Abstract
The COVID-19 pandemic had the unintended consequence of placing nurses in the spotlight because their knowledge and skills were in desperate need. While it will be years until we fully understand the impact that this pandemic has exacted on the nursing workforce, early studies have found that nurses have been traumatized by this event and many intend to leave the profession This seismic event only further exacerbated an already vulnerable and strained nursing workforce that pre-existed worldwide prior to COVID-19. The pandemic also highlighted the many challenges facing nursing leadership, in particular, how to create conditions to maintain and sustain a healthy nursing workforce. Nurses’ job satisfaction has emerged as an important predictor of whether nurses remain in an organization and stay in the profession. When examined more closely, job satisfaction has been related to nurses feeling empowered to exercise autonomy over their own practice and having agency. Autonomy and agency, in turn, are affected by their managers' leadership styles. Leaders are instrumental in setting the tone and creating the climate and culture that either values or devalues autonomy and agency. To help leaders create empowering conditions, we have developed a guide for leaders. This guide, based on the value-driven philosophy of leadership called Strengths-Based Nursing and Healthcare Leadership (SBNH-L), is founded on principles of person-centered, empowerment, relationship-focused, and innate capacities (ie, strengths) that are operationalized in eight core values. This guide can be used by leaders as their roadmap to create empowering workplace conditions that value and facilitate nurses’ autonomy and agency.
Keywords: nursing, professional autonomy, empowerment, job satisfaction, leadership, agency
Introduction
The year 2020 is already considered an inflection point in healthcare history, judged by many to be a game changer for nursing and healthcare systems worldwide.1 This decade began as a celebration of nurses when the World Health Organization designated 2020 as the Year of the Nurse and the Midwife to coincide with Florence Nightingale’s bicentennial birth. Nursing organizations worldwide committed to focusing on nurses’ unique contributions to healthcare enterprises, to make visible the work of nurses, and to explain why nurses are considered the backbone of most healthcare systems, with the intention of attracting needed investments in nursing and nursing leadership.2,3
As plans to celebrate nursing and lobby for investment in nursing were underway, the COVID-19 pandemic had the unintended consequence of placing nurses and nursing in the spotlight. As healthcare systems mobilized to care for the sick and dying and to focus on public health messaging to contain the spread of the virus, nurses became the frontline workers whose knowledge and skills were in desperate need. It will be years until we fully understand the impact that this pandemic has exacted on the nursing workforce, however, early studies have found that nurses are fearful, distressed, and traumatized and, many intend to leave the profession.4 Zhao’s study of 451 nurses from 5 hospitals in Wuhan, China, who provided direct patient care during the most infectious phase of the outbreak, experienced significant psychological distress but psychological distress could be mitigated by their work environments. Less distressed nurses had managers with an inclusive leadership style. Inclusive leaders involved their staff in decision-making-- a form of empowerment—and created workplace environments that were perceived to be psychologically safe.5
Nursing workforce strain pre-existed worldwide before the pandemic. COVID-19 just further exacerbated an already vulnerable and strained nursing workforce as well as an already identified crisis in nursing leadership.6
The years ahead will be dedicated to re-envisioning healthcare systems from the lessons learned from this pandemic. The challenge will be on how to create conditions to maintain and sustain a healthy nursing workforce. This challenge begins with nurse and healthcare leaders whose leadership and management styles create healthy, productive workplace environments for their staff and, whose leadership values align with the models of nursing care that they are promoting.7
Nurses’ Job Satisfaction: Autonomy, Agency, Empowerment, and Nursing Leadership
During the past three decades, in response to the looming and growing crisis of a nursing shortage and the difficulties in retaining a healthy nursing workforce, researchers have sought to identify factors that contribute to nurses’ ability to provide safe, quality patient/person centered care.8 A multitude of factors have been identified. However, what has consistently emerged as a robust variable is nurses’ job satisfaction.9
Job satisfaction has been defined as the favourableness or unfavourableness in which employees view their work.10 Job satisfaction has been found to predict nurses’ decision to remain in their organization and/or to stay in the profession.11 Given that job satisfaction or its corollary, job dissatisfaction, is an important determinant of patient care and nurse retention outcomes, the second line of research has been to understand what contributes to nurses’ job satisfaction.9
Nurses’ job satisfaction has been found to be related to workplace conditions and personal resources.12 In terms of workplace conditions, nurse-to-patient ratios have received a considerable amount of attention given that patient mortality, morbidity, and safety are related to these ratios.13
What has received considerably less attention is workplace conditions of how agency, autonomy, and empowerment, both structural and psychological, relate to job satisfaction despite the fact that the nursing literature has consistently demonstrated that there exists a clear link between nurse autonomy and satisfaction with work.14–16 (see Table 1 for definitions of these concepts). In studies that have included these concepts, the research has found that they are important determinants of job satisfaction which translate into intention to remain in an organization and the profession.17,18
Table 1.
Definition of Concepts: Agency, Autonomy, Structural Empowerment, Psychological Empowerment
| Agency/Agentic |
Agency is the capacity, condition, or state of action of individuals; of exerting power; and of feeling in command/control of their lives.19 Agentic is when an individual has the power to control his/her own goals, actions, and destiny.20 |
| Autonomy | The ability to act freely in accordance with one’s own knowledge and professional capacities without unnecessary inhibitions or bureaucracy and without requiring permission or consent.21,22 |
| Structural Empowerment | An organization-centric perspective on empowerment.23 How nurses become empowered by their work structures.24 |
| Psychological Empowerment | A person’s intrinsic motivation concerning how employees experience their work is influenced by perceived meaning, competence, self-determination and impact, and by workplace structures that are put in place to promote empowerment.23,25 |
In terms of agency, autonomy, and empowerment, agency is the least studied of these three concepts as they relate to job satisfaction. Agency has been examined in terms of Bandura’s theory of self-efficacy.26 We located two studies that linked nurses’ job satisfaction to agency.27 Nurses’ job satisfaction, along with self-efficacy and agentic capacities, had direct and indirect effects on nurses’ intention to leave.28 Self-efficacy predicted higher job satisfaction and, job satisfaction was related to lower turnover intention. While job satisfaction among Iranian nurses was not affected directly by nurses’ feelings of self-efficacy, it was important inasmuch as self-efficacy was related to commitment to the organization.29
Autonomy and empowerment have been linked to leadership styles. For example, Larabee et al.30 found that psychological empowerment, that is the degree to which nurses perceived they had control over their own practice, explained 54% of the variance of job satisfaction. In identifying specific factors that influenced perceived job satisfaction, antecedents of psychological empowerment such as personal hardiness as well as having nurse managers with a transformational leadership style, had a positive influence.
