Abstract
Background:
An emerging respiratory disease abbreviated as coronavirus disease 2019 was first reported in December 2019 in Wuhan city of China. The virus is zoonotic and tends to be transmitted between animals to humans and humans to humans. The major route of transmission of coronavirus disease 2019 is droplet and close contact. The Ethiopian Ministry of Health has initiated training for health care workers at a different level. Thus, the main objective of this study is to assess the knowledge, attitudes, and practices of health workers in Ethiopia toward coronavirus disease 2019 and its prevention techniques.
Method:
An institution-based multicenter cross-sectional study was conducted in each of eight teaching and referral hospitals. A total of 422 Ethiopian healthcare workers were selected for the assessment of knowledge, attitude, and practice toward coronavirus disease 2019. Data were collected using a structured questionnaire. A logistic regression model was used to identify factors associated with the attitude and knowledge of healthcare workers toward coronavirus disease 2019 at a significance level of p < 0.05.
Result:
Three hundred ninety-seven healthcare workers participated in the study, with a response rate of 94%. Among these, 88.2% and 94.7% of respondents had good knowledge and positive attitudes, respectively. A respondent with a history of chronic medical illness (odds ratio: 0.193, 95% confidence interval: 0.063–0.593), social media, telecommunication, and television/radio as a source of information were significantly associated with knowledge (odds ratio: 3.4, 95% confidence interval: 1.5–7.4, OR: 4.3, 95% confidence interval: 1.3–14.3 and odds ratio: 3.2, 95% confidence interval: 1.4–7.2). In addition, respondents with a history of chronic medical illness were significantly associated with a negative attitude toward coronavirus disease 2019.
Conclusion:
The knowledge and attitude were good while; the practice was relatively low. Sources of information such as social media, telecommunication, and television/radio were positively associated with healthcare workers' knowledge about coronavirus disease 2019.
Keywords: COVID-19, knowledge, attitude, practice, healthcare worker, Ethiopia
Background
An emerging respiratory disease was abbreviated as coronavirus disease 2019 (COVID 19), after it was first reported in December 2019 in Wuhan city of China. 1 The virus causing COVID-19 is a severe acute respiratory syndrome (SARS)-like coronavirus that had previously been reported in bats in China. 2 The virus is a zoonotic virus that has a tendency to be transmitted between animals to humans and humans to humans.
The major route of transmission of COVID-19 is droplet and close contact.3,4 This viral infection causes several diseases such as respiratory, enteric, hepatic, neurologic, and vascular systems.5,6 It has been characterized by a wide clinical future ranging from no symptoms to a severe form of respiratory illness, such as acute respiratory distress syndrome (ARDS). 7 The main symptoms of COVID-19 included fever, fatigue, and cough, which are similar to those of SARS-CoV- and Middle East respiratory syndrome (MERS-CoV)-infected cases. Less common symptoms, such as sputum production, headache, hemoptysis, and diarrhea, have been reported.8–10
The global community and Research and Development Blueprint Scientific Advisory Group acknowledged the research gaps in COVID-19. Awareness creation and changing attitudes were among the public health interventions recommended by the World Health Organization (WHO). Various studies have shown that demographic, social, and technological factors affect the level of knowledge, attitude, and practice toward disease and its prevention. 11 Health care professionals are expected to be at high risk for COVID-19 because of contact with confirmed and suspected cases at the frontline.
The Ethiopian health service system is federally decentralized along the nine regions and two self-administered cities namely Addis Ababa and Diredawa. Even if there has been a significant increase in the number of human resources for health, the Ethiopian healthcare system and healthcare workforce is challenging which might be worse during pandemic like COVID-19. 12 The country has about 143 hospitals as of 2007 report and most of them are running by ministry of health. A population to physician ratio is one physician for about 50,000 people which is well below the WHO standard of 1:10,000 and is over five times below the average for sub-Saharan Africa. 13
The Ethiopian Ministry of Health has initiated training for health care workers at different levels, although an effort to cover a wider range is poor. The WHO and Centers for Disease Control and prevention (CDC) also initiated a multidisciplinary approach to tackle COVID-19, of which awareness creation is the main. Having research on knowledge, practice, attitude, and associated factors of health workers toward COVID-19 and its prevention techniques have a pivotal impact in fighting against the disease specially when there is a lack information in this regard. Thus, this study aims to assess the knowledge, practice, and attitude of Ethiopian health workers toward COVID-19 and its prevention techniques.
