Abstract
Objective:
The consequences of the COVID-19 pandemic may lead to exceptional stress in pregnant women. In order to evaluate stress levels of pregnant woman in this difficult time, the Pandemic-Related Pregnancy Scale (PREPS) was introduced in the US. The present study introduces and validates the German version of the PREPS.
Study Design:
In total, 1364 German-speaking pregnant women from Germany and Switzerland took part in this online cohort study and completed the PREPS as well as gave information on sociodemographic, obstetric and other psychological factors.
Results:
A confirmatory factor analysis of the PREPS showed very good psychometric values and confirmed the structure of the original questionnaire. The PREPS comprises three dimensions: Infection Stress (5 items), Preparedness Stress (7 items) and Positive Appraisal (3 items). Furthermore, correlations between the PREPS and other psychological factors such as Pregnancy Specific Stress and Fear of Childbirth highlight convergent validity. The sensitivity of the questionnaire was demonstrated by its associations with several obstetric and COVID-19 related factors.
Conclusion:
The German PREPS showed good psychometric properties and is a useful instrument for future studies which aim to investigate the impact of pandemic-related stress on birth outcomes and postpartum factors.
Keywords: COVID-19, pandemic, pregnancy, stress, questionnaire
1. Introduction
Pregnancy is a time of many biopsychosocial transformations and challenges, which under certain circumstances, can be associated with significant distress for some women (1, 2). Several studies have highlighted an association between maternal stress during pregnancy and adverse birth outcomes such as preterm birth or low birth weight (3). Prenatal stress can also influence the emotional wellbeing of the mother and lead to adverse outcomes such as postnatal depression (4). The COVID-19 pandemic has had great impact on all areas of life as the lockdown and the social distancing rules led to radical changes in daily life. Although pregnant women are not classified as a high risk population, pandemic constraints and their potential effects have particular impact on pregnant women, leading to exceptional stress (5). Pregnant women face the fear of infection (6), which may harm them, their loved ones and their unborn baby. Although a recent systematic review including 49 studies highlighted that maternal transmission of a COVID-19 infection to the neonate is uncommon (7), it is not yet clear whether maternal COVID-19 infection might have negative effects on the fetus and neonate. Furthermore, the lockdown restrictions can cause substantial stress as routine medical appointments and prenatal classes may have been cancelled or were performed under special circumstances (8, 9). Pregnant women also face the challenge of potentially not having their partner or support person accompanying them during the birth process. Altogether, this can lead to an acute period of collective and individual stress (5, 9). However, more research is necessary to better understand the stress reaction of pregnant women in this special situation. To systematically evaluate the stress response experienced during the COVID-19 pandemic, Preis and colleagues (9, 10) recently introduced a multidimensional questionnaire in order to measure the extent of pandemic-related stress in pregnant women. The development of such a tool seems essential given that the course and duration of the COVID-19 pandemic outbreak is still unclear (11, 12)
The English Pandemic-Related Pregnancy Stress Scale
In April 2020, Preis and colleagues (9, 10) developed and introduced the Pandemic-Related Pregnancy Scale (PREPS) in the US population. It is a novel instrument, which measures pandemic-related stress as a multidimensional construct. The items of the questionnaire assess the concerns, thoughts and experiences pregnant women might have during the COVID-19 pandemic and how these unusual circumstances might affect them in their different life domains. The questionnaire comprises three dimensions, namely Preparedness Stress, Infection Stress and Positive Appraisal, highlighting that the pandemic impacts can generate stress, and at the same time activate positive appraisal processes. The questionnaire exhibited very good psychometric properties. A Confirmatory Factor Analysis showed excellent model fit (CFI = 0.93, TLI = 0.91, RMSEA= 0.07, SRMR = 0.057). Furthermore, external validity in relation to other similar scales was found as the PREPS correlated with instruments measuring fear of childbirth and pregnancy specific stress.
Aim of the present study
Our objectives were threefold: 1) to translate the original PREPS questionnaire to German in order to have an available resource for the German-speaking research and clinical community measuring pandemic-related stress in pregnancy; 2) to validate this questionnaire using a large German-speaking sample and test whether the factor structure of the original English PREPS questionnaire could be replicated in this population; 3) to compare the German version of the PREPS with other similar constructs such as general pregnancy-related stress and fear of childbirth in order to establish convergent validity. We additionally investigated the association of maternal obstetrical and socio-demographic factors with PREPS scores in order to test its sensitivity.
