Abstract
Objective:
This study examined the impact of a survivorship planning consultation (SPC) for patients with Hodgkin’s lymphoma (HL) and diffuse large B-cell lymphoma (DLBCL) on quality of life (QOL). We specifically assessed two potential moderators, cancer worry and perceived empathy, of the intervention effects on QOL.
Methods:
This cluster randomized, four-site trial examined the efficacy of a SPC; physicians received communication skills training and applied these skills in a survivorship-focused office visit using a care plan versus a control arm in which physicians were trained to and subsequently provided a time-controlled, manualized Wellness Rehabilitation Consultation (WRC) focused only on discussion of healthy nutrition and exercise. We examined the effect of the intervention on patients’ QOL and examined potential moderators--cancer worry and perceived physician empathy.
Results:
Forty-two physicians and 198 patients participated. There was no main effect of the intervention on any of the QOL dimensions (ps > 0.10). However, cancer worry was a significant moderator of the effects of the intervention on three QOL domains (physical p=0.04; social p=0.04; spiritual p=.01) and perceived empathy was a significant moderator of QOL (physical p=0.004; psychological p=0.04; social p=0.01). Specifically, the beneficial effects of the intervention were more pronounced among patients who initially reported higher levels of cancer worry and lower levels of physician empathy.
Conclusions:
This study identified two factors, perceived empathy and cancer worry, that were found to impact the QOL of patients who participated in this communication-based survivorship intervention.
Keywords: survivorship, quality of life, moderators, empathy, worry, lymphoma, communication, cancer, oncology
The number of individuals diagnosed with and surviving cancer continues to increase.1 The period immediately following active treatment and the transition into survivorship is challenging for many survivors as they often feel unprepared for what to expect next. Cancer worry and fear of cancer recurrence are frequently present during this transition.2 These challenges and some strategies to address them are described in the Institute of Medicine report, From Cancer Patient to Cancer Survivor: Lost in Transition.3 This report advocates for the use of survivorship care plans to better inform and assist patients with what to expect during the post-treatment phase and beyond.
Hematological cancers have been shown to have negative impact on physical, emotional, functional and social aspects of patients’ quality of life (QOL).4 This impact on QOL does not end when treatment ends, but rather survivors also report decrements in QOL in the months and years following diagnosis and treatment.5 Interventions that enhance QOL among survivors of lymphoma and other hematological cancers are needed.
The results of empirical studies have been mixed regarding the documented benefits of survivorship care plans.6–8 Only a few studies have found that using survivorship care plans resulted in improved outcomes.9,10 For example, a recent systematic review found that there was little evidence that survivorship care plans impacted the most commonly assessed outcomes (e.g., physical, functional and psychological well-being), though survivorship care plans did impact amount of information received and satisfaction with care.11 We recently published the results of a randomized trial that compared a survivorship planning consultation (SPC) to a wellness rehabilitation consultation (WRC). The SPC gave oncologists a new set of communication skills for delivering a structured survivorship care plan. The WRC focused only on a discussion of wellness and lifestyle factors. Patients in the SPC arm reported higher knowledge about their cancer and its treatment and had a greater uptake of physician recommendations regarding vaccinations in comparison to patients in the WRC arm.12 We hypothesized that the intervention was efficacious because, in addition to providing the care plan, it also provided an opportunity for physicians to practice using the care plan to discuss patients’ survivorship concerns.
In addition to examining direct effects of interventions, there is a need to evaluate the association between psychosocial variables and intervention effectiveness to determine if patient characteristics are associated with benefit from the survivorship planning consultation intervention.13 It may be, for example, that patients who have higher levels of cancer worry may derive greater benefit than those with lower levels of cancer worry. Cancer worry has been found to be associated with distress in a variety of cancer survivors.14–16 Another factor that may influence the efficacy of the intervention is patients’ perceptions of physician empathy. Patient-reported physician empathy has been found to be associated with better psychosocial adjustment and QOL.17,18
The purpose of this study was to further examine the impact of this survivorship planning consultation (SPC) on QOL (defined as physical, psychosocial, social and spiritual well-being). We specifically assessed two potential moderators, cancer worry and perceived physician empathy, of the intervention effects on these outcomes.
METHODS
Study Design
Sites were randomized to either SPC or WRC arms in a cluster-randomized design (2 sites had large number of lymphoma patients and 2 sites had fewer numbers of patients. The study was approved by the sites’ Institutional Review Boards. Additional details about study design are published elsewhere.12
Participants and Procedures
Physicians:
Participating physicians were oncologists who saw patients with newly diagnosed Hodgkin lymphoma (HL) or diffuse large B-cell lymphoma (DLBCL). Interested oncologists provided informed consent.
