Abstract
Purpose
This study aimed to describe substance use (SU) among adolescents and young adults (AYA) with chronic kidney disease (CKD), compare these findings with the general population, and identify associated risk factors.
Methods
708 AYA participants contributing 2475 person-visits from the Chronic Kidney Disease in Children (CKiD) Study were used to estimate prevalence rates of past year and 30-day alcohol, cigarette, e-cigarette and marijuana use, and were compared with national surveys. Repeated measures logistic regression estimated the association between SU and participant characteristics.
Results
There was nearly no SU among those 12 to 14 years, but use increased with age, and past year alcohol use was about 80% for those ≥22 years. Rates of use among males were constant or increased with age, while rates of use among females were lower after age 22 compared to ages 18 to 22. Associated risk factors included non-Black and non-Hispanic identity, older age, and worse disease severity. CKiD participants were less likely to use substances compared to the general population, especially those 14–18 years.
Conclusions
SU was less common in AYA with CKD than the general population, but differences were attenuated among those ≥18 years. Ages 12–14 appear to be the ideal time for prevention efforts. As the landscape of e-cigarette and marijuana policies change, these results underscore the need to understand how similar high-risk populations engage in SU.
Keywords: Kidney Diseases, Adolescent, Young Adult, Alcohol Drinking, Tobacco Use, Vaping, Marijuana Use, Epidemiology
INTRODUCTION
Children, adolescents and young adults (AYA) with chronic kidney disease (CKD) can experience many developmental challenges in the physical, cognitive and social domains (1). This population is at high risk of diminished quality of life, growth impairment, and long-term health complications that continue into adulthood (2–4), in addition to the normal psychosocial challenges of adolescence. Due to extensive time spent in clinics and parental management of their condition, AYA with CKD often report frustration at the limitations caused by their disease (5). This population may be at higher risk of using substances because novelty and experimentation may be particularly enticing, or they may be at lower risk because research has shown that dealing with a chronic condition heightens health awareness and discourages risky health behaviors (6). There is limited research to determine where AYA with CKD fall on this spectrum, and the aim of this analysis was to provide additional research to address the gap in knowledge.
Previous research identified harmful effects of secondhand smoke on pediatric CKD progression (7,8), particularly proteinuria. In addition, current and lifetime use of alcohol, cigarettes, e-cigarettes and marijuana were estimated in an adolescent-only population of up to 390 children with CKD, dialysis or with a kidney transplant (9,10). To our knowledge, a comprehensive investigation of alcohol, tobacco, e-cigarette and marijuana use across a wider age range of AYA with CKD prior to the initiation of transplant or dialysis in a large, representative cohort has not been completed.
The goal of this study was to characterize substance use (SU) in a representative population of children from 12 to young adults (older than 18 years of age) with CKD prior to the initiation of kidney replacement therapy (KRT), and identify risk factors for use in the Chronic Kidney Disease in Children (CKiD) Study. We aimed to quantify the prevalence rates of alcohol, tobacco, e-cigarette and marijuana usage in this population by age and sex, and compare findings to the general United States AYA population. We additionally aimed to identify putative associations between SU and clinical and demographic characteristics through a risk factor analysis. Within the CKiD study, we hypothesized that older participants would be more likely to use substances, and that those with more severe CKD would be less likely to use because of more complex disease management and poor general health. Compared to the US general AYA population, we hypothesized that CKiD participants would be less likely to use because of their experience living and dealing with their chronic condition.
METHODS
Study Population and Design
The CKiD Study is a multicenter, longitudinal cohort of children and AYA, enrolled between ages one and 16 years, with mild to moderate CKD recruited from 56 centers in the US (n=53) and Canada (n=3). CKiD completed three waves of recruitment: 2005–09 (median age at enrollment=10.9 years), 2011–14 (median age=12.0), and 2016–20 (median age=3.5).
Participants attended annual study visits with standardized collection of biological specimens and self-administered questionnaires. All participants and families provided informed assent/consent prior to study initiation, and protocols and procedures were approved by the Institutional Review Boards of participating sites. CKiD study design and methods have been previously described (1,11). Visits from 2005 through 2018 were used in this analysis.
Collection of Substance Use Measures
Participants ≥12 years of age answered questions on alcohol, cigarettes, e-cigarettes and marijuana. Instructions explained that responses were confidential. SU questions were implemented at study initiation in 2005, with the exception of e-cigarettes, and past 30-day alcohol and marijuana usage, which were implemented in September 2014.
At the baseline visit, participants were asked if they had ever used alcohol, cigarettes, e-cigarettes or marijuana, and whether they had used these substances over the past 30 days. For subsequent visits, they were asked if they had used each substance separately over the past year. For alcohol, if they answered yes, they were then asked “during the past 30 days, on how many days did you have at least one drink of alcohol?”. For cigarettes, if they answered yes to using in the past year, they were asked “do you currently smoke tobacco?” and, if yes, “in the past year, what is the average number of cigarettes, cigars, cigarillos or little cigars you smoke per week?”. For e-cigarettes, if they answered yes to using in the past year, participants were asked “during the past 30 days, on how many days did you use an electronic vapor product?”. Finally, for marijuana, participants were asked “in the past year, how many times have you used marijuana?” and “during the past 30 days, how many times have you used marijuana?”.
For each substance, participants were classified as yes/no ever, past year, and past 30-day/current users. To describe patterns of multiple SU, each person-visit was categorized as no use, alcohol only, alcohol plus one or two other substances, all four substances, or at least one substance but in the absence of alcohol.
Comparisons to National Estimates
Sex-stratified national prevalence estimates for ever and past 30-day SU came from three US representative surveys using appropriate age ranges for comparison. For those 14 to <18 years, estimates were from the 2017 Youth Risk Behavior Surveillance System, a CDC coordinated survey that is administered to high school students (generally >14 years) every two years (12,13). For ≥18 years, alcohol, cigarette and marijuana use estimates were from the 2017 National Survey on Drug Use and Health (14,15). Estimates of e-cigarette use among those ≥18 years were from the 2018 National Health Interview Survey (16).
