Abstract
Objective:
Number of People Living with Human Immune-deficiency Virus in Ghana is over 300,000 and unmet need for antiretroviral therapy is approximately 60%. This study sought to determine the quality of antiretroviral therapy services in selected ART sites in Ghana using the input-process-outcome approach.
Methods:
This is a descriptive cross-sectional case study that employed modified normative evaluation to assess quality of antiretroviral therapy services in the Oti and Volta regions of Ghana among People Living with HIV (n = 384) and healthcare providers (n = 16). The study was conducted from 11 March to 9 May 2019.
Results:
Resources for managing HIV clients were largely available with the exception of viral load machines, reagents for CD4 counts, and antifungals such as Fluconazole and Cotrimoxazole. Patients enrolled on antiretroviral therapy within 2 weeks was 71% and clients retained in care within 2 weeks of enrolment was 90%. Approximately 26% of enrolled clients recorded viral load suppression; 33% of People Living with HIV who were not insured with the National Health Insurance Scheme paid for some antiretrovirals and cotrimoxazole. Adherence to ART and Cotrimoxazole were 95% and 88%, respectively, using pill count on their last three visits. Time spent with clinical team was among the worst rated (mean = 2.98, standard deviation = 0.54) quality indicators by patients contrary to interpersonal relationship with health provider which was among the best rated (mean = 3.25, standard deviation = 0.41) indicators.
Conclusion:
Observed quality care gaps could potentially reverse gains made in HIV prevention and control in Ghana if not addressed timely; an important value addition of this study is the novel application of input-process-outcome approach in the context of antiretroviral therapy services in Ghana. There is also the need for policy dialogue on inclusion of medications for prophylaxis in antiretroviral therapy on the National Health Insurance Scheme to promote adherence and retention.
Keywords: Quality healthcare, antiretroviral therapy, human immune-deficiency virus, input-process-outcome, indicators, Ghana
Introduction
The criteria for assessing quality of healthcare are many and sometimes complex.1,2 Quality of health service delivery has been investigated extensively on Ghana3,4,5,6,7,8,9 but not comprehensively on Human Immune-deficiency Virus (HIV) and Acquired Immune Deficiency Syndrome (AIDS). HIV is one of the infectious diseases of public health importance in many African countries including Ghana. In Ghana, the estimated number of people living with HIV as at 2018 was 313,063 (91% adults and 9% children). 10 Volta and Oti regions in particular recorded HIV prevalence rate of 2.3% in 2017 above the national average of 2.1% in 2017. 11
Consequently, Ghana adapted the 90-90-90 UNAIDS global aspirational targets by 2020 when 90% of eligible clients should have known their status, 90% of those who know their status should have been on antiretroviral therapy (ART) and 90% of those on treatment should have their viral load suppressed. 12 Unfortunately, none of these targets have been met yet in many afflicted countries, including Ghana. By the end of December 2018, Ghana’s performance in respect of these targets was 66-37-64 with no hopes of attaining the 90-90-90 targets. 13 Likewise, only 110,000 out of 316,613 People Living with HIV (PLHIV) were on ART in 2018. Unmet need for ART in Ghana remains at approximately 60% and paediatric ART coverage is barely 30%. 13 Poor quality of ART services rendered to PLHIV is partly to blame for this poor performance in Ghana.
Even though ART enrolment rates in the Volta and Oti regions are above the national average, retention remains a challenge. Although 2306 new PLHIV clients were enrolled in ART in 2018, only 48% of them received sustained treatment. 10
Unfortunately, there is paucity of empirical literature on quality of ART services in the Volta and Oti regions of Ghana, albeit burden of the disease is high in these regions due to challenges of human and material medical logistics14,15 and non-adherence to standard treatment guidelines for HIV/AIDS.16,17,18,19 Moreover, application of the input-process-outcome quality care indicators are rarely used in the context of ART clinical care in Ghana and many resource-poor settings.
Even though some previous studies have investigated into quality of HIV services in Ghana 15 and elsewhere,17,18,19 none of these studies focused on input-process-outcome quality care indicators. Our study therefore adopted this approach to ascertain the quality of ART services for PLHIV to help address opportunities and threats to attaining the newly defined targets of 95-95-95 by the year 2030 in Ghana.
Interventions towards quality HIV services in Ghana
Quality HIV/AIDS care is defined as performance according to recommended standards of care and it also involves interventions that are known to be safe, affordable and have ability to alleviate disease complications and death among PLHIV.20,21 Standards of quality HIV/AIDS care are furthermore regarded as expectations of performance, and they represent a generic statement of what is expected of the HIV service or sentinel site. Standards are known to help improve quality of care obtainable, shape behaviour of positive service provision, eliminate undesirable variation in the process of care and provide a framework for measuring outcomes.22,23 A number of interventions have been initiated in Ghana to promote quality ART services. These interventions are briefly reviewed in this paper.
Differentiated service delivery in Ghana
Differentiated strategies across the cascade of HIV care has been adopted to meet the needs of diverse populations. With this differentiated service delivery concept, stable clients can now be offered medications up to 6 months refill dates. 13 A study by Barker 22 demonstrated that differentiated service delivery offers significant productive gains in terms of reduction in costs, health workforce needs and costs of scaling up community-based ART support services.
Introduction of Dolutegravir (Integrase Strand Transfer Inhibitor)
Dolutegravir based treatment is now the preferred first line regimen over reverse transcriptase inhibitors in all adults, adolescents and children weighing at least 20 kg in Ghana starting from July, 2019. This is because, Dolutegravir has been found to be more effective in achieving viral load suppression in a shorter time and better tolerated since it is protective against risk of discontinuation of treatment as a result of adverse effects from Boosted Protease Inhibitors and Efavirenz.
Consolidated guidelines for HIV care in Ghana (Test, Treat and Track)
Ghana updated its national HIV care guideline to include newly recommended HIV testing and linkage strategies, ARV drug regimens, formulations and diagnostics that are appropriate to the local setting. 13 Establishing linkage to care from the time the client is identified to follow-up care as the standard flow of HIV care which is in line with the 90/90/90 goals is the main reason for the consolidation of all existing guidelines into one document. 13
Other updates in the consolidated guidelines include introduction of provider-initiated testing and counselling at high yield areas like antenatal, outpatient, Directly Observed Treatment Short-course (DOTs) corner, emergency room, postnatal, child welfare and nutritional rehabilitation centres. Other components of the integrated guidelines are PLHIV diagnosed should be offered family and partner support testing as an index case so that contacts are diagnosed as well (contact tracing); men and key populations who do not come to clinics should be targeted with a differentiated service delivery in form of outreaches; and 3-test algorithm to improve true positivity rate in low prevalence countries.
Hence to diagnose HIV in Ghana, first response, oral-quick and SD bioline results must all be positive; EID algorithm has been updated to include DNA PCR testing at 9 months after negative test for the first 6 weeks of life should be done; any client who is not adherent to treatment should be offered enhanced adherence counselling. Finally, everyone who tests positive should be linked to care and treat all policy.
Adherence to standards
For the purpose of this study, adherence to standards is defined as compliance to HIV/AIDS diagnostic and treatment guidelines prescribed by guidelines for ART in Ghana. 10 Medication adherence refers to the entire process from selecting, initiating treatment to maintenance of a particular therapeutic medication regimen with the aim of controlling the viral replication. Discontinuity or cessation of part or all of the treatment in instances of missing doses, drug holidays, overdosing or under-dosing is referred to as non-adherence. 24
In view of this, viral load monitoring is very important as a means of monitoring treatment progress. It is also a means of avoiding the risk of staying on a failing first-line regimen and developing drug-resistance HIV variants. 25 High viral load translates into virological failure and increased morbidity. 25 In addition, recommendation for ART monitoring by World Health Organization (WHO) has changed from CD4 monitoring every 6 months to viral load testing. Nevertheless, in the absence of routine viral load testing, CD4 count and clinical monitoring ought to be used to confirm treatment failure. 25
Conceptual framework
Quality healthcare has been defined as attributes or properties of the process of care as well as goals or objectives of that process. 1 This study adopted the in-put-process-outcome framework by Donabedian 1 who argued that quality of medical care can be assessed based on input-process-outcome indicators. Components of the framework are briefly discussed.
