Abstract
Objective:
To determine the effectiveness of manualized panic-focused psychodynamic psychotherapy (PFPP) in routine care in Germany.
Method:
German psychoanalysts were trained according to the PFPP manual. Fifty-four consecutive outpatients with panic disorder (with or without agoraphobia) were randomly assigned in a 2:1 ratio to PFPP or cognitive-behavioural therapy (CBT) plus exposure therapy. Subjects (female 57.4%; mean age 36.2 years) had high rates of psychiatric (68.5%) and somatic (64.8%) comorbidity, and previous psychiatric treatments (57.4%). Assessments were performed pre- and posttreatment and at 6-month follow-up. The primary outcome measure was the Panic Disorder Severity Scale.
Results:
Both treatments were highly effective. In patients randomized to PFPP, remission was achieved in 44.4% at termination and by 50% at follow-up (CBT 61.1% and 55.6%, respectively). No significant differences were found. Emotional awareness, a posited moderator of good outcome in psychotherapies, was significantly higher in the CBT group at baseline. It was found to be a strong moderator of treatment effectiveness in both treatments. After adjusting for initial Levels of Emotional Awareness Scale (LEAS) scores, effect sizes (ESs) for the primary outcome were Cohen d = 1.28, from pre- to posttreatment, and d = 1.03, from pretreatment to follow-up, for PFPP, and d = 1.81 and 1.28 for CBT, respectively.
Conclusions:
PFPP was implemented effectively into clinical practice by psychoanalysts in the community in a sample with severe mental illness with large ESs. Assessment of LEAS may facilitate the identification of patients suitable for short-term psychotherapy.
(Clinical Trial Registration Number: German Clinical Trials Register, DRKS00000245; Universal Trial Number, U1111–1112–4245)
Keywords: panic-focused psychodynamic psychotherapy, cognitive-behavioural therapy, panic disorder, agoraphobia, effectiveness, follow-up
Mise en œuvre de la psychothérapie psychodynamique axée sur la panique dans la pratique clinique
Objectif :
Déterminer l’efficacité de la psychothérapie psychodynamique axée sur la panique (PPAP), pratiquée d’après un manuel, dans les soins courants en Allemagne.
Méthode :
Les psychanalystes allemands ont été formés en conformité avec le manuel de PPAP. Cinquante-quatre patients ambulatoires consécutifs souffrant de trouble panique (avec ou sans agoraphobie) ont été affectés au hasard dans un rapport de 2:1 à la PPAP ou la thérapie cognitivo-comportementale (TCC) en plus d’une thérapie d’exposition. Les sujets (femmes 57,4 %; âge moyen 36,2 ans) avaient des taux élevés de comorbidités psychiatriques (68,5 %) et somatiques (64,8 %), et de traitements psychiatriques précédents (57,4 %). Des évaluations ont été exécutées avant et après le traitement, et au suivi de 6 mois. La principale mesure des résultats était l’échelle de gravité du trouble panique.
Résultats :
Les deux traitements ont été très efficaces. Chez les patients affectés à la PPAP, la rémission a été atteinte chez 44,4 % des sujets au terme du traitement, et chez 50 % au suivi (TCC 61,1 % et 55,6 %, respectivement). Aucune différence significative n’a été observée. La conscience émotionnelle, un modérateur présumé de bons résultats en psychothérapie, était significativement plus élevée dans le groupe de la TCC au départ. Elle s’est révélée être un bon modérateur de l’efficacité du traitement dans les deux traitements. Après correction des scores initiaux à l’échelle des niveaux de conscience émotionnelle (LEAS), l’ampleur de l’effet (AE) des premiers résultats était d de Cohen = 1,28, d’avant à après traitement, et d = 1,03, d’avant le traitement au suivi, pour la PPAP, et d = 1,81 et 1,28 pour la TCC, respectivement.
Conclusions :
La PPAP a été mise en œuvre efficacement dans la pratique clinique par des psychanalystes de la communauté dans un échantillon souffrant de grave maladie mentale et présentant de larges AE. L’évaluation par la LEAS peut faciliter l’identification des patients à qui la psychothérapie à court terme convient.
(Numéro d’enregistrement d’essai clinique : German Clinical Trials Register, DRKS00000245; Universal Trial Number, U1111–1112–4245)
Numerous RCTs have established CBT, usually combined with exposure therapy, as the gold standard for effective treatment for panic disorder, with or without agoraphobia.1,2 Mean ESs of CBT were large,1 particularly in RCTs with low (<50% of patients; Cohen d = 1.23), compared with high (>50%; d = 0.83) rates of comorbidity. Psychological treatments, alone or combined with medication, were more effective than pharmacological treatments alone.3 However, a substantial proportion of patients (30% to 50%) do not respond to behavioural treatments or their combination with medications with demonstrated efficacy3,4; considerable proportions (25% to 35%) prematurely terminate treatment3 or relapse after termination.4 CBT has been very effective, yet some patients do not tolerate exposure therapy, a highly effective treatment component of CBT for panic disorder, for somatic (for example, unstable coronary heart disease) or psychological reasons (for example, fear of being overwhelmed).5 Thus there is a strong need to establish alternative and effective psychological treatments, particularly regarding psychodynamic psychotherapy, one of the treatments performed most frequently in clinical practice.