Covariates
Age was categorized in two-year bins from 12 to <22, and then ≥22 years. Kidney disease etiology was classified by underlying primary CKD diagnosis (non-glomerular/glomerular) (17,18). Estimated glomerular filtration rate (eGFR; ml/min|1.73m2) (19), proteinuria (urine protein-to-creatinine ratio; uPCR, mg/mgCr), and CKD risk categories were used to measure CKD severity, categorized as A, B and C, D and E, and F and eGFR<15 (end-stage kidney disease (ESKD)), representing mild to severe disease, respectively (20).
Sociodemographic variables included sex (male/female; (12)) race (Black/non-Black), ethnicity (Hispanic/non-Hispanic), annual income (≤$36,000, >$36,000 to ≤$75,000, >$75,000), maternal education (less than college vs. some college or more), and ever having previously lived in a household with a smoker. All sociodemographic variables were self-reported. Clinical comorbidities included uncontrolled high blood pressure (BP; systolic BP ≥120 or diastolic BP ≥80 (21)), and anemia (hemoglobin <5th percentile for age, sex and race (22)). Age, ever having previously lived with a smoker, eGFR, uPCR, CKD risk category, BP and anemia were treated as time-varying and were updated at each annual study visit.
Statistical Analyses
Prevalence rates for SU (ever, past year, current/30-day) were estimated by age category and sex per person-visit using repeated measures logistic regression models. Generalized estimating equations accounted for within-individual correlation to produce valid 95% confidence intervals. The same methods were used to calculate prevalence rates of SU, stratified by 14 to <18 vs. ≥18 years, for comparisons with the general population, as well as for estimating prevalence rates for combination SU. Analyses of combination SU were restricted to after September 2014 to allow all four substances to be reported. Additionally, we performed a supplementary analysis investigating how past year SU may change over calendar years within age groups. Time was stratified into two year increments (2005–06, 2007–08, up to 2017–18).
Repeated measures logistic regression models were used to estimate the odds ratios (ORs) for the association between kidney, clinical and demographic characteristics (as predictors) and past year and current use of each substance (as outcomes). For each outcome, bivariate models were first adjusted only for categorical age. Multivariate models were adjusted for age, sex, race, ethnicity, maternal education, income, primary CKD diagnosis, and CKD risk category, and then additionally for uncontrolled BP, and anemia.
To investigate the association of concomitant cigarette use with e-cigarettes, we compared the odds of current cigarette use with e-cigarette use as the exposure, controlling for age and sex. Using the same approach, we assessed the association between cigarette and e-cigarette use (past year and current) as the outcome, and living with a smoker as the exposure.
Statistical significance was assessed at p<0.05. Analyses were performed in Stata Version 15 (College Station, TX).
RESULTS
Description of Study Population
A total of 708 CKiD participants contributed 2475 person-visits, with 876 (35.4%) occurring after September 2014. The median number of person-visits contributed was 3 (IQR: 2, 5; maximum: 10); the median years over follow-up was 3.0 (IQR: 1.0, 5.0; maximum: 12.2).
Table 1 presents a description of the person-visit characteristics included in the analytic sample stratified by age (range: 12.0 to 27.5 years; a histogram of the age distribution is presented in Supplemental Figure 1). A total of 74.3% of person-visits were completed by those 12 to <18 years (1840/2475 person-visits) and 4.3% were ≥22 years. Visits from those in older age categories were more likely to have an annual household income of >$75,000 (42.3% for those ≥22 years vs. 28.0% among 12–13 years) and were more likely to have glomerular CKD (38.7% for ≥22 years vs. 23.1% for 12–13 years). eGFR was similar across groups, but uPCR increased with age.
Table 1.
Demographic and clinical characteristics of person-visits stratified by age among adolescents and young adults with CKD. The total number of person-visits is 2475 contributed by 708 individuals. Presented as n (%) or median [IQR].
