Abstract
In this article, we describe a case of neutrophilic dermatosis of the dorsal hands (NDDH) complicated with myelodysplastic syndrome and chronic active hepatitis C infection. NDDH was first suggested by Galaria et al in 2000. After comparing features of NDDH with Sweet syndrome in terms of encompassing clinical, laboratory, and histological characteristics, it can be concluded that “distributional or localized variant” of Sweet syndrome is classified as NDDH. Early diagnosis and treatment can improve prognosis. Systemic glucocorticoids are the mainstay of treatment.
Keywords: neutrophilic dermatosis of the dorsal hands, coexistence of myelodysplastic syndrome and Sweet syndrome, coexistence of hepatitis C and Sweet syndrome, management of neutrophilic dermatosis of the dorsal hands
Introduction
Sweet syndrome (SS), the eponym for acute febrile neutrophilic dermatosis, is a rare condition. Clinical symptoms, physical features, and pathologic findings are the distinguishing features of this disease. It is characterized by a constellation of clinical symptoms, physical features, and pathologic findings. These include fever, neutrophilia, painful erythematous, and violaceous skin lesions (papules, nodules, pustules, and hemorrhagic bullae). Pathology reveals dense dermal infiltrate consisting predominantly of mature neutrophils typically located in the upper dermis.1-3
Neutrophilic dermatosis of the dorsal hands (NDDH) is a distributional variant of this disease, which in morphology and response to treatment is similar to SS, but the location of the lesion is different and is mainly found on the dorsal aspect of the hands. The exact pathogenesis of SS still remains unknown to this date but is thought to be multifactorial. SS presents in various clinical settings: idiopathic, malignancy-associated, drug-induced, and infections. 1
The malignancy-associated SS occurs as a paraneoplastic syndrome in hematological conditions such as myelodysplastic syndrome (MDS).2,4 Most commonly reported to be related to acute myelogenous leukemia. This disease in particular the dermatosis may arise concurrently, precede, or follow the patient’s initial diagnosis. 1
Chronic active hepatitis (CAHC) has been associated with SS as a main viral etiology. It presents with various skin manifestations, including cryoglobulinemic vasculitis, porphyria cutanea tarda, and erythema multiforme.5,6
This case presents with NDDH associated with both MDS and CAHC infection.
Methods
Approval to report this case was obtained from the Institutional Review Board of Kern Medical. A retrospective review of the patient’s record was performed. Literature search was conducted on PubMed, Research Gate, Google Scholar, UpToDate, and Infectious Diseases Society of America’s Clinical Infectious Diseases Journal database. The following search terms were applied: Sweet syndrome, subtypes of Sweet syndrome, neutrophilic dermatosis management, myelodysplastic syndrome, and chronic active hepatitis C.
Case Presentation
A 76-year-old retired man with CHAC (hepatitis C antibody reactive, antibody index: >11.00 [<0.80: non-reactive, 0.8-0.99: equivocal, 1.00-10.99: reactive, >11.00: reactive, repeat testing using a different methodology will repeat reactive 95% of the time or greater]), JAK2-positive MDS chronic obstructive pulmonary disease, and prostate cancer status posttreatment presented with a 1-year history of recurrent skin lesions over the dorsum of both hands.
He presented with a whole host of medical problems elucidated above under the care of a myriad of practitioners. All of these were reasonably stable except for the pain in his lower extremities, which possibly was related to his MDS.
He spent significant amount of his time gardening without exposure to any noxious chemicals. He denied any recent travel and contact with animals. He first noted small disruptions of the integument on his hands that subsequently developed into bullous skin lesions. These lesions had been described as abscesses and eventually ulcerated. Multiple physicians had attempted to resolve the etiology of this malady over the year prior to his presentation to infectious disease at Kern Medical. Neither surgical nor antimicrobial therapy had resulted in a salutary response.
On physical examination, his appearance was cachectic, sallow, ill-appearing but without distress. Right hand findings were positive for small papules over the dorsal aspect. One centimeter lesion with edematous base over the left middle finger over the dorsum of the proximal interphalangeal joint was also noted (Figure 1).
Figure 1.
Clinical photographs of bilateral upper extremities with violaceous papules and nodules. (A, C) Right hand and (B) left hand at initial clinical presentation. (D) Left hand, third digit, dorsum proximal interphalangeal (PIP) joint prepped and marked for biopsy. (E) Left hand, fifth digit, neutrophilic dermatosis ulcerated lesion on dorsum surface extending from metacarpophalangeal joint to the PIP joint.
