Abstract
Background
Noninvasive respiratory support (NIRS) has been diffusely employed outside the intensive care unit (ICU) to face the high request of ventilatory support due to the massive influx of patients with acute respiratory failure (ARF) caused by coronavirus-19 disease (COVID-19). We sought to summarize the evidence on clinically relevant outcomes in COVID-19 patients supported by NIV outside the ICU.
Methods
We searched PUBMED®, EMBASE®, and the Cochrane Controlled Clinical trials register, along with medRxiv and bioRxiv repositories for pre-prints, for observational studies and randomized controlled trials, from inception to the end of February 2021. Two authors independently selected the investigations according to the following criteria: (1) observational study or randomized clinical trials enrolling ≥ 50 hospitalized patients undergoing NIRS outside the ICU, (2) laboratory-confirmed COVID-19, and (3) at least the intra-hospital mortality reported. Preferred Reporting Items for Systematic reviews and Meta-analysis guidelines were followed. Data extraction was independently performed by two authors to assess: investigation features, demographics and clinical characteristics, treatments employed, NIRS regulations, and clinical outcomes. Methodological index for nonrandomized studies tool was applied to determine the quality of the enrolled studies. The primary outcome was to assess the overall intra-hospital mortality of patients under NIRS outside the ICU. The secondary outcomes included the proportions intra-hospital mortalities of patients who underwent invasive mechanical ventilation following NIRS failure and of those with ‘do-not-intubate’ (DNI) orders.
Results
Seventeen investigations (14 peer-reviewed and 3 pre-prints) were included with a low risk of bias and a high heterogeneity, for a total of 3377 patients. The overall intra-hospital mortality of patients receiving NIRS outside the ICU was 36% [30–41%]. 26% [21–30%] of the patients failed NIRS and required intubation, with an intra-hospital mortality rising to 45% [36–54%]. 23% [15–32%] of the patients received DNI orders with an intra-hospital mortality of 72% [65–78%]. Oxygenation on admission was the main source of between-study heterogeneity.
Conclusions
During COVID-19 outbreak, delivering NIRS outside the ICU revealed as a feasible strategy to cope with the massive demand of ventilatory assistance.
Registration
PROSPERO, https://www.crd.york.ac.uk/prospero/, CRD42020224788, December 11, 2020.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13054-021-03697-0.
Keywords: Noninvasive ventilation, COVID-19, Intra-hospital mortality
Background
The rapid and massive spread of severe acute respiratory syndrome related to novel coronavirus (SARS-CoV-2) outbreak has put in crisis the healthcare systems of whole nations. Worldwide, the surge capacities of the hospitals have been severely stressed by the massive influx of patients admitted for acute respiratory failure (ARF) caused by coronavirus-19 disease (COVID-19) [1–3]. Among COVID-19 patients suffering from hypoxemic ARF, the rate of intubation has been reported ranging from 12 to 33% [3–5]. To face this exceptional demand of intensive care unit (ICU) resources, hospitals have increased ICU bays [6] and adapted many general wards into intermediate care units, with the aim of providing respiratory support and clinical monitoring to those hypoxemic ARF patients in whom the sole conventional oxygen supplement is ineffective [7].
Moreover, at the very beginning of the pandemic, the rate of patients receiving noninvasive respiratory support (NIRS) upon ICU admission was reported to range from 11 [8] (in Italy) to 56% (in China) [9]. At the same time, several studies demonstrated that NIRS outside the ICU was feasible and effective in preventing invasive mechanical ventilation (IMV) [10, 11]. However, a major concern while treating hypoxemic ARF patients by NIRS is related to the failure rate of NIRS, which could occur even in 50% of the cases with consequent recourse to IMV [12]. Also, excessive prolongation of NIRS may worsen lung injury because of patient self-inflicted lung injury occurrence [13] or delay IMV [14, 15].
The aim of this systematic review and meta-analysis was to estimate the overall intra-hospital mortality of COVID-19 patients assisted through NIRS outside the ICU and quantify the proportion of patients who failed NIRS and were subsequently intubated and treated in the ICU. Also, the estimate of patients who received NIRS as a ceiling ventilatory therapy and the related intra-hospital mortality were investigated.
Methods
Our systematic review and meta-analysis was realized following the Preferred Reporting Items for Systematic reviews and Meta-analysis (PRISMA) guidelines [16] and was registered on PROSPERO (CRD42020224788).
PICO question
We sought information about the application of NIRS—i.e., continuous positive airway pressure (CPAP) or noninvasive bi-level ventilation—outside the ICU (I) in adult patients admitted for hypoxemic ARF COVID-19 related (P) with or without comparator (C) and aimed to ascertain the intra-hospital mortality (O). For overall intra-hospital mortality we intended the punctual intra-hospital mortality reported by each enrolled study at database closure.
Search methods and study selection
We searched PUBMED®, EMBASE®, and the Cochrane Controlled Clinical trials register from inception to February 2021 for observational studies and randomized controlled trials without language restrictions. The search was performed using the following terms, combined according to database syntax (see Additional file 1 for search strategy): ‘COVID-19,’ ‘novel coronavirus 2019,’ ‘SARS-CoV-2,’ ‘severe acute respiratory syndrome coronavirus related,’ ‘SARS-CoV-19,’ ‘positive pressure respiration,’ ‘NIV,’ ‘noninvasive ventilation,’ ‘CPAP,’ ‘continuous positive airway pressure,’ ‘noninvasive positive pressure respiration,’ ‘NIPPV,’ ‘NRS,’ and ‘noninvasive respiratory support.’ For NIRS outside the ICU, we meant all the modalities of noninvasive bi-level and CPAP, regardless of the interface used, adopted to assist COVID-19 patients with hypoxemic ARF, with the exceptions of the high-flow nasal cannula.
We also reviewed the references of selected papers, review articles, commentaries, and editorials on this topic to identify other studies of interest missed during the primary search. Moreover, we surveyed medRxiv and bioRxiv, free online repositories for preprints in health science, from inception to end of February 2021, searching for clinical and preclinical investigations about NIRS application in COVID-19 patients outside the ICU.
Two authors (GC and TE) independently evaluated titles and abstracts obtained from the search to select investigations responding to the following inclusion requests: (1) observational study or randomized clinical trials enrolling ≥ 50 symptomatic hospitalized patients undergoing NIRS outside the ICU, (2) laboratory-confirmed COVID-19 defined by a positive result on a reverse-transcriptase-polymerase chain reaction assay of a nasopharyngeal and oropharyngeal swab or a sputum specimen, and (3) at least the primary outcome reported by the study. Case reports and case series with less than 50 patients were excluded, as they may observe no events due to the small size [17]. When multiple publications of the same research group/center described potentially overlapping cohorts, the authors selected the most recent publications. The same authors independently screened the full texts, and any disagreement was resolved through discussion or involving a third review author (EDR). When necessary, the corresponding authors of the included studies were contacted to obtain missing data related to study demographics, methods, outcomes, and clinical characteristics of patients analyzed.
