Abstract
Objectives:
To determine the primary reason for hospitalizations in systemic sclerosis (SSc) and impact of underlying interstitial lung disease (ILD) in a tertiary scleroderma center.
Methods:
A retrospective analysis on a subset of a scleroderma cohort from 2011 - 2019 was performed to assess causes for hospitalizations and mortality. A chart review was performed to extract demographics, primary reason for hospitalization and inpatient mortality. Admissions were classified as SSc (if hospitalization reason was related to primary organ dysfunction) and non-SSc related causes.
Results:
The mean age of the cohort was 53.1 years, 78% were women, and the mean disease duration was 5.2 years. Among 484 patients, 182 (37.6%) were admitted for a total of 634 admissions. In 382 SSc-related admissions, pulmonary hypertension (12.0%) and gastrointestinal dysmotility (11.0%), were major causes of urgent admissions; management of digital vasculopathy (26.1%) was the major reason for elective admissions. In 252 non-SSc related admissions, infection (respiratory:11.5%, skin and soft tissue: 6.3%) was the major reason for urgent admissions, and elective surgery (21.4%) was the major reason for elective admissions. We found 65% of all patients had underlying ILD and a greater proportion of patients with ILD were hospitalized (122 patients). Overall inpatient mortality was 9.3% and the leading cause for mortality was progressive pulmonary hypertension.
Conclusion:
Among a large cohort of SSc patients who are followed at a tertiary scleroderma center, 37.6% had hospital admissions, while worsening pulmonary hypertension, ILD, cardiac involvement and infectious complications were the major cause of mortality and morbidity.
Keywords: Systemic sclerosis, hospitalizations, lung fibrosis, mortality, morbidity
INTRODUCTION
Systemic Sclerosis (SSc) is an immune-mediated rheumatological disease characterized by vasculopathy and fibrosis of the skin and internal organs [1, 2]. SSc has high morbidity and the highest case fatality of all rheumatic diseases [3]. Cardio-pulmonary involvement, including pulmonary arterial hypertension (PAH) and interstitial lung disease (ILD) are now the major causes of death, as a consequence of reduced mortality in patients with scleroderma renal crisis since the institution of angiotensin converting enzyme inhibitors [4–7]. There is increasing interest in early screening and treatment of PAH and ILD to improve morbidity and outcomes [8–10]. Although approximately 70% have underlying ILD, 20-30% have progressive lung disease and treatment is largely reserved for them.
Previous studies have reviewed hospital admissions, including inpatient mortality, in large administrative databases or single centers. A majority of the studies were completed between 2000 and 2014 and have consistently shown that PAH, ILD, and cardiac involvement and infections constitute the major reasons for hospitalization and death in this patient population [4, 7, 11, 12]. Some studies also noted an increase in admissions for the treatment of digital ischemia with intravenous prostacyclin [13, 14].
The current study had two objectives: 1) To determine the reasons for hospitalizations (SSc and non-SSc related), length of stay, and cause of death; and 2) to determine the impact of underlying ILD on the previously mentioned parameters in a large tertiary care scleroderma referral center.
PATIENTS AND METHODS
Patients included in the study were selected from the cohort of patients followed in the University of Michigan (U-M) Scleroderma Program, which includes approximately 1500 patients. We selected a subset of patients who were being followed between July 2011 to September 2019. Using the SlicerDicer tool in EPIC®, software that allows for filtering and creating patient lists from the electronic medical records, we used “scleroderma” as a keyword to filter patients who had SSc. The list was reviewed and only patients that were seen by the senior author were included. The list was narrowed further to search for patients who had available of thoracic computed tomography (CT) for evaluation of ILD (484 patients). We reviewed all available hospitalization records at U-M for our final list of patients and 182 patients (37.6 %) were found to have required hospitalizations, some having multiple hospitalizations during our selected time period.
A chart review was performed on the selected patients to extract age, race, gender, primary reason for hospital admission, length of stay (LOS), current use of immunosuppressive medication, and vital status including cause of death. The primary reason for hospitalization was determined using the discharge diagnosis and review of the hospitalization encounter, including reviewing the consultants’ notes, laboratory and radiological data (if appropriate), and other supporting data and final decision was made by the first author in conjunction with the senior author. The diagnosis that best fit the events that occurred was used.
Admissions to the U-M hospital were categorized into elective and non-elective admissions. Elective admissions included a direct admission from a physicians’ or other healthcare provider’s office of any specialty or a planned admission for elective procedures or surgeries. Non-elective admissions included all admissions resulting from an emergency room or urgent care visit for further medical management in the hospital. These admissions were determined by the medical judgement of the emergency room physicians and any consulting specialists on the U-M staff that were brought in to assist in the care of the patient. Admissions were classified as related to SSc if the principal hospitalization reason was primary organ dysfunction due to SSc and /or its treatment, while all other reasons for hospitalization were categorized as non-SSc admissions, as done by Tyndall et al [4]. The involved organ system qualified as a scleroderma related diagnosis if review of the medical record recorded symptoms, signs and diagnostic lab work, imaging studies supporting worsening of the organ system. Patients were classified as being on immunosuppressive therapy if they were on prednisone (>10 mg/day) or immunosuppressive medications such as mycophenolate mofetil, cyclophosphamide, azathioprine, methotrexate, or other biologics, four weeks prior to or at the time of admission.
ILD was diagnosed by thoracic radiologists upon completion of a thoracic CT [15]. ILD was defined by the presence of bilateral, subpleural, lower lobe predominant distribution of either: reticular and/or ground glass opacity, with or without traction bronchiectasis, or honeycombing with the absence of a pattern that is predominantly nodular, cystic, peribronchovascular/central or upper lung predominant, mosaic attenuation, or consolidation. We diagnosed pulmonary hypertension on a right heart catheterization with mean pulmonary arterial pressure ≥ 25mmHg and further classified into pulmonary arterial hypertension (PAH), PH due to ILD and PH due to heart failure [16]
Mortality and cause of death were assessed that occurred at U-M and confirmed by reviewing the electronic medical record.