Patients:
Patients were recruited through their participating oncologists’ clinics. Eligibility criteria included: a new diagnosis of HL or DLBCL treated with curative intent; scans indicated they were in remission; age 18 years or older; and English-speaking. Patients were ineligible if they showed evidence of significant cognitive impairment. Patient recruitment occurred at the time they were informed of remission and assessments were completed at that time (baseline) and then again 1, 3 6, and 12 months later.
Study Groups
Survivorship Planning Consultation. The oncologists assigned to the SPC arm participated in a 5-hour communication skills training program. The communication skills training program included didactic information about lymphoma survivorship including exemplary videos demonstrating recommended communication strategies as well as survivorship-themed role-plays with standardized patients (trained actors); and a discussion about the benefits and barriers to SPC implementation.12
Approximately 1 months after the baseline visit, physicians conducted a 15-minute new consultation with their patients that focused on survivorship including a review of the scans showing remission status followed by discussion of the SPC and survivorship-related issues. The SPC provided a summary of the diagnosis details and treatments received, treatment-relevant toxicities, frequency of future visits, screening schedule, and review of health promotion behaviors. The SPC consultations were audio-recorded for fidelity monitoring12,19.
Wellness Rehabilitation Consultation. Physicians in the WRC arm received an in-person 2-hour training program focused only on wellness and lifestyle factors. Then, physicians in the WRC arm had a time-matched consultation with their patients one month after the baseline visit in which they reviewed scans showing remission status and discussed the benefit of healthy nutrition and walking to promote fitness. WRC consultations were audio-recorded for fidelity monitoring 12,20.
Measures
Demographics: At baseline, the following demographic information was collected from patients : race, ethnicity, education, marital status, and work status.
Cancer Worry Inventory (CWI)21 is a 24-item scale that assesses worries across the following domains: health or physical illness, fear of cancer recurrence, work, financial, religious or spiritual, family or friends, social and leisure activities, sexuality, self-appraisal and existential concerns. It has good psychometric properties16 and showed strong reliability in our sample (Cronbach’s alpha was .0.91). Total scores could range from 0 to 96.
Consultation and Relational Empathy (CARE) 22 assesses a patient’s perspective of their physicians’ empathy in emotional, cognitive and behavioral domains. This 10-item scale has been used in a variety of settings including oncology.23,24 An additional eight items were added that examined aspects of the Common Sense Model of Illness, revealing the patient’s view about how helpful the physician was at providing help with fear of recurrence, future expectations, tips for getting on with life, future, anti-cancer screening plans, self-monitoring, high risk behaviors, exercise and nutrition. Total scores could range from 18 to 90.
Quality of Life Cancer Survivor (QOL-CS)25 is a 41 item scale that assesses QOL in four domains: physical, psychosocial, social and spiritual well-being. It has been used to assess QOL in a variety of cancer populations including individuals with lymphoma.26–28 In our sample, Cronbach’s alphas ranged from 0.75 to 0.90. Subscale scores could range from 0 to 10.
Statistical Plan
Participant characteristics were described overall and by arm. Missingness was compared between experimental arms and by patient baseline characteristics, comparing both drop-out and cross-sectional missingness, all via Chi-square tests. Patient characteristics were also compared by experimental arm, again using a series of Chi-square tests. We examined whether the psychosocial measures changed over time and whether the trajectories differed by study arm using hierarchical linear models (HLM) with random intercepts for patients nested within sites.20 In addition to the main and interaction effects within these models, quadratic time effects were assessed for inclusion to account for non-linear trajectories. Next, we compared the study arms on psychosocial measures at 1-year followup again using HLM models, regardless of trajectory or rate of change, this time adjusting for baseline measure and the random per-clinic intercept, as only one observation was included per patient. Although patient demographics and disease characteristics did not differ significantly by arm, because randomization was at the site-level we conducted sensitivity analyses by fitting these models both with and without adjustment for demographic and disease covariates that were anticipated to affect outcomes. Finally, we examined whether baseline cancer worry and perceived empathy moderated the effects of the SPC intervention on the four dimensions of QOL using a series of moderation models. Each of the 1-year QOL measures were regressed on an indicator for study arm, the baseline value of the potential moderator, and an interaction effect of the moderator with study arm, again with a per-clinic intercept. As published previously, we were well powered for these analyses.12,20 A significant effect on the interaction term in the HLM analysis was considered evidence for the moderation hypothesis, and η2 was calculated as an effect size estimate for each significant moderator. All analyses were conducted in SAS version 9.4.
