Abstract
Kikuchi–Fujimoto disease (KFD), also known as histiocytic necrotizing lymphadenitis, is a benign, self-limiting inflammatory disorder of unknown etiology and pathogenesis. This report presents a rare case involving a man with 18F-fluorodeoxyglucose positron emission tomography/computed tomography (FDG PET/CT) hypermetabolism caused by KFD mimicking malignant lymphoma. The PET/CT maximum intensity projection showed multiple hypermetabolic lymphadenopathies and homogeneous FDG uptake in the bone marrow and spleen. Malignant lymphoma was initially suspected. The patient then underwent excision biopsy of one enlarged right cervical lymph node that was selected because it showed the highest FDG uptake in PET/CT, and examination of this biopsy specimen confirmed the diagnosis of KFD. PET/CT is useful for assessing the general condition of patients and can help to select lymph nodes for excision biopsy based on the highest FDG uptake. However, KFD can predispose to localized FDG uptake and limit the specificity of PET/CT by mimicking malignancy. Thus, positive results of PET/CT should be interpreted with caution.
Keywords: Positron emission tomography/computed tomography, lymphadenopathy, Kikuchi–Fujimoto disease, fluorodeoxyglucose, lymphoma, case report
Introduction
Kikuchi–Fujimoto disease (KFD), also known as histiocytic necrotizing lymphadenitis, is a benign, self-limiting inflammatory disorder of unknown etiology and pathogenesis. It is a relatively rare condition characterized by subacute necrotizing regional lymphadenopathy. KFD is frequently associated with mild fever and occasionally with other systemic symptoms.1–3 Kikuchi 4 and Fujimoto et al. 5 first described KFD in Japanese patients in 1972, and KFD has since been reported worldwide. It usually affects children and young adults. Most reports have indicated that KFD mainly affects ≤30-year-old female patients of Asian origin. 1 Lymph node involvement varies among patients with KFD, but the neck is the most common region of lymph node involvement. Many clinicians are unfamiliar with this disease, and it is difficult to differentiate from malignant lymphoma; this results in significant diagnostic challenges. The present report describes a rare case involving a man with 18F-fluorodeoxyglucose positron emission tomography/computed tomography (FDG PET/CT) hypermetabolism caused by KFD mimicking malignant lymphoma.
Case report
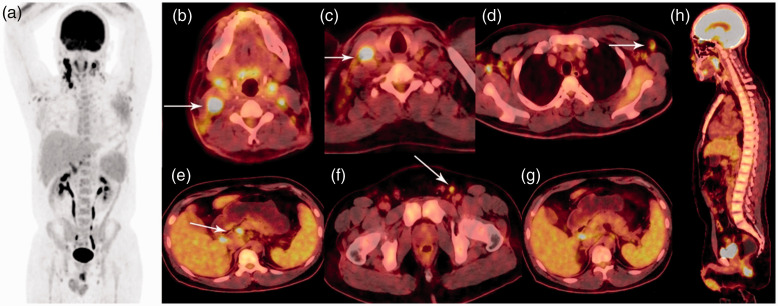
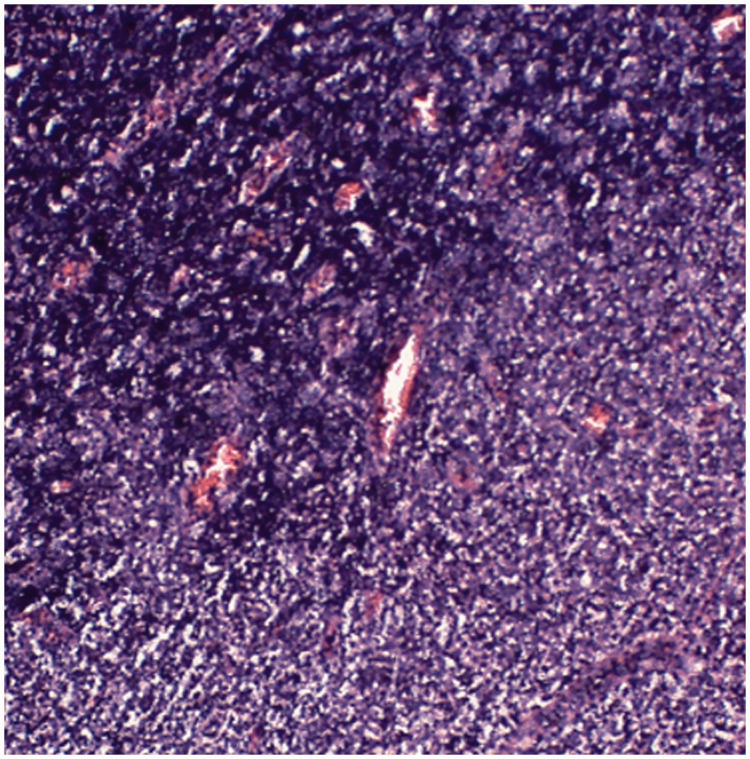
A 29-year-old man presented with palpable masses in the bilateral neck and a fever of 39°C. He had no other symptoms or signs, and physical examination revealed no abnormalities. Pertinent laboratory tests showed a dramatically increased C-reactive protein concentration (57.90 mg/L; reference range, 0–5 mg/L). The serum concentrations of IgG, IgA, IgM, IgE, C3, C4, carcinoembryonic antigen, alpha-fetoprotein, and cancer antigen 19-9 were within the reference ranges. Because of his clinical condition of fever and lymphadenopathy, the patient was suggested to undergo whole-body PET/CT. The PET/CT images were acquired on a Siemens Biograph mCT PET/CT scanner (Siemens Healthineers, Erlangen, Germany). The maximum intensity projection (MIP) PET/CT image showed intense accumulation of FDG in the lymph nodes (Figure 1(a)). PET/CT fusion images showed multiple areas of hypermetabolic lymphadenopathy in the bilateral cervical [maximum standardized uptake value (SUVmax), 17.9], right supraclavicular (SUVmax, 15.7), bilateral axillary (SUVmax, 6.3), abdominal (SUVmax, 7.6), and bilateral inguinal (SUVmax, 4.7) lymph nodes (Figure 1(b)–(f)). PET/CT