2. Methods
2.1. Participants
A total of 1,364 pregnant German-speaking women participated in this cohort study. In Germany, N=1,179 women completed the online questionnaire between May 4th-29th 2020 whereas in Switzerland, N=185 women took part between May 13th and June, 21st 2020 . Inclusion criteria were: current pregnancy (all gestational ages eligible), maternal age ≥ 18 years, and sufficient knowledge of the German language in order to respond to the online questionnaire. This study is part of a larger ongoing international cooperation project investigating the experiences of and women during the COVID-19 in different countries (10, 13). In Switzerland, the study was approved by the Ethics Committee from the Faculty of Arts and Social Sciences from the University of Zurich (Approval Nr. 20.6.2). In Germany, no ethical approval was necessary.
2.2. Materials
The Pandemic-Related Pregnancy Scale (PREPS) is a novel instrument developed by Preis and colleagues (9, 10) at the beginning of the COVID-19 pandemic in the US. The original PREPS comprises 17 items which assess different experiences, thoughts and concerns pregnant women may have during the COVID-19 pandemic. Participants are asked to rate each item on a 5 point Likert scale from 1 (very little) to 5 (very much). An exploratory and confirmatory factor analysis on the original instrument revealed that 15 items load on three factors: 1) the factor PREPS-Preparedness (7 items), which reflect stress regarding birth preparation and the early postpartum phase; 2) five items relate to stress about getting infected, in the sub-scale PREPS-Infection, and 3) the third factor, PREPS-Positive Appraisal (3 items), which relate to favorable aspects of being pregnant during the pandemic. Two items did not load on any factors and were therefore excluded. The confirmatory factor analyses from the original study showed excellent fit (CFI = 0.93, TLI = 0.91, RMSEA = 0.07, SRMR = 0.057) (10).
The Revised Prenatal Distress Questionnaire (14) comprises 17 items with pregnancy-related stressors in which women are asked to rate whether they are “feeling bothered, upset or worried” on a scale from 0 = not at all to 2 = very much. A mean score of the 17 items is calculated with higher scores indicating greater distress. Furthermore, the two-item Fear of Birth Scale (15), evaluates how women feel in respect to the upcoming birth. Women were asked to rate their feelings on a 100mm Visual Analogue Scale with the anchors calm vs. worried and no fear vs. strong fear. A mean score was calculated with higher scores indicating increased fear of childbirth.
Additionally, we evaluated the following socio-demographic and obstetrical factors: maternal age, parity, gestational age (divided by trimesters), risk pregnancy (yes/unsure/no), use of fertility treatment (yes/no), financial status (below average/average/above average), COVID-19 related financial loss, abuse history and relationship status. We also evaluated whether women were diagnosed with COVID-19 (yes/no), whether they thought they had COVID-19 without being tested (yes/unsure/no) and whether they had close contact with someone who was infected (yes/no). Additionally, one item asking about the perceived risk that loved ones could be infected with COVID-19 was used for which women rated their perceived risk on a scale from 1 = very little to 5 = very much. Moreover, four items using this same rating scale were used to measure COVID-19 related personal growth. A mean score was calculated. The five latter items were developed by Preis et al. (10) when creating the PREPS.
2.3. Translation process
The PREPS questionnaire was translated by two researchers fluent in English and German and thoroughly checked by the authors NKS and PLG (NKS is a native German speaker fluent in English and PLG is a native English speaker fluent in German). As we had a tight timeline to get the study started in the peak of the COVID-19 lockdown, we had to forgo the back translation of the questionnaire, which is usually recommended when translating questionnaire into other languages (16). However, we developed a German version of the PREPS which is semantically, conceptually and culturally equivalent to the English version (17). The questionnaire is available upon request from the first author.
2.4. Procedure
This validation study was administrated via the online platforms Sosci-Survey (www.soscisurvey.de) in Germany and Unipark (www.unipark.de) in Switzerland. Participants were recruited via Facebook posts, Facebook groups and distribution through different organizations for pregnant women (e.g. Motherhood). After reading the study information and giving their informed written consent, participants completed the questionnaire, which took approximately 15 minutes. In Germany, participants had the chance to enter a prize drawing to win one of ten 10 Euro Amazon vouchers, whereas in Switzerland, each woman was sent a small gift if they indicated they would want to receive one.
