Abstract
Cervical cancer is one of the commonest cancers afflicting women in low and middle income countries (LMIC), however both primary prevention with HPV vaccination, and secondary prevention with screening programs and treatment of pre-invasive disease are possible. A coordinated approach to eliminating cervical cancer, as has been called for by the World Health Organization, requires a complex series of steps at all levels of a health system. This article outlines the current state of cervical cancer prevention in LMIC, the innovations being employed to improve outcomes, and consideration of the next steps needed as we move towards global elimination.
Background
Cervical cancer contributes significantly to the burden of noncommunicable disease in low and middle income countries (LMIC). While cervical cancer is a preventable disease through human papillomavirus (HPV) vaccination and screening programs for pre-cancerous lesions, it continues to be one of the commonest cancers afflicting women in LMIC, and is the leading cause of death amongst women in 42 LMIC(1).
Since the mid 20th century, cervical cancer screening has resulted in a significant decline in cervical cancer cases and mortality in high income countries, while LMIC continue to struggle to see similar gains((2)1). A coordinated approach to the elimination of cervical cancer, as has been called for by the World Health Organization (WHO), requires a complex series of steps at all levels of a health system, and innovative approaches are needed to achieve this in LMIC. The global call to action outlines that by 2030, countries need to meet the “90-70-90” targets to achieve cervical cancer elimination; that is that 90% of girls are fully vaccinated against HPV vaccine by the age of 15, 70% of women are screened at 35 and 45 years of age, and 90% of those with a precancerous lesion are treated(3).
The mainstays of cervical cancer elimination are primary prevention with HPV vaccination, and secondary prevention with screening programs and treatment of pre-invasive disease. The HPV vaccine first became commercially available in the early 2000’s and implementation has resulted in reductions in HPV driven diseases, particularly in high income countries(4). Access to the HPV vaccine in LMIC ranges from small studies and implementation projects to coordinated national programs(5). Alongside HPV vaccination, screening programs for pre-malignant cervical lesions remain critical to the efforts to eliminate cervical cancer. Such programs in LMIC are hampered by organizational challenges, resource limitations, lack of cost-effectiveness and health service constraints(6, 7). Following on from HPV vaccination and cervical screening, women in LMIC must have adequate and safe access to treatment of pre-malignant lesions if elimination of the disease is ever to be achieved. Indeed, as noted, “screening alone has no intrinsic preventive value. It is only when a positive test result is linked to treatment that disease prevention can occur”(8).
This article outlines the current state of cervical cancer prevention in LMIC, the technological innovations being employed in the process, and consideration of the next steps needed as we move towards global elimination of this entirely preventable disease.
Cervical cancer prevention
Primary Prevention: Vaccination
The Gardasil® quadrivalent HPV vaccine (covering HPV types 16, 18, 6 and 11) was initially licenced for use in 2006, followed by the bivalent (HPV 16 and 18) Cervarix ® vaccine, with the Gardasil9® nonavalent vaccine (with the addition of HPV types 31, 33, 45, 52 and 58) being introduced into the market in 2018(9). Initial vaccine schedules were generally three doses of the quadrivalent vaccine, however subsequent evidence pointing to the efficacy of fewer doses (10, 11) has led most national programs and WHO to recommend a two dose regimen(12), which is likely to contribute to the ability to achieve vaccine coverage in LMIC. Moreover, analysis of the combined data from two large double blinded randomized controlled trials (the Costa-Rica Vaccine trial and the PApilloma TRIal against Cancer In young Adults (PATRICIA trial)) demonstrated that even a single dose of bivalent (16/18) vaccine conferred efficacy similar to a three dose regimen(13). This is particularly critical given the current shortage of available vaccines prevents global scale up to the level recommended by WHO. Moreover from a implementation perspective, single dose vaccinations reduce the overall reliance on the cold chain, as well as make the logistics of school and community based immunization programs more achievable(14). To that end, the Single-Dose HPV Vaccine Evaluation Consortium has been formed by eight global health and research organizations to “collate and synthesize existing evidence and evaluate new data about a potential single dose HPV vaccination schedule”(15).
As of October 2019, 98 countries have introduced HPV vaccinations into their immunization programs in some form(16). Achievable and sustainable HPV vaccination goals are critical to the elimination of cervical cancer and research must continue to focus on innovative ways to sustain implementation and coverage of vaccination programs, which may include variable school and community based strategies relevant to the local context(14). This is critical when, for example, it is estimated that less than 2% of a targeted population in Africa have been vaccinated with a single dose(17), which is in stark contrast to the coverage of (at least) single dose vaccination in other regions such as Australia (>80%)(18), the US (>60%)(19), Canada (>45%)(20), Mexico (80%)(21), Brazil (45%)(22), the United Kingdom (>85%)(23), and France (>30%)(24). While there are LMIC who have rolled out HPV vaccination as a standard part of the national schedule (e.g. Rwanda(25) and South African school based programs(26)) and those that have achieved partial vaccination(27), a review of clincaltrials.gov reveals that vaccine based clinical trials continue in several LMIC, mainly China, India and Latin America, many of which are implementation trials, highlighting the steps still to be taken in LMIC to achieve vaccine coverage.
Delivery of HPV vaccination programs in LMIC is complex, especially when one considers that some high income countries have also failed to achieved adequate coverage. This is no more evident than in Japan, where despite initial financial and in principle support for the vaccine, media reports of adverse effects and a large social media campaign against the vaccine ultimately led to the withdrawal of government support, further solidifying the community push back and ultimately resulting in very low immunization rates (<4%)(28). Similar challenges have been noted with the introduction of vaccination in LMIC, such as that seen in Colombia, where a mass psychogenic reaction in one town resulted in a drop in projected vaccine coverage from nearly 90% to 5%(29). Addressing such social and cultural barriers to the uptake of HPV vaccination will continue to form an important component of program roll out and sustainability in LMIC.
Of the 137 countries who report an Essential Medicines List, only 30 (22%) list HPV vaccination on that list(30). In some LMIC, HPV vaccination competes with other additions to the vaccination schedule (e.g. rotavirus) in terms of both allocation of finances and the capacity to meet the human resource needs of such programs(27). These are two very significant hurdles to vaccine implementation, and coordinated involvement of both country Ministries of Health as well as national immunization teams are critical to the success of any program(31). Overcoming those barriers has however been proven achievable, demonstrated most eloquently by Rwanda. Despite being one of the lowest income countries in the world, community and government leadership, in addition to manufacturer support and widespread social mobilisation lead to the immunization of more than 96% of eligible girls when the country’s vaccination program was first rolled out(25). Many LMIC have several of the infrastructure needs in place already, and the commitment to build upon this to achieve HPV vaccination is strong. For example in Tunisia, both existing vaccination rates as well as school attendance near 100% and so the professional society of obstetricians and gynecologists are vocal in their advocation that HPV vaccination can be achieved(32). It is clear that stakeholder support, the need for initial funding, steady supply of vaccines, capacity of the health system to deliver a new vaccine, and population acceptance must all be met in order to achieve acceptable national vaccination coverage.
Secondary Prevention: Screening
Secondary prevention of cervical cancer is initiated with screening, whereby women undergo one of three methods of detection of potential cervical pre-malignant pathology. Screening, has traditionally been performed with a cytological assessment of a cervical smear, obtained by a health care provider after direct visualization of the cervix through a speculum. In high-income settings, cytological screening is increasingly being replaced with screening for HPV DNA or mRNA, which can be done on clinician obtained (cervical or vaginal) or woman self-obtained (vaginal) samples. Finally, and common in LMIC, is (naked eye) visual inspection with acetic acid (VIA) or visual inspection with Lugol’s iodine (VILI), whereby the relevant solution is applied to the cervix and the topographic changes of potential pre-malignant lesions are observed. Each of these screening methods have challenges in LMIC with regards to implementing and maintaining programs and with the follow-on effect that women with a diagnosis of cervical cancer may then not have access to adequate treatment(33).
Traditional screening with a Papanicolaou (Pap) smear and cytological assessment has been a large component of reducing cervical cancer in high income countries, however in LMIC this approach is limited by the need for complex human, physical and system resources which can often not be met(34). While guidelines for high income countries recommend cervical cancer screening 2–5 yearly (in order to counter the low sensitivity of cytological based screening) over a woman’s at risk lifetime(35), the capacity to deliver such frequent screening in LMIC is limited. Moreover WHO now recommends screening with a HPV or VIA over the strategy of cytology based screening in LMIC(36).
HPV based screening has several advantages over cytological screening, including improved sensitivity, consequent capacity to increase the interval between tests, no need for highly trained cytopathologists, and ability for a rapid point of care result(37). Moves towards HPV-based screening in LMIC may overcome some of the constraints associated with traditional cytological screening, although the need still remains for adequate technology, physical, financial and human resources, patient acceptance and coordinated programs for implementation(38).
Implementing HPV DNA screening requires finances (there is often a high per-test cost) and infrastructure that may be limiting(38, 39), and this issue has led to rapid and resource conserving tests being developed for use in LMIC. The Xpert HPV assay (GeneXpert; Cepheid, Sunnyvale, CA) completes HPV testing in an hour(40), and the careHPV (QIAGEN, Gaithersburg, MD, USA) test returns a result for 14 strains of HPV in 2.5 hours, notably without the need for running water or electricity (powered by dry cell batteries) (39). This point of care testing has been evaluated in several LMIC and has a sensitivity in these settings of (81.%% – 88.9%) and specificity of (80% – 91.6%), which is comparable to more intensive HPV DNA laboratory based tested (91% and 84%)(41–43). In addition, HPV testing has the added benefit of allowing self-collected specimens for screening. Regardless of the test used, HPV testing still needs a complex series of steps at the infrastructure level, sample collection, and execution of the test to work in coordination, and this can fail at any point along the way(44). However, with more rapid HPV tests being developed which are increasingly simple to execute, the capacity to achieve screening in LMIC with HPV testing is increasingly likely. For example, the HPV AmpFire™ test can return results on 94 specimens in one hour, and the specimens and reagents can be stored at room temperature, minimizing the infrastructure requirements.
