Abstract
Introduction
The authors report a rare case of lag screw breakage in a patient treated using locking DHS with home-made trochanteric stabilizing plate (TSP) for pertrochanteric hip fracture.
Case presentation
A 67 year-old female was operated for pertrochanteric hip fracture with incompetent lateral wall using locking DHS with home-made TSP. At seven months postoperative, there was radiographic nonunion with breakage of the sliding lag screw. Patient was consequently scheduled for total hip replacement.
Discussion
Breakage of DHS lag screw has been attributed to multiple-cycle, low-stress fatigue failure associated with nonunion. Predisposing factors are: situation of the medial edge of the barrel at the level of the fracture site prohibiting fracture compression, and mechanical obstacle to the lag screw back sliding into the barrel. In our case, the use of handmade TSP interdicted lag screw back sliding and prevented fracture impaction which was already impaired by the location of the medial edge of the barrel at the fracture level. Additionally our fixation construct was very rigid because of the use of locking screws in the DHS side plate.
Conclusion
When DHS fixation is planned for unstable or potentially unstable trochanteric hip fracture the surgeon should be prepared by making available a TSP from the manufacturer in the operative room rather than improvising intra-operatively with handmade TSP; this augmentation device shouldn't interfere with lag screw back sliding. Furthermore the DHS barrel should ideally not impinge with the fracture site, and the use of locking screws in the DHS plate should be cautious.
Keywords: Pertrochanteric hip fractures, Intertrochanteric hip fractures, Dynamic hip screw (DHS) failure, Breakage of lag hip screw, Trochanteric stabilizing plate
Highlights
-
•
Our case highlights the modes of failure of DHS and describes the mechanism and risk factors for breakage of the lag screw.
-
•
Prevention of back sliding of the lag screw by the home-made TSP was a major risk factor for screw breakage.
-
•
Other factors are represented by the situation of the medial edge of the DHS barrel at the fracture site preventing any possible fracture impaction, and the use of locking screws in the DHS side plate which increased the rigidity of the construct and contributed concentrating the stress at the junction lag screw-barrel.
-
•
Our case is rare and is sparsely described in the literature.
1. Introduction
Dynamic hip screw (DHS) is one of the most popular devices utilized for the treatment of trochanteric hip fractures; this device may fail according to different modes such as cut-out of the lag screw, excessive back sliding of the lag screw, and pull-out of the side plate [1], [2], [3]. Failure usually occurs in unstable fracture patterns especially with lateral trochanteric wall incompetence and leads to excessive fracture impaction, varus displacement, femoral shaft medialization and limb shortening [4], [5]. Additional application of trochanter stabilizing plate (TSP) has been advised to prevent DHS failures; home-made TSP was suggested as promising alternative to the commercialized TSP by modifying pre-existing commercial plate for purposes of mechanical advantages, cost effectiveness and availability [6]. Failure by breakage of the sliding lag screw is an exceptional complication that has seldom been reported. We report herein a case of lag screw breakage in a patient treated using locking DHS associated with a home-made TSP for pertrochanteric hip fracture with incompetent lateral wall. Causes of this complication are discussed especially in the light of using locking DHS with home-made TSP system.
This case was reported in line with the SCARE criteria [7].