Data extraction and study quality
Data extraction was independently performed by two authors (GC and TE) who screened and selected the included studies extracted. Any disagreement was resolved by discussion or involving a third review author (EDR). Extracted data included: investigation features (e.g., study design, setting), demographic characteristics (e.g., age, sex, body mass index), presence of comorbidities (with special attention to hypertension, diabetes, kidney disease, respiratory disease, and cardiac disease), characteristics at hospital admission (e.g., oxygenation, respiratory rate, laboratory tests), treatments, NIRS regulations, and clinical outcomes.
The methodological quality of selected articles was assessed by an index that classifies nonrandomized studies as adequate, inadequate, or unclear [18].
Statistical analysis
The analysis was carried out on the data extracted from peer-reviewed manuscripts in combination with data obtained from pre-print investigations.
The descriptive analysis was conducted for all the selected variables considered in the included studies. Continuous or noncontinuous variables were reported as appropriate. Proportions with 95% confidence intervals (CI) and model fitting weights were computed using the DerSimonian-Laird method with a random-effects model, based on the expected heterogeneity. Heterogeneity across the studies was assessed through Q and I2 tests both, which were considered significant when the p-value was < 0.05 and I2 > 75% [19], and graphical evaluation of forest plots.
A general linear (mixed-effects) meta-regression model was performed by using the outcome as the dependent variable and the study size as the independent variable. Meta-regression was conducted to assess, in patients admitted for COVID-19 undergoing NIRS, the impact of age, gender, arterial oxygen tension to inspired oxygen fraction ratio (PaO2/FiO2) acquired on hospital admission, number of intubations, and number of ‘do-not-intubate’ (DNI) orders patients on the clinical outcomes investigated. Again, the observations were weighted by the inverse variance of the estimate to allow for possible heteroscedasticity.
Statistical analyses were conducted using R3.5.2 software (The R foundation).
Results
As depicted in Additional file 2, a total of 1956 records were identified from the search, including 1045 peer-reviewed studies and 911 pre-prints studies. After duplicates exclusion and full-text evaluation, 17 eligible studies were identified (14 peer-reviewed and 3 pre-prints) for a total of 18,204 patients with a suspected COVID-19-related infection at hospital admission of whom 3377 received NIRS outside ICU [10, 11, 20–34].
Characteristics of the included studies
The main characteristics of the included studies are reported in Additional file 3-Table 1. Except for one study conducted in Russia and two investigations performed in the UK, the leading part of the studies was conducted in Italy (82.4%) during the first wave of COVID-19 pandemic, from the end of February to the end of May 2020. Among the 17 enrolled investigations, 11 (64.7%) were single-center studies, whereas 6 (35.3%) were multicenter studies: of these, 2 investigations (33.3%) were prospectively conducted, while 4 were retrospectively carried out. The overall risk of bias was low for the studies included. The methodological quality of the included investigations assessed through methodological index for nonrandomized studies (MINORS) tool is reported in Additional file 3-Table 2 and Additional file 4.
Patient characteristics
The demographic characteristics are described in Additional file 3-Table 3. A total of 3377 patients were under NIRS outside the ICU. Of these, 2696 (79.8%) were males with an average age ranging from 60 to 75 years and an average body mass index ranging from 27 to 31.9 kg/cm2 (2413/3377 patients). The mean Charlson comorbidity index varied from a minimum of 1 to a maximum of 4 (1037/3377 patients). Among comorbidities, hypertension was reported in a higher number of studies compared to other comorbidities. Patients’ clinical characteristics on hospital admission are presented in Additional file 3-Table 4. PaO2/FiO2 at hospital admission was the most reported clinical variable in the included studies. Additional file 3-Table 5 describes the pharmacological therapies administered and the application of awake-prone position. The rate of hydroxychloroquine administration was the most reported pharmacological therapy among the included investigations. Eight studies reported the application of awake-prone position during NIRS. NIRS settings are described in Additional file 3-Table 6. When reported, CPAP was applied in 2764/3047 of the patients and helmet interface was used in 1855/2690 of the cases. Positive end-expiratory pressure varied from a mean value of 7 to 15 cm H2O (2870/3377 patients) and FiO2 ranged from a mean value of 50 to 68% (2467/3377 patients), respectively.
Clinical outcomes
Figure 1 depicts the overall intra-hospital mortality in patients noninvasively ventilated outside the ICU. Overall intra-hospital mortality rate was 36% [30–41%] in COVID-19 patients who received NIRS outside the ICU, with a high between-study heterogeneity (p < 0.0001, I2 = 90.4%).
Fig. 1.
Pooled overall intra-hospital mortality of patients assisted through noninvasive respiratory support outside the intensive care unit. The vertical dotted line refers to the summary estimate for overall intra-hospital mortality of patients assisted through noninvasive respiratory support outside intensive care unit. Red squares indicate the individual study estimates of the overall intra-hospital mortality of patients assisted through noninvasive respiratory support outside the intensive care unit, whereas the black horizontal lines indicate the 95% confidence interval of single studies. The diamond refers to the summary estimate with 95% confidence interval
As depicted in Fig. 2, when patients subjected to DNI orders were excluded from the global population of patients assisted by NIRS outside the ICU, the pooled intra-hospital mortality was 19% [15–24%] with a high between-study heterogeneity (p < 0.01, I2 = 83%).
Fig. 2.