Due to the challenges associated with HPV and cytological based screening approaches, the majority of LMICs use visual inspection of the cervix after application of acetic acid (VIA) as their method of screening(45). In addition to being low-cost(34), it has the added benefit of being able to provide an instant result, which can be followed by immediate treatment (so called “screen and treat”), including in HIV positive women(46). The sensitivity of VIA screening in primary care settings in LMIC was described in detail in the 90’s, including in a seminal trial of more than 10000 women, where the sensitivity of the test was shown to be 76.7% and it was apparent that this was a useful tool in cervical cancer prevention in LMIC(47). It is however hampered by high interobserver variability and lack of reproducibility(29), and, despite the initial trial, the sensitivity of the test is reported in other studies to be as low as 50%(48), so while it is inexpensive to administer, the over treatment of non-pathological lesions does not necessarily make it a cost-effective approach. That said, the ultimate cost of having no screening program or access to treatment may be greater, and the potential harms from overtreatment in this setting are likely minimal(49). Equally problematic is the fact that access to treatment of a VIA positive lesion may not be possible, which potentially also limits the utility of VIA as a screening test in many LMIC. However, comprehensive programs that deliver screen and treat have been demonstrated as feasible in LMIC, largely driven by engagement with local providers and available financial and political resources(50, 51), and lessons learned from these programs needs to be considered in implementing prevention strategies that link screening and treatment.
Despite increasing coverage of the HPV vaccine in LMIC, there remains a very current need for adequate screening (and treatment) programs, particularly for the millions of unvaccinated, HPV exposed women(38). There is clearly a complex interplay between HPV vaccination and screening given that the eventual symbiotic relationship that increasing vaccination has with decreasing the burden of treatment resulting from screening must compete right now with the need for both increased vaccination and increased screening of differing populations. In fact, El-Zein and colleagues argue that with increasing HPV vaccination coverage, there may come a time when the risks of screening outweigh the benefits(52), but we are not there yet. Approaches to developing screening programs in LMIC must consider the needs of millions of women right now as well as the evolution of the disease distribution with increasing HPV vaccination in their planning(35) and innovative models of addressing these needs concurrently are needed. A prime example is in Peru, where researchers have developed a “mother / child screen, treat and vaccinate” program, whereby the children and grandchildren of women presenting for cervical screening undergo vaccination(53).
Table 1 gives a snapshot of the state of existing national vaccination and screening programs in LMIC, according to data provided to the WHO and the Catalan Institute of Oncology (ICO) and the International Agency for Research on Cancer (IARC) Information Centre on HPV and Cancer. Screening programs may vary from opportunistic to organized, and while many countries do not have a national HPV program list on this table, they do have a variety of pilot and other HPV projects giving some vaccination coverage. Moreover, the presence of screening programs does not necessarily translate to high screening coverage in many LMIC(54). What is also clear is that very few LMIC have both vaccination (primary) and secondary prevention programs, and this should ultimately be the goal, given that WHO modelling for vaccination and screening shows that the introduction of both is really necessary for the elimination of cervical cancer in the LMIC with the highest burden of disease(55)
Table 1:
| HPV National Program | Screening program | HPV National Program | Screening program | HPV National Program | Screening program | HPV National Program | Screening program | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Afghanistan | No | Yes | Cuba | No | Yes | Korea, Dem. People’s Rep. | Peru | Yes | Yes | ||
| Albania | No | Yes | Djibouti | No | No | Kosovo(57) | No | No | Philippines(58) | Yes | Yes |
| Algeria | No | Yes | Dominica | No | Yes | Kyrgyz Republic | No | No | Russian Federation | No | Yes |
| American Samoa | Dominican Republic | Yes | Yes | Lao PDR | No | Yes | Rwanda | Yes | Yes | ||
| Angola | No | No | Ecuador | Yes | Yes | Lebanon | No | Yes | Samoa | No | No |
| Argentina | Yes | Yes | Egypt, Arab Rep. | No | Yes | Lesotho | Yes | Yes | São Tomé and Principe | Yes | No |
| Armenia | Yes | Yes | El Salvador | No | Yes | Liberia | No | No | Senegal | Yes | Yes |
| Azerbaijan | No | No | Equatorial Guinea | No | No | Libya | Yes | No | Serbia | No | Yes |
| Bangladesh | No | Yes | Eritrea | No | No | Madagascar | No | Yes | Solomon Islands | No | Yes |
| Belarus | No | Yes | Eswatini | No | No | Malawi | No | Yes | South Africa | Yes | Yes |
| Belize | Yes | Yes | Ethiopia | No | Yes | Malaysia | Yes | Yes | Sri Lanka | Yes | Yes |
| Benin | No | No | Fiji | Yes | Yes | Maldives | No | Yes | St. Lucia | No | Yes |
| Bhutan | Yes | Yes | Gabon | No | Yes | Mali | No | No | St. Vincent and the Grenadines | No | Yes |
| Bolivia | Yes | No | Gambia, The | No | No | Marshall Islands | Yes | Yes | Suriname | Yes | Yes |
| Bosnia and Herzegovina | No | Yes | Georgia | No | Yes | Mauritania | No | No | Tanzania(59) | Yes | Yes |
| Botswana | Yes | Yes | Ghana | No | Yes | Mexico | Yes | Yes | Thailand | No | Yes |
| Brazil | Yes | Yes | Grenada | No | No | Micronesia, Fed. Sts. | Yes | Yes | Timor-Leste | No | Yes |
| Bulgaria | Yes | Yes | Guatemala | Yes | Yes | Moldova | Tonga | No | Yes | ||
| Burkina Faso | No | Yes | Guinea | No | Yes | Mongolia | No | Yes | Tunisia | No | Yes |
| Burundi | No | No | Guinea-Bissau | No | No | Montenegro | No | Yes | Turkey | No | Yes |
| Cabo Verde | No | Yes | Guyana | Yes | Yes | Morocco | No | Yes | Turkmenistan | Yes | Yes |
| Cambodia | No | Yes | Haiti | No | Yes | Mozambique | No | Yes | Tuvalu | No | Yes |
| Cameroon | No | No | Honduras | Yes | Yes | Myanmar | No | Yes | Ukraine | No | Yes |
| Central African Republic | No | No | India | No | Yes | Namibia | No | Yes | Uzbekistan | No | Yes |
| Chad | No | No | Indonesia | Yes | Yes | Nepal | No | Yes | Vanuatu | No | Yes |
| China | No | Yes | Iran, Islamic Rep. | No | Yes | Nicaragua | No | Yes | Venezuela, RB | No | Yes |
| Colombia | Yes | Yes | Iraq | No | Yes | Niger | No | No | Vietnam | No | Yes |
| Comoros | No | No | Jamaica | Yes | No | Nigeria | No | No | West Bank and Gaza | No | No |
| Congo, Dem. Rep | No | No | Jordan | No | Yes | North Macedonia | Yes | Yes | Zambia | No | Yes |
| Congo, Rep. | No | No | Kazakhstan | Yes | Yes | Pakistan | No | Yes | Zimbabwe | No | Yes |
| Costa Rica | No | Yes | Kenya | No | Yes | Papua New Guinea | No | No | |||
| Côte d’Ivoire | No | Yes | Kiribati | No | Yes | Paraguay | Yes | Yes |
Data from these references unless otherwise indicated
No data found for countries with blank entries
Cervical assessment
Positive cervical screening (either cytology or HPV) needs to be followed by cervical assessment, with the standard of care in maximally resourced settings being colposcopy, whereby acetic acid and / or iodine is applied to the cervix and magnified examination is undertaken. The challenges with this in LMIC are the cost (equipment, supplies and maintenance), in addition to the training necessary to make the use of colposcope both safe and clinically adequate. Thus, the capacity to deliver well-resourced and well trained clinicians in colposcopy is a huge barrier in LMIC. Several unique technologies have been developed to overcome these issues.
Mobile colposcopes and microendoscopes
The Gynocular (Gynius AB, Stockholm, Sweden) is a portable low cost colposcope that is comparable in its efficacy to a standard colposcope. In addition to having been evaluated in high resource settings(60, 61), studies in LMIC demonstrate its applicability as a technology that works in the field and that can be used by both doctors and nurses(62–64). The Gynocular is battery driven, has comparable magnification to a traditional colposcope, and weighs around 400 grams(61). While proponents of technologies such as Gynocular argue that it overcomes the poor sensitivity of VIA(66) (which can be as low as 50%(48)), it remains that it is still a colposcope and therefore requires advanced training and resources to use and maintain. Some of this can be overcome by the fact that the Gynocular lends itself to the capturing of static images, which can be viewed by an expert colposcopist remote from the patient(67).
MobileODT (MobileODT, Tel Aviv, Israel) have developed the Enhanced Visual Assessment (EVA) system (mobileodt.com), a mobile colposcope that is embedded in an android smartphone for use in low resource settings. This digital colposcope may improve on the sensitivity of VIA alone, and has the added benefit of being linked to a mobile phone app, which allows both storing and sharing of images, potentially improving access to expert colposcopists in LMIC(38, 68). Moreover, as Peterson and colleagues showed in their study in Kenya, the mobile app allows for use of a decision aid, which can give real-time monitoring and evaluation by aggregating the data from all users. This resulted in both improved clinician confidence, as well as the ability for organizations to assess incidence of cervical pathology and effectiveness of screening programs(69).
