Abstract
Background:
A large, randomized trial showed no significant difference in survival to discharge between cardiopulmonary resuscitation (CPR) strategies of 30 compressions with pause for 2 ventilations per cycle (30:2) and continuous chest compression with asynchronous ventilations (CCC). Data from the same trial suggested that adherence to the intended CPR strategy was associated with significantly greater survival. We sought to determine the adherence rate with intended strategy and then explore the association of adherence with survival to discharge in the Resuscitation Outcomes Consortium (ROC).
Methods:
This secondary analysis of data from the ROC included three interventional trials and a prospective registry. We modified an automated software algorithm that classified care as 30:2 or CCC before intubation based on compression segment length (defined as the elapsed time from start of compressions to subsequent pause of ≥2 seconds), number of pauses per minute ≥2 seconds in length and chest compression fraction. Intended CPR strategy for individual agencies was based on study randomization (during trial phase) or local standard of care (during registry phase). We defined CPR delivered as adherent when its classification matched the intended strategy. We characterized adherence with intended strategy across trial and registry periods. We examined its association with survival to hospital discharge using multivariate logistic regression after adjustment for Utstein and other potential confounders. Effect modification with intended strategy was assessed through a multiplicative interaction term.
Results:
Included were 26,810 adults with out of hospital cardiac arrest, of which 10,942 had an intended strategy of 30:2 and 15,868 an intended strategy of CCC. The automated algorithm classified 12,276 cases as CCC, 7,037 as 30:2 and left 7,497 as unclassified. Adherence to intended strategy was 54.4%; this differed by intended strategy (58.6% for CCC vs 48.3% for 30:2). Overall adherence was less during the registry phase as compared to during the trial phase(s). The association between adherence and survival was modified by treatment arm (CCC OR: 0.72, 95% CI: 0.64–0.81 vs 30:2 OR: 1.05, 95% CI: 0.90–1.22; interaction p-value<0.01) after adjustment for known confounders.
Conclusion:
For intended strategy CCC, survival was significantly lower, OR (95%CI) = 0.72 (0.64, 0.81), when adhered to while for intended strategy 30:2, survival was higher, OR (95%CI) = 1.05 (0.90, 1.22), when adhered to. Intended strategy of 30:2 had lower adherence rates than CCC possibly a result of being a more difficult strategy to administer.
Keywords: cardiopulmonary arrest, adherence, continuous compressions, 30:2
Introduction
Survival rates from out-of-hospital cardiac arrest (OHCA) remain poor1–3, creating both a challenge and a significant opportunity for improvement. Current consensus is that high quality cardiopulmonary resuscitation (CPR) comprised of adequate chest compressions with minimal interruptions is important to increase chances of survival after OHCA. Previous studies have focused on the association of outcomes with CPR with regards to compression rate, depth and fraction6–10 as well as perishock pause, but none have focused on additional metrics that classify care based on compression and ventilation patterns.
Strategies promoted to increase the quality of CPR have included changes in recommended compression to ventilation ratios. The Resuscitation Outcomes Consortium's (ROC) Trial of Interrupted vs Continuous Compressions (ROC-CCC) did not detect a significant difference in the primary outcome of survival to discharge between two ventilation strategies: the AHA recommended strategy of 30 compressions with a pause for two ventilations (30:2) versus a strategy of continuous compressions (CCC) with asynchronous ventilation given without a pause.5 However, adherence to intended CPR technique may be an important neglected predictor of success. In the same trial, patients resuscitated with CPR performed with measurably good adherence to either the CCC or 30:2 protocol showed significantly higher survival than patients resuscitated with strategy that deviated from the intended protocol. Consistency and adherence to protocol can serve as a broad signal of overall team dynamics, which along with system performance monitoring and quality oversight are associated with improved outcomes.11
We previously developed an automated software algorithm that uses the length of compression segments (stop minus start times) and the pattern of compression pauses (defined as ≥2 seconds) to classify treatment as either 30:2, CCC, or Unclassified (i.e. – not fitting either strategy).12 We have since refined this algorithm after review of unclassified cases in ROC-CCC to better represent and distinguish between the two strategies. In this study, we used this modified algorithm to address two aims: a) Is adherence to an intended strategy associated with improved outcomes? b) How is adherence to an intended strategy affected by the presence or absence of an interventional trial?
