Abstract
Background
Recommendations for promoting mental health during the COVID-19 pandemic include maintaining social contact, through virtual rather than physical contact, moderating substance/alcohol use, and limiting news and media exposure. We seek to understand if these pandemic-related behaviors impact subsequent mental health.
Methods
Daily online survey data were collected on adults during May/June 2020. Measures were of daily physical and virtual (online) contact with others; substance and media use; and indices of psychological striving, struggling and COVID-related worry. Using random-intercept cross-lagged panel analysis, dynamic within-person cross-lagged effects were separated from more static individual differences.
Results
In total, 1148 participants completed daily surveys [657 (57.2%) females, 484 (42.1%) males; mean age 40.6 (s.d. 12.4) years]. Daily increases in news consumed increased COVID-related worrying the next day [cross-lagged estimate = 0.034 (95% CI 0.018–0.049), FDR-adjusted p = 0.00005] and vice versa [0.03 (0.012–0.048), FDR-adjusted p = 0.0017]. Increased media consumption also exacerbated subsequent psychological struggling [0.064 (0.03–0.098), FDR-adjusted p = 0.0005]. There were no significant cross-lagged effects of daily changes in social distancing or virtual contact on later mental health.
Conclusions
We delineate a cycle wherein a daily increase in media consumption results in a subsequent increase in COVID-related worries, which in turn increases daily media consumption. Moreover, the adverse impact of news extended to broader measures of psychological struggling. A similar dynamic did not unfold between the daily amount of physical or virtual contact and subsequent mental health. Findings are consistent with current recommendations to moderate news and media consumption in order to promote mental health.
Key words: COVID-19 pandemic, mental health, social isolation, media consumption, cross-lagged effects
Introduction
The COVID pandemic poses a significant challenge to mental health, with reports of increasing levels of anxiety, depressive symptoms, and psychological distress in the general population in multiple countries spanning across Asia, Europe, and the USA (2020; Pfefferbaum & North, 2020; Vindegaard & Benros, 2020). Several agencies and expert authorities have issued recommendations for promoting good mental health during the pandemic, including the Centers for Disease Control and World Health Organization (CDC, 2020; WHO, 2020). There are three central tenets in the recommendations. Firstly, individuals are encouraged to maintain social connections through virtual (phone, online) rather than physical contact (Brooks et al., 2020; CDC, 2020; WHO, 2020). Secondly, limiting the use of substances has been encouraged during the pandemic (Brooks et al., 2020; CDC, 2020), informed by evidence that isolation and stress are important risk factors for substance misuse, including alcohol use (Clay & Parker, 2020). Finally, moderating exposure to COVID-related news has also been recommended (Amsalem, Dixon, & Neria, 2020; CDC, 2020). This recommendation is supported by reports of associations between news/media consumption about COVID-19 and poor mental health, including anxiety and depressive symptoms (Gao et al., 2020; Ni et al., 2020; Olagoke, Olagoke, & Hughes, 2020). The efficacy of these recommendations rests on the assumption that these behaviors impact subsequent mental health, rather than mental health impacting the behavior. In this study, we test three hypotheses that underlie these current public health recommendations. Specifically, in line with current recommendations, we hypothesized that better mental health will be promoted by (1) maintaining virtual contact with others; (2) limiting the use of substances (alcohol and illicit drugs); and (3) limiting the amount of news that is consumed. The three hypotheses are directional in that all predict that behaviors will impact on subsequent mental health, rather than the opposite direction of effects.
To test the hypotheses, we apply random intercept cross-lagged panel modeling (RI-CLPM) to daily ‘diary’ survey data acquired in June 2020, in order to parse the effects of behavior on mental health and vice versa. RI-CLPM disentangles dynamic, within-person processes relating behaviors to mental health from more stable individual differences (Hamaker, Kuiper, & Grasman, 2015). The dynamic processes relating behavior and mental health within persons are delineated as lagged effects, both autoregressive and cross-lagged. The within-person cross-lagged measures indicate the degree to which a daily deviation from usual levels of one variable is related to change the following day in another. In essence, the cross-lagged effect maps how ‘state-like’ features of behavior and mental health exert a mutual influence over time. The random intercepts that are included in these models capture the more ‘trait-like’, stable aspects of behavior and mental health. Correlations between the random intercepts thus represent associations between the more stable facets of behavioral and psychological measures. In summary, using daily diary survey data, we determine if daily variation in key pandemic-related behaviors – keeping social distance from others, maintaining virtual contact, and watching news/media – has an effect on the subsequent mental health; a direction of effects that would be consistent with current recommendations.
Methods
Individuals were recruited via Qualtrics' actively managed, double-opt-in market research panels. We aimed to oversample African American, Hispanic, and low-income populations, given evidence of a disparate impact of COVID on these groups (Fitzpatrick, Harris, & Drawve, 2020; Sneed, 2020).
We thus created six categories to guide recruitment: African American and low income; African American and high income; Hispanic and low income, Hispanic and high income; White, non-Hispanic, and low income; and White, non-Hispanic, and high income. The sampling strategy thus aimed to recruit equal numbers from these six groups by targeting states that included counties with demographics that met this goal. As we were interested in the effects of social distancing, we further restricted recruitment to states with active ‘stay-at-home’ or ‘safer at home’ orders projected to be ongoing at the time daily diary recruitment aimed to be opened (May 15). This strategy led to the inclusion of the following states: Alabama, California, Oregon, Kentucky, Louisiana, Maine, Maryland, New Jersey, New York, Pennsylvania, Tennessee, Virginia, Washington, and Washington DC (online Supplementary Fig. S1a). After the study collection period ended, we evaluated infection rate trends during the daily diary data collection period (21 May through 16 June). Two trends emerged: states with rising and states with falling infections (online Supplementary Fig. S1a). This was used as a covariate in RICPLM models (see online Supplementary Table S10). Participants were compensated with $15 for completing the baseline survey and $1 for every daily survey completed.