Imaging resolution with the portable digital colposcopes may be improved by the innovate Point of Care Tampon digital Colposcope (POCkeT) colposcope (Zenalux Biomedical). This device, developed by a group at Duke University, is a small 20×140mm tampon shaped device which can be inserted in to the vagina and provide digital colposcopic images 30–40mm from the cervix. (70) The device is portable, waterproof, maintains sterility with a disposable sleeve, and produces images comparable to that of a standard colposcope(71).
Further to these colposcopic technologies, a high resolution microendoscope (HRME) was developed by Rice University to provide real-time diagnosis of high-grade cervical dysplasia, obviating the need for biopsy and pathologic interpretation. The HRME is a battery powered fluorescence microscope that provides real time imaging of cervical abnormalities after application of topical proflavine solution to the cervical surface(72), and has a sensitivity for detecting CIN 2+ in the order of 76%, with a specificity of 56%, which is greater than that reported for traditional colposcopy(73)
Portable colposcopy and microendoscopy lend themselves to overcoming some of the barriers to follow-up and treatment, particularly patients needing to be able to travel to specialist treatment centres for assessment and biopsy prior to treatment. Hunt et al showed in their cluster randomized trial that a mobile van can be fitted with point-of-care technologies including the HRME and improves follow up for abnormal cervical screening compared to when patients have to travel to a central hospital(74). However, portable colposcopy, in whatever form, is most effective as test when used in conjunction with cervical screening such as HPV or cytology, in order to increase positive predictive value(64), and so it remains such that while this is an excellent technological development, portable colposcopy does not overcome all of the barriers in cervical cancer screening in LMIC.
Smart phone technology
Estimates are that 6 of the 7 billion people on earth have access to a working mobile phone, and smart phones are becoming an increasingly used component of cervical cancer prevention. Without needing any additional technology, the use of smartphones to transmit VIA images to experts in locations remote from a clinical setting can allow the safe expansion of cervical screening programs in resource limited LMIC, as well as improve training and support for those potentially lower level health care workers providing the screening(75–83). This emerging research shows acceptable correlation between images taken with a smartphone and final histopathological diagnosis, including when the image is assessed by a clinician at a site remote to the patient. Furthermore, the ubiquity of smartphone use in LMIC also allows for patient acceptance of the process and aids in patient education regarding cervical screening(76). Barriers to this process include issues with network coverage and still needing appropriate and timely access to experts at the other end of the transmission(75).
Building upon basic image capture, the next stage of smart phone use in the prevention of cervical cancer is the use of artificial intelligence / deep learning algorithms such that true diagnostic power of the phone is realised. Complex deep learning algorithms resulting in an automated interpretation of cervical images will potentially improve upon the sensitivity of VIA and allow screening to be performed more easily across levels of health professionals(84). For example, Hu and colleagues applied AVE to a large series of static cervigram images and found it performed better in fact than when those same images were shown to colposcopists(85). Smartphones have great potential to increase access to safe and effective cervical cancer screening in LMIC but rigorous evaluation is needed.
Treatment
Screening is ineffective without effective links to safe treatment options for women with pre-malignant and malignant pathology. As the scope of this article is on cervical cancer prevention, the treatment options outlined below will be those for pre-malignant lesions, however we must be constantly aware that health systems cannot neglect cervical cancer treatment options alongside this. With respect to the treatment of pre-malignant lesions, treatment options include ablation with cryotherapy or thermal ablation, and excision with loop electrosurgical excision procedure (LEEP) or cold knife conization (CKC). For that past several years the majority of LMIC clinicians have been using cryotherapy, however other ablative and excisional options are also becoming more prevalent and subject to innovations in development and implementation(86).
Cryotherapy
Cryotherapy is the process of freezing a cervical lesion using carbon dioxide or nitrous oxygen to a temperature of −58°F for 3 minutes. Carbon dioxide is more often used as it is cheaper and more readily available. It has an effectiveness of between 77% and 93% for the treatment of high grade lesions(87). Cryotherapy can be performed by nurses and other mid-level providers across all levels of the health care system and lends itself well to a see and treat approach to cervical cancer screening(88). The primary challenge with cryotherapy in LMIC has always been the need for a reliable supply of gas, as both procurement and transport issues can interrupt the supply. The CryoPen® (TX, USA) has been specifically developed to address this issue, being a portable cryotherapy device, with an built-in gas system and requiring only a single application for treatment(89). A similar device called the CryoPop has been developed by Jhpiego (an affiliate of Johns Hopkins University) and an initial safety study in the Philippines (with the University of the Philippines) has just been completed, and results are awaited(90).
Thermoablation
An alternative to cryotherapy is thermoablation, whereby electricity rather than gas is used by rapidly heating the tissue with a probe set to a temperature of 212°F for 20–30 seconds. In their systematic review comparing thermoablation to cryotherapy in LMIC, de Fouw and colleagues showed similar cure rates for CIN 2 and 3 lesions in LMIC (91.6% compared with 82.6% respectively)(91). Similar to cryotherapy, thermoablation can be performed in various settings by different levels of health care providers. It can also be performed without anaesthesia, and unlike traditional cryotherapy, the equipment is highly portable, no large gas tanks are needed and a significant number of cases can be performed from a single charge of its battery(92). Due to its size and the short duration required for a treatment, thermoablation is technically easier to use that traditional cryotherapy, however ongoing research is still needed in to the efficacy and safety of thermoablation, including in specific high risk groups, such as women with HIV(86, 93). Innovations like this which are both easy to use an obtain and maintain resources are important considerations in the treatment of pre-malignant disease in LMIC. Having a range of options and optimising the best treatments in the context of specific settings is the way forward in ensuring the greatest number of high risk women are prevented from progression to invasive malignancy.
Excisional methods
While point of care treatments such as ablation will be the mainstay of treatment, particularly at the primary care level, the capacity to undertake excision of a premalignant cervical lesion with a LEEP or CKC is necessary to treat lesions which are unsuitable for ablation. Criteria for excisional treatment includes the transformation zone not being visible, the lesion covering more than 75% of the ectocervix, the lesion extending in to the endocervical canal, or the lesion is suspected to be malignant(94). However, the capacity of women to receive an excisional procedure in an accessible health care setting within a reasonable distance is significantly limited in LMIC. In one Tanzanian study, two thirds of the women needing a LEEP were diagnosed in a facility that could not provide one(95). While there are no major technological changes in the delivery of excisional procedures, innovations around access and service delivery are critical. A single excision procedure requires both permanent infrastructure (electrical supply, diathermy machine) as well as disposable supples including loop electrodes, local anaesthetic and its delivery system, and haemostatic agents. Thus, any consideration to scale-up to more excisional treatments, as they may be more considered more effective than cryotherapy or ablation (measured by residual or recurrent disease), must be measured against the overall cost-effectiveness of both approaches in LMIC(96–99).
The “screen and treat” approach
It is well more than a decade since Denny et al described the safety and efficacy in more than 6000 women in a randomized controlled trial of both HPV DNA and VIA based screen and treat programs in LMIC. Following assessment with both HPV and VIA, women were randomised to either treatment (cryotherapy if positive HPV or cryotherapy if positive VIA) or delayed assessment. Immediate treatment reduced the rate of CIN 2+ at 6 months post screening, and both HPV as well as VIA were safe approaches (rate of CIN 2+ at 6 months was 0.8 and 2.23% respectively) compared to delayed assessment after a positive screening test, which resulted in a CIN 2+ incidence at 6 month of 3.55% (100)
Delivery of screen and treat options in LMIC face many local contextual issues, including resource delivery, need for clinical encounters across more than one service, and provider and patient education and attitudes. Screening and treatment must exist in unison; in an analysis of nearly 45000 women in Nicaragua, only just over a quarter of women who were screen positive with HPV testing received treatment(120), a situation which is clearly untenable. Programs that optimise the dyad of screening and treatment remain the cornerstone of secondary cervical cancer prevention in LMIC and novel approaches are needed. Both screening and treatment using some of the methods outlined above, can be provided in LMIC by nurses and other mid-level health service providers, which optimises the capacity of women to access the service within a reasonable distance. Access and infrastructure are one thing, but women must also be aware of the reason and need for screening, with even female health care providers having limited utilization of services in one systematic review focused on African settings(121).
HIV
No discussion on the prevention of cervical cancer in LMIC is complete without consideration of the role of HIV in the disease. HIV positive women are at increased risk of acquiring HPV, estimated by Liu and colleagues in their systematic review as a RR of 2.64 (95% CI 2.04–3.42), then followed by an increased risk of developing high grade cervical dysplasia (HR 1.32, 95% CI 1.10–1.58)(122). Furthermore, it is estimated that approximately 1.5% of the millions of women living with HIV in LMIC have invasive cervical cancer(123), which is considered an Acquired Immunodeficiency (AIDS) defining illness(124). These risks and numbers are accentuated in sub Saharan Africa, where the incidence of HPV is nearly 25% (more than double that estimated in the rest of the world), and where the incidence of cervical cancer and consequent mortality far exceeds anywhere else in the world (1, 125, 126).
