Abstract
Purpose
The prevalence of non-specific posterior neck pain (NPNP) has been increasing yearly. There are several treatments for NPNP, but in this review, we will focus on thread-embedded acupuncture (TEA). TEA is used in the Republic of Korea, Taiwan, and China for managing musculoskeletal diseases, obesity, and sequelae of facial palsy. However, there is insufficient evidence on its effectiveness and safety. This study aims to assess the efficacy and safety of TEA for NPNP.
Methods
We will search the following nine electronic databases, from their inception to May 2020: MEDLINE, Embase, Cochrane Central Register of Controlled Trials, China National Knowledge Infrastructure, Citation Information by the National Information infrastructure, Korean Studies Information Service System, National Digital Science Library, Oriental Medicine Advanced Searching Integrated System, and Research Information Service System. Only randomized controlled trials of TEA for NPNP will be included. The methodological quality of the included trials will be assessed using the Cochrane risk-of bias tool. To conduct the meta-analysis, the risk ratio and mean difference with the 95% confidence interval will be used. Sensitivity analyses will be conducted based on this protocol.
Results
The results of this study will be submitted to a peer-reviewed journal for publication.
Conclusion
The results of this study would provide the evidence of whether TEA can be effective for treating NPNP.
Registration Number
PROSPERO CRD42020188346.
Keywords: posterior neck pain, polydioxanone, randomized controlled trials, systematic review
Introduction
There are several risk factors for neck pain, including trauma, previous neck pain history, sports and work injuries, infection, neoplasm, and herniated disc.1 According to the Health Insurance Review and Assessment service in the Republic of Korea, the number of patients with neck pain has been increasing yearly. According to previous study, 22–70% people experience neck pain at least once during their life. The prevalence of non-specific posterior neck pain (NPNP) increases with age.2 Recently, the prevalence of NPNP has been increasing because of the increased use of computers and smart-phones.3 Transcutaneous electrical nerve stimulation, spinal manipulation and pain control medication can be used for treating NPNP.4
Neck pain can be diagnosed based on the presence of accompanying symptoms, the duration of pain, and range of motion.5 Specific neck pain can be confirmed using imaging modalities such as magnetic resonance imaging, electromyography, or explorative therapeutic approaches such as nerve root blocks, and epidural injections. However, NPNP has no conclusive pain source and can accompany neck pain, upper extremity pain, or headache. In addition, it is not associated with apparent radiculopathies or myelopathies.6,7
Thread-embedded acupuncture (TEA) has been used for the treatment of musculoskeletal pain,8 obesity,9 and sequelae of facial palsy10 in East Asian countries. It is a special method of treatment involving acupuncture, in which polydioxanone is injected into the subcutaneous or muscle layer at specific acupoints, which provides long-lasting pain control effect compared to dry needling.11,12 The pain control mechanism of TEA is medicated via the Sig-1R receptor and mitogen-activated protein kinase (MAPK) or spinal serotonin 1A receptor, and the GluN1 subunit of N-methyl-d-aspartate receptor (NMDA). As TEA inhibits MAPK p38 in the spinal cord, it can also alleviate pain induced by complete Freund’s adjuvant’s inflammatory reaction.13 In a rat model, TEA controlled the activation of the GluN1 subunit of the NMDA receptor and blocked the Ca++ -dependent channels involved in inflammatory pain reaction.14
Although several randomized control trials (RCTs) have shown that TEA has a more effective and long-lasting therapeutic potential than sham thread, conventional analgesics, or other treatments,15,16 there is limited evidence on the therapeutic effect of TEA in NPNP.8 Therefore, this study aims to evaluate the effectiveness of TEA compared to that of other treatment methods in the treatment of NPNP. We will conduct a systematic review and meta-analysis to establish the basis for using TEA in the treatment of NPNP.
Materials and Methods
Study Registration
The protocol of this systematic review has been designed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols 2020.17 The study has been registered in the PROSPERO (CRD:42,020,188,346; http://www.crd.york.ac.uk/PROSPERO).
Ethical Review
Ethical approval is not necessary because patient data will not be included in the paper.