Input indicators: The reviewed literature generally describes these indicators as essential components relating to environmental conditions under which care is provided and the effect on the quality of healthcare rendered to clients. These indicators include material resources and e-medical equipment; human resources and organizational characteristics such as organization of the medical, pharmaceutical nursing and allied health staffs. The kind of supervision and performance review, methods of paying for healthcare are also considered as input quality indicators. 1
Process indicators: Process indicators, on the other hand, mean the activities that constitute healthcare including diagnosis, treatment or management, rehabilitation, prevention and patient education which are usually carried out by professional personnel. The process of healthcare delivery such as adherence to standard operating procedures and protocols are particularly important in assessment of healthcare quality. Quality care experts have intimated that the process indicators are critical because health outcomes are a product of these processes and must be given the needed attention. 1
Outcome Indicators: Outcome indicators in the service delivery value chain are measured in terms of recovery rates, prompt service delivery, restoration of function and survival.1,25 Other outcome measures are perceived social support during care, respect and dignity, and client-centred communication. Validity of outcome indicators as measures of quality is generally accepted and clients’ views of recovery, restoration and survival are often not questioned since outcome indicators tend to be objectively tangible and outwardly amenable to more exact measurement. 1
Limitations of relying on outcome quality indicators must, however, be acknowledged. For example, many factors independent of medical care may influence health outcomes. Care must therefore be taken to control vital factors other than medical care constant if valid conclusions are to be drawn. This paper thus adopts the novel approach of assessing healthcare quality using mainly input-process indicators to understand the quality care dynamics in the context of ART services.
Study objectives
In view of the demonstrated gaps in the literature on quality of HIV services in Ghana and other resource poor settings, this study sought to ascertain the quality of ART services for PLHIV to help address opportunities and threats to attaining the newly defined targets of 95-95-95 by the year 2030 in Ghana. Specifically, the sought to first ascertain quality of HIV services in the selected antiretroviral sites measured by the input, process and outcome quality care indicators; second, understand the perspectives of healthcare providers on challenges and interventions to promote quality HIV services to clients; finally, determine patients’ rated satisfaction with HIV services in the selected antiretroviral sites.
Method
Design
This is a descriptive cross-sectional case study that employed modified normative evaluation based on Donabedian’s model of healthcare quality. 1 The modified normative evaluation is an evaluation procedure where standards as per Ghana’s guidelines for HIV management are compared with the prevailing situation in the various study sites. The modified normative evaluation emphasizes context-specific evaluation approach as against a one-size-fits-all. 26 In this study, the approach was used to assess quality of HIV care in the selected ART sites using patient clinical records according to Ghana’s guidelines for HIV management. For the purpose of this paper, only the input and process indicators of healthcare quality are reported.
Setting and population
The study was conducted in Ho, Hohoe and Jasikan districts in the Volta and Oti regions. Volta and Oti regions are 2 of the 16 administrative regions in Ghana. Per the 2010 population and housing census, the population of Jasikan, Hohoe and Ho Municipal were 59,181; 262,046 and 271,881 respectively. 27 Three HIV Sentinel sites offering ART services as at June, 2019 were purposively selected from the three administrative districts. The three purposively selected ART sites were Jasikan District Hospital (rural), Hohoe Municipal Hospital (peri-urban) and Ho Teaching Hospital (urban). All these facilities are national sentinel sites for HIV management with fully functioning ART clinics. The target population size is the of clinical records of 1,500 PLHIV from the three ART sites at the time of conducting this study. Thus, Ho Teaching Hospital (N = 745), Hohoe Municipal Hospital (N = 450), and Jasikan District Hospital (N = 305).
Ho teaching hospital ART sentinel site
This ART site is hosted in a 240-bed capacity tertiary hospital under the Ministry of Health. It serves as the regional referral health facility in its catchment area including neighbouring Republic of Togo. The hospital records are averagely 160 daily attendance. Healthcare services provided include outpatient/inpatient services, dental, eye, family planning, mental health, maternal and child health, surgical, physiotherapy, radiography, herbal Medicine, pharmacy, internal medicine, laboratory, ART clinic and mortuary services.
Hohoe municipal hospital ART sentinel site
This ART site is hosted in a 178-bed secondary referral hospital under the Ghana Health Service (GHS). Average daily attendance is 150. Services provided in this secondary hospital include outpatient/admissions, pharmacy, laboratory, dental, physiotherapy, medical imaging, antenatal, maternity, surgical, ART, eye and mortuary services.
Jasikan district hospital ART sentinel site
This ART site is hosted in a 53-bed secondary hospital also under the GHS. Average daily out-patient attendance is 165. Services provided include outpatient/admissions, pharmacy, laboratory, pharmacy, X-ray, antenatal, maternity, ART, eye and other specialized services.
Sample size and sampling procedure
Target study population was all registered PLHIV above the age of 18 years enrolled in ART for at least six (6) months. Sample size for the clinical records review was 384 from all the three ART sites. The sample size was calculated using the formula: n = Z²PQ/d² where: n = sample size; Z = statistic for a 95% Confidence Interval; P = expected outcome; Q = complement of P and d = precision (fixed at 5%). Based on findings from a study conducted in Nigeria, 28 it was found that approximately 49% of PLHIV rated quality of service delivery as excellent. Thus, an expected outcome of 49% rated satisfaction was used for the sample size determination. At the time of conducting this study there was no known data on similar studies in Ghana hence reliance on evidence in Olowookere et al. 28 with the following assumed parameters: P (expected outcome = 0.487); Q (1 P = 1- 0.487 = 0.513); n = Z²PQ/d²; (1.96) 2 x 0.487 x 0.513/ (0.05); 2 = 383.84 ≈ 384.
Final selection of the sample was done using multi-stage sampling to allocate sample sizes to the ART sites. Percentage share of PLHIV in the Ho Teaching Hospital, Hohoe Municipal Hospital and Jasikan District are 50%, 30% and 20% respectively. Based on these proportions, the sample size allocation through quota system was as follows: Ho Teaching Hospital (50/100*384 = 191), Hohoe Municipal Hospital (30/100*384 = 115), and Jasikan District Hospital (20/100*384 = 79). Subsequently, clinical record reviews were conducted on all the 384 sampled PLHIV in each of the ART sites. Healthcare providers (n = 16) directly involved in the care of PLHIV were also purposively sampled and engaged through interviews to ascertain the providers’ perspectives on the quality of ART services.
Inclusion criteria
PLHIV enrolled in ART for at least 6 months, age 18 years or more, access care in the three ART sentinel sites and voluntarily agreed to participate in the study.
Exclusion criteria
The study excluded PLHIV who were lost to follow-up for over a year; those who were transferred in or out of selected ART sites, and those who visited the clinic for the first time on the day of data collection. Patients with Tuberculosis co-morbidities were equally excluded.
Data collection instruments
A modified normative evaluation tool based on an adapted Donabedian’s input–process–outcome model of health care quality. 28 Ghana’s guideline for HIV management informed data collection instrument items for the process and outcome quality indicators. Inventory data extraction tool designed according to the national resource requirement for the management of HIV in Ghana was used to assess input quality indicators.
Proxy measurement of antiretrovirals (ARVs) adherence rate
Adherence to ARVs was measured by dividing the number of people enrolled in ART and consistently took their ARVs without default (through pill count) over the total number of enrolled patients and multiplied by 100. The authors, however, acknowledge the limitations of using pill counts as a proxy for ARVs adherence. Pill count is highly subject to bias and might not account for missed doses due to falls and stock piling at home. 29
Validity and reliability
Face validity was done by giving data collection tools/extraction forms to independent reviewers in the field of HIV to determine whether questions measured the indicators of interest as per Donabedian 1 validated test items for measuring medical technical quality. Tools were also pre-tested in a comparable health facility in the Volta region to address ambiguity in questions and typographical errors to enhance internal validity. Also, all tool items were developed based on the study objectives alongside strict monitoring during the data collection, entry, cleaning and analysis.
Data collection procedure and data sources
Data collection in all the three ART sites lasted approximately 3 months from 11 March to 9 May 2019. In terms of the input quality indicators, availability of resources was assessed through inventory data extraction according to the national resource requirement for the management of HIV in Ghana. Health staff who were in-charge of various resources such as head of Pharmacy, Laboratory, Medical Superintendent and Health Services Administrators were interviewed for secondary data verification. Data collection technique entailed review of patient management records using data extraction tools. The steps were as follows: first, patient folder numbers (i.e manual folders or electronic folders through e-tracker) were used to retrieve medical records for data extraction on adherence to national guidelines and outcome of care.
In addition, availability of resources was checked with requirements of the Ghana National AIDS and Sexually Transmitted Infections (STIs) Control Programme (NACP). Data on outcome indicators of quality care were from clients’ clinical records and client satisfaction survey tools administered on site.
