 20, p=0,03) and “Onset-to-groin” (244,5 vs 227,5, p=0,02) times.
Table 4.
Time variables between the ER-NCGH groups during the first and second waves.
| Variables (min)* | First wave (N=56) | Second wave (N=49) | P Value |
|---|---|---|---|
| Onset-to-door | 88.5 (63–135.5) | 82 (60.75–106) | .13 |
| Door-to-CT | 47.5 (35–59.75) | 37 (28.5–49.5) | <.01 |
| Agreement - Arrival in NR† | 53 (35–66) | 40 (26.5–66) | .06 |
| Arrival in NR† - groin | 25 (17.5–26) | 20 (17–25) | .03 |
| Door-to-groin | 145 (115–176) | 135 (115.25–154.75) | .17 |
| Onset-to-groin | 244.5 (211–351.5) | 227.5 (176.75–270.5) | .02 |
| Groin-to-recanalization | 49.5 (33.75–63) | 44 (24.25–65.5) | .1 |
minutes shown as medians (IQR)
NR: neuroradiology.
Discussion
2019. vs 2020
The change in the proportion of patients coming from the ER-NCGH and from SC compromises the interpretation of the differences in the global samples between both years. It probably also explains why the only time metric that showed a slight tendency for decrease was the “Door-to-groin” variable (159 vs 150, p=0,78), since the “Door” time varies with origin and it will inevitably be lower in ER-NCGH patients. In order to avoid this confounding factor, we mainly focus the statistical analysis on the ER-NCGH subgroups, both in 2019 and in 2020.
Regarding the increase in the “Onset-to-door” during the first wave (50.5 min vs 88.5 min, p>0,01) the authors consider the following causes. Quarantine meant that patients would contact less with other people that could've otherwise detected the onset. On the other hand, the perception of the hospital as an unsafe place, with high probability of SARS-CoV-2 contagion, also caused patients to wait longer before resorting to medical assistance. Lastly, the time response of emergency care was naturally slowed down in part due to an extremely high demand, but also because of the implementation of safety measures, including the need to sanitize ambulances between each trip.
There was also a global increase in the time windows that took place after the patient got to a hospital. Likewise, the most likely explanation involves the inevitably time-consuming protocols put into motion to limit the spread of the virus. There was reallocation of resources and personnel to COVID-19 wards, and the now shorter staff had to wear personal protective equipment,13 further slowing down the handling of each patient. The creation of separate pathways for positive and negative patients might have further influenced the time of intra-hospital transport. There's also the added fact that professionals were not yet acquainted with these protocols. Considering the average time needed for the viral antigen test, stroke patients with pending results were treated as if they were positive, in order to reduce the risk of contagion.12
There is a consideration to be made about the difficult working conditions professionals were under during this time. Longer and more demanding shifts to cover for shortage of staff, and the immeasurable psychological impact of this experience, ultimately wore down professionals and surely affected their decision-making skills and the very efficacy of their work.
Our data show that during the first wave of the pandemic, there was an average increase of more than one hour in the time required to recanalize the occluded vessel since the onset of symptoms. According to the literature,14 this would mean a decrease of more than 10% in the probability of achieving functional independence at 3 months.
The tendency for the 2020 ER-NCGH patients to demonstrate better collateral circulation when compared to the sample from 2019, and for patients during the first wave to be younger, can reflect a selection bias. Whether purposely or not, the threshold for treatment during the pandemic was likely raised, and young age and good collaterals weigh in on this decision. It is also true that with delayed presentations, those that make it through selection will be more likely to have good collaterals. Lower ASPECTS scores in the global 2020 group can also be explained by the differences in time metrics, as with delayed presentations, the area of established infarct will be bigger and/or more noticeable. The number of cases with an ASPECTS considered too low for treatment, which empirically would also would have been higher in 2020, is not deductible from this study.
