Abstract
Background
Teledermatology (TD) has emerged as a critical way of delivering care remotely in the COVID-19 pandemic.
Objective
We conducted a systematic review to assess how TD has been implemented worldwide.
Methods
We searched PubMed, Scopus, Embase, Web of Science, and Google Scholar for articles on the use of TD for patient care, written in English and published from December 1, 2019, to October 15, 2020.
Results
Twenty-seven studies were included, involving 16,981 patients. There was significant uptake of TD during the pandemic. Synchronous TD appeared to be more commonly implemented than asynchronous TD. Common ambulatory dermatoses such as acne or eczema were reported to be more amenable to TD assessment and management. TD also appeared to be useful for the diagnosis of cutaneous involvement of COVID-19 infection and follow-up of stable oncodermatology cases.
Limitations
A pooled analysis of all relevant outcomes was not always possible due to the heterogeneity in the methodologies of included studies.
Conclusion
TD is a useful and convenient tool for the management of common ambulatory dermatoses in the COVID-19 pandemic.
Key words: coronavirus, COVID-19, SARS-CoV-2, systematic review, teledermatology, telehealth, telemedicine
Abbreviations used: FTF, face-to-face; TD, teledermatology
Capsule Summary.
-
•
There is a surge in the utilization of teledermatology during the COVID-19 pandemic.
-
•
Teledermatology can be utilized to manage common ambulatory dermatoses and assess cutaneous manifestations of COVID-19 infection, reserving a face-to-face appointment for urgent clinical cases. However, there remain further challenges to the utilization of teledermatology around the world.
Introduction
The emergence of COVID-19 had transformed the delivery of health care worldwide. Teledermatology (TD) has been utilized as a crucial method of delivering care remotely to patients during the COVID-19 pandemic.1 TD has been validated as an effective mode of care before the pandemic2, 3, 4; however, the scale and ubiquity in which TD is practiced during the pandemic has been unprecedented. TD can be defined as the practice of dermatology at a distance.5 Asynchronous TD involves the transfer of medical information and clinical photographs to a dermatologist for a review at a different time and location, whereas synchronous TD is usually conducted via video conferencing or telephone calls that allow real-time interaction between the patient and physician.6 Hybrid TD involves a combination of both asynchronous and synchronous methods. We planned to analyze and report on the worldwide utilization of TD for patient care during the COVID-19 pandemic.
Methods
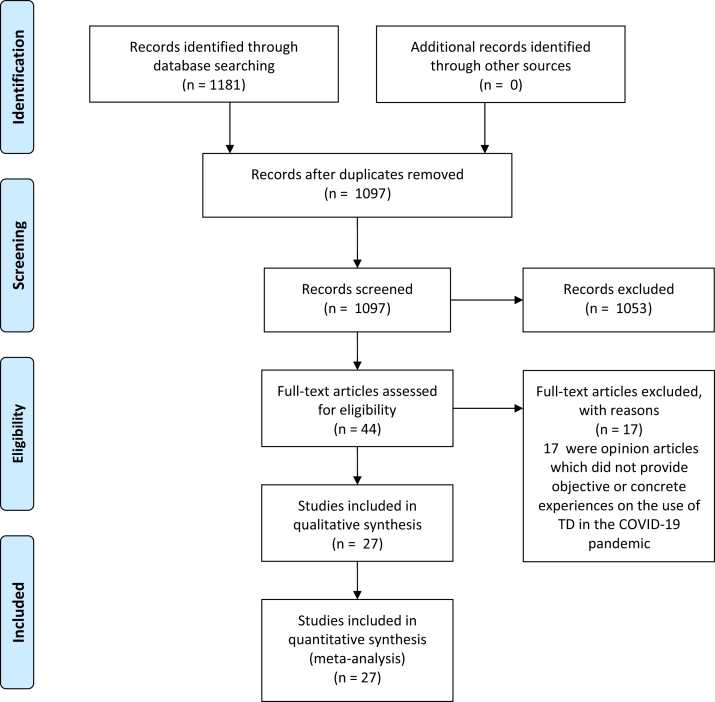
A study protocol was registered with the International Prospective Register of Systematic Reviews (CRD42021233065). We searched PubMed, Scopus, Embase, Web of Science, and Google Scholar for original articles written in English and published from December 1, 2019, to October 15, 2020. We excluded articles that lacked direct relevance to the use of TD for patient care in the COVID-19 pandemic (Fig 1). Articles that reported objective evidence or concrete experiences on the practice of TD were included for analysis. We extracted the following data from the included studies: country in which the study was conducted, method of TD, the population involved, dermatologic conditions managed, main findings, and limitations. The selection of articles for inclusion and data extraction was performed independently by C.H.L. and C.C.O. Any disagreements were resolved with the third independent author (S.Y.C.T.). A risk-of-bias assessment of all included studies was performed (Supplemental Table I available via Mendeley at https://doi.org/10.17632/xd6ftfpgmc.1). This systematic review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines.
Fig 1.
Summary of systematic review performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines. TD, Teledermatology.
Results
We summarized the findings of 27 articles on the use of TD for patient care, involving a total of 16,981 patients worldwide.
