Abstract
Mobile technology has become a ubiquitous part of everyday life and is changing the way we offer clinical care and perform clinical research. We have unprecedented access to data for one’s self-care, as well as for sharing with health care providers. Meeting the challenge posed by the influx of wearable device data requires a multidisciplinary team of researchers, clinicians, software developers, information technologists and statisticians. While the possibility of what can be achieved with the ever-evolving wearable technologies seems to be unlimited, regulatory agencies have provided a framework to establish standards for clinical applications, which will also impact research applications. Clinical programs and electronic medical records vendors should prepare to establish a framework to implement these technologies into clinicians’ workflow and to allow feedback to measure the impact on clinical outcome. In this article we discuss how a new brand of multidisciplinary care is evolving around mobile health devices and present a vision of up and coming technology in this space.
Introduction:
We have seen tremendous progress in understanding cancer biology and this has led to record number of new drug approvals for cancer. Patients with cancer continue to experience high rate of symptoms from their tumor in the form of fatigue, pain, decreased appetite, low mood or disturbed sleep. Cancer treatments are also associated with toxicity, which can negatively impact outcomes. Clinicians and researchers have struggled to measure these symptoms, as existing tools do not reflect true patient experiences. Current clinical tools have two major limitations. They are 1) difficult to reproduce across different clinical scenarios, 2) unable to measure or report symptoms in real time. In recent years we have seen growth in mobile health technology in all fields of medicine including oncology. In this article, we look to describe how modern day mobile and wearable technology is changing the way we offer clinical care and perform clinical research. We discuss a new brand of multidisciplinary care that is evolving around mobile health devices and present a vision of up and coming technology in this space.
Value proposition of wearable technologies and remote monitoring
The increasing availability and sophistication of mobile health technology continues to generate promise for oncology care and research 1. Mobile health, or mHealth, technology comprises devices that enable wireless communication or data transmission. The most common devices are mobile phones, and more recently smartphones and tablet computers, the latter of which can include sensors for activity, location, and biometrics. More recently, the commercial availability and consumer adoption of wearable devices and sensors has greatly increased, with the ability to connect wirelessly for data transmission and storage. Wearable health devices enable personal health tracking over extended periods of time. These include physical activity monitoring as well as ambulatory tracking of medically-relevant data such as vital signs and electrocardiography 2.
Most cancer treatments require episodic encounters between patients and their health care teams. Even during intensive treatment periods with chemotherapy, patients experience most of their care at home, away from the clinic setting. In the ambulatory setting, patients are typically required to monitor and evaluate diverse and complicated side effects themselves. Patients are also responsible for making potentially complex decisions on when to contact their health care team should side effects escalate 3.
Wearable and mobile technology can enable cost-effective and scalable opportunities for remote, and often real-time, monitoring of patients during critical periods of cancer care 4. By leveraging this technology, health care providers have access to both objective and patient-reported health data to facilitate clinical decisions that may result in better adherence, quality of life, and treatment outcomes. In addition, implementing mobile, wearable and sensor applications in clinical trials may better standardize data collection, and capture more precise and frequent data to better inform both study designs and understanding of the clinical benefits of therapies 1.
Systems that enable remote, real-time monitoring of patients’ symptoms and other health-related outcomes may offer cost-effective strategies to optimize cancer care outside of the clinic 5,3. Related systems that enable clinical decision-making have been used in the management of chronic conditions other than cancer 6. The need for additional research has been cited particularly to help define for which groups of patients and under which circumstances remote monitoring and wearable sensors are most appropriate, acceptable and effective, and offer the greatest value proposition for both patients and health care providers7,8.