Pooled intra-hospital mortality of patients assisted through noninvasive respiratory support outside the intensive care unit, net of the patients subjected to limitations of care. The vertical dotted line refers to the summary estimate for intra-hospital mortality of patients assisted through noninvasive respiratory support outside intensive care unit, excluding the patients subjected to limitations of care. Red squares indicate the individual study estimates of the overall intra-hospital mortality of patients assisted through noninvasive respiratory support outside the intensive care unit, excluding the patients subjected to limitations of care, whereas the black horizontal lines indicate the 95% confidence interval of single studies. The diamond refers to the summary estimate with 95% confidence interval
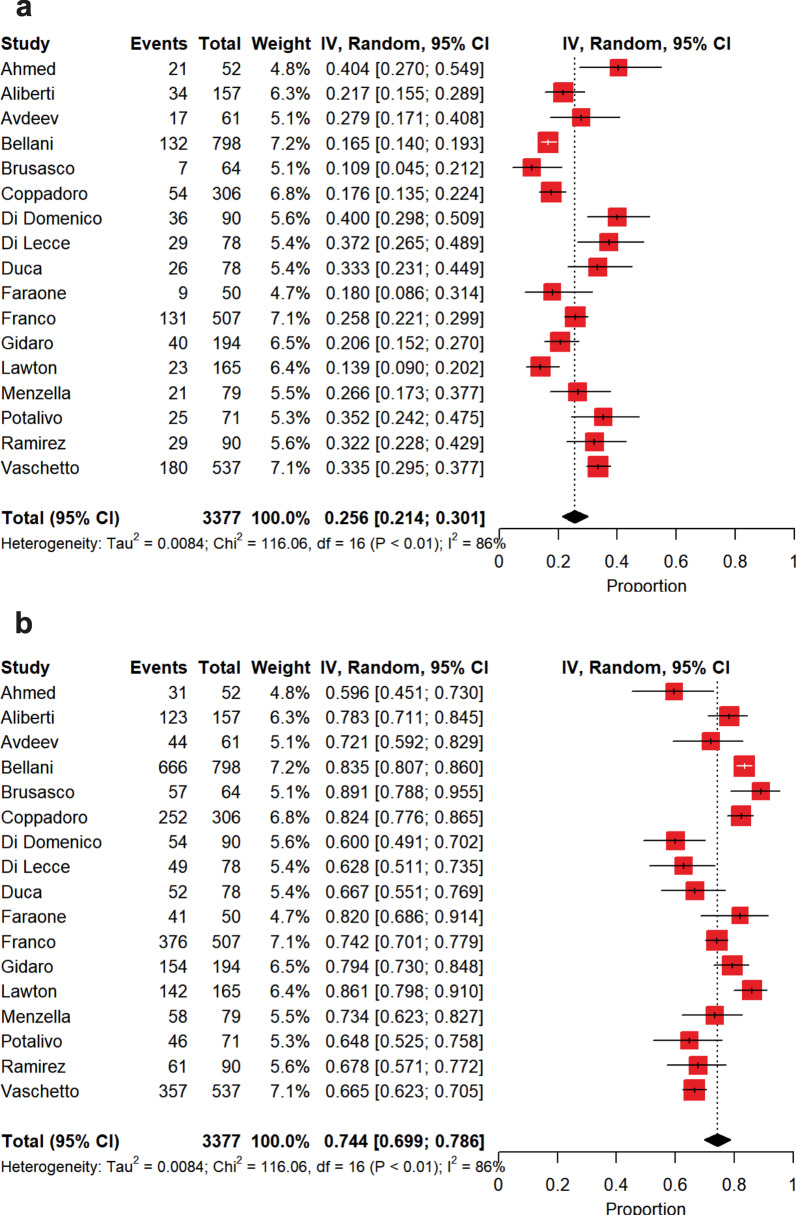
The estimate of intubation rate is shown in Fig. 3a. Pooled intubation estimate was 26% [21–30%], with a high between-study heterogeneity (p < 0.0001, I2 = 86.2%). In this case, the source of heterogeneity was only ascribed to PaO2/FiO2 on admission (p < 0.0001, I2 = 73.4%). The causes of IMV onset and the intubation criteria are described in Additional file 3-Tables 7 and 8. Among the included studies, 8 investigations attributed refractory hypoxemia to the cause of intubation.
Fig. 3.
Summary estimates of intubated patients following noninvasive respiratory support failure and of those patients who continued noninvasive respiratory support and did not experience intubation. a Summary estimate of intubated patients following noninvasive respiratory support failure. The vertical dotted line refers to the summary estimate of intubation in patients who failed noninvasive respiratory support. Red squares indicate the individual study estimates of the intubated patients following noninvasive respiratory support failure, whereas the black horizontal lines indicate the 95% confidence interval of single studies. The diamond refers to the summary estimate with 95% confidence interval. b Summary estimate of patients with noninvasive respiratory support who did not experience intubation. The vertical dotted line refers to the summary estimate of patients who continued noninvasive respiratory support and were not intubated. Red squares indicate the individual study estimates of patients who continued noninvasive respiratory support and were not intubated, whereas the black horizontal lines indicate the 95% confidence interval of single studies. The diamond refers to the summary estimate with 95% confidence interval
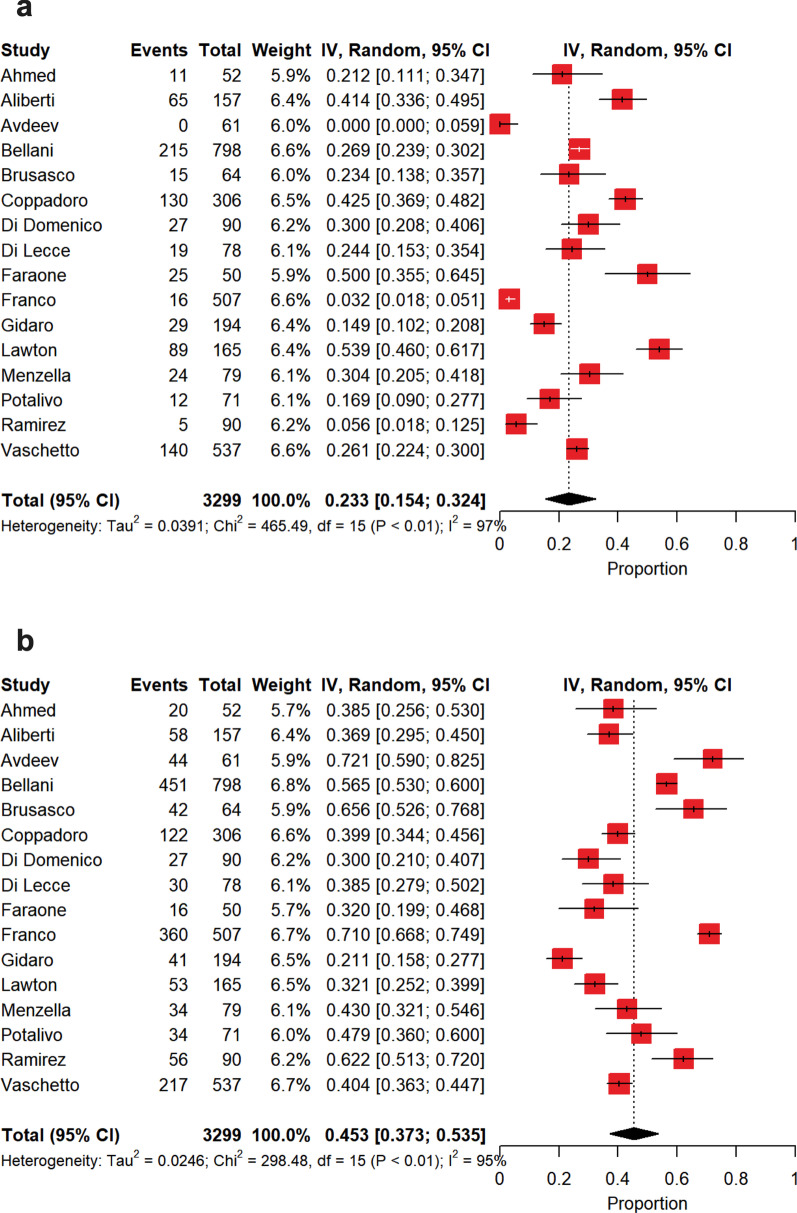
The summary estimate of nonintubated patients is depicted in Fig. 3b. Patients were not intubated in 74% [70–79%] of the cases, with a high between-study heterogeneity (p < 0.0001, I2 = 86.2%). Also in this case, this heterogeneity was only due to PaO2/FiO2 on admission (p < 0.0001, I2 = 73.4%). Among patients who did not experience intubation, a DNI order was expressed in a summary estimate of 23% [15–32%] of the cases (Fig. 4a), whereas patients were deemed as deserving ‘full treatment’ in 45% [37–54%] of the cases (Fig. 4b), with a high heterogeneity for both (DNI, p < 0.0001, I2 = 96.8%; ‘full treatment’, p < 0.0001, I2 = 95.0%). As depicted in Fig. 5a, in patients who failed NIV and were subsequently intubated, intra-hospital mortality reached 45% [36–54%], while in those subjects under NIRS who did not experience IMV intra-hospital mortality was of 30% [23–37%] (Fig. 5b), with high between-study heterogeneities in both the cases (intubation, p < 0.0001, I2 = 82.0%; nonintubation, p < 0.0001, I2 = 92.0%). In the subset of NIRS patients with DNI orders (Fig. 6a), intra-hospital mortality was of 72% [65–78%], with a moderate between-study heterogeneity (p < 0.0004, I2 = 65.0%), while in those under NIRS deserving ‘full treatment’ (Fig. 6b) intra-hospital mortality reached 2.6% [0.3–6.3%], with a high between-study heterogeneity (p < 0.0001, I2 = 85.7%).