RESULTS
Sample Characteristics
Forty-two physicians (22 SPC and 20 WRC) and 198 patients (117 at SPC sites and 81at WRC sites) were enrolled. Physicians across sites were similar on most characteristics except that physicians at the smaller WRC site reported fewer cases of DLBCL (mean of 5.1 versus 31.5–58.9 patients), and less time spent on research compared to those at other sites (91% reported ≤10% versus 25–43 at other sites). Across groups, 33% of physicians were female (59% SPC and 75% in WRC) and they were 50.3 years old (SD=11.1). They had practiced for on average 17.2 years (SD-11.0)
Patients were largely White, non-Hispanic (66%), and evenly distributed by gender (52% female) and between earlier and later stages at diagnosis (51% stages 1–2 and 48% stages 3–4). Patient age ranged from 18 to 87 years, 58% were married or living with partner, and 81% had college or post-graduate education. As shown in Table 1, patients reported QOL levels near or just above the middle of the range, moderate cancer worry and medium to high perceptions of physician empathy at baseline. Patient characteristics did not significantly differ by study arm. (all ps >0.10). Attrition did not differ between the arms by patient characteristics at any timepoint, though the SPC participants provided more complete data at the last 3 time-points (T4: p=0.01; T5 and T6: p<0.01). Intermittent missingness also did not differ by patient or disease characteristics, such that patients who completed all surveys were comparable to patients who missed at least one (all p>0.10). Additional details about physician and patient characteristics have been previously published. 12
Table 1.
Baseline QOL, Worry, and Empathy scores
| n | Mean (SD) | Min – Max | |
|---|---|---|---|
| QOL Physical | 155 | 7.60 (1.79) | 2.25 – 10 |
| QOL Psychological | 147 | 5.47 (1.53) | 0.28 – 8.94 |
| QOL Social | 156 | 6.24 (1.97) | 0.50 – 9.75 |
| QOL Spiritual | 162 | 5.89 (2.06) | 1.14 – 10 |
| Worry | 163 | 24.66 (16.60) | 0 – 77 |
| Empathy | 159 | 77.79 (14.17) | 20.57 – 90 |
Psychosocial Measure Trajectories over Time by Study Arm