2. Case presentation
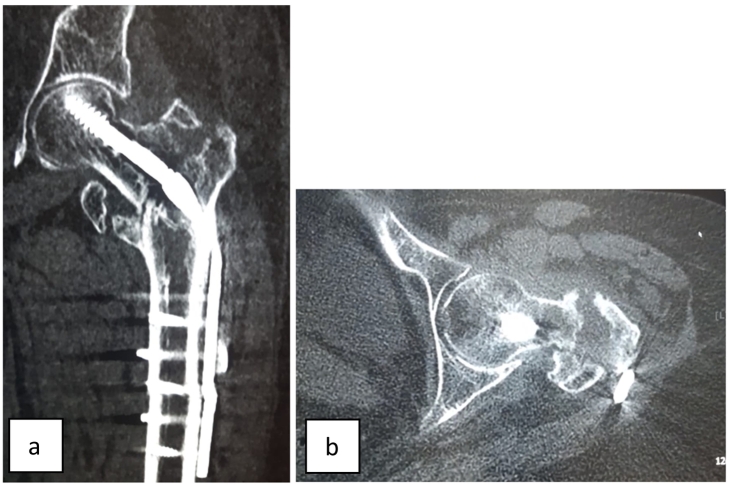
A 67 year-old female was admitted for pain and inability to bear weight on her left hip after falling at home. Radiographic assessment showed pertrochanteric left hip fracture with incompetent lateral wall (Fig. 1), type A2 according to recent modification of AO Classification [8]. Patient was operated 24 h after admission. Under spinal anesthesia with the use of orthopedic table, the procedure consisted on manipulative closed reduction followed by open internal fixation. A sliding lag screw of 95 mm length was first inserted in line with the central axis of the femoral neck on both AP and lateral views, and a locking six holes DHS (long barrel) was then adapted to the sliding screw and fixed to the lateral aspect of the proximal femur with one conventional cortical screw in the most distal hole followed by three locking screws in the adjacent proximal holes. Compression at the fracture site was achieved by using a compression screw for the sliding lag screw. During impaction of the DHS a non-displaced complete crack of the lateral trochanteric wall was identified starting at the entry site of the barrel. Use of additional stabilizing plate was decided to augment the lateral trochanteric wall as prevention of further complications related to its breach. A TSP was intra-operatively made by modifying a locking plate initially designed for medial tibial plateau fixation; it was contoured to the shape of the lateral aspect of the greater trochanter. The home-made TSP was superposed over the DHS as a modular proximal extension of the side plate and fixed to it with one conventional and one locking screw through the most proximal holes of the side plate just distal to the barrel. Post-operative radiographs showed good reduction of the hip fracture with satisfactory position of the hardware (Fig. 2). Patient was discharged home two days post-surgery and early toe-touch weight bearing was encouraged using walking frame. At two month follow-up the patient was comfortable and pain free; she was encouraged to start progressive weight bearing as tolerated. Absence of radiographic signs of bone healing was not considered alarming at that time. Next follow-ups were cancelled because of confinement related to the covid-19 pandemic. Patient presented back at seven month post-operative because of sudden onset of left hip pain. New radiographs demonstrated the presence of nonunion at the fracture site and breakage of the sliding lag screw at the junction with the barrel; the fracture reduction remained satisfactory and undisturbed (Fig. 3). These findings were confirmed by CT scan images (Fig. 4a, b). Patient was consequently scheduled for hardware removal and total hip replacement. Removal of the two plates with the lateral part of the broken lag screw was uneventful. Intra-operative findings confirmed the presence of nonunion. The TSP was obliterating the lateral orifice of the barrel preventing any possible back sliding of the lag screw; in addition its proximal part was perfectly contoured and firmly applied to the lateral aspect of the greater trochanter. The fixation-purchase of the threaded medial part of the broken lag screw into the femoral head was very solid; it was extracted as one unit with the femoral head.
Fig. 1.

Antero-posterior radiograph of the left hip showing pertrochanteric fracture with thin lateral wall, AO type A2.
Fig. 2.

Post-operative antero-posterior radiograph with satisfactory reduction and good position of the internal fixation hardware. Note the situation of the medial edge of the barrel at the level of the fracture site, the obliteration of the lateral orifice of the barrel by the TSP, and the well molding of the proximal part of the TSP to the lateral aspect of the greater trochanter.
Fig. 3.

Antero-posterior hip radiograph at 7 month follow-up demonstrating the nonunion of the fracture with breakage of the lag screw at the junction with the barrel.
Fig. 4.
(a) Coronal and (b) axial CT scan cuts confirming the nonunion and lag screw breakage.