Adults with online/smartphone access completed a baseline and daily survey, sent to their email/smartphone every evening. Written online consent was obtained from all participants. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The study was determined to be exempt from IRB review by the University of Pennsylvania.
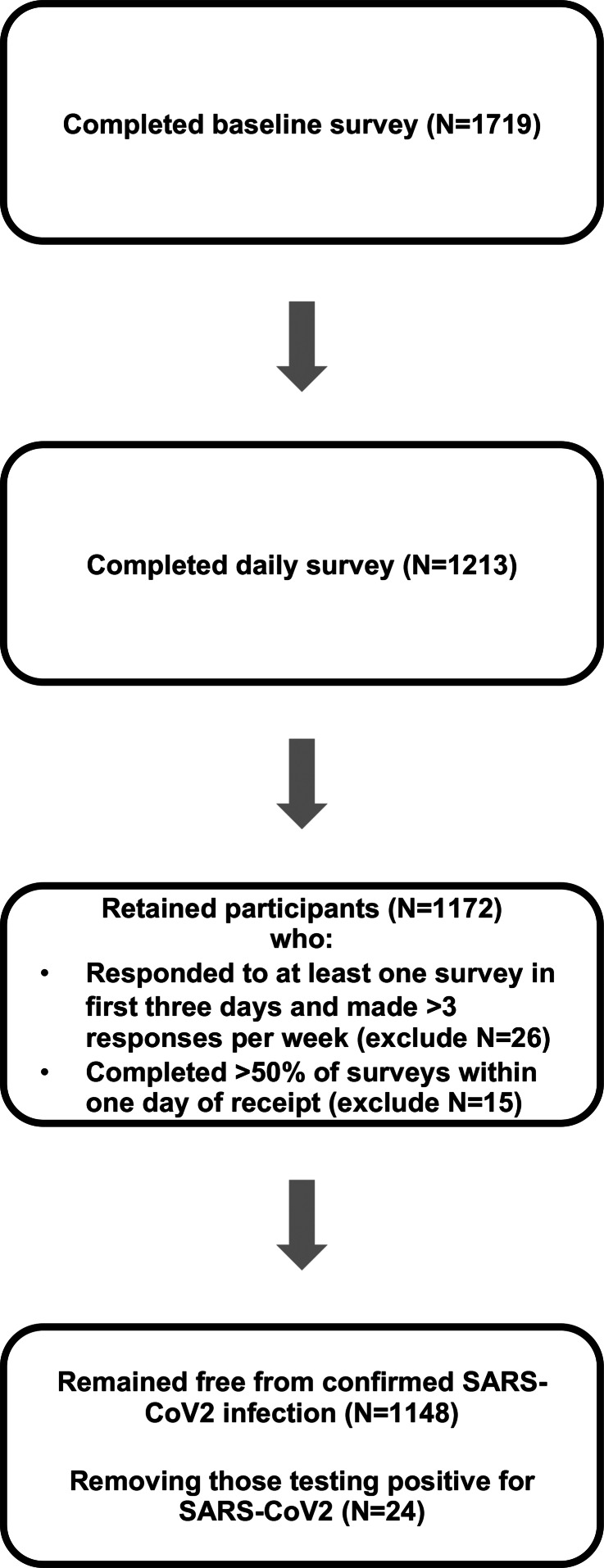
We set a target recruitment of 1750. Beginning 5 May, Qualtrics invited approximately 94 000 individuals through their panels to participate in the study. Recruitment was closed on 26 May following successful recruitment of 1719 participants and to facilitate transition to the daily diary. Of these 1719 individuals, 1213 joined the daily diary (open to all who completed the baseline survey). Of those, 1148 completed daily surveys and met our inclusion criteria for entry in the cross-lagged analyses (66.8% of the total who completed the baseline survey). Those who completed the daily diary questionnaire (N = 1148) tended to be older, white/non-Hispanic, female, and have higher income than those who did not complete the daily survey (see online Supplementary Table S1).
The criteria for inclusion were (1) completion of at least one response in the first 3 days of the 15 days of data collection, (2) completion of at least three responses per week of responses, (3) completion of at least half of surveys within 1 day of receipt. The proportion of missing data among the 1148 who were included in the cross-lagged analyses was low. Our final data set included 23 028 observations out of a possible 24 108 (21 responses per 1148 participants), giving a missingness rate of 4.5%. Imputation of the missing values was performed using maximum likelihood estimation within the lavaan function for each pairwise model.
The daily diary questionnaire
The survey contained 11 questions on mental health completed by participants every evening – full survey in online Supplementary material. The 11 questions pertaining to general mental health were adapted from the Patient Health Questionnaire-9 (PHQ-9) (Kroenke, Spitzer, & Williams, 2001) and General Anxiety Disorder-7 (GAD-7) (Spitzer, Kroenke, Williams, & Löwe, 2006). Items on COVID-related worrying were adaptations of the Disease Worry and Risk Perception scales, originally used in cancer research (Lerman et al., 1991) – see online Supplementary Table S2 for breakdown of mental health questions. Longitudinal confirmatory factor analyses were run in lavaan, R, using the function measEq.syntax in the package semTools. Fitted models included a one-factor solution containing all 11 questions, a two-factor solution splitting mental health from COVID-related worry, a three-factor solution containing questions split by source (GAD-7, PHQ-9, DWRPC), and a three-factor solution split by positive valence mental health, negative valence mental health, and COVID-related worry. This final solution provided the best fit in longitudinal confirmatory factor analysis across all levels of invariance included in models [configural (CFI: 0.999, RMSEA: 0.025), threshold (CFI: 0.999, RMSEA: 0.025), metric (CFI: 0.999, RMSEA: 0.025), scalar (CFI: 0.999, RMSEA: 0.025), and strict (CFI: 0.999, RMSEA: 0.028)] – see online Supplementary Table S3 for full results. The extracted factors were defined as psychological struggling (levels of sadness, anxiety, loneliness, and stress), psychological striving (levels of pleasure, happiness, optimism), and COVID-related worry (concerns of infection of self or others, and its impact on daily functioning).