First wave vs second wave
The comparison between the first and second waves was also directed at solely the ER-NCGH groups. This was decided based on the fact that during the second wave a few other, but not all, SC had reopened, and this would once again make data heterogeneous.
Our results highlight how our response to stroke during the second wave was markedly better, despite a much higher incidence of SARS-CoV-2 cases.7 The time metrics were overall better, particularly the ones inside the NCGH. The authors believe a better understanding of the disease and the experience gained during the first wave allowed for a better plan of action. The resources and staff available were not as limited and the algorithm for handling SARS-CoV-2 positive patients (or of unknown status) was fine-tuned.
Pre-hospital management
When comparing the global samples of 2019 and 2020, only the increase in the “Door-to-CT” and “Arrival in Neuroradiology – groin” times reached statistical significance. In fact, there was a slight trend towards reduced time in the “Agreement – arrival in neuroradiology” and “Door-to-groin” variables, bearing in mind that times from other hospitals are included in these. Even though “Onset-to-door” times during the first wave are increased in the ER-NCGH analysis, the same did not happen in a subgroup analysis of the SC group, where this variable tended towards a paradoxical decrease.
The viral spread saturated the healthcare in NCGH and this may have resulted in a “bottleneck effect” for patients presenting to the ER-NCGH. As previously mentioned, ambulances were exhausted and even though faster travel times are expected during quarantine due to the lack of traffic, this difference is not as significant for ambulances, which already have a priority network to bypass it. On the other hand, patients that present to SC often use their own means of transportation, which were now free of traffic, possibly contributing to shorter “Onset-to-door” times. Lastly, these statistics do not include stroke mimics and cases that did not end up needing, or were not eligible for, thrombectomy, and in which coming to the ER-NCGH could've been avoided altogether, thus preventing further saturation of its services and risk of contagion.
Keeping a pre-hospital organization around a tertiary referral center capable of thrombectomy is essential for holding the quality of care in stroke to the highest standards.15 , 16 Recent meta-analysis have favoured the “Directly to mothership” model over the “Drip and ship” one,17 , 18 and a study done in another Italian hospital (Ospedale Maggiore, Bologna) during the SARS-CoV-2 pandemic also shared this view.19 However, in the specific setting of NCGH, the sudden shut down of SC and redirection of stroke patients directly to the ER-NCGH, already overwhelmed with the surge of the SARS-CoV-2 infection, may not have worked in its favour.
Limitations
Among the limitations of this study are its retrospective nature, a relatively small sample size, particularly in the subgroup analysis, and the fact that it was based on a single-center experience – conclusions may not necessarily be extrapolated for other hospitals. One could argue that NCGH would not benefit as much with a change in the pre-hospital organization, or that the results would've been different if a “Mothership” model was already in place. In the case of our fellow colleagues from Ospedale Maggiore, Bologna, the Mothership model had been established 2 years prior to the pandemic.19 Lastly, a small percentage of data was missing, namely CT scans performed in other hospitals, which could not be reviewed for the purpose of this study.
Conclusion
During the first wave of the SARS-CoV-2 pandemic, the time from symptom onset to recanalization was increased, on average, by more than one hour. A better management was done during the second wave, where times were improved relative to the first wave, despite a much higher incidence of SARS-CoV-2 cases. Possible factors include the implementation of time-consuming measures to limit viral spread, changes in pre-hospitalar organization and reallocation of resources and personnel away from stroke care.
Grant support
None.
Sources of funding
None.
Declaration of Competing Interest
None.
Acknowledgments
The authors would like to thank all professionals involved in the management of stroke patients in Niguarda Ca' Granda Hospital and the Spoke Centers that collaborate as part of the stroke network.
References
- 1.Gomez C.R. Editorial: time is brain! J Stroke Cerebrovasc Dis. 1993;3(1):1–2. doi: 10.1016/S1052-3057(10)80125-9. [DOI] [PubMed] [Google Scholar]
- 2.WHO, World Health Organization. WHO coronavirus disease (COVID-19) dashboard. [Online]. https://covid19.who.int/. (accessed on March 30th, 2021).