The increased rate of HPV in HIV positive women makes this a particularly important group to screen in LMIC. There are concerns however that the low specificity of both cytology and HPV testing in settings where screen and treat is the standard of care put these women at risk of over treatment, in addition to increasing the burden on a resource constrained system. Kuhn et al demonstrated in their study of more than 1000 women in South Africa, that changing the threshold of HPV point of care testing (Xpert HPV Cepheid, Sunnyvale, CA, USA) results in small decline in sensitivity but a significant increase in specificity in HIV positive women (59.9% to 77%)(127), and this may be one way to address the problem of over treatment. Aside from HPV screening, programs that focus on the prevention and treatment of HIV are critical to the fight against cervical cancer. Hall et al modelled reductions in HPV with target HIV programs, for example the impact of voluntary male medical circumcision to reduce HIV transmission was estimated to reduce cervical cancer mortality by 26% at the year 2070(128).
Health system approaches to the prevention of cervical cancer in LMIC
The capacity to delivery cervical cancer screening requires a whole of health system approach, which will be contextually different in each LMIC. In their systematic review, Rahman and colleagues use the Levesque Patient-Centered Access to Health Care Framework to synthesise the specific barriers to cervical cancer screening identified in 19 studies from LMIC. They report demand related barriers of perception, the capacity to seek and reach screening, the ability to pay and the level of engagement in the process. From a supply point of view, they highlight issues with approachability, acceptability, availability, affordability and appropriateness(129). Each of these barriers lends itself to a review in itself; provided below is one example of integrating cervical cancer screening in to existing programs in LMIC, which may overcome several of the barriers outlined above.
Women in need of cervical screening in LMIC may also be in need of / benefit from other public health programs including HIV screening and treatment and access to family planning services(48). The multifaceted use of infrastructure, and the use of existing motivation to attend health services for other reasons (e.g. HIV testing) potentially allow for cervical cancer screening to be integrated and adopted in resource limited settings(130, 131). Davies et al demonstrated this in South Africa, where they recruited more than 450 women attending a safer conception program for HIV positive women to cervical screening. In a clear demonstration of the benefit of integrated programs such as this, they found more than half having cervical pathology and one in five women needing colposcopy(132). Moreover, the cost effectiveness of integrated programs cannot be underestimated. Vodicka et al demonstrated a more than halving of the costs associated with treatment of premalignant cervical lesions when built in to existing HIV clinic attendance(133). Similarly, the United States Agency for International Development and the National Academies of Sciences, Engineering, and Medicine have joined forces through the Partnerships for Enhanced Engagement in Research (PEER) to undertake implementation and subsequent scale up research in Malawi and Mozambique, focusing on the integration of cervical cancer screening and treatment in to voluntary family planning services(134). While integrated services are not the panacea to cervical cancer prevention, and themselves still require established and ongoing physical and financial resources, we would strongly advocate for this approach in settings where screening is currently limited or non-existent.
Moving forward
While there are many innovations described above directed at the prevention of cervical cancer in LMIC, each face challenges in both implementation and sustainability. It is clear that ultimately health system strengthening is a critical ongoing step in advancing the progress we have made so far in the elimination of cervical cancer(44), as the capacity to deliver cervical cancer screening is deeply rooted in a functioning larger health system(129). In addition to this, national will and global partnerships are needed to achieve adequate and sustained coverage with HPV immunization. Screening and treatment cannot be neglected, especially in the period of transition from a HPV exposed to a HPV immunized population, and programs to do this must be contextually appropriate and, ideally, dovetail with existing infrastructure in order to increase the likelihood of success and sustainability. Ultimately, it is possible to eliminate cervical cancer, but the road in LMIC is long, and will require much innovation, sensible use of resources and ongoing global support.
Figure 1.1 and 1.2.


MobileODT used for colposcopy training in Nepal
Figure 2.
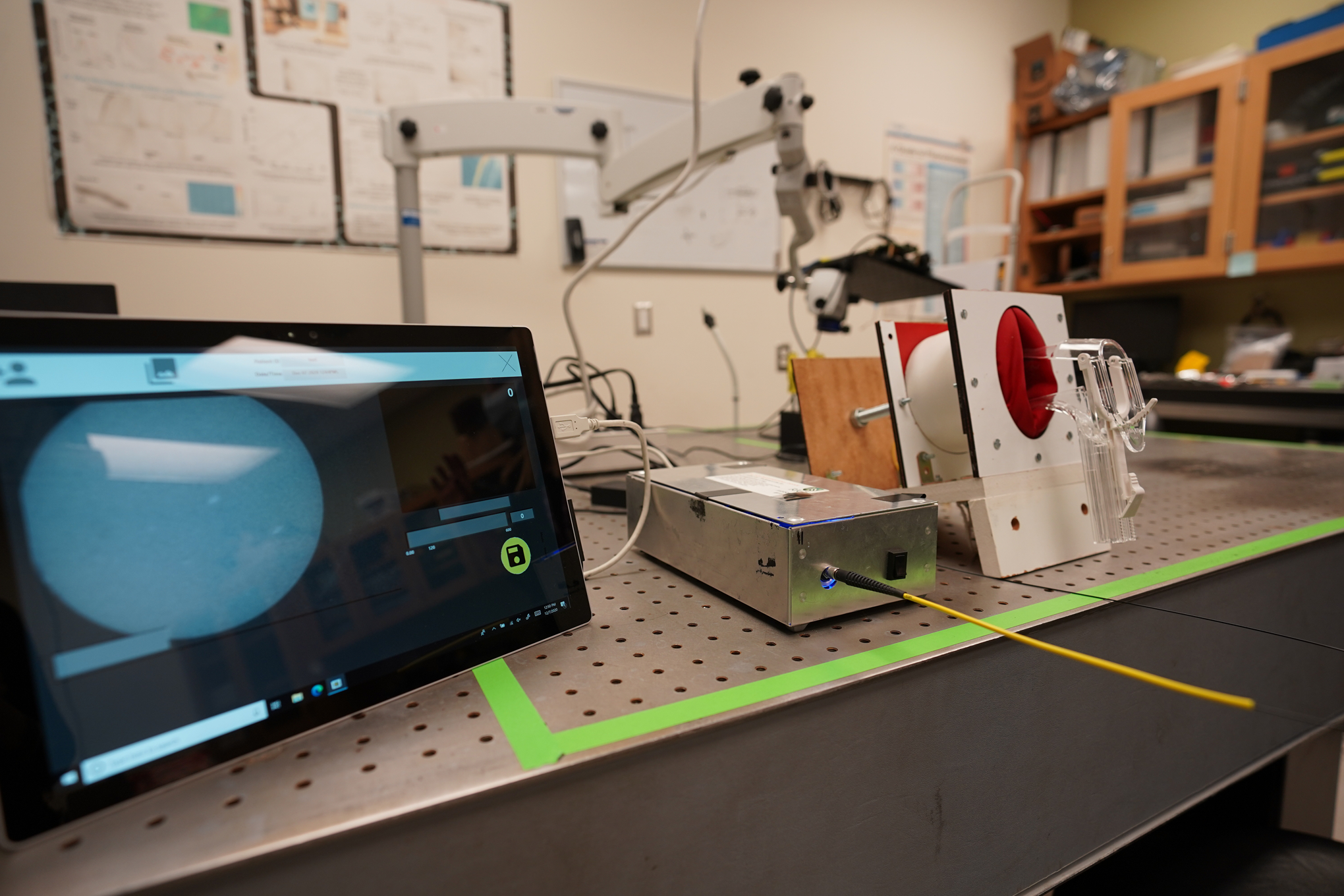
HRME
Figure 3.
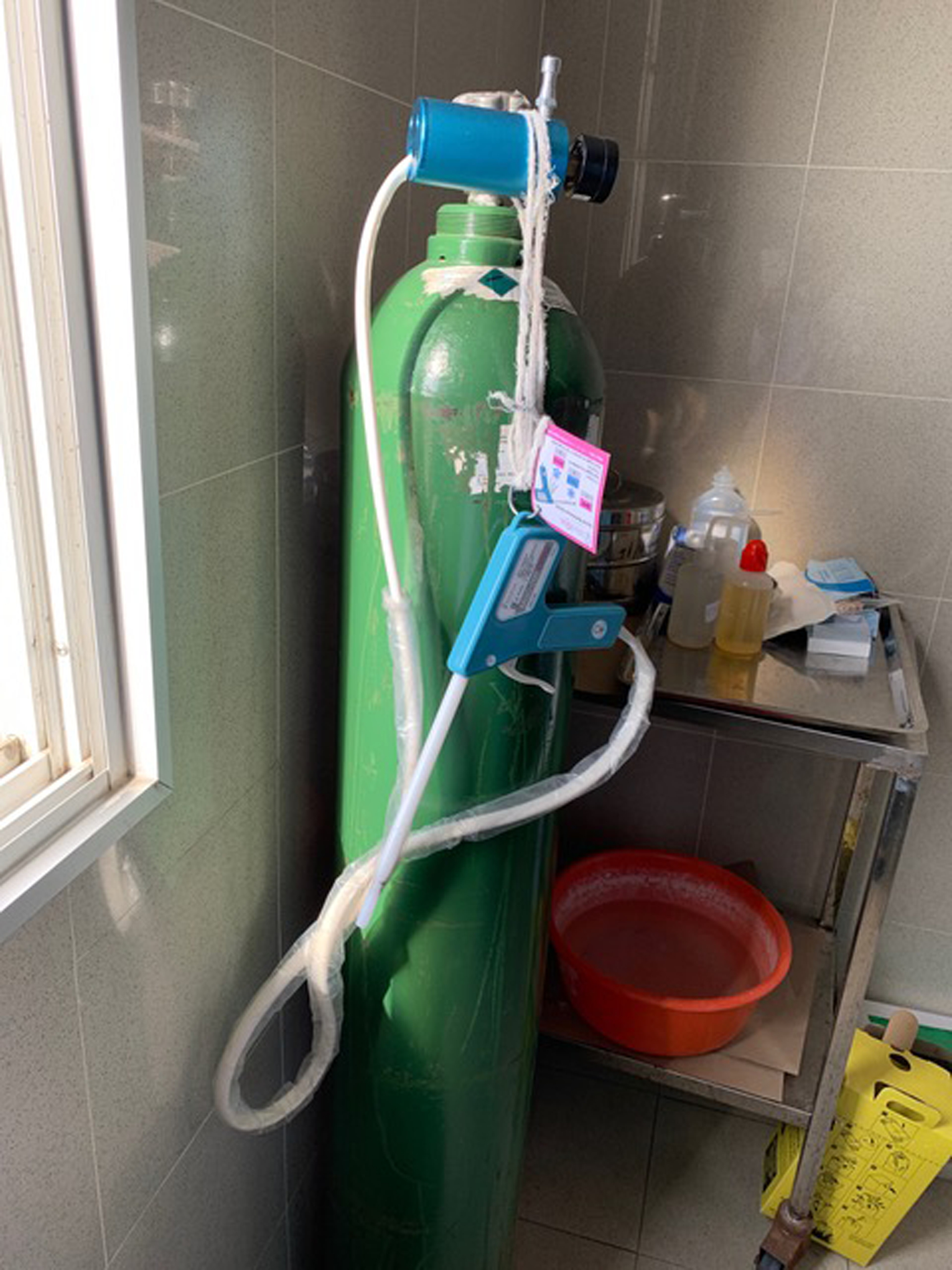
Crytotherapy set up for use in Mozambique
Funding:
ER Allanson is funded by a Jean Murray Jones Fellowship from the Royal Australian and New Zealand College of Obstetricians and Gynaecologists
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. [DOI] [PubMed] [Google Scholar]
- 2.Shaw PA. The history of cervical screening I: the pap. Test. Journal of Obstetrics and Gynaecology Canada. 2000;22(2):110–4. [Google Scholar]
- 3.World Health Organization. Global strategy towards the elimination of cervical cancer as a public health problem 2020 [Available from: https://ijgc.bmj.com/content/ijgc/early/2020/03/02/ijgc-2020-001285.full.pdf.