Statistical Analysis
Descriptive statistics were performed on the baseline demographics of the study population, comparing participants who are hospitalized vs. not hospitalized, and who had limited (≤ 4) vs. multiple (> 4; assessed as 75th percentile for number of hospitalizations) hospitalizations. For continuous variables that followed a normal distribution, the means and standard deviations were compared across groups using Student’s T test. For continuous variables that did not follow a normal distribution, the medians and ranges where compared using the Wilcoxon rank sum test. For categorical variables, counts and proportions were calculated and compared across groups using Chi-squared tests or Fisher exact test. A significance level of 0.05 was used for all baseline statistical tests. A univariate logistic model was fitted for each of the baseline demographics variables to look at their predictive effect on having/not having hospitalization. An odds ratio, and a P value were obtained for each variable. Number of hospitalizations were counted in the whole population, as well as by ILD +/− groups. Mean (SD) and Median (IQR) length of stay were reported for reason of hospitalization. Cox proportional hazards models were fitted to explore the survival probability comparing patients who were hospitalized due to cardiopulmonary issues vs. due to other reasons, and comparing patients who were hospitalized due to pulmonary involvement vs. due to other reasons. Survival plots were drawn and hazard ratios were calculated. All analyses were conducted in SAS 9.4 (SAS Institute Inc).
RESULTS
Our study included 484 patients, of which 182 (37.6%) patients had hospital admissions. The mean (SD) age of the cohort was 53.1(13.3) years, 78% were female, disease duration (from first non-Raynaud’s phenomenon symptom) was 5.2(7.0) years, 46% had diffuse cutaneous SSc (dcSSc), and 39% had limited cutaneous SSc (lcSSc). There were no differences in the demographics of patients who were or were not hospitalized (Table 1). However, non-hospitalized patients had a higher percent-predicted forced vital capacity (FVC%) (79.9% vs 74.3%), higher DLCO (65.6% vs 57.3%) and presence of anti-topoisomerase antibody (27% vs 14%) compared to hospitalized patients (p< 0.05 for all comparisons).
Table 1:
Baseline characteristics of the total cohort, stratified by those who were hospitalized versus not hospitalized
| Total n=484 | Hospitalized n=182 | Not hospitalized n=302 | p-value. | |
|---|---|---|---|---|
| Age1,Mean(SD)years | 53.1(13) | 53.8(13) | 52.7(13) | 0.383 |
| Female Sex, N(%) | 378(78) | 144(79) | 234(78) | 0.673 |
| Race, N(%) |
371(77) n=480 |
140(77) n=181 |
231(77) n=299 |
0.330 |
| White | ||||
| Black | 73(15) n=480 | 31(17) n=181 | 42(14) n=299 | |
| other | 36(8) n=480 | 10(6) n=181 | 26(9) n=299 | |
| Ethnicity, N(%) |
23(5) n=471 |
9(5) n=180 |
14(5) n=291 |
1.000 |
| Hispanic | ||||
| Non-Hispanic | 446(95) n= 471 | 170(95) n=180 | 276(95) n=291 | |
| Other | 2(0)n=471 | 1(1) n=180 | 1(0) n=291 | |
| Smoking, N(%) |
35(7) n=479 |
10(6) n=182 |
25(9) n=297 |
0.251 |
| Current Smoker | ||||
| Former Smoker | 171(36) n=479 | 72(40) n=182 | 99(33) n=297 | |
| Never Smoker | 273(57) n=479 | 100(55) n=182 | 173(58) n=297 | |
| Marital Status, N(%) |
117(25) n=471 |
50(28) n=181 |
67(23) n=290 |
0.333 |
| Single | ||||
| Married | 298(63) n=471 | 109(60) n=181 | 189(65) n=290 | |
| Divorced | 23(7) n=471 | 10(6) n=181 | 22(8) n=290 | |
| Widowed | 24(5) n=471 | 12(6) n=181 | 12(4) n=290 | |
| Systemic Sclerosis, N(%) |
187(39) |
65(36) |
122(40) |
0.751 |
| Limited | ||||
| Diffuse | 223(46) | 87(48) | 136(45) | |
| Sine | 28(6) | 12(7) | 16(5) | |
| Overlap | 46(10) | 18(10) | 28(9) | |
| Disease Duration2, Mean (SD) years | 5.2(7) | 5.1(7) | 5.3(7) | 0.382 |
| MRSS, Mean (SD) | 12.0(10) n=324 | 13.0(10) n=114 | 11.5(10) n=210 | 0.190 |
| Autoantibodies, N(%) |
392(91) n=433 |
146(90) n=163 |
246(91) n=270 |
0.596 |
| ANA | ||||
| Anti-Smith | 21(5) n=419 | 12(7) n=163 | 9(4) n=256 | 0.079 |
| Anti-Centromere | 83(22) n=386 | 34(23) n=147 | 49(21) n=239 | 0.542 |
| Anti-topoisomerase 1 | 94(22) n=424 | 22(14) n=158 | 72(27) n=266 | 0.0016 |
| Anti-RNA polymerase 3 | 61(23) n=264 | 21(22) n=94 | 40(24) n=170 | 0.826 |
| Anti-Ro | 74(18) n=423 | 28(17) n=166 | 46(18) N=257 | 0.785 |
| Anti-RNP | 58(14) n=417 | 25(15) n=164 | 33(13) n-253 | 0.526 |
| ILD3, N(%) | 317(65) | 122(67) | 195(65) |
0.617 |
| NSIP | 252(80) | 99(81) | 153(78) | |
| UIP | 41(13) | 13(11) | 28(14) | |
| Other | 24(8) | 10(8) | 14(7) | |
| PFT% Predicted Mean (SD) |
77.8(21) n=469 |
74.3(21) n=178 |
79.9(20) n=291 |
|
| FVC% | 0.004 | |||
| TLC% | 89.9(22) n=283 | 89.8(22) n=104 | 89.9(21) n=179 | 0.949 |
| DLCO% | 62.5(23.7) n=411 | 57.3(22.8) n=151 | 65.6(23.7) n=260 | 0.001 |
| Baseline Medication N,(%) | ||||
| Prednisone (≥ 1 week) | 118(24) | 50(28) | 68(23) | 0.22 |
| Cyclophosphamide | 11(2) | 7(4) | 4(1) | 0.111 |
| Mycophenolate Mofetil | 103(21) | 38(21) | 65(22) | 0.867 |
| Methotrexate | 42(9) | 16(9) | 26(9) | 0.945 |
| Hydroxychloroquine | 45(9) | 14(8) | 31(10) | 0.345 |
| Multiple Medications4 | 83(17) | 32(18) | 51(17) | 0.844 |
Note:
Age is calculated as ILD diagnosis date,
Disease Duration was defined as date of first non-Raynaud’s symptom to date of ILD diagnosis (only first HRCT is considered).