Ten studies reported on the use of asynchronous TD (Table I), 6 studies utilized synchronous TD (Table II), 8 studies utilized hybrid TD, and 3 studies did not specify the method of TD utilized (Table III). There had been a significant increase in the uptake of TD in dermatology practice worldwide during the pandemic.7, 8, 9, 10, 11 The prevalence of TD utilization across various institutions and countries was not consistently reported in most of the included articles. In a single-center study based in Texas, United States, Farshchian et al11 reported that more than 77% of all routine consultations were performed via TD.
Table I.
Asynchronous teledermatology
| Author, year | Country | Population; TD method(s) | Size | Findings | Limitations |
|---|---|---|---|---|---|
| Su et al,7 2020 | United States | Outpatients; asynchronous | 1564 | TD consultations increased by more than 20% during the pandemic. Common conditions managed were acne with isotretinoin or psoriasis with biologics. TD was able to facilitate routine dermatology care and open up FTF appointments for more urgent consultations. |
Limited reimbursement and limited efficacy data for TD |
| De Simone et al,13 2020 | Italy | Outpatients; asynchronous | 1032 | Surgical excisions of 416 oncodermatology cases completed with 53% of diagnostic appropriateness, comparable to prepandemic rate of 56%. TD also led to reduced health expenditure. | Not stated |
| Randolph et al,15 2021 | United States | Outpatients; asynchronous | 235 | Teletrichology is suitable for initial and follow-up examinations of telogen effluvium, alopecia areata, androgenic alopecia, frontal fibrosing alopecia, and central centrifugal cicatricial alopecia. | Poor image quality |
| Skayem et al,10 2020 | France | Outpatients; asynchronous | 182 | The increase in TD consultations was mostly due to suspected COVID-19 lesions. Cutaneous manifestations of COVID-19 infection included chilblains (72.5%), vasculitic lesions (7.5%), morbilliform rash (6.25%), pityriasis rosea-like lesions (3.75%), and urticaria (3.75%). | Not stated |
| Flynn et al,16 2020 | Ireland | Outpatients; asynchronous | 171 | Photo-triage system facilitated rapid assessment and treatment and reduced unnecessary FTF consultations. Common dermatoses managed were infantile haemangiomas (85%), port-wine stains (9%), vascular malformation (1%), and pyogenic granuloma (0.5%). |
Not stated |
| Marasca et al,12 2020 | Italy | Outpatients; asynchronous | 160 | Patients with acne who received SMS reminders had increased adherence to treatment and improved health-related quality of life. | Not stated |
| McDonald et al,17 2020 | United Kingdom | Outpatients; asynchronous | 122 | TD-based triage of skin cancer referrals were as follows: 35.1% discharged, 20.2% booked into surgery list, and 43.8% converted to FTF consultation. Histopathologic correlation with triage diagnosis was 72%. TD reduced the need for FTF appointments. | Not stated |
| Bergamo et al,8 2020 | Italy | Outpatients; asynchronous | 32 | In 27 (84.4%) of 32 TD consultations, diagnosis and treatment were provided and FTF consultations were avoided. 15.6% of TD referrals were converted to FTF consultations. Common dermatoses managed were tinea, corporis, psoriasis, eczema, intertrigo, photodermatitis, pityriasis rosea, and pyogenic granuloma. |
Low quality of clinical photographs; unable to conduct a proper physical examination and perform procedures. |
| McCrary et al,14 2020 | United States | Outpatients; asynchronous | 20 | Of all physicians, 59% self-rated “somewhat confident” in their dermoscopic abilities. Increased diagnostic accuracy (53.6%) with dermoscopic images, especially for malignant neoplasms. Dermoscopy-based TD led to appropriate triage of cases. | Not stated |
| Cartron et al,18 2020 | United States | Inpatients; asynchronous | 16 | Half of photographs used for TD were determined to be high-quality, whereas half were moderate quality. Of all TD consultations, 31.3% were converted to FTF consultation; 81.3% of TD consultations resulted in new diagnoses. TD consultations saved critical supplies of PPE. | Small sample size, no control group, and retrospective nature of the study. |
FTF, Face-to-face; PPE, personal protective equipment; SMS, short message service; TD, teledermatology.
Table II.