Daily news/media consumption was determined from three items: ‘How much time did you spend reading or listening to the news today?’, ‘Overall, how much time did you spend browsing social media today (e.g. Facebook, Twitter, TikTok, Instagram)?’, and ‘How much did you read or hear about the coronavirus pandemic today?’ This variable also showed a robust factor solution (configural CFI > 0.999, RMSEA 0.007; threshold CFI > 0.999, RMSEA < 0.0001; metric CFI > 0.999, RMSEA 0.01; scalar CFI > 0.999, RMSEA 0.025; strict CFI 0.999, RMSEA 0.035) when considering the repeated observations over time.
The daily amount of physical contact with others was determined for those within and outside of the home. Contact within the home was coded as the sum of people interacted with within the home environment (within 20 feet) and guests to the home environment (capping the maximum number of contacts at five). Contact outside the home was coded as the number of settings that involved close physical contact (within six feet) of others, with responses ranging from zero to seven settings. The settings were shopping/running errands, working, meeting a friend solo, meeting friends in a group setting, walking/leisurely activity alone, walking/leisurely activity with others, and attending organized meetings. Total physical contact was the sum of the within-home and outside-home contacts. Virtual contact was the summed amount of time participants reported interacting with family (zero to four, ranging from no contact to more than 2 h of contact) and friends (zero to four, ranging from no contact to more than 2 h of contact) each day.
Alcohol use coded as the number of daily alcoholic drinks consumed, from a minimum of zero to a maximum of five (for five or more alcoholic drinks). Substance use was coded as the number of substances used each day, including tobacco products, e.g. cigarettes and vapes, marijuana, opiates including heroin and other narcotics, and other drugs including amphetamines, cocaine, ecstasy, and hallucinogens. Responses ranged from zero (no substance use) to four (all four substances used).
Analysis
Random intercept cross-lagged panel analysis (implemented in Lavaan R) separated dynamic within-individual processes (measured as lagged effects between daily changes in behavior and mental health) from more stable individual differences in the variables (measured as the covariance between random intercepts – online Supplementary Fig. S1b, Supplementary Methods) (Hamaker et al., 2015; Mulder & Hamaker, 2020). The daily items are modeled as within-person latent factors and a latent intercept factor. The random intercepts are specified by creating a latent variable with the repeated measures as its indicators and fixing all the factor loadings to one. The covariance between the random intercepts indicates how stable individual differences in one measure are associated with another. The within-person components are specified as a latent variable for each measurement and constraining measurement error variances to zero. The model also specifies that within-person components at the first observation and the within-person residuals at all subsequent occasions are correlated within each occasion. For the between-person components, we specify that the random intercepts can be correlated. See online Supplementary Fig. S2 for a diagram of an example model.
The main analysis held the cross-lagged and auto-regressive effects constant over the 14 daily lags in the study. We used this approach as we did not expect relationships between mental health and behavior to vary substantially over this short time. The approach was also appropriate given the regular daily intervals between observations and favored on the grounds of parsimony as it estimates four parameters (two cross-lagged and two autoregresssive) compared with 56 parameters in the fully unconstrained model (four parameters for each of the 14 lags estimated in our 15-day study). We compared a constrained model against a fully unconstrained model (daily lag values allowed to vary). In line with recommendations, we used two indices of model fits: the difference between models in the comparative fit index (CFI), and differences in the root mean square error approximation (RMSEA) (Chen, 2007; Cheung & Rensvold, 2002). We adopted the recommended critical values of ΔCFI > −0.01 and ΔRMSEA > 0.01 as indicating that the constrained model provided a worse fit to the data than the unconstrained model. This approach is preferred to the examination of differences in χ2 of model fits, which has several limitations including being highly sensitive to sample size (Brannick, 1995). As can be seen from online Supplementary Table S4, the constrained and unconstrained models showed consistently acceptable fit using the CFI and RMSEA metrics. When applying the constraint, the global fit indices did not change substantially, and thus we adopt the theoretically preferred, more parsimonious constrained model in the main report.
As noted in the introduction, our goal was to test the directional hypotheses that emerge from current public health recommendations: better mental health will be promoted by (1) maintaining virtual contact with others; (2) limiting the use of substances (alcohol and illicit drugs); and (3) limiting the amount of news that is consumed. By their nature, the cross-lagged analyses we used test other directional effects (both autoregressive and the effects of mental health on later behavior). For completeness, we also tested cross-lagged effects within domains (does one behavior impact another, etc.). In total, we thus tested the relationships between 28 pairs of variables, each with two cross-lagged and two auto-regressive effects, making 112 effects. Of those 112 effects, three pertained to the primary hypotheses, and the remainder parse all possible pairwise combinations of cross-lagged and autoregressive effects. Reported p values were adjusted using the false discovery rate procedure to account for multiple testing (Benjamini & Hochberg, 1995).
