Case Report
A 78-year-old man presented with tearing chest pain with associated dyspnoea and dysphagia. He was an ex-smoker with no personal or family history of connective tissue disorders. CT angiography illustrated an aberrant right subclavian artery, coursing posterior to the trachea and oesophagus, with an associated 4.4 cm Kommerell’s diverticulum (Figure 1). Imaging also illustrated tracheal stenosis and oesophageal compression. A coronary angiogram demonstrated severe double vessel coronary artery disease. A staged procedure with aortic arch debranching and CABG (Figure 2), followed by a thoracic stent graft and Amplatzer plug to address the Kommerrel’s diverticulum was undertaken.
Figure 1: CT Reconstruction Illustrating Kommerell’s Diverticulum and an Aberrant Right Subclavian Artery.
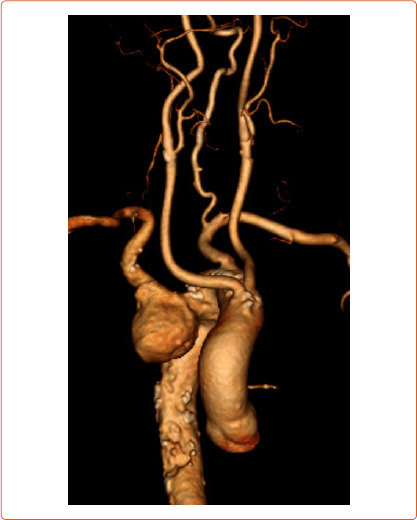
Figure 2: CT Reconstruction Illustrating a Debranched Left Common Carotid Artery and Subclavian Artery.
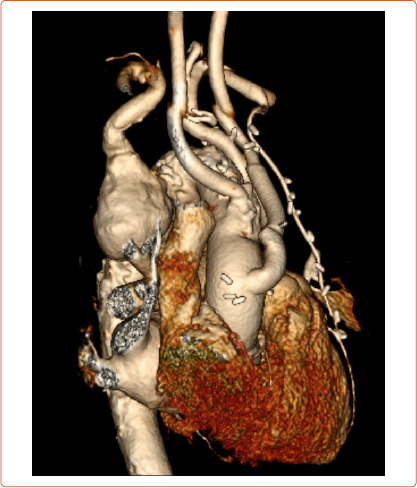
There is a double coronary artery bypass graft (left internal mammary artery to left anterior descending, and saphenous vein T graft to obtuse marginal artery).
His post-operative recovery was complicated by AF, hospital acquired pneumonia and delirium requiring reintubation for severe agitation. There was no immediate noticeable difference in swallowing; however, his breathing had improved.
Given CT angiography illustrated a non-dominant right vertebral artery, with known collateralisation to the arm, a decision was made not to perform a carotid subclavian bypass. Unfortunately, at routine 4-week follow-up the patient reported pre-syncopal episodes with associated right-hand paraesthesia, likely explained by vertebral-basilar insufficiency. A right carotid-subclavian artery bypass was performed to correct this.
There were no immediate post-operative complications and the patient was discharged home. At 6-week follow-up, he had improved right hand symptoms with no further pre-syncopal episodes and had improved swallow.
Figure 3: Angiography Illustrating Kommerell’s Diverticulum Before and After Deployment of Amplatzer Plug to Right Subclavian and Thoracic Aortic Stent Graft.

Discussion
Given the scarce evidence base, management should be tailored on a case by case basis to the individual patient. Surgical treatment remains controversial and should be considered if patients are symptomatic with some suggestion of a Kommerell’s diverticulum of >3cm being an indication for operating in a low-risk patient.[1] Open, endovascular and hybrid procedures have all been successfully performed with acceptable rates of morbidity and mortality.[2] This suggests that the choice of treatment should be tailored to the patient-specific anatomy, associated morbidity, and expertise of the treating surgical team.[5]
References
- 1.Vinnakota A,, Idrees JJ,, Rosinski BF, et al. Outcomes of repair of Kommerell diverticulum. Ann Thorac Surg. 2091;108:1745–50. doi: 10.1016/j.athoracsur.2019.04.122. [DOI] [PubMed] [Google Scholar]
- 2.Tanaka A,, Milner R,, Ota T. Kommerell’s diverticulum in the current era: a comprehensive review. Gen Thorac Cardiovasc Surg. 2015;63:245–59. doi: 10.1007/s11748-015-0521-3. [DOI] [PubMed] [Google Scholar]
- 3.Idrees J,, Keshavamurthy S,, Subramanian S, et al. Hybrid repair of Kommerell diverticulum. J Thorac Cardiovasc Surg. 2014;147:973–6. doi: 10.1016/j.jtcvs.2013.02.063. [DOI] [PubMed] [Google Scholar]
- 4.Kieffer E,, Bahnini A,, Koskas F. Aberrant subclavian artery: surgical treatment in thirty-three adult patients. J Vasc Surg. 1994;1:100–11. doi: 10.1016/s0741-5214(94)70125-3. [DOI] [PubMed] [Google Scholar]
- 5.van Bogerijen GH,, Patel HJ,, Eliason JL, et al. Evolution in the management of aberrant subclavian arteries and related Kommerell diverticulum. Ann Thorac Surg. 2015;100:47–53. doi: 10.1016/j.athoracsur.2015.02.027. [DOI] [PubMed] [Google Scholar]
- 6.Youssef A,, Ghazy T,, Kersting S,, Leip JL,, Hoffmann RT,, Kappert U, et al. Management of the left subclavian artery during TEVAR – complications and mid-term follow-up. Vasa. 2018;47:387–92. doi: 10.1024/0301-1526/a000713. [DOI] [PubMed] [Google Scholar]