| Age Categories | ||||||
|---|---|---|---|---|---|---|
| 12–13 | 14–15 | 16–17 | 18–19 | 20–21 | 22+ | |
| Person-Visitsa | 589 (23.8) | 641 (25.9) | 610 (24.6) | 357 (14.4) | 172 (6.9) | 106 (4.3) |
| Individualsb | 423 | 472 | 428 | 260 | 122 | 55 |
| Demographics | ||||||
| Male | 380 (64.5) | 391 (61.0) | 367 (60.2) | 208 (58.3) | 109 (63.4) | 57 (53.8) |
| Black Race | 117 (19.9) | 139 (21.7) | 113 (18.5) | 75 (21.0) | 41 (23.8) | 24 (22.6) |
| Hispanic Ethnicity | 71 (12.1) | 87 (13.7) | 71 (11.7) | 46 (12.9) | 21 (12.3) | 10 (9.4) |
| Maternal Education: < college | 205 (35.6) | 259 (41.7) | 220 (37.2) | 124 (35.8) | 54 (33.1) | 37 (36.3) |
| Annual Income | ||||||
| ≤$36k | 233 (40.3) | 250 (40.3) | 212 (35.8) | 112 (32.5) | 49 (29.5) | 32 (33.0) |
| >$36k to $75k | 183 (31.7) | 184 (29.6) | 163 (27.5) | 91 (26.4) | 42 (25.3) | 24 (24.7) |
| >$75k | 162 (28.0) | 187 (30.1) | 218 (36.8) | 142 (41.2) | 75 (45.2) | 41 (42.3) |
| Ever in household with smoker | 165 (28.0) | 207 (32.4) | 194 (31.9) | 121 (33.9) | 70 (40.7) | 34 (32.1) |
| Clinical Characteristics | ||||||
| Glomerular CKD | 136 (23.1) | 201 (31.4) | 235 (38.5) | 140 (39.2) | 64 (37.2) | 41 (38.7) |
| eGFR | 50 [36, 64] | 49 [34, 63] | 52 [36, 70] | 51 [38, 68] | 55 [39, 68] | 46 [32, 59] |
| uPCR | 0.29 [0.12, 0.94] | 0.44 [0.15, 1.32] | 0.40 [0.14, 1.16] | 0.55 [0.16, 1.44] | 0.42 [0.15, 1.15] | 0.63 [0.18, 1.55] |
| CKD Risk Category | ||||||
| A | 252 (45.2) | 212 (35.9) | 208 (36.2) | 137 (40.8) | 73 (46.5) | 36 (36.0) |
| B to C | 181 (32.4) | 209 (35.4) | 206 (35.8) | 129 (38.4) | 59 (37.6) | 41 (41.0) |
| D to E | 95 (17.0) | 117 (19.8) | 114 (19.8) | 42 (12.5) | 13 (8.3) | 13 (13.0) |
| F to ESKD | 30 (5.4) | 53 (9.0) | 47 (8.2) | 28 (8.3) | 12 (7.6) | 10 (10.0) |
| Uncontrolled BP | 108 (18.6) | 173 (27.6) | 194 (32.2) | 138 (39.3) | 72 (42.4) | 39 (37.1) |
| Anemia | 216 (37.8) | 225 (36.4) | 199 (33.5) | 103 (29.5) | 49 (30.4) | 31 (30.4) |
Columns of demographic and clinical characteristics represent numbers and percentages of person-visits, not individuals
As data are longitudinal, and study visits occurred annually, individuals may have contributed to more than one age group column, as well as to each column more than once
Substance Use Prevalence Rate Estimates in CKiD
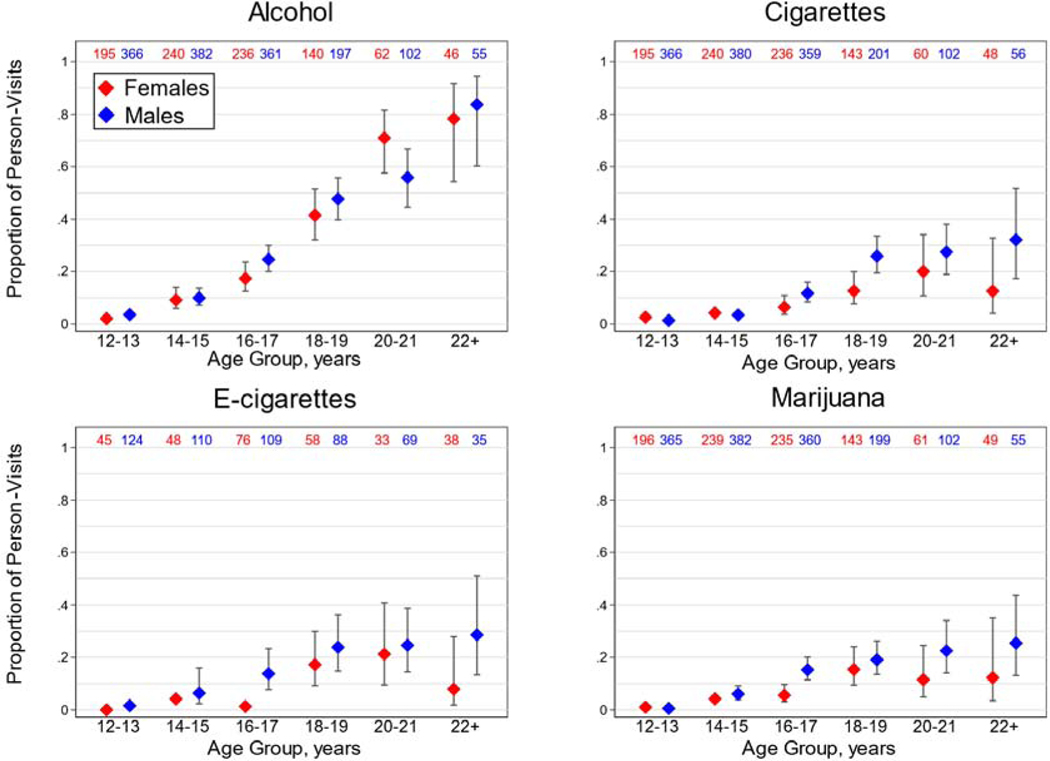
Figure 1 displays prevalence rates of past year alcohol, cigarette, e-cigarette and marijuana use. In general, SU increased with age and males reported more use. There was low reported past year use of all substances among those 12 to <14 years (<4% for alcohol, and <3% for cigarettes, e-cigarettes and marijuana). For alcohol, prevalence rates increased with age, the highest observed among those ≥22 years for both males and females (83.6% and 78.3%, respectively). Males consistently reported alcohol consumption at higher rates than females, with the exception of those 20 to 21 years, where 55.9% of males and 71.0% of females reported use. For past year cigarette usage, prevalence rates consistently increased with age among males (32.1% of those ≥22 years). While 20% of female person-visits among those 20 to 21 years reported cigarette use, this rate dropped to 12.5% for those ≥22 years. A similar trend was observed for e-cigarette use: males reported the highest rate in the ≥22 age group at 28.6%; females reported 21.2% e-cigarette use at 20 to 21 years, but only 7.9% at ≥22 years. Marijuana use was consistent with this pattern as well. Inferences were similar for ever and current use across all substances (Supplemental Figure 2).
Figure 1.
Prevalence rates of past year use for each substance, stratified by age category and child sex, presented as proportions with 95% confidence intervals. 95% CIs for estimates under 0.05 were not calculated. Number of contributing person-visits reported in red and blue for females and males, respectively.
We also investigated how age-specific past year SU changed over time (in two year intervals from 2005 to 2018), for alcohol, cigarettes, e-cigarettes and marijuana, but trends were largely constant with no discernable patterns over time (Supplemental Figure 3).