Synchronous teledermatology
| Author, year | Country | Population; TD method(s) | Size | Findings | Limitations |
|---|---|---|---|---|---|
| Gupta et al,22 2020 | India | Outpatients; synchronous | 300 | The commonest age group attending TD consultations was 20-40 years (40.7%), most resided in an urban environment, and 84% used a cell phone for TD consultation. Common conditions managed were eczema, dermatitis (19.3%), acne (14.6%), dermatophytosis, and fungal infections (15.7%). | Unable to palpate lesions perform procedures. TD limits the physician's ability to interact with patients. Possibility of missing or delaying diagnosis of incidental pathologies. |
| McGee et al,20 2020 | United States | Outpatients; synchronous | 274 | TD suitable for acne and nonspecific dermatitis. 60% of TD consults for lesions of concern converted to FTF consultation or biopsy or both. Older and non–English-speaking patients were less likely to access TD. | Limited proficiency with technology. Difficult to organize interpreter service. Patients hesitant to use TD. |
| Filippi et al,21 2020 | Italy | Outpatients; synchronous | 180 | In follow-up of 180 patients with psoriasis, 94.4% of cases remained well-controlled (less than 10% worsening of PASI). | Not stated |
| Villani et al,19 2020 | Italy | Outpatients; synchronous | 72 | TD is suitable for follow-up of patients with mild to moderate acne on topical therapies. All patients were satisfied with TD consultations. | Unable to conduct procedures. |
| Marasca et al,23 2020 | Italy | Outpatients; synchronous | 23 | Psychological video consultations for patients with chronic skin diseases reduced Dermatology Life Quality Index scores and improved overall psychological well-being. | Not stated |
| Farshchian et al,11 2020 | United States | Outpatients; synchronous | Not stated | More than 77% of consultations were conducted via TD. | Poor image quality, medicolegal liabilities, and concerns of patient privacy. Private practices have limited insurance coverage limiting uptake of TD. |
FTF, Face-to-face; PASI, Psoriasis Area and Severity Index; TD, teledermatology.
Table III.
Hybrid teledermatology and otherwise not specified
| Author, year | Country | Population; TD method(s) | Size | Findings | Limitations |
|---|---|---|---|---|---|
| Hydrid TD | |||||
| Kazi et al,9 2021 | United States | Outpatients; hybrid | 2623 | Increased TD consultation load (20 per 1,000 visits/year). 63.8% were synchronous TD. Less than 5% of TD visits converted to FTF consults. Common dermatosis managed were acne, dermatitis, and cutaneous neoplasms. |
Concerns with patient privacy and technological difficulties. Limited patient interaction with asynchronous TD. |
| Perkins et al,24 2020 | United States | Outpatients; hybrid | 1148 | Reduced FTF consultations with increased uptake of TD. Not suitable for total-body skin examinations Common dermatoses managed were acne, psoriasis, eczema, and rosacea. |
High costs of TD technology. Unable to conduct procedures. |
| Villani et al,26 2020 | Italy | Outpatients; hybrid | 620 | TD avoided the need for FTF consultation and reduced the risk of COVID-19 infection. High patient satisfaction and WhatsApp support group increased patient compliance. Common dermatoses managed were psoriasis, acne, and hidradenitis suppurativa. |
Limited data on efficacy, costs, feasibility, and accuracy of TD compared with FTF visits. |
| Brunasso et al,27 2020 | Italy | Outpatients; hybrid | 183 | Effective for follow-up of patients with psoriasis and acne on systemic therapy. TD allowed female physicians with family commitments to work from home. | Lack of patient privacy and no consistent quality; Medicolegal implications. |
| Shahidi-Dadras et al,28 2020 | Iran | Outpatients; hybrid | 167 | Inpatients with pemphigus vulgaris with previous rituximab therapy, TD-based survey identified 5 cases (2.99%) of COVID-19 infection. No reported cases of cutaneous manifestations of COVID-19 infection. | Lack of antibody testing or PCR testing for COVID-19. |
| Cinelli et al,29 2020 | Italy | Outpatients; hybrid | 105 | Follow-up of oncodermatology patients revealed the following: 50.5% had stable or improving conditions and 13.3% required an adjusted dose of the therapy previously prescribed. | Not stated |
| Mostafa et al,25 2020 | Egypt | Outpatients; hybrid | 70 | Reduced FTF consultations, TD efficient in triaging and treatment. High overall patient satisfaction, 91.5% of patients consider TD equivalent to FTF consultations. Common dermatoses managed: Urticaria, vitiligo, eczema, herpes zoster. |
Poor internet connection unable to support TD implementation; unable to conduct whole-body mole check and procedures, higher likelihood of misdiagnosis with limited photographs; and limited financial remuneration. |
| TD method not specified | |||||
| Franciosi et al,33 2020 | United States | Outpatients; TD method not specified |
6883 | TD consults have lower no-show rates than FTF consultations. Lack of private transportation, access to childcare, and inflexible work schedules contribute to higher no-show rates in the minority and Medicaid patients for FTF consultations. | Small sample size and single-institution experience. |
| Cristaudo et al,31 2020 | Italy | Outpatients; TD method not specified |
461 | 6.1% of all patients diagnosed with dermatitis of both hands. A higher incidence of irritant contact dermatitis was observed during the pandemic. | Not stated |
| Duong et al,32 2020 | France | Population not stated; WhatsApp messaging platform, including 400 dermatologists |
295 | 74% (N = 219) of cases were shared for the first time by the members, 4% (N = 11) were reposted from a dermatologist Facebook network, and 22% (N = 65) from the group administrator network. Chilblains or chilblain-like lesions represented 146 posts, and 149 posts included other suspected COVID-19–related skin eruption, for example, urticaria, rash, chickenpox-like or pityriasis rosea. 74% (N = 219) of cases were shared for the first time by the members, 4% (N = 11) were reposted from a dermatologist Facebook network, and 22% (N = 65) from the group admin-istrator network. Chilblains or chilblain-like lesions represented 146 posts, and 149 posts included other suspected COVID-19–re-lated skin eruption, for example, urticaria, rash, chickenpox-like or pityriasis rosea. Cutaneous manifestations of COVID-19 infection were chilblains or chilblain-like lesions, urticaria, rash, chickenpox-like or pityriasis rosea. |
Not stated |
| Lu et al,30 2020 | Australia | Outpatients; TD method not specified |
43 | TD utilized for skin cancer cases revealed the following: 11.6% of TD consultations were converted to FTF appointments due to inadequate or inaccurate assessment of the suspected malignant lesion. | Not stated |
FTF, Face-to-face; PCR, polymerase chain reaction; TD, teledermatology.