In their RCT, Milrod et al6 demonstrated efficacy of PFPP, a brief, time-limited psychodynamic intervention specifically devised for treatment of panic disorder, with or without agoraphobia. After completion of 12 weeks of this twice-weekly intervention, the reduction of panic severity was significantly greater, compared with patients treated with applied relaxation training, a behavioural intervention shown to be effective in patients with panic disorder.1 Large between-group ESs on the primary outcome PDSS6,7 favoured PFPP (d = 0.95); the proportion of responders (73%) exceeded applied relaxation training substantially (39%). Differences in ESs were particularly large in favour of PFPP in patients with comorbid personality disorders.8
However, additional trials are needed to determine its effectiveness and stability of symptom reduction when implemented into everyday clinical practice by nonresearch therapists. An important and unanswered question addressing the ultimate clinical utility of PFPP is whether community psychoanalysts and psychodynamic therapists, familiar with a long-term therapy model, will be able to administer this time-limited, symptom-focused psychodynamic therapy. Our study sought to address this question.
To test the effectiveness of PFPP as a manualized psychodynamic approach in clinical practice in Germany, we randomly assigned patients with panic disorder to psychoanalysts who attended a training course in this treatment by Dr Milrod and to experienced, certified CBT psychotherapists. To capture the intervention, as delivered in nonresearch settings, we included patients with mental and medical comorbidities (see below) who had failed previous pharmacological or psychological treatments. The purpose of our clinical trial was to determine the effectiveness of PEPP in routine clinical care in Germany.
Method
As we were primarily interested in the effectiveness of implementing PFPP in an RCT, subjects were allocated by an a priori computer-generated list in a 2:1 randomization ratio, either to PFPP or to manualized CBT plus exposure therapy.9 Patient recruitment and evaluation were carried out at the Clinic for Psychosomatic Medicine in Mainz, Germany, between January 2006 and April 2009 (German Clinical Trials Register, DRKS00000245; Universal Trial Number, U1111–1112–4245). Our study was approved by the ethics committee of the statutory physician board of Rhineland-Palatine (reference number 837.317.05 [4975]).
Subjects
To meet inclusion criteria, subjects were diagnosed with primary panic disorder, with or without agoraphobia, according to DSM-IV criteria,10 which includes a minimum of at least one panic attack per month. All subjects signed informed written consent. Further inclusion criteria were age (18 to 60 years), fluency in the German language, and living in the proximity of Mainz. Psychotropic medication, if present, had to be held constant. Psychosis, bipolar disorder, borderline or antisocial personality disorder, active substance abuse, severe medical or neurological disease, precluding exposure therapy and ongoing psychotherapy, were exclusion criteria.
Assessments
Independent, experienced evaluators, blinded to subject condition and therapist orientation, assessed subjects at baseline, at treatment termination, and at 6-month follow-up. All patients were diagnosed by the SCID-I (SCID—Clinician Version10) and SCID-II.11 The primary outcome measure was the PDSS.7,12 This clinician-administered, 7-item instrument reliably assesses the frequency of panic attacks, associated distress, anticipatory anxiety, agoraphobic fear or avoidance, panic-related sensations of fear and avoidance, and work and social impairment; the total score ranges from 0 (no) to 28 (extreme) panic severity and related impairments. The PDSS was analyzed as a continuous as well as a categorical variable. According to recent recommendations,12 we defined response as a 40% reduction from baseline, and remission as a score of less than 5 in patients with panic disorder without agoraphobia and by a score of less than 7 in those with agoraphobia. Other clinician-rated measures included the CGI scale (from 1 = normal to 7 = extremely ill),13 the 21-item HDRS,14 and the HARS, a measure of nonpanic, state anxiety.15
Self-report measures included the SCL-90-R (German version),16 assessing distress in the past week based on a list of somatic and mental dimensions, and the German version of the BDI.17
As many patients do not relate the bodily signs to the subjective experience of panic, we administered the LEAS,18,19 a reliable performance measure, to assess implicit (experiencing affective arousal as bodily sensation or action tendency) and explicit (experiencing affective arousal as a distinct feeling state) emotional awareness. We administered the short version of the LEAS, providing 10 emotion-provoking vignettes: subjects are asked to write down how they would feel in place of the protagonist of the vignette and how the other person involved in the scene would feel. The LEAS has proven sufficient psychometric properties (interrater reliability of r = 0.91), and norms for age, sex, and socioeconomic status have been established.18 We wanted to explore if panic patients with high emotional awareness are easier to engage therapeutically, as they more readily consider their symptoms as indicative of anxiety and engage in the exploration of their emotional meaning from whichever perspective treatment is pitched.
Interventions
As delineated by Milrod et al,6,20 PFPP focuses on underlying emotional meanings of physiological symptoms, including panic attacks, and on current social and emotional functioning. It postulates that panic symptoms carry a specific emotional significance, related to intrapsychic and interpersonal conflicts. People with panic disorder are assumed to have difficulty separating from important attachment figures and in perceiving themselves as being autonomous. Feeling dependent on others, they tend to deny autonomous strivings. Anger is experienced as dangerous, and it is therefore largely excluded from conscious awareness, while simultaneously triggering high levels of anxiety that lead to being overwhelmed by negative affect in panic attacks, perpetuating panic and phobic avoidance. Panic symptoms, in turn, reinforce conflicted interpersonal relationships in which patients feel excessively dependent on significant others, and frightened of losing them. PFPP helps patients to make emotional sense of their physical symptoms, and to recognize that their fears of an upcoming catastrophe reflect an internal conflict related to emotional states, often emerging from situations that trigger emotional states linked to formative relationships, rather than reflecting current reality. This insight is assumed to help them function more autonomously. Conflicted expectations are expected to occur in the interaction with the therapist, and a strong emphasis is placed on work involving transference.