Complete blood count demonstrated anemia with hemoglobin of 8.1 g/dL (13.2-17.4), thrombocytopenia with platelet count of 89 × 103/µL (150-450 × 103/µL), neutrophilia with neutrophil count of 9.2 × 103/µL (1.8-7.7 103/µL), eosinophilia with eosinophil count of 1.7 × 103/µL (< 0.7 × 103/µL), and elevated inflammatory indices (erythrocyte sedimentation rate 51 mm/h [<20 mm/h], C-reactive protein 2.50 mg/dL [<0.3 mg/dL]).
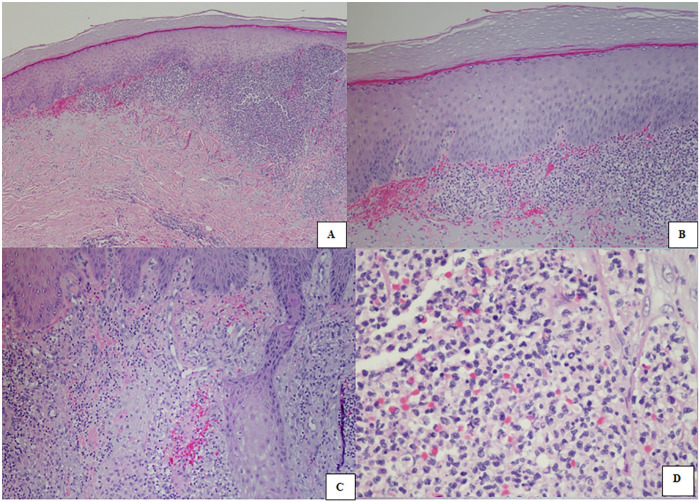
Cutaneous biopsy of a lesion on his left hand third digit showed an intense neutrophilic infiltration in the dermis with leukocytoclastic debris. Vasculitis was not observed (Figure 2). All the cultures including bacterial, fungal, and mycobacterial cultures remained negative.
Figure 2.
The microscopic findings of skin biopsy show the extensive dermal infiltration of neutrophils without vasculitis. The epidermis is spared. Hematoxylin-eosin stain. Magnification: (A) 4×, (B) 10×, (C) 10×, and (D) 40×.
A collaboration of the authors led to a diagnostic impression of NDDH. He was initiated on prednisone 40 mg/day orally for 60 days and discharged home. He was supposed to follow-up in 2 weeks but did not return.
At 3 weeks post discharge, he re-presented to the emergency department. He was evaluated and found to have end-stage liver disease. He re-presented with a new neutrophilic dermatosis lesion 4 weeks post discharge. The lesion measured 2 cm × 1 cm appearing on the medial left index finger extending from proximal to the medic carpal phalangeal joint to just proximal of the proximal interphalangeal joint (Figure 1E). Oral prednisone was increased to 60 mg daily for 90 days. 1
Subsequently, the patient made the decision to be on hospice care and was lost to follow-up.
Discussion
NDDH is commonly recognized to be a localized variant of SS that belongs to the spectrum of neutrophilic dermatoses. 7 The exact etiology still remains uncertain, but the preponderance of available evidence suggests the dermal infiltration by neutrophils as the predominant pathogenic mechanism. 8 Infection is the main differential diagnosis that one can consider for NDDH, for which antibiotics commonly can be used without any response. Atypical pyoderma gangrenosum (PG), acute porphyria tarda, pustular drug eruption, or vasculitis are in the differential diagnosis. 9 NDDH has been associated with both MDS and CAHC.
Based on our search as indicated above, there has not been a reported case of this variant of SS in a person who suffered from both MDS and CAHC. Since this is an unusual syndrome, it often as in this case has a protracted trial of local and systemic therapy to no avail. It is important that physicians particularly in infectious disease and hematology/oncology and plastic surgery be aware of this presentation in all of its manifestations. In order an early diagnosis and appropriate treatment can be initiated.