Methods
Setting and Design
This is a retrospective analysis of OOHCA patients enrolled in the Resuscitation Outcomes Consortium (ROC) between 2011–2017. During this time, patients were enrolled in either concurrent ROC-CCC and the Amiodarone, Lidocaine, or Placebo Study (ROC-ALPS)13 trials, a Registry or the Pragmatic Airway Resuscitation Trial (PART).14 Institutional Review Boards of participating institutions approved the parent studies under federal Exception from Informed Consent rules (21 CFR 50.24).
For this analysis, patients were classified according to their screening status at the time of their OHCA event. For instance, all patients screened for possible inclusion in ROC-CCC, ALPS or subsequently PART were considered as included in those trials for the purposes of this analysis, regardless of their actual enrollment in the trials themselves. Screening and eligibility criteria for each study have been provided elsewhere.16–19
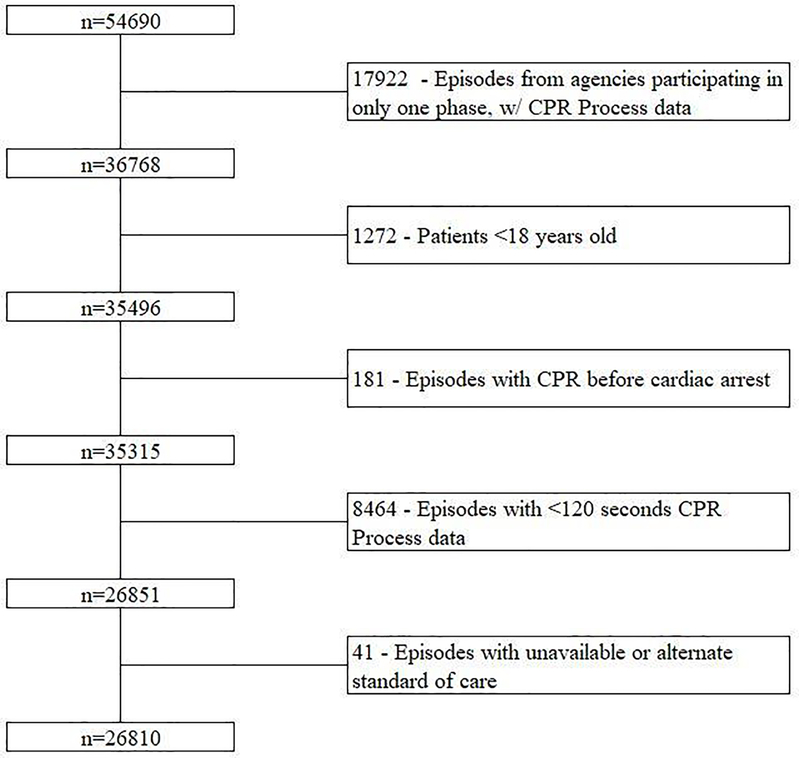
From the total population of 54,690 patients, 35,496 were adults initially treated by an agency that participated in at least two of the three ROC phases (Figure 1). We excluded 181 patients who received EMS compressions prior to the cardiac arrest, 8,464 who had <120 seconds of CPR data (to be consistent with a typical compression cycle) and 41 in whom we were unable to confirm the agency's intended strategy as either CCC or 30:2.
Figure 1.
CONSORT Patient Flow Diagram
Training and Monitoring
Prior to each trial commencement, emergency medical technicians and paramedics received initial and annual refresher training in-person and online. Data quality was monitored by an internal monitoring committee.15
For ROC CCC/ALPS and Registry, trained coordinators at each site reviewed and annotated ECG files from one of three manufacturers' monitor-defibrillators - Zoll M and X series (Zoll, Inc., Chelmsford, MA) which uses an accelerometer; Philips MRX (Philips, Inc., Amsterdam, The Netherlands) which uses an accelerometer and force sensor; or Physio-Control LifePak versions 12, 15 and 1000 (Physio-Control, Inc., Redmond, WA) which uses impedance. Each provided commercially available software to allow for annotation of wavelengths and analysis of chest compression data. ECG files from PART were reviewed by the lead author (RHS) who has more than a decade experience analyzing CPR process data and reviewing ECG files from these three manufacturers.