Results
The final cohort comprised 1148 adults who met the criteria for adequate data completion (41 did not complete data satisfactorily – Methods). We also removed the 24 subjects who tested positive for SARS-CoV2 during the study (N = 24) – participant flow is shown in Fig. 1. We aimed to have equal representation of African American (non-Hispanic), White non-Hispanic and Hispanic groups, but the final cohort contained fewer Hispanic members than anticipated [N = 327 (28.5%); White, non-Hispanic N = 463 (40.3%); African American, non-Hispanic N = 358 (31.2%)]. The gender breakdown of the final cohort was N = 658 (57.2%) female, N = 485 (42.2%) male, and N = 5 (0.04%) non-binary (did not identify as male or female). The average age was 40.7 years (s.d. 11.5). We sampled equally from states that had increasing and decreasing rates of confirmed SARS-CoV2 infection during the study – online Supplementary Fig. S1a. In total, 760 (66.2%) subjects entered the study on 21 May 2020 and 388 (33.8%) entered 6 days later, and we confine these analyses to the overlapping 15 days.
Fig. 1.
Participant workflow.
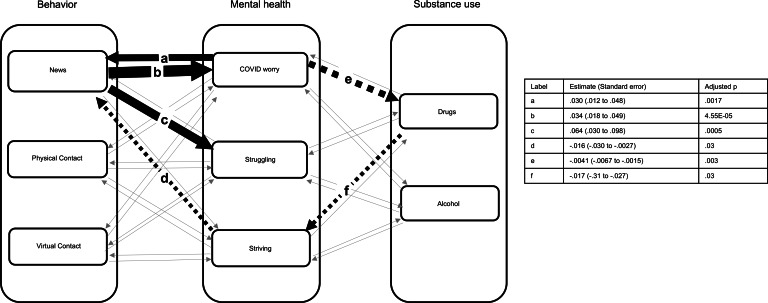
Our primary focus was on the cross-lagged effects of behaviors (daily physical and virtual contact with others, substance use and consumption of news/media) on mental health. Daily means and standard deviations for these variables are located in online Supplementary Table S5. Variables were not centered. Using RI-CLPM, we found that daily fluctuations in news/media consumption showed a significant cross-lagged effect on subsequent COVID-related worrying [standardized estimate = 0.034 (95% CI 0.018–0.049), adjusted p = 0.00005] – see Fig. 2. Thus, for a given individual, a higher than usual amount of news consumption on a given day is followed the next day by an increase in COVID-related worries. The inverse cross-lagged effect of COVID-related worries on subsequent media consumption was also present [estimate 0.03 (0.012–0.048), adjusted p = 0.0017]. Full autoregressive and cross-lagged effects for all possible combinations are given in Table 1, with significant cross-lagged effects following FDR correction illustrated in Supplementary Fig. S3.
Fig. 2.
Cross-lagged effects between mental health and both behavior (contact and news/media consumption) and substance use. Significant positive lags (a, b, c) are represented by full lines; negative lags (d, e, f) by dotted lines. Thickness of the connecting lines is proportional to the –log10 FDR p value. Values for the paths a, b, c, d, e, f are given in the table.
Table 1.
Cross-lagged and autoregressive parameters for all models tested (28 possible pairwise contrasts of three behavioral, three mental health, and two substance use variables)
| Cross lagged | Autoregressive | |||||||
|---|---|---|---|---|---|---|---|---|
| 1 → 2 | 2 → 1 | 1 → 1 | 2 → 2 | |||||
| Est (CI) | p | Est (CI) | p | Est (CI) | p | Est (CI) | p | |
| 1. News 2. Worry |
0.034 (0.018–0.049) | 0.00005 | 0.030 (0.012–0.048) | 0.002 | 0.23 (0.21–0.25) | <0.00001 | 0.19 (0.17–0.21) | <0.00001 |
| 1. News 2. Struggling |
0.064 (0.030–0.098) | 0.0005 | 0.0009 (−0.007 to 0.009) | 0.89 | 0.23 (0.22–0.25) | <0.00001 | 0.095 (0.078–0.113) | <0.00001 |
| 1. News 2. Striving |
−0.019 (−0.040 to 0.0015) | 0.11 | −0.016 (−0.030 to −0.0027) | 0.03 | 0.23 (0.22–0.25) | <0.00001 | 0.20 (0.19–0.22) | <0.00001 |
| 1. News 2. Physical contact |
0.021 (0.0062–0.036) | 0.01 | −0.0018 (−0.020 to 0.017) | 0.90 | 0.23 (0.22–0.25) | <0.00001 | 0.12 (0.098–0.13) | <0.00001 |
| 1. News 2. Virtual contact |
0.024 (0.0097–0.038) | 0.002 | −0.017 (−0.036 to 0.003) | 0.14 | 0.24 (0.22–0.25) | <0.00001 | 0.12 (0.10–0.14) | <0.00001 |
| 1. News 2. Drugs |
0.0015 (−0.0009 to 0.004) | 0.31 | 0.18 (0.066–0.30) | 0.003 | 0.23 (0.22–0.25) | <0.00001 | 0.18 (0.16–0.20) | <0.00001 |
| 1. News 2. Alcohol |
−0.0002 (−0.009 to 0.008) | 0.97 | 0.0006 (−0.031 to 0.033) | 0.97 | 0.23 (0.22–0.25) | <0.00001 | 0.17 (0.16–0.19) | <0.00001 |
| 1. Physical contact 2. Worry |
−0.0051 (−0.022 to 0.012) | 0.66 | −0.0017 (−0.018 to 0.015) | 0.89 | 0.12 (0.099–0.13) | <0.00001 | 0.20 (0.18–0.21) | <0.00001 |