The CBT intervention followed the treatment manual of Schneider and Margraf,9 specifying the following panic-specific treatment components:
Patient education and individual elaboration of the psycho-physiological model: catastrophic misinterpretation of bodily sensations, interoceptive conditioning, and consequent avoidance lead to a self-reinforcing catastrophic vicious circle.
Cognitive interventions aiming at reduction of negative cognitive bias, anticipatory anxiety, and catastrophic misinterpretation.
Construction of an individualized hierarchy of panic symptoms or avoidance eliciting situations or stimuli.
Behavioural experiments and exposure to situations and stimuli eliciting unpleasant physiological sensations to reduce avoidance behaviour, anxiety sensitivity, and conditioned responses to internal and external cues.
Relapse-prevention measures.
Both treatments were performed according to manuals.9,20 PFPP entailed 24 sessions (50 minutes each), twice-weekly, during 12 weeks. CBT was performed during the same time period, with the same total of therapist time (hours); however, exposure sessions varied in length (up to 2 hours); unlike PFPP, additional, individually tailored homework exercises and rehearsals were assigned in CBT.
Therapists
Therapist training was comprised of a 12-hour course on the application of PFPP, with the help of video sequences from treatments conducted by Dr Milrod and her study group. The 7 therapists were MDs or PhD psychologists who had previously undergone at least 5 years of psychodynamic or psychoanalytic training according to standards established by German law. Among the 7 therapists, 4 were in private practice and 3 were senior staff members of the Clinic for Psychosomatic Medicine. CBT was performed by 2 certified behaviour therapists (1 in private practice; 1 staff member of the Clinic). Their behaviour therapy training had included the manual,9 and they had regularly combined CBT and exposure treatments as part of their practice.
PFPP therapists met monthly for group supervision; CBT therapists received comparable frequencies of individual supervision. All treatments were videotaped as a basis for supervision and for later independent assessment of treatment adherence. The number of patients treated varied widely between therapists and conditions; in PFPP, 7 therapists treated between 1 and 6 patients; the 2 CBT therapists treated 3 and 12 patients, respectively.
Data Analysis
Data were analyzed by SPSS version 17.0 (SPSS Inc, Chicago, IL). We used Student t tests for continuous variables and Fisher exact tests for categorical variables. We chose the PDSS as our primary outcome measure. In the ITT analysis, we compared response and remission at posttreatment and at follow-up between PFPP and CBT. We defined dropouts from assessments as treatment failures, coding them as nonresponders. Thus we used a conservative estimate of the response rate. We adjusted continuous outcome data by baseline LEAS scores. The inclusion of LEAS was necessary because, by chance, patients treated in CBT scored significantly higher pretreatment than patients treated by PFPP. In a multiple regression analysis, we determined the effect of baseline symptoms of anxiety, depression, distress, LEAS, and treatment group on outcome. We calculated Cohen d by the pretreatment minus the posttreatment (follow-up) means, divided by the pooled standard deviations. Means were adjusted for initial LEAS scores, estimating the means of the dependent variables when LEAS was held constant (at mean 2.61). For comparisons of independent proportions, we used h, which is the difference between phi of group 1 minus φ of group 2, where φ is an arcsine transformation. Based on the sample size chosen, at alpha 0.05 (2-sided) only a large effect (d = 0.82) could be reliably detected statistically between groups.
Results
Trial Flow and Baseline Characteristics
Figure 1 shows the trial flow. Sixty-one consecutive patients consented to participate. They were identified in our outpatient clinic according to screening criteria out of a total of 221 patients seeking help for panic symptoms, with or without agoraphobia. On evaluation by SCID, a total of 7 patients were excluded, 5 withdrew consent for study participation, and 2 did not meet inclusion criteria. Thus 54 patients were randomized to PFPP (n = 36) or to CBT (n = 18).
Figure 1.