3. Discussion
DHS is worldwide largely used for the treatment of extracapsular pertrochanteric and intertrochanteric hip fractures; it is a fixed-angle implant formed by a side plate incorporating a barrel aiming to lodge a large lag screw which in turn is able to slide into the barrel. When the lag screw slides back, its lateral end protrudes from the lateral orifice of the barrel; this allows controlled fracture impaction resulting in greater load transfer from the implant to the bone, and enhances bone healing [1], [9]. Failure of DHS fixation is usually attributed to osteoporosis, fracture nonunion, poor quality of reduction, incorrect positioning of the lag screw in the femoral neck and head, and unstable fracture patterns [10], [11]; it usually leads to varus displacement of the proximal segment, medialization of the distal segment, and shortening of the lower limb. Common modes of DHS failure are represented by the cut-out of the lag screw-barrel from the femoral head, excessive back sliding of the lag screw from the femoral head-neck through the lateral orifice of the barrel, and pull-out of the cortical screws from the proximal femoral shaft with loosening of the side plate. Failure by bending or breakage of the lag screw is very rare. An experimental biomechanical cadaveric study by Haynes et al. [9] reported two modes of failure for the lag screw under static loading: screw migration in soft bone and screw bending in hard bone; the bending failure mode occurred at the fracture line and was related to the high shear forces at this level. Progressive bending can be qualified as a plastic deformity of the lag screw that precedes its rupture. Breakage of the lag screw is an exceptional mode of failure in clinical setting with only a very few sporadic case reports in the literature [2], [3], [12], [13], [14], [15], [16]; it has been attributed to multiple-cycle, low-stress fatigue failure usually associated with nonunion [2], [12], [13], [14]; as the fracture remains unhealed, the implant is exposed to repeated long-term loading that ends up by exceeding the maximum limit of its resistance to breakage [14]. Arastu et al. [17] reported an additional exceptional mode of clinical failure: early bending of the lag screw at the junction with the barrel resulting from low-cycle, high-stress failure in opposition to the previous mode; it was attributed to multiple factors: poor reduction, good bone quality, and utilization of plate with short barrel and long lag screw (115 mm) inducing a long lever arm with increased bending forces at the junction screw-barrel. The situation of the medial edge of the barrel at the level of the fracture site was accused prohibiting fracture compression-impaction and contributing to nonunion, an important factor of lag screw breakage [14]; such situation may be overlooked during surgery and the surgeon may use a plate with inappropriate or unsuitable barrel length. However the use of DHS with short barrel is not recommended when the length of the lag screw is more than 85 mm [9], [18]: a relative long screw with short barrel increases the bending forces at the junction screw-barrel because of the extended lever arm. Furthermore, as the internal threaded portion of the lateral part of the lag screw -where the compression screw is inserted- is considered a weak point exposed to higher bending stress, Spivak et al. [13] recommended that this internal threaded portion of the lag screw must be seated within the barrel rather than at the screw-barrel junction or outside the barrel itself. Consequently, the surgeon may face a difficult dilemma in some situations according to the fracture pattern and the fracture line location: coupling between a plate of appropriate barrel length not impinging into the fracture site and a lag screw of adequate length without increasing the lever arm while its internal threaded part remains lodged into the body of the barrel. On the other hand, mechanical obstacle to back sliding of the lag screw into the barrel was also accused to cause stress concentration at the junction screw-barrel leading to fatigue breakage of the lag screw especially in presence of delayed union or nonunion [2].