When nurse managers and leaders create conditions that both support and encourage nurses to exercise control over their own practice, nurses feel they have a greater degree of autonomy.31–33 Where structural empowerment exists, that is, where work structures are put in place that promote empowerment,34 it has been shown to promote job satisfaction35 and reduce burn-out in nurses.36 Further, where nurses are provided with the resources and emotional support that address their psychological, physical, and emotional needs to deal with and mitigate stress, nurses report greater job satisfaction and less burnout which in turn translates into patient-centered care and improved patient outcomes.24,37,38 Nurse leaders need to create conditions of empowerment both for their staff as well as for themselves.39
Thus, nurses’ job satisfaction and psychological/emotional/physical health are related to autonomy, agency, and empowerment, which in turn are affected by the nature and style of nurse leaders, the tone and culture they set both on their units and in their organization as well as the opportunities they create for their staff.40–43 Nurse managers have the capacity to facilitate empowering work conditions as well as to promote collaborative inter-professional and intra-professional relationships.44
The purpose of this paper is three-fold: First, to describe the concepts of agency, autonomy, and structural and psychological empowerment; Second, to examine leadership styles that contribute to nurses’ autonomy and empowerment; Third, to propose a value driven leadership framework, namely, Strengths-Based Nursing and Healthcare Leadership (SBNH-L), to guide nurse and healthcare leaders to create empowering conditions for nurses to encourage autonomy and exercise their agency.
Clarification of Concepts: Agency, Autonomy, Structural Empowerment, and Psychological Empowerment
Agency
Although agency has been infrequently studied in nursing, self-efficacy, a related construct, has been studied extensively and has emerged as a robust variable to predict and explain a wide range of phenomena that are within nurses’ scope of practice such as weight loss, diabetes management, breast cancer management and the like.45 Self-efficacy is a strength required for nurses to fulfill their advocacy role.46
Autonomy
Autonomy is an important concept of study within the nursing literature and its value in clinical practice and patient safety cannot be overstated.47,48 The abundant literature related to autonomy has resulted in a range of definitions. In clinical practice, autonomy has been delineated into three dimensions which include: clinical or practice autonomy, control over nursing practice autonomy, and job or work autonomy.22 Although individual, clinical, organizational, and professional autonomy have been identified in the literature as distinct concepts, these terms have often been used interchangeably.49 In this paper we focus on professional autonomy.
Professional autonomy refers to the ability to act in accordance with one’s own knowledge and professional capacities and to do so freely without fear, without unnecessary inhibitions or bureaucracy, and without having to get permission or consent.21,22 To be autonomous implies being self-governing and self-ruling50 and has been further described as self-determination or the ability to understand a situation, to deliberate, to plan, to make choices, and to pursue goals.51 By the same token, an autonomous individual has the ability to respect the self-determination of others.50 It should be noted that autonomy is an innate capacity, a basic need that is expressed in self-determination.52 Professional autonomy has been shown in the nursing literature to be negatively related to moral distress53 and positively related to quality of patient care.48 These latter two features of autonomy affect one’s ability to control one’s work situation.22 It has been proposed that healthcare organizations should focus on enhancing the professional autonomy of nurses in order to influence how they perceive their work as meaningful, which in turn will result in positive work outcomes.32 The outcome of meaningful work is linked to job satisfaction and is the subjective experience of believing in the value and significance of the work itself.54
Empowerment
The concept of empowerment in nursing has most frequently been based on the work of Kanter in organizational science.34 Kanter differentiates between formal and informal power. The former includes recognition and freedom to make choices which keeps a work environment operating at an optimal level. The latter is founded upon relationships with peers and team building and is supported with connections even outside the workplace.34 Whether formal or informal, an employee’s perception of their level of empowerment influences job satisfaction and is affected by having access to information, support, and resources. Professional advancement is a major component of Kanter’s theory of structural empowerment.34 Laschinger and colleagues55 further developed and expanded the concept of structural empowerment. Structural empowerment includes psychological empowerment which has an impact on both work-stress and satisfaction.55
Structural empowerment, an important predictor of positive work experiences, is affected by managers who foster trusting and civil work relationships.56 Structural empowerment implies that employees have access to workplace social structures which allow them to accomplish their work in ways which are meaningful.38 Structural empowerment is congruent with psychological empowerment, that is, a person’s intrinsic motivation.57 Psychological empowerment is when the individual believes they have power and are motivated to exercise their power.
Inter-Relationship Between Empowerment (Structural and Psychological), Agency, and Autonomy
Empowerment involves creating conditions, both structural and psychological, that encourages autonomy. Structural empowerment has been found to be related to psychological empowerment.38,55 Structural empowerment refers to the structure, policies, opportunities that are put in place designed to encourage participation, involvement, and engagement. It also includes the culture and climate that are created through relationships. These include how people are treated and the messages communicated, both verbally and non-verbally, by leaders and managers. Structural empowerment is reflected in the workplace culture and climate that encourages nurses to have voice and discourages silence; to act in accordance with their knowledge, skills, experience, and scope of practice; encourages innovation and experimentation; and rewards initiative, taking control, collaboration, and cooperation.24
Autonomy is the freedom to exercise control over one’s own nursing practice. Clinical decision-making results from clinical reasoning—having a clinical grasp of the situation, arriving at a clinical judgment of what is needed and then deciding what actions to take.58 Taking action is exercising agency. The nurse has to believe that they know what to do and that they can achieve the desired outcome (i.e., self-efficacy). It requires knowledge, skilled know-how, and confidence to act, and, then to actually carry out the planned act. A person with high self-efficacy will be agentic, that is, they will have a “can do” attitude and know how to make things happen.46 Agency is the highest form of empowerment.
It should be noted that no one can empower another. A person can only create conditions for another to take and exercise their own power.59 Thus, leaders create conditions by putting in place empowerment structures and creating a culture and climate, that is, psychological empowerment, through ways of relating that encourage nurses to have control over their own practice (autonomy) and exercise agency.
Leadership Styles That Contribute to Nurses’ Empowerment and Autonomy
Several studies have found that leadership can affect the quality of care, patient outcomes, and nurses’ workplace conditions.60,61 Different leadership styles have been found to correlate with quality of care.62,63 One leadership style that has been studied is Authentic Leadership based on the work of Avolio.64 Authentic leadership is defined as an approach that emphasizes building a leader’s legitimacy through honest relationships with followers, who value their follower’s input, and is built on ethical foundations.65 Authentic leadership has been related to both nurses’ perceived autonomy66 and structural empowerment.67
The other major leadership style that has been correlated with nurses’ empowerment, both structural and psychological, is Transformational Leadership.68,69 Transformational leadership is a style in which leaders encourage, inspire, and motivate employees to innovate and create change that help grow and shape the future success of the organization.70 Nurses working with these leaders have reported increases in their job satisfaction and improved patient safety outcomes.71
What has yet to be studied is the relationship between a leader's style and nurses’ agency. Human agency plays a critical role in an individual’s health72 and therefore, leaders need to be aware of how best to promote agency.