Data analysis and variable definitions
Field data were coded, cleaned and analysis done with SPSS-IBM Version 22. Descriptive Statistics were generated including Chi-square and Fisher’s Exact tests to ascertain associations between variables as appropriate. Summary statistics were generated for continuous variables, percentages and frequency distributions were generated for categorical variables.
In addition, after an orthogonal unrotated Principal Component Analysis (PCA), 8 out of the 32 items were retained for final analysis. Subsequently, summary statistics (means and standard deviations) were used to ascertain the average responses of patients on the Likert-type scale items. Test for statistical significance was set at 95% confidence level. Normality testing of data was done in GraphPad Prism to check for distribution, skewness and kurtosis before analysis. Visual inspection of data was done on SPSS-IBM to check for missing data and normality.
Data from the semi-structured interviews with health staff was captured, cleaned and coded using SPSS -IBM Version 22. Analysis strategy was mainly descriptive statistics to demonstrate staff perspectives on the quality of ART services in the three ART sites. Since the variables of interest were mainly quantitative measures in nature, the data collection approach was quantitative.
Input indicators: Proxies for input indicators were centred on resource availability. For the purposes of this study the input factors were: resource availability including antiretroviral medicines, laboratory reagents, equipment, trained healthcare providers and logistics.
Process indicators: On the other hand, process quality indicators were determined based on adherence to national guidelines for HIV diagnostic and treatment and Donabedian’s model for service quality. 1
These indicators were reviewed by clinicians working on the HIV control programme as well as those providing HIV care in the facilities to promote institutional relevance of the tool. Medication adherence as operationalized in this study ranged from treatment initiation to maintenance of a particular therapeutic medication regimen to control viral replication and improving
immune system function. Discontinuity or cessation of part or all of the treatment in instances of missing doses, drug holidays, overdosing or under-dosing is referred to as non-adherence.
Outcome indicators: Outcome quality indicators were measured using technical and functional quality proxies. The technical quality measures were patients’ adherence to medication and clinical improvement in functional status based on objective documentation in the clients’ clinical folders. Functional outcome quality care dimensions were client satisfaction scores on dimensions of healthcare quality. Total of 32 client perceived service quality indicators were developed based on national guidelines for HIV care and adapted Donabedian’s structure-process-outcome model of health care quality. After principal component analysis (PCA), the 32 factors were further scaled down to eight (8), comprising of patient satisfaction with general services; technical quality; interpersonal relations; communication; financial accessibility; time spent with clinical team; accessibility and convenience and other patient satisfaction factors. Five-point Likert-type scale used to measure satisfaction levels ranging from 1 = ‘Very dissatisfied’ – 5 ‘Very satisfied’.
Ethical consideration
This study was granted ethical approval by the Ghana Health Service (GHS) Ethical Review Committee (ERC) (clearance number: GHS-ERC009/08/19). Administrative approvals were also sought from the respective health facility heads. To promote anonymity of the study sites, codes used in place of participants’ names to guarantee their privacy and confidentiality. Collated data was kept on a password protected computer and kept with the Principal Investigator. Participation in the study was voluntary and participants were told to discontinue from the study anytime they so wish without consequences. Only participants who voluntarily signed the informed consent form were allowed to participate in the study.
Informed consent
Participation in the study was voluntary and were told to discontinue from the study anytime they so wish without consequences. Only participants who voluntarily signed the informed consent form were allowed to participate in the study. Written informed consent was obtained from all subjects. In the case of minors (persons below 18 years), written informed consent from legally authorized representatives (locus parentis) was obtained before they were included in the study. Please see Supplementary File 1 for Consent Forms for the various study respondents.
Findings
Demographic characteristics
Approximately 82% of the 384 study participants were females; over 90% were aged 31 + years while over 40% were married; more than 70% had at most middle or junior high school education qualification; nearly 82% were employed in the informal sector; over 90% were Christians; nearly 100% were on antiretrovirals (ARVs) and 41% of them had a health insurance cover; 58% of the respondents’ insurance status was not documented (see Table 1).
Table 1.
Summary of demographic characteristics of the population studied (n = 384).
| Variables | Statistic | |
|---|---|---|
| Sex | Frequency (f) | Percentage (%) |
| Male | 70 | 18 |
| Female | 314 | 82 |
| Age | ||
| <15 years | 5 | 1 |
| 15–30 years | 30 | 8 |
| 31–45 years | 157 | 41 |
| 45+ years | 192 | 50 |
| Marital status | ||
| Married | 163 | 43 |
| Co-habiting | 20 | 5 |
| Divorced | 96 | 25 |
| Widowed | 65 | 17 |
| Never-married | 40 | 10 |
| Educational status | ||
| Tertiary | 30 | 8 |
| Secondary | 72 | 19 |
| JHS/Middle level | 178 | 46 |
| Primary | 69 | 18 |
| No-education | 35 | 9 |
| Employment status | ||
| Formal | 43 | 11 |
| Informal | 313 | 82 |
| None | 28 | 7 |
| Residential location | ||
| Urban | 84 | 22 |
| Peri-urban | 43 | 11 |
| Rural | 257 | 67 |
| Religion | ||
| Christian | 356 | 93 |
| Moslem | 28 | 7 |
| Actively enrolled on antiretroviral | ||
| No | 4 | 1 |
| Yes | 380 | 99 |
| Health insurance status | ||
| Uninsured | 4 | 1 |
| Insured | 157 | 41 |
| No record | 223 | 58 |
Source: Field Data (March-May, 2019); *Note: all frequencies and percentages have been rounded off to the nearest decimal; JHS (Junior Higher School); Formal employment (in this context means employment with a government agency).
Table 2 shows the background characteristics of healthcare providers (n = 16) who were engaged in semi-structured interviews to ascertain their views on quality of HIV services to clients. Majority of the health providers were nurses and over 60% located in urban settings; 56% were males; 69% were married and 94% had at least tertiary education (see Table 2).
Table 2.
Demographic Characteristic of Care Providers (n = 16).
| Variable | Freq. (f)* | Percentage (%)* |
|---|---|---|
| Health facility Name | ||
| Hohoe Municipal Hospital | 5 | 31 |
| Jasikan District Hospital | 6 | 38 |
| Volta Regional Hospital | 5 | 31 |
| Professional category | ||
| Nurse | 4 | 25 |
| Pharmacist | 2 | 13 |
| BMS | 2 | 13 |
| Data manager | 2 | 13 |
| Physician | 1 | 6 |
| Pharmacy technician | 1 | 6 |
| Physician assistant | 1 | 6 |
| Disease control | 1 | 6 |
| Nutritionists/dietician | 1 | 6 |
| Orderly | 1 | 6 |
| Location | ||
| Urban | 10 | 63 |
| Peri-Urban | 6 | 34 |
| Total | 16 | 100 |
| Sex | ||
| Male | 9 | 56 |
| Female | 7 | 44 |
| Age | ||
| 18–30 | 7 | 44 |
| >30 | 9 | 56 |
| Marital status | ||
| Married | 11 | 69 |
| Never married/single | 5 | 31 |
| Education | ||
| Tertiary | 15 | 94 |
| Secondary | 1 | 6 |
Source: Field Data (March-May, 2019); *Note: all frequencies and percentages have been rounded off to the nearest decimal.
Medical resource availability for ART services (input quality indicators)
With the exception of the Hohoe Municipal hospital that used separate laboratory services for the ART clinic, the Ho Teaching Hospital and Jasikan District Hospital relied on the main laboratories of the facilities where the sites are located. It was observed that, retooling of the laboratories in Ho Teaching Hospital and Jasikan District Hospital was done with the help of funds from National AIDS Control Programme (NACP). Also, viral load tests and other required laboratory tests were mainly done at Ho Teaching Hospital which is located in the regional capital of the Volta Region. In addition, reagents for CD4 tests were consistently not available in all the three ART sites involved in this study (see Table 3).
Table 3.
