Introduction
Puffy hand syndrome is a rare entity associated with intravenous drug use (IVDU) that was first described in 1965 and affects between 7% and 16% of intravenous drug users.1,2 Clinical findings include painless, nonpitting edema and erythema of the dorsal side of bilateral hands, often beginning years after cessation of IVDU.3 The pathophysiology is favored to be a result of lymphatic obstruction and chronic destruction along with weakened vasculature secondary to the toxicity of heroin, buprenorphine, and any accompanying contaminants.4 Poor aseptic technique leads to the destruction of lymphatics and venules secondary to septic microthrombi.4 Other risk factors include female gender, injection into the hands, lack of tourniquet use, history of cellulitis, and/or venous thrombosis.2,3
The diagnosis of puffy hand syndrome is an exclusion. Histopathology and laboratory findings are nonspecific and unrevealing. The differential diagnosis includes heart failure, renal insufficiency, liver failure, erythromelalgia, scleroderma, rheumatoid arthritis, and systemic lupus erythematosus.1,3 Although there have not been any randomized controlled trials, there are a few reports of successful symptomatic treatment with compression.3,4 We present a case of puffy hand syndrome presenting initially during pregnancy and persisting postpartum.
Case report
A 35-year-old woman with a history of bipolar I disorder and chronic joint pain presented to the dermatology clinic with a 15-month history of swelling and redness of her hands. She denied any exacerbating factors, including temperature change. She endorsed occupational exposure to swimming pool chemicals; however, wearing gloves did not improve her symptoms. She endorsed chronic joint pain in her hands and back. Prior unsuccessful treatments included mupirocin ointment and over-the-counter emollients. She denied a history of coagulopathy.
She endorsed a 4-year history of injecting heroin, buprenorphine, suboxone, and morphine without tourniquet use into numerous areas from her chest to her toes, including both upper extremities. She described injecting routinely into the dorsal side of bilateral hands, wrists, and ventral side of forearms. Three years after the cessation of IVDU, she experienced an intermittent and gradual onset of painless, symmetric swelling of both hands. Two years later, during the second trimester of pregnancy, persistent edema with new erythema of hands and feet developed. She was hospitalized for cardiac and deep vein thrombosis evaluation. An echocardiogram showed a normal ejection fraction. No definitive diagnosis was made during this hospitalization. Following pregnancy, edema and erythema of her hands persisted, and at 11 months postpartum, she presented to the dermatology department.
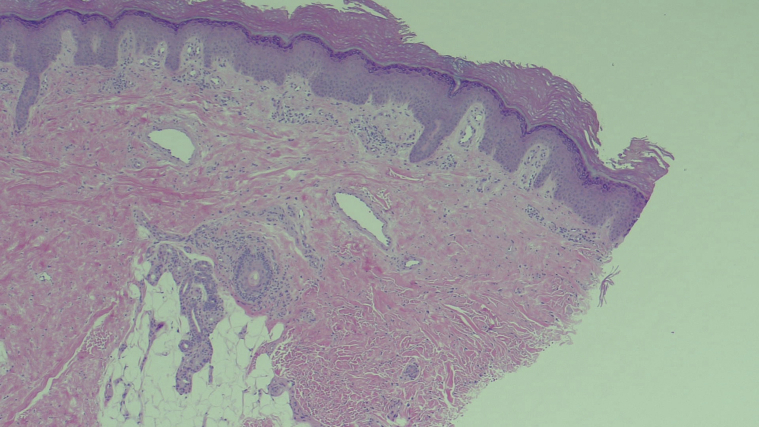
The cutaneous examination revealed erythema and edema of the dorsal side of her hands bilaterally with somewhat sharp demarcation at the wrist (Fig 1). Punch biopsy demonstrated nonspecific findings of small vessel ectasia and minimal perivascular lymphocytes (Fig 2).
Fig 1.

Cutaneous findings of puffy hand syndrome. Erythema and edema of the bilateral hands with demarcation at the wrist.
Fig 2.
Histologic findings of puffy hand syndrome. Nonspecific findings of punch biopsy showed small vessel ectasia and minimal perivascular lymphocytic infiltrate.
Laboratory evaluation revealed negative antinuclear antibody, extractable nuclear antigen panel, and rheumatoid factor. Creatine kinase and aldolase levels were mildly and insignificantly elevated to 177.0 units/L (reference range, 45.0-145.0 units/L) and 10.5 units/L (reference range, <7.7 units/L), respectively. Creatinine levels, hepatic function tests, and hepatitis panels drawn 6 months prior were all normal. No imaging was performed. The patient's history of IVDU; presence of painless, erythematous edema of the hands; and negative laboratory and histologic evaluation established the diagnosis of puffy hand syndrome. She was referred to a lymphedema clinic for compression gloves.
Discussion
This case presents an unusual opportunity to consider the differential diagnosis for erythematous, edematous hands, specifically during pregnancy in a patient with a history of IVDU. Given this patient's history of occupational chemical exposure, irritant and allergic contact dermatitis were considered. However, no signs of spongiosis on pathology made this less likely. The patient's concomitant chronic joint pain suggested a potential autoimmune etiology such as systemic lupus erythematosus, early edematous phase of scleroderma, or rheumatoid arthritis. However, screening laboratory tests, including antinuclear antibody and rheumatoid factor, were negative, and pathology did not show characteristic changes of connective tissue disease. Erythromelalgia was considered; however, she denied associated burning pain and fluctuation with temperature change classically described with this diagnosis.
To our knowledge, this is the second reported case of puffy hand syndrome initially presenting during pregnancy.4 One other case has been reported in a pregnant woman after 9 years of intravenous cocaine use. In this case, the patient similarly experienced transient fluctuations of bilateral hand edema until worsening and persisting thereafter. In our patient with a history of IVDU, we propose that physiologic hypervolemia of pregnancy5 accelerated the onset of her symptoms by overwhelming the capacity of weakened lymphatics and veins. Although this condition may be more well-recognized in the addiction medicine and vascular surgery realms, it should also be recognized by dermatologists. Knowledge of this disorder should prompt dermatologists to ask the applicable social history questions and prevent inappropriate and aggressive treatments for alternative diagnoses.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not required.
References
- 1.Dean S.M. Images in vascular medicine. A curious cause of bilateral upper extremity lymphedema: ‘puffy hand syndrome’. Vasc Med. 2020;25(1):92. doi: 10.1177/1358863X19890008. [DOI] [PubMed] [Google Scholar]
- 2.del Giudice P., Durant J., Dellamonica P. Hand edema and acrocyanosis: “puffy hand syndrome”. Arch Dermatol. 2006;142(8):1084–1085. doi: 10.1001/archderm.142.8.1084. [DOI] [PubMed] [Google Scholar]
- 3.Barton M., Fett N. Red puffy hand syndrome mistaken for inflammatory arthritis. Dermatol Online J. 2020;26(6):4–7. [PubMed] [Google Scholar]
- 4.Kovács A.L., Rózsa A., Kálmán E., Gyömörei C., Schmidt E., Gyulai R. Puffy hand syndrome. Eur J Dermatol. 2017;27(4):415–417. doi: 10.1684/ejd.2017.3028. [DOI] [PubMed] [Google Scholar]
- 5.Sanghavi M., Rutherford J.D. Cardiovascular physiology of pregnancy. Circulation. 2014;130(12):1003–1008. doi: 10.1161/CIRCULATIONAHA.114.009029. [DOI] [PubMed] [Google Scholar]