- 4.Drolet M, Bénard É, Boily M-C, Ali H, Baandrup L, Bauer H, et al. Population-level impact and herd effects following human papillomavirus vaccination programmes: a systematic review and meta-analysis. Lancet Infect Dis. 2015;15(5):565–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gallagher KE, Howard N, Kabakama S, Mounier-Jack S, Burchett HED, LaMontagne DS, et al. Human papillomavirus (HPV) vaccine coverage achievements in low and middle-income countries 2007–2016. Papillomavirus Res. 2017;4:72–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sankaranarayanan R Screening for cancer in low- and middle-income countries. Ann Glob Health. 2014;80(5):412–7. [DOI] [PubMed] [Google Scholar]
- 7.Vu M, Yu J, Awolude OA, Chuang L. Cervical cancer worldwide. Curr Probl Cancer. 2018;42(5):457–65. [DOI] [PubMed] [Google Scholar]
- 8.Blumenthal PD, Gaffikin L. Cervical cancer prevention: making programs more appropriate and pragmatic. Jama. 2005;294(17):2225–8. [DOI] [PubMed] [Google Scholar]
- 9.Toh ZQ, Kosasih J, Russell FM, Garland SM, Mulholland EK, Licciardi PV. Recombinant human papillomavirus nonavalent vaccine in the prevention of cancers caused by human papillomavirus. Infect Drug Resist. 2019;12:1951–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Markowitz LE, Drolet M, Perez N, Jit M, Brisson M. Human papillomavirus vaccine effectiveness by number of doses: Systematic review of data from national immunization programs. Vaccine. 2018;36(32 Pt A):4806–15. [DOI] [PubMed] [Google Scholar]
- 11.Bergman H, Buckley BS, Villanueva G, Petkovic J, Garritty C, Lutje V, et al. Comparison of different human papillomavirus (HPV) vaccine types and dose schedules for prevention of HPV-related disease in females and males. The Cochrane database of systematic reviews. 2019;2019(11):CD013479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Organization WH. Human papillomavirus vaccines: WHO position paper, October 2014. Weekly Epidemiological Record= Relevé épidémiologique hebdomadaire. 2014;89(43):465–91. [PubMed] [Google Scholar]
- 13.Kreimer AR, Struyf F, Del Rosario-Raymundo MR, Hildesheim A, Skinner SR, Wacholder S, et al.
- 14.Wigle J, Coast E, Watson-Jones D. Human papillomavirus (HPV) vaccine implementation in low and middle-income countries (LMICs): health system experiences and prospects. Vaccine. 2013;31(37):3811–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Single-Dose HPV Vaccine Evaluation Consortium. WORKING TOGETHER TO EVALUATE EVIDENCE ON SINGLE-DOSE HPV VACCINATION 2020. [Available from: https://path.azureedge.net/media/documents/SingleDoseHPV_FactSheet_2020.pdf.
- 16.World Health Organization. Vaccines in National Immunization Programme Update 2019. [Available from: https://www.who.int/docs/default-source/documents/immunization/data/vaccine-intro-status.pdf?sfvrsn=bb2857ec_2.
- 17.Bruni L, Diaz M, Barrionuevo-Rosas L, Herrero R, Bray F, Bosch FX, et al. Global estimates of human papillomavirus vaccination coverage by region and income level: a pooled analysis. The Lancet Global Health. 2016;4(7):e453–e63. [DOI] [PubMed] [Google Scholar]
- 18.Bruni LAG, Serrano B, Mena M, Gómez D, Muñoz J, Bosch FX, de Sanjosé S. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in Australia 10 December 2018 [Available from: https://hpvcentre.net/statistics/reports/AUS.pdf?t=1595206434139.
- 19.Bruni LAG, Serrano B, Mena M, Gómez D, Muñoz J, Bosch FX, de Sanjosé S. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in United States of America 10 December 2018 [Available from: https://hpvcentre.net/statistics/reports/USA.pdf?t=1595206602702.
- 20.Shapiro GK, Guichon J, Kelaher M. Canadian school-based HPV vaccine programs and policy considerations. Vaccine. 2017;35(42):5700–7. [DOI] [PubMed] [Google Scholar]
- 21.Bahena M, Carvajal-Suarez M, Soliman AS, Luo J, De Alba A. The influence of medical providers on HPV vaccination among children of Mexican mothers: a comparison between Mexico and the Midwest region of the United States. BMC Public Health. 2019;19(1):515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mendes Lobão W, Duarte FG, Burns JD, de Souza Teles Santos CA, Chagas de Almeida MC, Reingold A, et al. Low coverage of HPV vaccination in the national immunization programme in Brazil: Parental vaccine refusal or barriers in health-service based vaccine delivery? PloS one. 2018;13(11):e0206726–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bruni LAG, Serrano B, Mena M, Gómez D, Muñoz J, Bosch FX, de Sanjosé S. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in the United Kingdom 10 December 2018 [Available from: https://hpvcentre.net/statistics/reports/GBR.pdf?t=1595284976183.
- 24.Bruni LAG, Serrano B, Mena M, Gómez D, Muñoz J, Bosch FX, de Sanjosé S. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in France 10 December 2018 [Available from: https://hpvcentre.net/statistics/reports/FRA.pdf?t=1595285234612.