Eligibility Criteria
Only RCTs comparing TEA with conventional medicine treatments, traditional acupuncture, or sham TEA will be included in our systematic review. Observational studies, cohort studies, case reports, case series, quasi-RCTs, and animal studies will be excluded. We will also evaluate whether there is a risk of bias in each RCT. Furthermore, if inappropriate randomization is used in a RCT, it will be excluded from this systematic review.
Types of Participants
It is difficult to diagnose NPNP because it excludes all causes of specific neck pain. Therefore, we only target participants diagnosed with non-specific neck pain by expert practitioners. In particular, we will target patients with neck pain for ≥ 3 months without substantial relief with conservative treatment.
Inclusion Criteria
- Participants experiencing neck pain for ≥ 3 months.
- Participants diagnosed with NPNP by expert practitioners.
- Participants with radiculopathy or myelopathy without clear basis for the specific diagnosis.
- Participants aged in 18–65 years.
Exclusion Criteria
- Participants with posterior neck pain diagnosed with diagnostic tools or pain control injections.
-Participants with a definite diagnosis (eg cervical disc herniation, tumor, infection, and ossification of the posterior longitudinal ligament (OPLL)).
- Participants aged < 18 years or > 65 years.
- Pregnancy.
Types of Interventions and Comparisons
Articles evaluating TEA as intervention will be included. In these studies, the effects of TEA will be compared with those of other treatments (conventional treatment [including treatment with non-steroidal anti-inflammatory drugs (NSAIDs), serotonin uptake inhibitors, physical therapy, and education], sham TEA, or dry needling) or a simple treatment. Sham TEA is the same and is limited to those in which polydioxanone is not inserted into the body. Both TEA alone and combination treatment with TEA and conventional therapy will be included as interventions. All TEA interventions should be performed based on acupoint and meridian theories.
Outcome Measures
Pain intensity and functional status/disability will be the primary outcome. Quality of life and adverse events will be the secondary outcome. Pain intensity will be evaluated using the visual analogue scale (VAS), numeric rating scale (NRS), and neck pain and disability scale (NPDS). Functional status/disabilitywill be measured using the neck disability index (NDI). Quality of life will be evaluated using EuroQoL-5 dimension. Further, the adverse events reported in each RCT will be described.
Search Methods
Information Sources and Retrieval Strategy
We will search the following electronic database from their inception to May 2020: MEDLINE, Embase, Cochrane, China National Knowledge Infrastructure, Citation Information by the National Information Infrastructure, Korean Studies Information Service System, National Digital Science Library, Oriental Medicine Advanced Searching Integrated System, and Research Information Service System. No language restrictions were placed on the search of articles.
The following search terms will be used in our article: “Thread”, “Catgut”, “Needle”, “Acupuncture”, “Polydioxanone”, “Embed”, “Implantation”, “Posterior neck pain”, “Cervicalgia”, and “Randomized controlled trials”. For the Korean, Chinese, and Japanese databases, the aforementioned search terms will be translated into Korean, Chinese, and Japanese, respectively. Table 1–9 summarize the search strategy of each retrieval engine.
Table 1.
MEDLINE Search Strategy
| #1 | Posterior neck pain[MeSH] |
| #2 | Cervicalgia[MeSH] |
| #3 | Catgut[TIAB] OR Thread[TIAB] OR Polydioxanone[TIAB] OR Needle[TIAB] OR Acupuncture[TIAB] |
| #4 | Implantation[TIAB] OR Embed[TIAB] |
| #5 | Randomized controlled trial[Publication type] |
| #6 | Controlled clinical trial[Publication type] |
| #7 | Randomly[Publication type] |
| #8 | #1 OR #2 |
| #9 | #3 AND #4 |
| #10 | #5 OR #6 OR #7 |
| #11 | #8 AND #9 AND #10 |
Table 2.
