Abstract
Initially thought of as a respiratory infection, coronavirus disease-2019 (COVID-19) is now recognized as a complex disease with a wide clinical spectrum, including digestive involvement. While several studies have evaluated chest imaging findings in COVID-19, few papers have looked at the abdominal imaging features of these patients. Liver, biliary, pancreas and bowel involvement have been reported in COVID-19 infected patients. In this review, we aim to summarize currently available data related to abdominal imaging techniques in COVID-19, in accordance with relevant clinical and laboratory workup of these patients. Underlying mechanisms, indications and imaging findings related to COVID-19 are discussed based on published data. Also, practice points for clinicians are highlighted in order to adequately recognize digestive-related injuries of severe acute respiratory syndrome coronavirus 2 infection. While there’s been a steady accumulation of data with respect to abdominal imaging findings in COVID-19, currently available recommendations are based on limited research. There is a wide spectrum of abdominal imaging findings in COVID-19, which includes hepato-biliary, pancreatic and luminal pathology.
Keywords: COVID-19, Gastrointestinal, Digestive, Features, Imaging, Ultrasound, Computed tomography
Core Tip: Initially being thought of as a respiratory infection, coronavirus disease-2019 (COVID-19) is now widely recognized as a complex disease with systemic features. Gastrointestinal manifestations have been reported with high prevalence in severe acute respiratory syndrome coronavirus 2 infected patients, including gut, pancreas, liver and biliary dysfunction. In this review we summarize and analyze currently available evidence on abdominal imaging techniques, indications and findings in COVID-19, in accordance with relevant clinical and laboratory workup of these patients.
INTRODUCTION
In late December 2019, a cluster of pneumonia cases of unknown origin was reported in Wuhan, Hubei province, China. The causative agent was identified as a novel coronavirus, linked to the severe acute respiratory syndrome (SARS). The virus was named SARS coronavirus 2 (SARS-CoV-2) and the related disease coronavirus disease-2019 (COVID-19). The novel coronavirus rapidly spread worldwide, and since March 11th 2020, the date on which COVID-19 was declared a pandemic[1], over 150 million cases and 3.2 million COVID-19 associated deaths have been reported[2].
Initially being thought of as a respiratory infection, COVID-19 is now recognized as a complex disease with a wide spectrum of presentations, from viral pneumonia and flu-like symptoms to acute hepatitis and Kawasaki-like disease[3,4]. The systemic nature of COVID-19 is related to the interaction of SARS-CoV-2 with the human body, mediated by angiotensin converting enzyme 2 (ACE2) expressed on cell surfaces[5]. ACE2 is most abundant in alveolar epithelium, but is also found in large amounts in enterocytes, vascular endothelium, liver and biliary epithelium[6]. Binding of SARS-CoV-2 at these susceptible extrapulmonary sites can generate symptoms directly related to the infected organ. Moreover, several reports have identified SARS-CoV-2 to be present in stool samples of infected patients[7-9], and there have been proposals to use anal swabs for SARS-CoV-2 detection and follow-up of infected individuals[10].
With regard to involvement of the gastrointestinal tract, several studies have shown high prevalence of digestive symptoms in COVID-19[7,11,12]. This was explained by the high density of ACE2 receptor (the cell entry point for SARS-CoV-2) in the small bowel and pancreas, but also as a side effect of COVID-19 related therapy and secondary to systemic inflammation and ischemia[13]. Not least, laboratory changes reflecting on gut or hepato-bilio-pancreatic pathology have been reported in COVID-19. In this setting, abdominal imaging has been used to define the cause of symptoms and laboratory abnormalities in these patients.
While an abundance of papers has described chest imaging findings in COVID-19, few articles have focused on abdominal imaging features of these patients. In this review we aim to summarize and analyze current evidence on abdominal imaging techniques, indications and findings in COVID-19, in accordance with relevant clinical and laboratory workup of these patients.
ABDOMINAL IMAGING
Abdominal imaging reported in COVID-19 patients include abdominal ultrasound and cross-sectional imaging techniques such as computed tomography (CT) and magnetic resonance imaging (MRI). A literature search on the topic also revealed isolated reports of plain abdominal X-ray, endoscopy or positron emission tomography CT (PET-CT) findings in COVID-19 patients.