Methods
Study settings and design
This multicenter institution-based cross-sectional study was employed. Ethiopia is located in the horn of Africa and bordered by Eretria to the north, Djibouti, and Somalia to the east, Sudan and South Sudan to the west, and Kenya to the south. Ethiopia has a high central plateau that varies from 1290 to 3000 m (4232–9843 ft) above sea level. This country’s population is highly diverse, comprising over 80 different ethnic groups. The population exceeds 110,000,000, who live in an area of 1,127,127 km². Ethiopian Health care System is organized by a three-tier health care delivery system which includes the first level of a Woreda/District health system comprising a Primary Hospital, Health center, and health posts from a Primary health care unit (PHCU) with each health center having five satellite health posts. The second level in the tier is a General Hospital with a population coverage of 1–1.5 million people, and the third a Specialized Hospital that covers a population of 3.5–5 million. As of 2010, there were 195 hospitals, 2689 health centers, and 14,416 health posts in Ethiopia. Overall, the total health workforce is estimated at around 147,000 in Ethiopia currently. The study was carried out in 422 healthcare workers in eight randomly selected hospitals (Menelik II referral hospital, Felegehiwote comprehensive referral hospital, Hawassa University compressive specialized hospital, Jimma University specialized hospital, Dilla University referral hospital, Hayder referral hospital, Adigerat general hospital, Debre-Berhan referral hospital, and Debre-Tabor general Hospital) from 28 universities and university-affiliated hospital in Ethiopia. Participants were selected randomly from each hospital. All randomly selected healthcare workers in the selected hospitals who had the willingness to participate in the study were included in the study.
Sample size determination and data collection tools
The sample size (n) is calculated using a single proportion formula. By considering marginal error (E) 5%, the confidence interval of 95 % (Z = 1.96), and since there is no previous study in our country; we consider the 50% of proportion of having good knowledge about COVID-19. So that the calculated sample size was
With the assumption of 10% non-response rate, the final sample size was 424.
The study tool was developed based on extensive literature review, course material regarding emerging respiratory diseases including COVID-19 by WHO and the Ethiopian ministry of health at that occasion. After an initial draft of the questionnaire designed, it was validated by the following steps. First, the study tool was sent to researchers and healthcare workers from different backgrounds to give their expert opinion concerning the simplicity and importance of study tools. Second, a pretest was conducted in Nigist Eleni hospital and Arba Minch general hospital by selecting a small sample of health care workers (n = 22) on 5% of calculated sample size. Any modifications from the participants were considered and integrated into the final questionnaire while ensuring its consistency with the available literature. After a thorough discussion, a questionnaire was finalized by the authors and subsequently distributed to the participants for their response. Reliability was calculated by using SPSS v.25 and the value of Cronbach’s alpha was found to be 0.75. The data of the pilot study were not used for the final analysis.
Finally, the questionnaire consisted of four parts, which were used to collect information from healthcare workers. First, question assessing sociodemographic and general characteristics of healthcare workers, such as gender, age, educational status, work experience, marital status, profession, religion, travel history, source of information about COVID-19, and training on COVID-19. Second, the knowledge section comprised of 9 items; regarding signs and symptoms, characteristics of the diseases, etiology, risky group, transmission, and prevention were used to assess healthcare workers’ knowledge about COVID-19. Each question was responded as Yes and No. The correct answer was marked as 1 while the wrong answer was marked as 0. Third, attitude sections comprised of 10 questions assessing the attitude of healthcare workers’ toward COVID-19 prevention and treatment. Response of each question was recorded on a 5-point Likert-type scale follows strongly agree (1-point), agree (2-point), neutral (3-point), disagree (4-point), and strongly disagree (5-point). The total score ranges from 10 to 50, with an overall higher mean score indicates a positive attitude toward COVID-19. Then, the last and fourth part contains seven questions regarding the use of facemask, handwashing, social distance, and other preventive measures used to assess the practice of healthcare workers’ toward COVID-19 prevention. Each item was responded as Yes, No, and sometimes. See Supplemental file 2 for the detailed question used to assess healthcare workers’ knowledge, attitude, and practice.
Data interpretation and statistical analysis
After completeness of collection, data were first cross-checked manually for completeness and entered into Epi-Data version 3.1 statistical software transported to SPSS version 25 for further analysis cleaning. Knowledge about COVID-19 was measured using ninety knowledge questions and dichotomized into good knowledge and poor knowledge. The levels of knowledge, attitude, and practice were dichotomized into "good" and "poor" or “positive” and “negative” for attitude based on a 60% cut-off point of the total score within each domain of knowledge, attitude, and practice.
Healthcare worker attitude toward COVID-19 was assessed using a 5-point Likert-type scale, as individuals responding to positive attitudes were given scores of 5, 4, and 3, and a score of 2 and 1 was given for negative attitudes. Then, the score was dichotomized into a positive and negative attitude for each question.
Descriptive statistics were used to summarize tables and figures, and summary measures were used for data presentation. Outlier and multicollinearity were checked using standardized residual tests, variance inflation factor (VIF), and tolerance, respectively. Logistic regression analysis was used to identify factors associated with the attitude and knowledge of healthcare workers toward COVID-19. While Spearman's rank correlation coefficient was used to evaluate the relationship between knowledge, attitude, and practice. Correlations were interpreted using the following criteria:0–0.25 = weak correlation, 0.25–0.5 = fair correlation, 0.5–0.75 = good correlation and greater than 0.75 = excellent correlation
Binary logistic regression analysis was used to identify potential associated factors between dependent and independent variables. Multivariate logistic regression analysis was used to determine the association of the combination of risk factors with attitude and knowledge. All variables with a p < 0.25 in univariate analysis were entered jointly into multivariate logistic regression. Odds ratios (ORs) and 95% confidence intervals were then calculated. A p value less than 0.05 was considered significant. Model fit was assessed using the Hosmer-Lemeshow goodness of fit test.