2.5. Data analysis
To explore whether the factor structure of the German PREPS was similar to the factor structure of the original English version, we applied confirmatory factor analysis (CFA) using the statistical software AMOS 26.0. Additionally, with SPSS 26.0, bivariate Pearson’s correlations were calculated to investigate the associations of the PREPS with fear of childbirth, pregnancy-related stress, perceived infection risk of loved ones and personal growth. Univariate ANOVAs and independent-samples t-test were applied to investigate the influence of obstetric and socioeconomic factors.
3. Results
3.1. Demographics
The mean age of participants was 31.8 ± 4.3 years and most women were married or living in a stable partnership (N = 1,305, 95.7%). Only eleven women (< 1%) in the German-speaking sample were medically diagnosed with COVID-19.
3.2. Main results
The CFA showed very good fit indices for the German speaking sample, confirming the factor structure of the original English version (see Table 1).1 The factor structure and item loadings of the overall sample are presented in Figure 1. For the sub-scale Preparedness Stress (seven items), internal consistency was high (α = .81) with inter-item correlations all > .27. The sub-scale Infection Stress (five items) also showed high internal consistency (α = .86) with high inter-item correlations ( >. 36). Similar results were found for the third sub-scale, Positive Appraisal (3 items) with α = .71 and inter-item correlations > .36.
Table 1:
Confirmatory factor analysis for the German PREPS
| Models | χ2 | df | RMSEA | CFI | TLI | SRMR |
|---|---|---|---|---|---|---|
| Overall sample | 716,22 | 86 | .073 | .920 | .902 | .066 |
Figure 1:
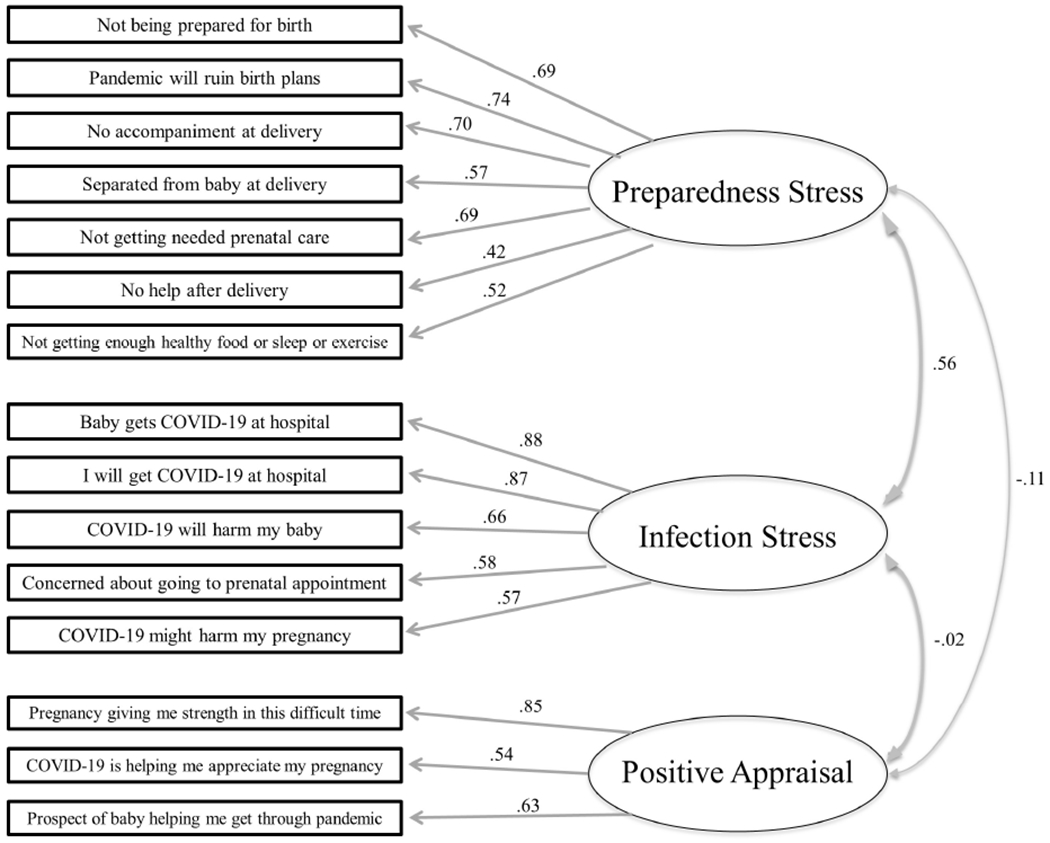
The factor structure and item loadings of the German Pandemic-Related Stress Scale
Preparedness Stress as well as Infection Stress correlated positively with fear of childbirth, pregnancy specific stress, perceived infection risk for loved ones and personal growth. Positive Appraisal was negatively correlated with fear of childbirth and positively with perceived infection risk for loved ones and personal growth. The complete correlation matrix is presented in Table 2.