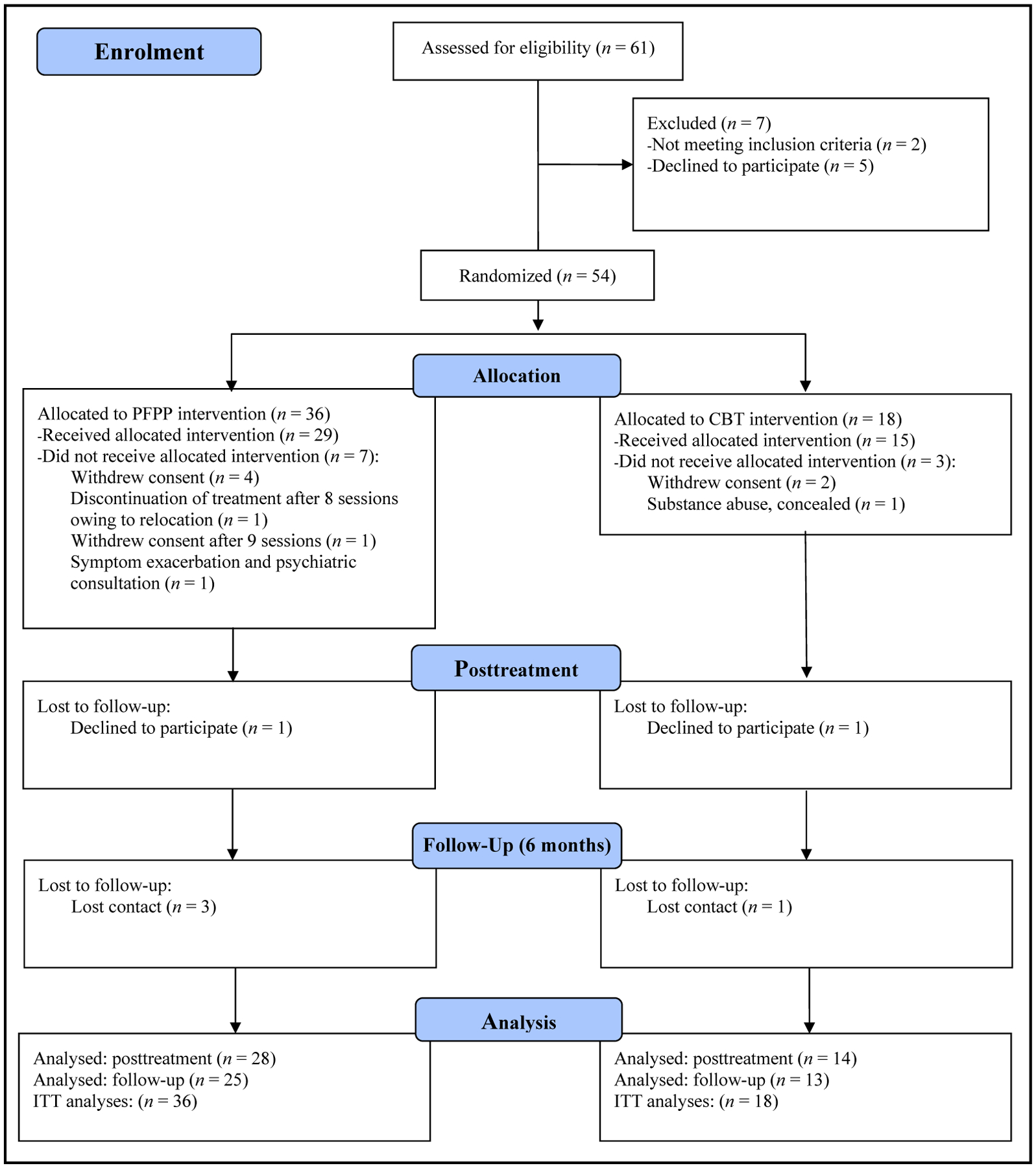
Trial flow
The 2 groups did not differ regarding drop-out rates. Among the PFPP group, 8 patients (22.2%) dropped out: 4 patients withdrew consent and did not initiate treatment, 2 patients discontinued treatment (1 had moved his home, the other 1 discontinued after 9 sessions), 1 patient required psychiatric consultation owing to exacerbation of symptoms, and 1 patient declined posttreatment assessment. Additionally, 3 patients refused follow-up assessment. Among the CBT group, 4 (22%) dropped out: 2 patients did not initiate treatment, 1 patient was excluded owing to a severe alcohol addiction concealed initially, and 1 refused termination assessment. One additional patient refused follow-up assessment. Table 1 shows baseline characteristics. No significant differences were found in demographic variables between the 2 treatment groups.
Table 1.
Baseline characteristics: PFPP, compared with CBT
| Total (n = 54) | PFPP (n = 36) | CBT (n = 18) | |||||
|---|---|---|---|---|---|---|---|
| Characteristic | Mean | SD | Mean | SD | Mean | SD | Pa |
| Age at entry, years | 36.22 | 10.80 | 37.97 | 11.02 | 32.72 | 9.69 | 0.09 |
| Chronicity of panic disorder | 7.67 | 9.25 | 6.92 | 9.43 | 9.17 | 8.95 | 0.41 |
| Global Assessment of Functioning score | 60.78 | 8.94 | 60.25 | 8.45 | 61.85 | 10.01 | 0.54 |
| PDSS score | 12.56 | 4.25 | 12.29 | 4.56 | 13.11 | 3.61 | 0.51 |
| Number of somatic disorders (if present) | 1.91 | 1.20 | 2.08 | 1.35 | 1.55 | 0.69 | 0.25 |
| Average number of treatments (if present) | 1.68 | 1.08 | 1.81 | 1.25 | 1.40 | 0.52 | 0.41 |
| LEAS | 2.61 | 0.54 | 2.48 | 0.52 | 2.87 | 0.45 | 0.01 |
| n | % | n | % | n | % | Pb | |
| Female, sex | 31 | 57.4 | 20 | 55.6 | 11 | 61.1 | 0.78 |
| Agoraphobia | 40 | 74.1 | 26 | 72.2 | 14 | 77.8 | 0.75 |
| Any mental comorbid condition | 37 | 68.5 | 25 | 69.4 | 12 | 66.6 | >0.99 |
| ≥1 Comorbid Axis I disorder | 32c | 59.3 | 21 | 58.3 | 11 | 61.1 | >0.99 |
| ≥1 Comorbid Axis II disorder | 19d | 35.2 | 14 | 38.9 | 5 | 27.8 | 0.55 |
| Comorbid depressive disorder | 12 | 22.2 | 6 | 16.7 | 6 | 33.3 | 0.32 |
| Comorbid somatic disorders | 35e | 64.8 | 24 | 66.7 | 11 | 61.1 | 0.77 |
| Previous psychiatric treatments | 31 | 57.4 | 21 | 58.3 | 10 | 55.6 | >0.99 |
| Antidepressants | 12 | 22.2 | 8 | 22.2 | 4 | 22.2 | >0.99 |
| Anxiolytics | 5 | 9.3 | 4 | 11.1 | 1 | 5.6 | 0.66 |
| Herbal sedatives | 5 | 9.3 | 4 | 11.1 | 1 | 5.6 | 0.66 |
P values according to t tests.