Comparisons to National Estimates
Table 2 compares CKiD prevalence rates of ever and current use with national US estimates, for those 14 to <18 and ≥18 years. CKiD prevalence rates were consistently lower than national estimates for both sexes, with the exception of e-cigarette use for those ≥18. Those 14 to <18 in CKiD reported considerably lower SU compared with the general population. For example, comparing CKiD vs. the general population for males, ever alcohol use was 25.6% vs. 58.1%, and ever cigarette use was 11.7% vs. 30.7%, respectively. However, disparities between CKiD and the general population did seem to attenuate when comparing estimates for those 14 to <18 years, to those ≥18 years for many substances.
Table 2.
Comparison of CKiD and United States national prevalence estimates for alcohol, cigarette, e-cigarette and marijuana use.
| 14 to under 18/High School | 18 and older | |||
|---|---|---|---|---|
| CKiD | National | CKiD | National | |
| Alcohol | ||||
| Ever | ||||
| Males | 21.4 25.6 30.3 | 56.2 58.1 60.0 | 56.5 64.6 71.9 | 78.9 80.1 81.3 |
| Females | 15.5 20.3 26.0 | 58.4 62.6 66.6 | 56.2 65.0 72.8 | 80.9 82.0 83.1 |
| Current | ||||
| Males | 2.5 5.0 9.5 | 25.1 27.6 30.1 | 36.9 46.1 55.6 | 55.7 57.2 58.7 |
| Females | 0.8 2.4 7.2 | 28.7 31.8 35.1 | 42.8 54.3 65.3 | 53.9 55.4 56.9 |
| Cigarettes | ||||
| Ever | ||||
| Males | 8.8 11.7 15.5 | 27.8 30.7 33.7 | 26.8 34.7 43.5 | 53.1 54.5 55.9 |
| Females | 4.8 7.5 11.7 | 23.9 27.3 31.0 | 16.1 24.7 35.9 | 43.0 44.5 46.0 |
| Current | ||||
| Males | 2.0 3.2 5.2 | 8.3 9.8 11.6 | 12.0 16.7 22.9 | 24.6 25.9 27.2 |
| Females | 1.1 2.3 4.9 | 6.0 7.8 9.9 | 3.3 6.8 13.3 | 17.7 18.7 19.7 |
| E-cigarettes | ||||
| Ever | ||||
| Males | 7.4 12.8 21.2 | 42.4 44.9 47.4 | 20.9 29.7 40.2 | 28.0 31.1 34.2 |
| Females | 1.2 4.0 12.4 | 35.8 39.7 43.9 | 17.9 28.7 42.5 | 19.0 21.6 24.2 |
| Current | ||||
| Males | 2.7 5.5 10.7 | 13.8 15.9 18.2 | 11.7 17.7 26.0 | 7.6 9.6 11.5 |
| Females | 0.4 1.6 6.2 | 8.8 10.5 12.7 | 7.1 12.4 20.9 | 3.1 4.5 5.9 |
| Marijuana | ||||
| Ever | ||||
| Males | 9.7 12.7 16.3 | 32.6 35.2 37.9 | 22.7 30.1 38.8 | 52.7 54.2 55.7 |
| Females | 3.7 6.1 9.9 | 32.6 35.9 39.3 | 12.0 19.4 29.6 | 49.8 51.3 52.8 |
| Current | ||||
| Males | 1.8 4.1 9.1 | 18.2 20.0 21.8 | 11.4 17.9 27.1 | 23.8 25.0 26.2 |
| Females | 0.1 0.8 5.5 | 17.4 19.6 22.0 | 5.5 10.9 20.4 | 18.0 19.2 20.4 |
Estimates presented as lower bound 95% CI percentage upper bound 95% CI. CKiD estimates are presented as prevalence rates, as person-visits were used as the denominator, and used data from both US and Canadian CKiD sites; US national estimates are presented as prevalences because individuals were used as the denominator. For those 14 to under 18 years, 2017 YRBSS data were used for all substances. For those 18 years and older, 2017 NSDUH data were used for alcohol, cigarette and marijuana estimates, and 2018 NHIS data were used for e-cigarette estimates.
Combination Substance Use and Measures of Frequency
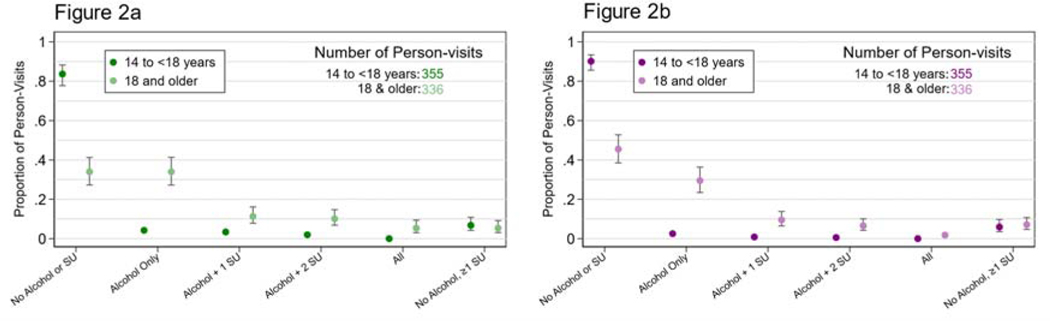
Because of minimal to no reported substance in the youngest age group, those 12 to <14 years were excluded from all further analyses in this manuscript. Figures 2a and 2b display past year and current combination SU as prevalence rates, stratified by 14 to <18 vs. ≥18 years in the CKiD cohort. For those 14 to <18, over 80% and 90% reported no SU over the past year and currently, respectively. For past year use among those ≥18 years, 33.9% reported using no substances, 33.9% reported solely using alcohol, 21.4% reported alcohol plus one or two other substances, and 5.4% reported all four. Only 5.4% reported using any substance(s) in the absence of alcohol. Current use exhibited a similar trend. We also described the frequency of SU among those 14 years and older reporting current use, averaged across sex and all ages. For alcohol, 49.1% reported consuming alcohol ≤2 days over the previous 30 days, and the proportion
Figure 2.