Table 2:
Correlation analysis between the three dimensions of the PREPS and psychological measures (N = 1,364)
| Range | M ± SD | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|---|
| 1. PREPS-Preparedness | 1-5 | 2.93 ± 0.94 | - - - | |||||
| 2. PREPS-Infection | 1-5 | 2.60 ± 1.03 | 0.53*** | - - - | ||||
| 3. PREPS-Positive Appraisal | 1-5 | 2.05 ± 0.91 | −0.02 | 0.04 | - - - | |||
| 4. Fear of Childbirth | 0-100 | 44.79 ± 27.99 | 0.58*** | 0.38*** | −0.08** | - - - | ||
| 5. Pregnancy Specific Stress | 0-2 | 0.70 ± 0.31 | 0.61*** | 0.42*** | 0.01 | 0.46*** | - - - | |
| 6. Perceived Infection Risk for Loved Ones | 1-5 | 3.70 ± 1.16 | 0.34*** | 0.52*** | 0.12*** | 0.21*** | 0.30*** | - - - |
| 7. Personal Growth | 1-5 | 2.44 ± 0.89 | 0.05 | 0.11*** | 0.47*** | 0.02 | 0.11*** | 0.18*** |
p < .001,
p < .01,
p < .05.
From our sample 16% (n = 219) reported high levels of Preparedness Stress (a score of 4 or above) whereas 12% (n = 168) reported high levels of Infection Stress. Regarding Positive Appraisal, 48% (n = 661) of participants scored less than 2 points, which reflects a low level of positive appraisal. The results of the associations of obstetrical and other factors of interest with the PREPS are presented in Table 3 showing that factors such as parity, fertility treatment, risk pregnancy, history of abuse, financial situation and cancelled appointments influence experienced stress levels.
Table 3:
Mean differences in the Pandemic-Related Stress Sub-Scales in relation to obstetrical and COVID-19 related factors
| N | Preparedness Stress | Infection Stress | Pos. Appraisal | |
|---|---|---|---|---|
| Parity | t = 3.98*** | t = .091 | t = 5.97*** | |
| Primipara | 702 | 3.03 ± 0.93 | 2.63 ± 1.02 | 2.19 ± 0.95 |
| Multipara | 662 | 2.83 ± 0.94 | 2.58 ± 1.05 | 1.90 ± 0.84 |
| Trimester | F = 1.96 | F = 3.16* | F = 2.08 | |
| 1st | 103 | 2.76 ± 0.97 | 2.71 ± 0.99 | 2.16 ± 0.98 |
| 2nd | 502 | 2.93 ± 0.96 | 2.68 ± 1.05 | 2.09 ± 0.93 |
| 3rd | 759 | 2.95 ± 0.92 | 2.54 ± 1.03 | 2.01 ± 0.89 |
| Had COVID-19 without medical diagnosis | F = 5.55** | F = 1.90 | F = 2.09 | |
| 921 | 2.87 ± 0.93 | 2.57 ± 1.02 | 2.02 ± 0.89 | |
| No | 348 | 3.05 ± 0.50 | 2.69 ± 1.05 | 2.14 ± 0.93 |
| Unsure | 95 | 3.07 ± 0.97 | 2.64 ± 1.10 | 2.00 ± 1.03 |
| Yes | ||||
| Fertility treatment | T = 2.00* | T = 2.07* | T = 0.71 | |
| Yes | 103 | 3.11 ± 0.94 | 2.81 ± 1.07 | 2.11 ± 0.79 |
| No | 1259 | 2.91 ± 0.94 | 2.59 ± 1.03 | 2.04 ± 0.92 |
| Risk pregnancy a | T = 3.20** | T = 3.08** | T = 1.78* | |
| Yes | 324 | 3.06 ± 0.92 | 2.74 ± 1.06 | 1.95 ± 0.83 |
| No | 986 | 2.87 ± 0.94 | 2.54 ± 1.03 | 2.07 ± 0.93 |
| Appointment cancelled | T = 7.48*** | T = 4.07*** | T = 0.10 | |
| Yes | 256 | 3.32 ± 0.88 | 2.84 ± 1.08 | 2.04 ± 0.87 |
| No | 1108 | 2.84 ± 0.93 | 2.55 ± 1.02 | 2.05 ± 0.92 |
| Abuse history | T = 2.60** | T = 1.03 | T = 0.72 | |
| Yes | 200 | 3.09 ± 0.95 | 2.67 ± 1.08 | 2.01 ± 0.97 |
| No | 1164 | 2.90 ± 0.94 | 2.59 ± 1.03 | 2.05 ± 0.91 |
| Lost income | t = 1.43 | t = 1.50 | t = 0.22 | |
| No | 1180 | 2.91 ± 0.95 | 2.59 ± 1.04 | 2.05 ± 0.92 |
| Yes | 184 | 3.02 ± 0.90 | 2.71 ± 1.02 | 2.06 ± 0.87 |
| Insurance | T = 2.10* | T = 0.45 | T = 0.55 | |