P values according to Fisher exact tests.
Depressive disorder (22%; n = 8 dysthymia, n = 2 recurrent, n = 2 single depressive episode), social phobia (24.1%), generalized anxiety disorder (16.7%), specific phobia (11.1%), somatization disorder (11.1%), alcohol abuse (5.6%), posttraumatic stress disorder (5.6%), eating disorder (3.7%) adjustment disorder (1.9%), depersonalization-derealization syndrome (1.9%)
Personality disorder not otherwise specified (33%; n = 18), avoidant (n = 5), obsessive–compulsive, dependent, or paranoid personality disorder (n = 1)
Neurological (migraine, epilepsy) and medical diseases (kidney, heart transplantation, chronic bowel disease).
The mean age of participants was 36.2 years. The majority (57.4%) were female. Panic symptoms had already lasted an average of 7.7 years. The mean Global Assessment of Functioning score was 60.8 (SD 8.94) and the mean PDSS was 12.56 (SD 4.25), representing patients with moderate illness who can be treated on an outpatient basis.12 The baseline LEAS score was significantly higher for CBT (P < 0.01) than for PFPP. Comorbid conditions and previous psychiatric treatments or medications did not differ between groups (Table 1): 59.3% showed current DSM Axis I comorbidity, including 22.2% with depressive disorders; 35.2% had at least 1 DSM Axis II comorbidity; and somatic diagnoses were present in 64.8% (n = 35). The majority (57.4%) had already undergone at least 1 (up to 5) previous treatments, mainly for panic disorder: 31.5% had received at least 1 inpatient treatment, 29.6% outpatient psychotherapy, and 7.5% had been exclusively treated with medication. At intake, 22.2% of patients were on antidepressants, 9.3% each were on anxiolytics or herbal sedatives, and 27.8% took other medication. Compared with completers, dropouts more often worked full time at treatment termination (88.9% and 41.9%, respectively) (χ2 = 6.58, df = 1, P = 0.02), and they reported a longer history of panic disorder than completers at follow-up (t = 2.40, df = 16.228, P = 0.03). Neither of these 2 variables was associated with outcome.
Primary Outcome
In the ITT analysis (Table 2), response was achieved at termination by PFPP in 47.2% and by CBT in 72.2% (χ2 = 3.04, df = 1, P = 0.15). ESs were φ = 1.51 for PFPP and φ = 2.03 for CBT. The ES difference was h = 0.52 (medium-size effect). At follow-up, the proportion of responders was comparable (47.2% PFPP; 55.6% CBT; χ2 = 0.33, df = 1, P = 0.77). The ESs were φ = 1.51 for PFPP and φ = 1.68 for CBT. ESs did not differ (h = 0.17).
Table 2.
Response and remission of panic symptoms based on the PDSS: treatment termination and follow-up
| Response (treatment termination) | Remission (treatment termination) | |||||
|---|---|---|---|---|---|---|
| Yes, % | No, % | X2, df, (P) | Yes, % | No, % | X2, df, (P) | |
| CBT | 72.2 | 27.8 | 3.04,1, (0.15) | 61.1 | 38.9 | 1.33, 1, (0.39) |
| PFPP | 47.2 | 52.8 | 44.4 | 55.6 | ||
| Response (follow-up) | Remission (follow-up) | |||||
| Yes, % | No, % | X2, df, (P) | Yes, % | No, % | X2, df, (P) | |
| CBT | 55.6 | 44.4 | 0.15, 1, (0.78) | 55.6 | 44.4 | 0.15, 1, (0.78) |
| PFPP | 50.0 | 50.0 | 50.0 | 50.0 | ||
Response: at least 40% reduction in panic symptoms from baseline (PDSS). Remission: a PDSS score of <5 and <7 in subjects with and without agoraphobia, respectively.
At termination, remission was achieved by 44.4% in the PFPP and by 61.1% in the CBT condition (χ2 = 1.33, df = 1, P = 0.39). ESs were φ = 1.46 for PFPP and φ = 1.79 for CBT; there was a small difference between groups (h = 0.33). At follow-up, remission was achieved by PFPP in 50.0%, and by CBT in 55.6% (χ2 = 0.15, df = 1, P = 0.78). ESs between PFPP (φ = 1.57) and CBT (φ = 1.68) did not differ (h = 0.11).
Table 3 shows changes for all outcome measures at treatment termination and at follow-up, separately for PFPP and for CBT, adjusted for the initial LEAS scores.
Table 3.