ILD pattern and disease duration are only compared among ILD+ patients.
Taking at least 2 immunosuppressive at baseline.
Abbreviations: MRSS=Modified Rodnan Skin Score; ILD=Interstitial Lung Disease; NSIP=Nonspecific interstitial pneumonia; UIP=Usual Interstitial pneumonia; FVC=Forced vital capacity; TLC=Total Lung capacity; DLCO=Diffuse capacity for carbon monoxide.
One hundred and eighty-two patients created a total of 634 hospital encounters, with 118 (65.8%) patients had more than one admission. For all hospital encounters, the mean (SD) age of the patient was 53.8 (13.0) years, 79% were female, disease duration was 5.1(7.0)) years, 48% had dcSSc, 36% had lcSSc, and 67% had ILD (Table 1).
Hospitalizations related to SSc
Of the 634 hospital encounters for 182 patients, 382 (60.2%) hospital admissions were for SSc-related due to worsening disease or treatment for SSc. Of the 257 urgent or emergent hospitalizations, the most common causes of were due to worsening of PH (17.0%), gastrointestinal (GI) dysmotility (upper & lower; 16.3%) and new or worsening cardiac arrhythmias (10.0%). For PH, majority of admissions were due to PAH (32 admissions) and PH due to ILD (14 admissions, Figure 1). For elective admissions (125 admissions), the most common causes of admissions were for intravenous prostacyclin (epoprostenol) for treatment of digital ischemia (61.6%) and inpatient chemotherapy or biologic therapy for underlying SSc (24%; Table 2).
Figure 1: Causes for hospitalization and mortality in patients with pulmonary hypertension.
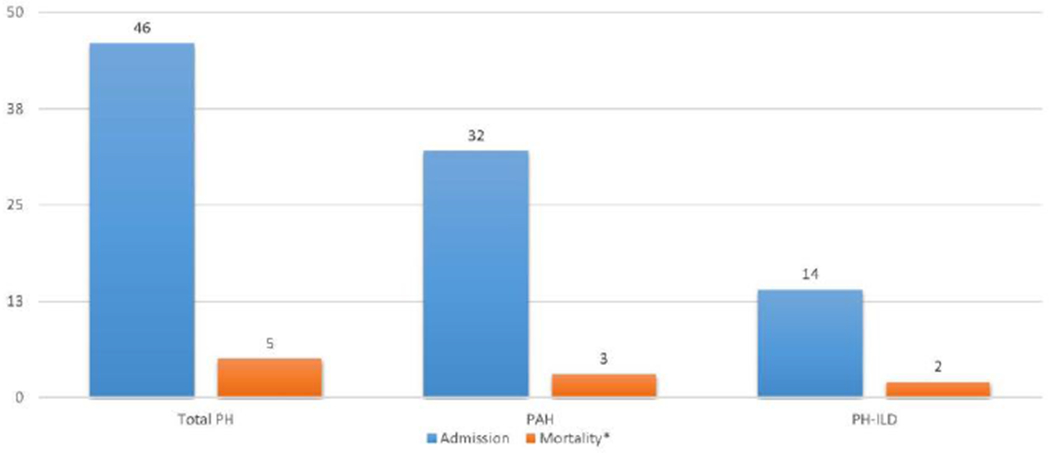
PH= Pulmonary hypertension PAH= Pulmonary arterial hypertension PH-ILD= Pulmonary hypertension – interstitial lung disease *Mortality related to pulmonary hypertension.
