Abstract
Access to remote appointments (RA) by telephone or video is increasing as technology advances and becomes more available to patients. This meta-analysis of randomized controlled trials (RCTs) aims to discover whether surgical patients are satisfied with RAs when compared with conventional outpatient clinics (OPC). A literature search of RCTs of surgical patient satisfaction of RAs versus OPC appointments was performed. The PubMed, EMBASE, OVID, Cochrane Library, and Google Scholar databases were searched to include articles from January 2000 to 2020. A random-effects meta-analysis model was used to compare outcomes. All 7 RCTs showed that patients were as satisfied with RAs as OPC appointments (RR = 1.00, [0.98-1.02]; P = .73). Furthermore, both patient cohorts would prefer RAs for future follow-up (RR = 2.29, [1.96-2.97]; P < .00001). One RCT found the cost to institutions was less in the RA group ($19.05 vs $52.76) and another found the patients would save $9.96 on transportation costs. The majority of RCTs suggested cost to patients and or institutions would be less for RA. In conclusion, surgical patients are satisfied with RAs and in fact would prefer them.
Keywords: general surgery, patient satisfaction, remote consultations, meta-analysis, randomized controlled trials, health information technology, outpatient satisfaction, telemedicine, technology
Introduction
The outpatient clinic (OPC) has long been a standard part of routine follow-up for surgical patients. However, there is increasing demand for surgical outpatient appointments due to a rise in new referrals from primary care (1). In order to cope with this demand, there has been a move toward modernization through remote appointments (RA). Access to RA by telephone or video is increasing worldwide as technology advances and becomes more accessible to patients and secondary care facilities, with a particular surge at the onset of the Covid-19 pandemic (2). This type of appointment may be helpful to patients who live remotely or who have limited mobility and struggle to attend appointments (3 –5). Conventional OPCs are a burden for those patients who have to travel long distances or arrange childcare or time off work to attend. There has therefore been a recent move to increase the use of RAs in the surgical outpatient setting in order to improve access for rural patients and to decrease the footfall in hospitals in light of the Covid-19 pandemic (4,6).
Although there seem to be some immediately apparent advantages to RA, there are also some hesitations with this type of appointment. Traditionally, health care professionals are trained to communicate face to face in a clinic setting and RA are likely to require different communication skills that will need to be learned. Additionally, patients won’t be able to be examined. It may not be possible for all patients to use the technology required and of course issues such as loss of connection or time delays.
The aim of this review is to explore the existing evidence comparing patient satisfaction with RA and conventional OPC. According to an extensive literature search, this is the first meta-analysis of randomized controlled trials (RCTs) that aims to review the existing evidence on RAs in comparison to conventional OPC appointments and aims to discover whether surgical patients are satisfied with RAs and to explore other advantages to this form of consultation.
Methods
A literature search for RCTs comparing surgical RA clinics versus conventional OPC consultations was performed. We included the 10 surgical specialties as defined by the Royal College of Surgeons of the United Kingdom and Ireland and gynecology (7). The PubMed, EMBASE, OVID, Cochrane Library, and Google Scholar databases were searched to include articles from the year 2000 to 2020. Search terms included telephone, virtual, telemedicine, surgical, outpatient, patient satisfaction, and RCTs in exploded and linked combinations. Full search terms are included in Appendix A. Our meta-analysis of RCTs was carried out following guidelines of Preferred Reporting Items for Systematic Reviews and Meta-analysis (8). To ensure complete capture of trials, the reference and citation lists of initial trials were trawled following the initial search.
Study Selection
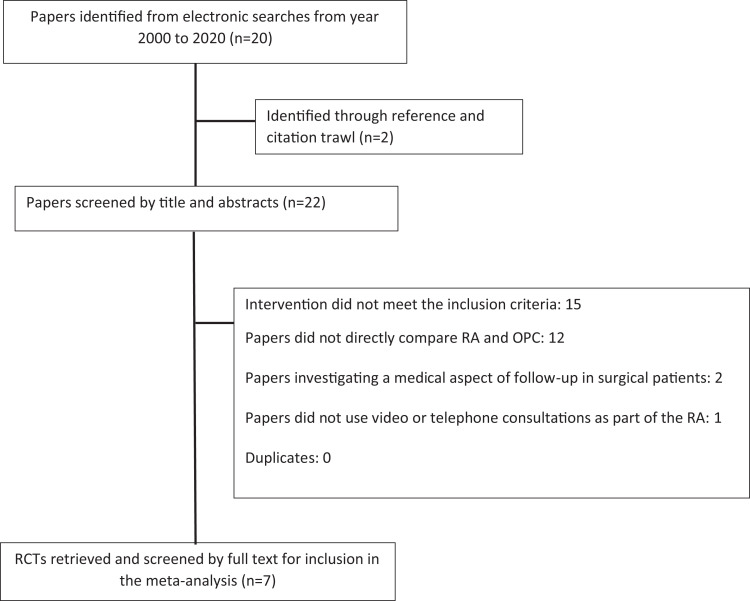
The literature search and exclusion were carried out by 3 independent authors. The study selection can be seen in Figure 1. Once identified the RCTs were then analyzed using the Revised Cochrane risk-of-bias tool for randomized trials ROB-2 to assess for bias as shown in Appendix B (9). Overall, all trials had a moderate to low risk of bias. The data were extracted independently by 2 authors. If there were any discrepancies with the collected data, the data point was independently verified by all authors. In all instances, this resulted in consensus agreement of the collected data point. This process negated any data collection errors.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) diagram detailing the process of study selection.