Measurement of CPR and Adherence
Methods for the automated algorithm are described elsewhere13 and were further refined for the current study to better represent the compression patterns of each CPR strategy. In brief we calculated three metrics for each patient – median compression segment length, defined as the number of seconds between the start of compressions and the first subsequent pause ≥2 seconds; the number of pauses per minute ≥2 seconds in length; and compression fraction, defined as the ratio of time during which compressions were being provided. Target ranges for each strategy were calculated assuming providers performed ideal compression patterns and rates consistent with contemporaneous AHA guidelines. Cases were classified as CCC or 30:2 if they met at least two of the three metrics for either arm, as defined in Table 1. In a convenience sample of cases from the ROC-CCC trial, this algorithm had good agreement with manual review by research coordinators (κ = 0.84).13
Table 1:
Classification Algorithm Criteria
| Updated Algorithm | Criteria for CCC | Criteria for 30:2 |
| Overall chest compression fraction | 0.80 – 0.98 | 0.60 – 0.85 |
| Median chest compression segment length (sec) | 90 – 150 | 10 – 25 |
| Chest compression pauses per minute | 0.25 – 1.0 | 1.5 – 4.0 |
| Original Algorithm | Criteria for CCC | Criteria for 30:2 |
| Overall chest compression fraction | 0.80 – 1.0 | 0.60 – 0.80 |
| Median chest compression segment length (sec) | 60 – 150 | 0 – 20 |
| Chest compression pauses per minute | 0 – 1 | 2 – 4 |
Compression rate and depth were not included as specific metrics in this study when distinguishing 30:2 from CCC. Both metrics are a reflection of overall quality CPR regardless of intended strategy and would not be expected to differ between CCC and 30:2.
Depending on trial and registry participation, intended CPR strategy was either protocolized or clinically adopted as part of the resuscitation practice at each agency. To be consistent with the respective intervention period, metrics were calculated during the first six minutes for ROC-CCC patients and prior to placement of the advanced airway for all others. A patient received adherent care if the algorithm classified care was consistent with the intended CPR strategy.
Statistical methods
Patient and EMS treatment characteristics were compared by intended strategy. Adherence rates were aggregated within agencies stratified by intended strategy and plotted across ROC phase (i.e., trial vs. registry). Survival to hospital outcome was stratified by adherence.
The relationship between adherence and survival to hospital discharge was examined via multivariate logistic regression after adjustment for intended CPR strategy, sex (male vs. female), age, initial EMS rhythm (Ventricular tachycardia/Ventricular fibrillation, Pulseless electric activity, Asystole, Other), witnessed status (EMS, bystander, not witnessed), bystander CPR (yes, no), time from dispatch call to first agency arrival and regional site because of the previously known association with outcome in the ROC datasets. When further stratified by intended strategy, unadjusted survival rates differed by adherence. As part of a posteriori analysis, we then added an adherence*intended strategy interaction term to check for effect modification..
CPR characteristics for patients that were unclassified by the algorithm were stratified by survival status and intended strategy. Survival was compared within intended strategy by the number of individual metrics met.
Analysis were performed in R v3.5.1 (R Core Team, Vienna, Austria).
Results
Of the 26,810 patients who were included in this analysis 10,942 (40.8%) had an intended CPR strategy of 30:2 and 15,868 (59.2%) had an intended CPR strategy of CCC. Across the two intended compression strategies, patients significantly differed in witness status and bystander CPR status (both p < 0.05, Table 2). Expectedly, patients with intended CCC strategy had higher mean CCF (0.87 vs 0.80), higher median compression segment length (83.2 sec vs 42.8 sec) and lower number of pauses per minute (0.7 vs 1.3) compared to those with intended 30:2 strategy.
Table 2.