Table 2:
Causes for hospitalizations related to systemic sclerosis, for the overall group and stratified by presence or absence of interstitial lung disease
| Total Admissions for all patients | With ILD | Without ILD | |||
|---|---|---|---|---|---|
| Reasons for Hospitalization | Total Admissions* | Elective Admissions | LOS, days (mean) | Total Admissions* | Total Admissions* |
| All Scleroderma related | 382 | 125 | 5.5 (6.4) | 231 | 151 |
| Digital Vasculopathy | 100 | 77 | 4.3 (2.4) | 39 | 61 |
| Intravenous Prostacyclin (epoprostenol) | 100 | 77 | 4.3 (2.4) | 39 | 61 |
| Gastroenterology | 91 | 0 | 5.2 (6.3) | 49 | 42 |
| GI dysmotility-upper | 21 | 0 | 3.9 (2.7) | 5 | 16 |
| GI bleed | 23 | 0 | 3.2 (2.9) | 15 | 8 |
| Gastritis/Ulcer | 23 | 0 | 3.8 (2.7) | 18 | 5 |
| GI Dysmotility – Lower | 21 | 0 | 10.5(10.8) | 9 | 12 |
| Small Intestinal Bowel Overgrowth | 3 | 0 | 4.7(3.1) | 2 | 1 |
| Cardiovascular | 54 | 5 | 4.1(3.5) | 40 | 14 |
| Pericarditis/ Pericardial Effusion | 8 | 0 | 5.4(3.9) | 6 | 2 |
| Arrythmias | 30 | 5 | 3.4(3.3) | 20 | 10 |
| Systolic Heart Failure | 9 | 0 | 5.0(4.6) | 9 | 0 |
| Diastolic Heart Failure | 7 | 0 | 4.3 (2.0) | 5 | 2 |
| Cardiopulmonary | 46 | 2 | 7.0 (7.4) | 28 | 18 |
| Pulmonary Hypertension | 46 | 2 | 7.0 (7.4) | 28 | 18 |
| Treatment/Infusion-related | 37 | 36 | 5.4 (7.6) | 34 | 3 |
| Rituximab/Cyclophosphamide Infusions | 31 | 30 | 2.2 (1.5) | 28 | 3 |
| Stem Cell Transplant | 6 | 6 | 21.8 (3.9) | 6 | 0 |
| Renal | 25 | 5 | 9.9 (11.9) | 19 | 6 |
| Scleroderma Renal Crisis | 11 | 0 | 15.6 (15.7) | 9 | 2 |
| HTN Urgency | 4 | 0 | 6.8 (7.7) | 3 | 1 |
| HTN Emergency | 5 | 0 | 6.8 (4.1) | 3 | 2 |
| Renal Transplant/ Rejection | 5 | 5 | 3.0 (1.2) | 4 | 1 |
| Pulmonary Involvement | 19 | 0 | 7.4 (9.7) | 18 | 1 |
| Aspiration Pneumonitis | 7 | 0 | 9.0 (12.9) | 6 | 1 |
| Interstitial Lung Disease | 12 | 0 | 6.5 (7.8) | 12 | 0 |
| Malnutrition/Failure to Thrive | 7 | 0 | 5.0 (2.4) | 4 | 3 |
| Musculoskeletal | 3 | 0 | 5.3 (3.2) | 0 | 3 |
| Myositis/Myonecrosis | 3 | 0 | 5.3 (3.2) | 0 | 3 |
Abbreviations: GI=gastrointestinal; HTN=Hypertension; LOS=length of Stay;
Total Admissions refers to all elective and emergent or urgent admissions.
The mean (SD) length of stay for SSc related illness was 5.5 (6.4) days. Of 182 patients, 10 died during inpatient stay due to SSc related illness; five deaths were due to worsening of cardio-pulmonary involvement(PH), two deaths were due to worsening ILD (n=2) and 3 deaths were due to other causes (Table 4).
Table 4.
Causes of Inpatient Mortality
| Cause of death | Total | ILD+ | ILD− |
|---|---|---|---|
| Cardiopulmonary | |||
| PH | 5 | 3 | 2 |
| Pulmonary | |||
| Progressive ILD | 2 | 2 | 0 |
| ARDS | 1 | 1 | 0 |
| Cardiac | |||
| Severe Aortic Stenosis w/Heart Failure | 1 | 0 | 1 |
| Arrythmia | 1 | 0 | 1 |
| STEMI | 1 | 1 | 0 |
| Gastroenterology | |||
| Severe GI Dysmotility with SBO | 1 | 1 | 0 |
| Cancer | |||
| Multiple Myeloma | 1 | 0 | 1 |
| Esophageal Cancer | 1 | 1 | 0 |
| Infection | |||
| Sepsis* | 1 | 1 | 0 |
| Pneumonia | 1 | 1 | 0 |
| Failure to thrive | 1 | 0 | 1 |
| Total Deaths | 17 | 11 | 6 |
Abbreviations: PH=Pulmonary Hypertension; SBO =Small Bowel Obstruction; ILD = Interstitial Lung Disease; ARDS= Acute respiratory distress syndrome; STEMI= ST elevation Myocardial infarction
Due to Pseudomonas Aeruginosa accompanied with ILD and Significant GI Dysmotility
Hospitalizations related to non-SSc causes
Admissions not directly attributed to SSc accounted for 38.8%, or 252, of the hospital encounters evaluated. The most common causes of urgent or emergent hospitalizations were due to respiratory infection in the background of immunosuppressive therapy (14%), skin or soft tissue infection in patients who were non-immunosuppressed (6.7%), followed by underlying malignancy (4.8%). For elective admissions (43 admissions), the majority of patients were admitted for surgery: GI surgery (28%), genitourinary surgery (28%) and orthopedic surgery (21%; Table 3).