Inclusion Criteria
RCTs
Patients of any surgical speciality
Follow-up patients
Comparison of RAs by telephone or video versus conventional OPC
Exclusion Criteria
Non-English language papers
Medical and other nonsurgical specialty clinics
Nonrandomised studies
Follow-up via other forms of technology such as software applications
Data Collection
The primary outcome measure was patient satisfaction. Secondary outcome measures included patient preference for future follow-up and cost to both patient and institutions. This data was extracted from each RCT.
Statistical Analysis
Review Manager (RevMan version 5.4.1) software was used to analyze the data. A random-effects meta-analysis model was used. Data is expressed in the form of a risk ratio. The heterogeneity of the data was investigated and quantified by I 2 tests.
Results
A total of 22 studies were identified by the initial search. Of these, 7 articles met the inclusion criteria and looked at our primary outcome of patient satisfaction. Characteristics of the included studies are detailed in Table 1. Excluded studies were analyzed for comment on the secondary outcomes of patient preference for future follow-up, and also costs to institutions and patients. The characteristics of these studies are also shown in Table 1.
Table 1.
Characteristics of Included RCTs for Patient Satisfaction, Patient Preference for Future Follow-Up, and/or Costs.
| Study | Country | Surgical subtype | Type of RA | RA group (n) | Conventional group (n) | Methods of quantifying satisfaction | Secondary outcome |
|---|---|---|---|---|---|---|---|
| Sathiyakumar et al (10) | United States | Orthopedics | Video | 7 | 9 | Likert scale style question on satisfaction | Follow-up and cost (patient) |
| Viers et al (11) | United States | Urology | Video | 28 | 27 | Likert scale style question on satisfaction | Follow-up and cost (patient) |
| Healy et al (12) | Ireland | General surgery | Telephone | 81 | 61 | Likert scale style question on satisfaction | Follow-up and cost (patient) |
| Buvik et al (13) | Norway | Orthopedics | Video | 196 | 185 | Selected questions from the Norwegian OutPatient Experiences Questionnaire | Cost (institution and patient) |
| Thompson et al (14) | United States | Gynecology | Telephone | 50 | 50 | S-CAHPS Questionnaire | |
| Augestad et al (15) | Norway | General surgery | Video | 52 | 58 | Norwegian OutPatient Experiences Questionnaire (OPEQ) | Follow-up and cost (patient) |
| Kane et al (16) | United States | Orthopedics | Video | 28 | 30 | Selected Questionnaire on satisfaction via online form on REDCap | Follow-up and cost (institution and patient) |
| Studies below are included in analysis of secondary outcomes only | |||||||
| Ma et al (17) | Australia | General surgery | Telephone | 66 | 79 | NA | Follow-up and cost (institution) |
| Cremades et al (18) | Spain | General surgery | Video | 74 | 90 | NA | Cost (institution) |
| Westra and Niessen (19) | The Netherlands | Plastic surgery | Video | 16 | 15 | NA | Cost (institution and patient) |
Abbreviations: RA, remote appointments; RCT, randomized controlled trial.
Seven RCTs were identified which assessed if patients were satisfied with RA rather than OPC, these were from 3 countries and included 1087 patients. This meta-analysis demonstrates that patients were equally satisfied with RAs compared to conventional OPC appointments (RR = 1, 95% CI = 0.98-1.02, P = .73) as demonstrated in Figure 2. There was no heterogenicity in this analysis (I 2 = 0%).
Figure 2.
Forest plot comparing rates of satisfaction in patients who had remote appointments (RA) versus outpatient clinic (OPC) follow-up.