Asynchronous TD
The conditions reported to be commonly managed through asynchronous TD are acne,7,12 psoriasis,7,8 oncodermatology cases,13,14 hair disorders,15 infantile haemangiomas,16 tinea, eczema, intertrigo, photodermatitis, pityriasis rosea, and pyogenic granuloma.8
Clinical photographs are essential to asynchronous TD. A triage system based on clinical photographs was reported to be useful in the management of routine dermatology conditions, reducing unnecessary face-to-face (FTF) consultations.7,16 Bergamo et al8 reported that in 84% of cases of common ambulatory dermatoses, diagnosis and management were successfully conducted with TD; only 15.6% of cases required conversion to a FTF review. McDonald et al17 used high-quality clinical images taken by medical photographers to triage TD consultations, which led to a discharge rate of 35.1%, with conversion to FTF consultations in 43.8% of cases, and the remaining 20.2% were booked into a procedure list. Histopathologic correlation with the suspected triage diagnosis was 72% for suspected skin cancer cases.17 However, clinical assessment can be limited by the suboptimal quality of photographs.8,15 Cartron et al18 found that only half of all photographs used for asynchronous TD were determined to be of high quality, resulting in 31.3% of all TD reviews being converted to FTF visits. Two other studies have reported that the quality of images used in asynchronous TD is low and nonstandardized, making it challenging to reach a diagnosis.8,15
Dermoscopy-assisted TD has been used in photo-triage cases for consultation.18 McCrary et al14 reported their experience on dermoscopy-based triaging of nonneoplastic and benign neoplastic lesions, showing that diagnostic accuracy of TD consultations increased from 45.3% to 53.6% with dermoscopic images, particularly for malignant cutaneous lesions.14
TD has been rightfully utilized during the COVID-19 pandemic. Following the alert of cutaneous involvement of COVID-19 infection in France, Skayem et al10 reported that the mean number of TD consultations per day surged from 9.28 to 36.4, primarily for suspected COVID-19 cutaneous lesions. Utilization of TD had prevented unnecessary FTF consultations, which indirectly resulted in a reduction in the use of critical personal protective equipment supplies.18
TD was also utilized in the management of skin cancers and dermatooncology patients. Asynchronous TD was used to triage and manage suspected melanoma cases—416 surgical excisions were performed with 53% diagnostic appropriateness, comparable to the prepandemic rate of 56%.13
Synchronous TD
The dermatologic conditions that were reported to be amenable to synchronous TD are acne,19,20 psoriasis,21 eczema,22 nonspecific dermatitis,20,22 and dermatophytosis. McGee et al20 found that approximately 60% of lesions of concern that were seen via TD had to be converted to FTF review or biopsy, or both, suggesting that assessment of lesions of concern for malignancy and whole-body skin checks were best accomplished via FTF consultations. Marasca et al23 reported that the use of psychological video consultations had improved psychological well-being and reduced Dermatology Life Quality Index scores of patients with chronic skin diseases.
In a retrospective, observational study involving 300 patients at 2 medical centers, Gupta et al22 reported that the profile of patients attending TD consultations differed from those attending FTF consultations. The most common age group of patients attending TD consultations was 20 to 40 years of age; the majority of them resided in an urban environment and used a mobile phone for TD consultation.22 Older and non–English-speaking patients were less likely to have access to synchronous TD.20 Similar to asynchronous TD, the image quality of synchronous TD may also be suboptimal, leading to a higher likelihood of missing incidental pathologies such as skin cancers.22
Hybrid TD
Dermatoses that are reported to be amenable to hybrid TD are acne,9,24 rosacea,24 psoriasis,24 eczema,24 cutaneous neoplasms,9 urticaria,25 vitiligo,25 herpes zoster,25 and hidradenitis suppurativa.26 A diagnosis of acne was reported to be more common with asynchronous TD than that with synchronous TD.9
In a large study involving 2623 patients, Kazi et al9 reported on their experience with utilizing hybrid TD in their institution, which showed that TD was also found to be an efficient mode of triaging and managing common conditions, reducing the need for FTF consultations24, 25, 26; 63.8% of consultations were conducted with synchronous TD. Interestingly, Kazi et al9 also reported that antibiotics and nonretinoid acne medications were more commonly prescribed with asynchronous TD than that with synchronous TD, whereas biologics and immunomodulators were more commonly prescribed via synchronous TD than that with asynchronous TD. The majority of patients with chronic conditions such as psoriasis and acne on systemic therapies can be managed via TD, showing that remote monitoring with TD was effective in maintaining remission and preventing poor outcomes.27 Kazi et al9 reported that synchronous TD is preferred for managing complex medical dermatology patients, including immunobullous disorders and connective tissue diseases.