Growing evidence supports the feasibility and benefits of using mobile and wearable technology and remote monitoring to improve outcomes in cancer patients during and after treatment. Studies have demonstrated the feasibility of implementing home-based sensors or wearable devices to measure various parameters (e.g., activity, weight, blood pressure, sleep, heart rate) along with mobile patient-reported outcome (PRO) reporting platforms with cancer patients undergoing chemotherapy or radiation treatment9,10,11. Collectively, these studies found high levels of acceptability and engagement with the technology, as demonstrated by a high degree of completion of monitoring requirements and device usage. These feasibility outcomes are a necessary step in furthering research and successful future implementation in clinical care. Randomized trials have shown that in-clinic and/or remote monitoring of symptoms during chemotherapy, when coupled with support by care providers upon worsening of symptoms, resulted in better quality of life, fewer treatment interruptions, and improved survival in cancer patients with or without metastatic disease 12–14. However, a recent systematic review of electronic systems for remote reporting and management of cancer treatment side effects only identified a few randomized trials, underscoring the need for additional rigorous research in this area. Greater attention should be paid toward measuring patient activation and engagement, which have been associated with better health outcomes 15.
The availability and widespread adoption of wearable physical activity monitors improves the ability to quantify physical activity in oncology care16. Recognizing the limitations of subjectively assessing performance status- a critical prognostic and clinical decision-making tool- preliminary studies suggest the feasibility of using wearable devices to capture real-time, objective activity data for assessment of performance status and physical function. Early findings show positive correlations between daily step counts and provider-assessed performance status and PROs (e.g., fatigue, quality of life, depressive symptoms), and observed reduced odds of adverse events with increased daily step counts 17. Higher levels of physical activity are associated with improved disease and quality of life outcomes after cancer diagnosis. Wearable activity devices also have the potential to help cancer survivors increase and maintain their activity levels. Studies have begun to explore the feasibility of wearable activity monitors in specific cancer populations. This includes endometrial cancer survivors, a group that is generally less physically active, and children with Acute Lymphoblastic Leukemia 18,19.
The ability to accurately track and store a broad range of objectively measurable health parameters offers unprecedented access to data for one’s self-care as well as for sharing with health care providers to aid in medical recommendations and management. However challenges exist in optimizing wearable and remote monitoring technology in oncology. This includes managing and interpreting the large amount of data generated from continuous monitoring, and strategies to integrate these data into electronic health records. The value proposition of wearable devices in oncology will increase by addressing these challenges and by identifying specific clinical scenarios where wearable technology and remote monitoring improves patient-centered outcomes and is feasible for both health care providers and patients.
Embarrassment of riches: Storing, managing, and interpreting the vast data produced by wearable technology and remote monitoring
Meeting the challenge posed by the influx of wearable device data requires a multidisciplinary team of researchers, clinicians, software developers, information technologists, and statisticians. Mobile technology has become a ubiquitous part of everyday life through smart watches, smart phones, and fitness bands. These popular consumer devices are attractive tools for monitoring patients remotely via activity tracking and electronic PRO. In addition, researchers have started incorporating these technologies into clinical trials. Storing, managing, and interpreting the vast data create new challenges.
Physical activity monitors, such as a FitBit fitness tracker (Fitbit, San Francisco, CA), Vivoactive smartwatch (Garmin, Olathe, KS), and the Apple Watch (Cupertino, CA) products collect individual’s data passively during the time that the device is worn via accelerometer, gyroscope, and heart rate sensors. Examples of data collected includes steps, distance walked or run, flights climbed, number of workout minutes, cycling distance, heart rate, sedentary minutes, light activity minutes, and vigorous activity minutes. Some of these are collected continuously while others are collected when the individual indicates that a particular activity is being performed, such as cycling. Heart rate monitoring, may occur at variable time points based on the user’s request and level of activity.
Collection
Prior to data collection, consent for sharing data will need to obtained from the patient. Individuals must have a reliable interface between their mobile technology and data collection, such as Wi-Fi or cellular service. As most data from connected devices are first transferred to and stored in the “cloud” in real-time this may be an issue for patients who live in remote areas or are traveling internationally. Each device’s capacity to store data can become an important factor in determining study objectives and selection of reliable devices. Multiple web based data warehouses have been developed to collate data from multiple devices. These services have dashboards to monitor patients and visualize data for commonly used measures such a physical activity, heart rate and sleep. Additional work is needed to develop tools for less validated measures such as cardiac rhythm, stress, blood pressure, pulmonary artery pressure, etc.