For unstable pertrochanteric fractures the additional use of TSP with the DHS has been recommended to prevent postoperative mechanical complications [4], [5], [19]; the TSP is dotted with an oval hole that lines up with the lateral orifice of the DHS barrel to allow back sliding of the lag screw. Lee et al. [6] treated early cut-out of lag screw with a TSP added to DHS; they used a handmade TSP by modifying a pre-existing spoon-shape buttress plate which was matched to support the lateral aspect of the greater trochanter: an oval hole of 3 cm length and 1 cm wide was made into this plate to line up with the level of the lag screw of the DHS in order to allow uneventful back sliding of the lag screw during secondary controlled fracture impaction. In our case, the handmade plate was completely obliterating the lateral orifice of the barrel without any free chamber or space to allow lag screw back sliding and fracture impaction. The lag screw was trapped between two points: the medial part of solid fixation-purchase of the lag screw threads into the bone of the femoral head as confirmed during the revision surgery, and the lateral part which was seized and hold into the barrel without any possible slide back because of the obstacle made by the TSP at the lateral orifice of the barrel. In fact, the fracture site initially located at the junction screw-barrel was “trapped” between two areas of solid fixation: a proximal area represented by the excellent holding of the lag screw in the femoral head as pre-mentioned, and a distal area represented by the rigid fixation of the side plate of the DHS to the femoral shaft because of the use of locking head screws. Actually the use of locking screws has made the device very rigid and not only the motion of lag screw was prevented by the augmented lateral plate hindering the sliding mechanism but any possible movement of the DHS plate in the shaft was also hampered because of the use of locking head screws. Furthermore the location of the medial border of the barrel at the fracture site along with the high riding situation of the TSP which was “pushing” on the proximal femoral segment also contributed preventing any secondary impaction at the fracture site and participated inducing nonunion. In addition, pull-out of the whole construct was very unlikely because of the relative good bone quality and the use of locking DHS system.
We believe this complex mechanical situation has resulted in fracture nonunion in addition to multiple-cycle, low-stress concentration at the junction screw-barrel that finally induced fatigue failure of the lag screw itself.
4. Conclusion
In conclusion, the barrel of DHS should not impinge with the fracture site of trochanteric hip fracture, and the lag screw should be able to slide back without any obstacle into the barrel of the DHS; utilization of TSP to increase stability in unstable fractures should not interfere with the back sliding mechanism of the lag screw; caution should be made so as handmade TSP should not obliterate the lateral orifice of the DHS barrel. Finally, we recommend that the decision to use a DHS plate for fixation of unstable or potentially unstable trochanteric fracture -because of thin trochanteric lateral wall- should be made after deep deliberation; in such condition the surgeon should be prepared to augment the construct with a lateral trochanteric stabilizing plate from the manufacturer rather than improvising with a handmade plate.
5. Patient perspective
The patient well understood and assimilated the complication of the index surgery; she consented for revision surgery with total hip replacement and expressed her final satisfaction from the end result.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
This study is exempt from ethical approval.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Writing the paper: Ali Hassan Chamseddine, Mohammad Boushnak, Abbas Dib
Data collection: Hassan Wardani, Mohammad Boushnak.
Supervision: Ali Hassan Chamseddine.
Registration of research studies
N/A.
Guarantor
Dr. Ali Hassan Chamseddine.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
The authors declare that they have no conflict of interest.
References
- 1.Chirodian N., Arch B., Parker M.J. Sliding hip screw fixation of trochanteric hip fractures: outcome of 1024 procedures. Injury. 2005;36:793–800. doi: 10.1016/j.injury.2005.01.017. [DOI] [PubMed] [Google Scholar]