There is speculation as to the factors that might explain why these two styles of leadership are effective. A major factor is that a leader’s way of relating contributes to staffs’ wellbeing that in turn leads to greater job satisfaction.65
What is missing and urgently needed is a leadership framework that can guide leaders to create workplace environments that specifically address issues of agency, autonomy, and empowerment. We propose a new leadership framework, Strengths-Based Nursing and Healthcare Leadership (SBNH-L), grounded in the real world of nursing practice that includes many of the relational features of Authentic and Transformational leadership yet goes beyond. SBNH-L is nested in the same value-driven philosophy as Strengths-Based Nursing and Healthcare (SBNH), a model of care.46
SBNH and Its Relationship to SBNH-Leadership
SBNH, developed by Laurie Gottlieb, is rooted in; the work of Florence Nightingale, the McGill Model of Nursing,73 and the Developmental Health Framework,74 which then evolved into a philosophy and value-driven approach to guide clinicians to enable them to provide compassionate, knowledgeable care.46 SBNH represents a paradigm shift from the current prevailing disease-focused, deficit-based, hierarchical model of care that predominates most healthcare systems.
SBNH guides nurses to actualize care that is deeply person-centered, involves processes of empowerment and relationality, that capitalizes on a person’s innate and acquired capacities (ie, strengths) which are required for health and healing.46 This approach involves noticing, mobilizing, developing, and working with a person and family's inner and outer strengths.46
SBNH is a potential game changer for nurses and healthcare providers.6 However, for SBNH to guide nursing care, it was recognized that this would require a leadership framework that aligned with SBNH. In advance of the publication of the book Strengths-Based Nursing Care: Health and Healing for Person and Family,46 the same SBNH values that guided clinicians in creating health and healing environments for individuals (i.e., patients, clients), families, communities were reconceptualized to guide leaders in creating healthy workplace environments for their staff.75 Many professions and disciplines, such as economics76, psychology,77 and management78 are undergoing similar shifts to a strengths-based approach with encouraging results.
Definition of SBNH-Leadership
SBNH-L is defined as a unique, value-driven, embodied approach that guides leaders and managers to create equitable and safe workplace cultures and environments that honour, develop, mobilize, and capitalize on the strengths of individuals and their team. SBNH leaders enable individuals, teams and organizations to provide knowledgeable, compassionate, safe, high quality person and family centered care. SBNH leaders have skilled know-how to bring about change.79
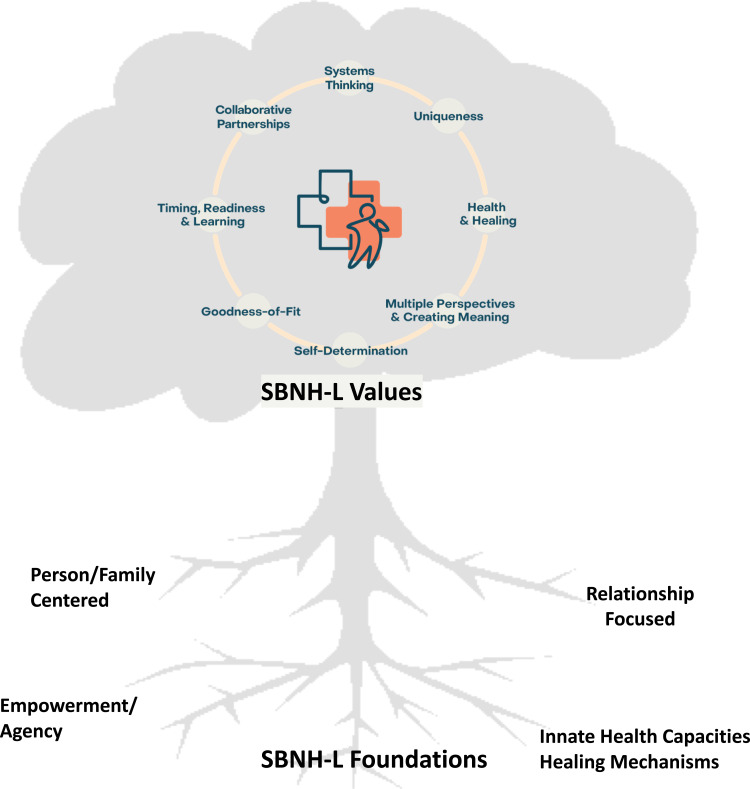
The SBNH-L underlying foundations of person-centered, empowerment, relationship-focused, and innate capacities are operationalized by eight core values. These values guide SBNH leaders’ actions and include; systems-thinking; uniqueness; health and healing; multiple perspectives and creating meaning; self-determination; goodness-of-fit; timing-readiness-learning; collaborative partnerships.79 (see Figure 1)
Figure 1.
Strengths-based Nursing and Healthcare Leadership (SBNH-L) values and foundations.
Notes: The SBNH-L foundations are operationalized in the eight SBNH-L values. The SBNH-L values are interconnected. The image in the centre of the values represent the unit of the leaders' concern which could include staff, point-of-care nurses, patient, family, team members, other colleagues, the unit, the organization and the like.
SBNH leaders strive to be humble, self-aware, authentic, open-minded, compassionate, courageous, credible, curious, creative, flexible, and resourceful. They have integrity, imagination, and operate from a growth mindset. They strive to be engaged, collaborative, systems-focused, solution-oriented, and evidenced informed. These SBNH leadership qualities determine how the four foundations and the eight core values are enacted.79
A Clinical Situation: SBNH-Leadership in Action
To contain the spread of COVID-19, healthcare institutions had to quickly pivot and institute policies, often prescribed by the government, that impacted staff, patients, and their families. One such policy was restricted visiting in which a minimal number of individuals including caregivers were permitted to visit during limited hours. Nurse Managers were charged with implementing this policy at the unit level. The following example illustrates how one Nurse Manager translated this policy, guided by SBNH-L values. SBNH-L values are capitalized in the text below. Table 2 presents the eight SBNH-L values and their definitions.
Table 2.