Summary of resources available for HIV care provision at the three facilities.
| Variables | Sub-categories | Statistic | |
|---|---|---|---|
| Frequency (f) | Percentage (%) | ||
| ARVs | Tenofovir + Lamivudine + Efavirenz | 5 | 83 |
| Tenofovir Lamivudine | 6 | 100 | |
| Efavirenz 600 mg: | 2 | 33 | |
| Nevirapine 200 mg | 6 | 100 | |
| Zidovudine + Lamivudine + Nevirapine | 4 | 67 | |
| Zidovudine + Lamivudine (adult) | 6 | 100 | |
| Zidovudine + Lamivudine (Paed) | 6 | 100 | |
| Zidovudine Syrup | 6 | 100 | |
| Nevirapine Syrup | 4 | 67 | |
| Abacavir + Lamivudine (Paed) | 2 | 33 | |
| Lopinavir/ritonavir (Third line and PEP) | 2 | 33 | |
| Cotrimoxazole Tablet | 5 | 83 | |
| Was Cotrimoxazole supplied from the RMS/NAC | 6 | 100 | |
| Tab Fluconazole 150 mg | 4 | 67 | |
| Tab Fluconazole 200 mg | 0 | 0 | |
| Fluconazole supplied from the RMS/NACP | 0 | 0 | |
| Patients paid for the medication | 2 | 33 | |
| Clinic aids | Nutritious Mixtures (FBF) | 4 | 67 |
| Demonstration Charts for patients | 2 | 33 | |
| Treatment guidelines and/or algorithms | 6 | 100 | |
| Trained staff | Laboratory staff | 6 | 100 |
| Pharmacy staff | 6 | 100 | |
| Prescriber/Clinician | 6 | 100 | |
| Task shift officer | 4 | ||
| Nurse | 6 | 100 | |
| Data manager | 6 | 100 | |
| Counsellor | 6 | 100 | |
| Nutritionist/dietician | 4 | 67 | |
| Social worker | 2 | 33 | |
| Psychosocial support provider | 2 | 33 | |
NACP: National AIDS Control Programme.
Source: Field Data (March-May, 2019); *Note: all frequencies and percentages have been rounded off to the nearest decimal.
In terms of availability of ARVs, it was also observed that all essential ARVs were available except Fluconazole Capsule 200 mg. Likewise, Nevirapine Syrup was not available at the pharmacies at the time of the researchers’ visit. Similarly, Cotrimoxazole was only available at intermittent periods in all facilities visited over the period.
Furthermore, demonstration charts were not available in one of the ART sites visited. Another observation was that in 33% of the cases, PLHIV who were not insured with the National Health Insurance Scheme (NHIS) paid for some ARVs and Cotrimoxazole at the Regional Medical Stores (RMS). In all three ART sites, there was lack of functional viral load machines, reagents for CD4 testing and PCR analyzers in the laboratories (see Table 3).
Adherence to standard protocols for ART services (process quality indicators)
The reviewed medical records showed that out of a total of 384 clients, 93 (24.2%) had their first time CD4 count tests done within 2 weeks after first ART clinic visit. Out of the 384 participants, 33.1% had baseline tests done before initiation of treatment based on type of medication being initiated and clinical suspicion.
In terms of the opportunistic infections therapy, percentage of eligible clients who had CD4 count below 350 cells/µl and on Cotrimoxazole prophylaxis was 14.8%; 90.1% of the 384 eligible PLHIV were continually retained in care by adhering to appointment dates consistently; only 7% of PLHIV had CD4 count tests done at least once in the last six (6) months. It was found that 70.6% of the PLHIV were on ARVs within two (2) weeks of assessment (see Table 4).
Table 4.
Summary of performance on process indicators of quality at the three hospitals.
| Quality indicators | Frequency (f) | Percentage % (95% CI) |
|---|---|---|
| Care during enrolment to HIV clinic | ||
| Received first-time CD4 count within 2 weeks after first HIV clinic visit | 93 | 24.2 (20.2, 28.8) |
| Had baseline liver/renal function tests and haemoglobin (Hb) tests done before initiation of ARVs. | 127 | 33.1 (28.5, 38.0) |
| Opportunistic infection prevention and ART follow-up | ||
| CD4 count < 350 cells/µl and currently on Cotrimoxazole prophylactic therapy | 57 | 14.8 (11.6, 18.8) |
| Patients with continued care | 346 | 90.1 (86.7, 92.7) |
| Patients who had CD4 count measured at least once during the last 6 months | 27 | 7.0 (4.9, 10.1) |
| Patients eligible for ARV who are currently on ARV | 376 | 97.9 (95.9, 99.0) |
| Patients started on ART within 2 weeks after clinical eligibility is confirmed | 271 | 70.6 (65.8, 74.9) |
| Patients started on ART who have viral suppression by 90% | 98 | 25.5 (21.4, 30.1) |
| Patients on NVP who had LFT at least once within 1 month after initiation of NVP-based ART | 40 | 22.0 (16.5, 28.6) |
| Patients on TFV based ARV | 194 | 50.5 (45.5, 55.5) |
| Patients on TFV who had RFT at least once within 1 month after initiation of TFV-based ART | 55 | 28.4(22.4, 35.1) |
| Patients started on ZDV who had HB at least once within 1 month after initiation of ZDV based HAART | 43 | 24.4 (18.6, 31.4) |
| Patients on ART for whom adherence is measured on last three visits | 344 | 89.6 (86.1, 92.3) |
| Patients lost to follow up within the last 6 months | 44 | 11.5 (8.6, 15.1) |
| Record completeness | ||
| Patients with previous ARV regimen changed for whom reason for change in regime is documented | 78 | 20.3 (16.6, 24.7) |
| Patients on ARV who had registered own and contact address of treatment supporter | 335 | 87.2 (83.5, 90.2) |
| Adherence to medications | ||
| Patients on ARV with at least 95% reported adherence on last visit | 337 | 87.8 (84.1, 90.7) |
| Patients on Cotrimoxazole prophylaxis with at least 95% reported adherence on last visit | 282 | 73.4 (68.8, 77.6) |
| Immunologic and clinical response to HIV care | ||
| Patients with CD4 count greater than 200 cells/µL documented (376 not documented, 3 < 200 cells/µL) | 5 | 1.3 (0.5, 3.1) |
| Bedridden or ambulatory patients who have improvement in functional status | 361 | 94.0 (91.1, 96.0) |
ARV: Antiretroviral; HIV: Human immunodeficiency virus; HAART: Highly active antiretroviral therapy; NV: Nevirapine; LFT: Liver functioning test; TFV; ZDV (Zidovudine); HB; CD4 (Cell Surface marker for T-helper lymphocytes).
Source: Field Data (March-May, 2019); *Note: all frequencies and percentages have been rounded off to the nearest decimal.
At the time of data collection, proportion of PLHIV on ARVs with at least 90% viral load suppression was 25.5% (98 out of 384). With respect to patient safety, out of 181 clients who initiated Zidovudine, 40 (22%) had baseline haemoglobin, renal function and liver function tests done. Moreover, 28.4% of the 194 PLHIV who initiated Tenofovir had baseline haemoglobin, renal function and liver function tests done. Furthermore, 43 out 150 PLHIV (24.4%) who initiated Nevirapine-based regimens had baseline haemoglobin, renal function and liver function tests done at least once a month to ascertain level of risk or safety. On nearly 100% of instances, renal function tests were not done before initiation of Tenofovir-based ARVs, the first line regimen. It was also found that 89.6% of the 384 PLHIV had their adherence levels measured; 20.3% of the 384 PLHIV had their regiments changed and documented. PLHIV who registered their addresses and caregivers were 335 (87.2%).
Patients’ adherence to medication and clinical improvement in functional status were used to measure the accomplishment of desired outcomes of quality care (see Table 4). Number of clients who had their first time CD4 count higher than 200 cells/µL of blood was 5 (1.3%). Large proportion of clients, 376 (97.9%) had no documentation on CD4 count tests. Patient’s functional status was assessed using documentation in the patients’ clinical folders. A total of 361 (94%) PLHIV had improvement in functional status (see Table 4).
Table 5 shows a summary of patient satisfaction scores on dimensions of healthcare quality. The worst perceived quality indicator was ‘general satisfaction’ (mean = 2.9, SD = 0.47), followed by ‘time spent with clinical team’ (mean = 2.98, SD = 0.54). ‘Interpersonal relationship with health provider’ was the most perceived positive indicator (mean = 3.25, SD = 0.41) (see Table 5).
Table 5.
Summary of mean patient satisfaction scores (n = 384).
| Patient Satisfaction indicators | Statistic | |
|---|---|---|
| Score | SD | |
| Satisfaction with general services | 2.90 | 0.47 |
| Technical Quality | 3.00 | 0.29 |
| Interpersonal relations | 3.25 | 0.41 |
| Communication | 3.08 | 0.41 |
| Financial accessibility | 3.07 | 0.58 |
| Time spent with Clinical Team | 2.98 | 0.54 |
| Accessibility and Convenience | 3.08 | 0.30 |
| Other satisfaction factors | 2.21 | 0.22 |
SD: standard deviation.