- 2.Jakobsen B.W. Breakage of a sliding hip screw. A case report. Acta Orthop. Scand. 1987;58:292–293. doi: 10.3109/17453678709146490. [DOI] [PubMed] [Google Scholar]
- 3.Amis A.A., Bromage J.D., Larvin M. Fatigue fracture of a femoral sliding compression screw–plate device after bone union. Biomaterials. 1987;8:153–157. doi: 10.1016/0142-9612(87)90106-2. [DOI] [PubMed] [Google Scholar]
- 4.Babst R., Renner N., Biedermann M., Rosso R., Heberer M., Harder F., Regazzoni P. Clinical results using the trochanter stabilizing plate (TSP): the modular extension of the dynamic hip screw (DHS) for internal fixation of selected unstable intertrochanteric fractures. J. Orthop. Trauma. 1998;12:392–393. doi: 10.1097/00005131-199808000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Gupta R.K., Sangwan K., Kamboj P., Punia S.S., Walecha P. Unstable trochanteric fractures: the role of lateral wall reconstruction. Int. Orthop. 2010;34:125–129. doi: 10.1007/s00264-009-0744-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee P.C., Yu S.W., Hsieh P.H., Chuang T.Y., Tai C.L., Shih C.H. Treatment of early cut-out of a lag screw using a trochanter supporting plate. Arch. Orthop. Trauma Surg. 2004;124:119–122. doi: 10.1007/s00402-003-0607-8. [DOI] [PubMed] [Google Scholar]
- 7.for the SCARE Group. Agha R.A., Franchi T., Sohrabi C., Mathew G. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 8.Kellam J.F., Meinberg E.G., Agel J., Karam M.D., Roberts C.S. Fracture and dislocation classification compendium-2018. international comprehensive classification of fractures and dislocations committee. J. Orthop. Trauma. 2018;32(Supp 1):S34. doi: 10.1097/BOT.0000000000001063. [DOI] [PubMed] [Google Scholar]
- 9.Haynes R.C., Pöll R.G., Miles A.W., Weston R.B. An experimental study of the failure modes of the Gama locking nail and AO dynamic hip screw under static loading: a cadaveric study. Med. Eng. Phys. 1997;19:446–453. doi: 10.1016/s1350-4533(97)00003-9. [DOI] [PubMed] [Google Scholar]
- 10.Gundle R., Gargan M.F., Simpson A.H. How to minimize failures of fixation of unstable intertrochanteric fractures. Injury. 1995;26:611–614. doi: 10.1016/0020-1383(95)00125-S. [DOI] [PubMed] [Google Scholar]
- 11.Kim W.Y., Han C.H., Park J.I., Kim J.Y. Failure of intertrochanteric fracture fixation with a dynamic hip screw in relation to pre-operative fracture stability and osteoporosis. Int. Orthop. 2001;25:360–362. doi: 10.1007/s002640100287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khanna A., Parker M. Rare mode of dynamic hip screw failure. Hip Int. 2008;18:239–241. doi: 10.5301/hip.2008.5373. [DOI] [PubMed] [Google Scholar]
- 13.Spivak J.M., Zuckerman J.D., Kummer F.J., Frankel V.H. Fatigue failure of the sliding screw in hip fracture fixation: a report of three cases. J. Orthop. Trauma. 1991;5:325–331. doi: 10.1097/00005131-199109000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Necas L., Hrubina M., Cibula Z., Behounek J., Krivanek S., Horak Z. Fatigue failure of the sliding hip screw – clinical and biomechanical analysis. Comput. Methods Biomech. Biomed. Eng. 2017 doi: 10.1080/10255842.2017.1363192. Published online 09 August 2017. [DOI] [PubMed] [Google Scholar]
- 15.Manicom O., Karoubi M., Mseddi M., Demoura A., Hernigou P. Fracture de la Vis cervicale d’une Vis-plaque à glissement: À propos d’un cas à 1,5 an de recul. Rev. Chir. Orthop. 2006;92:602–605. doi: 10.1016/S0035-1040(06)75919-0. [DOI] [PubMed] [Google Scholar]
- 16.Hrubina M., Skotak M., Krumpl O., Mika P., Letocha J. Osteosynthetic material breakage in patient treated with DHS for proximal femoral fracture. Rozhl. Chir. 2013;91:146–150. [PubMed] [Google Scholar]
- 17.Arastu M.H., Phillips L., Duffy P. An unusual failure of a sliding hip screw in the immediate post-operative period. Inj. Extra. 2013;44:23–27. doi: 10.1016/j.injury.2012.10.011. [DOI] [Google Scholar]
- 18.Simpson A.H., Varty K., Dodd C.A. Sliding hip screws: modes of failure. Injury. 1989;20:227–231. doi: 10.1016/0020-1383(89)90120-4. [DOI] [PubMed] [Google Scholar]
- 19.Hsu C.E., Chiu Y.C., Tsai S.H., Lin T.C., Lee M.H., Huang K.C. Trochanter stabilising plate improves treatment outcomes in AO/OTA 31–A2 intertrochanteric fractures with critical thin femoral lateral walls. Injury. 2015;46:1047–1053. doi: 10.1016/j.injury.2015.03.007. [DOI] [PubMed] [Google Scholar]