Storage
The data from physical activity monitors must be transferred from the individual’s wearable device to a secure database that has the ability to store very large amounts of content. For example, our study of ~300 patients who wore the Apple Watch daily for 3 months yielded 6 million kilobytes of data20. This may exceed the capacity of a medical institution’s computer systems. Solutions include external cloud-based products with a secure user interface, such as Microsoft Azure, Oracle Database, Google Cloud, Amazon Aurora, and others.
Remote monitoring of PROs, on the other hand, does not create nearly the same data storage challenges, simply because the amount of content is much smaller. Just like physical activity data, PROs must be transferred and stored in a secure server to ensure patient privacy. If being used in the clinical setting, it is ideal for the PROs to integrate into the electronic health record system.
Management
The data stored in the database, which may be local or in a cloud-based server, must then be accessed. Generally access is via a secure user interface with a complex password (“sourcekey”) of 50–100 characters. Due to the large volume of content, transfer of data may take a considerable amount of time (hours or even days) if not housed locally. This limits the ability to access the activity data in real-time, which is an issue particularly if the devices are used in the clinical setting.
In addition, updates to the operating system of the device may cause issues. All devices’ firmware need to be updated, including devices not yet distributed and those already in use by individuals. There may be issues related to data output. Dates of updates must be known by the IT and statistical team to be on the alert for aberrant values around the time of an update. Interoperability between systems will be key for this to thrive. This will require the community to agree on common elements, develop standard methodology and define normal ranges.
Interpretation
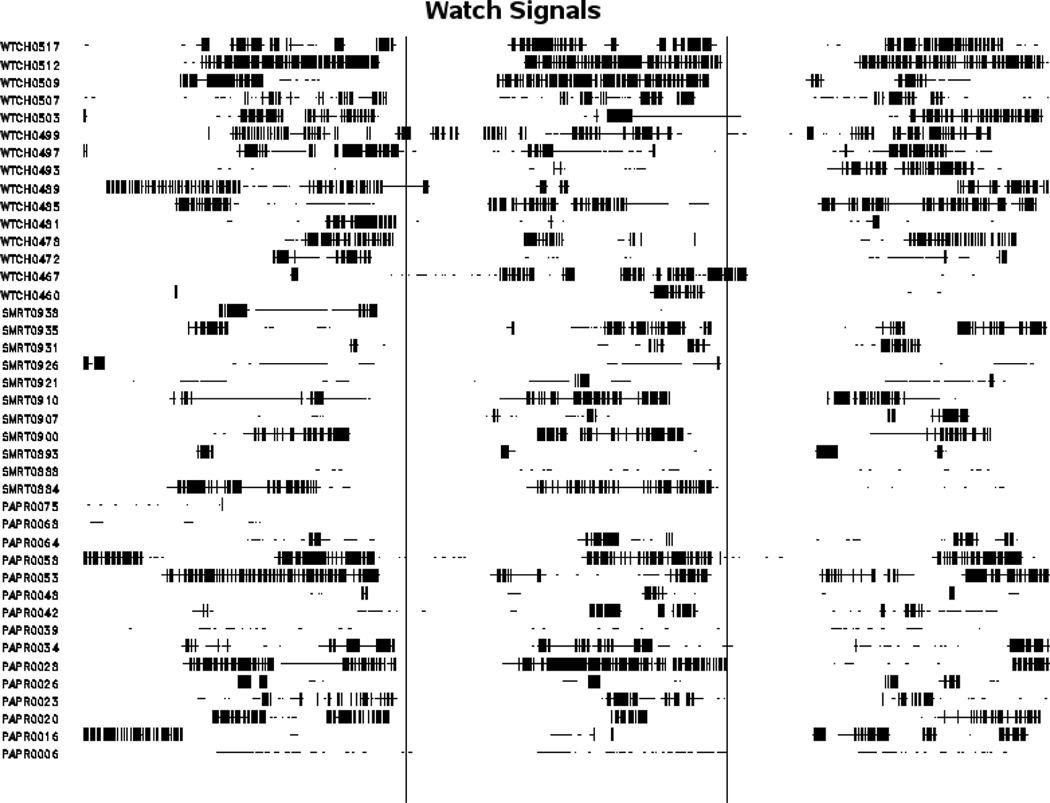