Ethical consideration
Ethical clearance and approval was obtained from Dilla University Institutional Review Board (Dilla, Ethiopia; protocol: 007/20-12; Dec 20/2019). Written informed consent was obtained from respondents who participated in the study. All the information was kept confidential, and no individual identifiers were collected. The methodology in this study followed the international guidelines for observational studies according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) 2010 statement (see Supplemental file 1 for the detailed checklist of STROBE criteria).
Result
A total of 397 healthcare workers were interviewed in this research, which yields a response rate of 94%. More than half of 203 (51.1%) participants were between 26 and 30 years old, with a mean age of 29.28 ± 5.44. The majority, 225 (56.7%) of the participants were males. Most respondents (35.5%) were nurses, and 16% were physicians. Seventy-six (19.1%) participants had a history of traveling in the last month as seen in Table 1.
Table 1.
Sociodemographic characteristics of health workers.
| Variable | Number | Percent | |
|---|---|---|---|
| Age | >25 | 97 | 24.4 |
| 26–30 | 203 | 51.1 | |
| >30 | 97 | 24.4 | |
| Gender | Female | 172 | 43.3 |
| Male | 225 | 56.7 | |
| Level of education | Diploma | 72 | 18.1 |
| BSc degree | 249 | 62.7 | |
| Masters and above | 76 | 19.1 | |
| Marital status | Married | 186 | 46.9 |
| Unmarried | 211 | 53.1 | |
| Religion | Orthodox | 273 | 68.8 |
| Catholic | 6 | 1.5 | |
| Protestant | 84 | 21.2 | |
| Muslim | 30 | 7.6 | |
| Others** | 4 | 1.0 | |
| Profession | Physician | 63 | 15.9 |
| Anesthetist | 102 | 25.7 | |
| Nurse | 141 | 35.5 | |
| Pharmacy | 26 | 6.5 | |
| Others* | 65 | 16.4 | |
| Work experience | >5 years | 104 | 26.2 |
| 2–5 years | 141 | 35.5 | |
| <2 years | 152 | 38.3 | |
| Training on COVID-19 | Yes | 26 | 6.5 |
| No | 371 | 93.5 | |
| Travel history | Yes | 76 | 19.1 |
| No | 321 | 80.9 | |
| Chronic medical illness | Yes | 30 | 7.6 |
| No | 367 | 92.4 |
= medical laboratory, midwifery, and public health.
= Wakefeta.
Knowledge of HCWs toward COVID-19
This study revealed that 350 (88.2%) participants had good knowledge about COVID-19. The respondents' correct answer rates on the manifestation of COVID-19 were 66.5%. Approximately, 75.5% and 82.6% of participants said that COVID-19 has no specific treatment or vaccine, respectively.
Attitude of HCWs toward COVID-19
We found that 376 (94.7%) participants had a positive attitude toward COVID-19. The majority (75.6%) of respondents said that COVID-19 is a seriously dangerous disease, and 69.3% perceived that they were at high risk of contracting the disease. Approximately 51.4% of respondents believed that taking hot drinks prevented COVID-19 infection, 38.5% of respondents said COVID-19 would not spread in hot climate areas, and 15.4% of respondents believed herbal medication would cure COVID-19.
Practice of HCWs toward COVID-19
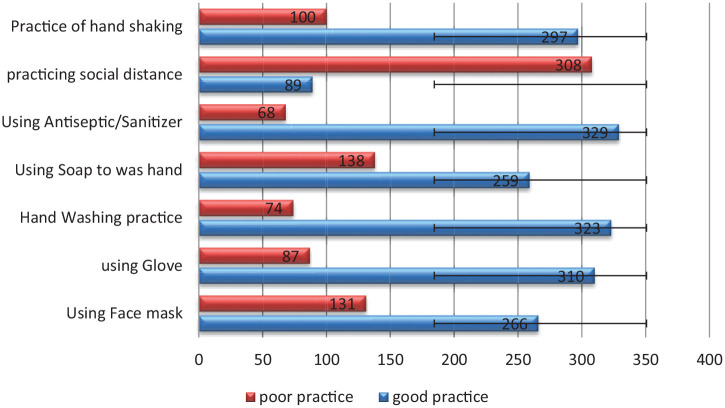
This study showed that 252 (63.5%) of participants had good practice toward COVID-19 and its prevention. Based on our results, 67.3% of respondents were using a facemask, 81.4% were practicing handwashing, and only 22.4% of respondents were practicing social distance as seen in a Figure 1.
Figure 1.
Practice of health workers toward COVID-19 and prevention.