- 3.Maas M.B., Singhal A.B. Unwitnessed stroke: impact of different onset times on eligibility into stroke trials. J Stroke Cerebrovasc Dis. 2013;22:241–243. doi: 10.1016/j.jstrokecerebrovasdis.2011.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO, World Health Organization. Sharing COVID-19 experiences: the Italian response [Online]. https://www.euro.who.int/en/countries/italy/publications/video-sharing-covid-19-experiences-the-italian-response (accessed on March 30th, 2021).
- 5.Agosti E., et al. Coronavirus Disease 2019 (COVID-19) outbreak: single-center experience in neurosurgical and neuroradiologic emergency network tailoring. World Neurosurg. 2020;138:548–550. doi: 10.1016/j.wneu.2020.04.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zoia C., et al. Neurosurgery during the COVID-19 pandemic: update from Lombardy, northern Italy. Acta Neurochir. 2020;162:1221–1222. doi: 10.1007/s00701-020-04305-w. (Wien) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.A. Dambrosio. Italia - nuovi casi new. Flourish team [Online] https://public.flourish.studio/visualisation/3638338/?, accessed on March 30th, 2021.
- 8.Tan J.C., et al. Systematic comparison of perfusion-CT and CT-angiography in acute stroke patients. Ann Neurol. 2007;61(6):533–543. doi: 10.1002/ana.21130. Jun. [DOI] [PubMed] [Google Scholar]
- 9.R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2013. R: A Language and Environment for Statistical Computing. http://www.R-project.org/ [Google Scholar]
- 10.Ai T., et al. Correlation of Chest CT and RT-PCR Testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020;296(2):E32–E40. doi: 10.1148/radiol.2020200642. Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shi H., et al. CT screening for early diagnosis of SARS-CoV-2 infection – Author's reply. Lancet Infect Dis. 2020;20:1011. doi: 10.1016/S1473-3099(20)30247-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Qureshi A.I., et al. Management of acute ischemic stroke in patients with COVID-19 infection: Insights from an international panel. Am J Emerg Med. 2020;8:1548. doi: 10.1016/j.ajem.2020.05.018. e5-1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO, World Health Organization . COVID-19: Essential health services; 2020. Prevention, Identification and Management of Health Worker Infection in the Context of COVID-19. 30 Oct. [Google Scholar]
- 14.Saver J.L., et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA. 2016;316:1279–1288. doi: 10.1001/jama.2016.13647. [DOI] [PubMed] [Google Scholar]
- 15.Jasen O., et al. Standards of practice in interventional neuroradiology. Neuroradiology. 2017;59:541–544. doi: 10.1007/s00234-017-1837-8. [DOI] [PubMed] [Google Scholar]
- 16.Pierot L., et al. Standards of practice in acute ischemic stroke intervention: international recommendations. J Neurointerv Surg. 2018;10:1121–1126. doi: 10.1136/neurintsurg-2018-014287. [DOI] [PubMed] [Google Scholar]
- 17.Romoli M., et al. Mothership versus drip-and-ship model for mechanical thrombectomy in acute stroke: a systematic review and meta-analysis for clinical and radiological outcomes. J Stroke. 2020;22:317–323. doi: 10.5853/jos.2020.01767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ismail M., et al. Mothership versus drip and ship for thrombectomy in patients who had an acute stroke: a systematic review and meta-analysis. J Neurointerv Surg. 2019;11:14–19. doi: 10.1136/neurintsurg-2018-014249. [DOI] [PubMed] [Google Scholar]
- 19.Zini A., et al. The stroke mothership model survived during COVID-19 era: an observational single-center study in Emilia-Romagna, Italy. Neurol Sci. 2020;41:3395–3399. doi: 10.1007/s10072-020-04754-2. [DOI] [PMC free article] [PubMed] [Google Scholar]