Baseline and CPR Characteristics by Intended CPR strategy
| Intended 30:2 | Intended CCC | |
|---|---|---|
| Patient Characteristics | ||
| n | 10942 | 15868 |
| Sex, n (%) | ||
| Male | 6904 (63.1) | 10075 (63.5) |
| Female | 4033 (36.9) | 5777 (36.4) |
| Unknown | 5 (0.0) | 16 (0.1) |
| Median Age (IQR) | 65 (54, 78) | 66 (54, 78) |
| Witness Status, n (%) | ||
| EMS | 1203 (11.0) | 1548 (9.8) |
| Bystander | 3914 (35.8) | 5817 (36.7) |
| Not witnessed | 5313 (48.6) | 8054 (50.8) |
| Unknown | 512 (4.7) | 449 (2.8) |
| Bystander CPR, n (%) | ||
| Yes | 4622 (42.2) | 7336 (46.2) |
| No | 6129 (56.0) | 8089 (51.0) |
| Unknown | 191 (1.7) | 443 (2.8) |
| Initial Rhythm, n (%) | ||
| VT/VF | 2282 (20.9) | 3435 (21.6) |
| Asystole | 2722 (24.9) | 3807 (24.0) |
| PEA | 5557 (50.8) | 8007 (50.5) |
| No Shock | 326 (3.0) | 540 (3.4) |
| Unknown | 55 (0.5) | 79 (0.5) |
| Time from Dispatch to Arrival (minutes), mean (sd) | 5.5 (2.5) | 5.8 (3.4) |
| CPR Characteristics | ||
| Chest Compression Fraction | ||
| Mean (sd) | 0.80 (0.12) | 0.87 (0.10) |
| CCF < 0.60, n (%) | 587 (5.4) | 400 (2.5) |
| 0.60 ≤ CCF < 0.70, n (%) | 1189 (10.9) | 591 (3.7) |
| 0.70 ≤ CCF < 0.80, n (%) | 2999 (27.4) | 1778 (11.2) |
| 0.80 ≤ CCF < 0.90, n (%) | 4120 (37.7) | 5815 (36.6) |
| 0.90 ≤ CCF ≤ 1.0, n (%) | 2047 (18.7) | 7284 (45.9) |
| Median Compression Segment Length (seconds) | ||
| Mean (sd) | 42.8 (42.0) | 83.2 (64.4) |
| Pauses per minute | ||
| Mean (sd) | 1.3 (0.7) | 0.7 (0.4) |
| Algorithm Classification | ||
| CCC, n (%) | 2977 (27.2) | 9299 (58.6) |
| 30:2, n (%) | 5290 (48.3) | 1747 (11.0) |
| Unclassified, n (%) | 2675 (24.4) | 4822 (30.4) |
IQR = Interquartile Range; sd = standard deviation; VT/VF = Ventricular Tachycardia/Ventricular fibrillation; PEA = Pulseless electric activity; CCF = Chest Compression Fraction
Adherence
Using the automated algorithm, 12,276 (45.8%) were classified as CCC, 7,037 (26.2%) were classified as 30:2 and 7,497 (28.0%) were unclassified. Overall adherence to the intended CPR strategy was 54.4%. When stratified by intended CPR strategy, adherence was 58.6% for CCC and 48.3% for 30:2. Compared to CCC/ALPS, agency specific adherence rates decreased during the Registry period for agencies with an intended strategy of 30:2 (agency mean 60.0% vs 47.4%) and increased for intended strategy CCC (agency mean 55.6% vs 64.8%) (Appendix Figure 1a). For the subset of agencies that participated in PART, adherence rates were higher in PART than original CCC/ALPS levels for both intended strategy CCC (CCC/ALPS: 58.1% - Registry: 50.4% - PART: 64.8%) and 30:2 (33.4%-12.6%-38.8%) after a decrease during Registry (Appendix Figure 1b).