| Private | 194 | 2.80 ± 0.93 | 2.58 ± 0.97 | 2.08 ± 0.98 |
| Statutory | 1167 | 2.95 ± 0.94 | 2.61 ± 1.05 | 2.04 ± 0.90 |
| Financial situation | F = 3.87* | F = 4.03* | F = 1.03 | |
| Below average | 166 | 3.09 ± 0.98 | 2.74 ± 1.09 | 2.07 ± 0.89 |
| Average | 952 | 2.93 ± 0.94 | 2.62 ± 1.03 | 2.07 ± 0.93 |
| Above average | 245 | 2.83 ± 0.92 | 2.46 ± 1.04 | 1.97 ± 0.87 |
p < .001,
p < .01,
p < .05,
54 women were unsure whether their pregnancy is a risk pregnancy and were excluded from this analysis.
4. Discussion
The aim of the current study was to translate the PREPS questionnaire into German and subsequently to psychometrically validate it using a large representative German speaking population. Our findings revealed that the translated questionnaire shows very good confirmatory fit to the data from the German population. Furthermore, the three factors (Preparedness Stress, Infection Stress and Positive Appraisal) exhibited good internal consistency and acceptable inter-item correlations. Additionally, significant correlations were revealed between the PREPS stress sub-scales and both fear of childbirth and general pregnancy specific stress, highlighting the convergent validity of the PREPS. Furthermore, the analysis showed that several factors such as primiparity, being pregnant through fertility treatment, having a high risk pregnancy, cancelled medical appointments during the pandemic as well as having a below average income are associated with higher levels of perceived stress during the COVID-19 pandemic, confirming the sensitivity of the questionnaire and opening up venues for future research.
Interestingly, factors such as conceiving through fertility treatment, having a high-risk pregnancy, having had cancelled prenatal appointments and a financial situation below average contributed to higher Preparedness Stress and Infection Stress. On the other hand, parity, gestational trimester, a history of abuse and having a statutory health insurance showed distinct associations with only one of the PREPS sub-scales. The findings that women who conceived through fertility treatment and primiparas experience higher stress levels are in accordance with previous studies showing that these women also experience higher pregnancy-related stress in general (18, 19). Of note, women with a history of abuse displayed higher pandemic-related stress on the Preparedness Stress sub-scale, suggesting that a history of abuse may render women more vulnerable to further stressors. Although only eleven women had a medically confirmed diagnosis of COVID-19, an additional 95 women believed they were infected and another 348 were unsure. Our analyses showed that women who believed or were unsure whether they were infected with COVID-19 displayed higher Preparedness Stress, highlighting that mere uncertainty about being infected may be causing them distress. This finding corroborates studies in different contexts (e.g. breast cancer) correlating uncertainty about having a disease with higher distress (20). This should encourage health providers to facilitate COVID-19 testing to pregnant women considering that uncertainty about infection may be contributing to higher stress levels.