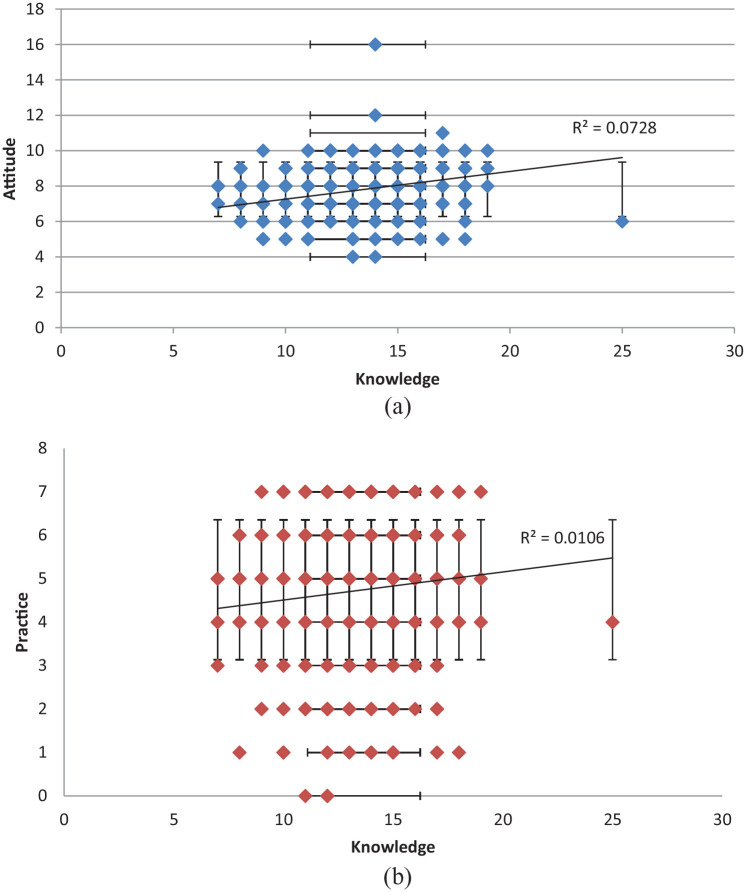
Correlation between knowledge, attitude, and practice
Our study revealed that there was a weak positive correlation between knowledge, attitude, and practice toward COVID-19 disease (r = 0.13, 95% confidence interval (CI) = 3.1–5.2, p ⩽ 0.001). This indicates that the impact of knowledge and attitude on practice was very small as seen in a Figure 2.
Figure 2.
Correlation scatter among knowledge, attitude, and practice in Ethiopian healthcare workers: (a): knowledge vs attitude and (b): knowledge vs practice.
Factors associated with knowledge
Among the independent variables that were assessed, having a history of chronic medical illness was associated negatively with the knowledge level of HCWs, and the source of information (social media/Internet, government, television/radio, telecommunication, and peer) was associated with good knowledge level in the bivariable analysis (OR: 4.7, 95% CI: 2.5–8.8, OR: 2.5, 95% CI: 1.3–50, OR: 3.3, 95% CI: 1.8–6.3, OR: 7.3, 95% CI: 3.0–17.6 and OR: 4.6, 95% CI: 1.6–13.3). The multivariable analysis revealed that the use of social media, telecommunication, and television/radio as a source of information were significantly associated with knowledge (OR: 3.4, 95% CI: 1.5–7.4, OR: 4.3, 95% CI: 1.3–14.3 and OR: 3.2, 95% CI: 1.4–7.2) as seen in Table 2.
Table 2.
Univariate and multivariate logistic regression analysis showing predictors of knowledge about COVID-19 (good vs poor) (N = 397).
| Variable | COVID-19 knowledge |
COR | AOR | ||
|---|---|---|---|---|---|
| Good | Poor | ||||
| Age | >25 | 89 (91.8%) | 8 (8.2%) | 2.198 (.893–5.408) | 1.837 (.458–7.361) |
| 26–30 | 180 (88.7%) | 23 (11.3%) | 1.546 (.776–3.082) | 1.278 (.495–3.295) | |
| >30 | 81 (83.5%) | 16 (16.5%) | Ref | Ref | |
| Gender | Female | 152 (88.4%) | 20 (11.6%) | 1.036 (.560–1.918) | |
| Male | 198 (88.0%) | 27 (12.0%) | Ref | ||
| Level of education | Diploma | 62 (86.1%) | 10 (13.9%) | Ref | Ref |
| BSc degree | 216 (86.7%) | 33 (13.3%) | 1.056 (.493–2.261) | .525 (.206–1.337) | |
| Masters and above | 72 (94.7%) | 4 (5.3%) | 2.903 (.867–9.719) | .931 (.213–4.073) | |
| Marital status | Married | 162 (87.1%) | 24 (12.9%) | .826 (.449–1.519 | |
| Unmarried | 188 (89.1%) | 23 (10.9%) | Ref | ||
| Religion | Orthodox | 245 (89.7%) | 28 (10.3%) | 2.917 (.293–28.995) | |
| Catholic | 5 (83.3%) | 1 (16.7%) | 1.667 (.074–37.728) | ||
| Protestant | 69 (82.1%) | 15 (17.9%) | 1.533 (.149–15.776) | ||
| Muslim | 28 (93.3%) | 2 (6.7%) | 4.667 (.320–68.032) | ||
| Others | 3 (75.0%) | 1 (25.0%) | Ref | ||
| Work experience | >5 years | 128 (84.2%) | 24 (15.8%) | .762 (.368–1.575) | 1.622 (.497–5.288) |
| 2–5 years | 131 (92.9%) | 10 (7.1%) | 1.871 (.787–4.452) | 2.738 (.960–7.810) | |
| <2 years | 91 (87.5%) | 13 (12.5%) | Ref | Ref | |
| Training on COVID-19 | Yes | 20 (76.9%) | 6 (23.1%) | .414 (.157–1.091) | .572 (.166–1.970) |
| No | 330 (88.9%) | 41 (11.1%) | Ref | Ref | |
| Travel history | Yes | 67 (88.2%) | 9 (11.8%) | 1.000 (.461–2.167) | |
| No | 283 (11.8%) | 38 (88.2%) | Ref | ||
| Chronic medical illness | Yes | 20 (66.7%) | 10 (33.3%) | .224 (.098–.515) | .193 (.063–.593) |
| No | 330 (10.1%) | 37 (89.9%) | Ref | Ref | |
| Social media as a source of information | Yes | 272 (93.2%) | 20 (6.8%) | 4.708 (2.506–8.845) | 3.408 (1.563–7.428) |
| No | 78 (74.3%) | 27 (25.7%) | Ref | Ref | |
| Government as a source of information | Yes | 173 (93.0%) | 13 (7.0%) | 2.556 (1.305–5.009) | 1.375 (.572–3.307) |
| No | 177 (83.9%) | 34 (16.1%) | Ref | Ref | |
| Television/Radio | Yes | 262 (92.3%) | 22 (7.7%) | 3.383 (1.817–6.300) | 3.266 (1.465–7.282) |