Fig. 4.
Summary estimates of patients with limitations of care and of those under ‘full treatment’ who were not intubated. a Summary estimate of nonintubated patients with limitations of care. The vertical dotted line refers to the summary estimate of patients with limitations of care. Red squares indicate the individual study estimates of the patients with limitations of care, whereas the black horizontal lines indicate the 95% confidence interval of single studies. The diamond refers to the summary estimate with 95% confidence interval. b Summary estimate of patients under ‘full treatment’ who were not intubated. The vertical dotted line refers to the summary estimate of patients under ‘full treatment’ who were not intubated. Red squares indicate the individual study estimates of patients under ‘full treatment’ who were not intubated, whereas the black horizontal lines indicate the 95% confidence interval of single studies. The diamond refers to the summary estimate with 95% confidence interval
Fig. 5.
Summary estimates of intra-hospital mortality observed in intubated patients following noninvasive respiratory support failure and of that reported in patients who continued noninvasive respiratory support and did not experience intubation. a Summary estimate of intra-hospital mortality observed in intubated patients following noninvasive respiratory support failure. The vertical dotted line refers to the summary estimate of intra-hospital mortality observed in intubated patients who failed noninvasive respiratory support. Red squares indicate the individual study estimates of intra-hospital mortality observed in intubated patients following noninvasive respiratory support failure, whereas the black horizontal lines indicate the 95% confidence interval of single studies. The diamond refers to the summary estimate with 95% confidence interval. b Summary estimate of intra-hospital mortality of patients with noninvasive respiratory support who did not experience intubation. The vertical dotted line refers to the summary estimate of intra-hospital mortality of patients with noninvasive ventilation who did not experience intubation. Red squares indicate the individual study estimates of intra-hospital mortality of patients with noninvasive respiratory support who did not experience intubation, whereas the black horizontal lines indicate the 95% confidence interval of single studies. The diamond refers to the summary estimate with 95% confidence interval
Fig. 6.
Summary estimates of intra-hospital mortality observed in patients with limitations of care and of that reported in patients under ‘full treatment’ who were not intubated. a Summary estimate of intra-hospital mortality observed in patients with limitations of care. The vertical dotted line refers to the summary estimate of intra-hospital mortality observed in patients with limitations of care. Red squares indicate the individual study estimates of intra-hospital mortality observed in patients with limitations of care, whereas the black horizontal lines indicate the 95% confidence interval of single studies. The diamond refers to the summary estimate with 95% confidence interval. b Summary estimate of intra-hospital mortality observed in patients under ‘full treatment’ who were not intubated. The vertical dotted line refers to summary estimate of intra-hospital mortality observed in patients under ‘full treatment’ who were not intubated. Red squares indicate individual study estimates of intra-hospital mortality observed in patients under ‘full treatment’ who were not intubated, whereas the black horizontal lines indicate the 95% confidence interval of single studies. The diamond refers to the summary estimate with 95% confidence interval
In Additional file 3-Table 9, hospital length of stay, NIRS and IMV duration, along with time lag between NIRS and IMV onset were reported. Interestingly, NIRS-to-IMV time lag varied from a mean value of 72 h to a mean value of 137 h (1524/3377 patients).
Discussion
In the present systematic review and meta-analysis patients admitted for COVID-19 and requiring NIRS outside the ICU were characterized by an overall intra-hospital mortality of 36%.
During COVID-19 outbreak, NIRS was demonstrated to be feasible both in- and outside ICU, in a percentage of patients ranging between 11 and 62% [3, 8, 9, 35, 36]. Despite the lack of a strong recommendation in pandemic viral illness [15], several observational studies suggest that the application of NIRS was clinically useful in stabilizing the clinical course of patients with mild-to-moderate ARF COVID-19 related [3, 9]. However, due to a potential imbalance between the exceptional demand for ventilatory assistance during COVID-19 pandemic and hospital surge capacity, one might suppose that NIRS practiced outside ICU would be characterized by an increase in intra-hospital mortality compared to NIRS applied in the ICU for COVID-19 patients with ARF. Indeed, data from our 3377 patients showed that (1) NIRS outside the ICU was feasible in the COVID-19 pandemic scenario and (2) in our global patients’ population receiving NIRS outside the ICU, the pooled intra-hospital mortality of 19%, net of patients subjected to DNI orders, was quite similar to intra-hospital mortality observed in the helmet NIRS group from a recent randomized-controlled trial, conducted in COVID-19 patients admitted to ICU [38].
In our population pooled intubation rate was of 26%. This finding kept with IMV onset reported in severe acute respiratory syndrome [39], but was lower than that described for H1N1 pneumonia [40], and middle eastern respiratory syndrome outbreak [41]. In our context, the most reported cause of intubation was refractory hypoxemia, when the reasons for IMV commencement were described, with an average NIRS-to-IMV time lag varying from a minimum of 55 h to a maximum of 137 h, respectively, when reported. Once intubated, in this subset of patients who experienced NIRS failure, we observed a pooled intra-hospital mortality of 45%, consistent with that observed in intubated ARDS patients who failed NIRS [37]. In interpreting our data, it is worth to consider that an undue prolongation of NIRS with a consequent delayed intubation probably played a key role in the lung injury progression, as described by patient self-induced lung injury theory [42].
The rate of DNI order application has increased over time in the last two decades, reaching 32% in patients admitted for ARF undergoing NIRS or high flow oxygen therapy [43], in nonpandemic context. In this subset of patients, a pooled survival of 56% at hospital discharge has been reported regardless of whether patients were managed in the ICU or hospital ward [44]. However, the DNI order decision-making process is particularly tricky because it is affected by demographic and clinical factors, i.e., age and illness severity, along with patient/family involvement [43]. According to our findings, in the COVID-19 pandemic context, the summary estimate of the patients, in whom a DNI decision was pursued, was 23% with a pooled intra-hospital mortality of 72%. It is worth to point out that our data were obtained during the first wave of COVID-19 outbreak, with the well-described concerns of hospital and ICU surge capacity [7, 45].