Ultrasound
Abdominal ultrasound is being routinely used in patients with abdominal complaints. With regard to COVID-19, ultrasound (US) has been mostly indicated to evaluate for abdominal pain and abnormal liver function tests. While sometimes the abdominal pain does not reflect digestive pathology and is probably referred pain as the one seen in basilar pneumonias, the prevalence of transaminitis in COVID-19 has been estimated at 15%[14]. Sonographic examination has been also ordered for abdominal distention, suspected sepsis, increase in renal function tests or drop in hemoglobin[15]. Abdominal sonographic scanning also includes evaluation of hydration status by assessment of the inferior vena cava, presence of ascites (also pericardial or pleural effusions) or hydronephrosis[16].
In the study by Abdelmohsen et al[15] which aimed to characterize the sonographic abdominal imaging findings in COVID-19 intensive care patients, the most frequent sonographic finding was hepatomegaly (56.09%), followed by biliary system disease (41.4%) consisting of gallbladder wall thickening, mural hyperemia, intraluminal mud and pericholecystic fluid. Results are similar to those reported by Bhayana et al[17], with gallbladder sludge and distention being seen in 54% of right upper quadrant ultrasound studies. In this latter study, US also detected portal venous gas in one patient, which was confirmed by CT scan. US can also be used for guiding drainage procedures, as reported in cases of COVID-19-related acute cholecystitis[18].
A rather high prevalence of fatty liver has been reported in COVID-19 patients who underwent US examination, likely attributable to the established association between SARS-CoV-2 infection and obesity[17,19].
Taking into account the altered coagulation in COVID-19 and the potential thrombotic complications, US can be of value in evaluating the abdominal vasculature. Doppler US can be used to assess for venous or arterial thrombosis. Decreased vascularity at Doppler examination can indicate infarction and needs further studies. Contrast-enhanced US has been reported to adequately detect abdominal microcirculatory disorders by assessing mesenteric blood flow, liver and kidney perfusion[20].
A concern regarding US in COVID-19 patients was related to sonographer exposure while performing the examination. In order to minimize the scanning time, there have been proposals to capture cine clips and proceed with postprocessing of images after the examination[21].
CT
Several papers have looked at abdominal CT findings in COVID-19. Most frequent features seen on abdominal CT in COVID-19 patients were bowel wall thickening, fluid-filled colon, pneumatosis, pneumoperitoneum, intussusception, and ascites[22]. Abdominal findings in COVID-19 are detected either by ordering an abdominal scan in a SARS-CoV-2 positive patient, or by incidentally detecting ground-glass opacities in lung bases during an abdominal scan ordered for non-COVID related reasons.
CT scan has been usually indicated for prominent, otherwise unexplained digestive pain or for suspected complications such as mesenteric thrombosis or bowel ischemia[12,17]. Also, elevations in serum amylase and lipase have been reported in COVID-19; while the increased values of pancreatic enzymes did not usually reflect pancreatitis, there are reports of COVID-19 associated acute pancreatitis documented by CT[23-29]. Others, however, have considered inappropriate to define a causal relationship between SARS-CoV-2 and acute pancreatitis, due to insufficient etiological workup[30].
MRI
MRI has been rarely reported in COVID-19 patients, significantly less than US and CT[17]. In a study by Shiralkar et al[31], MRI was indicated for liver dysfunction; no acute findings were seen. A potential limitation of abdominal MRI studies in COVID-19 is the prolonged examination time in patients suffering from respiratory failure. Although MRI is an excellent modality for the evaluation of biliary disease, findings are usually non-specific as cholestasis is related to the high expression of ACE2 receptor in cholangiocytes.
DISCUSSIONS
In front of this novel threat for humanity, knowledge is continuously evolving with unprecedented efforts from the academic community. Despite good evidence on gastrointestinal involvement in COVID-19, related to the abundant expression of ACE2 receptors in the gut and biliary endothelium, there is a paucity of data regarding the imaging approach of digestive-related symptoms or laboratory test abnormalities of these patients. Moreover, currently available data on abdominal imaging in COVID-19 is retrospective in nature and limited by significant heterogeneity with respect to indications, protocol and follow-up of pathological findings.