SBNH-L Values with Definitions and Guiding Questions
| SBNH-L Values | Definitions | Sample Guiding Questions |
|---|---|---|
|
Value # 1- SYSTEMS THINKING |
Systems thinking is a holistic approach that frames the conceptualization of a system’s parts interacting with the whole in an interconnected manner. Systems exist at the micro, meso, and macro levels. | What do I need to consider or to think about when putting a policy or directive in place? How does my department or unit fit within the larger healthcare institution? As a nurse manager, how does the organization foster autonomy and agency? How do these policies impact what I do at the unit level? |
|
Value #2 – UNIQUENESS |
Uniqueness defines the person, staff, unit, organization, and their specialness. What they do best; who they are; and what they strive to be. Uniqueness is reflected in the capacities, capabilities, skills, talents, and potentials (ie, strengths) that are present or that can be developed. Uniqueness can also refer to an issue, situation, or problem. |
What is similar or different about this issue, situation, problem? What is special about each nurse? My unit? My organization? What do they each do best and what is working? How do I develop a staff member's strengths (eg, capacities, competencies, skills) to help them be more autonomous and have greater agency? How can I help my staff notice, recognize, mobilize, or develop their patient’s strengths to meet their specific needs? |
|
Value # 3 –HEALTH and HEALING |
Health is about creating wholeness whereas Healing is about restoring wholeness. Health involves developing capacities, capabilities, competencies, and skills needed to adapt, cope, relate, regulate, rally to achieve goals, grow, develop, and flourish. Healing involves repair, rehabilitation, recovery, renewal. | How can I develop each staff member’s capabilities, skills, capacities to enable them to grow, develop, and thrive? How do I recognize and then, deal with unhealthy and unsafe workplace environments that impede autonomy and interfere with agency? How do I recognize trauma, burnout, and the need to create conditions for healing? How do I support my staff when challenging situations arise? |
|
Value #4 –MULTIPLE PERSPECTIVES/CREAT-ING MEANING |
Multiple perspectives. Individuals have different beliefs, understandings, interpretations that affect their way of being and their responses. Creating meaning refers to the processes by which a person makes sense of an experience, to arrive at an understanding. |
Whose perspective do I need to know about to understand diversity of views when dealing with a challenge, a change in situation/policy, in order to move forward? How do I accommodate and work with different perspectives? Do I take the time to discuss with each nurse their beliefs, understandings, and needs with regards to autonomy and agency? What support can I give my staff? |
|
Value #5 –SELF-DETERMINATION |
Self-determination is about free will to take charge, make choices, and feel in control. Self- determination requires autonomy and skills of agency. Self-determination is about decision-making—the processes involved in arriving at a plan of action and enacting that plan. | How do I help staff identify the areas they can change and, or have some control over? How do I help staff consider what information they need to have in order to make decisions? What structures do I need to put in place that will encourage staff to be more autonomous and exercise their agency? How can I encourage staff to have greater psychological empowerment and understand in which areas of their practice they have autonomy and can be agentic? |
|
Value #6 –GOODNESS-OF-FIT |
Goodness-of-fit is about the “match” between the demands of the environment and the capabilities/capacities of the individual. Individuals shape and are shaped by their many life-worlds. Environments include the physical aspects (eg, space, lighting, noise) and social (eg, relational, emotional tone and culture). Individuals grow and thrive in environments where there is a goodness-of-fit and they experience difficulties and are distressed in “poorness-of-fit” environments. |
What considerations do I need to think about or put in place for staff to be at their very best? What types of structures do I need to put in place that would enable staff to give person-centered, compassionate care? How do I ensure that my staff have the resources and tools required to meet the needs of the work environment and to do their work? How do I create a culture that values self-empowerment, autonomy, and agency and that potentiates the fit with each staff member’s personal and professional goals and skills? |
| Value # 7 –LEARNING, TIMING, READINESS | Learning is the process of acquiring new knowledge, understandings, skills, behaviors, attitudes, values, beliefs, cognitions (thinking). Learning is an innate capacity required for personal and professional development. Learning can occur through formal education and practical experience. Learning is maximized when the learner is ready and motivated to engage and reflect on their experiences. Readiness is a prerequisite for learning and consider a plan of action. Timing involves being attuned to personal, temporal, and contextual factors to maximize goal achievement. | What do I need to consider to nurture a climate that values learning? How do I recognize cues of readiness? How do I time interventions to maximize success? What resources do I need to lobby for to enhance learning opportunities for my staff? What structures do I need to put in place that encourage staff to broaden and deepen their knowledge and skills? What skills and knowledge do my staff need to have to be agentic? |
|
Value # 8 – COLLABORATIVE PARTNERSHIP |
Collaborative partnership recognizes that relationships are reciprocal- each person brings something to the relationship or interaction from which the other can learn. Collaboration is the art of working together in trusting, supportive ways to achieve a purpose. Partnership requires a willingness to share power rather than exert power in order to control. Collaborative partnership is working together on mutually agreed upon goals recognizing the expertise and experience of the other. | What considerations do I need to think about to promote collaboration among team members? How do I help my staff understand power—why power is important, what power looks like in different situations with different people, how to share power with others, and how to use their own power effectively? What role can I play with other colleagues and team members to improve and strengthen collaboration and partnerships? |
Notes: Table derived from Hubley, P., Gottlieb, L.N., Durrant, M. Strengths-Based Nursing and Healthcare Leadership (SBNH-L): Value-Driven Capacities for Leaders. Ingram School of Nursing, McGill University, Montreal, Canada, 2020 and the values are based on Gottlieb, L.N. (2013). Strengths-Based Nursing Care: Health and healing for person and family. NY: Springer Publishing.
A Clinical Example from an In-Patient Surgical Unit
Anticipating that nurses on all shifts would be faced with questions related to the change in visitation policy, Nurse Manager Booth held several staff meetings to inform staff of the change. She provided them with the written communique about the policy issued by the government and adapted to their organization by the hospital administration. SBNH-L value: SYSTEMS THINKING. Nurse Manager Booth also invited other members of the healthcare team to these meetings including physicians and social workers so that, as a team, they could discuss their reactions and thoughts related to this policy. SBNH-L values: MULTIPLE PERSPECTIVES; COLLABORATIVE PARTNERSHIP. Nurse Manager Booth understood that the policy was open to some interpretation when it came to patient safety and to the welfare and well-being of patients and staff. SBNH-L value: HEALTH. Her concern was how this policy would affect the few elderly patients currently on her unit who had undergone hip repair surgery after falling and in particular, one elderly gentleman who was disoriented and suffered from dementia. Nurse Manager Booth told her staff to use their clinical judgement when they had requests to allow family members and caregivers to be with a specific patient. Nurse Manager Booth outlined to her staff what things they should consider when interpreting the policy such as its impact on a particular patient, other patients on the unit, other nurses’ availability to care for the patients, and how their clinical judgment would respect the government and institutional directives. SBNH-L values: SELF-DETERMINATION; SYSTEMS THINKING.
Patient Smith, an elderly gentleman, was admitted on Nurse Manager Booth's unit. He suffered from several co-morbidities including dementia. In the late evening and during the night, Mr. Smith would become agitated and scream. His caregiver, who had been granted permission to visit during the day, asked Nurse Jones, the evening nurse, if he could spend the night with Mr. Smith. His presence seemed to calm Mr. Smith, decrease his agitation and disruptive behavior. SBNH-L value: UNIQUENESS. Nurse Jones was aware that the policy did not include overnight caregiver presence, however, given that Nurse Manager Booth expected all caregiver requests to be considered carefully, Nurse Jones consulted with the nurse in charge on the evening shift to help her make a decision, SBNH-L value: SELF-DETERMINATION. They reviewed the policy, decided to consult with the physician, and the three of them discussed the possibility of medication changes which could be made to help decrease Mr. Smith’s night-time agitation. SBNH-L value: COLLABORATIVE PARTNERSHIP. The efficacy of a new medication treatment as well as Mr. Smith’s response to it would need to be evaluated. SBNH-L value: UNIQUENESS. Nurse Jones considered the risks and benefits of permitting the caregiver to spend the night with Mr. Smith. SBNH-L value: SELF-DETERMINATION. She considered how reliable the caregiver was in terms of respecting proper personal protective equipment requirements and noted that the caregiver had a very caring and appropriate approach with Mr. Smith. SBNH-L value: GOODNESS-OF-FIT. Nurse Jones also reviewed the patient’s medical chartwhich indicated that on previous nights when Mr. Smith had been alone, he had been difficult to care for and had been disruptive to the other patients on the unit . SBNH-L value: SYSTEMS THINKING. Finally, Nurse Jones made the decision to allow the caregiver to stay overnight. She emailed Nurse Manager Booth to let her know of the situation and documented her assessment in Mr. Smith's medical file. SBNH-L value: SELF-DETERMINATION. Overnight, Mr. Smith's agitation was well managed by the caregiver and there were no incidents. Nurse Manager Booth responded to Nurse Jones’ e-mail to tell her that she supported her decision and was very proud of her that she had made the right decision for Mr. Smith and for the other patients and staff on their unit. . SBNH-L value: HEALTH OF STAFF MEMBER. Nurse Manager Booth then held a staff meeting in which staff discussed how to identify, assess, and deal with “special circumstances” by reviewing Nurse Jones’ clinical reasoning and decision-making. SBNH-L value: LEARNING. Nurse Manager Booth listened to the concerns posed by the staff and the challenges which they felt could be anticipated. SBNH-L value: MULTIPLE PERSPECTIVES. Together, they brainstormed possible ways of dealing with these challenges while respecting the spirit of the revised visitation policy within the context of patient and staff needs. SBNH-L value: GOODNESS- OF-FIT.