fusion images showed mild, homogeneous FDG uptake in the spleen (SUVmax, 4.0) and bone marrow of the vertebral bodies (SUVmax, 4.8) (Figure 1(g), (h)). The patient was initially suspected to have malignant lymphoma because PET/CT showed intense accumulation of FDG in the lymph nodes, including the abdominal lymph nodes; the MIP image also showed mild, homogeneous FDG uptake in the spleen and bone marrow of the vertebral bodies; and the clinical presentation was characterized by systemic changes and a lack of consistent laboratory findings. The patient then underwent excision biopsy of one enlarged right cervical lymph node selected because it showed the highest FDG uptake in PET/CT. Examination of this biopsy specimen confirmed the diagnosis of KFD. The histopathologic examination of the lymph node showed numerous lymphohistiocytic cells and karyorrhectic debris (Figure 2). KFD is a benign and self-limiting disease, and its main features are acute or subacute cervical lymphadenopathy and fever. 6 KFD most commonly affects <30-year-old female patients of Asian origin;7,8 it less commonly develops in men, as in the present case. KFD can predispose to FDG uptake in localized lymph nodes and limit the specificity of FDG PET/CT by mimicking malignant lymphoma.9–11
Figure 1.
Whole-body PET/CT scan findings. (a) The MIP image showed intense accumulation of FDG in the lymph nodes. (b)–(f) PET/CT fusion images showed multiple areas of hypermetabolic lymphadenopathy in the bilateral cervical, right supraclavicular, bilateral axillary, abdominal, and bilateral inguinal lymph nodes (white arrowhead). (g), (h) PET/CT fusion images showed mild, homogeneous FDG uptake in the spleen and bone marrow of the vertebral bodies.
Figure 2.
Histopathological examination. Histopathologic examination of a lymph node specimen showed numerous lymphohistiocytic cells and karyorrhectic debris (hematoxylin and eosin stain; magnification, ×100).
KFD is a self-limiting disease that usually persists for several months. Only symptomatic treatment is needed for fever or pain. After excision biopsy of the lymph node in this case, the patient underwent symptomatic treatment and steroid therapy (methylprednisolone and prednisone). Two months later, a follow-up ultrasound examination revealed no abnormally enlarged cervical or axillary lymph nodes.
Discussion
KFD is a relatively rare benign, self-limiting condition characterized by subacute necrotizing regional lymphadenopathy. KFD most commonly affects <30-year-old female patients of Asian origin. Although it more frequently presents in young women, the pediatric and geriatric populations may also be affected; however, KFD less commonly presents in young men, as in the present case. 12 The pathogenesis of KFD is unclear. Infectious and autoimmune disorders are considered common causes. The ineffectiveness of antibiotics for KFD suggests a viral origin. Moreover, histopathologic findings also suggest viral infection. Some studies have shown an association between KFD and Epstein–Barr virus or systemic lupus erythematosus; however, these associations have not been definitively proven. 6 Because KFD remains a poorly recognized disease with nonspecific symptoms, it is difficult to distinguish from other diseases. 13 Histopathologic examination of the lymph nodes of these patients is necessary. Autoimmune disorders, especially systemic lupus erythematosus, are frequently reported in patients with KFD. Treatment guidelines for KFD are not well established in the literature. Most patients with KFD show a self-limiting disease course, and observation is the most common management regimen.