Among the variables investigated, PaO2/FiO2 on admission was the main factor sustaining the between-study heterogeneities of the investigated outcomes. These data suggest that, in our context, there was most likely a great variability in the modalities of proceeding toward intubation or continuing NIRS. In this regard, other factors, such as the availability of resources and the strategy of their allocation, might have adversely influenced the process of care [7, 45].
As a clinical implication, our findings, in agreement with previous suggestions [47], support the use of NIV for hypoxemic ARF due to COVID-19 also outside ICU, in the intermediate care unit setting.
The present investigation has several limitations requiring to be discussed. The enrolled studies were mainly retrospective investigations conducted during the first wave of COVID-19 pandemic from the end of February to the end of May 2020. Accordingly, it is worth to take into account the critical issues of the specific historical moment, characterized by the crisis of the hospital surge capacity response and the lack of a well-defined therapeutic approach. We could not provide insights on the modalities of NIRS application, conduction, and monitoring in the different settings explored because of the paucity of data retrieved. The leading part of the included studies was carried out in Italy. Thus, our conclusions cannot be generalized to other countries with different policies, practices, medical ethics, social attitudes, cultures, and religions [48–51]. We could not draw any conclusions about the efficacy of NIRS in curbing the overall intra-hospital mortality in the light of our data. Indeed, the present analysis was conducted on data retrieved exclusively from retrospective and prospective, nonrandomized investigations, accounting for indication bias and confounding. We included 3 pre-print investigations [32–34] in our analysis because of the relatively small number of studies enrolled at the time of search closure (end of February 21). This latter aspect along with the high between-study heterogeneity, the lack of a specific time point of intra-hospital mortality observation, and, in some cases, the poor data reporting could limit the possibility to draw definitive conclusions from our data.
Conclusions
This systematic review and meta-analysis summarized the evidence reported from the first wave of COVID-19 outbreak on the incidence of overall intra-hospital mortality in hospitalized patients undergoing NIRS outside the ICU. Despite the concerns arising from the crisis of hospital surge capacity response and the lack of a clinically effective therapy, delivering NIRS outside the ICU revealed overall as a feasible strategy to cope with the massive demand of ventilatory assistance even for those patients with care limitations. Our findings require to be confirmed in future investigations addressing the same topic over the following waves of COVID-19 outbreak.
Supplementary Information
Additional file 1. Search strategy of electronic database.
Additional file 2. Enrollment flow diagram.
Additional file 3. Characteristics of the enrolled investigations, overall clinical characteristics of the populations investigated in the enrolled studies, and list of studies excluded after reading the full text.
Additional file 4. Methodological quality of the included investigations.
Acknowledgements
We thank the collaborators:
Francesca Facondini1, MD; Maddalena Bitondo1, MD; Mara Paneroni2, MSc; Francesco Corradi3,4, MD, PhD; Chiara Cogliati5, MD; Matteo Fontana6, MD; Nicola Facciolongo6, MD; Andrea Duca7, MD; Dario Winterton8, MD; Jonathan Montomoli1, MD; Elisiana Carpagnano, MD9; Annalisa Benini8, MD; Robert Fruscio8,10, MD; Luisa Verga8, MD, Paolo Mazzola8,10, MD; Marco Carbone8,10 MD, Giacomo Mulinacci8,10 MD, Alessandro Soria8 MD, Beatrice Noè8,10, MD; Eduardo Beck11, MD; Riccardo Di Sciacca8, MD; Davide Ippolito8, MD; Giuseppe Bellelli 8,10, MD; Giuseppe Citerio8,10, MD; Maria Grazia Valsecchi10, MD; Andrea Biondi8,10, MD; Alberto Pesci8,10, MD; Paolo Bonfanti8,10, MD, Davide Gaudesi10, PhD; Laura Antolini10, PhD; Massimo Borelli12, MD; Federica De Giacomi13, MD; Giancarlo Bosio13, MD; Nicola Latronico14,15, MD; Matteo Filippini15, MD; Marco Gemma16, MD; Federico Cioffi17, MD; Claudia Giannotti17, MD; Benvenuto Antonini18, MD; Nicola Petrucci19, MD; Simone Maria Zerbi20, MD; Paolo Maniglia21, MD; Gian Paolo Castelli22, MD; Giovanni Marino23, MD; Matteo Subert24, MD; Danilo Radrizzani25, MD; Teresa S. Mediani26, MD; Ferdinando Luca Lorini27, MD; Filippo Maria Russo27, MD; Angela Faletti28, MD; Andrea Beindorf29, MD; Remo Daniel Covello30, MD; Stefano Greco31, MD; Marta M. Bizzarri32, MD; Giuseppe Ristagno33, MD; Francesco Mojoli34, MD; Andrea Pradella35, MD; Paolo Severgnini36, MD; Marta Da Macallè36, MD; Andrea Albertin37, MD; Tommaso Tonetti38, MD; Emanuele Rezoagli10,39,40, MD, PhD; Giovanni Vitale39, MD; Aurora Magliocca10, 39, MD; Gianluca Cappelleri41, MD; Mattia Docci10, 42, MD; Filippo Serra10, MD; Emanuela Rossi10, MD; Francesco Blasi43,44, MD; Pierachille Santus45, MD; Valer Monzani46, MD; Antonio Messina47, MD, PhD.
Affiliations:
1Department of Anesthesia and Intensive Care, Infermi Hospital, AUSL della Romagna, Rimini, Italy
2Respiratory Rehabilitation Unit Lumezzane, ICS Maugeri IRCCS, Brescia, Italy.