A Guide for Managers/Leaders: SBNH-L Value Guided Questions to Create Empowering Conditions That Promote Staff Autonomy and Agency
This guide is for managers and leaders to help them create a culture and set- a tone that encourages staff to empower themselves to have greater autonomy over their own practice and have the confidence to act (ie, be agentic). The guide, based on SBNH-L values, comprise sample questions that managers/leaders could ask of themselves (see Table 2). This section is organized in terms of each SBNH-L value with sample questions and then illustrated with excerpts from the above clinical example. Table 2).
Value 1: Systems Thinking
What do I need to consider or to think about when putting a policy or directive in place?
How does my department or unit fit within the larger healthcare institution?
As a nurse manager, how does the organization foster autonomy and agency? How do these policies impact what I do at the unit level?
Illustration from the clinical example: Nurse Manager Booth, guided by the value of systems thinking, encouraged discussion of the institutional policy and its impact on patients and staff members with her team. She encouraged staff to examine and question the institutional policy and gave them permission to consider the patient’s needs and circumstances in light of the policy and to anticipate its impact on specific patients, the other patients on the unit, and on the staff caring for them.
Value 2: Uniqueness
-
What is similar or different about this issue, situation or problem?
What is special about each nurse? My unit? My organization?
What do they each do best and what is working?
How do I develop a staff member's strengths (eg, capacities, competencies, skills) to help them be more autonomous and have greater agency?
How can I help my staff notice, recognize, mobilize, or develop each of their patient’s strengths to meet their specific needs?
Illustration from the clinical example: Nurse Manager Booth, guided by the value of uniqueness, understood the uniqueness of the situation brought about by the pandemic and the need to anticipate and adapt the hospital's visitation policy accordingly. Nurse Jones was able to identify the unique needs of Mr. Smith, and based on her clinical judgment, arrived at a decision that was in his best interest as well as for the other patients on the unit and for the staff.
Value 3: Health and Healing
How can I develop each staff member’s capabilities, skills, capacities that will enable them to grow, develop, and thrive?
How do I recognize and then deal with unhealthy and unsafe workplace environments that impede autonomy and interfere with agency?
How do I recognize trauma, burnout, and the need to create conditions for healing?
How do I support my staff when challenging situations arise?
Illustration from the clinical example: Nurse Manager Booth, guided by the value of Health and Healing, helped to develop Nurse Jones’ capacity for taking charge of her own practice by praising and reinforcing the wisdom of her clinical judgment and decision-making. By upholding the visitation policy, Nurse Jones was trying to prevent the virus from being brought to her unit that would put her patients and staff at risk. She had to balance the rationale for this policy with the needs of Mr. Smith, and the concern for the other patients and nurses. She considered the benefit of promoting a calm, quiet healing environment so that other patients could sleep, and to ensure that the other nurses on the unit would be available to care for them.
Value 4: Multiple Perspectives
Whose perspective do I need to know about to understand diversity of views when dealing with a challenge or a change in situation/policy in order to move forward?
How do I accommodate and work with different perspectives?
Do I take the time to discuss with each nurse their beliefs, understandings, and needs with regards to autonomy and agency? What support can I give my staff?
Illustration from the clinical example: Nurse Manager Booth, guided by the value of Multiple Perspectives, held a de-briefing staff meeting during which she elicited each team member’s concerns, reactions, and perspectives with regards to this new visitation policy as it would affect care on her unit.
Value 5: Self-Determination
How do I help staff identify the areas they can change and, or have some control over?
How do I help staff consider what information they need to make decisions?
What structures do I need to put in place that will encourage staff to be more autonomous and exercise their agency?
How can I encourage staff to have greater psychological empowerment and understand in which areas of their practice they have autonomy and can be agentic?
Illustration from the clinical example: Nurse Manager Booth, guided by the value of Self-Determination, created conditions whereby Nurse Jones felt empowered to make the decision allowing Mr. Smith’s caregiver to remain with him overnight even though it went contrary to the visitation policy. Her staff were capable and willing to make their own decisions based on information about the new visitation directive and their own clinical judgement as it related to Mr. Smith and to the other patients and the staff on the unit.
Value 6: Goodness-of-Fit
What considerations do I need to think about or put in place for staff to be at their very best?
What types of structures do I need to put in place that would enable staff to give person-centered, compassionate care?
How do I ensure that my staff have the resources and tools required to meet the needs of their work environment and to do their work?
How do I create a culture that values self-empowerment, autonomy, and agency and that potentiates the fit with each staff member’s personal and professional goals and skills?
Illustration from the clinical example: Nurse Manager Booth, guided by the value of Goodness-of- fit, created an environment where nurses felt that they could exercise autonomy over their own practice as was evidenced by the actions they took.
Value 7: Learning, Timing, and Readiness
What do I need to consider to nurture a climate that values learning?
How do I recognize cues of readiness?
How do I time interventions to maximize success?
What resources do I need to lobby for to enhance learning opportunities for my staff?
What structures do I need to put in place that encourage staff to broaden and deepen their knowledge and skills?
What skills and knowledge do my staff need to have to be agentic?
Illustration from the clinical example: Nurse Manager Booth, guided by the value of Learning, Timing, and Readiness, held a meeting following the incident with Mr. Smith to review and reflect on Nurse Jones' decision-making. She recognized this was a teachable moment from which the team could learn. The Nurse Manager had also created conditions where Nurse Jones felt empowered to seek information and assess the situation in order to make a decision.
Value 8: Collaborative Partnership
What considerations do I need to think about to promote collaboration among team members?
How do I help my staff understand power—why power is important; what power looks like in different situations with different people; how to share power with others; and how to use their own power effectively?
