Abstract
Introduction and importance
Psychiatric symptoms may be a mode of the revelation of several endocrinopathies, but rarely in primary hyperaldosteronism, which can increase psychiatric comorbidity, as well as cardiovascular risk.
Case presentation
We report a case of a 26-year-old engineer, who suffered from atypical psychosis before being hospitalized for a state of agitation, he presented with high blood pressure and severe hypokalemia. An etiological assessment revealed a right adrenal adenoma, which was afterward resected, with a very good evolution.
Clinical discussion
In this association, a high-level of aldosterone and hypokalemia can be behind these manifestations that present in an atypical form. Treatment is medical by anti-aldosterone or surgical by resection of the adenoma, but the challenge now is to know if we can or not stop psychotropic treatment after the treatment of the adenoma. In our case, the treatment was stopped six months after the resection of the adenoma, with very good outcomes until now.
Conclusion
Despite the high prevalence of psychiatric illnesses, it is always necessary to look for the organic causes that may be behind these pathologies, especially if they are in atypical forms.
Learning points
-
•
The organic aetiologies of psychiatric pathologies are frequent but very underestimated, being able to threaten the vital prognosis (suicide).
-
•
A good detailed clinical examination can point to an organic etiology which, once treated, avoids complications and relapses.
-
•
Its management must be multi-disciplinary.
Keywords: Hyperaldosteronism, Hypertension, Anxiety, Depression, Adrenalectomy, Case report
Highlights
-
•
Psychiatric pathologies are very numerous, of which the etiologies are diverse. Organic causes are frequent but unfortunately are very underestimated, hence the prognosis is always poor with a great risk of threatening the vital prognosis (suicide)
-
•
Its management must be multi-disciplinary
-
•
A good detailed clinical examination can point to an organic etiology which, once treated, avoids resorting to abusive diagnostic means and can also avoid complications and relapses.
1. Introduction
Neuropsychiatric symptoms as representative of endocrinopathies have been previously described in the literature with high co-morbidity [1]. Their prevalence appears to be much higher in Cushing's syndrome, hyperprolactinemia, and thyroid disease [1]. Until now, only a few studies have reported these symptoms in patients with primary hyperaldosteronism (PH). In this mini-review, we report a case of PH revealed by an atypical psychosis, and through it, we aim to explain its pathophysiology and the influence of different therapeutic strategies.
Our case report was written according to SCARE guidelines [2].
2. Case presentation
A 26-year-old male patient, engineer as a profession, from north Africa, with no pathological history (In particular, there are not genetic or psychosocial family history, neither drug history), suffered from an atypical psychosis (anxiety, depression, demoralization, decreased energy, decreased concentration, decreased interest in previously pleasurable activities, insomnia, with an irritable mode) for over four months (he had no past or family history of psychopathy). He was treated by a psychiatrist with neuroleptic (Haldol) and anxiolytic (Bromazepam), but without improvement. Then, he was admitted for a state of agitation, requiring injectable neuroleptic and anxiolytic therapy.
On clinical examination, he presented with mania and delusional syndrome, polyuric-polydipsic syndrome and elevated blood pressure. The biological analysis found severe hypokalemia (1.9 mmol/L). Nicardipine in the self-syringe pusher, with injectable and oral potassium supplementation have been initially introduced.
Faced with this atypical psychosis and these associated signs, an etiological exploration was realized: Brain CT scan, natremia, calcemia, thyroid function test and dosage of urinary methoxylated derivatives were normal. Dosage of activity aldosterone/renin was elevated (161 pmol/mU (normal value < 64)), then an abdominal CT scan was performed and showed a right adrenal cortical adenoma (14 ∗ 11 mm) (Fig. 1/2).
Fig. 1.

Axial view of abdominal CT scan was performed and showed a right adrenal cortical adenoma.
Fig. 2.