| 1. Physical contact 2. Struggling |
−0.0068 (−0.045 to 0.031) | 0.80 | 0.0032 (−0.042 to 0.011) | 0.52 | 0.12 (0.099–0.13) | <0.00001 | 0.10 (0.080–0.11) | <0.00001 |
| 1. Physical contact 2. Striving |
0.0055 (−0.017 to 0.028) | 0.74 | −0.0077 (−0.020 to 0.0048) | 0.32 | 0.12 (0.099–0.13) | <0.00001 | 0.20 (0.19–0.22) | <0.00001 |
| 1. Physical contact 2. Drugs |
0.0009 (−0.0018 to 0.0036) | 0.61 | −0.022 (−0.13 to 0.083) | 0.78 | 0.12 (0.10–0.14) | <0.00001 | 0.18 (0.16–0.20) | <0.00001 |
| 1. Physical contact 2. Alcohol |
0.009 (−0.0003 to 0.019) | 0.09 | 0.0059 (−0.024 to 0.036) | 0.78 | 0.12 (0.098–0.13) | <0.00001 | 0.17 (0.15–0.19) | <0.00001 |
| 1. Physical contact 2. Virtual contact |
0.0005 (−0.015 to 0.016) | 0.97 | −0.0035 (−0.022 to 0.015) | 0.78 | 0.12 (0.099–0.13) | <0.00001 | 0.12 (0.11–0.14) | <0.00001 |
| 1. Virtual contact 2. Worry |
0.0065 (−0.012 to 0.025) | 0.59 | −0.00064 (−0.016 to 0.015) | 0.97 | 0.12 (0.11–0.14) | <0.00001 | 0.20 (0.18–0.21) | <0.00001 |
| 1. Virtual contact 2. Struggling |
0.032 (−0.008 to 0.072) | 0.17 | 0.002 (−0.005 to 0.009) | 0.66 | 0.12 (0.11–0.14) | <0.00001 | 0.097 (0.080–0.11) | <0.00001 |
| 1. Virtual contact 2. Striving |
0.022 (−0.0017 to 0.047) | 0.11 | 0.0058 (−0.0058 to 0.017) | 0.44 | 0.12 (0.11–0.14) | <0.00001 | 0.20 (0.18–0.22) | <0.00001 |
| 1. Virtual contact 2. Drugs |
−4.9 × 10−05 (−0.003 to 0.003) | 0.97 | 0.078 (−0.02 to 0.18) | 0.17 | 0.12 (0.11–0.14) | <0.00001 | 0.18 (0.16–0.20) | <0.00001 |
| 1. Virtual contact 2. Alcohol |
0.0086 (−0.0014 to 0.019) | 0.14 | −0.0098 (−0.037 to 0.018) | 0.59 | 0.13 (0.11–0.14) | <0.00001 | 0.17 (0.16–0.19) | <0.00001 |
| 1. Drugs 2. Worry |
0.022 (−0.085 to 0.13) | 0.78 | −0.0041 (−0.0067 to −0.0015) | 0.003 | 0.18 (0.16–0.20) | <0.00001 | 0.20 (0.18–0.21) | <0.00001 |
| 1. Drugs 2. Struggling |
0.073 (−0.16 to 0.31) | 0.65 | −0.0007 (−0.0018 to 0.0005) | 0.35 | 0.18 (0.16–0.20) | <0.00001 | 0.096 (0.079–0.11) | <0.00001 |
| 1. Drugs 2. Striving |
−0.17 (−0.31 to −0.027) | 0.03 | 0.0007 (−0.0013 to 0.0027) | 0.59 | 0.18 (0.16–0.20) | <0.00001 | 0.20 (0.19–0.22) | <0.00001 |
| 1. Alcohol 2. Worry |
0.012 (−0.018 to 0.042) | 0.53 | −0.0010 (−0.010 to 0.0081) | 0.89 | 0.17 (0.16–0.19) | <0.00001 | 0.20 (0.18–0.21) | <0.00001 |
| 1. Alcohol 2. Struggling |
−0.035 (−0.10 to 0.031) | 0.40 | 0.0017 (−0.0024 to 0.0058) | 0.53 | 0.17 (0.16–0.19) | <0.00001 | 0.097 (0.079–0.11) | <0.00001 |
| 1. Alcohol 2. Striving |
−0.0017 (−0.041 to 0.038) | 0.97 | 0.0065 (−0.0004 to 0.014) | 0.10 | 0.17 (0.16–0.19) | <0.00001 | 0.20 (0.19–0.22) | <0.00001 |
| 1. Drugs 2. Alcohol |
0.026 (−0.034 to 0.085) | 0.52 | 0.0023 (−0.002 to 0.007) | 0.44 | 0.18 (0.16–0.20) | <0.00001 | 0.17 (0.16–0.19) | <0.00001 |
| 1. Worry 2. Struggling |
0.071 (0.034–0.11) | 0.0003 | 0.012 (0.0044–0.020) | 0.003 | 0.19 (0.18–0.21) | <0.00001 | 0.092 (0.075–0.11) | <0.00001 |
| 1. Worry 2. Striving |
−0.019 (−0.041 to 0.0035) | 0.14 | −0.02 (−0.033 to −0.007) | 0.003 | 0.19 (0.18–0.21) | <0.00001 | 0.20 (0.18–0.22) | <0.00001 |
| 1. Struggling 2. Striving |
−0.011 (−0.021 to −0.0004) | 0.07 | −0.099 (−0.13 to −0.070) | 5.1 × 10−11 | 0.079 (0.061–0.097) | <0.00001 | 0.20 (0.18–0.22) | <0.00001 |
Effects are standardized with 95% confidence intervals and FDR-adjusted p values. Significant cross-lagged effects (following adjustment are shown in bold).
Daily fluctuations in news consumption also exacerbated psychological struggling [estimate 0.064 (0.03–0.098), adjusted p = 0.0005]. By contrast, striving had a negative cross-lagged effect on subsequent news consumption [−0.016 (−0.0027 to −0.03), adjusted p = 0.03], meaning above-average striving decreased the amount of news consumed the following day. A path from news to striving was not present.
Daily increases in substance use, but not alcohol consumption, were associated with subsequent decreases in psychological striving [−0.17 (−0.03 to −0.31), adjusted p = 0.03] and COVID-related worrying significantly decreased subsequent drug use [−0.0041 (−0.0015 to −0.0067), adjusted p = 0.003].