During the COVID-19 pandemic, TD was utilized to successfully identify 5 cases of COVID-19 infection in a cohort of 167 Iranian patients with pemphigus vulgaris who received previous rituximab therapy.28
Cinelli et al29 reported that the majority of dermatooncology patients had improved or remained clinically stable when followed-up with TD. However, inadequate or inaccurate assessment occurred in 11.6% of TD consultations for suspected cancerous skin lesions, which required conversion to FTF appointments, resulting in a mean delay in care of 9.8 days.30 In addition, Perkins et al24 reported that whole-body skin checks and lesions of concern requiring biopsy were less amenable to management with TD.
TD method not specified
There are 4 studies in which the method of TD was not specified. Cristaudo et al31 reported that a higher incidence of irritant hand dermatitis was observed via TD consultations during the pandemic compared with that during the prepandemic era. Lu et al30 reported on the use of TD for the assessment and management of skin cancers—11.6% of TD cases had to be converted to an FTF visit due to inaccurate or inadequate assessment of the suspected malignant lesion.
Duong et al32 showed that mobile TD was useful in the characterization of cutaneous manifestation of COVID-19 infection. During the COVID-19 pandemic, 400 French dermatologists shared information and clinical images of 295 cases via the WhatsApp mobile messaging application, which led to subsequent discussion and conclusion that chilblains is the most common cutaneous manifestation of COVID-19 infection.32
Francisosi et al33 found that TD has lower no-show rates than FTF visits, possibly related to the lack of transportation, poor access to child care, and inflexible work arrangements that discourage patients from attending FTF visits, accounting for higher no-show rates, especially in the minority groups and those from a lower socioeconomic status. Conversely, there were a greater number of Medicaid enrollees and those under the age of 50 years attending TD consultations in the United States.33
Discussion
In this review, there was no reporting of the prevalence of TD utilization rate in almost all of the included studies, with only 1 study reporting a TD utilization rate of 77% within a health care institution in the United States.11 Synchronous forms of TD were reported to be more commonly used than asynchronous TD.9,34,35 Common ambulatory dermatoses such as acne and eczema were reported to be more amenable to management via TD. However, medically complex conditions such as immunobullous diseases and connective tissue diseases are reported to be more suitable for hybrid TD.9 These complex cases would likely require in-depth history taking via synchronous TD, supplemented by high-quality clinical images, in order to facilitate appropriate clinical assessment and management. TD has been aptly utilized in the fight against the COVID-19 pandemic, assisting with remote management of routine ambulatory dermatosis and diagnosis of cutaneous manifestations of COVID-19 infection.10,28,32 There had been a rise in COVID-19–related dermatoses, such as maskne, hand eczema, and irritant contact dermatitis from the use of handrubs.34,36, 37, 38, 39, 40, 41, 42 TD is well-suited to manage these pandemic-related dermatoses without the need for FTF appointments. TD would allow patients to maintain access to dermatologic care remotely, while minimizing the risk of COVID-19 transmission.
There are conflicting results on the use of TD for skin cancers and oncodermatology cases. Assessment of suspected malignant skin lesions such as melanoma via TD was associated with comparable diagnostic accuracy, which is enhanced with dermatoscopic photographs and has a good histopathologic correlation with the suspected triage diagnosis. Cinelli et al29 reported that most oncodermatology patients either improved or remained stable when followed-up with TD. However, Lu et al30 argued that inaccurate assessment of malignant lesions via TD occurred in 11.6% of all cases, requiring conversion into FTF visits and a delay in care.24 Additionally, whole-body skin checks and assessing lesions of concern requiring biopsy were less suitable for TD.43 This is likely because patients may not be able to take pictures or videos of hard-to-reach areas to facilitate visual diagnosis. These areas include the back, buttocks, posterior aspect of the upper and lower limbs, and soles. Additionally, patients may not feel comfortable taking pictures or showing sensitive areas of their body, such as the genital region, via video consultations. Hence, addressing these concerns are best accomplished with FTF consultations.8
The incorporation of TD into routine clinical care can be an effective way of remotely managing common skin diseases. From this review, the rate of conversion from a TD consultation to an FTF visit ranged from 11.6% to 43.8%, suggesting that more than half of routine dermatology clinic caseloads can be successfully managed via TD. TD also has significantly lower no-show rates compared with FTF visits. Thus, for health care systems around the world, the use of TD would translate to minimizing the risk of COVID-19 transmission,26 saving critical supplies of personal protective equipment,18 strategic deployments of limited medical manpower and resources, and extending access to dermatologic care to a greater number of people.
However, successful TD consultations rely on high-quality clinical photographs,9,17,44,45 especially for asynchronous TD. Studies have suggested that the use of high-quality clinical photographs for TD consultations increased the diagnostic accuracy and reduced FTF consultations during the pandemic.17,44,45 TD consultations have been well-received by the majority of patients,19 and it can be utilized to boost adherence to medical treatment12,29 and improve the patients' quality of life.