Table 3:
Reasons for hospitalizations not related to underlying systemic sclerosis, for the overall group and stratified by presence or absence of interstitial lung disease
| All Patients | With ILD | Without ILD | |||
|---|---|---|---|---|---|
| Reasons for Hospitalizations | Total Admissions* | Elective Admissions | LOS Days (mean) | Total Admissions* | Total Admissions* |
| All Non-Scleroderma related | 252 | 43 | 5.7 (7.1) | 171 | 81 |
| Infections | 83 | 2 | 5.8 (6.8) | 65 | 18 |
| Immunosuppressants | 46 | 0 | 5.4 (5.3) | 42 | 4 |
| Respiratory | 29 | 0 | 5.2 (3.7 | 27 | 2 |
| Genitourinary | 4 | 0 | 1.5 (0.6) | 4 | 0 |
| Skin/Soft tissues | 9 | 0 | 3.9 (3.4) | 8 | 1 |
| Bloodstream Infections | 2 | 0 | 16.5 (19.1) | 1 | 1 |
| Line-related | 0 | 0 | - | 0 | 0 |
| GI Infection | 2 | 0 | 12.5 (3.5) | 2 | 0 |
| Non-Immunosuppressants | 37 | 2 | 6.2 (8.3) | 23 | 14 |
| Respiratory | 10 | 0 | 5.3 (6.3) | 10 | 0 |
| Genitourinary | 1 | 0 | 3.0 | 0 | 1 |
| Skin/Soft tissues | 16 | 2 | 6.9(11.6) | 3 | 13 |
| Bloodstream Infections | 7 | 0 | 7.3(3.0) | 7 | 0 |
| Line-Related | 1 | 0 | 2 | 1 | 0 |
| GI Infection | 2 | 0 | 4 (0) | 2 | 0 |
| Surgery | 54 | 37 | 5.2 (5.4) | 29 | 25 |
| Orthopedic | 19 | 9 | 4.6 (4.0) | 8 | 11 |
| Transplants | 2 | 2 | 16.5 (6.4) | 2 | 0 |
| GI | 17 | 12 | 7.5 (6.6) | 8 | 9 |
| Genitourinary | 12 | 12 | 2.3 (1.1) | 7 | 5 |
| Endocrine Surgery | 2 | 1 | 1.0 (0) | 2 | 0 |
| Lung Surgery | 2 | 1 | 2.0(0) | 2 | 0 |
| Cardiovascular | 18 | 2 | 5.3 (4.3) | 13 | 5 |
| ACS | 7 | 0 | 4.4 (3.6) | 5 | 2 |
| Valvular Dysfunction | 4 | 1 | 9.3(4.8) | 3 | 1 |
| Peripheral vascular Disease | 2 | 1 | 2.0 (0) | 2 | 0 |
| Aneurysm- Intracranial/ Renal | 2 | 0 | 4.5 (2.1) | 1 | 1 |
| Syncope | 3 | 0 | 5.0 (6.1) | 2 | 1 |
| Renal | 16 | 0 | 3.4 (3.2) | 12 | 4 |
| Acute Kidney Injury | 9 | 0 | 4.3(4.0) | 7 | 2 |
| Chronic Kidney Disease | 2 | 0 | 2.5 (0.7) | 1 | 1 |
| Electrolyte Imbalance | 5 | 0 | 2.2 (1.6) | 4 | 1 |
| Pulmonary | 15 | 0 | 6.9 (7.7) | 12 | 3 |
| Pneumothorax | 7 | 0 | 4.9 (2.3) | 7 | 0 |
| Reactive Airway Disease/ARDS | 7 | 0 | 5.9 (6.8) | 5 | 2 |
| COPD | 1 | 0 | 29.0 | 0 | 1 |
| Others** | 13 | 1 | 4.6 (5.4) | 10 | 3 |
| Gastroenterology | 11 | 0 | 4.5 (2.6) | 5 | 6 |
| Traumatic GI bleed | 2 | 0 | 6.0 (2.8) | 0 | 2 |
| Pancreatitis | 2 | 0 | 4.5(2.1) | 0 | 2 |
| Choledocholithiasis | 3 | 0 | 5.0 (4) | 1 | 2 |
| Abdominal Pain | 3 | 0 | 3.7 (2.1) | 3 | 0 |
| GI Dysmotility-Opioids | 1 | 0 | 2.0 | 1 | 0 |
| Cancer | 11 | 1 | 6.5 (5.5) | 10 | 1 |
| Lung Cancer | 5 | 1 | 6.2 (6.1) | 5 | 0 |
| Multiple Myeloma | 1 | 0 | 14.0 | 0 | 1 |
| Cancer of Unknown Primary | 1 | 0 | 1.0 | 1 | 0 |
| Breast cancer | 1 | 0 | 4.0 | 1 | 0 |
| Esophageal Cancer | 1 | 0 | 2.0 | 1 | 0 |
| Lymphoma | 2 | 0 | 9.5 (5.0) | 2 | 0 |
| Blood Disorder | 11 | 0 | 3.3 (2.0) | 5 | 6 |
| DVT/PE/APS | 6 | 0 | 3.7 (2.7) | 4 | 2 |
| Hematoma/Bleeding | 5 | 0 | 2.8 (0.5) | 1 | 4 |
| Neurology | 9 | 0 | 18.1(20.6) | 4 | 5 |
| ICH | 4 | 0 | 13.0 (11.3) | 2 | 2 |
| CVA | 1 | 0 | 8.0 | 0 | 1 |
| Bell’s Palsy | 1 | 0 | 1.0 | 0 | 1 |
| Polyneuropathy | 2 | 0 | 18.0 (14.1) | 1 | 1 |
| Seizure | 1 | 0 | 66.0 | 1 | 0 |
| Endocrine | 3 | 0 | 3.7 (0.6) | 2 | 1 |
| Thyrotoxicosis | 1 | 0 | 4.0 | 0 | 1 |
| Adrenal Insufficiency | 1 | 0 | 3.0 | 1 | 0 |
| Diabetic Keto Acidosis | 1 | 0 | 4.0 | 1 | 0 |
| Other Immune*** | 4 | 0 | 8.5 (5.7) | 2 | 2 |
| MSK | 4 | 0 | 2.5 (0.6) | 2 | 2 |
Abbreviations: ARDS=Acute respiratory Distress Syndrome; COPD=Chronic Obstructive Pulmonary Disease; ACS=Acute Coronary Syndrome; GI=Gastrointestinal; DVT=Deep Vein Thrombosis; PE=Pulmonary embolism; ICH=Intracranial Hemorrhage; CVA=cerebrovascular Accident; APS=Anti phospholipid antibody syndrome; LOS=Length of Stay; MSK=Musculoskeletal
Total Admissions refers to all elective and emergent or urgent admissions
Others= drug related adverse events, falls, rehab, vaginal delivery
Others Immune= lupus nephritis, inflammatory arthritis, ulcerative colitis and vasculitis
The mean (SD) length of stay for illness not related to SSc was 5.7 (7.1) days. Seven patients died during inpatient stay due to cancer (n=2), infection (n=2), ST elevation MI (n=1), acute respiratory distress syndrome (n=1) and aortic stenosis (n=1; Table 4).
We explored the relationship between SSc manifestations and patient survival. Significantly higher risk of death was observed in hospitalizations due to cardiopulmonary (or PH) than due to any other reasons (HR: 3.4 (95% CI, 1.3, 8.6), P=0.012; Figure 2A); and in hospitalizations due to pulmonary involvement than due to any other reasons (HR: 4.8 (95% CI, 1.7, 13.5), P=0.003; Figure 2 B).