Collected data may require significant cleanup prior to interpretation. For example, additional activity data may be collected and stored in duplicate if individuals use exercise apps which also collect physical activity data (such as Strava, Runkeeper, etc.). In addition, the time zone for the activity monitor may not match the location (Apple Watch reports all data at Greenwich time). Gaps exist in the data, as activity is not continuously recorded (see figure 1). This makes it difficult to determine if individual is inactive vs. not wearing the device, as individuals need to wear the device a minimum number of hours per day in order to get reliable data for that day (in our study, we chose a minimum of seven hours/day and if any data was recorded by the watch during an hour, individuals were credited with wearing the device for the entire hour). Lastly, one needs to determine how to analyze the data - continuous measures may need to be converted to summary measures, such as average values per day. See table 1 as an example of final summarized data from a study utilizing wearable devices.
Figure 1.
Output of heart rate monitoring in a study of patients utilizing Apple Watches, with gaps in data and variable times of heart rate data collection
Table 1.
Example of Summary of Activity Levels in the One Week in a Clinical Study Utilizing the Apple Watch
| Activity Level | Mean (SD) | Range |
|---|---|---|
| Mean Steps Per Day | 4419.5 (3651.9) | 0 to 20,721.5 |
| Mean Distance Walking or Running Per Day (m) | 3210.1 (2925.4) | 0 to 19,959.7 |
| Mean Flights Climbed Per Day | 1.7 (2.6) | 0 to 18.0 |
| Mean Active Energy Burned Per Day (kcal) | 134.6 (115.1) | 0 to 733.0 |
| Mean Minutes of Workouts Per Day | 8.8 (35.6) | 0 to 408.2 |
| Mean Minutes of Exercise Per Day | 10.9 (14.6) | 0 to 99.0 |
| Mean Cycling Distance Per Day (m) | 53.6 (899.6) | 0 to 15,106.8 |
| Mean Minutes Sedentary Per Day | 257.5 (160.1) | 0.2 to 817.0 |
| Mean Minutes With Light Activity Per Day | 22.1 (21.7) | 0 to 135.5 |
| Mean Minutes With Moderate Activity Per Day | 4.2 (8.3) | 0 to 71.2 |
| Mean Minutes With Vigorous Activity Per Day | 0.5 (2.2) | 0 to 26.7 |
| Mean Heart Rate | 83.1 (10.5) | 63.8 to 193.6 |
For PROs, it is important that the database is built with a software developer and statistician working in concert, such that minimal conversion of data is necessary. Without coordination, PROs may be stored as XML files or streams of characters which require significant time and effort to convert. Once cleanup is performed, analysis can take place in any statistical software package, such as SAS, R, or STATA.