We examined whether the psychosocial measures changed over time and whether the trajectories differed by study arm (Figure 1). Overall, worry significantly declined over time (p< 0.001) and there was a significant increase in perceived physician empathy (p<0.001) and QOL in physical (p<0.001), psychological (p=0.03) and social (p<0.001) domains. Quadratic time effects were significant for empathy (p<0.001), worry (p<0.001), and QOL domains of physical (p=0.005) and social (p=0.004). Over the course of the study, perceived empathy was significantly different by study arm, with patients in the SPC arm perceiving greater physician empathy over time than those in the WRC arm (p=0.04). There were no other differences over time by study arm (all ps >0.10).
Figure 1.
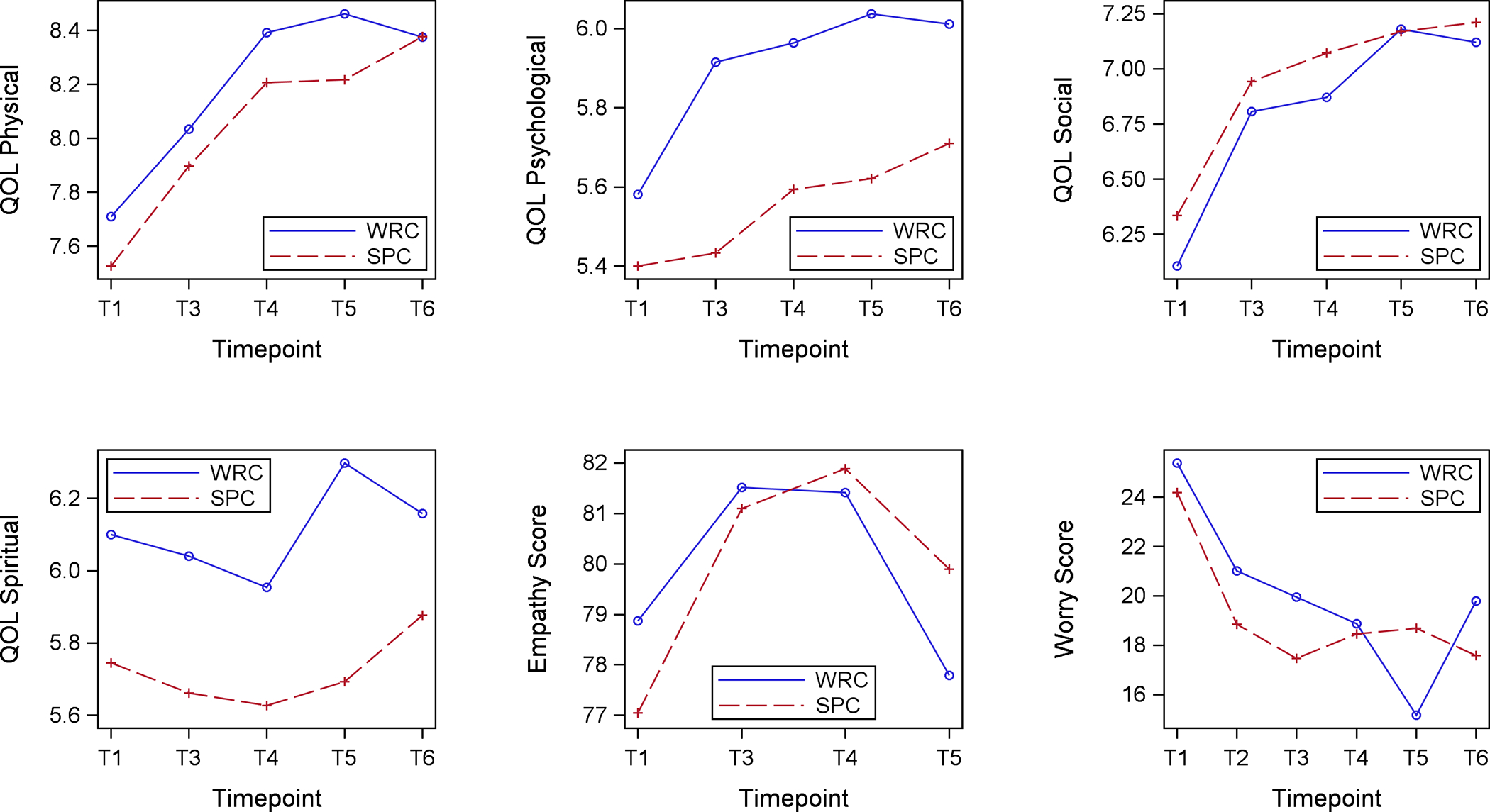
Means of Psychosocial Measures Over Time, by Study Arm
Intervention Effects on QOL at One Year Follow Up
Adjusting for baseline measures, there was no impact of the intervention on physical, psychological, social or spiritual domains of QOL one year post-intervention (each with p>0.10). Multivariable analysis adjusting for potentially confounding variables including both patient characteristics (gender, race marital status, education and disease stage) and physician gender, revealed similar parameter estimates.
Psychosocial Factors (Cancer Worry and Perceived Empathy) as Moderators of Intervention Effect on QOL
Results indicated that cancer worry was a significant moderator of the effects of the intervention on three QOL domains (physical p=0.04; social p=0.04; spiritual p=.01; Table 2). Additionally, perceived empathy was a significant moderator of the effects on two of these same QOL domains plus another (physical p=0.004; psychological p=0.04; social p=0.01). The effect sizes of these moderating effects were small (η2 ranging from 0.026 to 0.043) for all but the moderation of empathy for physical QOL (η2 = 0.076) and moderation of worry for spiritual QOL (η2 = 0.050), which both had effect sizes in the medium range. As depicted in Figure 2, generally, the beneficial effects of the intervention were more pronounced among patients who initially reported higher levels of cancer worry and lower levels of physician empathy. We conducted additional analyses that included potential confounding variables including gender, race, marital status, education and disease stage and there were similar parameter estimates in these models.
Table 2.