Embase Search Strategy
| #1 | “Posterior neck pain”/exp |
| #2 | “Cervicalgia”/exp |
| #3 | ((Neck* or Cervical*) and pain*): ti, ab, kw |
| #4 | Implantation OR Embed: de, ab, ti |
| #5 | Catgut OR Thread OR Polydioxanone OR Needle OR Acupuncture: de, ab, ti |
| #6 | “Crossover procedure”:de OR “Double-blind procedure”:de OR “Randomized controlled trial”:de OR “Single-blind procedure”:de OR (Random* OR Factorial* OR Crossover* OR Cross NEXT/1 over* OR Placebo* OR doubl* NEAR/1 blind* OR singl* NEAR/1 blind* OR Assign* OR Allocat* OR Volunteer*):de, ab, ti |
| #7 | #1 OR #2 OR #3 |
| #8 | #4 AND #5 |
| #9 | #7 AND #8 |
| #10 | #6 AND #9 |
Table 3.
Cochrane Search Strategy
| #1 | Mesh descriptor: [Cervicalgia] explode all trees |
| #2 | MeSH descriptor: [Post neck pain] explode all trees |
| #3 | ((Neck* or cervical*) and pain*):ti, ab, kw |
| #4 | Catgut OR Thread OR Polydioxanone OR Needle OR Acupuncture:ti, ab, kw |
| #5 | Implantation OR Embed:ti, ab, kw |
| #6 | #1 OR #2 OR #3 |
| #7 | #4 AND #5 |
| #8 | #6 AND #7 |
Table 4.
China National Knowledge Infrastructure Search Strategy
| #1 | SU=(“Cervicalgia”+“Posterior neck pain”) AND SU=(Randomized) AND SU=(Catgut +Thread+Polydioxanone+Needle+Acupuncture) AND SU=(Implantation+Embed) |
| #2 | AB=(“Cervicalgia”+“Posterior neck pain”) AND AB=(Randomized) AND AB=(Catgut +Thread+Polydioxanone+Needle+Acupuncture) AND AB=(Implantation+Embed) |
| #3 | TI=(“Cervicalgia”+“Posterior neck pain”) AND TI=(Randomized) AND TI=(Catgut +Thread+Polydioxanone+Needle+Acupuncture) AND TI=(Implantation+Embed) |
Table 5.
Citation Information by National Information Infrastructure Search Strategy
| #1 | (“Cervicalgia” OR “Posterior neck pain”) |
| #2 | (Catgut OR Thread OR Polydioxanone OR Needle OR Acupuncture) |
| #3 | (Implantation OR Embed) |
| #4 | #2 AND #3 |
| #5 | #1 AND #4 |
Table 6.
Korean Studies Information Service System Search Strategy
| #1 | (“Cervicalgia” OR “Posterior neck pain”) |
| #2 | (Catgut OR Thread OR Polydioxanone OR Needle OR Acupuncture) |
| #3 | (Implantation OR Embed) |
| #4 | #2 AND #3 |
| #5 | #1 AND #4 |
Table 7.
National Digital Science Library Search Strategy
| #1 | (“Cervicalgia” OR “Posterior neck pain”) |
| #2 | (Catgut OR Thread OR Polydioxanone OR Needle OR Acupuncture) |
| #3 | (Implantation OR Embed) |
| #4 | #2 AND #3 |
| #5 | #1 AND #4 |
Table 8.
Oriental Medicine Advanced Searching Integrated System Search Strategy
| #1 | (“Cervicalgia” OR “Posterior neck pain”) |
| #2 | (Catgut OR Thread OR Polydioxanone OR Needle OR Acupuncture) |
| #3 | (Implantation OR Embed) |
| #4 | #2 AND #3 |
| #5 | #1 AND #4 |
Table 9.