3Anesthesia and Intensive Care Unit, E.O. Ospedali Galliera, Genoa, Italy
4Department of Surgical, Medical, Molecular Pathology and Critical Care Medicine, University of Pisa, Pisa, Italy
5Department of Biomedical and Clinical Sciences Luigi Sacco, University of Milan, Ospedale Luigi Sacco, Milan, Italy
6Pneumology Unit, Arcispedale Santa Maria Nuova, Azienda USL-IRCCS di Reggio Emilia, Reggio Emilia, Italy
7Emergency Department, ASST Papa Giovanni XXIII, Bergamo, Italy
8ASST Monza, San Gerardo Hospital, Monza, Italy
9Cardiothoracic Department, Respiratory Unit, University Hospital, Bari, Italy
10Department of Medicine and Surgery, University of Milan-Bicocca, Monza
11ASST Monza, Desio Hospital, Desio, Italy
12Department of Anesthesia and Intensive Care Medicine, Treviglio—Caravaggio Hospital, ASST Bergamo Ovest, Treviglio, Italy
13Division of Pulmonary Medicine, Cremona Hospital, ASST Cremona, Cremona, Italy
14Department of Anesthesiology, Intensive Care and Emergency, Spedali Civili University Hospital, ASST Spedali Civili, Brescia, Italy
15Department of Surgical Specialties, Radiological Sciences and Public Health, University of Brescia, Brescia, Italy
16Department of Anesthesia and Intensive Care Unit, Fatebenefratelli Hospital, ASST Fatebenefratelli Sacco, Milan, Italy
17Department of Anesthesiology and Intensive Care, Luigi Sacco Hospital, ASST Fatebenefratelli Sacco, Polo Universitario, University of Milan, Milan, Italy
18Department of Anesthesiology and Intensive Care Medicine, Manerbio Hospital, ASST Garda, Brescia, Italy
19Department of Anesthesia and Intensive Care Unit, Desenzano Hospital, ASST Garda, Desenzano, Brescia, Italy
20Anesthesia and Intensive Care Unit 2, Sant’Anna Hospital, ASST Lariana, San Fermo della Battaglia, Como, Italy
21Department of Anesthesia and Intensive Care Medicine, Alessandro Manzoni Hospital, ASST Lecco, Lecco, Italy
22Department of Anesthesia and Intensive Care Medicine, Carlo Poma Hospital, ASST Mantova, Mantova, Italy
23Department of Anesthesia and Intensive Care Medicine, Vizzolo Predabissi Hospital, ASST Melegnano e della Martesana, Melegnano, Milan, Italy
24Department of Anesthesia and Intensive Care Medicine, Melzo—Gorgonzola Hospital, ASST Melegnano e della Martesana, Milano, Italy
25Department of Anesthesia and Intensive Care Medicine, Legnano Hospital, ASST Ovest milanese, Legnano, Milano, Italy
26Department of Anesthesia and Intensive Care Medicine, Vigevano Hospital, ASST Pavia, Vigevano, Pavia, Italy
27Department of Anesthesia and Intensive Care, ASST Papa Giovanni XXIII, Bergamo, Italy
28Department of Anesthesia and Intensive Care Medicine, Gardone Val Trompia Hospital, ASST Spedali Civili, Brescia, Italy
29Department of Anesthesia and Intensive Care Medicine, Montichiari Hospital, ASST Spedali Civili, Brescia, Italy
30Department of Anesthesia and Intensive Care Medicine, Busto Arsizio Hospital, ASST Valle Olona, Varese, Italy
31Department of Anesthesia and Intensive Care Medicine, Saronno Hospital, ASST Valle Olona, Varese, Italy
32Department of Anesthesia and Intensive Care Medicine, Vimercate Hospital, ASST Vimercate, Monza e Brianza, Italy
33Department of Anesthesia, Intensive Care and Emergency, Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milan, Italy
34Department of Anesthesia and Intensive Care Unit, Fondazione IRCCS Policlinico San Matteo and University of Pavia, Pavia, Italy
35Department of Anaesthesia and Intensive Care Medicine, Humanitas Clinical and Research Center – IRCCS, via Manzoni 56, 20089 Rozzano (Mi) – Italy
36Biotechnology and Life Sciences Department, Insubria University—Anesthesia and Intensive Care Circolo and Fondazione Macchi Hospital, ASST Sette Laghi, Varese (Italy)
37Department of Anesthesia and Intensive Care Medicine, San Giuseppe Hospital, Milan, Italy
38Department of Anesthesia and Intensive Care Medicine, Policlinico di Sant’Orsola, Alma Mater Studiorum University of Bologna, Bologna, Italy
39Policlinico San Marco, San Donato Group Hospitals, Zingonia, Bergamo, Italy
40Department of Anesthesia and Intensive Care Medicine, San Gerardo Hospital, ASST Monza, Monza e Brianza, Italy
41Humanitas Gavazzeni, Bergamo (Italy)
42Policlinico San Pietro, Ponte San Pietro, Italy
43Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico, Respiratory Unit and Cystic Fibrosis Adult Center, Milan, Italy. University of Milan,
44Department of Pathophysiology and T transplantation, Milan, Italy
45Ospedale L. Sacco, ASST Fatebenefratelli-Sacco, Division of Respiratory Diseases, Milano, Italy.
46Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico, Department of Medicine – Acute Medical Unit, Milan, Italy
47Department of Anesthesia and Intensive Care Medicine, Humanitas Clinical and Research Center – IRCCS, Rozzano, Italy
Abbreviations
- ARDS
Acute respiratory distress syndrome
- ARF
Acute respiratory failure
- CPAP
Continuous positive airway pressure
- CI
Confidence interval
- COVID-19
Coronavirus-19 disease
- DNI
Do-not-intubate
- ICU
Intensive care unit
- IMV
Invasive mechanical ventilation
- NIRS
Noninvasive respiratory support
- PaO2/FiO2
Arterial oxygen tension on inspired oxygen fraction ratio
- SARS-CoV-2
Severe acute respiratory syndrome related to novel coronavirus
Authors' contributions
All authors listed concur with the submitted version of the manuscript and with the listing of the authors. In particular, all authors meet the following criteria for authorship: 1. substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; 2. drafting or revising the manuscript; 3. final approval of the version submitted for publication; 4. accountability for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. GC, TE helped in acquisition and analysis of data for the work. GC contributed to conception and design of the work; DA statistically analyzed the data; GC, EDR interpreted the data for the work; GC, RV, PN, ST, EDR drafted the manuscript; RC, FM, SA, AC, GB, GF, GG, MC, AP, MV, TL, VMR, SLDD, OR, AG, AP, GN, CB, ST shared supplemental data from their databases; GC, TE, RC, FM, SA, AC, GB, GF, GG, MC, AP, MV, TL, VMR, SLDD, OR, AG, AP, GN, CB, ST, PN, ST, RV, EDR revised the final version.