| No | 88 (77.9%) | 25 (22.1%) | Ref | Ref | |
| Telecommunication | Yes | 181 (96.8%) | 6 (3.2%) | 7.319 (3.030–17.679) | 4.328 (1.308–14.316) |
| No | 169 (80.5%) | 41 (19.5% | Ref | Ref | |
| Peer | Yes | 106 (96.4%) | 4 (3.6%) | 4.670 (1.635–13.340) | .967 (.235–3.984) |
| No | 244 (85.0%) | 43 (15.0%) | Ref | Ref | |
| Religious place | Yes | 84 (90.3%) | 9 (9.7%) | 1.333 (.619–2.871) | |
| No | 266 (87.5%) | 38 (12.5%) | Ref | ||
AOR: adjusted odds ratio; COR: crude odds ratio.
Factors associated with attitude
The multivariable analysis results of this study showed that only a history of chronic illness had a statistically significant association with the attitude toward COVID-19 at a 5% level of significance as seen in Table 3. Regarding the confidence of HCWs in treating confirmed COVID-19, the level of knowledge was significantly associated (OR: 2.3, 95% CI: 1.17–4.54, p = 0.15). In addition, HCWs with good knowledge levels were associated with maintaining self-isolation and visiting hospitals if they manifested symptoms of COVID-19.
Table 3.
Univariate and multivariate logistic regression analysis showing predictors of attitude about COVID-19 (good vs poor) (N = 397).
| Variable | COVID-19 Attitude |
COR (95% CI) | AOR (95% CI) | ||
|---|---|---|---|---|---|
| good | Poor | ||||
| Age | >25 | 91 (93.8%) | 6 (6.2%) | .652 (.178–2.388) | |
| 26–30 | 192 (94.6%) | 11 (5.4%) | .751 (.233–2.421) | ||
| >30 | 93 (95.9%) | 4 (4.1%) | Ref | ||
| Gender | Female | 163 (94.8%) | 9 (5.2%) | 1.020 (.420–2.480) | |
| Male | 213 (94.7%) | 12 (5.3%) | Ref | ||
| Level of education | Diploma | 66 (91.7%) | 6 (8.3%) | Ref | |
| Bsc degree | 235 (94.4%) | 14 (5.6%) | 1.526 (.564–4.126) | .208 (.023–1.860) | |
| Masters and above | 75 (98.7%) | 1 (1.3%) | 6.818 (.800–58.107) | .322 (.040–2.605) | |
| Marital status | Married | 180 (96.8%) | 6 (3.2%) | 2.296 (.872–6.045) | 1.643 (.544–4.964) |
| Unmarried | 196 (92.9%) | 15 (7.1%) | Ref | Ref | |
| Religion | Orthodox | 257 (94.1%) | 16 (5.9%) | ||
| Catholic | 6 (100.0%) | 0 (0.0%) | |||
| Protestant | 80 (95.2%) | 4 (4.8%) | |||
| Muslim | 29 (96.7%) | 1 (3.3%) | |||
| Others | 4 (100.0%) | 0 (0.0%) | |||
| Work experience | >5 years | 146 (96.1%) | 6 (3.9%) | 2.589 (.911–7.359) | 2.246 (.662–7.617) |
| 2–5 years | 136 (96.5%) | 5 (3.5%) | 2.894 (.958–8.739) | 2.463 (.772–7.862) | |
| <2 years | 94 (90.4%) | 10 (9.6%) | Ref | Ref | |
| Training on COVID-19 | Yes | 26 (100.0%) | 0 (0.0%) | ||
| No | 350 (94.3%) | 21 (5.7%) | |||
| Travel history | Yes | 74 (97.4%) | 2 (2.6%) | 2.328 (.530–10.216) | |
| No | 302 (94.1%) | 19 (5.9%) | Ref | ||
| Chronic medical illness | Yes | 25 (83.3%) | 5 (16.7%) | .228 (.077–.673) | .217 (.069–.690) |
| No | 351 (95.6%) | 16 (4.4%) | Ref | Ref | |
| Social media as a source of information | Yes | 278 (95.2%) | 14 (4.8%) | 1.418 (.556–3.617) | |
| No | 98 (93.3%) | 7 (6.7%) | Ref | ||
| Government as source of information | Yes | 175 (94.1%) | 11 (5.9%) | .791 (.328–1.908) | |
| No | 201 (95.3%) | 10 (4.7%) | Ref | ||
| Television/radio | Yes | 268 (94.4%) | 16 (5.6%) | .775 (.277–2.169) | |
| No | 108 (95.6%) | 5 (4.4%) | Ref | ||
| Telecommunication | Yes | 178 (95.2%) | 9 (4.8%) | 1.199 (.493–2.912) | |
| No | 198 (94.3%) | 12 (5.7%) | Ref | ||
| Peer | Yes | 102 (92.7%) | 8 (7.3%) | .605 (.244–1.502) | |
| No | 274 (95.5%) | 13 (4.5%) | Ref | ||
| Religious place | Yes | 85 (91.4%) | 8 (8.6%) | .475 (.190–1.183) | .494 (.189–1.289) |
| No | 291 (95.7%) | 13 (4.3%) | Ref | Ref | |
AOR: adjusted odds ratio; CI: confidence interval; COR: crude odds ratio.