The lack to fulfill the diagnostic criteria by Maverakis et al 10 did not support atypical PG. 11 Pathology, negative ANCA, and normal urinalysis were not suggestive of vasculitis. The diagnosis of SS is based on major and minor criteria initially established by Su and Liu in 1986, 12 later modified by von den Driesch in 199413-15 (Appendix 1, available online). This patient met both major criteria and 2 minor criteria. 13
SS typically does not ulcerate. If it is present, underlying hematologic malignancy is the usual suspect. Typical SS, atypical SS, and atypical PG have been suggested to represent NDDH particularly when manifesting in this distinctive anatomic distribution.16,17 Papillary dermal edema, diffuse infiltrate of neutrophils without vasculitis can be prominently seen on histology analysis. Admixed lymphocytes are another interesting finding. 7 MDS, acute myeloid leukemia, or lymphoma are the most common hematologic disorders associated with SS.4,16-18 In MDS, refractory anemia is associated with the onset of SS. 2
Although hepatitis B infections are reported to be a potential trigger of SS, 4 previous case reports have associated with CHAC infection.6,19-22
In conclusion, NDDH is best understood as a distributional variant of SS in which lesions exclusively occur on the dorsal aspects of both hands. It is rare but most commonly seen as a paraneoplastic syndrome or an association with infection. It may also be drug-induced or idiopathic. In most of these cases, the initial clinical diagnosis is infection. Antibiotic treatments and surgical debridements may follow without success. This case serves as an essential reminder while highlighting the systemic manifestations of SS. It also demonstrates the importance of interdisciplinary collaboration between infectious disease specialists, hematologists/oncologists, pathologists, and specialized surgeons to facilitate effective diagnosis, triage, management, and outcomes of patients suffering from NDDH. Additionally, recognizing this disorder should prompt clinicians to investigate for any associated malignancy or other systemic disorder.
Supplemental Material
Supplemental material, sj-pdf-1-hic-10.1177_23247096211037458 for Neutrophilic Dermatosis in Myelodysplastic Syndrome and Chronic Active Hepatitis C by Rupam Sharma, Royce H. Johnson, Arash Heidari, Matthew Malerich, William R. Stull and Everardo Cobos in Journal of Investigative Medicine High Impact Case Reports
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: Ethical approval for this case report was obtained from the Kern Medical Institutional Review Board (Approval ID: 20072).
Informed Consent: Written informed consent was obtained from the patient for publication of this case report.
ORCID iDs: Rupam Sharma  https://orcid.org/0000-0003-3457-4371
https://orcid.org/0000-0003-3457-4371
Arash Heidari  https://orcid.org/0000-0003-1091-348X
https://orcid.org/0000-0003-1091-348X
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Cohen PR. Sweet’s syndrome—a comprehensive review of an acute febrile neutrophilic dermatosis. Orphanet J Rare Dis. 2007;2:34. doi: 10.1186/1750-1172-2-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Matsuzawa Y, Adachi E, Takahashi A, et al. Cytokine profile in Sweet’s syndrome under the treatment of pulmonary toxoplasmosis complicated with myelodysplastic syndrome. Intern Med. 2019;58:2079-2083. doi: 10.2169/internalmedicine.2372-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sweet RB. An acute febrile neutrophilic dermatosis. Br J Dermatol. 1964;76:349-356. doi: 10.1111/j.1365-2133.1964.tb14541.x [DOI] [PubMed] [Google Scholar]
- 4. Kawakami T, Kawase A, Takeuchi S, et al. Sweet syndrome subsequent to relapsing polychondritis and myelodysplastic syndrome in a Japanese patient. Acta Derm Venereol. 2008;88:517-519. doi: 10.2340/00015555-0488 [DOI] [PubMed] [Google Scholar]
- 5. Soylu S, Gül Ü, Kılıç A. Cutaneous manifestations in patients positive for anti-hepatitis C virus antibodies. Acta Derm Venereol. 2007;87:49-53. doi: 10.2340/00015555-0186 [DOI] [PubMed] [Google Scholar]