Some interesting observations from the German-speaking sample compared to the US original validation sample (10) should be mentioned here. Overall, pandemic-related stress in the German-speaking sample was lower than in the US and fewer women had their prenatal appointments cancelled (19% in the German-speaking sample vs. 53% in the US) or lost income (13% in the German-speaking sample vs. 40% in the US). As the US faced a more drastic lockdown and severe course of the pandemic, it is not surprising that American pregnant women are more affected and stressed than pregnant women in Germany and Switzerland. However, both in Germany and Switzerland, constraints such as cancelled appointments or not being able to bring the partner or a supporting person to prenatal appointments and the birth led to higher stress levels in pregnant women. A detailed comparison of the magnitude and overall impact of the COVID-19 pandemic on perinatal mental health in women from different countries is a primary aim of our ongoing large cooperation project.
As early studies have shown that the COVID-pandemic may lead to higher anxiety and stress (5, 6, 9), the German PREPS presented and validated here could be of great use for future studies to investigate the impact of pandemic-related stress on birth outcomes, maternal postnatal depression, mother-infant bonding and infant cognition., as a great body of evidence has already shown the negative effect of high stress levels on these outcomes. (3, 4, 21–23). Additionally, it would be valuable to use the PREPS to identify women who experience high levels of pandemic-related stress early in pregnancy in order to offer them stress-reducing interventions to prevent unfavorable outcomes.
Conclusion
The present study introduces the psychometric validated German version of the PREPS scale, which exhibited good psychometric properties. Therefore, this questionnaire is a reliable and valid measure to investigate pandemic-related maternal well-being with a focus on perceived stress of pregnant women in German-speaking samples. Future research should investigate the possible impact of the additional perceived stress on postnatal maternal and infant outcomes such as maternal postnatal depression, mother infant bonding and infant cognitive development in order to better understand the consequences of prenatal stress and develop preventive strategies to protect mother and child from stress over-exposure.
Acknowledgements
We would like to thank Romina Bergmann and Laureen Blettenberg for their help with the translations.
Abbreviations:
- CFA
confirmatory factor analysis
- COVID-19
Coronavirus Disease 2019
- PREPS
Pandemic-Related Pregnancy Scale
Appendix
Table A1:
Confirmatory factor analyses for the German PREPS conducted separately for the data from Germany and Switzerland as well as for the overall sample
| Models | χ2 | df | RMSEA | CFI | TLI | SRMR |
|---|---|---|---|---|---|---|
| German sample | 662.10 | 86 | .075 | .915 | .896 | .067 |
| Swiss sample | 163.1 | 86 | .070 | .925 | .908 | .082 |
| Overall sample | 716,22 | 86 | .073 | .920 | .902 | .066 |
Footnotes
We also conducted the CFA for the German and Swiss data individually and for both, very good fit indices were revealed (see Appendix, Table A1). Therefore, we decided to combine the data and report the results for the overall German speaking sample as the German speaking questionnaire is intended to be used throughout German speaking countries.
Conflict of Interest statement
None to declare.
Data statement
The dataset used and analysed d the current study is available from the corresponding author on reasonable request.
References
- 1.Rallis S, Skouteris H, McCabe M, Milgrom J. A prospective examination of depression, anxiety and stress throughout pregnancy. Women and Birth. 2014. December;27(4):E36–E42. [DOI] [PubMed] [Google Scholar]
- 2.La Marca-Ghaemmaghami P, Ehlert U. Stress During Pregnancy Experienced Stress, Stress Hormones, and Protective Factors. European Psychologist. 2015;20(2):102–19. [Google Scholar]
- 3.Staneva A, Bogossian F, Pritchard M, Wittkowski A. The effects of maternal depression, anxiety, and perceived stress during pregnancy on preterm birth: A systematic review. Women and Birth. 2015. September;28(3):179–93. [DOI] [PubMed] [Google Scholar]