Combinations of previous year (Figure 2a) and current (Figure 2b) substance use stratified by those 14 to <18 years of age vs. 18 or older among those who reported using during the corresponding time period. The maximum age observed was 27.5 years.
Those in ‘No Alcohol or SU’ category reported using no substances; those in the ‘Alcohol Only’ category reported using solely alcohol; those in the ‘Alcohol + 1 SU’ category reported using alcohol plus one of the other reported substances (cigarettes, e-cigarettes or marijuana); those in the ‘Alcohol + 2 SU’ category reported using alcohol plus any combination of two of the other reported substances; those in the ‘All’ category reported using all four substances; those in the ‘No Alcohol, ≥1 SU’ category reported using cigarettes, e-cigarettes or marijuana singularly or in any combination but in the absence of alcohol. 95% CIs for estimates under 0.05 were not calculated. SU = substance use. declined as use increased. For cigarettes, 28.6% reported smoking ≤2 cigarettes per week, and 20.5% reported more than 30 cigarettes per week. For e-cigarettes, 57.8% reported using ≤2 days over the past month. Marijuana was more evenly distributed, with 25.4% and 27.1% reporting using ≤2 and 21–30 times over the previous month, respectively. A full description is presented in Supplemental Figure 4.
Substance Use Risk Factor Analysis
Table 3 presents model results of risk factors for past year SU for those ≥14 years: models were bivariate (adjusted for age only), and multivariate (adjusted for age, sociodemographic and clinical variables). Those 14 to <18 years had consistently lower odds of past year use of any substance compared to those 18 to <20 years. Older age was typically associated with increased odds of past year use with a few exceptions: those ≥22 years were equally or less likely to use both cigarettes and e-cigarettes.
Table 3.
Bivariate and multivariate logistic regression models showing the odds ratios of past year substance use as the outcome for those 14 and older. Presented as OR (95% CI). Significant findings are bolded.
| Alcohol | Cigarette | E-cigarette | Marijuana | |||||
|---|---|---|---|---|---|---|---|---|
| Variable | Bivariateb | Multivariatec–e | Bivariate | Multivariate | Bivariate | Multivariate | Bivariate | Multivariate |
| Age categorya | ||||||||
| 14 to <16 | 0.13 (0.09, 0.19) | 0.12 (0.08, 0.18) | 0.15 (0.09, 0.25) | 0.12 (0.07, 0.22) | 0.22 (0.08, 0.59) | 0.23 (0.08, 0.67) | 0.26 (0.16, 0.42) | 0.21 (0.12, 0.35) |
| 16 to <18 | 0.34 (0.26, 0.45) | 0.34 (0.25, 0.46) | 0.41 (0.30, 0.58) | 0.38 (0.26, 0.56) | 0.35 (0.17, 0.73) | 0.40 (0.18, 0.90) | 0.61 (0.43, 0.85) | 0.58 (0.40, 0.84) |
| 18 to <20 | REF | REF | REF | REF | REF | REF | REF | REF |
| 20 to <22 | 1.95 (1.39, 2.74) | 2.24 (1.55, 3.23) | 1.28 (0.89, 1.84) | 1.29 (0.83, 2.01) | 1.14 (0.62, 2.10) | 1.25 (0.61, 2.59) | 1.06 (0.66, 1.70) | 1.00 (0.59, 1.69) |
| ≥22 | 5.25 (2.33, 11.85) | 5.29 (2.28, 12.26) | 1.17 (0.60, 2.30) | 0.99 (0.48, 2.05) | 0.80 (0.33, 1.94) | 0.74 (0.27, 2.04) | 1.12 (0.54, 2.32) | 1.15 (0.54, 2.49) |
| Male | 1.19 (0.83, 1.70) | 1.30 (0.89, 1.90) | 1.89 (1.12, 3.18) | 2.12 (1.23, 3.65) | 2.23 (1.21, 4.11) | 1.96 (0.99, 3.86) | 1.96 (1.17, 3.28) | 2.19 (1.27, 3.76) |
| Black race | 0.44 (0.27, 0.70) | 0.56 (0.34, 0.94) | 0.38 (0.19, 0.76) | 0.36 (0.16, 0.81) | 0.54 (0.27, 1.09) | 0.72 (0.30, 1.71) | 0.62 (0.33, 1.18) | 0.59 (0.29, 1.19) |
| Hispanic ethnicity | 0.91 (0.50, 1.65) | 1.15 (0.61, 2.17) | 0.52 (0.24, 1.10) | 0.54 (0.23, 1.28) | 0.35 (0.12, 1.04) | 0.42 (0.12, 1.48) | 0.66 (0.28, 1.55) | 0.63 (0.25, 1.61) |
| Maternal education: less than college |
0.70 (0.48, 1.02) | 0.78 (0.50, 1.20) | 1.17 (0.71, 1.94) | 1.20 (0.68, 2.11) | 1.17 (0.62, 2.21) | 1.55 (0.72, 3.35) | 1.05 (0.64, 1.72) | 1.05 (0.63, 1.74) |
| Income | ||||||||
| ≤$36k | 0.56 (0.34, 0.91) | 0.61 (0.36, 1.03) | 0.73 (0.39, 1.36) | 0.90 (0.46, 1.76) | 0.43 (0.20, 0.92) | 0.36 (0.15, 0.89) | 1.11 (0.61, 2.02) | 1.27 (0.68, 2.39) |
| >$36k to $75k | REF | REF | REF | REF | REF | REF | REF | REF |
| >$75k | 1.23 (0.80, 1.89) | 1.20 (0.75, 1.90) | 0.86 (0.49, 1.51) | 0.90 (0.50, 1.64) | 0.72 (0.34, 1.54) | 0.82 (0.38, 1.77) | 1.17 (0.66, 2.07) | 1.09 (0.61, 1.98) |
| Glomerular | 1.10 (0.77, 1.58) | 1.24 (0.84, 1.82) | 0.98 (0.60, 1.61) | 1.21 (0.72, 2.03) | 1.02 (0.55, 1.90) | 1.19 (0.61, 2.33) | 0.94 (0.58, 1.52) | 1.05 (0.64, 1.74) |
| CKD Risk Category | ||||||||
| A | REF | REF | REF | REF | REF | REF | REF | REF |
| B to C | 1.05 (0.73, 1.50) | 1.29 (0.88, 1.87) | 1.40 (0.88, 2.24) | 1.57 (0.95, 2.61) | 1.29 (0.64, 2.63) | 1.64 (0.75, 3.57) | 1.06 (0.66, 1.72) | 1.22 (0.76, 1.95) |
| D to E | 1.18 (0.74, 1.89) | 1.20 (0.74, 1.96) | 1.84 (1.02, 3.30) | 1.58 (0.83, 3.01) | 1.53 (0.68, 3.44) | 1.95 (0.83, 4.63) | 1.12 (0.64, 1.98) | 1.01 (0.55, 1.86) |
| F to ESKD | 1.26 (0.76, 2.09) | 1.36 (0.77, 2.39) | 3.33 (1.78, 6.25) | 2.89 (1.45, 5.78) | 3.79 (1.47, 9.76) | 3.64 (1.24, 10.73) | 1.59 (0.84, 3.04) | 1.39 (0.71, 2.72) |
| Uncontrolled BP | 1.00 (0.75, 1.34) | 1.02 (0.74, 1.42) | 1.50 (1.01, 2.21) | 1.18 (0.76, 1.85) | 1.40 (0.84, 2.32) | 1.23 (0.66, 2.30) | 1.82 (1.29, 2.56) | 1.71 (1.14, 2.57) |