Most frequent indications for US examination in SARS-CoV-2 positive patients were upper abdominal pain and altered liver function tests. COVID-19-related liver injury is usually mild and transient, but liver failure can occur in the setting of sepsis or coagulopathy with microthrombosis[21]. While Doppler examination might be limited in detecting small vessel thrombosis, assessment of mesenteric and liver vasculature patency is well done by contrast-enhanced CT scan or gadolinium-enhanced MRI. Usually, abdominal CT scan is indicated in cases of suspected bowel ischemia/ perforation, solid organ infarction (spleen, kidney), sepsis or cholestasis-related complications[21]. Segmental or diffuse thickening of the gut wall, along with distended intestinal lumen is a frequent finding in COVID-19 and can present as gastritis, enteritis, colitis or combination of these[21]. Bowel findings in COVID-19 are supposed to be caused be either direct viral infection of gut epithelium or by small-vessel thrombosis with consecutive ischemia[17].
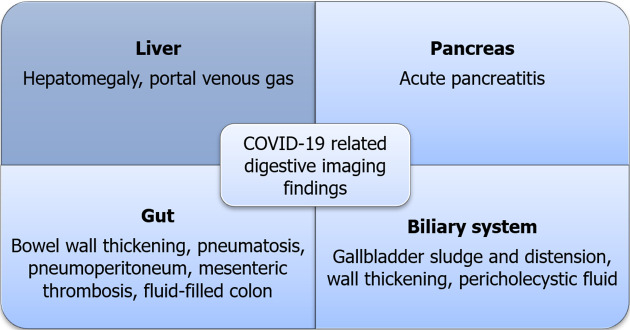
Along with ischemic complications, CT scan can also depict hemorrhagic complications such as hematomas or hemorrhagic transformation of bowel ischemia[21]. Besides its diagnostic role, abdominal imaging has also demonstrated prognostic value upon detection of ischemic gastrointestinal complications in COVID-19, which has been shown to be associated with higher mortality[32,33]. The most frequent findings on abdominal imaging in COVID-19 are summarized in Figure 1.
Figure 1.
Summary of coronavirus disease-2019 related abdominal imaging findings.
Not least, cross-sectional abdominal imaging performed in symptomatic individuals not suspected of having COVID-19 can alert clinicians of the possibility of SARS-CoV-2 infection by detection of ground-glass opacities on sections of the upper abdomen which are also capturing the lung bases. Thus, a CT scan ordered for a non-pulmonary indication can incidentally detect COVID-19 patients, before occurrence of respiratory manifestations.
To sum up, abdominal ultrasound and cross-sectional imaging techniques such as CT scan can accurately assess for gastrointestinal involvement in SARS-CoV-2 infected patients, particularly in a clinically significant setting; knowledge of the underlying mechanisms of hepatobiliary, pancreatic and gut alterations in COVID-19 and a high index of suspicion is mandatory for prompt detection of digestive-related injuries of SARS-CoV-2 infection (Table 1). Further studies looking at abdominal microvasculature and follow-up of patients with abdominal features related to COVID-19 are warranted to better depict the imaging features of this infection.
Table 1.
Summary of proposed mechanisms and abdominal imaging techniques recommended for gastrointestinal involvement in coronavirus disease-2019[13,34,35]
|
|
Proposed mechanism
|
Abdominal imaging
|
| Hepato-biliary | Direct viral cytopathic injury; Congestive hepatopathy; Drug-induced liver injury; Systemic inflammatory response; Exacerbation of preexistent chronic liver disease | Ultrasound to check gallbladder and biliary tree; CT/MRI to asses for perfusion injury and complications |
| Pancreas | Direct viral cytopathic injury; Systemic inflammation; Dehydration | CT scan to assess severity and complications of pancreatitis, and evaluate for alternative diagnosis; Ultrasound to check for biliary etiology or alternative diagnosis, also for diagnosis and follow-up of complications in pancreatitis |
| Gastrointestinal tract | Direct viral cytopathic injury; Systemic inflammation; Thrombosis; Adverse effects of COVID-19-related drugs | CT scan to assess for clinically similar alternative diagnosis, to detect extension and severity of bowel inflammation and to check the vascular patency |
COVID-19: Coronavirus disease-2019; CT: Computed tomography; MRI: Magnetic resonance imaging.