Changes in primary PDSS and secondary outcome criteria of patients with panic disorder from pretreatment to treatment termination and 6-month follow-up: PFPP, compared with CBT, adjusted for initial LEAS scores
| PFPP | CBT | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable and time point | na | Meanb | SDc | ESd | na | Meanb | SDc | ESd |
| PDSS | ||||||||
| Pre- to posttreatment | 29 | 5.91 | 4.63 | 1.28 | 15 | 8.55 | 4.73 | 1.81 |
| Pretreatment to 6-month follow-up | 27 | 6.45 | 6.29 | 1.03 | 14 | 8.11 | 6.36 | 1.28 |
| CGI | ||||||||
| Pre- to posttreatment | 29 | 1.78 | 1.08 | 1.65 | 15 | 1.70 | 1.10 | 1.55 |
| Pretreatmet to 6-month follow-up | 26 | 1.83 | 1.38 | 1.33 | 14 | 2.39 | 1.38 | 1.73 |
| HARS | ||||||||
| Pre- to posttreatment | 29 | 7.05 | 7.70 | 0.92 | 15 | 11.46 | 7.86 | 1.46 |
| Pretreatment to 6-month follow-up | 26 | 8.14 | 10.15 | 0.80 | 14 | 8.99 | 10.29 | 0.87 |
| HDRS | ||||||||
| Pre- to posttreatment | 29 | 4.38 | 6.68 | 0.66 | 15 | 9.81 | 6.80 | 1.44 |
| Pretreatment to 6-month follow-up | 26 | 5.42 | 7.94 | 0.68 | 14 | 8.94 | 8.04 | 1.11 |
| SCL-90-R Global Severity Index | ||||||||
| Pre- to posttreatment | 28 | 0.20 | 0.42 | 0.48 | 15 | 0.33 | 0.43 | 0.77 |
| Pretreatment to 6-month follow-up | 24 | 0.20 | 0.39 | 0.51 | 11 | 0.36 | 0.42 | 0.86 |
| BDI | ||||||||
| Pre- to posttreatment | 28 | 1.27 | 7.67 | 0.13 | 14 | 3.06 | 7.87 | 0.39 |
| Pretreatment to 6-month follow-up | 24 | 1.75 | 7.97 | 0.22 | 11 | 4.13 | 8.02 | 0.51 |
Completer sample (per-protocol analyses)
Means and SDs are adjusted for pretreatment LEAS scores, by estimating the latent means, with LEAS held constant at the arithmetic average of the whole sample; SDs were calculated from the standard errors of the estimated latent mean (multiplied by the square root of its n);
The reported ES are the quotient between the mean difference score (pretreatment mean minus posttreatment and [or] follow-up mean) divided by its standard deviation (Cohen d). Unadjusted ES for PDSS (posttreatment/follow-up): 1.15/0.95 (PFPP), 2.26/1.61 (CBT); CGI: 1.42/1.22 (PFPP), 1.87/2.16 (CBT); HARS: 0.88/0.66 (PFPP), 1.55/1.51 (CBT); HDRS: 0.60/0.58 (PFPP), 1.58/1.91 (CBT); SCL-90-R Global Severity Index: 0.28/0.45 (PFPP), 1.15/1.03 (CBT); BDI: 0.07/0.23 (PFPP), 0.50/0.49 (CBT).
Scores on the PDSS, the primary outcome measure, declined from pre- to posttreatment and from posttreatment to follow-up. Corrected ESs for PFPP were d = 1.28 and 1.03, respectively. These were d = 1.81 and 1.28, respectively, for CBT (uncorrected ESs in Table 4). A total of 5 (13.2%) participants of the completer sample (3 from PFPP, 2 from CBT) sought additional psychotherapy during follow-up (4 outpatient and 2 inpatient psychotherapy). Two patients from the CBT condition received additional CBT. Two PFPP patients sought inpatient treatment—1 owing to a relapse, 1 after severe psychosocial stress (10-year-old daughter was missing)—1 began a new CBT.
Table 4.
Prediction of change in PDSS scores at treatment termination and at follow-up by multiple regression analysis (forced entry)
| b (SE)a | Pb | |
|---|---|---|
| PDSS score: pre- to posttreatment (n = 44) | ||
| Constant | −5.64 (3.38) | 0.25 |
| LEAS baseline | 2.88 (0.92) | 0.004 |
| Treatment group | −1.10 (1.13) | 0.34 |
| PDSS baseline | 1.04 (0.18) | <0.001 |
| HARS baseline | 0.03 (0.12) | 0.83 |
| CGI baseline | −1.64 (0.62) | 0.01 |
| HDRS baseline | 0.22 (0.15) | 0.16 |
| SCL-90R GSI baseline | −1.72 (2.06) | 0.41 |
| BDI baseline | −0.08 (0.10) | 0.40 |
| Personality disorder | −1.52 (1.23) | 0.22 |
| Agoraphobia | −1.69 (1.23) | 0.18 |
| R2 = 0.65 | ||
| PDSS-score: pretreatment to follow-up (n = 41) | ||
| Constant | −6.69 (6.71) | 0.42 |
| LEAS baseline | 3.20 (2.04) | 0.13 |
| Treatment group | −0.41 (2.09) | 0.84 |
| PDSS baseline | 0.98 (0.34) | 0.007 |
| HARS baseline | 0.16 (0.22) | 0.49 |
| CGI baseline | −1.75 (1.18) | 0.15 |
| HDRS baseline | 0.28 (0.29) | 0.35 |
| SCL-90-R GSI baseline | −2.07 (3.99) | 0.61 |
| BDI baseline | −0.17 (0.11) | 0.37 |
| Personality disorder | −1.16 (2.38) | 0.63 |
| Agoraphobia | −1.58 (2.37) | 0.51 |
| R2 = 0.25 | ||
b: unstandardized regression coefficient and standard error (SE).
P values are not corrected for multiple testing. Completer sample (per protocol analyses).