Research Information Service System Search Strategy
| #1 | (“Cervicalgia” OR “Posterior neck pain”) |
| #2 | (Catgut OR Thread OR Polydioxanone OR Needle OR Acupuncture) |
| #3 | (Implantation OR Embed) |
| #4 | #2 AND #3 |
| #5 | #1 AND #4 |
Analysis
Study Selection
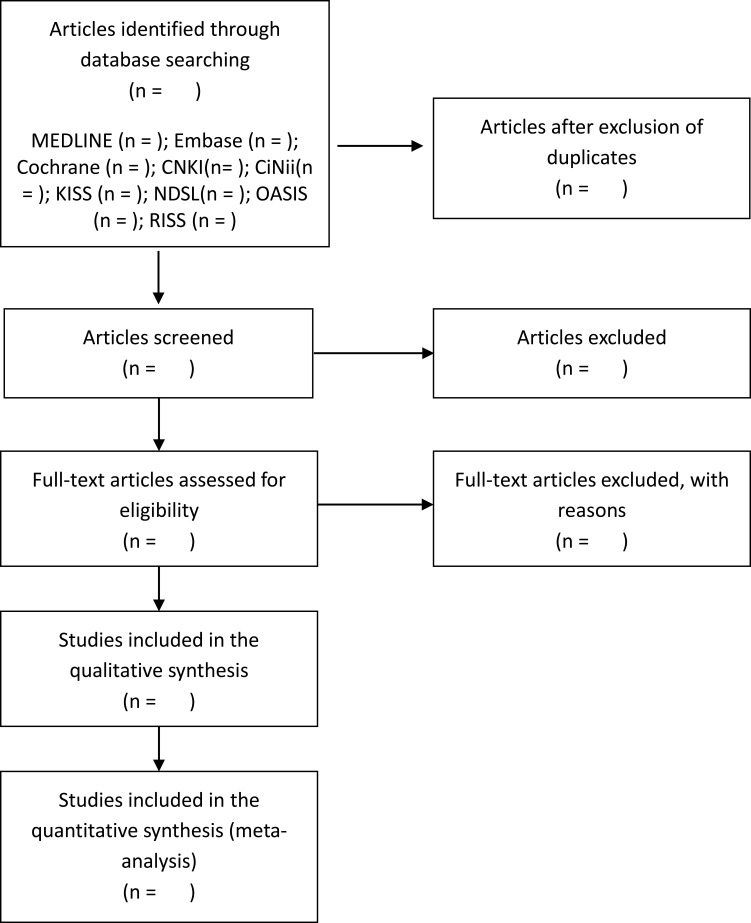
Two reviewers (JY and YC) will screen the titles and abstracts of all extracted articles to exclude duplicate and irrelevant studies. The full text of the remaining articles will be assessed for their suitability based on our inclusion criteria. Disagreements between reviewers will be resolved by consensus. If the difference of opinion is not resolved, a third reviewer (BK) will make the final decision. Figure 1 shows the algorithm for study selection.
Figure 1.
Flow chart of the selection process according to the Preferred Reporting Items for Systematic Reviews and Meta-analysis.
Notes: Adapted from Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71.24. Creative Commons license and disclaimer available from: http://creativecommons.org/licenses/by/4.0/legalcode.17
Abbreviations: KISS, Korean Studies Information Service System; RISS, Research Information Service System; OASIS, Oriental Medicine Advanced Searching Integrated System; CNKI, China National Knowledge Infrastructure; CiNii, Citation Information by the National Information Infrastructure.
Data Extraction and Management
After conducting the search procedure, two researchers (JY and YC) will independently complete the screening procedure. First, overlapping studies will be excluded. Subsequently, the remaining studies will be excluded based on our assessments of the abstract, title, and full text. The selected data will include study characters such as: (a) general information (publication year, title, authors, journal name, and country), (b) study characteristics (study design, sample size, randomization method, and blinding method), (c) participant characteristics (age, sex, race, diagnostic characteristics, and intensity and duration of symptoms) (d) intervention (type of TEA/control intervention, treatment details and duration, and intervention frequency and dropout).
Assessment of Reporting Quality and Risk of Bias
Two reviewers (JY and YC) will independently assess the risk of bias using the Cochrane Collaboration risk-of-bias tool in the Cochrane handbook. This tool includes six domains: random sequence generation, allocation concealment, blinding of participants, blinding of outcome assessment, selective outcome reporting, and incomplete outcome data. We will judge each domain as “low risk”, “high risk”, or “unclear risk”.
Measures of Treatment Effect
We will measure therapeutic effect of TEA as the mean difference (MD) or standardized mean difference (SMD). MD with 95% confidence interval (CI) will be used to assess the effect of continuous data (VAS, NPDS, NRS, and other outcome measures). SMD will be used to estimate the study outcome if different outcome scales or tools are used in articles. The risk ratio (RR) with 95% CI will be used to assess the effect of dichotomous data.