Moderation Effects of Worry and Empathy
| QOL Physical | QOL Psych | QOL Social | QOL Spiritual | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Moderator | Covariate | B (SE) | p-value | B (SE) | p-value | B (SE) | p-value | B (SE) | p-value |
| Worry | Worry | −0.07 (0.01) | <.001 | −0.06 (0.01) | <.001 | −0.10 (0.02) | <.001 | −0.06 (0.02) | 0.005 |
| SPC | −0.81 (0.43) | 0.061 | −0.93 (0.56) | 0.097 | −0.86 (0.57) | 0.135 | −1.43 (1.19) | 0.233 | |
| Worry × SPC | 0.03 (0.02) | 0.038 | 0.03 (0.02) | 0.086 | 0.04 (0.02) | 0.039 | 0.06 (0.02) | 0.014 | |
| Empathy | Empathy | 0.05 (0.01) | 0.001 | 0.03 (0.01) | 0.033 | 0.07 (0.02) | <.001 | 0.04 (0.02) | 0.053 |
| SPC | 4.21 (1.46) | 0.005 | 2.82 (1.57) | 0.075 | 5.19 (2.08) | 0.014 | 2.82 (2.25) | 0.212 | |
| Empathy × SPC | −0.06 (0.02) | 0.004 | −0.04 (0.02) | 0.043 | −0.06 (0.03) | 0.015 | −0.03 (0.03) | 0.176 | |
For each model, the 12-month QOL measure is regressed on an indicator of SPC, the baseline value of the potential moderator, and an interaction effect. Each model also includes a random per-clinic intercept. This table represents 8 models, one for each moderator – outcome dyad.
Figure 2.
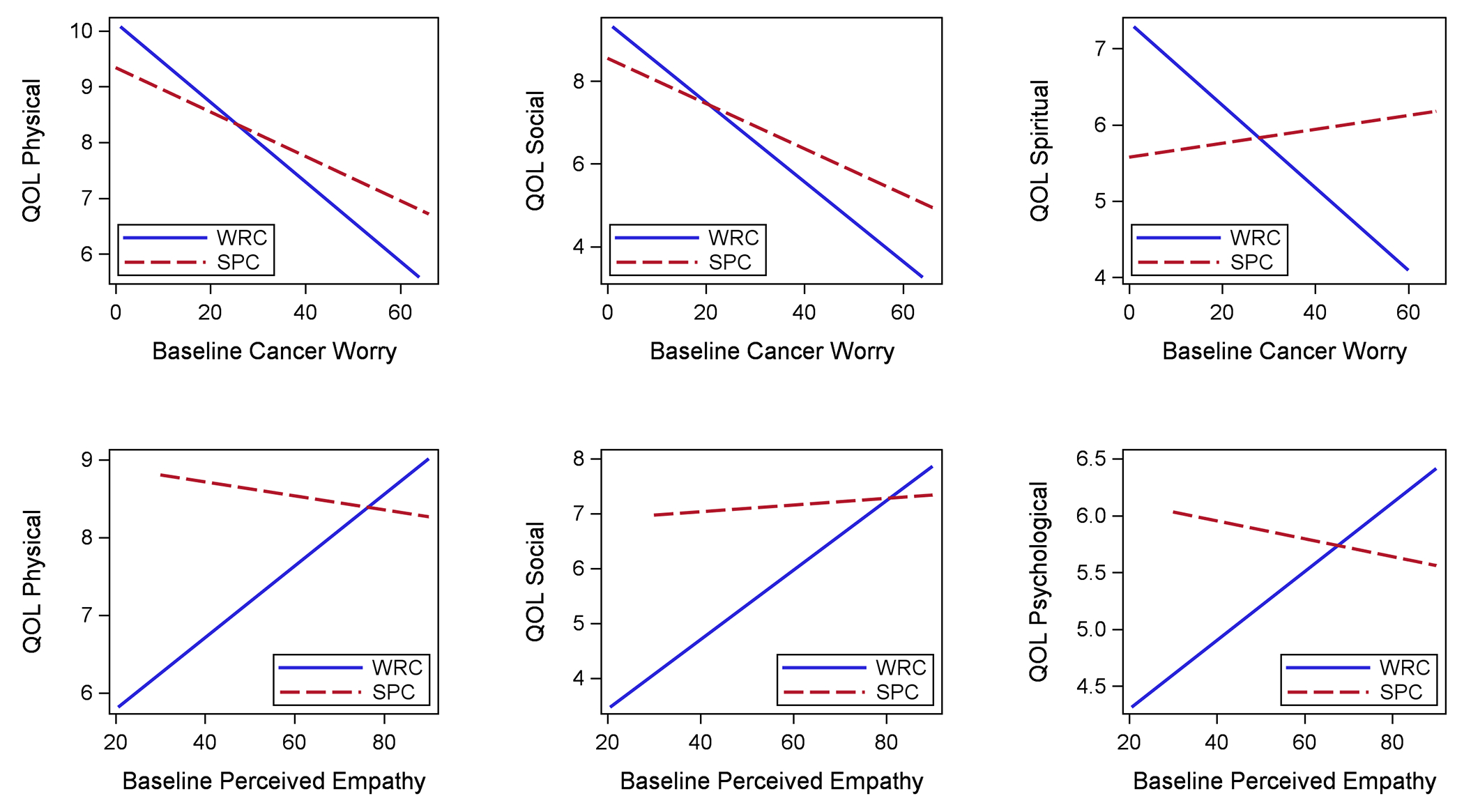
Association between Quality of Life Outcomes at 1 Year and Baseline Empathy or Worry, by Study Arm
DISCUSSION
For patients in both groups, QOL improved in the year following treatment completion but there was no significant intervention effect on QOL; patients whose physicians participated in the SPC intervention did not have higher QOL scores 12 months after the intervention compared with those in the WRC. Importantly, however, baseline perceived empathy and cancer worry moderated the effect of the intervention. That is, this communication-based survivorship care intervention was more effective for patients who at the transition into survivorship had more cancer worry, and for those who perceived their doctors as having lower levels of empathy. This is consistent with other work which has demonstrated that cancer worry persists into survivorship for many cancer patients.29 It also highlights the important role of perceived empathy, which has been associated with better QOL in patients who have difficulty expressing their emotions.30 Interestingly, cancer worry did not moderate the impact of the intervention on psychological QOL, whereas it did all the other domains of QOL. This may be due to the fact that the psychological QOL domain includes factors associated with worry such as fear of recurrence whereas the other domains assess less related factors such as functional ability, family relationships, finances, religiosity and transcendence. Relatedly, empathy did not moderate social QOL, perhaps because they both include social aspects.
Worry about cancer and fear of cancer recurrence is problematic among cancer survivors. While both SPC and WRC arms had their most recent scan (indicating remission) results formally reviewed, use of the survivorship care plan may have conveyed greater confidence about the goal of cure and declaration of becoming a survivor than the control arm WRC consultation. Given that a number of psychological interventions are being tested in an effort to reduce the burden that fear of cancer recurrence brings,31–33 this outcome from a single outpatient consult by an oncologist is noteworthy.