LEAS, treatment group: 0 = CBT, 1 = PFPP; PDSS, HARS, CGI, HDRS, SCL-90-R Global Severity Index, BDI, comorbid personality disorder, presence of agoraphobia: 0 = no, 1 = yes
Table 4 shows the results of the regression analyses on the changes of the PDSS score, from pre- to posttreatment and from pretreatment to follow-up. LEAS baseline, PDSS baseline, and CGI were predictors explaining 65% of variance of the change of the PDSS score, from pre- to posttreatment. Only PDSS baseline was a predictor from pretreatment to follow-up. Treatment group was not a significant predictor of outcome.
Secondary Outcomes
Both treatments had large effects on global functioning (as measured by the CGI) and on general anxiety (as measured by the HARS); CBT also had a strong effect on depression (as measured by the HDRS, but not the BDI) and distress at follow-up. The other ESs were small to moderate (Table 3). Regarding secondary outcomes, there were moderate ES differences favouring CBT for HARS and HDRS at termination and small ES differences favouring CBT at follow-up (CGI, HDRS, and SCL-90-R).
Discussion
Overall, our study showed that PFPP can be effectively implemented as a short-term treatment for panic disorder, with and without agoraphobia, into routine care in Germany by psychoanalysts who had been trained in and used a long-term PFPP treatment model. Two thirds of our sample had comorbid Axis I or II diagnoses.1 Most of our patients also suffered from comorbid medical conditions and had undergone previous psychiatric treatment, highlighting the severity of the diagnoses.
Based on ITT analysis, 47.2% of the patients who were randomized to PFPP achieved response and 44.4% achieved remission at termination. While not statistically significant, there were small-to-moderate ES differences favouring CBT (response 72.2%, remission 55.6%). At termination, ESs for the PDSS, our primary outcome, were large for both groups (PFPP: d = 1.15; after correcting for initial LEAS scores d = 1.28; CBT: d = 2.26; d = 1.81 after correction). We also demonstrated large treatment effects in both conditions on general anxiety and on psychosocial functioning. PFPP also had moderate effects on depression (HDRS) and small-to-moderate effects on distress. CBT had strong effects on depression (HDRS), moderate-to-large effects on distress, and small-to-moderate effects on the BDI score.
At 6-month follow-up, PFPP continued to be effective as evidenced by stable response and remission (50%) rates, which were comparable to CBT (55.6%). ESs at follow-up were large in both treatments (1.03 for PFPP and 1.28 for CBT). Thus small-to-moderate ES differences of our primary outcome (scores and response and [or] remission rate) at termination favouring CBT were no longer present. PFPP posits that termination constitutes a crisis in treatment enabling the patient to work through issues of separation, which may account for a slightly lower response and (or) remission at termination, while long-term effect on panic symptoms are comparable to CBT.
Limitations
We performed an effectiveness study to determine the feasibility of implementing PFPP into clinical practice in a different language from the one in which it was developed, and in the context of a different health care system. We chose to compare it with gold standard treatment, CBT with exposure therapy as performed by experts in this modality, to evaluate whether dynamic clinicians used to a long-term treatment model could adapt their style effectively to this symptom-focused, time-limited psychoanalytic intervention.20 The 2 CBT therapists had been trained and routinely practiced the manualized study treatment. The most effective CBT therapist carried the highest caseload (n = 12); the high ESs exceeded previous CBT trials with comparably high rates of comorbidity.1 The psychoanalysts in the study were experienced in performing long-term treatments (with high and low frequency), applying short-term psychotherapy only to patients in acute crisis and to determine indication for long-term treatment. They had neither a background in symptom-focused, time-limited treatment nor in PFPP. Future comparative trials will need to strive for better therapist matching. As psychoanalysts in Germany do not routinely perform manualized, short-term training treatments, it will be advisable to have them perform pilot cases before entering patients into a clinical trial. Owing to limited funding, we were restricted to small sample sizes. As our focus was on implementation of a new treatment, randomization was performed in a 2:1 ratio. The study was not powered for detection of nonequivalence of the 2 treatments.
The LEAS reliably and validly assesses different levels of implicit and explicit affect processing, and has been used extensively and standardized in the German population.18,19 For patients experiencing panic seemingly out of the blue, we considered the LEAS a potentially important patient variable. Indeed, baseline LEAS had a strong effect at treatment termination. As we found a significant baseline difference favouring the CBT condition, we took LEAS into account in our statistical analyses. While an interesting finding in itself, however, its effect on outcome was not our primary hypothesis. While most ESs were comparable, several ESs between groups were slightly to moderately larger for CBT at termination, levelling out to follow-up. Note that, in our conservative analysis, as in many CBT trials, over 40% of patients did not respond in the long run to either intervention. Regardless of treatment condition, at follow-up, 13.2% of the sample sought additional treatment. Thus there may be a need for longer treatment interventions in this highly comorbid sample. Stratifying patients by LEAS may be a promising strategy to be tested in future studies.
Clinical Implications
PFPP can be effectively implemented into psychodynamic practice.
Treatment effects are stable at 6-month follow-up.
Awareness of one’s emotions is associated with more benefit from short-term psychotherapy.
Limitations
Our study was not sufficiently powered for an equivalence trial.
Owing to the small sample size, we cannot say which patients benefit most from treatment.