Source: Field Data (March-May, 2019); SD (Standard deviation).
Note: mean and standard deviation scores rounded to the nearest. High standard deviation suggests better satisfaction with the service component and vice versa.
Healthcare providers’ perspectives on quality of ART services
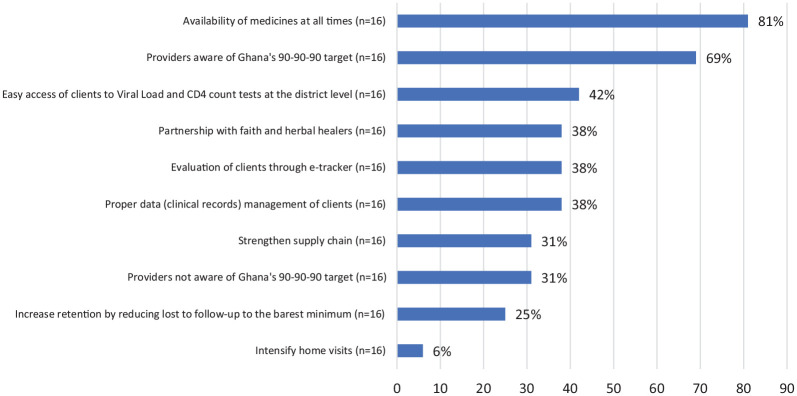
Healthcare providers involved in the care of PLHIV were engaged to determine their knowledge levels on ART protocols and perceptions of the quality of ART services rendered to clients. Table 6 shows the responses of healthcare providers in respect of quality of ART services. It was found that 69% of staff had knowledge on Ghana’s status with respect to UNAIDS 90-90-90 strategic goal (see Figure 1). Majority of staff (81%) believed that availability of medicines (ARVs and prophylactic medicines) will improve care. This was followed by easy access to Viral Load and CD4 count machines at the district level and proper management of clients’ data. HIV self-testing and monitoring was the least considered (6%) (see Figure 1).
Table 6.
Summary of responses from care provider semi-structured interviews.
| Indicators | Statistic | ||
|---|---|---|---|
| During medication/logistic/equipment shortage | Obs. | Freq. (f) | Percent. (%) |
| Tell clients there is shortage | 16 | 2 | 13 |
| Arrange request through stores to Regional Medical Stores (RMS) | 16 | 10 | 63 |
| Contact colleagues from sister facilities for support | 16 | 11 | 69 |
| Average duration for stock replacement | |||
| Not predictable | 16 | 5 | 31 |
| Wait on last mile distribution schedule from RMS | 16 | 6 | 38 |
| Within one week | 16 | 3 | 19 |
| After a month | 16 | 1 | 6 |
| More than a month | 16 | 1 | 6 |
| Medicines/logistical challenges | |||
| Frequent shortages | 15 | 1 | 7 |
| Products with short shelve lives being issued from RMS | 15 | 3 | 20 |
| Lack of Viral Load Machines | 15 | 9 | 60 |
| Lack of reagents | 15 | 1 | 7 |
| Lack of paediatric doses of medications | 15 | 2 | 13 |
| Views on the 90-90-90 strategic goal | |||
| Very ambitious | 16 | 6 | 38 |
| Focus on preventive measures instead of managing PLHIV | 16 | 3 | 19 |
| Just appropriate | 16 | 8 | 50 |
| Not well resourced to help attain goal | 16 | 1 | 6 |
| Ghana’s ability to achieve 90-90-90 strategic goal | |||
| Can be achieved by 2020 | 16 | 1 | 6 |
| Can be achieved but not in 2020 | 16 | 14 | 88 |
| Can only be achieved when there is total committed political will | 16 | 4 | 25 |
| Recommendations towards eradicating HIV by 2030 | |||
| Preventive measures | 16 | 7 | 44 |
| Political will | 16 | 3 | 19 |
| Education and sensitization | 16 | 14 | 88 |
| Efforts targeting males and key populations | 16 | 4 | 25 |
PLHIV: People living with HIV; RMS: Regional Medical Stores.
Source: Field Data (March-May, 2019).
Note: mean and standard deviation scores rounded to the nearest.
Figure 1.
Providers’ awareness of Ghana 90-90-90 target and thoughts on ways to improve HIV care quality.
Source: Field Data (March-May, 2019); *Note: mean and standard deviation scores rounded to the nearest.
Regarding resource management, it was observed that support from sister facilities was the main option (68.8%) considered by providers in situations of shortages followed by reliance on the Last Mile Distribution (LMD) for schedule delivery of commodities. Time taken to replenish stock was however not predictable. Lack of viral load checking machines was the main challenge facing care providers. Finally, education/sensitization (87.5%) and preventive measures (43.8%) were highly considered by healthcare providers as a means of eradicating the epidemic by 2030 (see Table 6).
Discussion
Over 80% of the population of PLHIV being females in this study reflects the national picture on a relatively higher HIV/AIDS prevalence among females than males. 30 This observation is partly due to the compulsory prevention of mother to child transmission of HIV (PMTCT) where females are tested as part of the routine antenatal care (ANC) services. Interpretation of the study findings should therefore be made within this context since opinions expressed on quality of ART services are likely to be influenced by the female-dominated sampled respondents.
Findings from this study generally revealed that important components of ART services were not sufficiently rendered to clients. However, 71% of eligible clients were enrolled on ART within 2 weeks of diagnosis compared to the 60% unmet need for ART according to 2016 NACP report. 13 This observation is reassuring because the benefits and importance of early ART in reducing both AIDS and non-AIDS associated diseases have been established by large-scale clinical trials.31,32
Nonetheless, there is the need for increased adherence to national guidelines on initiation and monitoring of ART to avoid complications. 30 Ghana’s ART coverage is among the lowest in Africa compared to Eastern and Southern Africa countries. There is therefore the need to intensive campaigns on testing, enrolment and retention in ART. One of the key interventions towards achieving high ART coverage is to address stigma, prioritize client-centred quality of care services coupled with enhanced quality care standards.
In addition, it was observed that the quality of care provided to clients during enrolment onto ART was not optimal, evident in only 7% of these clients offered CD4 count within 2 weeks of initiation after first clinic visit. Similar observation was made by Braun et al. 33 who concluded that between 1 and 4 weeks after seroconversion, there is intense viral replication and substantial decline in CD4 count. Even though CD4 count is no longer a requirement for starting ARVs, it is important for monitoring immune function.34,35,36
A comparable study suggests that low adherence to therapy and resistance to antiretroviral medications is one of the main hindrances to successful ART. 37 Retention in care is therefore of great importance towards eradicating HIV/AIDS in Africa and perhaps other countries confronted with the pandemic. According to the Centres for Disease Control and Prevention (CDC), 38 only 40% of HIV-positive individuals were retained in continuous ART globally, albeit poor retention in care for HIV infection has a negative impact on survival of PLHIV. 39
However, this study found that 90% of clients were retained in care which is an improvement over reported sentinel survey figures of 39%, 48% and 40% for 2016, 2017 and 2018 respectively.13,30 It is therefore imperative to encourage patients to use available internal resources to intensify outreach programmes which have proven to work towards promoting enrolment and retention in ART. 40 Likewise, a comparative study by Schafer et al. 41 demonstrated that to prevent immune deterioration, prolong life and decrease the risk of HIV transmission, all persons diagnosed with HIV infection should continually remain in care with sustained access to Highly Active Retroviral Therapy (HAART), prophylaxis care and other medical services. 42
In addition, even though viral load monitoring has been endorsed by the WHO as the gold standard for monitoring treatment, CD4 count is used to monitor and confirm treatment failure43,44in place of this gold standard. In this study, viral load testing appears to be a main challenge facing ART sites located in peri-urban and rural areas due to absence of equipment, comparable to studies conducted elsewhere on accessibility to ART services.45,46,47,48,49,50,51 Similarly, CD4 count reagents were also found to be in short supply across all facilities studied, partly due to the introduction of the treat-all policy which recommends that irrespective of CD4 count level, treatment should be initiated in order to ensure quick and immediate enrolment into ART care. 13 In light of this, national survey to include other sentinel facilities across the 16 regions of Ghana can be done to arrive at a more concrete conclusion.