- 25.Binagwaho A, Ngabo F, Wagner CM, Mugeni C, Gatera M, Nutt CT, et al. Integration of comprehensive women’s health programmes into health systems: cervical cancer prevention, care and control in Rwanda. Bulletin of the World Health Organization. 2013;91(9):697–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Delany-Moretlwe S, Kelley KF, James S, Scorgie F, Subedar H, Dlamini NR, et al. Human Papillomavirus Vaccine Introduction in South Africa: Implementation Lessons From an Evaluation of the National School-Based Vaccination Campaign. Glob Health Sci Pract. 2018;6(3):425–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gallagher KE, LaMontagne DS, Watson-Jones D. Status of HPV vaccine introduction and barriers to country uptake. Vaccine. 2018;36(32):4761–7. [DOI] [PubMed] [Google Scholar]
- 28.Ueda Y, Enomoto T, Sekine M, Egawa-Takata T, Morimoto A, Kimura T. Japan’s failure to vaccinate girls against human papillomavirus. Am J Obstet Gynecol. 2015;212(3):405–6. [DOI] [PubMed] [Google Scholar]
- 29.Cordoba-Sanchez V, Tovar-Aguirre OL, Franco S, Arias Ortiz NE, Louie K, Sanchez GI, et al. Perception about barriers and facilitators of the school-based HPV vaccine program of Manizales, Colombia: A qualitative study in school-enrolled girls and their parents. Preventive medicine reports. 2019;16:100977-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jarvis JD, Woods H, Bali A, Oronsaye E, Persaud N. Selection of WHO-recommended essential medicines for noncommunicable diseases on National Essential Medicines Lists. PloS one. 2019;14(8):e0220781–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gallagher KE, Howard N, Kabakama S, Mounier-Jack S, Griffiths UK, Feletto M, et al. Lessons learnt from human papillomavirus (HPV) vaccination in 45 low- and middle-income countries. PloS one. 2017;12(6):e0177773–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ferjaoui MA. HPV vaccination: a Tunisian challenge. International Journal of Gynecologic Cancer. 2020;30(8):1248-. [DOI] [PubMed] [Google Scholar]
- 33.Lortet-Tieulent J, Georges D, Bray F, Vaccarella S. Profiling global cancer incidence and mortality by socioeconomic development. Int J Cancer. 2020. [DOI] [PubMed] [Google Scholar]
- 34.Mezei AK, Armstrong HL, Pedersen HN, Campos NG, Mitchell SM, Sekikubo M, et al. Cost-effectiveness of cervical cancer screening methods in low- and middle-income countries: A systematic review. Int J Cancer. 2017;141(3):437–46. [DOI] [PubMed] [Google Scholar]
- 35.Jeronimo J, Castle PE, Temin S, Denny L, Gupta V, Kim JJ, et al. Secondary Prevention of Cervical Cancer: ASCO Resource-Stratified Clinical Practice Guideline. J Glob Oncol. 2017;3(5):635–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.World Health Organization. WHO guidelines for screening and treatment of precancerous lesions for cervical cancer prevention: World Health Organization; 2013. [PubMed] [Google Scholar]
- 37.Koliopoulos G, Nyaga VN, Santesso N, Bryant A, Martin‐Hirsch PPL, Mustafa RA, et al. Cytology versus HPV testing for cervical cancer screening in the general population. Cochrane Database of Systematic Reviews. 2017(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kundrod KA, Smith CA, Hunt B, Schwarz RA, Schmeler K, Richards-Kortum R. Advances in technologies for cervical cancer detection in low-resource settings. Expert Rev Mol Diagn. 2019;19(8):695–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ying H, Jing F, Fanghui Z, Youlin Q, Yali H. High-risk HPV nucleic acid detection kit-the careHPV test -a new detection method for screening. Sci Rep. 2014;4:4704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Einstein MH, Smith KM, Davis TE, Schmeler KM, Ferris DG, Savage AH, et al. Clinical evaluation of the cartridge-based GeneXpert human papillomavirus assay in women referred for colposcopy. Journal of clinical microbiology. 2014;52(6):2089–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Katanga J, Kjaer SK, Manongi R, Wu CS, Iftner T, Waldstrom M, et al. Performance of careHPV, hybrid capture 2 and visual inspection with acetic acid for detection of high-grade cervical lesion in Tanzania: A cross-sectional study. PLoS One. 2019;14(6):e0218559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jeronimo J, Bansil P, Lim J, Peck R, Paul P, Amador JJ, et al. A multicountry evaluation of careHPV testing, visual inspection with acetic acid, and papanicolaou testing for the detection of cervical cancer. Int J Gynecol Cancer. 2014;24(3):576–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang M, Hu S, Zhao S, Zhang W, Pan Q, Zhang X, et al. Accuracy of triage strategies for human papillomavirus DNA-positive women in low-resource settings: A cross-sectional study in China. Chin J Cancer Res. 2017;29(6):496–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cubie HA, Campbell C. Cervical cancer screening - The challenges of complete pathways of care in low-income countries: Focus on Malawi. Womens Health (Lond). 2020;16:1745506520914804-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dykens JA, Smith JS, Demment M, Marshall E, Schuh T, Peters K, et al. Evaluating the implementation of cervical cancer screening programs in low-resource settings globally: a systematized review. Cancer causes & control : CCC. 2020;31(5):417–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Viviano M, DeBeaudrap P, Tebeu P-M, Fouogue JT, Vassilakos P, Petignat P. A review of screening strategies for cervical cancer in human immunodeficiency virus-positive women in sub-Saharan Africa. International journal of women’s health. 2017;9:69–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Visual inspection with acetic acid for cervical-cancer screening: test qualities in a primary-care setting. University of Zimbabwe/JHPIEGO Cervical Cancer Project. Lancet. 1999;353(9156):869–73. [PubMed] [Google Scholar]
- 48.Sahasrabuddhe VV, Parham GP, Mwanahamuntu MH, Vermund SH. Cervical cancer prevention in low- and middle-income countries: feasible, affordable, essential. Cancer Prev Res (Phila). 2012;5(1):11–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.WHO Guidelines Approved by the Guidelines Review Committee. WHO Guidelines for Screening and Treatment of Precancerous Lesions for Cervical Cancer Prevention. Geneva: World Health Organization; Copyright © World Health Organization 2013.; 2013. [PubMed] [Google Scholar]
- 50.Gaffikin L, Blumenthal PD, Emerson M, Limpaphayom K. Safety, acceptability, and feasibility of a single-visit approach to cervical-cancer prevention in rural Thailand: a demonstration project. Lancet. 2003;361(9360):814–20. [DOI] [PubMed] [Google Scholar]
- 51.Blumenthal PD, Gaffikin L, Deganus S, Lewis R, Emerson M, Adadevoh S. Cervical cancer prevention: safety, acceptability, and feasibility of a single-visit approach in Accra, Ghana. Am J Obstet Gynecol. 2007;196(4):407.e1–8; discussion .e8–9. [DOI] [PubMed] [Google Scholar]
- 52.El-Zein M, Richardson L, Franco EL. Cervical cancer screening of HPV vaccinated populations: Cytology, molecular testing, both or none. Journal of clinical virology : the official publication of the Pan American Society for Clinical Virology. 2016;76 Suppl 1(Suppl 1):S62–S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Identifier: NCT01338051 The Development of a “Mother/Child, Screen, Treat and Vaccinate Program” in Manchay and Iquitos, Peru (PERCAPS) [Internet]. National Library of Medicine (US). 2019. [cited 07/07/2020]. Available from: https://clinicaltrials.gov/ct2/show/NCT01338051. [Google Scholar]
- 54.Bruni LAG, Serrano B, Mena M, Gómez D, Muñoz J, Bosch FX, de Sanjosé S. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in the World 22 January 2019 [Available from: https://hpvcentre.net/datastatistics.php.
- 55.Brisson M, Kim JJ, Canfell K, Drolet M, Gingras G, Burger EA, et al. Impact of HPV vaccination and cervical screening on cervical cancer elimination: a comparative modelling analysis in 78 low-income and lower-middle-income countries. Lancet (London, England). 2020;395(10224):575–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.World Health Organization. Cancer country profiles 2020 2020. [Available from: https://www.who.int/cancer/country-profiles/en/.
- 57.Zejnullahu Raçi P, Hošnjak L, Poljak M, Lepej S, Vince A. Pre-vaccination prevalence of high-risk human papillomaviruses (HPV) in women from Kosovo and their related sociodemographic characteristics. Ginekol Pol. 2018;89(9):485–94. [DOI] [PubMed] [Google Scholar]
- 58.Republic of the Philippines Department of Health. SCHOOL-BASED HUMAN PAPILLOMAVIRUS (HPV) IMMUNIZATION LAUNCHED IN MANDALUYONG CITY Manilla, Philippines: 2020. [Available from: https://www.doh.gov.ph/node/10736. [Google Scholar]
- 59.Runge AS, Bernstein ME, Lucas AN, Tewari KS. Cervical cancer in Tanzania: A systematic review of current challenges in six domains. Gynecologic oncology reports. 2019;29:40–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kallner HK, Persson M, Thuresson M, Altman D, Shemer I, Thorsell M, et al. Diagnostic colposcopic accuracy by the gynocular and a stationary colposcope. Int J Technol Assess Health Care. 2015;31(3):181–7. [DOI] [PubMed] [Google Scholar]
- 61.Ngonzi J, Bajunirwe F, Wistrand C, Mayanja R, Altman D, Thorsell M, et al. Agreement of colposcope and gynocular in assessment of cervical lesions by swede score: a randomized, crossover pilot trial. J Low Genit Tract Dis. 2013;17(4):372–7. [DOI] [PubMed] [Google Scholar]