CONCLUSION
While there’s been a steady accumulation of data with respect to abdominal imaging findings in COVID-19, currently available recommendations are based on limited research. There is a wide spectrum of abdominal imaging findings in COVID-19, which includes hepato-biliary, pancreatic and luminal pathology. Underlying mechanisms behind the wide spectrum of digestive involvement in COVID-19 include direct viral infection, small-vessel thrombosis and systemic inflammation. Prompt recognition of abdominal imaging findings in COVID-19 is mandatory to adequately guide management and improve prognosis of these patients. Also, abdominal imaging in patients with primarily digestive symptoms not initially suspected of COVID-19 can alert clinicians about the possibility of SARS-CoV-2 infection if typical lesions are found on evaluation of lung bases.
Footnotes
Conflict-of-interest statement: The authors declare no conflicts of interest.
Manuscript source: Invited manuscript
Peer-review started: February 7, 2021
First decision: May 6, 2021
Article in press: June 23, 2021
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: Romania
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cabezuelo AS, Cure E S-Editor: Zhang H L-Editor: Filipodia P-Editor: Li X
Contributor Information
Daniel Vasile Balaban, Department of Internal Medicine and Gastroenterology, Carol Davila University of Medicine and Pharmacy; Dr. Carol Davila Central Military Emergency University Hospital, Bucharest 020021, Romania. vbalaban@yahoo.com.
Oana Madalina Baston, Department of Radiology, Medical Imaging and Interventional Radiology, Carol Davila University of Medicine and Pharmacy; Dr. Carol Davila Central Military Emergency University Hospital, Bucharest 020021, Romania.
Mariana Jinga, Department of Internal Medicine and Gastroenterology, Carol Davila University of Medicine and Pharmacy; Dr. Carol Davila Central Military Emergency University Hospital, Bucharest 020021, Romania.
References
- 1.World Health Organization. WHO Director-General's opening remarks at the media briefing on COVID-19. [cited 6 Nov 2020]. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 .
- 2.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang C, Shi L, Wang FS. Liver injury in COVID-19: management and challenges. Lancet Gastroenterol Hepatol. 2020;5:428–430. doi: 10.1016/S2468-1253(20)30057-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Consiglio CR, Cotugno N, Sardh F, Pou C, Amodio D, Rodriguez L, Tan Z, Zicari S, Ruggiero A, Pascucci GR, Santilli V, Campbell T, Bryceson Y, Eriksson D, Wang J, Marchesi A, Lakshmikanth T, Campana A, Villani A, Rossi P CACTUS Study Team. Landegren N, Palma P, Brodin P. The Immunology of Multisystem Inflammatory Syndrome in Children with COVID-19. Cell. 2020;183:968–981.e7. doi: 10.1016/j.cell.2020.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH, Nitsche A, Müller MA, Drosten C, Pöhlmann S. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020;181:271–280.e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203:631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Han C, Duan C, Zhang S, Spiegel B, Shi H, Wang W, Zhang L, Lin R, Liu J, Ding Z, Hou X. Digestive Symptoms in COVID-19 Patients With Mild Disease Severity: Clinical Presentation, Stool Viral RNA Testing, and Outcomes. Am J Gastroenterol. 2020;115:916–923. doi: 10.14309/ajg.0000000000000664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, Tan W. Detection of SARS-CoV-2 in Different Types of Clinical Specimens. JAMA. 2020;323:1843–1844. doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu Y, Guo C, Tang L, Hong Z, Zhou J, Dong X, Yin H, Xiao Q, Tang Y, Qu X, Kuang L, Fang X, Mishra N, Lu J, Shan H, Jiang G, Huang X. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol Hepatol. 2020;5:434–435. doi: 10.1016/S2468-1253(20)30083-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sun M, Guo D, Zhang J, Teng HF, Xia J, Liu P, Ge QX, Wang MY. Anal swab as a potentially optimal specimen for SARS-CoV-2 detection to evaluate hospital discharge of COVID-19 patients. Future Microbiol. 2020;15:1101–1107. doi: 10.2217/fmb-2020-0090. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 11.Tariq R, Saha S, Furqan F, Hassett L, Pardi D, Khanna S. Prevalence and Mortality of COVID-19 Patients With Gastrointestinal Symptoms: A Systematic Review and Meta-analysis. Mayo Clin Proc. 2020;95:1632–1648. doi: 10.1016/j.mayocp.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheung KS, Hung IFN, Chan PPY, Lung KC, Tso E, Liu R, Ng YY, Chu MY, Chung TWH, Tam AR, Yip CCY, Leung KH, Fung AY, Zhang RR, Lin Y, Cheng HM, Zhang AJX, To KKW, Chan KH, Yuen KY, Leung WK. Gastrointestinal Manifestations of SARS-CoV-2 Infection and Virus Load in Fecal Samples From a Hong Kong Cohort: Systematic Review and Meta-analysis. Gastroenterology. 2020;159:81–95. doi: 10.1053/j.gastro.2020.03.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pasha SB, Swi A, Hammoud GM. Gastrointestinal and hepatic manifestations of COVID-19 infection: Lessons for practitioners. World J Meta-Anal. 2020;8:348–374. [Google Scholar]
- 14.Sultan S, Altayar O, Siddique SM, Davitkov P, Feuerstein JD, Lim JK, Falck-Ytter Y, El-Serag HB AGA Institute. AGA Institute Rapid Review of the Gastrointestinal and Liver Manifestations of COVID-19, Meta-Analysis of International Data, and Recommendations for the Consultative Management of Patients with COVID-19. Gastroenterology. 2020;159:320–334.e27. doi: 10.1053/j.gastro.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abdelmohsen MA, Alkandari BM, Gupta VK, ElBeheiry AA. Diagnostic value of abdominal sonography in confirmed COVID-19 intensive care patients. Egypt J Radiol Nucl Med. 2020;51:198. [Google Scholar]
- 16.Cheung S, Quiwa JC, Pillai A, Onwu C, Tharayil ZJ, Gupta R. Superior Mesenteric Artery Thrombosis and Acute Intestinal Ischemia as a Consequence of COVID-19 Infection. Am J Case Rep. 2020;21:e925753. doi: 10.12659/AJCR.925753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bhayana R, Som A, Li MD, Carey DE, Anderson MA, Blake MA, Catalano O, Gee MS, Hahn PF, Harisinghani M, Kilcoyne A, Lee SI, Mojtahed A, Pandharipande PV, Pierce TT, Rosman DA, Saini S, Samir AE, Simeone JF, Gervais DA, Velmahos G, Misdraji J, Kambadakone A. Abdominal Imaging Findings in COVID-19: Preliminary Observations. Radiology. 2020;297:E207–E215. doi: 10.1148/radiol.2020201908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ying M, Lu B, Pan J, Lu G, Zhou S, Wang D, Li L, Shen J, Shu J From the COVID-19 Investigating and Research Team. COVID-19 with acute cholecystitis: a case report. BMC Infect Dis. 2020;20:437. doi: 10.1186/s12879-020-05164-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Medeiros AK, Barbisan CC, Cruz IR, de Araújo EM, Libânio BB, Albuquerque KS, Torres US. Higher frequency of hepatic steatosis at CT among COVID-19-positive patients. Abdom Radiol (NY) 2020;45:2748–2754. doi: 10.1007/s00261-020-02648-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jung EM, Stroszczynski C, Jung F. Contrast enhanced ultrasonography (CEUS) to detect abdominal microcirculatory disorders in severe cases of COVID-19 infection: First experience. Clin Hemorheol Microcirc. 2020;74:353–361. doi: 10.3233/CH-209003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Revzin MV, Raza S, Srivastava NC, Warshawsky R, D'Agostino C, Malhotra A, Bader AS, Patel RD, Chen K, Kyriakakos C, Pellerito JS. Multisystem Imaging Manifestations of COVID-19, Part 2: From Cardiac Complications to Pediatric Manifestations. Radiographics. 