Discussion
Healthcare workers are frontline workers who are directly involved in COVID-19 prevention and treatment in Ethiopia and other countries, and their ability to systematically react to the disease in their community and treatment center will depend on their knowledge, attitude, and practice of healthcare workers. To the best of our understanding, this is the first study investigating KAP toward COVID-19 and its prevention among healthcare workers of teaching and referral hospitals of Ethiopia. This study was conducted to fill the gap in the literature and provide a reference on KAP among health care workers. We found that the majority of the participants (88.2%) had good knowledge about COVID-19-related issues. This finding is consistent with a report by other studies that approximately 90% of healthcare workers knew COVID-19.14–16 This high percentage of knowledge about COVID-19 among healthcare workers is due to prolonged exposure to information since its a global topic of discussion in the media and public. Another reason could be the effort of the government and media in providing information starting from the time of the outbreak. This is strengthened by the association of source of information with knowledge regarding COVID-19, and it is similar to the finding of other studies. 17
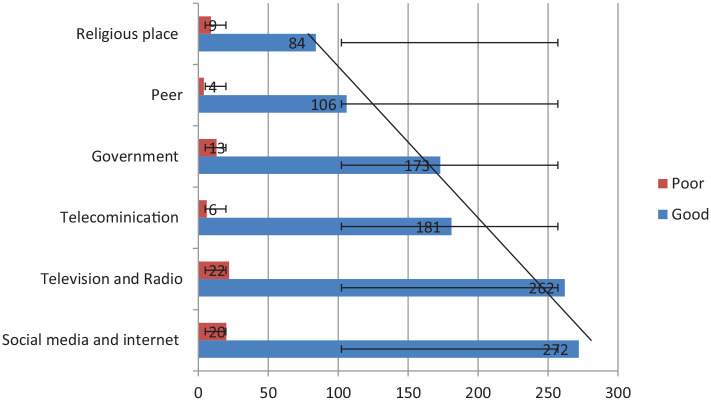
We found that the majority of healthcare workers gathered information regarding COVID-19 from social media (73.6%) and television (71.5%) as seen in Figure 3. This differs from previously published findings in Saudi Arabia, where the website of the Ministry of Health is the main source of information. 18 Our study showed that the source of information has a positive relationship with HCW knowledge. For instance, 93% of social media users have good knowledge compared to those not using social media (74%) as source knowledge for the disease. Similar findings were reported from previous studies in Vietnam, 19 but different from studies in Saudi Arabia (36%) and the UAE (40%), in which a relatively small percentage of HCWs used social media as a source of information about COVID-19.18,20,21 This might be because, during the SARS outbreak, the issue was not a global concern like COVID-19.
Figure 3.
Distribution source of information and knowledge of healthcare workers concerning COVID-19.
The majority of HCWs are aware that patients with comorbid illness are at high risk of infection and mortality from COVID-19, which accounts for approximately 91.1%. The finding of our study is also consistent with the finding of Vietnam healthcare workers’ knowledge of COVID-19. 19
This study showed that there is a significant association between sources of information (social media, telecommunication, and television/radio) and HCWs’ knowledge about COVID-19. This is also similar to the findings of studies in Vietnam and China.17,19,22
Those who use social media as a source of information had approximately three times more chances of having good knowledge about COVID-19 than those not using social media as a source of information. This result is in line with studies conducted in China, Vietnam, Iran, and Indonesia in which the main source of knowledge was social media.14,17,19,23 On the contrary, a study from Saudi and UAE showed that only a small percentage of HCWs used social media as a source of knowledge about COVID-19.18,20 This might be due to the use of global crises of outbreak social media platforms as a facilitator and distributor of COVID-19-related information for HCWs during this critical time. The other reason for the difference could be that the study was performed during the active phase of the outbreak when HCWs were exposed to much information about the disease. We understand from this that social media is a great way of providing the latest update about this COVID-19 pandemic for individuals and the community.