The Future of Wearable Technologies and Remote Monitoring in Health Care
The advances in the development of wearable and remote monitoring devices are growing exponentially. These platforms will provide more accurate measurements of physical status and physiological parameters in more convenient ways, and will soon influence different aspects of healthcare practices, from prevention (e.g., activity and eating behavior tracking, stress-level monitoring, dehydration warning), diagnosis (e.g., early detection), to disease management (e.g., drug-dose monitoring and reminders). In particular, efforts are underway in building the next generation wearable sensors to detect cancer-related chemical and biomarkers21. For example, wearable bandage and microneedle electrochemical sensing platforms have been developed to detect the presence of the tyrosinase enzyme biomarker on both the skin surface and within skin moles for rapid screening of skin melanoma 22
Parallel to the pursuit of more specific, sensitive, and stable devices is the powerful application of artificial intelligence (AI) using machine learning and data mining. The connectivity between devices and to the internet enables not only continuous data acquisition but also real-time information processing. For example, newer generations of commercially available activity trackers and smartwatches monitor both body movements and heart rate; providing personal analytics such as energy expenditure and sleep cycles. Based on the data, algorithms could be developed to identify patterns and help users recognizing how their behaviors might be impacting their health (e.g., a better night of sleep follows by a more active day than one’s usual level). Integration of data from different sources (e.g., mood, stress level, food log) would further enrich the knowledge base for algorithm development to refine the summary of past behaviors and experience and to predict future behaviors and the impact on health.
Swedish authors recently used machine learning algorithms to accurately predict outcomes in a large dataset of heart failure patients. This new mode of classification identified four distinct phenotypes that differed significantly in outcomes and responses to therapy. Provocatively, the algorithm predicted survival far better than the current gold standard, left ventricular ejection fraction (C-statistic 0.83 vs 0.52, respectively). 23
In addition to shaping the “quantified-self” trend for improving self-awareness, the big data and vast information from wearables also makes remote patient surveillance systems more comprehensive and offers opportunities for clinicians and healthcare professionals to make decisions and even intervene in real-time. For example, if an oncologist is interested in encouraging preoperative physical activity level in patients, data from activity trackers could be used to trigger messages being sent to patients and remind them to exercise if their activity goal is not met for the day. Again, algorithms could be built to further personalize the content and timing of such messages based on patients’ demographics, disease stage, psychosocial variables, and environments. AI would also be able to keep refining and optimizing the messages from continuous learning as more data feeds in.
While the possibilities of what one could do with the ever-evolving wearable technologies seem to be unlimited, one of the caveats is that we have to rely on the assumption that the devices will be working reliably as intended, constantly. Nevertheless, not all wearable devices are regulated in the same way. The majority of consumer-facing wearable products have no published data about their accuracy values. Wearable devices and digital health software are regulated by the U.S. Food & Drug Administration (FDA) if they claim a medical use intent. For example, the Apple Watch features heart rate measurement since its Series 1 model released in 2016. Because the intended use for the heart rate measurement is not for medical- but wellness-related purposes (e.g., to estimate workout intensity), it is not under FDA’s regulation. In late 2018, the release of Apple Watch Series 4 marks the first direct-to-consumer product that comes with FDA-approved built-in electrocardiogram (ECG) functionality. Shortly after, Alphabet also announced that its Verily Study Watch had been cleared by the FDA as a medical device that can record, store, transfer, and display ECG data. The race to have an FDA stamp on their wearable products signals a high interest from the technology companies entering the healthcare market, which further speeds up the medical device penetration among regular consumers. Recognizing this rising trend, FDA is also working on updating and refining their plan in guiding and regulating digital health-related products24.
Wearable devices and digital health software will change the way we practice medicine and perform clinical research. Primary care clinicians and cardiologists have begun seeing patients with self-detected arrhythmia. From a research perspective, the Apple Heart Study (NCT03335800), to be presented in 2019, will measure the detection of atrial fibrillation in 500,000 wearers of the newest Apple Watch. This study will shed light on the previously-unknown ambient prevalence of atrial fibrillation in a large population. It is the beginning of a new era in cardiology and will influence other fields of medicine in the near future.
Ever more screening and quantification of human biology is not a sure win. In atrial fibrillation screening with electrocargiograms, for instance, low disease prevalence, misdiagnosis, overuse of downstream testing, and high costs highlight the need for clinical trials that measure outcomes before widespread acceptance of novel monitoring technologies. 25 Clinical programs and electronic medical records vendors should prepare to establish a framework to implement these technologies into clinicians’ workflow and to allow feedback to measure the impact they have on clinical care.