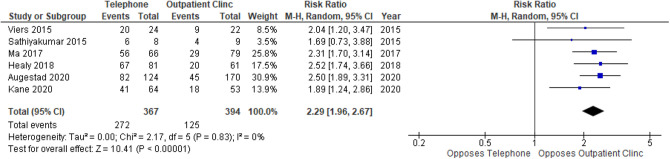
Six RCTs comprising of 761 patients were used to assess whether patients would prefer RA in preference to OPC in the future. This meta-analysis demonstrates that both groups of patients have clearly stated their preference for RAs for future follow-up as shown in Figure 3 (RR = 2.29, 95% CI = 1.96-2.67, P < .00001). There is no observed heterogeneity in the data (I 2 = 0%).
Figure 3.
Forest plot comparing if patients would select the same type of follow-up again.
One RCT performed a cost analysis and found that the cost to institutions was less in the RA group ($19.05 vs $52.76) (17). This was calculated by looking at the costs of staff salary, room hire, telephone call costs, and also factored in the did not attend rate in both RAs and standard OPC. This RCT did not assess patient satisfaction. Five further RCTs that did not perform a formal cost analysis suggested that RAs would cost less to the institutions (13,15,16,18,19). These papers proposed that costs would be reduced through the need for less clinic room space; fewer administrative and nursing staff on the day of clinic; less cleaning of rooms and also a reduction in the cost by decreasing the need for patient transport services. Seven RCTs also suggested that costs to patients are less in the RA group in terms of loss of earnings from time taken off work, time taken to travel, and or costs of travel and parking (10 –13,15,16,19). Although no formal cost analysis was performed one RCT proposed that patients would save $9.96 on transportation costs alone (16).
Discussion
This is the first comparative meta-analysis for the use of RAs in place of conventional OPC appointments for surgical patients. Although from a limited number of RCTs, data from our analysis of 7 RCTs suggests that the majority of patients were satisfied with receiving routine follow-up surgical care by RA rather than an OPC review. These results are demonstrated in the forest plot in Figure 2. The forest plot in Figure 3 demonstrates that patients from both cohorts would prefer RA in the future. This is in line with other studies (20,21). Of the 6 studies, only the study by Sathiyakumar et al failed to demonstrate a preference for RA. This is likely due to the small sample sized used in this study. It is possible that patients didn’t have a preference for follow-up either through RA or conventional OPC if they had no prior experience; however, once they had, their preference swayed in favor of RA.
The cost to patient and institutions was found to be lower in the RA group in all the RCTs that looked at this as an outcome; however, not all RCTs had performed a formal cost analysis and had simply suggested costs would be lower citing a number of reasons including lower staffing costs, less need for patient transport, and decreased costs of travel, parking, and time off work for patients. This again needs to be treated with caution as there may well be hidden costs—namely set-up of RAs that may become apparent when a formal cost analysis is conducted.
In this study, we have taken considerable steps to reduce selection and publication bias by identifying all relevant published RCTs. There are few studies comparing the methods of surgical follow-up, this is the first meta-analysis to specifically address the acceptability and patient satisfaction outcomes of RAs in place of conventional OPC. Although results appear positively in favor of RAs, we have identified some limitations with our analysis. There is a paucity of information about this subject due to the small number of studies looking at RA in comparison to conventional OPC. There is a low to moderate risk of bias across the included studies. The studies were small, and the method of measuring patient satisfaction is variable, though no heterogeneity of data was detected in the meta-analysis. Additionally, long-term follow-up data is not captured. There is therefore a need for good quality prospective and comparative evaluations of RAs versus conventional OPC appointments in surgical patient’s care, which seek to collect information on all aspects of such care. There is no indication from the published studies that RA surgical follow-up has an impact on the frequency of adverse events, though this needs to be confirmed in future research as does exploration in to surgeon satisfaction with this approach. This meta-analysis does not include studies with a formal comparison in the complexity of consultations between both groups but provides insights into patients’ future preference of a mode of consultation and satisfaction with RA. The study has not specifically looked at different patient groups, and therefore, the results should be applied generally to the outpatient setting but may not be applicable in certain patient groups, for example, those with hearing difficulties, learning difficulties, or patients where language barriers are an issue.
All of the studies included in this analysis were concluded prior to the Covid-19 pandemic, however during the pandemic, the use of RAs in surgical clinics increased worldwide (22,23). The Royal College of Surgeons of England advised the use of RAs in order to try and reduce the backlog of patients awaiting OPC appointments as part of its adaptation of surgical services and in doing so reduce the footfall in hospitals (24 –26). Given that the majority of patients in the analysis were found to prefer RAs it is highly likely that even more patients would be supportive of RAs during and following the pandemic.