- 4.Underwood L, Waldie KE, D’Souza S, Peterson ER, Morton SMB. A Longitudinal Study of Pre-pregnancy and Pregnancy Risk Factors Associated with Antenatal and Postnatal Symptoms of Depression: Evidence from Growing Up in New Zealand. Maternal and Child Health Journal. 2017. April;21(4):915–31. [DOI] [PubMed] [Google Scholar]
- 5.Saccone G, Florio A, Venturella R, De Angelus MC, Zullo F, Di Spiezio Sardo A. Psychological impact of coronavirus disease 2019 in pregnant women. American Journal of Obstretics and Gynecology; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020. March;395(10227):912–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Walker KF, O’Donoghue K, Grace N, Dorling J, Comeau JL, Li W, et al. Maternal transmission of SARS-COV-2 to the neonate, and possible routes for such transmission: A systematic review and critical analysis. Bjog. 2020. June 12. Epub 2020/06/13.eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Caparros-Gonzalez RA, Alderdice F. The COVID-19 pandemic and perinatal mental health. Journal of Reproductive and Infant Psychology.38(3):223–5. doi: 10.1080/02646838.2020.1786910. [DOI] [PubMed] [Google Scholar]
- 9.Preis H, Mahaffey B, Heiselman C, Lobel M. Pandemic-related pregnancy stress and anxiety among women pregnant during the COVID-19 pandemic. Am J Obstet Gynecol MFM: © 2020 Published by Elsevier Inc; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Preis H, Mahaffey B, Lobel M. Psychometric properties of the Pandemic-Related Pregnancy Stress Scale (PREPS). Journal of Psychosomatic Obstetrics & Gynecology; in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bertozzi AL, Franco E, Mohler G, Short MB, Sledge D. The challenges of modeling and forecasting the spread of COVID-19. Proceedings of the National Academy of Sciences of the United States of America. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Howard J, Rahim Z. Coronavirus may ‘never go away,’ says WHO official. CNN; 2020, May 14. [Google Scholar]
- 13.Ilska M, Kotodziej-Zaleska A, Brandt-Salmeri A, Preis H, Lobel M. Psychometric evaluation of the Polish version of the Pandemic-Related Pregnancy Stress Scale. under review. [Google Scholar]
- 14.Ibrahim SM, Lobel M. Conceptualization, measurement, and effects of pregnancy-specific stress: review of research using the original and revised Prenatal Distress Questionnaire. Journal of Behavioral Medicine. 2020. February;43(1):16–33. [DOI] [PubMed] [Google Scholar]
- 15.Haines H, Pallant JF, Karlstrom A, Hildingsson I. Cross-cultural comparison of levels of childbirth-related fear in an Australian and Swedish sample. Midwifery. 2011. August;27(4):560–7. [DOI] [PubMed] [Google Scholar]
- 16.Jones PS, Lee JW, Phillips LR, Zhang XWE, Jaceldo KB. An adaptation of Brislin’s translation model for cross-cultural research. Nursing Research. 2001. Sep-Oct;50(5):300–4. [DOI] [PubMed] [Google Scholar]
- 17.Berry JW. CROSS-CULTURAL COMPARABILITY. International Journal of Psychology. 1969 1969;4(2):119–28. [Google Scholar]
- 18.Gillespie SL, Mitchell AM, Kowalsky JM, Christian LM. Maternal parity and perinatal cortisol adaptation: The role of pregnancy-specific distress and implications for postpartum mood. Psychoneuroendocrinology. 2018. November;97:86–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gourounti K Psychological stress and adjustment in pregnancy following assisted reproductive technology and spontaneous conception: A systematic review. Women & Health. 2016. January;56(1):98–118. [DOI] [PubMed] [Google Scholar]
- 20.Lang EV, Berbaum KS, Lutgendorf SK. Large-Core Breast Biopsy: Abnormal Salivary Cortisol Profiles Associated with Uncertainty of Diagnosis. Radiology. 2009. March;250(3):631–7. [DOI] [PubMed] [Google Scholar]
- 21.Hopkins J, Miller JL, Butler K, Gibson L, Hedrick L, Boyle DA. The relation between social support, anxiety and distress symptoms and maternal fetal attachment. Journal of Reproductive and Infant Psychology. 2018;36(4):381–92. [DOI] [PubMed] [Google Scholar]
- 22.Korja R, Nolvi S, Grant KA, McMahon C. The Relations Between Maternal Prenatal Anxiety or Stress and Child’s Early Negative Reactivity or Self-Regulation: A Systematic Review. Child Psychiatry & Human Development. 2017. December;48(6):851–69. [DOI] [PubMed] [Google Scholar]
- 23.Graignic-Philippe R, Dayan J, Chokron S, Jacquet AY, Tordjman S. Effects of prenatal stress on fetal and child development: A critical literature review. Neuroscience and Biobehavioral Reviews. 2014. June;43:137–62. [DOI] [PubMed] [Google Scholar]