With the emergence of wearable technologies, changes in how we evaluate, treat, and manage patients are inevitable. As clinicians and healthcare professionals, one could be an innovator or early adopter to push the boundary of what is possible, or be a conservative who raises critical concerns to ensure the integrity of medical practice and to protect our patients. The wisest clinicians will surely be the ones who mix both early adoption with a conservative bent, so as to separate hype from true benefit.
Summary:
Wearable technology is changing the way we collect and analyze health related data.
Data from mobile health devices require multidisciplinary teams to store and analyze the measures in a clinically relevant manner.
The volume of data produced by these devices needs specific technology to support handling and visualization.
Newer devices have enabled quantification of many health related measures and regulatory bodies have offered guidance on wearable technology.
Tweet: @yueliao @drcthompson @S_K_Peterson @drjohnm @ShaalanBeg
How are wearable devices changing the way we practice medicine? #ASCO19
What is the future of wearable devices and remote monitoring in health care? #ASCO19
So you want to use wearable devices in your clinical trial? What do you need to know? #ASCO19
Contributor Information
Yue Liao, Division of Cancer Prevention and Population Sciences, Department of Behavioral Science, MD Anderson Cancer Center, Houston, Texas.
Carrie Thompson, Division of Hematology, Department of Internal Medicine, Mayo Clinic, Rochester MN.
Susan Peterson, Division of Cancer Prevention and Population Sciences, Department of Behavioral Science, MD Anderson Cancer Center, Houston, Texas.
John Mandrola, Baptist Health Louisville, Louisville, Kentucky.
Muhammad Shaalan Beg, Division of Hematology and Medical Oncology, Department of Internal Medicine, UT Southwestern Medical Center.
References:
- 1.Cox SM LA, Volschemboum SL. Use of Wearable, Mobile, and Sensor Technology in Cancer Clinical Trials. JCO Clinical Cancer Informatics 2018;2:1–11. [DOI] [PubMed] [Google Scholar]
- 2.Dias D, Paulo Silva Cunha J. Wearable Health Devices-Vital Sign Monitoring, Systems and Technologies. Sensors (Basel) 2018;18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kofoed S, Breen S, Gough K, Aranda S. Benefits of remote real-time side-effect monitoring systems for patients receiving cancer treatment. Oncol Rev 2012;6:e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peterson SK PK . Creating a Health Information Technology Infrastructure to Support Comparative Effectiveness Research in Cancer. In: Hesse B AD, ed. Oncology Informatics: Academic Press; 2016:357–72. [Google Scholar]
- 5.Hicks LL, Fleming DA, Desaulnier A. The application of remote monitoring to improve health outcomes to a rural area. Telemed J E Health 2009;15:664–71. [DOI] [PubMed] [Google Scholar]
- 6.Ong MK, Romano PS, Edgington S, et al. Effectiveness of Remote Patient Monitoring After Discharge of Hospitalized Patients With Heart Failure: The Better Effectiveness After Transition -- Heart Failure (BEAT-HF) Randomized Clinical Trial. JAMA Intern Med 2016;176:310–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martin S, Kelly G, Kernohan WG, McCreight B, Nugent C. Smart home technologies for health and social care support. Cochrane Database Syst Rev 2008:CD006412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilson SR, Cram P. Another sobering result for home telehealth-and where we might go next. Arch Intern Med 2012;172:779–80. [DOI] [PubMed] [Google Scholar]