Neither physical nor virtual contact with others had a significant cross-lagged effect on mental health. Findings held when considering physical contact either within or outside the home: no significant lags with any mental health variable emerged when inside and outside contact were treated as distinct variables – online Supplementary Table S6. Additionally, all results were non-significant when virtual contact with work colleagues was added to virtual contact with close family and friends.
We found significant cross-lagged effects between the mental health items: for example, striving significantly decreased subsequent COVID-related worries [−0.02 (−0.033 to −0.007), adjusted p = 0.003]. By contrast, psychological struggling increased subsequent COVID-related worries [0.012 (0.0044–0.020), adjusted p = 0.003], and vice versa [0.071 (0.034–0.11), adjusted p = 0.0003]. We also found significant cross-lagged effects between the behavioral items. For example, daily increases in news intake were associated with subsequent increases in physical contact [0.021 (0.0062–0.036), adjusted p = 0.01].
Associations between the more stable components of the behavioral and psychological measures (i.e. the covariations between random intercepts) differed from cross-lagged effects (Table 2). For example, while individual differences in physical contact with others were associated with increased striving, alcohol and drug intake (i.e. random intercepts covaried), there were no significant cross-lagged, dynamic effects between the same variables.
Table 2.
Covariances of the stable individual differences in behavioral, substance use, and mental health variables
| Striving | COVID-worry | News/media consumption | Physical contact | Virtual contact | Alcohol | Substance use | |
|---|---|---|---|---|---|---|---|
| Struggling | −2.24 (−2.58 to −1.91) p < 0.0001 | 2.95 (2.55–3.35) p < 0.0001 | 1.36 (1.03–1.68) p < 0.0001 | −0.15 (−0.36 to 0.049) p = 0.17 | 0.28 (0.09–0.48) p = 0.007 | 0.12 (−0.002 to 0.23) p = 0.08 | 0.069 (−0.003 to 0.14) p = 0.08 |
| Striving | −1.09 (−1.42 to 0.76) p < 0.0001 | −0.12 (−0.41 to 0.16) p = 0.44 | 0.48 (0.29–0.67) p < 0.0001 | 0.32 (0.15–0.50) p = 0.0006 | 0.025 (−0.08 to 0.13) p = 0.67 | 0.008 (−0.06 to 0.07) p = 0.81 | |
| COVID-worry | 2.18 (1.83–2.54), p < 0.0001 | 0.06 (−0.16 to 0.28) p = 0.63 | 0.39 (0.19–0.60) p = .0004 | 0.17 (0.04–0.29) p = 0.01 | 0.1 (0.024–0.28) p = 0.02 | ||
| News/media consumption | 0.088 (−0.1 to 0.28) p = 0.42 | 0.8 (0.62–0.98) p < 0.0001 | 0.18 (0.07–0.29) p = 0.002 | 0.066 (0.0004–0.13) p = 0.07 | |||
| Physical contact | 0.23 (0.12–0.35) p = 0.0002 | 0.13 (0.06–0.21) p = 0.0006 | 0.058 (0.0015–0.10) p = 0.01 | ||||
| Virtual contact | 0.094 (0.028–0.16) p = 0.01 | −0.023 (−0.06 to 0.017) p = 0.33 | |||||
| Alcohol | 0.13 (0.10–0.15) p < 0.0001 |
The covariances between the random intercepts are given with 95% confidence intervals, with FDR-adjusted p values.
To examine whether race/ethnicity and income level significantly impact the main findings, we compared model fits in which lagged effects were allowed to vary by race/ethnicity against those that constrained the lags to be the same across race/ethnic groups. Fit indices in constrained and unconstrained models were nearly identical, and thus we conclude that moderation of the cross-lagged effects by racial/ethnic identity and income level did not emerge as a substantial effect (online Supplementary Table S7). Reports of a past diagnosis of either a depressive (N = 270) or anxiety disorder (N = 307) also did not emerge as significant moderators (online Supplementary Table S8).
We tested whether the impacts of COVID worry remained after treating worry as two factors: one pertaining to fear of becoming infected by SARS-CoV2 and the other relating to its impact on daily functioning. The main cross-lagged findings, wherein COVID-worry was significantly associated with news intake (in both directions) and substance use, held when COVID-related worry was treated as two factors (online Supplementary Table S9). Significant findings in the main analysis also held after covarying for gender, age, date of study entry, and state trends in confirmed infections (online Supplementary Table S10).
Discussion
We map a vicious cycle within individuals between news/media consumption and COVID-19-related worry. Watching more news than usual on a given day significantly increased COVID-19-related worry the next day, and vice versa. An adverse effect of media consumption was also detected on measures of psychological struggling. Notably, psychological striving reduced media consumption, though reduced media consumption did not impact subsequent striving.
We did not find cross-lagged effects between physical and virtual contact with others on subsequent change in mental health. This is surprising given previous evidence of social isolation having an adverse impact on mental health: a longitudinal study of older adults has shown that social disconnectedness and perceived isolation lead to increased depression and anxiety symptoms (although that study was not conducted during the current pandemic) (Santini et al., 2020). It is however noteworthy that the more stable measure of individual differences in overall levels of physical contact was associated with greater striving and less struggling (i.e. the respective random intercepts were correlated). It is possible that the strong associations between more stable individual differences in behavior and mood overshadowed the impact of daily fluctuations in mood and behavior on one another, as characterized by the cross-lagged effects. However, the direction of effects cannot be inferred from associations between the stable individual differences; such directionality can only be deduced from the cross-lagged effects.