PET/CT plays an important role in the management of malignant diseases. However, FDG avidity increases with elevations in glycolysis and glucose transporter activity, which are not cancer-specific. Thus, false-positive FDG uptake in benign lesions may occur. 14 KFD can predispose to localized FDG uptake and limit the specificity of PET/CT by mimicking malignancy.
We have herein described a man with palpable masses in the bilateral neck. PET/CT showed intense accumulation of FDG in the lymph nodes, including the abdominal lymph nodes. Because the MIP image also showed mild, homogeneous FDG uptake in the spleen and bone marrow of the vertebral bodies, the patient was initially suspected to have malignant lymphoma. He then underwent excision biopsy of one enlarged right cervical lymph node, which confirmed the diagnosis of KFD.
PET/CT imaging of KFD was first reported in 2003. 15 The imaging findings of KFD are easily confused with those of malignant lymphoma; therefore, positive results on PET/CT should be interpreted with caution. KFD should be considered when PET/CT shows intense accumulation of FDG in lymph nodes with or without involvement of lymph nodes in the peritoneal or retroperitoneal regions. We included 10 reports in our final literature review.7,9,15–22 Including the present case, 60 cases of KFD with PET/CT imaging have been reported to date (Table 1).
Table 1.
PET/CT characteristics of patients with KFD
| Year/reference | Case | Sex | Age, years | Lymph node condition |
|---|---|---|---|---|
| 2020/Present case | 1 | M | 29 | Bilateral cervical (SUVmax, 17.9), right supraclavicular (SUVmax, 15.7), bilateral axillary (SUVmax, 6.3), abdominal (SUVmax, 7.6), and bilateral inguinal (SUVmax, 4.7) lymph nodes |
| 2003/Liao and Chen[ 15 ] | 1 | F | 26 | Right neck, bilateral supraclavicular fossae, mediastinal, left pulmonary hilar, and left axillary nodes |
| 2007/Kim et al.[ 16 ] | 1 | F | 10 | Right cervical, supraclavicular, porta hepatic, aortocaval, and right para-aortic regions |
| 2008/Kaicker et al.[ 17 ] | 1 | F | 19 | Supraclavicular (SUVmax, 10.5) and hilar (SUVmax, 4) lymph nodes |
| 2010/Ito et al.[ 18 ] | 7 | 1 M, 6 F | 23–66 | 6.25 ± 3.32 |
| 2011/Tsujikawa et al.[ 7 ] | 8 | NA | NA | 6.4 ± 1.5 |
| 2013/Kong et al.[ 19 ] | 22 | 14 M, 8 F | 9–73 | 6.2–29.4 |
| 2014/Kim et al.[ 9 ] | 8 | 3 M, 5 F | 9–17 | 8.3–22.5 |
| 2015/Zhang et al.[ 20 ] | 9 | 4 M, 5 F | 17–60 | 4.2 ± 2.2 |
| 2017/Aoyama et al.[ 21 ] | 1 | F | 30 | Right cervical lymph node (SUVmax, 19.0) |
| 2019/Horino et al.[ 22 ] | 1 | F | 21 | Cervical, supraclavicular, axillary, and pelvic lymph nodes |
M, male; F, female; SUVmax, maximum standardized uptake value; NA, not available.