| Anemia | 0.86 (0.63, 1.19) | 0.86 (0.60, 1.21) | 0.91 (0.61, 1.36) | 0.58 (0.36, 0.95) | 1.27 (0.76, 2.14) | 0.89 (0.46, 1.73) | 1.20 (0.80, 1.80) | 1.14 (0.71, 1.81) |
Bivariate models for age category (14 or older) were univariate, with no other variables besides age included in model
Bivariate models, with the exception of age category models, included the variable at hand as well as age category (14 or older)
Odds ratios obtained for multivariate estimates for all variables besides uncontrolled BP and anemia adjusted for the following covariates: age category (14 or older), male sex, black race, Hispanic ethnicity, maternal education, income, glomerular disease, and risk category (Model 1)
Odds ratios obtained for multivariate estimates for uncontrolled BP used Model 1 + uncontrolled BP
Odds ratios obtained for multivariate estimates for anemia used Model 1 + anemia
Males were more likely to smoke cigarettes (adjusted OR: 2.12, 95%CI: 1.23, 3.65) and marijuana (aOR: 2.19, 95%CI: 1.27, 3.76) over the past year. Participants identifying as Black were less likely to report use; this was statistically significant for alcohol (aOR: 0.56, 95%CI: 0.34, 0.94) and cigarettes (aOR: 0.36 95%CI: 0.16, 0.81). Severe CKD, based on CKD risk category, was associated with higher odds of cigarette (aOR: 2.89, 95%CI: 1.45, 5.78) and e-cigarette use (aOR: 3.64, 95%CI: 1.24, 10.73). Uncontrolled BP was associated with higher odds of use for all substances, but only marijuana was statistically significant (aOR 1.71, 95%CI: 1.14, 2.57). The same models were fit for current use with similar results (Supplemental Table 1).Lastly, we found that the odds of current cigarette use was 8.71 (95%CI: 4.01, 18.90) times higher among those who reported currently using e-cigarettes, controlling for age and sex. The odds ratio of past year and current cigarette use for those who ever lived with a smoker (vs. never lived with a smoker), controlling for age and sex, was 2.99 (95%CI: 1.94, 4.60) and 4.54 (95%CI: 2.69, 7.69), respectively. For e-cigarettes, those who had had ever previously lived with a smoker had increased odds of past year (OR: 2.48, 95%CI: 1.34, 4.60) and past 30-day (OR: 2.43, 95%CI: 1.25, 4.71) e-cigarette use.
DISCUSSION
Using a large cohort of AYA with CKD, we described SU in this population, compared prevalence rates to national estimates, and identified risk factors for use of each substance. Consistent with previous studies, older age was strongly associated with SU (23) and alcohol was the most commonly reported (12), a phenomenon also observed in the general adolescent population (24). While prevalence rates of nearly all substances consistently increased with age and plateaued among adolescent and young adult males, young adult females appeared to lose interest: cigarette, e-cigarette and marijuana use decreased by early adulthood.
The prevalence rates of current alcohol use in this cohort were lower than prevalence estimates in the general population, and the disparity was greater among those 14–18 years. This was consistent with most substances (with the exception of e-cigarettes among young adults). These findings were also congruent with previous literature in a mostly non-CKD young adult population (25). Given the chronic nature of pediatric kidney diseases, we expected less use compared to peers overall because of parental supervision and potentially health-protective behaviors. Increased autonomy in young adults with CKD may lead to this diminished disparity with the general population, and highlights the importance of supporting the transition from pediatric to adult care through education and encouraging self-management of CKD, including limiting or abstaining from substances. However, these differences could in part be due to selection bias because CKiD participants and their families are involved in a longitudinal cohort study and may not be representative of the larger pediatric CKD population in terms of these behaviors (the Hawthorne effect).
Participants 12 to <14 years consistently reported nearly no current SU (0% to <1%), and incident and regular use in this population typically occurred after age 14, which has been observed in similar populations (10). Detecting incident use was a key feature of our study design, suggesting that interventions to discourage SU initiation will be optimal for those under 14 years.
Among those who did report SU, the frequency was relatively low. Nearly half of alcohol users reported only one or two drinks in the past month. Similarly, among those reporting e-cigarette use, about 60% reported using only one or two days in the past month. However, there were limited longitudinal data for e-cigarettes compared to other substances, and rapidly changing trends in e-cigarette use among AYA warrants further analysis (26). Similarly, while marijuana use and frequency among current users were low, there is a need for continued data collection as legalization policies for medical and recreational purposes become more common.