Individual differences in virtual contact emerged as a double-edged sword, being associated with both positive and negative facets of mental health. The positive association may reflect the role of virtual contact in promoting a sense of social connectedness; the negative association may reflect the heavy presence of COVID-related information on social media. As expected, daily increases in the number of substances used had an adverse impact on mental health, decreasing subsequent levels of psychological striving. This adds to the evidence in favor of moderating substance use during the pandemic, particularly as individuals with substance use disorders may be at increased risk of being infected with COVID-19 (Ornell et al., 2020). However, this pattern does not account for fluctuations in the amount of other substances used, which was not assessed.
The analytic approach used (RI-CLPM) has several advantages over traditional cross-lagged analyses. Traditional cross-lag panel models are unable to fully account for variables that are at least partially time-invariant through just the autoregressive correlations (Hamaker et al., 2015). Additionally, by separating between-person and within-person differences, the RI-CLPM has also been found to provide more accurate mapping of the direction of cross-lagged effects than classic cross-lagged analytic approaches (Hamaker et al., 2015). Finally, RI-CPLM provides better fitting models than traditional cross-lagged analyses due to the capture of trait-like stability through the inclusion of random intercepts (Mulder & Hamaker, 2020). Nonetheless, while the RI-CLPM approach parses the direction of effects between behavior and mental health, it does not demonstrate causal connections, which requires other experimental designs.
The study has several limitations. Firstly, the survey was offered only in English, limiting the participation of some populations. The survey also required consistent Internet/smartphone access, possibly excluding some lower-income individuals. We limited survey items to not overburden participants, and thus coverage of mental health was narrowed. Twenty-four individuals tested positive for SARS-CoV2 during the study, a rate of approximately 1% per week, which is in line with general population rates. Given the small size of this group, we were unable to draw contrasts between those with and without confirmed infection. The study occurred at a phase in the pandemic when most states had implemented strict social distancing policies, and we are thus unable to assess the impact of the ongoing relaxation of these policies. Finally, our daily measures of substance use were limited, particularly for substances beyond alcohol, where we collected data only on the number not quantity of substances used. This approach might inflate the impact of relatively light use of several substances and underestimate the impact of heavy use of one substance.
As noted in the introduction, we were interested in potential disparate impacts on racial/ethnic minorities and those with limited income; by design, we oversampled these groups. This sampling strategy could limit the generalizability of our findings to the general population. However, given that these populations are particularly vulnerable to COVID and the economic risks associated with the pandemic, we felt that it was important to oversample these groups. It is also important to note that the cross-lagged effects between behavior and mental health measures did not differ by racial/ethnic groups and income, suggesting that the findings may hold for the more general population. Finally, we note that a recent study of online recruitment resources found that Qualtrics panels came closest to a national probability sample on a majority of demographic variables and types of media consumption, outperforming other platforms [Mechanical Turk (MTurk) and Facebook] (Boas, Christenson, & Glick, 2020).
We did not find lagged effects to vary substantially by race and ethnicity, given that the fits of models that held lags constant or allowed them to vary by race/ethnicity did not differ substantially. Despite this null finding, we note disparities in rates of many other COVID domains, including the risk of SARS-CoV2 infection, hospitalization, and death in African-American and Hispanic populations during this pandemic (Price-Haywood, Burton, Fort, & Seoane, 2020; Webb Hooper, Napoles, & Perez-Stable, 2020). Additionally, diagnosis of neither a past depressive nor past anxiety disorder emerged as a significant moderator of the lagged effects, a contrast with prior studies finding associations between a history of mental illness and worse mental health outcomes during the pandemic (Alonzi, La Torre, & Silverstein, 2020; Kwong et al., 2020; O'Connor et al., 2020).
In conclusion, we find that a relatively simple behavior change – watching less news/media – may reduce subsequent adverse mental health outcomes. These findings move beyond prior reports of associations between watching the news on highly distressing topics and poor mental health by demonstrating a dynamic impact of news on mental health that unfolds over days within the individual (Gao et al., 2020; Ni et al., 2020; Olagoke et al., 2020; Pfefferbaum & North, 2020). The benefits of media as an information source and means of engagement in public discourse may be balanced against its possible deleterious impact on mental health. Our finding that levels of psychological striving were associated with subsequent decreases in news intake provides another possible point of intervention. Thus, interventions that promote facets of striving such as happiness and optimism could help break the vicious cycle between news/media consumption and COVID-related worry that we delineate.
Financial support
PS and LK received intramural NHGRI/NIMH awards from the National Human Genome Research Institute and the National Institute of Mental Health, as well as the National Institutes of Health's Office of Behavioral and Social Science Research.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S0033291721001896.
click here to view supplementary material
Data
The de-identified data that support the findings of this study will be made available upon request to the corresponding author.
Conflict of interest
None.