- 9.Wright AA, Raman N, Staples P, et al. The HOPE Pilot Study: Harnessing Patient-Reported Outcomes and Biometric Data to Enhance Cancer Care. JCO Clinical Cancer Informatics 2018:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Innominato P, Komarzynski S, Karaboue A, et al. Home-Based e-Health Platform for Multidimensional Telemonitoring of Symptoms, Body Weight, Sleep, and Circadian Activity: Relevance for Chronomodulated Administration of Irinotecan, Fluorouracil-Leucovorin, and Oxaliplatin at Home-Results From a Pilot Study. JCO Clin Cancer Inform 2018;2:1–15. [DOI] [PubMed] [Google Scholar]
- 11.Peterson SK, Shinn EH, Basen-Engquist K, et al. Identifying early dehydration risk with home-based sensors during radiation treatment: a feasibility study on patients with head and neck cancer. J Natl Cancer Inst Monogr 2013;2013:162–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Basch E, Deal AM, Kris MG, et al. Symptom Monitoring With Patient-Reported Outcomes During Routine Cancer Treatment: A Randomized Controlled Trial. J Clin Oncol 2016;34:557–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Basch E, Deal AM, Dueck AC, et al. Overall Survival Results of a Trial Assessing Patient-Reported Outcomes for Symptom Monitoring During Routine Cancer Treatment. JAMA 2017;318:197–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kearney N, McCann L, Norrie J, et al. Evaluation of a mobile phone-based, advanced symptom management system (ASyMS) in the management of chemotherapy-related toxicity. Support Care Cancer 2009;17:437–44. [DOI] [PubMed] [Google Scholar]
- 15.Warrington L, Absolom K, Conner M, et al. Electronic Systems for Patients to Report and Manage Side Effects of Cancer Treatment: Systematic Review. J Med Internet Res 2019;21:e10875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beg MS, Gupta A, Stewart T, Rethorst CD. Promise of Wearable Physical Activity Monitors in Oncology Practice. J Oncol Pract 2017;13:82–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gupta A, Stewart T, Bhulani N, et al. Feasibility of Wearable Physical Activity Monitors in Patients With Cancer. JCO Clin Cancer Inform 2018;2:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rossi A, Frechette L, Miller D, et al. Acceptability and feasibility of a Fitbit physical activity monitor for endometrial cancer survivors. Gynecol Oncol 2018;149:470–5. [DOI] [PubMed] [Google Scholar]
- 19.Hooke MC, Gilchrist L, Tanner L, Hart N, Withycombe JS. Use of a Fitness Tracker to Promote Physical Activity in Children With Acute Lymphoblastic Leukemia. Pediatr Blood Cancer 2016;63:684–9. [DOI] [PubMed] [Google Scholar]
- 20.Thompson CA YY, Bartz A, Kumar A, Ruddy KJ, Stan DL, Uhm JH, Warsame RM, Witzig TE, Novotny PJ, Sloan J. Patient-reported outcomes, emoji, and activity measured on the Apple Watch in cancer patients. Journal of Clinical Oncology 2018;36:6501-. [Google Scholar]
- 21.Yang YB, Yang XD, Yang YJ, Yuan Q. Aptamer-functionalized carbon nanomaterials electrochemical sensors for detecting cancer relevant biomolecules. Carbon 2018;129:380–95. [Google Scholar]
- 22.Ciui B, Martin A, Mishra RK, et al. Wearable Wireless Tyrosinase Bandage and Microneedle Sensors: Toward Melanoma Screening. Adv Healthc Mater 2018;7:e1701264. [DOI] [PubMed] [Google Scholar]
- 23.Ahmad T, Lund LH, Rao P, et al. Machine Learning Methods Improve Prognostication, Identify Clinically Distinct Phenotypes, and Detect Heterogeneity in Response to Therapy in a Large Cohort of Heart Failure Patients. J Am Heart Assoc 2018;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Digital Health Innovation Action Plan. 2018. at https://www.fda.gov/downloads/MedicalDevices/DigitalHealth/UCM568735.pdf.)
- 25.Mandrola J, Foy A, Naccarelli G. Screening for Atrial Fibrillation Comes With Many Snags. JAMA Intern Med 2018;178:1296–8. [DOI] [PubMed] [Google Scholar]