These results suggest the need not only to focus interventions on all patients with a given illness or condition, but rather to examine whether specific subgroups of patients may benefit from tailored interventions. In order to optimize both efficiency and effectiveness, it is best to focus our interventions on those patients who are most likely to derive the greatest benefit. While moderation hypotheses are sometimes criticized in the absence of main intervention effects, this strict definition has limitations such as the case when the moderator reverses the effect and thus moderation analysis allows us to determine for whom the intervention was most effective regardless of overall effect on the general population.34
That perceived empathy increased in the SPC arm over time compared with the WRC arm is evidence of the value of communication skills training in helping oncologists to develop strategies to discuss survivorship care plans and be person-centered in their relationship with the patient. Although the complexity and specific content of these 15-minute interventions differed, leading to different lengths of training offered to oncologists depending on their site’s randomized assignment, discussion of a survivorship care plan is a detailed task that can be optimized by an empathic stance. The contribution of this communication skills training has been highlighted elsewhere.19,35
Study Limitations
Limitations of the study should be noted. First, participants were primarily non-Hispanic Caucasians and exclusively English-speaking. Future studies should examine the impact of survivorship care plans in more ethnically, culturally, and socioeconomically diverse populations, to determine if outcomes differ. Additionally, while we tested the intervention at hospitals of varying size and patient volume, all four sites were teaching hospitals, which could limit its generalizability; assessing the efficacy of the intervention in community oncology clinics and hospitals would add valuable insight into the generalizability of our findings. Further, though the goal of the current moderation analysis was to simply identify for whom or under what circumstances the SPC arm may be more beneficial, the changes in both empathy and worry over time may indicate a more complex and dynamic relationship between these psychological constructs and the QOL outcomes. Additionally, it may be that other characteristics, that were not examined such as physician gender or ethnicity, may have an influence on these associations. Future work is needed to further explore these and other potentially relevant characteristics.
Clinical Implications
The results of this randomized study identify two factors, perceived empathy and cancer worry, that were found to impact the QOL of patients who participated in this communication-based survivorship intervention. It should be noted that the effect sizes were in the small to medium range. Specifically, two of the moderator effects, empathy for physical QOL and worry for spiritual QOL both had effect sizes in the medium ranges and are likely to be clinically significant differences. The clinical significance of these results should be further investigated.