Conclusion
In a health care environment of increasing cost, demand, and a need for greater efficiency, it is important that we look at the research of this nature to see whether RAs are fit for purpose. This meta-analysis has shown that surgical patients are satisfied with RAs and in fact may prefer them to conventional face-to-face appointments. As a welcome bonus RAs provisionally cost less for the patients and institutions. Further prospective research is needed to ensure the safety of such appointments and confirm patient (and surgeon) satisfaction. In addition, a formal cost analysis needs to be performed to see what the impact on costs to patients and institutions is.
Appendix A
Search terms used to identify studies
Telephone
Virtual
Telemedicine
Surgical
Outpatient
Clinic
Standard
Conventional
Face-to-face
Patient satisfaction
RCT
Appendix B
Table A1.
RCT Risk of Bias Table (as per Revised Cochrane Risk-of-Bias Tool for Randomized Trials [RoB 2]).
| Domain 1: Risk of bias arising from the randomization process | Domain 2: Risk of bias due to deviations from the intended interventions | Domain 3: Missing outcome data | Domain 4: Risk of bias in measurement of the outcome | Domain 5: Risk of bias in selection of the reported result | Overall risk of bias | |
|---|---|---|---|---|---|---|
| Sathiyakumar et al | Low | Low | Low | Low | Low | Low |
| Viers et al | Some concerns | Low | Low | Low | Low | Low |
| Healy et al | Low | Low | Low | Some concerns | Low | Low |
| Buvik et al | Low | Low | Low | Low | Low | Low |
| Thompson et al | Low | Low | Low | Some concerns | Low | Low |
| Augestad et al | Low | Low | Low | Low | Low | Low |
| Kane et al | Low | Low | Low | Some concerns | Low | Low |
| Ma et al | Low/some concerns | Low | Some concerns | Some concerns | Low | Low |
| Cremades et al | Some concerns | Low | Low | Low | Low | Low |
| Westra and Niessen | Some concerns | Low | Some concerns | Low | Low | Low |
Abbreviation: RCT, randomized controlled trial.
Footnotes
Authors’ Note: This article is a systematic review and meta-analysis of previously published patient data it therefore does not contain any primary data from human (or animal) subjects. Informed consent for patient information to be published in this article was not obtained because this article is a systematic review and meta-analysis of previously published data and does not contain any primary data from human subjects.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Emily V Oates, MBChB, BMSc, MSC, MRCS  https://orcid.org/0000-0002-8021-0539
https://orcid.org/0000-0002-8021-0539
References
- 1. Elective Care Transformation Programme. Transforming Elective Care Services: General Surgery. NHS England; 2019. [Google Scholar]
- 2. Blandford A, Wesson J, Amalberti R, AlHazme R, Allwihan R. Opportunities and challenges for telehealth within, and beyond, a pandemic. Lancet Glob Health. 2020;8:e1364–5. doi:10.1016/S2214-109X(20)30362-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Miller GG, Levesque K. Telehealth provides effective pediatric surgery care to remote locations. J Pediatr Surg. 2002;37:752–4. doi:10.1053/jpsu.2002.32270 [DOI] [PubMed] [Google Scholar]
- 4. Zanaboni P, Scalvini S, Bernocchi P, Borghi G, Tridico C, Masella C. Teleconsultation service to improve healthcare in rural areas: acceptance, organizational impact and appropriateness. BMC Health Serv Res. 2009;9:238. doi:10.1186/1472-6963-9-238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chrapah S, Becevic M, Washington KT, Sheets LR, Wallach E, Chitima R, et al. Patient and provider satisfaction with pediatric urology telemedicine clinic. J Patient Exp. 2021;8:1–6. doi:10.1177/2374373520975734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. National Health Service. NHS England. Using the NHS and other health services during coronavirus. 2020. Updated December 7, 2020. Accessed December 12, 2020. https://www.nhs.uk/conditions/coronavirus-covid-19/using-the-nhs-and-other-health-services/
- 7. The Joint Committee on Surgical Training. About us. 2021. Updated February 3, 2021. Accessed May 1, 2021. https://www.jcst.org/about-us/
- 8. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6. doi:10.1371/journal.pmed.1000097 [PMC free article] [PubMed] [Google Scholar]