Pill count, self-report and pharmacy records are the methods recommended by the national guidelines for measuring adherence. 30 From this study, it was found that, the most common method of adherence to ART services by care providers (mostly pharmacists) was pill counting. With this method, patients were informed to bring back all medications during every clinic visit so that total number of tablets remaining could be counted and recorded. By means of calculation and taking cognizance of the quantities of medications dispensed on previous visit, the care provider is able to determine level of adherence. This practice has equally been documented in other countries outside Ghana.48,49,50,51,52 Nevertheless, this method has tendencies of introducing bias since it does not take into account missed doses due to falls and deliberate stock piling at home by patients in order to paint a picture of adherence as alluded to by Giardini et al. 29 and Valencia et al. 53 in similar studies. Pill count however has proven beneficial for care providers in monitoring adherence because of constraints of delays in accessing viral load results on time.
Adherence to ARVs was found to be 88% while Cotrimoxazole was 73%, similar to findings in Mugavero et al.. 54 It is therefore assumed that with easy access to viral load testing at the periphery, total number of clients virally suppressed will easily be captured which is likely to be high.
Documentation of patients’ record was found to be a major challenge. Only 20% of changes in regimen according to Ghana’s ART guidelines 30 was recorded, suggesting a potential lack of communication or consultation with team members at every level of the health system. This low level of documentation has the potential to adversely affect continuity of care, patient adherence and development of HIV resistant strains.
The tendency of non-suppression of viral load is high in the study areas since only 26% of those tested had viral loads suppressed. This observation might stem from viral resistance, shortages, patient discomfort and side effects which must be properly documented. Previous studies have alluded to similar reasons for non-suppression of viral load in many African countries.55,56,57 If documentation is done properly, appropriate actions are taken such as enhanced adherence counselling for non-adherent clients. In cases of non-suppression of virus, Dolutegravir-based combination pack can be introduced as recommended by NACP. 30
Review of resource availability showed that, most medications were available with the exception of intermittent shortage of Cotrimoxazole and Fluconazole tablets for prophylaxis and management of opportunistic infections. This observation is consistent with findings by Assefa et al. 58 in a district hospital which revealed the need for availability of laboratory tests and medications for the treatment of opportunistic infections as components of care provision.
During shortage of Cotrimoxazole (usually supplied by the NACP through the Regional Medical Stores) facilities resort to the use of non-funded products which were mostly paid for by the client. It was found in this study that the situation was as a result of challenges associated with NHIS such as non-payment of claims for prophylaxis. Conversely, insured HIV clients were able to access the medication for treatment of opportunistic infections using their NHIS cards. Policy dialogue towards including ARVs in the exemption list of the NHIS will promote financial accessibility to ART services.
Contrary to studies by Kober and Van Damme 59 and Addo-Atuah et al 60 which found inadequate skilled healthcare providers and resources for initiating ART, this study found otherwise. Even though most resources were available, important components of care according to national treatment guidelines were not provided for a large number of patients similar to findings by Alemayehu et al. 61 who argued that availability of resources does not guarantee quality of care.
About 82% of healthcare providers were of the view that, if medicines are available all the time, care provision will improve as argued by Eaton et al. 2 This can however be true if patients adhere to treatment and caregivers also prescribe the right medication for the right patient. Likewise, access to viral load at the point of care was recommended by Garrett et al. 62 as a means of care improvement while Rice et al. 63 argued for good data systems to track HIV care.
Other recommendations by healthcare providers were evaluation of patients through e-tracker introduced by the Ghana Health Service (GHS); partnership with faith and herbal healers; strengthening supply chain; increasing retention in care; intensifying home visits; maintaining confidentiality of clients; home-based HIV services, and self-testing. Even though 50% of providers believed the UNAIDS 90-90-90 goal was appropriate, 88% thought the target could be achieved but not in 2020 due to challenges in quality of HIV services in the country. This conclusion by the health staff elucidates the critical role of service quality in attaining health system targets related to HIV. Studies on Ghana64,65and elsewhere6,66,67,68 have alluded this concern.
Limitations
First, it must be explicitly acknowledged that the huge gender imbalance in the study population is an important limitation and interpretation of the findings should be made cognizant of this gap which future studies are encouraged to address. Second, self-reported responses from clients on the process and outcome indicators of quality ART services pose potential subjectivity challenges since the researchers could not independently verify some of the information given by the respondents. Moreover, responses might have been influenced by the personal experiences of clients which perhaps did not necessarily reflect the complete picture of ART service in the study regions. Nonetheless, the combination of other objective measures of ART service quality minimized the potential effect of subjective responses from clients. Finally, the study was conducted in two out of 16 administrative regions of Ghana which also posed generalizability challenges. However, the geopolitical distribution the Volta and Oti regions are similar to the coastal, middle and northern belts of Ghana which favours some level of national representativeness.
Implications for research
First, researchers, policy makers and implementers should prioritize quality HIV services including universal access to ART services; additionally, there is need for enhanced political will towards committing more human and material resources to fight the HIV pandemic. Finally, point of care viral load assay should be considered as means of improving care alongside maximizing available essential human and material resources for HIV services, especially in deprived settings. Future researchers are encouraged to design more nationally representative studies that include larger sample size from other regions with more cosmopolitan features.
Conclusion
Overall, it was discovered that the main constraints to providing optimal quality ART services were lack of viral load machines, reagents for CD4 tests and lack of medications for the management of opportunistic infections (e.g. Fluconazole 200 mg). With regards to standards of care, level of viral load suppression was found to be low and majority un-determined coupled with the fact that conducting baseline tests before initiation of medications received little attention. Clients who were not actively insured with the NHIS did not also have financial access to ARVs which potentially induced dropped out and subsequently complications.
These field evidences predicted Ghana’s failure to achieve the 90-90-90 goal in 2020. The Ghana AIDS Commission (GAC) and NACP therefore need to embark on consistent review of policy guidelines, including the consolidated guidelines for HIV care in Ghana to address these challenges.
Health managers must learn to be dynamic and more sensitive to context specific healthcare quality challenges to prefer targeted interventions for such challenges. The Ghana AIDS Commission and related bodies must also demonstrate more innovation and broader stakeholder engagement to Even though this study was conducted in three ART sites in the Volta and Oti regions of Ghana, the results resonate with the general national picture. Policy makers and health managers are hence encouraged to learn lessons from these results.
Supplemental Material
Supplemental material, sj-pdf-1-smo-10.1177_20503121211036142 for Quality of antiretroviral therapy services in Ghana: Implications for the HIV response in resource-constrained settings by Robert Kaba Alhassan, Courage Edem Ketor, Anthony Ashinyo, Mary Eyram Ashinyo, Jerry John Nutor, Conrad Adjadeh and Emmanuel Sarkodie in SAGE Open Medicine
Supplemental material, sj-pdf-2-smo-10.1177_20503121211036142 for Quality of antiretroviral therapy services in Ghana: Implications for the HIV response in resource-constrained settings by Robert Kaba Alhassan, Courage Edem Ketor, Anthony Ashinyo, Mary Eyram Ashinyo, Jerry John Nutor, Conrad Adjadeh and Emmanuel Sarkodie in SAGE Open Medicine
Acknowledgments
The researchers acknowledge the support of the regional directors of health in the two selected regions. Also, the researchers also recognize the support of the National AIDS Control Programme (NACP) and Ghana AIDS Commission (GAC), respondents and frontline health staff at the various ART sites.
Footnotes
Author Contributions: RKA Analysed the data; Wrote the paper; Significant content peer-review; CEK Conceived and designed the experiments; Performed the experiments; Analysed the data; Contributed materials/analysis tools; Wrote the paper; Significant content peer-review; AS MA JJN ES CA Significant content peer-review.
Availability of data and materials: All relevant data are within the manuscript
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics approval: Written informed consent was obtained from all the adult participants in accordance with the Ghana Health Service Research Ethics Committee (ERC). Only participants who voluntarily consented to participate in writing were included in this study. The study was thus granted ethical approval by the Ghana Health Service (GHS) Ethical Review Committee (ERC) (clearance number: GHS-ERC009/08/19). Administrative approvals were also sought from the facility heads of the study sites. To promote anonymity of the study ART sites, pseudonyms were used and codes used in place of participants’ names to guarantee their privacy and confidentiality. Collated data was kept on a password protected computer and kept with the Principal Investigator.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Participation in the study was voluntary and were told to discontinue from the study anytime they so wish without consequences. Only participants who voluntarily signed the informed consent form were allowed to participate in the study. Written informed consent was obtained from all subjects. In the case of minors (persons below 18 years), written informed consent from legally authorized representatives (locus parentis) was obtained before they were included in the study. Please see Supplementary File 1 for Consent Forms for the various study respondents.