Furthermore, our study revealed that HCWs’ knowledge of COVID-19 was positively correlated with having a positive attitude and good practice toward COVID-19 and its prevention technique. This finding is in line with study done in Indonesia. 24 In addition, HCWs with good knowledge of COVID-19 were significantly associated with the confidence of treating confirmed cases of COVID-19 and maintaining self-isolation if they manifest symptoms of the disease. Our findings are consistent with a previous KAP study in China. 15
Regarding knowledge related to vaccination, this study found 82.6% of participants answered as there was no specific vaccine for COVID-19 during the study period. The result was higher than a cross-sectional study done in India where only 58.9% of health care professionals knew there is no vaccine during the study period. 25 A possible variation for this is our study was done in a tertiary hospital where the majority of the campaign against COVID-19 is made. A higher result compared to this study was observed in China, with 89% of health care workers knew the vaccine availability for COVID-19 during the study period. Although the study was done similarly during the early outbreak, the variation was because China had early exposure to the virus as the information regarding treatment and vaccine is affected by this. 19
In this study, the overall positive attitude toward COVID-19 was 94.7% among Ethiopian healthcare workers. This was significantly lower among HCWs with comorbid illnesses. Although attitudes toward COVID-19 were positive, most HCWs (69.6%) perceived that they were at high risk of contracting the disease, and approximately 75% recognized that COVID-19 is a seriously dangerous disease. This perception is possibly related to the shortage of personal protective equipment and inadequate training on COVID-19 in the country.
Approximately, 63% of healthcare workers had good practice toward prevention methods of coronavirus disease; approximately 67% of HCWs wore facemask in public, and 36.4% practiced frequent handwashing with soap. However, these practices toward COVID-19 were lower than the practice of many other countries.15,17,21,26 The possible reason for this difference might be due to the shortage of infrastructure and inadequate training provided for the healthcare workers. This suggests that further implementation and encouragement from the government is required for the application of good practice toward COVID-19 and its preventions.
Regarding the practice of health care professionals, this study shows 81.4% were practicing handwashing with alcohol and soap. This result was lower compared to a study by Gambhir RS et al., where 94.2% of health care professionals were using alcohol rub or soap and water to clean their hands after treating patients. Variation might be due to prior exposure to similar outbreak and difference in hospital protocol. 27
This study has some limitations. One of the limitations is that bias occurred as a result of the study design (cross-sectional) since the study took the information at specified time points, and cause and effect associations cannot be studied. To reduce this potential bias, different mechanisms were used. The other limitation was the lack of sufficient similar studies, which limits comparison with other studies. However, identifying knowledge gaps, attitudes, and practices can be used to develop effective interventions and establish baseline levels to set priorities for program managers. Finally, the study pinpointed ways of information dissemination or by whom to disseminate, which are very important for the preparation and prevention of disease.
Conclusion
In conclusion, the majority of healthcare workers in Ethiopia appeared to have good knowledge and a positive attitude about COVID-19 despite relatively poor practice regarding COVID-19 prevention during the outbreak. In addition, sources of information (social media/Internet, television, and telecommunication) have a positive association with the knowledge of HCWs regarding COVID-19. Further study is needed to be done to evaluate factors that contribute to the practice of healthcare workers.
Supplemental Material
Supplemental material, sj-pdf-1-smo-10.1177_20503121211034389 for Knowledge, attitude, and practice of healthcare workers toward COVID-19 and its prevention in Ethiopia: A multicenter study by Bedru Jemal, Zemedu Aweke, Simeneh Mola, Sileshi Hailu, Sileshi Abiy, Getahun Dendir, Abere Tilahun, Biruk Tesfaye, Agmuas Asichale, Derartu Neme, Teshome Regasa, Hailemariam Mulugeta, Kassaw Moges, Mohamedrabi Bedru, Siraj Ahmed and Diriba Teshome in SAGE Open Medicine
Footnotes
Authors’ contributions: B.J., Z.A., and S.M.: substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data. S.H., S.A., G.D., A.T., B.T., and D.T. drafted the article or substantively revised it critically for important intellectual content. A.A., D.N., T.R., H.M., K.M., and M.B. contributed to the creation of new software used in the work. All authors have approved the submitted version and any substantially modified version that involves the author's contribution to the study; agreed both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from the Institutional Review Board of Dilla University College of Health Sciences and Medicine with protocol number Ref protocol: duchm/irb/007/19-12; on 20 December, 2019.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from all subjects before the study.
ORCID iDs: Bedru Jemal  https://orcid.org/0000-0002-4194-4724
https://orcid.org/0000-0002-4194-4724
Diriba Teshome  https://orcid.org/0000-0001-5449-5262
https://orcid.org/0000-0001-5449-5262
Availability of data and material: The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Supplemental material: Supplemental material for this article is available online.