Funding
Not applicable.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The following authors declare to have no conflicts of interest: Prof Gianmaria Cammarota, Dr. Teresa Esposito, Dr. Francesco Menzella, Prof Stefano Aliberti, Dr Michele Vitacca, Prof V. Marco Ranieri, Prof Onofrio Resta, Dr Antonio Gidaro, Dr Antonella Potalivo, Dr Giuseppe Nardi, Dr Claudia Brusasco, and Prof Rosanna Vaschetto. Dr. Roberto Cosentini reports personal fees from Fisher & Paykel, outside the submitted work. Prof. Giuseppe Foti declares conference fees from DIMAR. Dr. Andrea Coppadoro has a patent and received consultancy fees from Flowmeter. Prof. Giacomo Grasselli declares personal fees (payment for lectures) from Getinge, Biotest, Draeger Medical, MSD, Fisher&Paykel; travel/accommodation/congress registration support from Biotes and Getinge; unrestricted research grant from Fisher&Paykel, MSD all outside the submitted work. Prof. Giacomo Bellani reports personal fees from Dimar and Intersurgical and is owner of a patent potentially related to this manuscript, personal fees from Draeger, Getinge, Hamilton, GE Healthcare not related to this work. Prof. Maurizio Cecconi reported personal fees from Edwards Lifesciences, Directed Systems, and Cheetah Medical outside the submitted work. Prof. Antonio Pesenti reports personal fees from Maquet, Xenios, Baxter, and Boehringer Ingelheim, outside the submitted work. Dr. Sandro Luigi Di Domenico declares relationship with Menarini group on behalf of Dynamicon education s.r.l. Dr. Tom Lawton is involved in the development of an open-source CPAP device for use in low-income countries under an EPSRC grant (no funding received). Prof. Paolo Navalesi declares to have received: grants, personal fees, and nonfinancial support from Maquet Critical Care; grants and nonfinancial support from Draeger and Intersurgical S.p.A; and personal fees from Oriopharma, Philips, Resmed, MSD, and Novartis, in each case for reasons that remain unrelated to the submitted work. Prof. Navalesi also contributed to the development of the patented ‘helmet Next,’ the royalties for which are paid to Intersurgical Spa. Prof. Navalesi contributed to the development of a device not discussed in the present study with patent application number: EP20170199831. Dr. Simonetta Tesoro received conference fees from MSD. Prof. Edoardo De Robertis received conference fees from MSD and Baxter.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rosanna Vaschetto and Edoardo De Robertis share the co-senior authorship
References
- 1.Zhou P, Yang X Lou, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature; 2020. [DOI] [PMC free article] [PubMed]
- 2.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet; 2020. [DOI] [PMC free article] [PubMed]
- 3.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA J Am Med Assoc. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goyal P, Choi JJ, Pinheiro LC, Schenck EJ, Chen R, Jabri A, et al. Clinical characteristics of Covid-19 in New York City. N Engl J Med. 2020;382:2372–2374. doi: 10.1056/NEJMc2010419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA - J Am Med Assoc. 2020. [DOI] [PMC free article] [PubMed]
- 6.Cammarota G, Ragazzoni L, Capuzzi F, Puiulvirenti S, Santangelo E, Verdina F, et al. Critical care surge capacity to respond to the COVID-19 pandemic in Italy : a rapid and affordable solution in the Novara Hospital. Prehosp Disaster Med. 2020;35:431–433. doi: 10.1017/S1049023X20000692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vitacca M, Nava S, Santus P, Harari S. Early consensus management for non-ICU ARF SARS-CoV-2 emergency in Italy: from ward to trenches. Eur Respir J. 2020;55:2000632. doi: 10.1183/13993003.00632-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA - J Am Med Assoc. 2020. [DOI] [PMC free article] [PubMed]
- 9.Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med Elsevier Ltd. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Franco C, Facciolongo N, Tonelli R, Dongilli R, Vianello A, Pisani L, et al. Feasibility and clinical impact of out-of-ICU noninvasive respiratory support in patients with COVID-19-related pneumonia. Eur Respir J. 2020;56:2002130. doi: 10.1183/13993003.02130-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vaschetto R, Barone-Adesi F, Racca F, Pissaia C, Maestrone C, Colombo D, et al. Outcomes of COVID-19 patients treated with continuous positive airway pressure outside the intensive care unit. ERJ Open Res. 2021;7:00541–2020. doi: 10.1183/23120541.00541-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Frat JP, Thille AW, Mercat A, Girault C, Ragot S, Perbet S, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015;372:2185–2196. doi: 10.1056/NEJMoa1503326. [DOI] [PubMed] [Google Scholar]
- 13.Brochard L, Slutsky AS, Pesenti A. Critical care perspective mechanical ventilation to minimize progression of lung injury in acute respiratory failure. Am J Respir Crit Care Med. 2017;195:438–442. doi: 10.1164/rccm.201605-1081CP. [DOI] [PubMed] [Google Scholar]
- 14.Brochard L, Lefebvre JC, Cordioli RL, Akoumianaki E, Richard JCM. Noninvasive ventilation for patients with hypoxemic acute respiratory failure. Semin Respir Crit Care Med. 2014;35:492–500. doi: 10.1055/s-0034-1383863. [DOI] [PubMed] [Google Scholar]
- 15.Rochwerg B, Brochard L, Elliott MW, Hess D, Hill NS, Nava S, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50:1–20. doi: 10.1183/13993003.02426-2016. [DOI] [PubMed] [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, Altman DG, Group TP. Preferred reporting items for systematic reviews and meta-analyses : the PRISMA statement. PLOS Med. 2009;6. [PMC free article] [PubMed]
- 17.Potere N, Valeriani E, Candeloro M, Tana M, Porreca E, Abbate A, et al. Acute complications and mortality in hospitalized patients with coronavirus disease 2019: a systematic review and meta-analysis. Crit Care Critical Care. 2020;24:1–12. doi: 10.1186/s13054-020-03022-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (Minors): Development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 19.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. J Intell Inf Syst. 2006;27:159–184. doi: 10.1007/s10844-006-2974-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Menzella F, Fontana M, Salvarani C, Massari M, Ruggiero P, Scelfo C, et al. Efficacy of tocilizumab in patients with COVID-19 ARDS undergoing noninvasive ventilation. Crit Care. 2020;24:589. doi: 10.1186/s13054-020-03306-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ramirez GA, Bozzolo EP, Castelli E, Marinosci A, Angelillo P, Damanti S, et al. Continuous positive airway pressure and pronation outside the intensive care unit in COVID 19 ARDS. Minerva Med. Italy; 2020. [DOI] [PubMed]