What role can I play with other colleagues and team members to improve and strengthen collaboration and partnerships?
Illustration from the clinical example: Nurse Manager Booth, guided by the value of Collaborative Partnership, shares her power with her staff by recognizing and valuing their expertise, inviting them to discuss the new visitation policy and its implementation. She also encouraged them to exercise their own power to make decisions in her absence while respecting the goals of the restricted visitation policy.
Conclusion
Leadership is integral to creating conditions that permit nurses to work in environments where they feel empowered to be autonomous and exercise their own agency. In so doing, nurses will experience job satisfaction which then can affect their decision to remain within their organization and the profession, and most importantly, improve safety and the quality of care provided to patients and their families. The nature and style of nursing leadership is perhaps the most critical factor in determining the culture and climate that will be created on a unit and within an organization. In this paper, we have provided a new leadership framework, Strengths-Based Nursing Leadership (SBNH-L), which can help leaders to create environments which specifically address issues of autonomy, agency, and empowerment grounded in the actual realities of nursing. SBNH-L goes beyond other leadership styles to offer practical guidance to nurse leaders to help staff reach their full potential.
Funding Statement
Canadian Institute of Health Research, Grant number: PWP-159070. Social Sciences and Humanities Research Council of Canada, Grant number: 895-2018-4018.
Author Contributions
All of the authors took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors have declared that no competing interests exist.
References
- 1.Swaithes L, Dziedzic K, Sharp CA, Ellis B, Walsh N. Context, context, context: how has Covid-19 changed implementation globally and how can we ‘lock in’ learning? Rheumatology. 2020;59(8):1804–1807. doi: 10.1093/rheumatology/keaa387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.International Council of Nurses. Nurses: A Voice to Lead Nursing the World to Health. Geneva, Switzerland: ICN; 2020. [Google Scholar]
- 3.Nursing now global campaign. Available from: www.nursingnow.com. Accessed June26, 2021.
- 4.Labrague LJ, De Los Santos JAA. COVID-19 anxiety among front-line nurses: predictive role of organisational support, personal resilience and social support. J Nurs Manag. 2020;28(7):1653–1661. doi: 10.1111/jonm.13121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhao F, Ahmed F, Faraz NA. Caring for the caregiver during COVID-19 outbreak: does inclusive leadership improve psychological safety and curb psychological distress? A Cross-Section Study. Int J Nurs Studies. 2020;110:103725. doi: 10.1016/ijnurstu.2020.103725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hewson A. Leading nursing beyond 2020 – the challenge and the opportunity. J Nurs Manag. 2020;28(4):767–770. doi: 10.1111/jonm.13022 [DOI] [PubMed] [Google Scholar]
- 7.Cummings GG, MacGregor T, Davey M, et al. Leadership styles and outcome patterns for the nursing workforce and work environment: a systematic review. Int J Nurs Studies. 2010;47(3):363–385. doi: 10.1016/j.ijnurstu.2009.08.006 [DOI] [PubMed] [Google Scholar]
- 8.Hegney DG, Rees CS, Osseiran-Moissson R, et al. Perceptions of nursing workloads and contributing factors, and their impact on implicit care rationing: a Queensland, Australia Study. J Nurs Manag. 2019;27(2):371–380. doi: 10.1111/jonm.12693 [DOI] [PubMed] [Google Scholar]
- 9.Yasin YM, Kerr MS, Wong CA, Belanger CH. Factors affecting job satisfaction among acute care nurses working in rural and urban settings. J Adv Nurs. 2020;76(9):2359–2368. doi: 10.1111/jan.14449 [DOI] [PubMed] [Google Scholar]
- 10.Greishaber LD, Deering PP. Job satisfaction of nursing assistants in long-term care. Healthcare Superv. 1995;13:18–28. [PubMed] [Google Scholar]
- 11.Karlsson A-C, Gunningberg L, Backstrom J, Poder U. Registered nurses’ perspectives of work satisfaction, patient safety and intention to stay – a double-edged sword. J Nurs Manag. 2019;27(7):1359–1365. doi: 10.1111/jonm.12816 [DOI] [PubMed] [Google Scholar]
- 12.Halcomb E, Smyth E, McInnes S. Job satisfaction and career intentions of registered nurses in primary health care: an integrative review. BMC Fam Pract. 2018;19(1):136. doi: 10.1186/s12875-018-0819-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aiken LH, Ceron C, Simonetti M, et al. Hospital nurse staffing and patient outcome. Rev Med Clín Las Condes. 2018;29:322–327. [Google Scholar]
- 14.Aiken LH, Clark SP, Sloane DM, Lake ET, Cheney T. Effects of hospital care environment on patient mortality and nurse outcomes. J Nurs Admin. 2008;38(5):223–229. doi: 10.1097/01.NNA.0000312773.42352.d7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Finn CP. Autonomy: an important component for nurses’ job satisfaction. Int J Nurs Studies. 2001;38(3):349–357. doi: 10.1016/S0020-7489(00)00065-1 [DOI] [PubMed] [Google Scholar]
- 16.Lake ET, Friese CR. Variations in nurse practice environments: relation to staffing and hospital characteristics. Nurs Res. 2006;55(1):1–9. doi: 10.1097/00006199-200601000-00001 [DOI] [PubMed] [Google Scholar]
- 17.Camveren M, Yurumezoglu K. Why do young nurses leave their organizations? A Qualitative Descriptive Study. Int Nurs Rev. 2020. doi:10/1111/inr.12633 [DOI] [PubMed] [Google Scholar]
- 18.Goodare P. Literature review: why do we continue to lose our nurses? Aust J Adv Nurs. 2016;34:50–56. [Google Scholar]
- 19.Napper P, Rao A. The Power of Agency. New York, NY: St Martin’s Press; 2019. [Google Scholar]
- 20.Bjerede M, Gielniak M. What is agentic learning and why is it important? 2017. Available from: www.gettingsmart.com/2017/11/what-is-agentic-learning-and-why-is-it-important? Accessed June26, 2021.