Survival
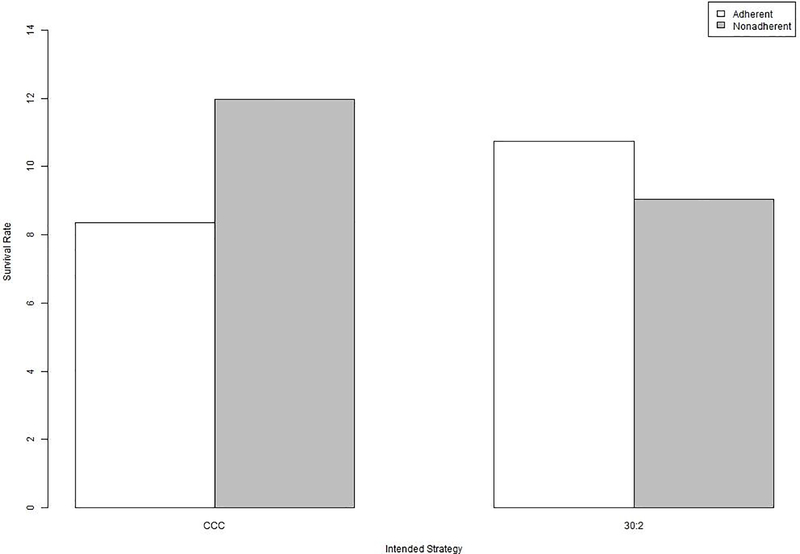
Unadjusted survival to hospital discharge was lower, OR (95% CI) = 0.86 (0.79, 0.93), when there was adherence to the intended CPR strategy. However, the association of survival with adherence was modified by intended strategy (CCC OR: 0.72, 95%CI: 0.64 – 0.81, 30:2 OR: 1.05, 95% CI: 0.90 – 1.22; interaction p-value<0.01, Table 3 and Figure 2) after adjustment for known confounders including site.
Table 3. –
Adjusted Logistic Regression Estimates for Survival to Hospital Discharge
| 95%CI | |
|---|---|
| Adherent via algorithm | 1.05 (0.90, 1.22) |
| Intended CPR strategy | |
| 30:2 | Reference |
| CCC | 1.20 (1.04, 1.38) |
| Adherent*Intended CCC | 0.69 (0.57, 0.83) |
| Sex | |
| Female | Reference |
| Male | 0.96 (0.87, 1.07) |
| Age | 0.97 (0.97, 0.98) |
| Witness Status | |
| Not witnessed | Reference |
| EMS | 3.20 (2.70, 3.79) |
| Bystander | 2.36 (2.10, 2.65) |
| No Bystander CPR | Reference |
| Bystander CPR | 1.30 (1.17, 1.45) |
| Initial Rhythm | |
| VT/VF | Reference |
| PEA | 0.26 (0.23, 0.29) |
| Asystole | 0.06 (0.05, 0.07) |
| No Shock | 0.14 (0.10, 0.21) |
| Arrival Time (min) | 0.92 (0.90, 0.94) |
| Site A | Reference |
| Site B | 1.50 (1.24, 1.81) |
| Site C | 1.57 (1.21, 2.04) |
| Site D | 1.99 (1.58, 2.52) |
| Site E | 2.11 (1.80, 2.48) |
| Site F | 1.31 (1.10, 1.54) |
| Site G | 2.96 (2.55, 3.44) |
| Site H | 0.70 (0.46, 1.08) |
VT/VF = Ventricular Tachycardia/Ventricular fibrillation; PEA = Pulseless electric activity
Figure 2.
Survival estimates by strategy and adherence
Within the subgroup of cases with nonadherent care, survival was nearly double for intended strategy CCC cases classified as 30:2 (12.1%) compared to intended strategy 30:2 cases classified as CCC (6.9%). Unclassified cases that met zero metrics on either arm had a survival of 6.6%.
Within the subgroup of nonadherent intended strategy CCC cases, those that met at least one 30:2 metric had higher survival (13.6%) than those that met no 30:2 metrics (10.0%).
Discussion
Our analysis demonstrates that when adhered to, intended strategy CCC had significantly lower survival OR (95%CI) = 0.72 (0.64, 0.81) while intended strategy 30:2 had higher survival, OR (95%CI) = 1.05 (0.90, 1.22). Although unadjusted survival rates were not significantly different between the two intended CPR strategies (both 9.9%), when considered in context of adherence (a potential reflection of quality care), survival differed according to adherence to the intended CPR strategy.