Although KFD can predispose to localized FDG uptake and limit the specificity of PET/CT by mimicking malignancy, PET/CT can also provide important information. Xu et al. 23 compared a case of KFD in a young Chinese woman with relevant cases in the literature and proposed a diagnostic flow chart of KFD to facilitate diagnosis and treatment and thus avoid misdiagnosis and mistreatment. Chen et al. 24 reported that unilateral cervical lymphadenopathy was the most frequent form of lymph node involvement in patients with KFD. Extracervical lymphadenopathy in the abdomen, pelvis, inguinal region, axillae, and mediastinum is not uncommon and is associated with bilateral involvement of the cervical lymph nodes. 24 In the present case, the PET/CT images showed the patient’s whole-body lymph node condition, thus providing valuable information on extracervical lymphadenopathy. Tsujikawa et al. 7 reported the usefulness of PET/CT for distinguishing KFD and malignant lymphoma. They reported that KFD and aggressive non-Hodgkin’s lymphoma showed a significantly higher corrected SUV than that of indolent non-Hodgkin’s lymphoma. Additionally, using both the SUV and partial-volume–corrected SUV, PET/CT can help to distinguish between KFD and malignant lymphoma. 7 Kong et al. 19 analyzed the FDG PET/CT findings of 22 patients with KFD and reported that KFD could result in multiple hypermetabolic lymph nodes throughout the body and that PET/CT images showed a generalized distribution of relatively small lymph nodes with high FDG uptake. Kim et al. 9 retrospectively reviewed the medical records of 23 patients with KFD and 33 patients with malignant lymphoma and reported that patients with malignant lymphoma tended to present with extranodal involvement or huge conglomerated lymphadenopathies; in contrast, patients with KFD had generalized lymphadenopathy without extranodal involvement.
PET/CT shows the general regions of the lymph nodes and can aid in decision-making regarding appropriate biopsy sites. Thus, for patients who show lymphadenopathy with high FDG uptake, extranodal involvement, or huge conglomerated lymphadenopathies on PET/CT, we suggest preparing the patient for chemotherapy with intravenous fluid hydration while waiting for the pathologic confirmation. For patients who show lymphadenopathy with only nodal involvement, we suggest waiting for confirmation of the diagnosis by pathologic examination, as in the present case. Histopathologic examination of the lymph nodes and long-term follow-up after symptomatic treatment and steroid therapy are also necessary. If conditions permit, a review of PET/CT findings after treatment will provide further understanding of the disease.
Supplemental Material
Supplemental material, sj-pdf-1-imr-10.1177_03000605211032859 for Positron emission tomography/computed tomography hypermetabolism of Kikuchi–Fujimoto disease mimicking malignant lymphoma: a case report and literature review by Shu Wang, Bulin Du, Xuena Li and Yaming Li in Journal of International Medical Research
Acknowledgements
We would like to thank the patient for consenting to the publication of this report and all research staff involved in this case study.
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a grant from the First Hospital of China Medical University, National Natural Science Foundation (81971652).
ORCID iD: Shu Wang https://orcid.org/0000-0003-1734-9770
Ethics approval and consent to participate
This study is based on a clinical case; therefore, ethical approval was not required by our institution. Written consent was obtained from the study participant. This study is reported in accordance with the CARE guidelines. 23
Data sharing
All data are presented in the article.
References
- 1.Bosch X, Guilabert A, Miquel R, et al. Enigmatic Kikuchi-Fujimoto disease: a comprehensive review. Am J Clin Pathol 2004; 122: 141–152. [DOI] [PubMed] [Google Scholar]
- 2.Hutchinson CB, Wang E. Kikuchi-Fujimoto disease. Arch Pathol Lab Med 2010; 134: 289–293. [DOI] [PubMed] [Google Scholar]
- 3.Pepe F, Disma S, Teodoro C, et al . Kikuchi-Fujimoto disease: a clinicopathologic update. Pathologica 2016; 108: 120–129. [PubMed] [Google Scholar]
- 4.Kikuchi M. Lymphadenitis showing focal reticulum cell hyperplasia with nuclear debris and phagocytes: a clinicopathological study. Acta Hematol Jpn 1972; 35: 379–380. [Google Scholar]