2020;40:1866–1892. doi: 10.1148/rg.2020200195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lui K, Wilson MP, Low G. Abdominal imaging findings in patients with SARS-CoV-2 infection: a scoping review. Abdom Radiol (NY) 2021;46:1249–1255. doi: 10.1007/s00261-020-02739-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.de-Madaria E, Siau K, Cárdenas-Jaén K. Increased Amylase and Lipase in Patients With COVID-19 Pneumonia: Don't Blame the Pancreas Just Yet! Gastroenterology. 2021;160:1871. doi: 10.1053/j.gastro.2020.04.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de-Madaria E, Capurso G. COVID-19 and acute pancreatitis: examining the causality. Nat Rev Gastroenterol Hepatol. 2021;18:3–4. doi: 10.1038/s41575-020-00389-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aloysius MM, Thatti A, Gupta A, Sharma N, Bansal P, Goyal H. COVID-19 presenting as acute pancreatitis. Pancreatology. 2020;20:1026–1027. doi: 10.1016/j.pan.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McNabb-Baltar J, Jin DX, Grover AS, Redd WD, Zhou JC, Hathorn KE, McCarty TR, Bazarbashi AN, Shen L, Chan WW. Lipase Elevation in Patients With COVID-19. Am J Gastroenterol. 2020;115:1286–1288. doi: 10.14309/ajg.0000000000000732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Szatmary P, Arora A, Thomas Raraty MG, Joseph Dunne DF, Baron RD, Halloran CM. Emerging Phenotype of Severe Acute Respiratory Syndrome-Coronavirus 2-associated Pancreatitis. Gastroenterology. 2020;159:1551–1554. doi: 10.1053/j.gastro.2020.05.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hadi A, Werge M, Kristiansen KT, Pedersen UG, Karstensen JG, Novovic S, Gluud LL. Coronavirus Disease-19 (COVID-19) associated with severe acute pancreatitis: Case report on three family members. Pancreatology. 2020;20:665–667. doi: 10.1016/j.pan.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pinte L, Baicus C. Pancreatic involvement in SARS-CoV-2: case report and living review. J Gastrointestin Liver Dis. 2020;29:275–276. doi: 10.15403/jgld-2618. [DOI] [PubMed] [Google Scholar]
- 30.Juhász MF, Ocskay K, Kiss S, Hegyi P, Párniczky A. Insufficient etiological workup of COVID-19-associated acute pancreatitis: A systematic review. World J Gastroenterol. 2020;26:6270–6278. doi: 10.3748/wjg.v26.i40.6270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shiralkar K, Chinapuvvula N, Ocazionez D. Cross-Sectional Abdominal Imaging Findings in Patients With COVID-19. Cureus. 2020;12:e9538. doi: 10.7759/cureus.9538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Keshavarz P, Rafiee F, Kavandi H, Goudarzi S, Heidari F, Gholamrezanezhad A. Ischemic gastrointestinal complications of COVID-19: a systematic review on imaging presentation. Clin Imaging. 2021;73:86–95. doi: 10.1016/j.clinimag.2020.11.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Horvat N, Pinto PVA, Araujo-Filho JAB, Santos JMMM, Dias AB, Miranda JA, de Oliveira CV, Barbosa CS, Morais TC, N Assuncao-Jr A, Nomura CH, Viana PCC. Abdominal gastrointestinal imaging findings on computed tomography in patients with COVID-19 and correlation with clinical outcomes. Eur J Radiol Open. 2021;8:100326. doi: 10.1016/j.ejro.2021.100326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bruno G, Fabrizio C, Santoro CR, Buccoliero GB. Pancreatic injury in the course of coronavirus disease 2019: A not-so-rare occurrence. J Med Virol. 2021;93:74–75. doi: 10.1002/jmv.26134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schaefer EAK, Arvind A, Bloom PP, Chung RT. Interrelationship Between Coronavirus Infection and Liver Disease. Clin Liver Dis (Hoboken) 2020;15:175–180. doi: 10.1002/cld.967. [DOI] [PMC free article] [PubMed] [Google Scholar]