Managing Missing Data
To acquire missing data, we will contact the corresponding authors of the studies. If we do not get any response, we will include only the available data.
Assessment of a Reporting Bias
We will assess reporting bias using a funnel plot if the number of studies used in the analysis is sufficient.
Assessment of a Heterogeneity
We will assess heterogeneity across studies using the I2 value derived from the χ2 test. The I2 statistic will be calculated to assess inconsistencies in the results of the included studies. To assess substantial heterogeneity, we will explore possible causes by conducting sensitivity and subgroup analyses.
Data Synthesis and Grading of Quality of Evidence
We will use the Review Manager (REVMAN, The Nordic Cochrane Center, The Cochrane Collaboration, REVMAN program version 5.3; Copenhagen; 2014) to conduct a meta-analysis and calculate the RR or MD. The 95% CI will be used to calculate the pooled estimate of the effect size in a random-effects or fixed-effects model. If we cannot conduct a meta-analysis because of a lack of clinical trials, we will present the effect size and 95% CI of all outcomes in each clinical study and describe the important results in the Discussion section of our article. The development and Evaluation (GRADE) approach will be used to summarize the meta-analysis and grade the strength of evidence.18
Sensitivity Analysis
We will conduct sensitivity analysis to identify the robustness of the results. The methodological quality will be assessed using the risk-of-bias tool. According to this procedure, low-quality trials will be excluded and a second meta-analysis will be conducted.
Discussion
As NPNP is the second most common musculoskeletal disorder after chronic low back pain, it can be a major health and economic burden for many people.19 NPNP affects 30–50% adults annually and it is refractory to treatment.20 Therefore, management of NPNP is difficult for practitioners worldwide.
In traditional medicine, many studies on acupuncture treatment for NPNP have been conducted. According to some studies, acupuncture can be considered a long-lasting and cost-effective treatment.21,22 In recent years, several modern treatment modalities, such fire needling,23 TEA, pharmacoacupuncture,24 and acupotomy3 have been combined with traditional acupuncture for the treatment of NPNP.
In particular, TEA uses a combination of a guide needle and polydioxanone thread. The guide needle is removed after insertion in the muscular or subcutaneous layer, while the polydioxanone thread is retained at the acupoints. The polydioxanone thread dissolves over time. Therefore, there is no need to perform the cumbersome process of thread removal.8 The possible side effects of TEA include bruising, bleeding, redness and pain, and foreign body sensation. To prevent possible infections after TEA, the clean needle technique using protective gears, such as latex glove, should be employed.25
Several studies have been conducted to prove the safety and effectiveness of TEA. Kim et al15 and Chu et al16 conducted RCTs and reported that TEA was not associated with serious side effects of TEA and that it significantly improved the quality of life of patients. Kim et al26 reported that there was a significant improvement of pain relief in TEA compared to that with conventional physical therapy. However, they reported one case of pneumothorax. Since rare side effects such as pneumothorax are often reported, it is important for traditional medicine practitioners to accumulate more high-level evidence of safety and effectiveness of TEA.
The purpose of our study is to evaluate the efficacy and safety of TEA for NPNP and provide clinical evidence for traditional practitioners using TEA in clinical practice. This review may also be helpful to conventional medicine practitioners who are seeking information about TEA.
Funding Statement
This study is supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI20C1405) and by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (No. NRF-2020R1F1A1071584).
Abbreviations
TEA, thread-embedded acupuncture; MAPK, mitogen-activated protein kinase; NMDA, N-methyl-d-aspartate receptor; RCT, randomized controlled trial; MD, mean difference; SMD, standardized mean difference; RR, risk ratio; CI, confidence interval; VAS, visual analog scale; GRADE, Grades of Recommendation, Assessment, Development, and Evaluation; NRS, numeric rating scale; NPDS, neck pain and disability scale.