These results highlight the need to include factors that are proposed to influence the effect of the intervention when conducting intervention studies. If patients have high levels of cancer worry, they may be at risk for poorer survivorship outcomes, a carefully constructed consultation at the end of their treatment that reviews what they have gone through and what needs to be attended to in their future has the potential to moderate fear of recurrence and thus enhance future QOL.
Funding Acknowledgement:
This study was supported by National Cancer Institute (R01 CA 151899, Co-PIs D Kissane and S Horwitz) and the Cancer Center Support Grant (CCSG-Core Grant; P30 CA008748; PI: Craig B. Thompson, MD) from the National Cancer Institute of the National Institutes of Health.
Footnotes
Conflict of Interest: All authors declare that they have no conflicts of interest.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional committees and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The protocol #11-180 was approved by the Institutional Research Board at Memorial Sloan Kettering Cancer Center.
Data Availability Statement:
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- 1.American Cancer Society. Cancer Facts and Figues 2018. Atlanta: American Cancer Society;2018. [Google Scholar]
- 2.Lebel S, Maheu C, Lefebvre M, et al. Addressing fear of cancer recurrence among women with cancer: a feasibility and preliminary outcome study. J Cancer Surviv. 2014;8(3):485–496. [DOI] [PubMed] [Google Scholar]
- 3.Institute of Medicine, Council NR. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC: The National Academies Press; 2006. [Google Scholar]
- 4.Allart-Vorelli P, Porro B, Baguet F, Michel A, Cousson-Gélie FJBCJ. Haematological cancer and quality of life: a systematic literature review. 2015;5(4):e305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baxi SS, Matasar MJ. State-of-the-art issues in Hodgkin’s lymphoma survivorship. Curr Oncol Rep. 2010;12(6):366–373. [DOI] [PubMed] [Google Scholar]
- 6.Brennan ME, Gormally JF, Butow P, Boyle FM, Spillane AJ. Survivorship care plans in cancer: a systematic review of care plan outcomes. Br J Cancer. 2014;111(10):1899–1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Faul LA, Shibata D, Townsend I, Jacobsen PB. Improving survivorship care for patients with colorectal cancer. Cancer Control. 2010;17(1):35–43. [DOI] [PubMed] [Google Scholar]
- 8.Grunfeld E, Julian JA, Pond G, et al. Evaluating survivorship care plans: results of a randomized, clinical trial of patients with breast cancer. J Clin Oncol. 2011;29(36):4755–4762. [DOI] [PubMed] [Google Scholar]
- 9.Maly R, Liang L, Liu Y, Griggs J, Ganz P. Randomized controlled trial of survivorship care plans among low-income, predominantly Latina breast cancer survivors. J Clin Oncol. 2017;35(16):1814–1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nissen MJ, Tsai ML, Blaes AH, Swenson KK, Koering S. Effectiveness of treatment summaries in increasing breast and colorectal cancer survivors’ knowledge about their diagnosis and treatment. Journal of Cancer Survivorship. 2013;7(2):211–218. [DOI] [PubMed] [Google Scholar]
- 11.Jacobsen PB, DeRosa AP, Henderson TO, et al. Systematic review of the impact of cancer survivorship care plans on health outcomes and health care delivery. J Clin Oncol. 2018:JCO. 2018.2077. 7482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parker PA, Banerjee SC, Matasar MJ, et al. Efficacy of a survivorship-focused consultation versus a time-controlled rehabilitation consultation in patients with lymphoma: a cluster randomized controlled trial. Cancer. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jacobsen PB. Screening for Psychological Distress in Cancer Patients: Challenges and Opportunities. J Clin Oncol. 2007;25(29):4526–4527. [DOI] [PubMed] [Google Scholar]
- 14.Deimling GT, Bowman KF, Sterns S, Wagner LJ, Kahana B. Cancer-related health worries and psychological distress among older adult, long-term cancer survivors. Psychooncology. 2006;15(4):306–320. [DOI] [PubMed] [Google Scholar]
- 15.Götze H, Taubenheim S, Dietz A, Lordick F, Mehnert-Theuerkauf AJPO. Fear of cancer recurrence across the survivorship trajectory: Results from a survey of adult long-term cancer survivors. 2019. [DOI] [PubMed] [Google Scholar]