- 22.Avdeev SN, Yaroshetskiy AI, Tsareva NA, Merzhoeva ZM, Trushenko NV, Nekludova GV, et al. Noninvasive ventilation for acute hypoxemic respiratory failure in patients with COVID-19. Am J Emerg Med. 2021;39:154–157. doi: 10.1016/j.ajem.2020.09.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brusasco C, Corradi F, Di Domenico A, Raggi F, Timossi G, Santori G, et al. Continuous positive airway pressure in Covid-19 patients with moderate-to-severe respiratory failure. Eur Respir J. 2020;57:2002524. doi: 10.1183/13993003.02524-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Duca A, Memaj I, Zanardi F, Preti C, Alesi A, Della Bella L, et al. Severity of respiratory failure and outcome of patients needing a ventilatory support in the Emergency Department during Italian novel coronavirus SARS-CoV2 outbreak: preliminary data on the role of Helmet CPAP and non-invasive positive pressure Ventilation. EClinicalMedicine Elsevier Ltd. 2020;24:1–7. doi: 10.1016/j.eclinm.2020.100419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aliberti S, Radovanovic D, Billi F, Sotgiu G, Costanzo M, Pilocane T, et al. Helmet CPAP treatment in patients with COVID-19 pneumonia: a multicentre cohort study. Eur. Respir. J. 2020;56:2001935. doi: 10.1183/13993003.01935-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Di Domenico SL, Coen D, Bergamaschi M, Albertini V, Ghezzi L, Cazzaniga MM, et al. Clinical characteristics and respiratory support of 310 COVID-19 patients, diagnosed at the emergency room: a single-center retrospective study. Int Emerg Med. 2020;16:1051–1060. doi: 10.1007/s11739-020-02548-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Faraone A, Beltrame C, Crociani A, Carrai P, Lovicu E, Filetti S, et al. Effectiveness and safety of noninvasive positive pressure ventilation in the treatment of COVID-19-associated acute hypoxemic respiratory failure: a single center, non-ICU setting experience. Int Emerg Med. 2020;1–8. [DOI] [PMC free article] [PubMed]
- 28.Potalivo A, Montomoli J, Facondini F, Sanson G, Lazzari Agli LA, Perin T, et al. Sixty-day mortality among 520 Italian hospitalized COVID-19 patients according to the adopted ventilatory strategy in the context of an integrated multidisciplinary clinical organization: a population-based cohort study. Clin Epidemiol. 2020;12:1421–1431. doi: 10.2147/CLEP.S278709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Di Lecce V, Carpagnano GE, Pierucci P, Quaranta VN, Barratta F, Zito A, et al. Baseline characteristics and outcomes of COVID-19 patients admitted to a respiratory intensive care unit (RICU) in Southern Italy. Multidiscip Respir Med. 2020;15:704. doi: 10.4081/mrm.2020.704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bellani G, Grasselli G, Cecconi M, Antolini L, Borelli M, Giacomi F De, et al. Noninvasive ventilatory support of COVID-19 patients outside the intensive care units (WARd-COVID). Ann Am Thorac Soc. 2021. [DOI] [PMC free article] [PubMed]
- 31.Coppadoro A, Fruscio R, Verga L, Soria A, Noe B, Sciacca R Di, et al. Helmet CPAP to Treat Hypoxic Pneumonia Outside the ICU : An Observational Study During the COVID- 19 Outbreak. Crit Care. 2020;25. [DOI] [PMC free article] [PubMed]
- 32.Gidaro A, Samartin F, Brambilla AM, Cogliati C, Ingrassia S, Banfi F, et al. Occurrence of pneumothorax and pneumomediastinum in Covid-19 patients during non-invasive ventilation with continuous positive airway pressure. medRxiv. 2020; [DOI] [PMC free article] [PubMed]
- 33.Noeman-Ahmed Y, Gokaraju S, Powrie DJ, Amran DA, El Sayed I, Roshdy A. Predictors of CPAP outcome in hospitalised COVID-19 patients. medRxiv. 2020. [DOI] [PubMed]
- 34.Lawton T, Corp AP, Javid R, MacNally L, McCooe M, Newton E. Reduced ICU demand with early CPAP and proning in COVID-19 at Bradford: a single centre cohort. medRxiv. 2020. [DOI] [PMC free article] [PubMed]
- 35.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bellani G, Laffey JG, Pham T, Madotto F, Fan E, Brochard L, et al. Noninvasive ventilation of patients with acute respiratory distress syndrome: insights from the LUNG SAFE study. Am J Respir Crit Care Med. 2017;195:67–77. doi: 10.1164/rccm.201606-1306OC. [DOI] [PubMed] [Google Scholar]
- 38.Grieco DL, Menga LS, Cesarano M, Rosà T, Spadaro S, Bitondo MM, et al. Effect of helmet noninvasive ventilation vs high-flow nasal oxygen on days free of respiratory support in patients with COVID-19 and moderate to severe hypoxemic respiratory failure: the HENIVOT randomized clinical trial. JAMA - J Am Med Assoc. 2021;325:1731–1743. doi: 10.1001/jama.2021.4682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cheung TMT, Yam LYC, So LKY, Lau ACW, Kong BMH, Yung RWH. Effectiveness of noninvasive positive pressure ventilation in the treatment of acute respiratory failure in severe acute respiratory syndrome. Chest. 2004;126:845–850. doi: 10.1378/chest.126.3.845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Esquinas AM, Egbert Pravinkumar S, Scala R, Gay P, Soroksky A, Girault C, et al. Noninvasive mechanical ventilation in high-risk pulmonary infections: a clinical review. Eur Respir Rev. 2014;23:427–438. doi: 10.1183/09059180.00009413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Alraddadi BM, Qushmaq I, Al-Hameed FM, Mandourah Y, Almekhlafi GA, Jose J, et al. Noninvasive ventilation in critically ill patients with the middle east respiratory syndrome. Influenza Other Respi Viruses. 2019;13:382–390. doi: 10.1111/irv.12635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brochard L, Slutsky A, Pesenti A. Mechanical ventilation to minimize progression of lung injury in acute respiratory failure. Am J Respir Crit Care Med. 2017;195:438–442. doi: 10.1164/rccm.201605-1081CP. [DOI] [PubMed] [Google Scholar]
- 43.Wilson ME, Mittal A, Karki B, Dobler CC, Wahab A, Curtis JR, et al. Do-not-intubate orders in patients with acute respiratory failure: a systematic review and meta-analysis. Intensive Care Med. 2020;46:36–45. doi: 10.1007/s00134-019-05828-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wilson ME, Majzoub AM, Dobler CC, Curtis JR, Nayfeh T, Thorsteinsdottir B, et al. Noninvasive ventilation in patients with do-not-intubate and comfort-measures-only orders: a systematic review and meta-analysis. Crit Care Med. 2018;46:1209–1216. doi: 10.1097/CCM.0000000000003082. [DOI] [PubMed] [Google Scholar]
- 45.Alhazzani W, Moller MH, Arabi YM, Loeb M, Gong MN, Fan E, et al. Surviving sepsis campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19) Intensive Care Med. 2020;46:854–87. doi: 10.1007/s00134-020-06022-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Grasselli G, Greco M, Zanella A, Albano G, Antonelli M, Bellani G, et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Intern Med. 2020;1–11. [DOI] [PMC free article] [PubMed]
- 47.Chalmers JD, Crichton ML, Goeminne PC, Cao B, Humbert M, Shteinberg M, et al. Management of hospitalised adults with coronavirus disease-19 (COVID-19): a European Respiratory Society living guideline. Eur Respir J. 2021;57:2100048. doi: 10.1183/13993003.00048-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Quill CM, Ratcliffe SJ, Harhay MO, Halpern SD. Variation in decisions to forgo life-sustaining therapies in US ICUs. Chest. 2014;146:573–582. doi: 10.1378/chest.13-2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Long AC, Brumback LC, Curtis JR, Avidan A, Baras M, De RE, et al. Agreement with consensus statements on end-of-life care: a description of variability at the level of the provider, hospital, and country. Crit Care Med. 2020;47:1396–1401. doi: 10.1097/CCM.0000000000003922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Santonocito C, Ristagno G, Gullo A, Weil MH. Do-not-resuscitate order: a view throughout the world. J Crit Care. 2013;28:14–21. doi: 10.1016/j.jcrc.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 51.Johnson Shen M, Prigerson HG, Paulk E, Trevino K, Penedo FJ, Tergas AI, et al. Impact of end-of-life discussions on the reduction of Latino/non-Latino disparities in DNR order completion. Cancer. 2016;122:1749–1756. doi: 10.1002/cncr.29973. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Search strategy of electronic database.
Additional file 2. Enrollment flow diagram.
Additional file 3. Characteristics of the enrolled investigations, overall clinical characteristics of the populations investigated in the enrolled studies, and list of studies excluded after reading the full text.
Additional file 4. Methodological quality of the included investigations.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.