References
- 1. World Health Organization. Global surveillance for COVID-19 disease caused by human infection with novel coronavirus (COVID-19): interim guidance, 27 February 2020. Geneva: World Health Organization, 2020. [Google Scholar]
- 2. Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020; 579(7798): 270–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chan JFW, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 2020; 395(10223): 514–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of Novel coronavirus–infected pneumonia. New Engl J Med 2020; 382(13): 1199–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chan JFW, Lau SKP, Woo PCY. The emerging novel Middle East respiratory syndrome coronavirus: the “knowns” and “unknowns.” J Formos Med Assoc 2013; 112(7): 372–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zumla A, Chan JFW, Azhar EI, et al. Coronaviruses — drug discovery and therapeutic options. Nat Rev Drug Discov 2016; 15(5): 327–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Yin Y, Wunderink RG. MERS, SARS and other coronaviruses as causes of pneumonia. Respirology 2018; 23(2): 130–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395(10223): 497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA 2020; 323(11): 1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) Outbreak in China. JAMA 2020; 323(13): 1239. [DOI] [PubMed] [Google Scholar]
- 11. Bedford J, Enria D, Giesecke J, et al. COVID-19: towards controlling of a pandemic. Lancet 2020; 395(10229): 1015–1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Richard G. Reviewing Ethiopia’s health system development. JMAJ 2009; 52(4): 279–286. [Google Scholar]
- 13. Kombe G, Galaty D, Gadhia R, et al. The Human and financial resource requirements for scaling up HIV/AIDS services in Ethiopia. Bethesda, MD: The Partners for Health Reformplus Project, Abt Associates Inc, 2005. [Google Scholar]
- 14. Erfani A, Shahriarirad R, Ranjbar K, et al. Knowledge, attitude and practice toward the novel coronavirus (COVID-19) outbreak: a population-based survey in Iran. Bull World health Organ. Epub ahead of print 30 March 2020. DOI: 10.247/BLT.20.256651. [DOI] [Google Scholar]
- 15. Zhou M, Tang F, Wang Y, et al. Knowledge, attitude and practice regarding COVID-19 among health care workers in Henan, China. J Hosp Infect 2020; 105: 183–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Saqlain M, Munir MM, Rehman S, et al. Knowledge, attitude, practice and perceived barriers among healthcare professionals regarding COVID-19: a cross-sectional survey from Pakistan. medRxiv, 2020, https://www.medrxiv.org/content/10.1101/2020.04.13.20063198v2 [DOI] [PMC free article] [PubMed]
- 17. Zhong B-L, Luo W, Li H-M, et al. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci 2020; 16(10): 1745–1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Asaad A, El Sokkary R, Alzamanan M, et al. Knowledge and attitudes towards Middle East respiratory sydrome-coronavirus (MERS-CoV) among health care workers in south-western Saudi Arabia. Eastern Med Health J 2020; 26(4): 435–442. [DOI] [PubMed] [Google Scholar]
- 19. Huynh G, Nguyen TNH, Vo KN, et al. Knowledge and attitude toward COVID-19 among healthcare workers at District 2 Hospital, Ho Chi Minh City. Asian Pacific J Tropical Med 2020; 13(6): 260. [Google Scholar]
- 20. Abbag HF, El-Mekki AA, Al Bshabshe AAA, et al. Knowledge and attitude towards the Middle East respiratory syndrome coronavirus among healthcare personnel in the southern region of Saudi Arabia. J Infect Public Health 2018; 11(5): 720–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bhagavathula AS, Aldhaleei WA, Rahmani J, et al. Novel coronavirus (COVID-19) knowledge and perceptions: a survey of healthcare workers. medRxiv, 2020, https://www.medrxiv.org/content/10.1101/2020.03.09.20033381v2
- 22. Shi Y, Wang J, Yang Y, et al. Knowledge and attitudes of medical staff in Chinese psychiatric hospitals regarding COVID-19. Brain Behav Immun Health 2020; 4: 100064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Adella Halim D, Kurniawan A, Agung FH, et al. Understanding of young people about COVID-19 during early outbreak in Indonesia. Asia Pac J Public Health 2020; 32(6–7): 363–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rizki SA, Kurniawan J, Budimulia P, et al. Knowledge, attitude, and practice in indonesian health care workers regarding COVID-19. Asia Pac J Public Health. Epub ahead of 19 April 2021. DOI: 10.1177/10105395211011017. [DOI] [PubMed] [Google Scholar]
- 25. Parikh PA, Shah BV, Phatak AG, et al. COVID-19 pandemic: knowledge and perceptions of the public and healthcare professionals. Cureus 2020; 12(5): e8144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kumar J, Katto MS, Siddiqui AA, et al. Knowledge, attitude, and practices of healthcare workers regarding the use of face mask to limit the spread of the new coronavirus disease (COVID-19). Cureus 2020; 12: e7737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Singh Gambhir R, Singh Dhaliwal J, Aggarwal A, et al. Covid-19: a survey on knowledge, awareness and hygiene practices among dental health professionals in an Indian scenario. Rocz Panstw Zakl Hig 2020; 71(2): 223–229. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-smo-10.1177_20503121211034389 for Knowledge, attitude, and practice of healthcare workers toward COVID-19 and its prevention in Ethiopia: A multicenter study by Bedru Jemal, Zemedu Aweke, Simeneh Mola, Sileshi Hailu, Sileshi Abiy, Getahun Dendir, Abere Tilahun, Biruk Tesfaye, Agmuas Asichale, Derartu Neme, Teshome Regasa, Hailemariam Mulugeta, Kassaw Moges, Mohamedrabi Bedru, Siraj Ahmed and Diriba Teshome in SAGE Open Medicine