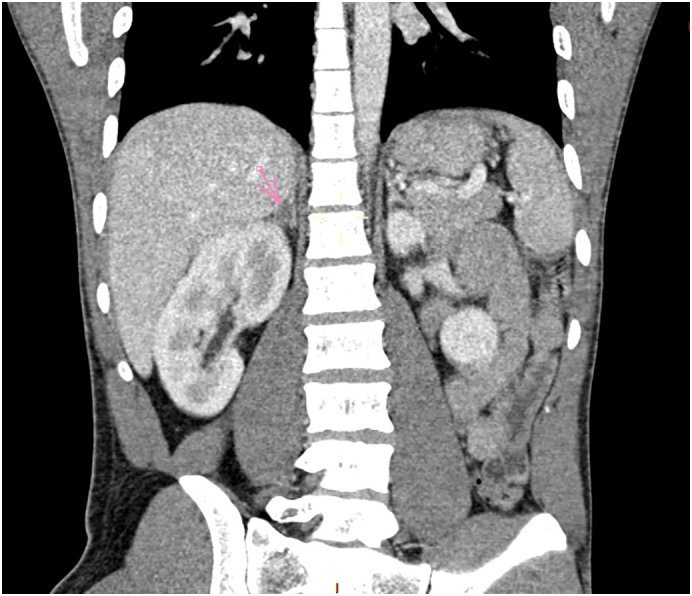
Coronal view of abdominal CT scan was performed and showed a right adrenal cortical adenoma.
After a multidisciplinary meeting, the patient was six weeks on anti-aldosterone (spironolactone at a progressive dose of up to 200 mg/day) for preoperative preparation, with normalization of blood pressure and kalemia. Then, a Laparoscopic resection of adenoma was performed (Fig. 3) by an experienced professor of visceral surgery with the aid of an assistant professor in the same speciality.
Fig. 3.

Macroscopic view of the resected mass.
The anatomopathological study that revealed an adrenal cortical adenoma without signs of malignancy (Fig. 4).
Fig. 4.
Microscopic views of the resected mass showing an adrenal cortical adenoma without signs of malignancy.
Postoperative evolution was good without complications. Spironolactone was immediately stopped with a good control of blood pressure and kalemia. Six months ago, all psychotropic drugs were stopped, and the outcome was favorable; the patient did not present depression, anxiety or a state of agitation, and he was very satisfied of his improvement and he has embarked on his previous job as an engineer.
The patient has an appointment every six months to check for psychiatric symptoms, blood pressure and kalemia.
3. Discussion
3.1. Descriptive
Primary hyperaldosteronism (PH) or Conn's syndrome (CS) is the most common cause of secondary arterial hypertension, which can be due to adrenal adenoma or bilateral adrenal hyperplasia [3]. PH is usually revealed by treatment-resistant hypertension [4], but it may be also revealed by psychiatric symptoms such as depression, anxiety, irritable mood and impaired quality of life [5] (Table 1).
Table 1.
Different studies showing the different presentations of psychiatric symptoms in PH-patients.
| Psychiatric symptoms | Sonino et al. [10] | Sonino et al. [6] | Apostolopoulou et al. [5] | Our patient |
|---|---|---|---|---|
| Generalized anxiety disorder | 60% | 30.4% | 50% | Yes |
| Obsessive-compulsive disorder | 10% | 13% | No | |
| Panic disorder | 10% | 8.7% | No | |
| Major depression disorder | 10% | 8.7% | 25% | Yes |
| Persistent somatization | 20% | 8.7% | No | |
| Irritable mode | 10% | 73.5% | Yes | |
| Demoralization | 50% | 8.7% | Yes |
3.2. Epidemiology
PH as a case revealed by depression was reported for the first time in 1979 by Malinow [4]. Its prevalence is indeterminate until now. Initially, it was controversial that high blood pressure is responsible for these neuropsychiatric manifestations, but over time, several studies have been performed in this domain. Nicoletta et al. [6] have found that anxiety, depression and irritable mood were more frequent in PH than in essential hypertension (EH), although that the blood pressure values were similar in both cases. They noted also that hypokalemia was only found in patients with irritability. In addition, Emanuele et al. found increased plasma aldosterone levels in patients suffering from depression compared with control subjects [7].