- 5.Fujimoto Y, Kozima Y, Yamaguchi K. Cervical subacute necrotizing lymphadenitis: a new clinicopathologic entity. Naika 1972; 20: 920–927. [Google Scholar]
- 6.Perry AM, Choi SM. Kikuchi-Fujimoto disease: a review. Arch Pathol Lab Med 2018; 142: 1341–1346. [DOI] [PubMed] [Google Scholar]
- 7.Tsujikawa T, Tsuchida T, Imamura Y, et al. Kikuchi-Fujimoto disease: PET/CT assessment of a rare cause of cervical lymphadenopathy. Clin Nucl Med 2011; 36: 661–664. [DOI] [PubMed] [Google Scholar]
- 8.Makis W, Ciarallo A, Gonzalez-Verdecia M, et al. Systemic lupus erythematosus associated pitfalls on (18)F-FDG PET/CT: reactive follicular hyperplasia, Kikuchi-Fujimoto disease, inflammation and lymphoid hyperplasia of the spleen mimicking lymphoma. Nucl Med Mol Imaging 2018; 52: 74–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim JE, Lee EK, Lee JM, et al. Kikuchi-Fujimoto disease mimicking malignant lymphoma with 2-[(18)F]fluoro-2-deoxy-D-glucose PET/CT in children. Korean J Pediatr 2014; 57: 226–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li B, Zhang Y, Hou J, et al. Synchronous Kikuchi-Fujimoto disease and gastric adenocarcinoma mimicking malignant lymphoma on (18)F-FDG PET/CT. Rev Esp Med Nucl Imagen Mol 2016; 35: 277–278. [DOI] [PubMed] [Google Scholar]
- 11.Escudier A, Courbage S, Meignin V, et al. [Kikuchi-Fujimoto disease mimicking malignant lymphoma in adolescents]. Arch Pediatr 2017; 24: 471–475. [DOI] [PubMed] [Google Scholar]
- 12.Santana A, Lessa B, Galrão L, et al. Kikuchi-Fujimoto's disease associated with systemic lupus erythematosus: case report and review of the literature. Clin Rheumatol 2005; 24: 60–63. [DOI] [PubMed] [Google Scholar]
- 13.Chamulak GA, Brynes RK, Nathwani BN. Kikuchi-Fujimoto disease mimicking malignant lymphoma. Am J Surg Pathol 1990; 14: 514–523. [DOI] [PubMed] [Google Scholar]
- 14.Cook GJ, Wegner EA, Fogelman I. Pitfalls and artifacts in 18FDG PET and PET/CT oncologic imaging. Semin Nucl Med 2004; 34: 122–133. [DOI] [PubMed] [Google Scholar]
- 15.Liao AC, Chen YK. Cervical lymphadenopathy caused by Kikuchi disease: positron emission tomographic appearance. Clin Nucl Med 2003; 28: 320–321. [DOI] [PubMed] [Google Scholar]
- 16.Kim CH, Hyun OJ, Yoo Ie R, et al. Kikuchi disease mimicking malignant lymphoma on FDG PET/CT. Clin Nucl Med 2007; 32: 711–712. [DOI] [PubMed] [Google Scholar]
- 17.Kaicker S, Gerard PS, Kalburgi S, et al. PET-CT scan in a patient with Kikuchi disease. Pediatr Radiol 2008; 38: 596–597. [DOI] [PubMed] [Google Scholar]
- 18.Ito K, Morooka M, Kubota K. Kikuchi disease: 18F-FDG positron emission tomography/computed tomography of lymph node uptake. Jpn J Radiol 2010; 28: 15–19. [DOI] [PubMed] [Google Scholar]
- 19.Kong E, Chun K, Hong Y, et al. 18F-FDG PET/CT findings in patients with Kikuchi disease. Nuklearmedizin 2013; 52: 101–106. [DOI] [PubMed] [Google Scholar]
- 20.Zhang J, Dong MJ, Liu KF, et al . (18)F-Fluorodeoxyglucose positron emission tomography/computed tomography in patients with Kikuchi-Fujimoto disease: a nine-case series in China. Int J Clin Exp Med 2015; 8: 21034–21043. [PMC free article] [PubMed] [Google Scholar]
- 21.Aoyama KI, Otsuru M, Uchibori M, et al. Kikuchi-Fujimoto disease with 18F-fludeoxyglucose uptake in cervical lymph nodes on dual-time-point imaging positron emission tomography/computed tomography mimicking malignant disease. World J Nucl Med 2017; 16: 68–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Horino T, Ichii O, Terada Y. Is recurrent Kikuchi-Fujimoto disease a precursor to systemic lupus erythematosus? Rom J Intern Med 2019; 57: 72–77. [DOI] [PubMed] [Google Scholar]
- 23.Xu S, Sun W, Liu J. Kikuchi-Fujimoto disease: a case report and the evaluation of diagnostic procedures. BMC Oral Health 2019; 19: 223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen LC, Wang CJ, Chang YC, et al . Distribution of lymphadenopathy in patients with Kikuchi disease. J Microbiol Immunol Infect 2019. [DOI] [PubMed] [Google Scholar]
- 25.Gagnier JJ, Kienle G, Altman DG, et al. The CARE Guidelines: Consensus-based Clinical Case Reporting Guideline Development. Glob Adv Health Med 2013; 2: 38–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-imr-10.1177_03000605211032859 for Positron emission tomography/computed tomography hypermetabolism of Kikuchi–Fujimoto disease mimicking malignant lymphoma: a case report and literature review by Shu Wang, Bulin Du, Xuena Li and Yaming Li in Journal of International Medical Research