Figure 2:
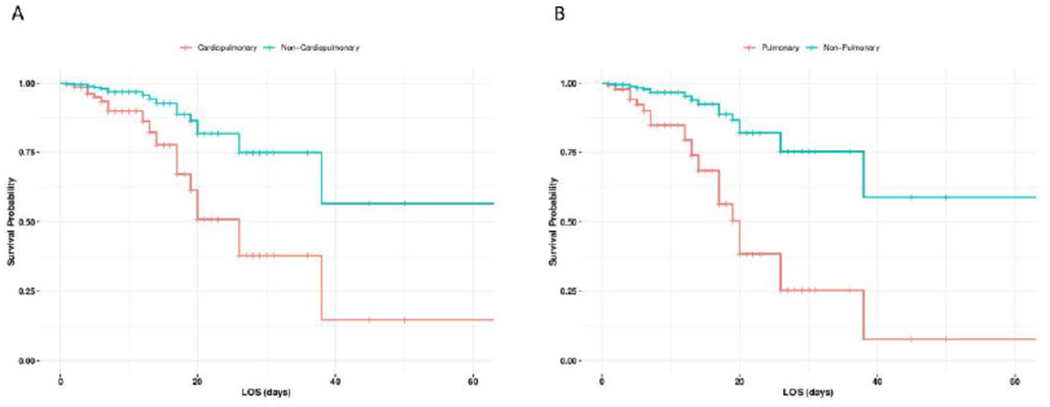
Cox Proportional probability of survival for patients with cardiopulmonary involvement versus no cardiopulmonary involvement (A) or pulmonary involvement versus no pulmonary involvement(B)
Impact of underlying ILD on hospitalization
Among the 484 patients evaluated in this study, 65% had ILD on CT (93% of which were confirmed on high-resolution computed tomography (HRCT)) and 35% had no underlying ILD. A greater proportion of the patients with ILD were hospitalized (122 patients) than those without ILD (60 patients). Patients with underlying ILD were more likely to have dcSSc (56.6% vs 30.0%), anti-topoisomerase antibody (20.2 % vs 1.6%) and more likely to be married (68.6% vs 43.3%; all are statistically significant at p< 0.05).
Of the 634 admissions, 402 (63.4%) encounters were in patients with ILD and 232 (36.6%) were in patients without ILD. Among the 402 admissions in ILD patients, the most common causes of urgent or emergent admissions related to SSc were due to PH (n=28) and cardiac arrhythmias (n=20). For elective admissions for ILD patients, the most common causes were intravenous epoprostenol for digital ischemia (n=39) and chemotherapy/biologics (n=28).
For admissions not related to SSc for ILD patients, respiratory infection (n=27) was the major etiology of hospitalization, followed by malignancy (n=10), while surgery was the major cause of elective admissions (n=29). Of the 17 patients who died during their hospital stay, 11 (65%) had underlying ILD (Table 4).
Impact of demographics and clinical characteristics on number of hospitalizations
We assessed if the number of hospitalizations per patient was influenced by baseline clinical and relevant characteristics, as shown in Table 1. There were 36 patients classified as having multiple hospitalizations (defined as > 4 admissions) and 146 patients as limited hospitalizations. The patients with multiple hospitalizations had lower FVC% (mean FVC 67.5% vs. 76.1%, p < 0.027) and greater proportion of oral prednisone use at baseline (47.2% vs. 22.6%, p=0.003). Use of multiple immunosuppressive therapies at baseline was greater in multiple (>4) hospitalizations 27.8% vs. 15.1%, p= 0.07. Other parameters, including autoantibodies, were not statistically different (data not shown). We also assessed the baseline characteristics as univariate predictors for hospitalization using the logistic regression. In this analysis, anti-topoisomerase antibody negativity (odds ratio =0.44, p=0.002), lower FVC% (odds ratio = 0.99, p=0.005) and DLCO% (odds ratio =0.98%, p=0.001) were predictors of hospitalization.
DISCUSSION
In this retrospective analysis from a large tertiary SSc cohort, we found that 37.6% of SSc patients were hospitalized at the primary institution. The most common causes of urgent or emergent admissions included cardio-pulmonary worsening, GI dysmotility and infections. For elective admissions, the most common reasons were intravenous prostacyclin for digital ischemia, inpatient chemotherapy or biologics therapy, and planned surgeries. Underlying ILD was associated with higher numbers of hospitalization (67%) than those without ILD and the inpatient mortality was 9.3%. In addition, lower FVC%, a surrogate of severe ILD, multiple immunosuppressive therapies, and use of prednisone resulted in a greater number of hospitalizations.
Previous studies have explored the reasons for hospitalizations in SSc patients, and many of the studies have relied on administrative databases, such as National Inpatient Sample (NIS; large publicly available all-payer inpatient healthcare database) [6, 11, 12], due to the rarity of SSc. Chung et al [11] reviewed the NIS database between 2002 and 2003 and found the major reasons for hospitalizations included disorder of the circulatory system (i.e. congestive heart failure, acute myocardial infarction, arrhythmias; 21.9%), gastrointestinal system (12.7%), musculoskeletal system (osteoporosis/fracture and septic arthritis; 12.0%) and respiratory system (11.5%). Amoda et al [5] reviewed admissions with SSc in NIS between 2010 and 2014, and found that a majority of admissions were non-elective (86.2%). Poudel et al [6] reviewed NIS from 2012 to 2013 and found 9,731 hospitalizations in the sample representing an estimated 48,655 hospitalizations nationwide in patients with SSc (0.09%). The most common reasons for hospitalization were infection (17.4%), cardiovascular (15.9%), gastrointestinal (13.3%), musculoskeletal (12.2%), and pulmonary (10.9%) involvement. In an administrative database in Italy, the major reasons for hospitalization included ILD (26.9%), osteoporosis (12.5%), PAH (7.7%), esophageal dysmotility (7.0%), and critical digital ischemia/ulcer (4.9%). Administrative databases are limited as they utilize ICD codes for diagnosis and related complications but are unable to confirm the specific reasons for admission. In addition, NIS database is deidentified and it is not able to capture if patients are being admitted multiple times, which can inflate the percentage of patients that are admitted.