So, all these studies signs that these manifestations are directly because of PH and not anymore due to severe levels of hypertension.
3.3. Physio-pathology
Its physio-pathology remains unclear. Aldosterone is known as the major ligand of mineralocorticoid receptors (MR), and it can penetrate the blood-brain barrier. What is hypothetical until now is that excessive aldosterone may induce disturbances in the balance of glucocorticoid receptors (GR) and MR, which may be responsible for symptoms appearance [8]. The place of renin in this physio-pathology is still unknown.
3.4. Diagnosis
In our case, the patient suffered from these psychiatric manifestations for a long time; he did not present any neurosensory signs of arterial hypertension, and the detection of his high blood pressure was accidental. It means that the psychiatric manifestations are because of the elevated level of aldosterone and severe hypokalemia, such as mentioned in the studies above.
3.5. Treatment and follow up
PH treatment includes adrenalectomy or mineralocorticoid receptor antagonists (MRA). The challenge now is to know which therapeutic strategy to favor in this case. Recent studies in this domain have focused on the post-therapeutic evolution, particularly on improving the quality of life and the disappearance of psychiatric manifestations on the one hand, and on the need to continue anti-psychotic therapy on the other. In returning to the literature (Table 2, Table 3), adrenalectomy is favored over MRA, since that hyperaldosteronism is increasingly accompanied by increased cardiovascular risk, of course without forgetting the side effects of long-period MRA-treatment [1].
Table 2.
different studies showing the level of effectiveness of surgical treatment.
Table 3.
Different studies showing the level of effectiveness of medical treatment.
Sukor et al. [9] showed that the post-therapeutic evolution at three months is much better with adrenalectomy than with medical therapy, while it is almost the same at six months.
In our case, neuroleptic and anxiolytic were gradually stopped three months after the resection of the adenoma, currently and after six months of the resection, our patient presents normal blood pressure, he is hopeful, motivated, and does not present any of the old symptoms.
4. Conclusion
Based on this case, after a review of the literature, and because of its poorly understood physio-pathology, Primary Hyperaldosteronism remains a pathology requiring multi-disciplinary management. Here, appears the importance of a good diagnostic approach in psychiatric illnesses, particularly in their atypical forms.
Consent of patient
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
None.
Funding
There's no financial support.
Guarantor
Nabila Isamili, Noha El Ouafi, Mohammed Bouziane.
Research registration number
None.
CRediT authorship contribution statement
H. Rasras: Conception, Literature review, Analysis, Data collection, Writing - Review & editing
F. Laouan: Conception, Analysis, Data collection, Writing - Review & editing
R. Jabi: Conception, Software, Writing - Review & editing
M. Bouziane: Conception, Methodology, Supervision
N. El Ouafi: Conception, Methodology, Supervision
N. Ismaili: Conception, Methodology, Supervision.
Declaration of competing interest
Non-conflicts.
Acknowledgements
Non applicable.