- 21.Kramer M, Schmalenberg C. Development and evaluation of essentials of magnetism tool. J Nurs Admin. 2004;34(7):365–378. doi: 10.1097/00005110-200407000-00010 [DOI] [PubMed] [Google Scholar]
- 22.Kramer M, Maguire P, Schmalenberg CE. Excellence through evidence. The what, when, and where of clinical autonomy. J Nurs Admin. 2006;36(10):479–491. doi: 10.1097/00005110-200610000-00009 [DOI] [PubMed] [Google Scholar]
- 23.Spreitzer GM. Taking stock: a review of more than twenty years of empowerment research at work. In: The SAGE Handbook of Organizational Behavior. Vol. 1. Thousand Oaks, CA: SAGE Publications; 2008:54–72. [Google Scholar]
- 24.Choi S, Kim M. Effects of structural empowerment and professional governance on autonomy and job satisfaction of the Korean nurses. J Nurs Manag. 2019;27(8):1664–1672. doi: 10.1111/jonm.12855 [DOI] [PubMed] [Google Scholar]
- 25.Spreitzer GM. Psychological empowerment in the workplace: dimensions, measurement, validation. Acad Manag J. 1995;38:1442–1465. [Google Scholar]
- 26.Bandura A. Social cognitive theory. In: Vasta R, editor. Annals of Child Development. Six Theories of Child Development. Vol. 6. Greenwich, CT: JAI Press; 1989:1–60. [Google Scholar]
- 27.Borgogoni L, Cenciotti R, Consiglio C. Test Agent. Milano: Ed Utilia -HR Now and Next; 2016. [Google Scholar]
- 28.De Simone S, Planta A, Cicotto C. The role of job satisfaction, work engagement, self-efficacy and agentic capacities on nurses’ turnover intention and patient satisfaction. Appl Nurs Res. 2018;39:130–140. doi: 10.1016/j.apnr.2017.11.004 [DOI] [PubMed] [Google Scholar]
- 29.Chegini Z, Janati A, Asghari-Jafarabadi M, Khosravizadeh O. Organizational commitment, job satisfaction, organizational justice and self-efficacy among nurses. Nurs Pract Today. 2019;6:86–93. [Google Scholar]
- 30.Larabee JH, Janney MA, Ostrow CL, Withrow GL, Hobbs GR Jr, Burant C. Predicting registered nurse job satisfaction and intent to leave. J Nurs Admin. 2003;33(5):271–283. doi: 10.1097/00005110-200305000-00003 [DOI] [PubMed] [Google Scholar]
- 31.Oshodi TO, Bruneau B, Crockett R, et al. Registered nurses’ perceptions and experiences of autonomy: a Descriptive Phenomenological Study. MBC Nurs. 2019;18:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Both-Nwabuwe JMC, Lips-Wiersma M, Dijkstra MTM, Beersma B. Understanding autonomy–meaningful work relationship in nursing: a theoretical framework. Nurs Outlook. 2020;68(1):104–113. doi: 10.1016/j.outlook.2019.05.008 [DOI] [PubMed] [Google Scholar]
- 33.Supametaporn P. The conceptualization of professional nursing autonomy. J Nurs Sci. 2013;31:80–86. [Google Scholar]
- 34.Kanter RM. Men and Women of the Corporation. 2nd ed. New York, NY: Basic Books; 1993. [Google Scholar]
- 35.Orgambidez A, Almeida H. Exploring the link between structural empowerment and job satisfaction through the mediating effect of role stress: Across-Sectional Questionnaire Study. Int J Nurs Stud. 2020;109:103672. doi: 10.1016/j.ijnurstu.2020.103672 [DOI] [PubMed] [Google Scholar]
- 36.Orgambidez A, Almeida H. Core burnout and power in Portuguese nursing staff. An explanatory model based on structural empowerment. Workplace Health Saf. 2019;67(8):391–398. doi: 10.1177/2165079918822648 [DOI] [PubMed] [Google Scholar]
- 37.Mohamed FR, Mahmoud SR, Hafez KHA, Mahmoud TM. Nurses empowerment at primary health care centers and its relation with quality of work life. J Nurs Educ Pract. 2019;9(10):79–86. doi: 10.5430/jnep.v9n10p79 [DOI] [Google Scholar]
- 38.Spence Laschinger HK, Leiter MP, Day A, Gilin-Oore D, Mackinnon SP. Building empowering work environments that foster civility and organizational trust. Nurs Res. 2012;61(5):316–325. doi: 10.1097/NNR.0b013e318265a58d [DOI] [PubMed] [Google Scholar]
- 39.Abel SE, Hall M, Swartz MJ, et al. Empowerment of front-line leaders in an online learning, certificate programme. J Nurs Manag. 2020;28(2):359–367. doi: 10.1111/jonm.12933 [DOI] [PubMed] [Google Scholar]
- 40.Trus M, Galdikiene N, Balciunas S, et al. Connection between organizational culture and climate and empowerment: the perspective of nurse managers. Nurs Health Sci. 2018;21(1):54–62. doi: 10.1111/nhs.12549 [DOI] [PubMed] [Google Scholar]
- 41.Lunden A, Teras M, Kvist T, Hagmann-Laitila A. Transformative agency and tensions in knowledge management- A qualitative interview study for nurse leaders. J Clin Nurs. 2019;28(5–6):969–979. doi: 10.1111/jocn.14694 [DOI] [PubMed] [Google Scholar]
- 42.El Banan SHA. Nurse managers practices and its relation to staff nurses’ autonomy and satisfaction at a selected hospital. Int J Nurs Didactics. 2020;10:15–23. [Google Scholar]
- 43.Bowles JR, Batchellor J, Adams JM, Zimmermann D, Pappas S. Nursing’s leadership role in advancing professional practice/work environments as part of the quadruple aim. Nurs Admin Q. 2019;43(2):157–163. doi: 10.1097/NAQ.0000000000000342 [DOI] [PubMed] [Google Scholar]
- 44.Faulkner J, Laschinger H. Effects of structural and psychological empowerment on perceived respect in nurses. J Nurs Manag. 2008;16(2):214–221. doi: 10.1111/j.1365-2834.2007.00781.x [DOI] [PubMed] [Google Scholar]
- 45.Lenz ER, Shortridge-Baggett LM, Eds. Self-Efficacy in Nursing: Research and Measurement Perspectives. NY: Springer Pub Co; 2002. [Google Scholar]
- 46.Gottlieb LN. Strengths-Based Nursing Care: Health and Healing for Person and Family. New York: Springer Publishing; 2013. [Google Scholar]
- 47.Oshodi T, Bruneau B, Crockett R, Kinchington F, Nayar S, West E. Registered nurses’ perceptions and experiences of autonomy: a Descriptive Phenomenological Study. BMC Nurs. 2019;18(1):51. doi: 10.1186/s12912-019-0378-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rao AD, Kumar A, McHugh M. Better nurse autonomy decreases the odds of 30-day mortality and failure to rescue. J Nurs Scholar. 2017;49(1):73. doi: 10.1111/jnu.12267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gagnon L, Bakker D, Montgomery P, Palkovits JA. Nurse autonomy in cancer care. Cancer Nurs. 2010;33(3):E21–28. doi: 10.1097/NCC.0b013e3181c98985 [DOI] [PubMed] [Google Scholar]
- 50.McParland J, Scott PA, Arndt M, et al. Autonomy and clinical practice 1: identifying areas of concern. Br J Nurs. 2000;9(8):507–513. doi: 10.12968/bjon.2000.9.8.6309 [DOI] [PubMed] [Google Scholar]