Author Contributions
All authors made a significant contribution to this review, including conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas. All authors took part in drafting, revising, and critically reviewing the article. The final version to be published has been approved by all authors, and they have agreed on the journal to which the article has been submitted as well as agreed to be accountable for all aspects of the work. Jun-Yeon Kim and Byung-Kwan Seo equally contributed to this article as first author.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Cohen SP, Hooten WM. Advances in the diagnosis and management of neck pain. BMJ. 2017;358:j3221. [DOI] [PubMed] [Google Scholar]
- 2.Yang C-S, Kim I-T, Kim Y-E, Kim B-Y, Seo B-N, Park J-E. A systematic review of acupuncture-moxibustion treatments for nonspecific chronic neck pain. Korean J Acupunct. 2017;34(4):209–230. doi: 10.14406/acu.2017.026 [DOI] [Google Scholar]
- 3.Jun S, Lee JH, Gong HM, et al. Efficacy and safety of combined treatment of miniscalpel acupuncture and non-steroidal anti-inflammatory drugs: an assessor-blinded randomized controlled pilot study. Trials. 2018;19(1):1–7. doi: 10.1186/s13063-017-2418-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peters R, Schmitt MA, Verhagen AP, Pool-Goudzwaard AL, Mutsaers J-H, Koes BW. Comparing the range of musculoskeletal therapies applied by physical therapists with postgraduate qualifications in manual therapy in patients with non-specific neck pain with international guidelines and recommendations: an observational study. Musculoskelet Sci Pract. 2020;46:102069. doi: 10.1016/j.msksp.2019.102069 [DOI] [PubMed] [Google Scholar]
- 5.Childs JD, Cleland JA, Elliott JM, et al. Neck pain: clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopaedic section of the American physical therapy association. J Orthop Sport Phys Ther. 2008;38(9):A1–A34. doi: 10.2519/jospt.2008.0303 [DOI] [PubMed] [Google Scholar]
- 6.Seo B-K, Lee J-H, Kim P-K, Baek Y-H, Jo D-J, Lee S. Bee venom acupuncture, NSAIDs or combined treatment for chronic neck pain: study protocol for a randomized, assessor-blind trial. Trials. 2014;15(1):1–8. doi: 10.1186/1745-6215-15-132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gross A, Forget M, St George K, et al. Patient education for neck pain. Cochrane Database Syst Rev. 2012;3. doi: 10.1002/14651858.CD005106.pub4 [DOI] [PubMed] [Google Scholar]
- 8.Cho Y, Lee S, Kim J, Kang JW, Lee J-D. Thread embedding acupuncture for musculoskeletal pain: a systematic review and meta-analysis protocol. BMJ Open. 2018;8(1):e015461. doi: 10.1136/bmjopen-2016-015461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garcia-Vivas JM, Galaviz-Hernandez C, Fernandez-Retana J, et al. Transcriptomic profiling of adipose tissue in obese women in response to acupuncture catgut embedding therapy with moxibustion. J Altern Complement Med. 2016;22(8):658–668. doi: 10.1089/acm.2015.0200 [DOI] [PubMed] [Google Scholar]
- 10.Park YC, Goo BH, Lee CH, et al. Clinical effectiveness of thread-embedding acupuncture in the treatment of bell’s palsy sequelae: a randomized, patient-assessor-blinded, controlled, clinical trial. Eur J Integr Med. 2020;37:101113. doi: 10.1016/j.eujim.2020.101113 [DOI] [Google Scholar]
- 11.Shin HJ, Lee D-J, Kwon K, et al. The success of thread-embedding therapy in generating hair re-growth in mice points to its possibly having a similar effect in humans. J Pharmacopunct. 2015;18(4):20. doi: 10.3831/KPI.2015.18.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park JM, Lee JS, Lee EY, Du RJ, Jo NY, Lee CK. A systematic review on thread embedding therapy of knee osteoarthritis. Korean J Acupunct. 2018;35(4):159–165. doi: 10.14406/acu.2018.028 [DOI] [Google Scholar]