While survival was higher with adherence to 30:2 our analysis suggests that this strategy had lower adherence rates than CCC. In almost all situations, nonadherence was due to infrequent resuscitation encounters (i.e. - medics on average treated only 1–2 cardiac arrests a year), confusion over the intended strategy or a chaotic scene. This finding held even during the Registry period during which 30:2 adherence decreased, suggesting that the protocolized crossing over of strategies was not its main cause. One reason why adherence for CCC increased over time might be that it is simpler than 30:2 to remember and administer consistently and mimics how ventilation is practiced after placement of an advanced airway.
Notably, the higher survival observed with nonadherence to CCC may have been due to due to a quarter of those cases having actually received 30:2. This study subgroup had a survival rate which was almost double that of cases intended for 30:2 cases who actually received CCC (12.1% vs 6.9%). In addition, within the set of nonadherent CCC cases that were unclassified, the 80% that met at least one 30:2 metric had a higher survival (13.6%) than the 20% that met no 30:2 metrics (10.0%).
These survival results warrant careful interpretation. The finding that when adhered to, the 30:2 strategy is associated with greater survival may be driven by the presence of pauses for ventilation which some have suggested result in less alveolar damage than asynchronous ventilation in CCC.20 Even when 30:2 is not strictly adhered to our analysis suggests that more frequent pauses for breaths (i.e. every 60 seconds compared to 90 or 120 seconds) are associated with better outcome.
In the future, care providers and their agencies may benefit from feedback on how well their CPR strategy was completed in addition to individual metrics like rate, depth or fraction. Regular training to reinforce these metrics has the potential to improve resuscitation outcome.
Use of an automated software algorithm, such as the one employed for this study, may enhance review of resuscitations for compliance with a specific CPR protocol. The modified automated software algorithm provides functionality to review a large number of files rapidly, but manual review of ECG files may remain important. In the ROC-CCC trial, coordinators classified care as either 30:2 or CCC at a rate of 50% higher than the algorithm (and showed similar higher survival rates for 30:2).5 This suggests that there may be other factors influencing our findings. Specifically, aggregating data may miss characteristics of individual compressions segments. Future research is needed to determine the sensitivity and specificity of this automated algorithm. Inclusion of such an algorithm in ECG software may provide a mix of objective data while also allowing for subjective review.
Our study had several strengths, beginning with the large sample size that spanned over 50 diverse agencies from the US and Canada. Access to ECG files was unprecedented and for PART, adherence to intended strategy data are being reported for the first time. Conversely, the study has some limitations. First, multiple devices by multiple manufacturers were used across agencies, so there was inherent variability in measurement. Second, reasons for pauses in compressions were not annotated thus limiting the ability to account for pauses due to reasons other than CPR strategy. Third, since the ROC-CCC trial was randomized by cluster, there may have been a carryover effect upon crossover that could explain some adherence challenges. Fourth, we did not have ventilation measures in which to monitor quality. Finally, we excluded nearly ¼ of eligible cases due to limited CPR Process measures (e.g. < 120 seconds).
Conclusion
For intended strategy CCC, survival was significantly lower, OR (95%CI) = 0.72 (0.64, 0.81), when adhered to while for intended strategy 30:2, survival was higher, OR (95%CI) = 1.05 (0.90, 1.22), when adhered to. Intended strategy of 30:2 had lower adherence rates than CCC possibly a result of being a more difficult strategy to administer.
Supplementary Material
Appendix Figure 1. Agency Adherence over Trial Periods
A) – Agencies participating in ROC CCC or ALPS and Registry
B) – Agencies participating in ROC CCC/ALPS, Registry and PART
Table 4.