Single center studies can also provide insight on the reasons for hospitalization. In a 13-year study from Iran, Sheenvendah et al [14] identified digital ulcer and ILD as the most common causes of hospitalizations among the SSc-related events with infection being most common in non-SSc related admissions. In a single center study from Thailand [12], hospitalizations were divided equally between SSc-related and non-SSc related events; the most common reasons for hospitalization were PAH (34.3%) and scleroderma renal crisis (11.1%) for SSc-related admissions, and infection (46.5 %) was the most common reason for non-SSc related hospitalizations.
In our current study, the main organ systems for SSc-related admissions included cardiopulmonary and gastrointestinal involvement and were consistent with the data published by Chung et al [11]. The majority of PH hospitalization was due to PAH (Figure 1), which was consistent with the recent publication from our group [16]. The only exception was that our study showed high admissions for digital ischemia (including treatment resistant Raynaud’s phenomenon and digital ulcers), which was not found in the study performed by Chung et al [11]. Intravenous prostacyclin, such as iloprost, for the treatment of peripheral vascular involvement (such as Raynaud’s phenomenon) is approved in Europe and routinely used in practice [17], although it is not yet approved for use in the US. In the US, prostacyclin infusion,such as epoprostenol requires inpatient admission for the treatment of severe digital ischemia due to the lack of coverage by insurance as an outpatient infusion.
For non-SSc related hospitalizations, infections (primarily pulmonary infections) and elective surgeries are leading causes of hospitalizations. Differences in the reasons for hospitalizations among different cohorts may be reflective of site or country specific management, the decade when the data was collected, and whether data collection was from chart review or an administrative database. U-M is a referral center in the mid-western region of the US, where patients are referred for more severe SSc, such as severe digital ischemia or cardio-pulmonary management.
Our analysis revealed an inpatient mortality due to SSc of 9.3%. This is higher than single center (5.0%)[18] and NIS database (5.0 - 8.1%) studies [5, 6, 11], all of which were using US based hospitalization data. In a US single center study from 2001 to 2011, the inpatient mortality was 5.0% with aspiration and lung disease (with or without underlying ILD) as the main reasons for inpatient mortality[6]. This difference may be due to our large referral base, and may explain a somewhat higher inpatient mortality than the NIS database, which represents all SSc-related admissions in US hospitals. The major reasons for mortality at our center included worsening PH and ILD, which has significant burden on healthcare cost [19]. These data are somber since it is standard at our center to proactively screen patients for cardiopulmonary involvement [9, 20] , highlighting a high unmet need in the management of PH and ILD. Changes in FVC% and DLCO should be monitored closely and guide therapeutic decisions as it influences long term survival[8] Our data are consistent with the EUSTAR database [4], where they identified the major causes of mortality as pulmonary fibrosis (35%), PAH (26%), infections (33%), and malignancy (31%). In addition, the causes of inpatient mortality may differ in other countries. In a single center study from Thailand [12], the inpatient mortality was 16.8%, with congestive heart failure as the leading SSc-related cause and bacterial pneumonia as the leading non-SSc cause of mortality. In a study from Iran, Sheenvendah et al [14] found a high in-hospital mortality of 16.5% with a majority of deaths due to ILD and PH, likely related to advanced disease. The higher inpatient mortality seen in the Thailand and Iranian cohorts are related to infections and cardiopulmonary involvement, respectively [12, 14].
The mean LOS for our cohort was 5.5 days for SSc related and 5.7 days for non-SSc related admissions. We observed 22 hospitalization records, during or after which the patient died, and the mean LOS was 13.7 days. The remaining 612 hospitalizations did not end in patient death, and the mean LOS was 5.7 days. Though the event of death might have caused underestimation of LOS because the patient was too sick, the LOS ending in death is still significantly longer than LOS not ending in death (P < .0001). In the NIS database, the mean LOS was 6.6 days [6] and 8.6 days [5] with a range of four to eight days for other studies [13, 14]. At our center, longer mean LOS were associated with renal involvement due to SSc (mean 9.88 days), largely scleroderma renal crisis, whereas non-SSc admissions due to renal involvement were only 3.44 days. Admissions for intravenous prostacyclin had a mean of 4.29 days. Chung et al [11] showed that presence of ILD increased the odds of in-hospital death by 2.63 fold and increased LOS by 7.25%. In the Iranian cohort, older patients had longer LOS in the hospital [14].
The limitations of this study include that it is a single-center study that only included admissions at U-M and may have missed admissions that occurred at other hospitals. Since U-M program is tertiary care program that accounts for patients from Mid-West and parts of Canada, we did not have access to comprehensive discharge summaries or access to electronic medical records from outside hospitals. Additionally, we only reviewed a subset of the patients seen at U-M for SSc, which may represent a practice pattern of the senior author not seen by other providers, such as the use of intravenous prostacyclin for digital ischemia and providing care to sicker patients with cardiopulmonary involvement. As a retrospective chart review no predefined criteria could be used to classify organ dysfunction, however the reason for each hospitalization in the medical records was carefully reviewed by first author in conjunction with the senior author and the best diagnosis that fits the documented medical problem was used to classify organ dysfunction. Another limitation is that the results obtained may be more generalizable to Caucasian SSc patients living in mid-west as the cohort evaluated lacks ethnic diversity.
In summary, SSc continues to have high morbidity and mortality, largely related to internal organ involvement and significant infections. The presence of ILD increased the rate of hospitalizations and mortality in SSc patients, irrespective of primary etiology of hospitalization. Early screening and detection of cardiopulmonary involvement and careful utilization of immunosuppressive therapies will be key in the management of SSc. New therapeutics should focus on reducing toxicity and finding novel pathways, as seen with anti-fibrotic agents, for the treatment of SSc.