There are several limitations associated with the use of TD. TD does not allow clinicians to perform bedside physical examination or procedures such as skin biopsies at the same opportunity during the consultation,8,22,28 potentially leading to misdiagnosis and a delay in the care provided when a conversion to FTF visit is required. This is especially relevant during this pandemic, as reducing the number of encounters that patients have with health care workers is paramount to reducing the risk of COVID-19 transmission. Asynchronous TD also restricts the ability of the clinician to interact with patients to establish rapport.22 Furthermore, there are concerns of medicolegal implications and the possibility of a breach of patient privacy when medical information is transmitted electronically.9,11,27 In developing countries, the lack of infrastructure for stable internet connection impedes the access to TD.8,25
There appears to be limited data on financial reimbursement for TD consultations in the pandemic. The lack of government support and financial reimbursements in certain countries may have prohibited the utilization of TD.7,25 In the United States, TD consultations conducted by public institutions are covered by Medicaid insurance, whereas private practices are restricted by varying levels of insurance coverage.9,11,45
In order to encourage uptake of TD, more has to be done to promote the TD as an accurate46,47 and feasible option of replacing FTF consultations and improving communication between clinicians and patients.32 Professional bodies have developed clinical guidelines and resources to guide health care providers to implement TD during the pandemic.48 Health care institutions should consider training clinicians to provide high-quality TD services. Governments could consider enhancing existing information technology infrastructure and providing appropriate financial reimbursements to support TD.
Limitations
The limitations of this study include restricting the search of articles to those written only in English. Due to the heterogeneity of the methodologies used in different studies, the outcomes reported in these studies were different and inconsistent. Therefore, it was not always possible to conduct a pooled analysis of all relevant outcomes. Additionally, most of the included studies reported a combination of descriptive, quantitative, and experiential data on the use of TD during the pandemic, and there were limited data on financial support from governments for TD.
Conclusion
This review showed that TD can be used for remote assessment and management of common ambulatory dermatoses, reducing the risk of transmission of COVID-19. Future studies should address the extended use of TD for patient care and educational purposes since the start of the pandemic. The findings derived from this study would be useful for optimizing existing TD services, given the resurgence of COVID-19 cases around the world.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not required as per the institutional policy of Singapore General Hospital.
References
- 1.Price K.N., Thiede R., Shi V.Y., Curiel-Lewandrowski C. Strategic dermatology clinical operations during the coronavirus disease 2019 (COVID-19) pandemic. J Am Acad Dermatol. 2020;82(6):e207–e209. doi: 10.1016/j.jaad.2020.03.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Warshaw E.M., Hillman Y.J., Greer N.L. Teledermatology for diagnosis and management of skin conditions: a systematic review. J Am Acad Dermatol. 2011;64(4):759–772. doi: 10.1016/j.jaad.2010.08.026. [DOI] [PubMed] [Google Scholar]
- 3.Snoswell C., Finnane A., Janda M., Soyer H.P., Whitty J.A. Cost-effectiveness of store-and-forward teledermatology: a systematic review. JAMA Dermatol. 2016;152(6):702–708. doi: 10.1001/jamadermatol.2016.0525. [DOI] [PubMed] [Google Scholar]
- 4.Mounessa J.S., Chapman S., Braunberger T. A systematic review of satisfaction with teledermatology. J Telemed Telecare. 2018;24(4):263–270. doi: 10.1177/1357633X17696587. [DOI] [PubMed] [Google Scholar]
- 5.Eedy D.J., Wootton R. Teledermatology: a review. Br J Dermatol. 2001;144(4):696–707. doi: 10.1046/j.1365-2133.2001.04124.x. [DOI] [PubMed] [Google Scholar]
- 6.Finnane A., Dallest K., Janda M., Soyer H.P. Teledermatology for the diagnosis and management of skin cancer: a systematic review. JAMA Dermatol. 2017;153(3):319–327. doi: 10.1001/jamadermatol.2016.4361. [DOI] [PubMed] [Google Scholar]
- 7.Su M.Y., Das S. Expansion of asynchronous teledermatology during the COVID-19 pandemic. J Am Acad Dermatol. 2020;83(6):e471–e472. doi: 10.1016/j.jaad.2020.08.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bergamo S., Calacione R., Fagotti S. Teledermatology with general practitioners and pediatricians during COVID-19 outbreak in Italy: preliminary data from a second-level dermatology department in North-Eastern Italy. Dermatol Ther. 2020;33(6):e14040. doi: 10.1111/dth.14040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kazi R., Evankovich M.R., Liu R. Utilization of asynchronous and synchronous teledermatology in a large health care system during the COVID-19 pandemic. Telemed J E Health. 2021;27(7):771–777. doi: 10.1089/tmj.2020.0299. [DOI] [PubMed] [Google Scholar]