- 62.Nessa A, Roy JS, Chowdhury MA, Khanam Q, Afroz R, Wistrand C, et al. Evaluation of the accuracy in detecting cervical lesions by nurses versus doctors using a stationary colposcope and Gynocular in a low-resource setting. BMJ Open. 2014;4(11):e005313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Basu P, Banerjee D, Mittal S, Mandal R, Ghosh I, Das P, et al. Evaluation of a compact, rechargeable, magnifying device to triage VIA and HPV positive women in a cervical cancer screening program in rural India. Cancer Causes Control. 2016;27(10):1253–9. [DOI] [PubMed] [Google Scholar]
- 64.Newman H, Hu J, Li X, He J, Bradford L, Shan S, et al. Evaluation of portable colposcopy and human papillomavirus testing for screening of cervical cancer in rural China. Int J Gynecol Cancer. 2019;29(1):23–7. [DOI] [PubMed] [Google Scholar]
- 65.Identifier: NCT03931083 Screening Test Accuracy of Gynocular™, HR-HPV Testing, VIA for Detection of Cervical Neoplastic Lesions, in Women Living With HIV [Internet]. Bethesda (MD): National Library of Medicine (US). 2019. [cited 19/06/2020]. Available from: https://clinicaltrials.gov/ct2/show/NCT03931083. [Google Scholar]
- 66.Nessa A, Wistrand C, Begum SA, Thuresson M, Shemer I, Thorsell M, et al. Evaluation of stationary colposcope and the Gynocular, by the Swede score systematic colposcopic system in VIA positive women: a crossover randomized trial. Int J Gynecol Cancer. 2014;24(2):339–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Taghavi K, Banerjee D, Mandal R, Kallner HK, Thorsell M, Friis T, et al. Colposcopy telemedicine: live versus static swede score and accuracy in detecting CIN2+, a cross-sectional pilot study. BMC Womens Health. 2018;18(1):89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Thay S, Goldstein A, Goldstein LS, Govind V, Lim K, Seang C. Prospective cohort study examining cervical cancer screening methods in HIV-positive and HIV-negative Cambodian Women: a comparison of human papilloma virus testing, visualization with acetic acid and digital colposcopy. BMJ open. 2019;9(2):e026887–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Peterson CW, Rose D, Mink J, Levitz D. Real-Time Monitoring and Evaluation of a Visual-Based Cervical Cancer Screening Program Using a Decision Support Job Aid. Diagnostics (Basel, Switzerland). 2016;6(2):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lam CT, Krieger MS, Gallagher JE, Asma B, Muasher LC, Schmitt JW, et al. Design of a Novel Low Cost Point of Care Tampon (POCkeT) Colposcope for Use in Resource Limited Settings. PloS one. 2015;10(9):e0135869–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lam CT, Mueller J, Asma B, Asiedu M, Krieger MS, Chitalia R, et al. An integrated strategy for improving contrast, durability, and portability of a Pocket Colposcope for cervical cancer screening and diagnosis. PLoS One. 2018;13(2):e0192530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pierce MC, Guan Y, Quinn MK, Zhang X, Zhang W-H, Qiao Y-L, et al. A pilot study of low-cost, high-resolution microendoscopy as a tool for identifying women with cervical precancer. Cancer prevention research (Philadelphia, Pa). 2012;5(11):1273–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Parra SG, Rodriguez AM, Cherry KD, Schwarz RA, Gowen RM, Guerra LB, et al. Low-cost, high-resolution imaging for detecting cervical precancer in medically-underserved areas of Texas. Gynecol Oncol. 2019;154(3):558–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hunt B, Fregnani JHTG, Schwarz RA, Pantano N, Tesoni S, Possati-Resende JC, et al. Diagnosing Cervical Neoplasia in Rural Brazil Using a Mobile Van Equipped with In Vivo Microscopy: A Cluster-Randomized Community Trial. Cancer prevention research (Philadelphia, Pa). 2018;11(6):359–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yeates KE, Sleeth J, Hopman W, Ginsburg O, Heus K, Andrews L, et al. Evaluation of a Smartphone-Based Training Strategy Among Health Care Workers Screening for Cervical Cancer in Northern Tanzania: The Kilimanjaro Method. J Glob Oncol. 2016;2(6):356–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Asgary R, Cole H, Adongo P, Nwameme A, Maya E, Adu-Amankwah A, et al. Acceptability and implementation challenges of smartphone-based training of community health nurses for visual inspection with acetic acid in Ghana: mHealth and cervical cancer screening. BMJ Open. 2019;9(7):e030528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sharma D, Rohilla L, Bagga R, Srinivasan R, Jindal HA, Sharma N, et al. Feasibility of implementing cervical cancer screening program using smartphone imaging as a training aid for nurses in rural India. Public Health Nurs. 2018;35(6):526–33. [DOI] [PubMed] [Google Scholar]
- 78.Bae JK, Roh HJ, You JS, Kim K, Ahn Y, Askaruly S, et al. Quantitative Screening of Cervical Cancers for Low-Resource Settings: Pilot Study of Smartphone-Based Endoscopic Visual Inspection After Acetic Acid Using Machine Learning Techniques. JMIR Mhealth Uhealth. 2020;8(3):e16467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tran PL, Benski C, Viviano M, Petignat P, Combescure C, Jinoro J, et al. PERFORMANCE OF SMARTPHONE-BASED DIGITAL IMAGES FOR CERVICAL CANCER SCREENING IN A LOW-RESOURCE CONTEXT. Int J Technol Assess Health Care. 2018;34(3):337–42. [DOI] [PubMed] [Google Scholar]
- 80.Ricard-Gauthier D, Wisniak A, Catarino R, van Rossum AF, Meyer-Hamme U, Negulescu R, et al. Use of Smartphones as Adjuvant Tools for Cervical Cancer Screening in Low-Resource Settings. J Low Genit Tract Dis. 2015;19(4):295–300. [DOI] [PubMed] [Google Scholar]
- 81.Catarino R, Vassilakos P, Scaringella S, Undurraga-Malinverno M, Meyer-Hamme U, Ricard-Gauthier D, et al. Smartphone Use for Cervical Cancer Screening in Low-Resource Countries: A Pilot Study Conducted in Madagascar. PLoS One. 2015;10(7):e0134309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Urner E, Delavy M, Catarino R, Viviano M, Meyer-Hamme U, Benski AC, et al. A Smartphone-Based Approach for Triage of Human Papillomavirus-Positive Sub-Saharan African Women: A Prospective Study. JMIR Mhealth Uhealth. 2017;5(5):e72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gallay C, Girardet A, Viviano M, Catarino R, Benski AC, Tran PL, et al. Cervical cancer screening in low-resource settings: a smartphone image application as an alternative to colposcopy. Int J Womens Health. 2017;9:455–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Guo P, Xue Z, Long LR, Antani S. Cross-Dataset Evaluation of Deep Learning Networks for Uterine Cervix Segmentation. Diagnostics (Basel, Switzerland). 2020;10(1):44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hu L, Bell D, Antani S, Xue Z, Yu K, Horning MP, et al. An Observational Study of Deep Learning and Automated Evaluation of Cervical Images for Cancer Screening. J Natl Cancer Inst. 2019;111(9):923–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Maza M, Schocken CM, Bergman KL, Randall TC, Cremer ML. Cervical Precancer Treatment in Low- and Middle-Income Countries: A Technology Overview. J Glob Oncol. 2016;3(4):400–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Martin‐Hirsch PPL, Paraskevaidis E, Bryant A, Dickinson HO. Surgery for cervical intraepithelial neoplasia. Cochrane Database of Systematic Reviews. 2013(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.World Health Organization. Comprehensive Cervical Cancer Control. A guide to essential practice. Geneva; WHO 2006. 2018. [PubMed] [Google Scholar]
- 89.Identifier: NCT03084081 An Innovative Treatment for Cervical Precancer (UH3) (UH3) [Internet]. National Library of Medicine (US). 2019. [cited 07/07/2020]. Available from: https://clinicaltrials.gov/ct2/show/record/NCT03084081. [Google Scholar]
- 90.Identifier: NCT02367625 Performance, Safety, and Efficacy of a New Cyrotherapy Device for Cervical Dysplasia [Internet]. National Library of Medicine (US). 2019. Available from: https://clinicaltrials.gov/ct2/show/NCT02367625. [Google Scholar]
- 91.de Fouw M, Oosting RM, Rutgrink A, Dekkers OM, Peters AAW, Beltman JJ. A systematic review and meta‐analysis of thermal coagulation compared with cryotherapy to treat precancerous cervical lesions in low‐and middle‐income countries. International Journal of Gynecology & Obstetrics. 2019;147(1):4–18. [DOI] [PubMed] [Google Scholar]
- 92.Cremer ML, Conzuelo-Rodriguez G, Cherniak W, Randall T. Ablative Therapies for Cervical Intraepithelial Neoplasia in Low-Resource Settings: Findings and Key Questions. J Glob Oncol. 2018;4:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Identifier: NCT04191967 Thermocoagulation for Treatment of Precancerous Cervical Lesions [Internet]. Bethesda (MD): National Library of Medicine (US). 2019. [cited 19/06/2020]. Available from: https://clinicaltrials.gov/ct2/show/NCT04191967. [Google Scholar]
- 94.Santesso N, Mustafa RA, Schünemann HJ, Arbyn M, Blumenthal PD, Cain J, et al. World Health Organization Guidelines for treatment of cervical intraepithelial neoplasia 2–3 and screen‐and‐treat strategies to prevent cervical cancer. International Journal of Gynecology & Obstetrics. 2016;132(3):252–8. [DOI] [PubMed] [Google Scholar]
- 95.Besanaą G, Giattasą MR, Plotkiną M, Mohammed M, Makeneą C, Curran K. Access to Loop Electrosurgical Excision Procedure (LEEP) in Cervical Cancer Prevention Is Critical for HIV-Endemic Settings: Experiences from Tanzania.