Previous e-cigarette use in high school children has been shown to be predictive of future cigarette use (27), and there is evidence that children living with a smoker are more likely to use cigarettes (28). In the present study, the odds of current cigarette use were far greater among those who reported using e-cigarettes, and the odds of past year and current cigarette and e-cigarette use among who had ever previously lived with a cigarette smoker were significantly higher as well. If AYA with CKD have a household member who smokes or uses substances, or if they themselves are using e-cigarettes, clinical considerations for this group is warranted. These findings also highlight the potential benefits of broader tobacco cessation campaigns which could benefit children living in smoking households.
We anticipated that those with worse kidney function would be less likely to engage in SU due to poor health, but the results did not support this hypothesis. Although we note that the overall prevalence rate for current use was low, more severe disease was associated with increased odds of cigarette smoking. A previous CKiD study showed that secondhand smoke exposure was associated with nephrotic range proteinuria (7), which was consistent with the results for cigarette smoking observed in this analysis. There may be confounding related to the close relationship between older age and disease severity because of the progressive nature of pediatric CKD, and cigarette smoking is more likely among older participants. Further research on the impact of cigarette smoking on CKD is needed to address this relationship.
There were several limitations to our analysis. First, although participants were assured of confidential responses, reporting bias remains a concern. We expect that SU was under-reported for AYA, and acknowledge that differential reporting bias may be present in subpopulations. For example, we observed that Black participants were less likely to report use, and previous literature has demonstrated differential marijuana reporting among Black young adults without CKD (29). Second, there were no data on reason for SU, such as social settings (parties) versus isolation (coping or self-medication) which would be helpful to explain use and tailor interventions. Third, national surveys used slightly different questionnaires (13,14,16), but still offer important context to interpret study results. Additionally, there were limited data for those ≥22 years due to progression to KRT (18), and these data were not collected among those after KRT initiation. Our inferences are only generalizable to AYA with CKD prior to KRT. Lastly, biomarkers of SU were not collected which could identify potential reporting bias and agreement through objective measures.
CONCLUSIONS
Although all participants were considered at risk for SU, we demonstrated that those ≥18 years who identify as non-Black and non-Hispanic with worse disease severity are likely at highest risk, although the reasons for this are not entirely clear. We note that these risk factors are not deterministic or causal but may be used to guide clinicians on conversations regarding alcohol, cigarette, e-cigarette and marijuana use. Ages 12–14 may be the optimal time to initiate conversations and screening within this population in order to prevent use, using methods like Screening, Brief Intervention, and Referral to Treatment (referred to as SBIRT), or tools such as the Brief Screener for Tobacco, Alcohol and other Drugs (BSTAD) or Screening to Brief Intervention (S2BI), all of which have been validated and recommended for use in adolescent populations (30–32). It was encouraging that this population overall used substances at lower rates than the general population, indicating positive health choices on average and, at least with parental support, management of their condition by limiting SU.
These findings provide important SU data among AYAs with a history of a pediatric CKD. As new products like e-cigarettes evolve, marijuana policies change, and alcohol and tobacco remain public health problems, important conversations on SU prevention efforts should also be informed by the epidemiology in unique and high-risk populations like AYA with CKD.
Supplementary Material
ACKNOWLEDGMENTS
Data in this manuscript were collected by the Chronic Kidney Disease in Children prospective cohort study (CKiD) with clinical coordinating centers (Principal Investigators) at Children’s Mercy Hospital and the University of Missouri - Kansas City (Bradley Warady, MD) and Children’s Hospital of Philadelphia (Susan Furth, MD, PhD), Central Biochemistry Laboratory (George Schwartz, MD) at the University of Rochester Medical Center, and data coordinating center (Alvaro Muñoz, PhD and Derek K. Ng, PhD) at the Johns Hopkins Bloomberg School of Public Health. CKiD is supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases, with additional funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, and the National Heart, Lung, and Blood Institute (U01 DK066143, U01 DK066174, U24 DK082194, U24 DK066116). The CKiD website is located at https://statepi.jhsph.edu/ckid, a list of CKiD collaborators can be found in the Supplementary Material and at https://statepi.jhsph.edu/ckid/site-investigators/.