- 10.Skayem C., Cassius C., Ben Kahla M. Teledermatology for COVID-19 cutaneous lesions: substitute or supplement? J Eur Acad Dermatol Venereol. 2020;34(10):e532–e533. doi: 10.1111/jdv.16630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Farshchian M., Potts G., Kimyai-Asadi A., Mehregan D., Daveluy S. Outpatient teledermatology implementation during the COVID-19 pandemic: challenges and lessons learned. J Drugs Dermatol. 2020;19(6):683. [PubMed] [Google Scholar]
- 12.Marasca C., Ruggiero A., Fontanella G., Ferrillo M., Fabbrocini G., Villani A. Telemedicine and support groups could be used to improve adherence to treatment and health-related quality of life in patients affected by inflammatory skin conditions during the COVID-19 pandemic. Clin Exp Dermatol. 2020;45(6):749. doi: 10.1111/ced.14245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Simone P., Iorio A., Ardigo M. Comment on “Rescheduling of clinical activities and teleconsulting for public dermatology. Two prompt answers to COVID-19 emergency”. Int J Dermatol. 2020;59(10):1284. doi: 10.1111/ijd.15026. [DOI] [PubMed] [Google Scholar]
- 14.McCrary M.R., Rogers T., Yeung H., Krueger L., Chen C.S. Would dermoscopic photographs help triage teledermatology consults in the COVID-19 era? Clin Cancer Res. 2020;28:PO-042. [Google Scholar]
- 15.Randolph M., Al-Alola A., Tosti A. Diagnosis of hair disorders during the COVID-19 pandemic: an introduction to teletrichoscopy. J Eur Acad Dermatol Venereol. 2021;35(3):e167–e168. doi: 10.1111/jdv.16989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Flynn A., O'Connor C., Murphy M. Photo-triage of infantile hemangiomas: potential to reduce healthcare exposure in the COVID19 pandemic. J Dermatolog Treat. August 12, 2020 doi: 10.1080/09546634.2020.1808153. [DOI] [PubMed] [Google Scholar]
- 17.McDonald C.R., Watson L., Shim T., Ilchyshyn A. Community-based medical photography improves skin cancer teledermatology triage during the national COVID-19 pandemic. Br J Dermatol. 2020;183(suppl 1):207. [Google Scholar]
- 18.Cartron A.M., Rismiller K., Trinidad J.C.L. Store-and-forward teledermatology in the era of COVID-19: a pilot study. Dermatol Ther. 2020;33(4):e13689. doi: 10.1111/dth.13689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Villani A., Annunziata M.C., Abategiovanni L., Fabbrocini G. Teledermatology for acne patients: how to reduce face-to-face visits during COVID-19 pandemic. J Cosmet Dermatol. 2020;19(8):1828. doi: 10.1111/jocd.13519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McGee J.S., Reynolds R.V., Olbricht S.M. Fighting COVID-19: early teledermatology lessons learned. J Am Acad Dermatol. 2020;83(4):1224–1225. doi: 10.1016/j.jaad.2020.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Filippi F., Loi C., Evangelista V., Bardazzi F. COVID-19 era: a chance to learn something new about monitoring psoriatic patients in biological therapy. Dermatol Ther. 2020;33(4):e13805. doi: 10.1111/dth.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gupta M., Bhargava S. The profile of teledermatology consultations during the COVID-19 pandemic: an observational study. Our Dermatol Online. 2020;11(suppl 2):10–12. [Google Scholar]
- 23.Marasca C., De Rosa A., Fabbrocini G. Psychological teleconsultations in patients suffering from chronic skin diseases during the COVID-19 era: a service to improve patients' quality of life. J Dermatolog Treat. October 12, 2020 doi: 10.1080/09546634.2020.1809625. [DOI] [PubMed] [Google Scholar]
- 24.Perkins S., Cohen J.M., Nelson C.A., Bunick C.G. Teledermatology in the era of COVID-19: experience of an academic department of dermatology. J Am Acad Dermatol. 2020;83(1):e43–e44. doi: 10.1016/j.jaad.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mostafa P.I.N., Hegazy A.A. Dermatological consultations in the COVID-19 era: is teledermatology the key to social distancing? An Egyptian experience. J Dermatolog Treat. July 7, 2020 doi: 10.1080/09546634.2020.1789046. [DOI] [PubMed] [Google Scholar]
- 26.Villani A., Megna M., Scalvenzi M., Fabbrocini G., Ruggiero A. Teledermatology and chronic skin diseases: real life experience in a Southern Italian dermatologic centre. Dermatol Ther. 2020;33(6):e13839. doi: 10.1111/dth.13839. [DOI] [PubMed] [Google Scholar]
- 27.Brunasso A.M.G., Massone C. Teledermatologic monitoring for chronic cutaneous autoimmune diseases with smartworking during COVID-19 emergency in a tertiary center in Italy. Dermatol Ther. 2020;33(4):e13495. doi: 10.1111/dth.13695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shahidi-Dadras M., Abdollahimajd F., Ohadi L. COVID-19 in pemphigus vulgaris patients with previous rituximab therapy: a tele-medicine experience. J Dermatolog Treat. July 9, 2020 doi: 10.1080/09546634.2020.1789041. [DOI] [PubMed] [Google Scholar]