Trial registration: Not applicable because this study is not a clinical trial and did not require a trial registration.
ORCID iDs: Robert Kaba Alhassan  https://orcid.org/0000-0003-4227-4854
https://orcid.org/0000-0003-4227-4854
Jerry John Nutor  https://orcid.org/0000-0002-7562-6281
https://orcid.org/0000-0002-7562-6281
Emmanuel Sarkodie  https://orcid.org/0000-0002-1464-2472
https://orcid.org/0000-0002-1464-2472
Supplemental material: Supplemental material for this article is available online.
References
- 1. Donabedian A. Evaluating the quality of medical care. Milbank Quart 2005; 83(4): 691–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Eaton EF, Tamhane AR, Burkholder GA, et al. Unanticipated effects of new drug availability on antiretroviral durability: implications for comparative effectiveness research. Open Forum Infect Dis 2016; 3(2): ofw109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Alhassan RK, Nketiah-Amponsah E, Arhinful DK. Design and implementation of community engagement interventions towards healthcare quality improvement in Ghana: a methodological approach. Health Econ Rev 2016; 6(1): 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Alhassan RK, Nketiah-Amponsah E. Frontline staff motivation levels and health care quality in rural and urban primary health facilities: a baseline study in the Greater Accra and Western regions of Ghana. Health Econ Rev 2016; 6(1): 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Alhassan RK, Nketiah-Amponsah E, Spieker N, et al. Assessing the impact of community engagement interventions on health worker motivation and experiences with clients in primary health facilities in Ghana: a randomized cluster trial. PLoS ONE 2016; 11(7): e0158541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Alhassan RK, Nketiah-Amponsah E, Akazili J, et al. Efficiency of private and public primary health facilities accredited by the National Health Insurance Authority in Ghana. Cost Eff Resour Alloc 2015; 13: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Alhassan RK, Nketiah-Amponsah E, Spieker N, et al. Effect of community engagement interventions on patient safety and risk reduction efforts in primary health facilities: evidence from Ghana. PLoS ONE 2015; 10(11): e0142389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Alhassan RK, Duku SO, Janssens W, et al. Comparison of perceived and technical healthcare quality in primary health facilities: implications for a sustainable National Health Insurance Scheme in Ghana. PLoS ONE 2015; 10(10): e0140109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Alhassan RK, Spieker N, van Ostenberg P, et al. Association between health worker motivation and healthcare quality efforts in Ghana. Human Resour Health 2013; 11(1): 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ministry of Health (MoH). 2017 HIV Sentinel Survey Report. Guidelines for Antiretroviral Therapy in Ghana. 6th ed. Accra Ghana: Ministry of Health, 2018. [Google Scholar]
- 11. Ghana AIDS Commission (GAC). National and sub-national HIV and AIDS estimates and projections, 2017, http://www.ghanahealthservice.org/ghs-subcategory.php?cid=2&scid=43 (accessed 18 May 2021).
- 12. World Health Organization and UNAIDS. Guidelines on co-trimoxazole prophylaxis for HIV-related infections among children, adolescents and adults. Recommendations for a public health approach. Geneva: WHO, 2006. [Google Scholar]
- 13. National AIDS Control Programme (NACP); Ghana Health Service (GHS). Guideline for Antiretroviral Therapy in Ghana. Accra, Ghana: Ghana Health Service, 2019. [Google Scholar]
- 14. Tun W, Okal J, Schenk K, et al. Limited accessibility to HIV services for persons with disabilities living with HIV in Ghana Uganda and Zambia. J Int AIDS Soc 2016; 19(5 Suppl. 4): 20829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Addo SA, Abdulai M, Yawson A, et al. Availability of HIV services along the continuum of HIV testing, care and treatment in Ghana. BMC Health Serv Res 2018; 18(1): 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Anchalia MM, D'Ambruoso L. Seeking solutions: scaling-up audit as a quality improvement tool for infection control in Gujarat India. Int J Qual Health Care 2011; 23(4): 464–470. [DOI] [PubMed] [Google Scholar]
- 17. Minior T, Douglas M, Edgil D, et al. The critical role of supply chains in preventing human immunodeficiency virus drug resistance in low-and middle-income settings. J Infect Dis 2017; 216(9): S812–S815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Seeberger UG, Valadez JJ. Are health workers reduced to being drug dispensers of antiretroviral treatment? A randomized cross-sectional assessment of the quality of health care for HIV patients in northern Uganda. Health Policy Plan 2019; 34(8): 559–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ahonkhai AA, Bassett IV, Ferris TG, et al. Improving HIV outcomes in resource-limited countries: the importance of quality indicators. BMC Health Serv Res 2012; 12(1): 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Burua A, Nuwaha F, Waiswa P. Adherence to standards of quality HIV/AIDS care and antiretroviral therapy in the West Nile Region of Uganda. BMC Health Serv Res 2014; 14(1): 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Adjetey V, Obiri-Yeboah D, Dornoo B. Differentiated service delivery: a qualitative study of people living with HIV and accessing care in a tertiary facility in Ghana. BMC Health Serv Res 2019; 19(1): 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Barker C, Dutta A, Klein K. Can differentiated care models solve the crisis in HIV treatment financing? Analysis of prospects for 38 countries in sub-Saharan Africa. J Int AIDS Society 2017; 20(Suppl. 4): 216–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. American Public Health Association. Adherence to HIV Treatment Regimens: Recommendations for Best Practices. Washington DC: American Public Health Association, 2004, www.apha.org/ppp/hiv (accessed 18 May 2021). [Google Scholar]
- 24. Kukoyi O, Renner L, Powell J, et al. Viral load monitoring and antiretroviral treatment outcomes in a pediatric HIV cohort in Ghana. BMC Infect Dis 2015; 16(1): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Doubova SV, García-Saisó S, Pérez-Cuevas R, et al. Barriers and opportunities to improve the foundations for high-quality healthcare in the Mexican Health System. Health Policy Plan 2018; 33(10): 1073–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Worthen BR, Sanders JR, Fitzpatrick JL. Educational evaluation: Alternative approaches and practical guidelines. 3rd ed. Boston, MA: Allyn & Bacon, 2004. [Google Scholar]
- 27. Ghana Statistical Service (GSS). 2010 population & housing census: summary report of final results. Accra, 2010, https://statsghana.gov.gh/gssmain/fileUpload/pressrelease/2010_PHC_National_Analytical_Report.pdf (accessed 18 May 2021). [Google Scholar]
- 28. Olowookere SA, Fawole OI, Adekanle DA, et al. Patterns and correlates of intimate partner violence to women living with HIV in Osogbo Southwest Nigeria. Violence against Women 2015; 21(11): 1330–1340. [DOI] [PubMed] [Google Scholar]
- 29. Giardini A, Martin MT, Cahir C, et al. Toward appropriate criteria in medication adherence assessment in older persons: position paper. Aging Clin Exp Res 2016; 28(3): 371–381. [DOI] [PubMed] [Google Scholar]
- 30. National AIDS Control Programme (NACP); Ghana Health Service (GHS). Consolidated Guidelines for HIV Care in Ghana: Test Treat and Track. Accra, Ghana: Ghana Health Service, 2019. [Google Scholar]
- 31. Insight Start Study Group . Initiation of antiretroviral therapy in early asymptomatic HIV infection. New Engl J Med 2015; 373(9): 795–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Temprano ANRS Study Group . A trial of early antiretrovirals and isoniazid preventive therapy in Africa. New Engl J Med 2015; 373(9): 808–822. [DOI] [PubMed] [Google Scholar]
- 33. Braun DL, Kouyos RD, Balmer B, et al. Frequency and spectrum of unexpected clinical manifestations of primary HIV-1 infection. Clin Infect Dis 2015; 61(6): 1013–1021. [DOI] [PubMed] [Google Scholar]
- 34. Ford N, Meintjes G, Pozniak A, et al. The future role of CD4 cell count for monitoring antiretroviral therapy. Lancet Infect Dis 2015; 15(2): 241–247. [DOI] [PubMed] [Google Scholar]