- 6. Guo D, Parsons LM. Sweet syndrome in a patient with chronic hepatitis C. J Cutan Med Surg. 2014;18:436-438. doi: 10.2310/7750.2014.13211 [DOI] [PubMed] [Google Scholar]
- 7. Mobini N, Sadrolashrafi K, Michaels S. Neutrophilic dermatosis of the dorsal hands: report of a case and review of the literature. Case Rep Dermatol Med. 2019;2019:8301585. doi: 10.1155/2019/8301585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cohen PR. Skin lesions of sweet syndrome and its dorsal hand variant contain vasculitis: an oxymoron or an epiphenomenon? Arch Dermatol. 2002;138:400-403. doi: 10.1001/archderm.138.3.400 [DOI] [PubMed] [Google Scholar]
- 9. Larsen H, Danielsen A, Krustrup D, Weismann K. Neutrophil dermatosis of the dorsal hands. J Eur Acad Dermatology Venereol. 2005;19:634-637. doi: 10.1111/j.1468-3083.2005.01241.x [DOI] [PubMed] [Google Scholar]
- 10. Maverakis E, Ma C, Shinkai K, et al. Diagnostic criteria of ulcerative pyoderma gangrenosum: a Delphi consensus of international experts. JAMA Dermatol. 2018;154:461-466. doi: 10.1001/jamadermatol.2017.5980 [DOI] [PubMed] [Google Scholar]
- 11. George C, Deroide F, Rustin M. Pyoderma gangrenosum—a guide to diagnosis and management. Clin Med (Lond). 2019;19:224-228. doi: 10.7861/clinmedicine.19-3-224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Su WP, Liu HN. Diagnostic criteria for Sweet’s syndrome. Cutis. 1986;37:167-174. [PubMed] [Google Scholar]
- 13. von den Driesch P. Sweet’s syndrome (acute febrile neutrophilic dermatosis). J Am Acad Dermatol. 1994;31:535-556. doi: 10.1016/S0190-9622(94)70215-2 [DOI] [PubMed] [Google Scholar]
- 14. Walker DC, Cohen PR. Trimethoprim-sulfamethoxazole-associated acute febrile neutrophilic dermatosis: case report and review of drug-induced Sweet’s syndrome. J Am Acad Dermatol. 1996;34(5 pt 2):918-923. doi: 10.1016/S0190-9622(96)90080-8 [DOI] [PubMed] [Google Scholar]
- 15. Cohen PR. Diagnosing the Sweet syndrome. Ann Intern Med. 1989;110:573-574. doi: 10.7326/0003-4819-110-7-573_2 [DOI] [PubMed] [Google Scholar]
- 16. Walling HW, Snipes CJ, Gerami P, Piette WW. The relationship between neutrophilic dermatosis of the dorsal hands and sweet syndrome: report of 9 cases and comparison to atypical pyoderma gangrenosum. Arch Dermatol. 2006;142:57-63. doi: 10.1001/archderm.142.1.57 [DOI] [PubMed] [Google Scholar]
- 17. Del Pozo J, Sacristan F, Martinez W, Paradela S, Fernández-Jorge B, Fonseca E. Neutrophilic dermatosis of the hands: presentation of eight cases and review of the literature. J Dermatol. 2007;34:243-247. doi: 10.1111/j.1346-8138.2007.00261.x [DOI] [PubMed] [Google Scholar]
- 18. Hirai I, Sakiyama T, Konohana A, Takae Y, Matsuura S. A case of neutrophilic dermatosis of the dorsal hand in acute leukemia—a distributional variant of Sweet’s syndrome [in German]. J Dtsch Dermatol Ges. 2015;13:1033-1034. doi: 10.1111/ddg.12644 [DOI] [PubMed] [Google Scholar]
- 19. Tan E, Yosipovitch G, Giam YC, Tan SH. Bullous Sweet’s syndrome associated with acute hepatitis B infection: a new association. Br J Dermatol. 2000;143:914-916. doi: 10.1046/j.1365-2133.2000.03810.x [DOI] [PubMed] [Google Scholar]
- 20. Baz K, Yazici AC, Kaya TI, et al. Neutrophilic dermatosis of the hands (localized Sweet’s syndrome) in association with chronic hepatitis C and sarcoidosis. Clin Exp Dermatol. 2003;28:377-379. doi: 10.1046/j.1365-2230.2003.01299.x [DOI] [PubMed] [Google Scholar]
- 21. Deasy AM, Walker B, Layton AM, Lacey CJN. Sweet’s syndrome in a patient with haemophilia, HIV and hepatitis C infection. Int J STD AIDS. 2012;23:e11-e13. doi: 10.1258/ijsa.2009.009314 [DOI] [PubMed] [Google Scholar]
- 22. Coelho J, Lourenco S, Marques J, Mendonça P, Malhado JA. Neutrophilic dermatosis of the dorsal hands associated with chronic hepatitis C virus infection. Indian J Dermatol Venereol Leprol. 2008;74:478-480. doi: 10.4103/0378-6323.44304 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-hic-10.1177_23247096211037458 for Neutrophilic Dermatosis in Myelodysplastic Syndrome and Chronic Active Hepatitis C by Rupam Sharma, Royce H. Johnson, Arash Heidari, Matthew Malerich, William R. Stull and Everardo Cobos in Journal of Investigative Medicine High Impact Case Reports