- 29.Cinelli E., Fabbrocini G., Fattore D., Marasca C., Damiani G., Annunziata M.C. Safe distance, safe patients! Therapeutic management of oncological patients affected by cutaneous and mucosal adverse events during the COVID-19 pandemic: an Italian experience. Support Care Cancer. 2020;28(9):3991–3993. doi: 10.1007/s00520-020-05563-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lu D., Webb A. Pitfalls of telehealth in the management of skin cancer: a COVID-19 perspective. Australas J Plast Surg. 2020;3:64–66. [Google Scholar]
- 31.Cristaudo A., Pigliacelli F., Pacifico A., Damiani G., Iacovelli P., Morrone A. Teledermatology and hygiene practices during the COVID-19 pandemic. Contact Dermatitis. 2020;83(6):536. doi: 10.1111/cod.13683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Duong T.A., Velter C., Rybojad M. Did Whatsapp® reveal a new cutaneous COVID-19 manifestation? J Eur Acad Dermatol Venereol. 2020;34(8):e348–e350. doi: 10.1111/jdv.16534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Franciosi E.B., Tan A.J., Kassamali B., O'Connor D.M., Rashighi M., LaChance A.H. Understanding the impact of teledermatology on no-show rates and health care accessibility: a retrospective chart review. J Am Acad Dermatol. 2021;84(3):769–771. doi: 10.1016/j.jaad.2020.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Altunisik N., Turkmen D., Calikoglu E., Sener S. Views and experiences of dermatologists in Turkey about teledermatology during the COVID-19 pandemic. J Cosmet Dermatol. 2020;19(10):2460–2463. doi: 10.1111/jocd.13677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moscarella E., Pasquali P., Cinotti E., Tognetti L., Argenziano G., Rubegni P. A survey on teledermatology use and doctors' perception in times of COVID-19. J Eur Acad Dermatol Venereol. 2020;34(12):e772–e773. doi: 10.1111/jdv.16843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Singh M., Pawar M., Bothra A., Choudhary N. Overzealous hand hygiene during the COVID 19 pandemic causing an increased incidence of hand eczema among general population. J Am Acad Dermatol. 2020;83(1):e37–e41. doi: 10.1016/j.jaad.2020.04.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tan S.W., Oh C.C. Contact dermatitis from hand hygiene practices in the COVID-19 pandemic. Ann Acad Med Singap. 2020;49(9):674–676. [PubMed] [Google Scholar]
- 38.Alsaidan M.S., Abuyassin A.H., Alsaeed Z.H., Alshmmari S.H., Bindaaj T.F., Alhababi A.A. The prevalence and determinants of hand and face dermatitis during COVID-19 pandemic: a population-based survey. Dermatol Res Pract. 2020;2020:6627472. doi: 10.1155/2020/6627472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bhatia R., Sindhuja T., Bhatia S. Iatrogenic dermatitis in times of COVID-19: a pandemic within a pandemic. J Eur Acad Dermatol Venereol. 2020;34(10):e563–e566. doi: 10.1111/jdv.16710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kiely L.F., Moloney E., O'Sullivan G., Eustace J.A., Gallagher J., Bourke J.F. Irritant contact dermatitis in healthcare workers as a result of the COVID-19 pandemic: a cross-sectional study. Clin Exp Dermatol. 2021;46(1):142–144. doi: 10.1111/ced.14397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lan J., Song Z., Miao X. Skin damage among health care workers managing coronavirus disease-2019. J Am Acad Dermatol. 2020;82(5):1215–1216. doi: 10.1016/j.jaad.2020.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Teo W.L. Diagnostic and management considerations for “maskne” in the era of COVID-19. J Am Acad Dermatol. 2021;84(2):520–521. doi: 10.1016/j.jaad.2020.09.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Asabor E.N., Bunick C.G., Cohen J.M., Perkins S.H. Patient and physician perspectives on teledermatology at an academic dermatology department amid the COVID-19 pandemic. J Am Acad Dermatol. 2021;84(1):158–161. doi: 10.1016/j.jaad.2020.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Haider Z., Zaki I. Teledermatology in the West Midlands during the COVID-19 pandemic. Br J Dermatol. 2020;183(suppl 1):203–204. [Google Scholar]
- 45.Gorrepati P.L., Smith G.P. Analysis of availability, types, and implementation of teledermatology services during COVID-19. J Am Acad Dermatol. 2020;83(3):958–959. doi: 10.1016/j.jaad.2020.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Piccolo D., Smolle J., Wolf I.H. Face-to-face diagnosis vs telediagnosis of pigmented skin tumors: a teledermoscopic study. Arch Dermatol. 1999;135(12):1467–1471. doi: 10.1001/archderm.135.12.1467. [DOI] [PubMed] [Google Scholar]
- 47.Keller J.J., Johnson J.P., Latour E. Inpatient teledermatology: diagnostic and therapeutic concordance among a hospitalist, dermatologist, and teledermatologist using store-and-forward teledermatology. J Am Acad Dermatol. 2020;82(5):1262–1267. doi: 10.1016/j.jaad.2020.01.030. [DOI] [PubMed] [Google Scholar]
- 48.COVID-19: teledermatology. American Academy of Dermatology. https://www.aad.org/member/practice/coronavirus/clinical-guidance Accessed March 1, 2021.