- 51.Brown JM, Kitson AL, McKnight TJ. Challenges in Caring: Explorations in Nursing and Ethics. London: Chapman and Hall; 1992. [Google Scholar]
- 52.Deci EL, Ryan RM. Intrinisic Motivation and Self-Determination in Human Behavior. New York, NY; 1985. [Google Scholar]
- 53.Papathanassoglou ED, Karanikola MN, Kalafati JW, Giannakopoulou M, Lemonidou C, Alabarran JW. Professional autonomy, collaboration with physicians, and moral distress among European intensive care nurses. Am J Crit Care. 2012;21(2):e41–e52. doi: 10.4037/ajcc2012205 [DOI] [PubMed] [Google Scholar]
- 54.Lips-Wiersma M, Wright S. Measuring the meaning of MW: development and validation of the comprehensive MW scale (CMWS). Group Organ Manag. 2012;37(5):655–685. doi: 10.1177/1059601112461578 [DOI] [Google Scholar]
- 55.Laschinger HK, Finegan J, Shamian J, Wilk P. Impact of structural and psychological empowerment on job strain in nursing work settings: expanding Kanter’s model. J Nurs Admin. 2001;31:5260–5272. [DOI] [PubMed] [Google Scholar]
- 56.Ta’an WF, Alhurani J, Alhalal E, Al-Dwaikat TN, Al-Faaori I. Nursing empowerment: how job performance is affected by a structurally empowered work environment. J Nurs Admin. 2020;50(12):635–641. doi: 10.1097/NNA.0000000000000951 [DOI] [PubMed] [Google Scholar]
- 57.Abel SE, Hand MW. Exploring, defining, and illustrating a concept: structural and psychological empowerment in the workplace. Nurs Forum. 2018;53(4):579–584. doi: 10.1111/nuf.12289 [DOI] [PubMed] [Google Scholar]
- 58.Benner P, Hooper Kyriadakis P, Stannard D. Critical Wisdom and Interventions in Acute Critical Care. 2nd ed. New York, NY: Springer Publ; 2011. [Google Scholar]
- 59.Gibson CH. A concept analysis of empowerment. J Adv Nurs. 1991;16(3):354–361. doi: 10.1111/j.1365-2648.1991.tb01660.x [DOI] [PubMed] [Google Scholar]
- 60.Germain PB, Cummings GG. The influence of nursing leadership on nurse performance: a systematic literature review. J Nurs Manag. 2010;16(4):425–439. doi: 10.1111/j.1365-2834.2010.01100.x [DOI] [PubMed] [Google Scholar]
- 61.Wong CA. Connecting nursing leadership and patient outcome; state of the science. J Nurs Manag. 2015;23(3):275–278. doi: 10.1111/jonm.12307 [DOI] [PubMed] [Google Scholar]
- 62.Sfantou DF, Laliotis A, Patalarou AE, Sifaki-Pistolia D, Matalliotakis M, Patelarou E. Importance of leadership style towards quality of care measures in healthcare settings; A systemic review. Healthcare(Basel). 2017;5(4):73. doi: 10.3390/healthcare5040073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zaghini F, Fiorini J, Piredda M, Fida R, Sili A. The relationship between nurse managers’ leadership style and patients’ perception of the quality of the care provided by nurses: cross sectional survey. Int J Nurs Studies. 2020;101:103446. doi: 10.1016/j.ijnurstu.2019.103446 [DOI] [PubMed] [Google Scholar]
- 64.Avolio BJ, Garner WL. Authentic leadership development: getting to the root of positive forms of leadership. Leadersh Q. 2005;16(3):315–338. doi: 10.1016/j.leaqua.2005.03.001 [DOI] [Google Scholar]
- 65.Nelson K, Boudrias J-B, Brunet L, et al. Authentic leadership and psychological well-being in nurses: the mediating role of work-climate at the individual level of analysis. Burnout Res. 2014;1(2):90–101. doi: 10.1016/j.burn.2014.08.001 [DOI] [Google Scholar]
- 66.Malik N, Dhar RL. Authentic leadership and its impact on extra role behaviour of nurses: the mediating role of psychological capital and the moderating role of autonomy. Personal Rev. 2017;46(2):277–296. doi: 10.1108/PR-05-2015-0140 [DOI] [Google Scholar]
- 67.Regan S, Laschinger HKS, Wong CA. The influence of empowerment, authentic leadership, and professional practice environments on nurses’ perceived interprofessional collaboration. J Nurs Manag. 2016;24(1):E54–E61. doi: 10.1111/jonm.12288 [DOI] [PubMed] [Google Scholar]
- 68.Boamah S. Linking nurses’ clinical leadership to patient care quality: the role of transformational leadership and workplace empowerment. Can J Nurs Res. 2017;50(1):9–19. doi: 10.1177/0844562117732490 [DOI] [PubMed] [Google Scholar]
- 69.Asif M, Jameel A, Hussain A, Hwang J, Sahito N. Linking transformational leadership with nurse-assessed adverse patient outcomes and the quality of care: assessing the role of job satisfaction and structural empowerment. Int J Environ Res Public Health. 2019;16(13):2381. doi: 10.3390/ijerph16132381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pearson MM. Transformational leadership principles and tactics for the nurse executive to shift nursing culture. J Nurs Admin. 2020;50(3):142–153. doi: 10.1097/NNA.0000000000000858 [DOI] [PubMed] [Google Scholar]
- 71.Boamah SA, Laschinger HKS, Wong C, Clarke S. Effect of transformational leadership on job satisfaction and patient safety outcomes. Nurs Outlook. 2018;66(2):180–189. doi: 10.1016/j.outlook.2017.10.004 [DOI] [PubMed] [Google Scholar]
- 72.Sarngadharan RC, Nandu KT. Human agency, social structure and forming of health consciousness and perception. Eur J Mol Clin Med. 2020;7:59105916. [Google Scholar]
- 73.Gottlieb LN, Rowat K. The McGill model of nursing: a practice-derived model. Adv Nurs Sci. 1987;9(4):51–61. doi: 10.1097/00012272-198707000-00008 [DOI] [PubMed] [Google Scholar]
- 74.Gottlieb LN, Gottlieb B. The developmental/health framework within the McGill model of nursing: “laws of nature” guiding whole person care. Adv Nurs Sci. 2007;30(1):E43–57. doi: 10.1097/00012272-200701000-00013 [DOI] [PubMed] [Google Scholar]
- 75.Gottlieb LN, Gottlieb B, Shamian J. Principles of strengths-based nursing leadership for strengths-based nursing care: a new paradigm for nursing and healthcare for the 21st century. Nurs Leadersh. 2012;25(2):38–50. doi: 10.12927/cjnl.2012.22960 [DOI] [PubMed] [Google Scholar]
- 76.Nusbaum MC. Creating Capabilities: The Human Development Approach. Cambridge Mass, Bellnap Press of Harvard University; 2011. [Google Scholar]
- 77.Csikszentmihalyi M. Flow and Foundations of Positive Psychology. New York: Springer; 2014. [Google Scholar]
- 78.Rath T, Conchie B. Strengths-Based Leadership. New York: Gallup Press; 2008. [Google Scholar]
- 79.Hubley P, Gottlieb LN, Durrant M. Strengths Based Nursing and Healthcare Leadership (SBNH-L): Value-Driven Capacities for Leaders. Unpublished Work. Montreal, Canada: Ingram School of Nursing, McGill University; 2020. [Google Scholar]