- 96.Greene SA, De Vuyst H, John-Stewart GC, Richardson BA, McGrath CJ, Marson KG, et al. Effect of Cryotherapy vs Loop Electrosurgical Excision Procedure on Cervical Disease Recurrence Among Women With HIV and High-Grade Cervical Lesions in Kenya: A Randomized Clinical Trial. JAMA. 2019;322(16):1570–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hurtado-Roca Y, Becerra-Chauca N, Malca M. Efficacy and safety of cryotherapy, cold cone or thermocoagulation compared to LEEP as a therapy for cervical intraepithelial neoplasia: Systematic review. Rev Saude Publica. 2020;54:27-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.D’Alessandro P, Arduino B, Borgo M, Saccone G, Venturella R, Di Cello A, et al. Loop Electrosurgical Excision Procedure versus Cryotherapy in the Treatment of Cervical Intraepithelial Neoplasia: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Gynecology and minimally invasive therapy. 2018;7(4):145–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lince-Deroche N, van Rensburg C, Roseleur J, Sanusi B, Phiri J, Michelow P, et al. Costs and cost-effectiveness of LEEP versus cryotherapy for treating cervical dysplasia among HIV-positive women in Johannesburg, South Africa. PLoS One. 2018;13(10):e0203921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Denny L, Kuhn L, De Souza M, Pollack AE, Dupree W, Wright TC Jr., Screen-and-treat approaches for cervical cancer prevention in low-resource settings: a randomized controlled trial. Jama. 2005;294(17):2173–81. [DOI] [PubMed] [Google Scholar]
- 101.Identifier: NCT04092257 HPV-Based Screen-and-Treat Demonstration Project in Lilongwe [Internet]. Bethesda (MD): National Library of Medicine (US). 2019. [cited 19/06/2020]. Available from: https://clinicaltrials.gov/ct2/show/NCT04092257. [Google Scholar]
- 102.Identifier: NCT04000503 Integrated Cervical Cancer Screening in Mayuge District Uganda (ASPIRE Mayuge) (ASPIRE) [Internet]. Bethesda (MD): National Library of Medicine (US). 2019. [cited 19/06/2020]. Available from: https://clinicaltrials.gov/ct2/show/NCT04000503. [Google Scholar]
- 103.Identifier: NCT03942705 A New Approach to Cervical Cancer Prevention in Kenya [Internet]. Bethesda (MD): National Library of Medicine (US). 2019. [cited 19/06/2020]. Available from: https://clinicaltrials.gov/ct2/show/NCT03942705. [Google Scholar]
- 104.Identifier: NCT03514459 Testing an Implementation Science Tool to Increase Cervical Cancer Screening in Mombasa, Kenya [Internet]. National Library of Medicine (US). 2019. [cited 19/06/2020]. Available from: https://clinicaltrials.gov/ct2/show/NCT03514459. [Google Scholar]
- 105.Identifier: NCT02124252 Community-Driven Cervical Cancer Prevention in Western Kenya [Internet]. National Library of Medicine (US). 2019. [cited 19/06/2020]. Available from: https://clinicaltrials.gov/ct2/show/NCT02124252. [Google Scholar]
- 106.Identifier: NCT03808064 Community-based Intervention for Cervical Cancer Screening Uptake in Nepal (COBIN-C) [Internet]. Bethesda (MD): National Library of Medicine (US). 2019. [cited 19/06/2020]. Available from: https://clinicaltrials.gov/ct2/show/NCT03808064. [Google Scholar]
- 107.Identifier: NCT03789513 Evaluation of Screening Algorithms Based on Self-collection and HPV Testing With Partial Genotyping for the Prevention of Cervical Cancer Among HIV-infected Women in Low-income Countries (AIMA-CC) [Internet]. National Library of Medicine (US). 2019. [cited 19/06/2020]. Available from: https://clinicaltrials.gov/ct2/show/NCT03789513. [Google Scholar]
- 108.Identifier: NCT03757299 Promoting Comprehensive Cervical Cancer Prevention and Better Women Health in Cameroon (PCCCP) [Internet]. National Library of Medicine (US). 2019. [cited 19/06/2020]. Available from: https://clinicaltrials.gov/ct2/show/NCT03757299. [Google Scholar]
- 109.Identifier: NCT03713697 Self-Collection and Human Papillomavirus (HPV) Testing in Unscreened Women: a Feasibility Study in Brazil (HPV) [Internet]. National Library of Medicine (US). 2019. [cited 19/06/2020]. Available from: https://clinicaltrials.gov/ct2/show/NCT03713697. [Google Scholar]
- 110.Identifier: NCT03386695 Acceptability and Validity of Self Sampling for High Risk HPV Detection Among Women in Maharashtra (HPV) [Internet]. National Library of Medicine (US). 2019. [cited 19/06/2020]. Available from: https://clinicaltrials.gov/ct2/show/NCT03386695. [Google Scholar]
- 111.Identifier: NCT02247999 Improving Cervical Cancer Screening Among HIV-Infected Women in India [Internet]. National Library of Medicine (US). 2019. [cited 19/06/2020]. Available from: https://clinicaltrials.gov/ct2/show/NCT02247999. [Google Scholar]
- 112.Identifier: NCT03345875 Feasibility and Acceptability of HPV Self-Collection Cervical Cancer Screening and Treatment in Botswana [Internet]. National Library of Medicine (US). 2019. [cited 19/06/2020]. Available from: https://clinicaltrials.gov/ct2/show/NCT03345875. [Google Scholar]
- 113.Identifier: NCT03324009 2-stage Cervical Cancer Screening in Botswana [Internet]. National Library of Medicine (US). 2019. [cited 19/06/2020]. Available from: https://clinicaltrials.gov/ct2/show/NCT03324009. [Google Scholar]
- 114.Identifier: NCT02956031 Screening Study for Cervical Pre-cancer and Cancer Prevention in South African Women. (DiaVACCS) [Internet]. National Library of Medicine (US). 2019. [cited 19/06/2020]. Available from: https://clinicaltrials.gov/ct2/show/NCT02956031. [Google Scholar]
- 115.Identifier: NCT02693379 Cervical Cancer Screening in Madagascar Using Smartphone Photos and Mobile Telemedicine [Internet]. National Library of Medicine (US). 2019. [cited 19/06/2020]. Available from: https://clinicaltrials.gov/ct2/show/NCT02693379. [Google Scholar]
- 116.Identifier: NCT02688816 Comparison of Cervical Cancer Screening Tests in HIV-infected Women in Lusaka, Zambia [Internet]. National Library of Medicine (US). 2019. [cited 19/06/2020]. Available from: https://clinicaltrials.gov/ct2/show/NCT02688816. [Google Scholar]
- 117.Identifier: NCT02680613 Pilot Study of a Mobile Health Approach to Reduce Barriers to Cervical Cancer Screening in Tanzania (KCCPAS) [Internet]. National Library of Medicine (US). 2019. [cited 19/06/2020]. Available from: https://clinicaltrials.gov/ct2/show/NCT02680613. [Google Scholar]
- 118.Identifier: NCT02509702 Use of SMSs to Improve Attendance to Cervical Cancer Follow-up Screening [Internet]. National Library of Medicine (US). 2019. [cited 19/06/2020]. Available from: https://clinicaltrials.gov/ct2/show/NCT02509702. [Google Scholar]
- 119.Identifier: NCT02576262 HPV Integration Testing for Human Papillomavirus-Positive Women [Internet]. National Library of Medicine (US). 2019. Available from: https://clinicaltrials.gov/ct2/show/NCT02576262. [Google Scholar]
- 120.Holme F, Maldonado F, Martinez-Granera OB, Rodriguez JM, Almendarez J, Slavkovsky R, et al. HPV-based cervical cancer screening in Nicaragua: from testing to treatment. BMC Public Health. 2020;20(1):495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Finocchario-Kessler S, Wexler C, Maloba M, Mabachi N, Ndikum-Moffor F, Bukusi E. Cervical cancer prevention and treatment research in Africa: a systematic review from a public health perspective. BMC women’s health. 2016;16:29-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Liu G, Sharma M, Tan N, Barnabas RV. HIV-positive women have higher risk of human papilloma virus infection, precancerous lesions, and cervical cancer. AIDS (London, England). 2018;32(6):795–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Patel P, Rose CE, Collins PY, Nuche-Berenguer B, Sahasrabuddhe VV, Peprah E, et al. Noncommunicable diseases among HIV-infected persons in low-income and middle-income countries: a systematic review and meta-analysis. AIDS (London, England). 2018;32 Suppl 1(Suppl 1):S5–S20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Mapanga W, Girdler-Brown B, Feresu SA, Chipato T, Singh E. Prevention of cervical cancer in HIV-seropositive women from developing countries through cervical cancer screening: a systematic review. Syst Rev. 2018;7(1):198-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Lekoane KMB, Kuupiel D, Mashamba-Thompson TP, Ginindza TG. Evidence on the prevalence, incidence, mortality and trends of human papilloma virus-associated cancers in sub-Saharan Africa: systematic scoping review. BMC cancer. 2019;19(1):563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Black E, Richmond R. Prevention of Cervical Cancer in Sub-Saharan Africa: The Advantages and Challenges of HPV Vaccination. Vaccines. 2018;6(3):61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kuhn L, Saidu R, Boa R, Tergas A, Moodley J, Persing D, et al. Clinical evaluation of modifications to a human papillomavirus assay to optimise its utility for cervical cancer screening in low-resource settings: a diagnostic accuracy study. Lancet Glob Health. 2020;8(2):e296–e304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Hall MT, Smith MA, Simms KT, Barnabas RV, Canfell K, Murray JM. The past, present and future impact of HIV prevention and control on HPV and cervical disease in Tanzania: A modelling study. PloS one. 2020;15(5):e0231388–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Rahman R, Clark MD, Collins Z, Traore F, Dioukhane EM, Thiam H, et al. Cervical cancer screening decentralized policy adaptation: an African rural-context-specific systematic literature review. Glob Health Action. 2019;12(1):1587894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Mwanahamuntu MH, Sahasrabuddhe VV, Kapambwe S, Pfaendler KS, Chibwesha C, Mkumba G, et al. Advancing cervical cancer prevention initiatives in resource-constrained settings: insights from the Cervical Cancer Prevention Program in Zambia. PLoS Med. 2011;8(5):e1001032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Sigfrid L, Murphy G, Haldane V, Chuah FLH, Ong SE, Cervero-Liceras F, et al. Integrating cervical cancer with HIV healthcare services: A systematic review. PloS one. 2017;12(7):e0181156–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Davies NECG, Chersich M, Mullick S, Naidoo N, Makhoba N, Rees H, et al. Integrating Cervical Cancer Screening Into Safer Conception Services to Improve Women’s Health Outcomes: A Pilot Study at a Primary Care Clinic in South Africa. Sexually transmitted diseases. 2019;46(2):91–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Vodicka EL, Chung MH, Zimmermann MR, Kosgei RJ, Lee F, Mugo NR, et al. Estimating the costs of HIV clinic integrated versus non-integrated treatment of pre-cancerous cervical lesions and costs of cervical cancer treatment in Kenya. PloS one. 2019;14(6):e0217331–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.The National Academies of Sciences Engineering and Medicine. Expanding Cervical Cancer Screening and Preventive Therapy (CCS&PT) through Introducing New Technologies and Integrating with Voluntary Family Planning 2020. [Available from: https://www.nationalacademies.org/our-work/expanding-cervical-cancer-screening-and-preventive-therapy-ccspt-through-introducing-new-technologies-and-integrating-with-voluntary-family-planning.