CPR Measures of Nonadherent Care by Survival Status
| Intended strategy 30:2 |
Intended strategy CCC |
|||
|---|---|---|---|---|
| Died | Survived | Died | Survived | |
| N | 5621 | 619 | 6049 | 879 |
| Pause per minutes, mean (sd) | 0.80 (0.43) | 0.84 (0.47) | 1.01 (0.68) | 1.05 (0.62) |
| Median compression segment length, mean (sd) | 71.2 (52.0) | 61.2 (48.7) | 74.8 (99.3) | 52.6 (62.7) |
| CCF, mean (sd) | 0.85 (0.13) | 0.81 (0.17) | 0.82 (0.13) | 0.78 (0.16) |
| Metrics met, n (%1) | ||||
| 2 of opposite strategy | 2761 (93.1) | 204 (6.9) | 1521 (87.9) | 210 (12.1) |
| 1 of opposite strategy only | 608 (90.3) | 65 (9.7) | 658 (86.0) | 107 (14.0) |
| 1 of intended strategy only | 537 (87.9) | 74 (12.1) | 1504 (88.9) | 187 (11.1) |
| 1 of each strategy | 1116 (87.9) | 153 (12.1) | 1563 (86.6) | 242 (13.4) |
| Zero of either strategy | 101 (88.6) | 13 (11.4) | 493 (93.4) | 35 (6.6) |
– Percentages are calculated across rows and represent survival rates
Acknowledgements
This study was supported by grant 5R21HL145423-02 from National Heart Lung and Blood Institute. The Resuscitation Outcomes Consortium institutions participating in the studies were supported by a series of cooperative agreements from the NHLBI, including 5U01 HL077863 (University of Washington Data Coordinating Center), HL077866 (Medical College of Wisconsin), HL077867 (University of Washington), HL077871 (University of Pittsburgh), HL077873 (Oregon Health and Science University), HL077881 (University of Alabama at Birmingham), HL077885 (Ottawa Health Research Institute), and HL077887 (University of Texas Southwestern Medical Center/Dallas). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung and Blood Institute or the National Institutes of Health. The NHLBI did not have any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Conflicts of Interest:
Robert Schmicker, Peter Kudenchuk, Jim Christenson, Christian Vaillancourt, Henry Wang and Mohamud Daya reported no conflicts.
Tom Aufderheide is the site Principal Investigator of the Milwaukee site for the ROC grant.
Ahamed Idris has research grants from the National Institutes of Health and the Center for Disease Control and Prevention. He is an unpaid volunteer of the American Heart Association National Emergency Cardiovascular Care Committee and an unpaid volunteer of the Clinical Advisory Board for Stryker Belfast, Northern Ireland.
Graham Nichol reported the following conflicts: Salary support from Leonard A Cobb~ Medic One Foundation Endowed Chair in Prehospital Emergeny Care, University of Washington; Consultant and Research Contract, ZOLL Circulation Inc. San Jose, CA; Consultant, Acute Care Program, General Electric Health Care Inc., Chicago, IL and Roche Inc., Chicago, IL; Consultant, Kestra Medical Technologies, Kirkland, WA; Research Contract, ZOLL Medical Inc., Chelmsford, MA; Research Contract, Abiomed Inc., Danvers, MA. Research Contract, General Electric Health Care Inc., Chicago, IL.
Footnotes
Access to data and data analysis
Robert Schmicker had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Centers for Disease Control and Prevention. 2014. Cardiac Arrest Registry to Enhance Survival (CARES) National Summary Report. 2014. https://mycares.net/sitepages/uploads/2015/2014%20Non-Traumatic%20National%20Summary%20Report.pdf. Accessed June 1, 2020.