- 9. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366. doi:10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 10. Sathiyakumar V, Apfeld JC, Obremskey WT, Thakore RV, Sethi MK. Prospective randomized controlled trial using telemedicine for follow-ups in an orthopedic trauma population: a pilot study. J Orthop Trauma. 2015;29:e139–45. doi:10.1097/BOT.0000000000000189 [DOI] [PubMed] [Google Scholar]
- 11. Viers BR, Lightner DJ, Rivera ME, Tollefson MK, Boorjian SA, Karnes RJ, et al. Efficiency, satisfaction, and costs for remote video visits following radical prostatectomy: a randomized controlled trial. Eur Urol. 2015;68:729–35. doi:10.1016/j.eururo.2015.04.002 [DOI] [PubMed] [Google Scholar]
- 12. Healy P, McCrone L, Tully R, Flannery E, Flynn A, Cahir C, et al. Virtual outpatient clinic as an alternative to an actual clinic visit after surgical discharge: a randomised controlled trial. BMJ Qual Saf. 2019;28:24–31. doi:10.1136/bmjqs-2018-008171 [DOI] [PubMed] [Google Scholar]
- 13. Buvik A, Bugge E, Knutsen G, Småbrekke A, Wilsgaard T. Patient reported outcomes with remote orthopaedic consultations by telemedicine: a randomised controlled trial. J Telemed Telecare. 2019;25:451–9. doi:10.1177/1357633X18783921 [DOI] [PubMed] [Google Scholar]
- 14. Thompson JC, Cichowski SB, Rogers RG, Qeadan F, Zambrano J, Wenzl C, et al. Outpatient visits versus telephone interviews for postoperative care: a randomized controlled trial. Int Urogynecol J. 2019;30:1639–46. doi:10.1007/s00192-019-03895-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Augestad KM, Sneve AM, Lindsetmo RO. Telemedicine in postoperative follow-up of STOMa PAtients: a randomized clinical trial (the STOMPA trial). Br J Surg. 2020;107:509–18. doi:10.1002/bjs.11491 [DOI] [PubMed] [Google Scholar]
- 16. Kane LT, Thakar O, Jamgochian G, Lazarus MD, Abboud JA, Namdari S, et al. The role of telehealth as a platform for postoperative visits following rotator cuff repair: a prospective, randomized controlled trial. J Shoulder Elbow Surg. 2020;29:775–83. doi:10.1016/j.jse.2019.12.004 [DOI] [PubMed] [Google Scholar]
- 17. Ma Y, Jones G, Tay YK, Hunter T, Holden D, Rodgers-Wilson S, et al. Post-operative telephone review is safe and effective: prospective study—Monash outpatient review by phone trial. ANZ J Surg. 2018;88:434–9. doi:10.1111/ans.14280 [DOI] [PubMed] [Google Scholar]
- 18. Cremades M, Ferret G, Parés D, Navinés J, Espin F, Pardo F, et al. Telemedicine to follow patients in a general surgery department. a randomized controlled trial. Am J Surg. 2020;219:882–7. doi:10.1016/j.amjsurg.2020.03.023 [DOI] [PubMed] [Google Scholar]
- 19. Westra I, Niessen FB. Implementing real-time video consultation in plastic surgery. Aesthetic Plast Surg. 2015;39:783–90. doi:10.1007/s00266-015-0526-4 [DOI] [PubMed] [Google Scholar]
- 20. Barsom EZ, van Dalen ASHM, Bluss van Oud-Alblas M, et al. Comparing video consultation and telephone consultation at the outpatient clinic of a tertiary referral centre: patient and provider benefits. BMJ Innovations 2021;7:95–102. [Google Scholar]
- 21. Welch BM, Harvey J, O’Connell NS, McElligott JT. Patient preferences for direct-to-consumer telemedicine services: a nationwide survey. BMC Health Serv Res. 2017;17:784. doi:10.1186/s12913-017-2744-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hollander JE, Carr BG. Virtually perfect? telemedicine for covid-19. N Engl J Med. 2020;382:1679–81. doi:10.1056/NEJMp2003539 [DOI] [PubMed] [Google Scholar]
- 23. Greenhalgh T, Wherton J, Shaw S, Morrison C. Video consultations for covid-19. BMJ. 2020; 368. doi:10.1136/bmj.m998 [DOI] [PubMed] [Google Scholar]
- 24. Griffin S. Covid-19: waiting times in England reach record highs. BMJ. 2020; 370. doi:10.1136/bmj.m3557 [DOI] [PubMed] [Google Scholar]
- 25. National Health Service. NHS roadmap to safely bring back routine operations. Updated May 14, 2020. Accessed December 12, 2020. https://www.england.nhs.uk/2020/05/nhs-roadmap/
- 26. Royal College of Surgeons of England. COVID-19: good practice for surgeons and surgical teams. Updated April 3, 2020. Accessed December 12, 2020. https://www.rcseng.ac.uk/standards-and-research/standards-and-guidance/good-practice-guides/coronavirus/covid-19-good-practice-for-surgeons-and-surgical-teams/