- 16.Custers JA, Gielissen MF, Janssen SH, de Wilt JH, Prins JBJSCiC. Fear of cancer recurrence in colorectal cancer survivors. 2016;24(2):555–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lelorain S, Bredart A, Dolbeault S, Sultan S. A systematic review of the associations between empathy measures and patient outcomes in cancer care. Psychooncology. 2012;21(12):1255–1264. [DOI] [PubMed] [Google Scholar]
- 18.Neumann M, Wirtz M, Bollschweiler E, et al. Determinants and patient-reported long-term outcomes of physician empathy in oncology: a structural equation modelling approach. 2007;69(1–3):63–75. [DOI] [PubMed] [Google Scholar]
- 19.Banerjee SC, Matasar MJ, Bylund CL, et al. Survivorship care planning after participation in communication skills training intervention for a consultation about lymphoma survivorship. Transl Behav Med. 2015;5(4):393–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parker PA, Banerjee SC, Matasar MJ, et al. Protocol for a cluster randomised trial of a communication skills intervention for physicians to facilitate survivorship transition in patients with lymphoma. BMJ Open. 2016;6(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.D’Errico GM, Galassi JP, Schanberg R, Ware WB. Development and validation of the cancer worries inventory: A measure of illness-related cognitions. J Psychosoc Oncol. 1999;17:119–137. [Google Scholar]
- 22.Mercer SW, Maxwell M, Heaney D, Watt GC. The consultation and relational empathy (CARE) measure: development and preliminary validation and reliability of an empathy-based consultation process measure. Fam Pract. 2004;21(6):699–705. [DOI] [PubMed] [Google Scholar]
- 23.Wirtz M, Boecker M, Forkmann T, Neumann MJPe, counseling. Evaluation of the “Consultation and Relational Empathy”(CARE) measure by means of Rasch-analysis at the example of cancer patients. 2011;82(3):298–306. [DOI] [PubMed] [Google Scholar]
- 24.Johnson L, Gorman C, Morse R, Firth M, Rushbrooke SJEjocc. Does communication skills training make a difference to patients’ experiences of consultations in oncology and palliative care services? 2013;22(2):202–209. [DOI] [PubMed] [Google Scholar]
- 25.Ferrell BR, Dow KH, Grant M. Measurement of the quality of life in cancer survivors. Qual Life Res. 1995;4:523–531. [DOI] [PubMed] [Google Scholar]
- 26.Dow KH, Ferrell BR, Leigh S, Ly J, Gulasekaram PJBcr, treatment. An evaluation of the quality of life among long-term survivors of breast cancer. 1996;39(3):261–273. [DOI] [PubMed] [Google Scholar]
- 27.Ahles TA, Saykin AJ, Furstenberg CT, et al. Quality of life of long-term survivors of breast cancer and lymphoma treated with standard-dose chemotherapy or local therapy. 2005;23(19):4399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mols F, Aaronson NK, Vingerhoets AJ, et al. Quality of life among long-term non-Hodgkin lymphoma survivors: a population-based study. 2007;109(8):1659–1667. [DOI] [PubMed] [Google Scholar]
- 29.Stanton AL, Rowland JH, Ganz PAJAP. Life after diagnosis and treatment of cancer in adulthood: Contributions from psychosocial oncology research. 2015;70(2):159. [DOI] [PubMed] [Google Scholar]
- 30.Lelorain S, Cattan S, Lordick F, et al. In which context is physician empathy associated with cancer patient quality of life? 2018;101(7):1216–1222. [DOI] [PubMed] [Google Scholar]
- 31.van de Wal M, Thewes B, Gielissen M, Speckens A, Prins JJJoCO. Efficacy of blended cognitive behavior therapy for high fear of recurrence in breast, prostate, and colorectal cancer survivors: the SWORD study, a randomized controlled trial. 2017;35(19):2173–2183. [DOI] [PubMed] [Google Scholar]
- 32.Pyszczynski T, Solomon S, Greenberg J. Thirty years of terror management theory: From genesis to revelation. In: Advances in experimental social psychology. Vol 52. Elsevier; 2015:1–70. [Google Scholar]
- 33.Butow PN, Turner J, Gilchrist J, et al. Randomized trial of ConquerFear: a novel, theoretically based psychosocial intervention for fear of cancer recurrence. 2017;35(36):4066–4077. [DOI] [PubMed] [Google Scholar]
- 34.MacKinnon DP, L.J. L How and for whom? Mediation and moderation in Helath Psychology. Health Psychol. 2008;27(2):S99–S100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Franco K, Shuk E, Philip E, et al. Communication between oncologists and lymphoma survivors during follow-up consultations: A qualitative analysis. J Psychosoc Oncol. 2017;35(5):513–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