- 2.Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zive DM, Schmicker R, Daya M, et al. Survival and variability over time from out of hospital cardiac arrest across large geographically diverse communities participating in the Resuscitation Outcomes Consortium. Resuscitation. 2018;131:74–82. [DOI] [PubMed] [Google Scholar]
- 4.Kleinman ME, Brennan EE, Goldberger ZD, et al. Part 5: Adult Basic Life Support and Cardiopulmonary Resuscitation Quality: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132:S414–S435 [DOI] [PubMed] [Google Scholar]
- 5.Nichol G, Leroux B, Wang H, et al. Trial of Continuous or Interrupted Chest Compressions during CPR. N Engl J Med. 2015;373:2203–2214. [DOI] [PubMed] [Google Scholar]
- 6.Lipowicz AA Cheskes S, Gray SH et al. Incidence, outcomes and guideline compliance of out-of-hospital maternal cardiac arrest resuscitations: A population-based cohort study. Resuscitation. 2018;132:127–132. [DOI] [PubMed] [Google Scholar]
- 7.Sutton RM, Reeder RW, Landis W, et al. Chest compression rates and pediatric in-hospital cardiac arrest survival outcomes. Resuscitation. 2018;130:159–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheskes S, Schmicker RH, Rea T, et al. The association between AHA CPR quality guideline compliance and clinical outcomes from out-of-hospital cardiac arrest. Resuscitation. 2017;116:39–45. [DOI] [PubMed] [Google Scholar]
- 9.Idris AH Guffey D, Pepe PE, et al. Chest compression rates and survival following out-of-hospital cardiac arrest. Crit Care Med. 2015;43:840–848. [DOI] [PubMed] [Google Scholar]
- 10.Stiell IG, Brown SP, Christenson J, et al. What is the role of chest compression depth during out-of-hospital cardiac arrest resuscitation?. Crit Care Med. 2012;40:1192–1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dyson K, Brown SP, May S, et al. Community lessons to understand resuscitation excellence (culture): Association between emergency medical services (EMS) culture and outcome after out-of-hospital cardiac arrest. Resuscitation. 2020. November;156:202–209. [DOI] [PubMed] [Google Scholar]
- 12.Wang HE, Schmicker RH, Herren H et al. Classification of cardiopulmonary resuscitation chest compression patterns: manual versus automated approaches. Acad Emerg Med. 2015;22:204–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kudenchuk PJ, Brown SP, Daya M, et al. Amiodarone, Lidocaine, or Placebo in Out-of-Hospital Cardiac Arrest. N Engl J Med. 2016;374:1711–1722. [DOI] [PubMed] [Google Scholar]
- 14.Wang HE, Schmicker RH, Daya MR, et al. Effect of a Strategy of Initial Laryngeal Tube Insertion vs Endotracheal Intubation on 72-Hour Survival in Adults With Out-of-Hospital Cardiac Arrest: A Randomized Clinical Trial. JAMA. 2018;320:769–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schmicker RH, Nichol G, Callaway CW, Cheskes S, Sopko G, Wang HE. Study Monitoring in Emergency Care Trials: Lessons from the Resuscitation Outcomes Consortium Continuous Chest Compressions Trial. Acad Emerg Med. 2019. October;26:1152–1157. [DOI] [PubMed] [Google Scholar]
- 16.Brown SP, Wang H Aufderheide TP, et al. CCC methods A randomized trial of continuous versus interrupted chest compressions in out-of-hospital cardiac arrest: rationale for and design of the Resuscitation Outcomes Consortium Continuous Chest Compressions Trial. Am Heart J. 2015. March;169:334–341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kudenchuk PJ, Brown SP, Daya M, et al. Resuscitation Outcomes Consortium-Amiodarone, Lidocaine or Placebo Study (ROC-ALPS): Rationale and methodology behind an out-of-hospital cardiac arrest antiarrhythmic drug trial. Am Heart J. 2014. May;167:653–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang HE, Prince DK, Stephens SW, et al. Design and implementation of the Resuscitation Outcomes Consortium Pragmatic Airway Resuscitation Trial (PART). Resuscitation. 2016. April;101:57–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morrison LJ, Nichol G, Rea TD, et al. Rationale, development and implementation of the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Resuscitation. 2008. August;78:161–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jo S, Lee JB, Jin YH. Continuous or Interrupted Chest Compressions during CPR. N Engl J Med. 2016. March 24;374:1194–5. [DOI] [PubMed] [Google Scholar]
- 21.Hallstrom A, Rea TD, Sayre MR, et al. Manual chest compression vs use of an automated chest compression device during resuscitation following out-of-hospital cardiac arrest: a randomized trial. JAMA. 2006. June 14;295:2620–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix Figure 1. Agency Adherence over Trial Periods
A) – Agencies participating in ROC CCC or ALPS and Registry
B) – Agencies participating in ROC CCC/ALPS, Registry and PART