References
- 1.Funder JW, Carey R.M., Mantero F., Murad M.H., Reincke M., Shibata H., Stowasser M., Joung W.F., Jr. The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 2016;101:1899–1916. doi: 10.1210/jc.2015-4061. [DOI] [PubMed] [Google Scholar]
- 2.for the SCARE Group. Agha R.A., Franchi T., Sohrabi C., Mathew G. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 3.Käyser S.C., Dekkers T., Groenewoud H.J., van der Wilt G.J., Carel Bakx J., van der Wel M.C., Hermus A.R., Lenders J.W., Deinum J. Study heterogeneity and estimation of prevalence of primary aldosteronism: a systematic review and meta-regression analysis. J. Clin. Endocrinol. Metab. 2016;101:2826–2835. doi: 10.1210/jc.2016-1472. [DOI] [PubMed] [Google Scholar]
- 4.Malinow K.C., Lion J.R. Hyperaldosteronism (Conn’s disease) presenting as depression. J. Clin. Psychiatry. 1979;40:358–359. [PubMed] [Google Scholar]
- 5.Apostolopoulou K., Kunzel H.E., Gerum S., Merkle K., Schulz S., Fischer E., Pallauf A., Brand V., Bidlingmaier M., Enders S., Beuschlein F., Reincke M. Gender differences in anxiety and depressive symptoms in patients with primary hyperaldosteronism: a cross-sectional study. World J. Biol. Psychiatry. 2014;15:26–35. doi: 10.3109/15622975.2012.665480. [DOI] [PubMed] [Google Scholar]
- 6.Psychological Assessment of Primary Aldosteronism: A Controlled Study Nicoletta Sonino, Elena Tomba, Maria Luisa Genesia, Chiara Bertello, Paolo Mulatero, Franco Veglio, Giovanni A. Fava, and Francesco Fallo Departments of Statistical Sciences (N.S.) and Medical and Surgical Sciences (F.F.), University of Padova, and Department of Mental Health (N.S.), 35128 Padova, Italy; Department of Psychiatry (N.S., G.A.F.), State University of New York at Buffalo, Buffalo, New York 14260; Laboratory of Psychosomatics and Clinimetrics (E.T., G.A.F.), Department of Psychology, University of Bologna, 40127 Bologna, Italy; and Department of Medicine and Experimental Oncology (M.L.G., C.B., P.M., F.V.), University of Torino, 10126 Torino, Italy.
- 7.Emanuele E., Geroldi D., Minoretti P., Coen E., Politi P. Increased plasma aldosterone in patients with clinical depression. Arch. Med. Res. 2005;36:544–548. doi: 10.1016/j.arcmed.2005.03.046. [DOI] [PubMed] [Google Scholar]
- 8.Jezova D., Hlavacova N. Endocrine factors in stress and psychiatric disorders. focus on anxiety and salivary steroids. Ann. N. Y. Acad. Sci. 2008;1148:495–503. doi: 10.1196/annals.1410.050. [DOI] [PubMed] [Google Scholar]
- 9.Sukor N., Kogovsek C., Gordon R.D., Robson D., Stowasser M. Improved quality of life, blood pressure, and biochemical status following laparoscopic adrenalectomy for unilateral primary aldosteronism. J. Clin. Endocrinol. Metab. 2010;95:1360–1364. doi: 10.1210/jc.2009-1763. [DOI] [PubMed] [Google Scholar]
- 10.Sonino N., Fallo F., Fava G.A. Psychological aspects of primary aldosteronism. Psychother. Psychosom. 2006;75(5):327–330. doi: 10.1159/000093956. [DOI] [PubMed] [Google Scholar]
- 11.Ahmed A.H., Gordon R.D., Sukor N., Pimenta E., Stowasser M. Quality of life in patients with bilateral primary aldosteronism before and during treatment with spironolactone and/or amiloride, including a comparison with our previously published results in those with unilateral disease treated surgically. J. Clin. Endocrinol. Metab. 2011;96(9):2904–2911. doi: 10.1210/jc.2011-0138. [DOI] [PubMed] [Google Scholar]
- 12.VelemaM Dekkers T., Hermus A., Timmers H., Lenders J., Groenewoud H., Schultze Kool L., Langenhuijsen J., Prejbisz A., van der Wilt G.-J., Deinum J., Investigators S.P.A.R.T.A.C.U.S. Quality of life in primary aldosteronism: a comparative effectiveness study of adrenalectomy and medical treatment. J. Clin. Endocrinol. Metab. 2018;103(1):16–24. doi: 10.1210/jc.2017-01442. [DOI] [PubMed] [Google Scholar]