References
- Alonzi, S., La Torre, A., & Silverstein, M. W. (2020). The psychological impact of preexisting mental and physical health conditions during the COVID-19 pandemic. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S236–S238. doi: 10.1037/tra0000840 [DOI] [PubMed] [Google Scholar]
- Amsalem, D., Dixon, L. B., & Neria, Y. (2020). The coronavirus disease 2019 (COVID-19) outbreak and mental health: Current risks and recommended actions. JAMA Psychiatry, 78(1), 9–10. doi: 10.1001/jamapsychiatry.2020.1730 [DOI] [PubMed] [Google Scholar]
- Benjamini, Y., & Hochberg, Y. (1995). Controlling the false discovery rate – a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society Series B-Statistical Methodology, 57(1), 289–300. doi: 10.1111/j.2517-6161.1995.tb02031.x [DOI] [Google Scholar]
- Boas, T. C., Christenson, D. P., & Glick, D. M. (2020). Recruiting large online samples in the United States and India: Facebook, mechanical turk, and qualtrics. Political Science Research and Methods, 8(2), 232–250. doi: 10.1017/psrm.2018.28 [DOI] [Google Scholar]
- Brannick, M. T. (1995). Critical comment on applying covariance structure modeling. Journal of Organizational Behavior, 16(3), 201–213. doi: 10.1002/job.4030160303 [DOI] [Google Scholar]
- Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet (London, England), 395(10227), 912–920. doi: 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. (2020). Coping with stress. Your Health. Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html. [Google Scholar]
- Chen, F. F. (2007). Sensitivity of goodness of fit indexes to lack of measurement invariance. Structural Equation Modeling: A Multidisciplinary Journal, 14(3), 464–504. doi: 10.1080/10705510701301834 [DOI] [Google Scholar]
- Cheung, G. W., & Rensvold, R. B. (2002). Evaluating goodness-of-fit indexes for testing measurement invariance. Structural Equation Modeling: A Multidisciplinary Journal, 9(2), 233–255. doi: 10.1207/S15328007SEM0902_5 [DOI] [Google Scholar]
- Clay, J. M., & Parker, M. O. (2020). Alcohol use and misuse during the COVID-19 pandemic: A potential public health crisis? Lancet Public Health, 5(5), e259. doi: 10.1016/S2468-2667(20)30088-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick, K. M., Harris, C., & Drawve, G. (2020). Fear of COVID-19 and the mental health consequences in America. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S17–S21. doi: 10.1037/tra0000924 [DOI] [PubMed] [Google Scholar]
- Gao, J., Zheng, P., Jia, Y., Chen, H., Mao, Y., Chen, S., … Dai, J. (2020). Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE, 15(4), e0231924. doi: 10.1371/journal.pone.0231924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamaker, E. L., Kuiper, R. M., & Grasman, R. P. (2015). A critique of the cross-lagged panel model. Psychological Methods, 20(1), 102–116. doi: 10.1037/a0038889 [DOI] [PubMed] [Google Scholar]
- Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwong, A. S. F., Pearson, R. M., Adams, M. J., Northstone, K., Tilling, K., Smith, D., … Timpson, N. J. (2020). Mental health before and during the COVID-19 pandemic in two longitudinal UK population cohorts. British Journal of Psychiatry, 218(6), 1–10. doi: 10.1192/bjp.2020.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lerman, C., Trock, B., Rimer, B. K., Jepson, C., Brody, D., & Boyce, A. (1991). Psychological side effects of breast cancer screening. Health Psychology, 10(4), 259–267. doi: 10.1037//0278-6133.10.4.259 [DOI] [PubMed] [Google Scholar]
- Mulder, J. D., & Hamaker, E. L. (2020). Three extensions of the random intercept cross-lagged panel model. Structural Equation Modeling: A Multidisciplinary Journal, 28(4), 1–11. doi: 10.1080/10705511.2020.1784738. [DOI] [Google Scholar]
- Ni, M. Y., Yang, L., Leung, C. M. C., Li, N., Yao, X. I., Wang, Y., … Liao, Q. (2020). Mental health, risk factors, and social media use during the COVID-19 epidemic and cordon sanitaire among the community and health professionals in Wuhan, China: Cross-sectional survey. JMIR Mental Health, 7(5), e19009. doi: 10.2196/19009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor, R. C., Wetherall, K., Cleare, S., McClelland, H., Melson, A. J., Niedzwiedz, C. L., … Robb, K. A. (2020). Mental health and well-being during the COVID-19 pandemic: Longitudinal analyses of adults in the UK COVID-19 mental health & wellbeing study. British Journal of Psychiatry, 218(6), 1–8. doi: 10.1192/bjp.2020.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olagoke, A. A., Olagoke, O. O., & Hughes, A. M. (2020). Exposure to coronavirus news on mainstream media: The role of risk perceptions and depression. British Journal of Health Psychology, 25(4), 865–874. doi: 10.1111/bjhp.12427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ornell, F., Moura, H. F., Scherer, J. N., Pechansky, F., Kessler, F. H. P., & von Diemen, L. (2020). The COVID-19 pandemic and its impact on substance use: Implications for prevention and treatment. Psychiatry Research, 289, 113096. doi: 10.1016/j.psychres.2020.113096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum, B., & North, C. S. (2020). Mental health and the Covid-19 pandemic. New England Journal of Medicine, 383(6), 510–512. doi: 10.1056/NEJMp2008017 [DOI] [PubMed] [Google Scholar]
- Price-Haywood, E. G., Burton, J., Fort, D., & Seoane, L. (2020). Hospitalization and mortality among black patients and white patients with Covid-19. New England Journal of Medicine, 382(26), 2534–2543. doi: 10.1056/NEJMsa2011686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santini, Z. I., Jose, P. E., York Cornwell, E., Koyanagi, A., Nielsen, L., Hinrichsen, C., … Koushede, V. (2020). Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. The Lancet Public Health, 5(1), e62–e70. doi: 10.1016/s2468-2667(19)30230-0 [DOI] [PubMed] [Google Scholar]
- Sneed, R. S. (2020). Social and psychological consequences of the Covid-19 pandemic in African-American communities: Lessons from Michigan. Psychological Trauma: Theory, Research, Practice, and Policy, 12(5), 446–448. doi: 10.1037/tra0000881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Vindegaard, N., & Benros, M. E. (2020). COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain, Behavior, and Immunity, 89, 531–542. doi: doi: 10.1016/j.bbi.2020.05.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb Hooper, M., Napoles, A. M., & Perez-Stable, E. J. (2020). COVID-19 and racial/ethnic disparities. JAMA, 323(24), 2466–2467. doi: 10.1001/jama.2020.8598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (2020) Mental health and psychosocial considerations during the COVID-19 outbreak. Retrieved from https://www.who.int/publications/i/item/WHO-2019-nCoV-MentalHealth-2020.1.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S0033291721001896.
click here to view supplementary material
Data Availability Statement
The de-identified data that support the findings of this study will be made available upon request to the corresponding author.