Acknowledgements
No extramural funding was obtained for the study. The authors have no conflict of interest to report. Dr Milrod was paid as a consultant to train study therapists in PFPP. We greatly appreciate the dedicated work of the therapists from private practiced who performed the outpatient treatments: U Bastian, C Lohmeier-Zenz, U Porsch, H Riedell-Heger, and S Benna.
Abbreviations
- BDI
Beck Depression Inventory
- CBT
cognitive-behavioural therapy
- CGI
clinical global impression
- DSM
Diagostic and Statistical Manual of Mental Disorders
- ES
effect size
- HARS
Hamilton Anxiety Rating Scale
- HDRS
Hamilton Depression Rating Scale
- ITT
intention to treat
- LEAS
Levels of Emotional Awareness Scale
- PDSS
Panic Disorder Severity Scale
- PFPP
panic-focused psychodynamic psychotherapy
- RCT
randomized controlled trial
- SCID
Structured Clinical Interview for DSM-IV
- SCL-90-R
Symptom Checklist-90-Revised
References
- 1.Sánchez-Meca J, Rosa-Alcázar AI, Marín-Martínez F, et al. Psychological treatment of panic disorder with or without agoraphobia: a meta-analysis. Clin Psychol Rev. 2010;30:37–50. [DOI] [PubMed] [Google Scholar]
- 2.American Psychiatric Association (APA). Practice guideline for the treatment of patients with panic disorder. 2nd ed. Washington (DC): APA; 2009. [Google Scholar]
- 3.Barlow DH, Gorman JM, Shear MK, et al. Cognitive-behavioral therapy, imipramine, or their combination for panic disorder: a randomized controlled trial. JAMA. 2000;283:2529–2536. [DOI] [PubMed] [Google Scholar]
- 4.Furukawa TA, Watanabe N, Churchill R. Combined psychotherapy plus antidepressants for panic disorder with or without agoraphobia. Cochrane Database Syst Rev. 2007;(1):CD004364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Neudeck P, Lang TH. Reizkonfrontationsmethoden [Exposition methods]. In: Wittchen HU, Hoyer J, editors. Klinische Psychologie & Psychotherapie [Clinical psychology & psychotherapy]. Heidelberg (DE): Springer; 2011. p 530–542. German. [Google Scholar]
- 6.Milrod B, Leon AC, Busch F, et al. A randomized controlled clinical trial of psychoanalytic psychotherapy for panic disorder. Am J Psychiatry. 2007;164:265–272. [DOI] [PubMed] [Google Scholar]
- 7.Shear MK, Brown TA, Barlow DH, et al. Multicenter collaborative Panic Disorder Severity Scale. Am J Psychiatry. 1997;154:1571–1575. [DOI] [PubMed] [Google Scholar]
- 8.Milrod BL, Leon AC, Barber JP, et al. Do comorbid personality disorders moderate panic-focused psychotherapy? An exploratory examination of the American Psychiatric Association practice guideline. J Clin Psychiatry. 2007;68:885–891. [DOI] [PubMed] [Google Scholar]
- 9.Schneider S, Margraf J. Agoraphobie und Panikstörung. Band 3. Fortschritte der Psychotherapie [Agoraphobia and panic disorder. Vol 3. Progress in psychotherapy]. In: Schulte D, Grawe K, Hahlweg K, et al. , editors. Göttingen (DE): Hogrefe Verlag; 1998. German. [Google Scholar]
- 10.First MB, Spitzer RL, Gibbon M, et al. Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version (SCID-CV). Washington (DC): American Psychiatric Press, Inc; 1996. [Google Scholar]
- 11.First MB, Gibbon M, Spitzer RL, et al. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II). Washington (DC): American Psychiatric Press, Inc; 1997. [Google Scholar]
- 12.Furukawa TA, Katherine Shear M, Barlow DH. Evidence-based guidelines for interpretation of the Panic Disorder Severity Scale. Depress Anxiety. 2009;26:922–929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guy W. ECDEU Assessment manual for psychopharmacology. Rockville (MD): US Department of Health and Human Services; 1976. p 218–222. [Google Scholar]
- 14.Hamilton M The Hamilton Depression Rating Scale. J Neurol Neurosurg Psychiatry. 1960;23:56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hamilton M. Anxiety scale (HAMA). In: Collegium Internationale Psychiatriae Scalarum, editor. Internationale Skalen für Psychiatrie [International scales for psychiatry]. Göttingen (DE): Beltz Test GmbH; 1996. German. [Google Scholar]
- 16.Franke GH. SCL-90-R. Die Symptom-Checkliste von Derogatis—Deutsche Version Göttingen (DE): Beltz; 1995. German. [Google Scholar]
- 17.Hautzinger M, Bailer M, Worall H, et al. Beck-Depressions-Inventar, 2. Auflage Göttingen (DE): Hogrefe; 2001. German. [Google Scholar]
- 18.Lane RD, Quinlan DM, Schwartz GE, et al. The Levels of Emotional Awareness Scale: a cognitive-developmental measure of emotion. J Pers Assess. 1990;55:124–134. [DOI] [PubMed] [Google Scholar]
- 19.Subic-Wrana C, Bruder S, Thomas W, et al. Emotional awareness deficits in inpatients of a psychosomatic ward: a comparison of two different measures of alexithymia. Psychosom Med. 2005;67:483–489. [DOI] [PubMed] [Google Scholar]
- 20.Milrod BL, Busch FN, Cooper AM, et al. Manual of panic-focused psychodynamic psychotherapy. Washington (DC): American Psychiatric Press; 1997. [Google Scholar]