- 13.Du K, Wang X, Chi L, Li W. Role of sigma-1 receptor/p38 MAPK inhibition in acupoint catgut embedding–mediated analgesic effects in complete freund’s adjuvant-induced inflammatory pain. Anesth Analg. 2017;125(2):662–669. doi: 10.1213/ANE.0000000000001857 [DOI] [PubMed] [Google Scholar]
- 14.Cui W-Q, Sun W-S, Xu F, et al. Spinal serotonin 1A receptor contributes to the analgesia of acupoint catgut embedding by inhibiting phosphorylation of the N-methyl-d-aspartate receptor GluN1 subunit in complete freund’s adjuvant-induced inflammatory pain in rats. J Pain. 2019;20(1):16–e1. doi: 10.1016/j.jpain.2018.07.011 [DOI] [PubMed] [Google Scholar]
- 15.Kim E, Kim Y-S, Kim Y Il, et al. Effectiveness and safety of polydioxanone thread-embedding acupuncture as an adjunctive therapy for patients with chronic nonspecific neck pain: a randomized controlled trial. J Altern Complement Med. 2019;25(4):417–426. doi: 10.1089/acm.2018.0228 [DOI] [PubMed] [Google Scholar]
- 16.Chu Y-X, Cui W-Q, Xu F, et al. Acupoint embedding of polyglactin 910 sutures in patients with chronic pain due to cervical spondylotic radiculopathy: a multicenter, randomized, controlled clinical trial. Evid Based Complement Altern Med. 2018;2018:1–11. doi: 10.1155/2018/3465897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Higgins JPT, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions. John Wiley & Sons; 2019. [Google Scholar]
- 19.Ferrari R, Russell AS. Neck pain. Best Pract Res Clin Rheumatol. 2003;17(1):57–70. doi: 10.1016/S1521-6942(02)00097-9 [DOI] [PubMed] [Google Scholar]
- 20.Goode AP, Freburger J, Carey T. Prevalence, practice patterns, and evidence for chronic neck pain. J Altern Complement Med. 2010;62(11):1594–1601. doi: 10.1002/acr.20270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Witt CM, Jena S, Brinkhaus B, Liecker B, Wegscheider K, Willich SN. Acupuncture for patients with chronic neck pain. Pain. 2006;125(1):98–106. doi: 10.1016/j.pain.2006.05.013 [DOI] [PubMed] [Google Scholar]
- 22.Willich SN, Reinhold T, Selim D, Jena S, Brinkhaus B, Witt CM. Cost-effectiveness of acupuncture treatment in patients with chronic neck pain. Pain. 2006;125(1):107–113. doi: 10.1016/j.pain.2006.06.006 [DOI] [PubMed] [Google Scholar]
- 23.Zhou J, Li X, Zhao J, Wang L, Lei W, Yan Y. Treatment of 30 patients with cervical spondylotic radiculopathy by acupuncture plus warming-needle moxibustion: a randomized controlled trial. World J Acupunct Moxibustion. 2014;24(4):24–28. doi: 10.1016/S1003-5257(15)60023-X [DOI] [Google Scholar]
- 24.Kim Y-J, Kim T-R, Woo C-H, Shin B-C. Comparative effectiveness of Hwangryunhaedok-tang pharmacopuncture, essential bee venom pharmacopuncture and Jungsongouhyul pharmacopuncture for cervical pain caused by traffic accidents: a retrospective observational study. J Korean Med Rehabil. 2018;28(2):83–89. doi: 10.18325/jkmr.2018.28.2.83 [DOI] [Google Scholar]
- 25.Yun Y-H, Son J-W, Ko S-G, Choi I-H. Disinfection, sterilization and aseptic technique for thread embedding acupuncture. J Korean Med Ophthalmol Otolaryngol Dermatol. 2016;29(1):103–112. doi: 10.6114/jkood.2016.29.1.103 [DOI] [Google Scholar]
- 26.Kim JI, Han C-H, Jeon JH, et al. Effectiveness and safety of polydioxanone thread embedding acupuncture compared to physical therapy in the treatment of patients with non-specific chronic neck pain: an assessor-blinded, randomized, controlled, clinical Trial. J Pain Res. 2021;14:201. doi: 10.2147/JPR.S276941 [DOI] [PMC free article] [PubMed] [Google Scholar]