- 35. Mwesigire DM, Martin F, Seeley J, et al. Relationship between CD4 count and quality of life over time among HIV patients in Uganda: a cohort study. Health Qual Life Outcome 2015; 13(1): 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rodriguez WR, Christodoulides N, Floriano PN, et al. A microchip CD4 counting method for HIV monitoring in resource-poor settings. PLoS Med 2005; 2(7): e182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Gardner EM, McLees MP, Steiner JF, et al. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis 2011; 52(6): 793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Centres for Disease Control Prevention (CDC). Centers for disease control and prevention. Vital signs: HIV diagnosis, care, and treatment among persons living with HIV–united States, 2011. MMWR Morbid Mortal Weekly Rep 2011; 63(47): 1113–1117. [PMC free article] [PubMed] [Google Scholar]
- 39. Giordano TP, Gifford AL, White AC, Jr, et al. Retention in care: a challenge to survival with HIV infection. Clin Infect Dis 2007; 44(11): 1493–1499. [DOI] [PubMed] [Google Scholar]
- 40. Thompson MA, Mugavero MJ, Amico KR, et al. Guidelines for improving entry into and retention in care and antiretroviral adherence for persons with HIV: evidence-based recommendations from an international association of physicians in AIDS care panel. Ann Intern Med 2012; 156(11): 817–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Schafer JJ, Gill TK, Sherman EM, et al. ASHP guidelines on pharmacist involvement in HIV care. Am J Health-Syst Pharm 2016; 73(7): 468–494. [DOI] [PubMed] [Google Scholar]
- 42. Cabana MD, Jee SH. Does continuity of care improve patient outcomes? J Family Practice 2004; 53(12): 974–980. [PubMed] [Google Scholar]
- 43. World Health Organization (WHO). World Health Organization: standards for quality HIV care: a tool for quality assessment improvement and accreditation. Geneva: World Health Organization, 2004, https://www.who.int/hiv/pub/prev_care/en/standardsquality.pdf?ua=1 (accessed 18 May 2021) [Google Scholar]
- 44. World Health Organization (WHO). Guidelines guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV. World Health Organization, 2015, https://www.who.int/hiv/pub/guidelines/earlyrelease-arv/en/#:~:text=First%2C%20antiretroviral%20therapy%20(ART),part%20of%20combination%20prevention%20approaches (accessed 18 May 2021). [PubMed]
- 45. Moyo S, Gaseitsiwe S, Mohammed T, et al. Cross-sectional estimates revealed high HIV incidence in Botswana rural communities in the era of successful ART scale-up in 2013-2015. PLoS ONE 2018; 13(10): e0204840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Le Roux KW, Davis EC, Gaunt CB, et al. A case study of an effective and sustainable antiretroviral therapy program in rural South Africa. AIDS Patient Care STDS 2019; 33(11): 466–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Gomez GB, Venter WDF, Lange JMA, et al. North-South corridor demonstration project: ethical and logistical challenges in the design of a demonstration study of early antiretroviral treatment for long distance truck drivers along a transport corridor through South Africa Zimbabwe, and Zambia. Adv Prev Med 2013; 2013: 190190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Pfeiffer J, Montoya P, Baptista AJ, et al. Integration of HIV/AIDS services into African primary health care: lessons learned for health system strengthening in Mozambique-a case study. J Intern AIDS Soc 2010; 13(1): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Kalichman SC, Amaral CM, Stearns H, et al. Adherence to antiretroviral therapy assessed by unannounced pill counts conducted by telephone. J Gen Intern Med 2007; 22(7): 1003–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Bangsberg DR, Hecht FM, Clague H, et al. Provider assessment of adherence to HIV antiretroviral therapy. Jaids-hagerstown MD- 2001; 26(5): 435–442. [DOI] [PubMed] [Google Scholar]
- 51. Berg KM, Arnsten JH. Practical and conceptual challenges in measuring antiretroviral adherence. J Acquir Immune Defic Syndr 2006; 43(Suppl. 1): S79–S87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Biressaw S, Abegaz WE, Abebe M, et al. Adherence to Antiretroviral Therapy and associated factors among HIV infected children in Ethiopia: unannounced home-based pill count versus caregivers’ report. BMC Pediatrics 2013; 13(1): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Valencia S, León M, Losada I, et al. How do we measure adherence to anti-tuberculosis treatment. Expert Rev Anti Infect Ther 2017; 15(2): 157–165. [DOI] [PubMed] [Google Scholar]
- 54. Mugavero M, Ostermann J, Whetten K, et al. Barriers to antiretroviral adherence: the importance of depression, abuse, and other traumatic events. AIDS Patient Care STDS 2006; 20(6): 418–428. [DOI] [PubMed] [Google Scholar]
- 55. Myers B, Lombard C, Joska JA, et al. Associations between patterns of alcohol use and viral load suppression amongst women living with HIV in South Africa. AIDS Behav 2021; 19: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Bulage L, Ssewanyana I, Nankabirwa V, et al. Factors associated with virological non-suppression among HIV-positive patients on antiretroviral therapy in Uganda August 2014–July 2015. BMC Infect Dis 2017; 17(1): 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Filiatreau LM, Pettifor A, Edwards JK, et al. Associations Between Key Psychosocial Stressors and Viral Suppression and Retention in Care Among Youth with HIV in Rural South Africa. AIDS Behav 2021; 25(8): 2358–2368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Assefa Y, Alebachew A, Lera M, et al. Scaling up antiretroviral treatment and improving patient retention in care: lessons from Ethiopia, 2005-2013. Global Health 2014; 10(1): 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Kober K, Van Damme W. Scaling up access to antiretroviral treatment in Southern Africa: who will do the job? Lancet 2004; 364(9428): 103–107. [DOI] [PubMed] [Google Scholar]
- 60. Addo-Atuah J, Gourley D, Gourley G, et al. Accessibility of antiretroviral therapy in Ghana: convenience of access. SAHARA J 2012; 9(2): 74–87. [DOI] [PubMed] [Google Scholar]
- 61. Alemayehu YK, Bushen OY, Muluneh AT. Evaluation of HIV/AIDS clinical care quality: the case of a referral hospital in North West Ethiopia. Int J Qual Health Care 2009; 21(5): 356–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Garrett NJ, Drain P, Werner L, et al. Diagnostic accuracy of the point-of-care Xpert® HIV-1 viral load assay in a South African HIV clinic. J Acquired Immun Defic Syndrom 2016; 72(2): e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Rice B, Boulle A, Baral S, et al. Strengthening routine data systems to track the HIV epidemic and guide the response in sub-Saharan Africa. JMIR Public Health Surv 2018; 4(2): e36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Amankwah AK. Facilitators and barriers to antiretroviral therapy adherence among HIV AIDS patients: a multi-case study of Sunyani regional and municipality. Master of Philosophy in Health Management, University of Ghana, 2015, http://197.255.68.203/handle/123456789/8158 (accessed 18 May 2021). [Google Scholar]
- 65. Dapaah JM. HIV/AIDS treatment in two Ghanaian hospitals: experiences of patients, nurses and doctors. Leiden: African Studies Centre, 2012, https://hdl.handle.net/1887/18624 (accessed 18 May 2021).
- 66. Kyayise A, Kyeyagalire R, Livesley N, et al. Private-for-profit HIV/AIDS care in Uganda: an assessment. Technical Report, USAID Health Care Improvement Project. Chevy Chase, MD: University Research Co, 2008. [Google Scholar]
- 67. Nigatu D, Dinegde NG, Sendo EG. Cotrimoxazole prophylaxis treatment adherence and associated factors among human immunodeficiency virus (HIV) exposed children in public hospitals in Ilubabor Zone Southwest Ethiopia, 2018. Open Public Health J 2019; 12(1): 184–198. [Google Scholar]
- 68. Okwera A, Mafigiri DK, Guwatudde D, et al. Level of understanding of co-trimoxazole use among HIV infected, recurrent pulmonary tuberculosis suspects at a national referral tuberculosis clinic in Kampala Uganda: a qualitative analysis. Afr Health Sci 2015; 15(1): 49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-smo-10.1177_20503121211036142 for Quality of antiretroviral therapy services in Ghana: Implications for the HIV response in resource-constrained settings by Robert Kaba Alhassan, Courage Edem Ketor, Anthony Ashinyo, Mary Eyram Ashinyo, Jerry John Nutor, Conrad Adjadeh and Emmanuel Sarkodie in SAGE Open Medicine
Supplemental material, sj-pdf-2-smo-10.1177_20503121211036142 for Quality of antiretroviral therapy services in Ghana: Implications for the HIV response in resource-constrained settings by Robert Kaba Alhassan, Courage Edem Ketor, Anthony Ashinyo, Mary Eyram Ashinyo, Jerry John Nutor, Conrad Adjadeh and Emmanuel Sarkodie in SAGE Open Medicine