LIST OF ABBREVIATIONS
- AYA
adolescents and young adults
- CKD
chronic kidney disease
- CKiD
the Chronic Kidney Disease in Children Study
- SU
substance use
- YRBSS
Youth Risk Behavior Surveillance System
- NSDUH
National Survey on Drug Use and Health
- NHIS
National Health Interview Survey
- eGFR
estimated glomerular filtration rate
- uPCR
urine protein-to-creatinine ratio
- ESKD
end-stage kidney disease
- BP
blood pressure
- OR
odds ratio
- aOR
adjusted odds ratio
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Copelovitch L, Warady BA, Furth SL. Insights from the Chronic Kidney Disease in Children (CKiD) Study. Clin J Am Soc Nephrol 2011;6:2047–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferris ME, Gipson DS, Kimmel PL, Eggers PW. Trends in treatment and outcomes of survival of adolescents initiating end-stage renal disease care in the United States of America. Pediatr Nephrol 2006;21:1020–6. [DOI] [PubMed] [Google Scholar]
- 3.Kaspar CDW, Bholah R, Bunchman TE. A Review of Pediatric Chronic Kidney Disease. Blood Purif 2016;41:211–7. [DOI] [PubMed] [Google Scholar]
- 4.Whyte DA, Fine RN. Chronic kidney disease in children. Pediatr Rev 2008;29:335–41. [DOI] [PubMed] [Google Scholar]
- 5.Gutman T, Hanson CS, Bernays S, Craig JC, Sinha A, Dart A, et al. Child and Parental Perspectives on Communication and Decision Making in Pediatric CKD: A Focus Group Study. Am J Kidney Dis 2018;72:547–59. [DOI] [PubMed] [Google Scholar]
- 6.Weitzman ER, Salimian PK, Rabinow L, Levy S. Perspectives on substance use among youth with chronic medical conditions and implications for clinical guidance and prevention: A qualitative study. PLoS One 2019;14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Omoloja A, Jerry-Fluker J, Ng DK, Abraham AG, Furth S, Warady BA, et al. Secondhand smoke exposure is associated with proteinuria in children with chronic kidney disease. Pediatr Nephrol 2013;28:1243–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Omoloja A, Tyc VL. Tobacco and the pediatric chronic kidney disease population. Pediatr Nephrol 2015;30:235–43. [DOI] [PubMed] [Google Scholar]
- 9.Omoloja A, Chand D, Greenbaum L, Wilson A, Bastian V, Ferris M, et al. Cigarette smoking and second-hand smoking exposure in adolescents with chronic kidney disease: a study from the Midwest Pediatric Nephrology Consortium. Nephrol Dial Transplant 2011;26:908–13. [DOI] [PubMed] [Google Scholar]
- 10.Xiao N, Stolfi A, Malatesta-Muncher R, Bholah R, Kogon A, Eddington A, et al. Risk Behaviors in Teens with Chronic Kidney Disease: A Study from the Midwest Pediatric Nephrology Consortium. Int J Nephrol 2019;2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Furth SL, Cole SR, Moxey-Mims M, Kaskel F, Mak R, Schwartz G, et al. Design and Methods of the Chronic Kidney Disease in Children (CKiD) Prospective Cohort Study. Clin J Am Soc Nephrol 2006;1:1006–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Queen B, et al. Youth Risk Behavior Surveillance —United States, 2017 2018;67:479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Overview | YRBSS | Adolescent and School Health | CDC 2018. https://www.cdc.gov/healthyyouth/data/yrbs/overview.htm. Accessed June 10, 2019.
- 14.NSDUH - About the Survey n.d. https://nsduhweb.rti.org/respweb/about_nsduh.html. Accessed February 3, 2020.
- 15.2017 NSDUH Detailed Tables | CBHSQ Data n.d. https://www.samhsa.gov/data/report/2017-nsduh-detailed-tables. Accessed February 3, 2020.
- 16.NHIS - About the National Health Interview Survey n.d. https://www.cdc.gov/nchs/nhis/about_nhis.htm. Accessed February 18, 2020.
- 17.Ng DK, Moxey-Mims M, Warady BA, Furth SL, Muñoz A. Racial differences in renal replacement therapy initiation among children with a nonglomerular cause of chronic kidney disease. Ann Epidemiol 2016;26:780–787.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ng DK, Matheson MB, Warady BA, Mendley SR, Furth SL, Muñoz A. Incidence of Initial Renal Replacement Therapy Over the Course of Kidney Disease in Children. Am J Epidemiol 2019;188:2156–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ng DK, Schwartz GJ, Schneider MF, Furth SL, Warady BA. Combination of pediatric and adult formulas yield valid glomerular filtration rate estimates in young adults with a history of pediatric chronic kidney disease. Kidney Int 2018;94:170–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Furth SL, Pierce C, Hui WF, White CA, Wong CS, Schaefer F, et al. Estimating Time to ESRD in Children With CKD. Am J Kidney Dis 2018;71:783–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics 2017;140. [DOI] [PubMed] [Google Scholar]
- 22.Hollowell JG, van Assendelft OW, Gunter EW, Lewis BG, Najjar M, Pfeiffer C, et al. Hematological and iron-related analyes-reference data for persons aged 1 year and over: United States, 1988–94. Vital Health Stat 11 2005:1–156. [PubMed] [Google Scholar]
- 23.2016–2017 NSDUH State Estimates Categorized into Five Groups by Age Group | CBHSQ Data n.d. https://www.samhsa.gov/data/report/2016-2017-nsduh-state-estimates-categorized-five-groups-age-group. Accessed August 20, 2020.
- 24.CDC. Teen Substance Use & Risks. Centers for Disease Control and Prevention; 2020. https://www.cdc.gov/ncbddd/fasd/features/teen-substance-use.html. Accessed February 10, 2021. [Google Scholar]
- 25.Stam H, Hartman EE, Deurloo JA, Groothoff J, Grootenhuis MA. Young Adult Patients with a History of Pediatric Disease: Impact on Course of Life and Transition into Adulthood. J Adolesc Health 2006;39:4–13. [DOI] [PubMed] [Google Scholar]
- 26.Evans-Polce RJ, Veliz P, Boyd CJ, McCabe SE. Initiation Patterns and Trends of E-Cigarette and Cigarette Use Among U.S. Adolescents. J Adolesc Health 2020;66:27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bold KW, Kong G, Camenga DR, Simon P, Cavallo DA, Morean ME, et al. Trajectories of E-Cigarette and Conventional Cigarette Use Among Youth. Pediatrics 2018;141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vuolo M, Staff J. Parent and Child Cigarette Use: A Longitudinal, Multigenerational Study. Pediatrics 2013;132:e568–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ramo DE, Liu H, Prochaska JJ. Reliability and validity of young adults’ anonymous online reports of marijuana use and thoughts about use. Psychol Addict Behav 2012;26:801–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Levy SJL, Williams JF, Prevention C on SUA. Substance Use Screening, Brief Intervention, and Referral to Treatment. Pediatrics 2016;138. [DOI] [PubMed] [Google Scholar]
- 31.Kelly SM, Gryczynski J, Mitchell SG, Kirk A, O’Grady KE, Schwartz RP. Validity of Brief Screening Instrument for Adolescent Tobacco, Alcohol, and Drug Use. Pediatrics 2014;133:819–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Levy S, Weiss R, Sherritt L, Ziemnik R, Spalding A, Van Hook S, et al. An Electronic Screen for Triaging Adolescent Substance Use by Risk Levels. JAMA Pediatr 2014;168:822–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.