Acknowledgments
Grants/Financial Support:
NIH Funded AR063120: Outcomes Research in Rheumatic Diseases (K24)
NIH Funded T32AR007080 Training Grant Supporting Dr. Dave Roofeh
Conflict of Interest:
Dr. Dinesh Khanna: Grant support: NIH, Immune Tolerance Network, Bayer, BMS, Horizon, Pfizer; Consultant: Acceleron, Actelion, Amgen, Bayer, Blade Therapeutics, Boehringer Ingelheim, CSL Behring, Corbus, Cytori, Galapagos, Genentech/ Roche, GSK, Horizon Merck, Mitsubishi Tanabe Pharma, Regeneron, Sanofi-Aventis, and United Therapeutics; CME programs: Impact PH; Stocks: Eicos Sciences, Inc; Leadership/Equity position -Medical lead, Scleroderma Development, CiviBioPharma/Eicos Sciences, Inc.
REFERENCES
- 1.DENTON CP, KHANNA D: Systemic sclerosis. Lancet 2017; 390:1685–1699. [DOI] [PubMed] [Google Scholar]
- 2.NAGARAJA V, CERINIC MM, FURST DE et al. : Current and future outlook on disease modification and defining low disease activity in systemic sclerosis. Arthritis & rheumatology (Hoboken, NJ) 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.KHANNA D, TASHKIN DP, DENTON CP et al. : Etiology, Risk Factors, and Biomarkers in Systemic Sclerosis with Interstitial Lung Disease. Am J Respir Crit Care Med 2020; 201:650–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.TYNDALL AJ, BANNERT B, VONK M et al. : Causes and risk factors for death in systemic sclerosis: a study from the EULAR Scleroderma Trials and Research (EUSTAR) database. Ann Rheum Dis 2010; 69:1809–1815. [DOI] [PubMed] [Google Scholar]
- 5.AMODA O, RAVAT V, DATTA S, SAROHA B, PATEL RS: Trends in Demographics, Hospitalization Outcomes, Comorbidities, and Mortality Risk among Systemic Sclerosis Patients. Cureus 2018; 10:e2628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.RAM POUDEL D, GEORGE M, DHITAL R et al. : Mortality, length of stay and cost of hospitalization among patients with systemic sclerosis: results from the National Inpatient Sample. Rheumatology (Oxford) 2018; 57:1611–1622. [DOI] [PubMed] [Google Scholar]
- 7.NOVIANI M, SAFFARI SE, TAN JL et al. : Mortality and hospitalization outcomes of interstitial lung disease and pulmonary hypertension in the Singapore systemic sclerosis cohort. Semin Arthritis Rheum 2019. [DOI] [PubMed] [Google Scholar]
- 8.BARSOTTI S, ORLANDI M, CODULLO V et al. : One year in review 2019: systemic sclerosis. Clin Exp Rheumatol 2019; 37 Suppl 119:3–14. [PubMed] [Google Scholar]
- 9.ROOFEH D, JAAFAR S, VUMMIDI D, KHANNA D: Management of systemic sclerosis-associated interstitial lung disease. Curr Opin Rheumatol 2019; 31:241–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.ROOFEH D, KHANNA D: Management of systemic sclerosis: the first five years. Curr Opin Rheumatol 2020; 32:228–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.CHUNG L, KRISHNAN E, CHAKRAVARTY EF: Hospitalizations and mortality in systemic sclerosis: results from the Nationwide Inpatient Sample. Rheumatology (Oxford) 2007; 46:1808–1813. [DOI] [PubMed] [Google Scholar]
- 12.NETWIJITPAN S, FOOCHAROEN C, MAHAKKANUKRAUH A, SUWANNAROJ S, NANAGARA R: Indications for hospitalization and in-hospital mortality in Thai systemic sclerosis. Clin Rheumatol 2013; 32:361–367. [DOI] [PubMed] [Google Scholar]
- 13.PIGA M, CASULA L, SANNA S et al. : Population-based analysis of hospitalizations for patients with systemic sclerosis in a West-European region over the period 2001-2012. Rheumatol Int 2016; 36:73–81. [DOI] [PubMed] [Google Scholar]
- 14.SHENAVANDEH S, NASERI R: Assessment of hospitalization and mortality of scleroderma in-patients: a thirteen-year study. Reumatologia 2017; 55:163–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.YOUNG A, VUMMIDI D, VISOVATTI S et al. : Prevalence, Treatment, and Outcomes of Coexistent Pulmonary Hypertension and Interstitial Lung Disease in Systemic Sclerosis. Arthritis & rheumatology (Hoboken, NJ) 2019; 71:1339–1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.JAAFAR S, VISOVATTI S, YOUNG A et al. : Impact of the revised haemodynamic definition on the diagnosis of pulmonary hypertension in patients with systemic sclerosis. Eur Respir J 2019; 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.POPE J, FENLON D, THOMPSON A et al. : Iloprost and cisaprost for Raynaud’s phenomenon in progressive systemic sclerosis. Cochrane Database Syst Rev 2000:CD000953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.SEHRA ST, KELLY A, BAKER JF, DERK CT: Predictors of inpatient mortality in patients with systemic sclerosis: a case control study. Clin Rheumatol 2016; 35:1631–1635. [DOI] [PubMed] [Google Scholar]
- 19.FISCHER A, KONG AM, SWIGRIS JJ, COLE AL, RAIMUNDO K: All-cause Healthcare Costs and Mortality in Patients with Systemic Sclerosis with Lung Involvement. J Rheumatol 2018; 45:235–241. [DOI] [PubMed] [Google Scholar]
- 20.AMJADI SS, ROOFEH D, NAMAS R, KHANNA D: Management of systemic sclerosis-associated interstitial lung disease in the current era. Int J Rheum Dis 2020; 23:137–139. [DOI] [PMC free article] [PubMed] [Google Scholar]


