Abstract
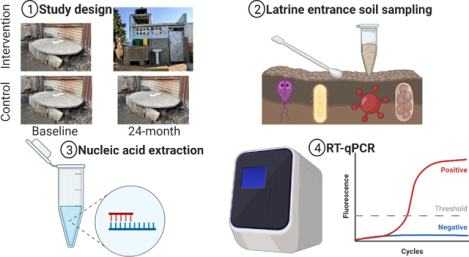
Environmental fecal contamination is common in many low-income cities, contributing to a high burden of enteric infections and associated negative sequelae. To evaluate the impact of a shared onsite sanitation intervention in Maputo, Mozambique on enteric pathogens in the domestic environment, we collected 179 soil samples at shared latrine entrances from intervention (n= 49) and control (n= 51) compounds during baseline (pre-intervention) and after 24 months (post-intervention) as part of the Maputo Sanitation Trial. We tested soils for the presence of nucleic acids associated with 18 enteric pathogens using a multiplex reverse transcription qPCR platform. We detected at least one pathogen-associated gene target in 91% (163/179) of soils and a median of 3 (IQR=1, 5) pathogens. Using a difference-in-difference analysis and adjusting for compound population, visibly wet soil, sun exposure, wealth, temperature, animal presence, and visible feces, we estimate the intervention reduced the probability of detecting ≥1 pathogen gene by 15% (adjusted prevalence ratio, aPR=0.85; 95% CI: 0.70, 1.0) and the total number of pathogens by 35% (aPR =0.65; 0.44, 0.95) in soil 24 months following the intervention. These results suggest that the intervention reduced the presence of some fecal contamination in the domestic environment, but pathogen detection remained prevalent 24-months following the introduction of new latrines.
Keywords: Onsite sanitation, urban slum, latrines, fecal sludge management, exposure
Graphical Abstract
INTRODUCTION
Onsite sanitation systems are designed to sequester human feces away from human contact and prevent the transport of fecal-oral pathogens through well-defined transmission pathways.1 Large-scale, rigorous randomized controlled trials (RCTs) of onsite sanitation systems – including sanitation alone and combinations of water, sanitation, and hygiene (WASH) interventions – have found mixed effects on health outcomes, such as diarrhea and child growth.2–7 Assessing the impact of WASH interventions on enteric pathogens in the environment can improve our understanding of pathogen transmission from an infected individual to a new host via the environment, a core intermediate outcome of these trials. Such data may help explain why some WASH interventions observed improved health outcomes and others did not.8
There is a growing body of literature that soils contaminated by feces in public and domestic environments pose infection risks.9–13 In health impact trials that assess improved onsite sanitation systems, soils are assessed to measure how effectively the intervention sequestered human feces.14–18 Latrines and septic tanks are useful barriers against the transport of human feces into the environment. However, enteric pathogens may still move into soils through open defecation19, unhygienic pit emptying20,21, fecally contaminated greywater22,23, improper disposal of children’s feces or anal cleansing materials24,25, latrine flooding20,26,27, animal feces28–30, or subsurface transport from unlined pits31–33. Domestic soils contaminated by enteric pathogens can pose infection risks beyond incidental34 and direct35 soil ingestion: contaminated soil may be transported to hands, food, fomites, or household stored water.36 For these reasons, soils may be a useful matrix to assess the impact of onsite sanitation interventions.
Detecting enteric pathogens via molecular methods is increasingly used to assess the impact of WASH interventions on the transport of these pathogens through the environment.37–39 Molecular detection of pathogens offers additional insights, as health impact studies have historically relied on fecal indicator bacteria (FIB), as a proxy for enteric pathogens for reasons of cost, capacity and feasibility.17,36,40–42 However, a 2016 meta-analysis43 found that improved sanitation had no effect on the presence of FIB in the environment, possibly because these indicators are often pervasive in low-income settings15,16,36,44–46 and common FIB, like E. coli, may be naturalized in the environment47–49.
The Maputo Sanitation (MapSan) Trial was the first rigorous controlled before-and-after trial to evaluate the effect of an urban onsite sanitation intervention on child health.24,50,51 We conducted the trial in low-income, informal neighborhoods in Maputo, Mozambique, where WASH conditions are poor, and the burden of enteric disease is high.20,24,44,52 Water and Sanitation for the Urban Poor (WSUP, a non-governmental organization) delivered the intervention to compounds composed of household clusters that shared sanitation and courtyard space. Control compounds were concurrently enrolled from the same or adjacent neighborhoods as intervention compounds and continued using existing shared sanitation infrastructure. Detailed descriptions of the inclusion criteria for intervention and control compounds are described elsewhere.20,24
The intervention was built inside the compound boundary and was part of the households’ living environment. WSUP replaced shared onsite sanitation systems in poor condition with pour-flush toilets that included septic tanks and soak-away pits. There were two versions of the intervention: shared latrines, serving 15–20 individuals, and community sanitation blocks for compounds with >20 residents. Shared latrines became the property of the residents and included a toilet, superstructure, septic tank, and a lined infiltration pit. Community sanitation blocks officially remained the property of the municipality and included the same infrastructure as a shared latrine, but contained multiple toilets (one toilet per twenty people), a new piped water connection with a water storage tank, sink pedestal for handwashing (no running water but the drain was connected to the septic tank), rainwater harvesting tank, cement laundry basin, and community sanitation blocks used by ≥60 residents received a urinal on an external wall of the structure which drained to the septic tank. Compound residents that received community sanitation blocks formed sanitation management committees, which were responsible for maintaining the sanitation infrastructure. The septic tanks in the shared latrines and community sanitation blocks were sized according to the number of users and were designed to be emptied every two years.
A latrine entrance is an ideal soil sampling location to determine the effectiveness of onsite sanitation interventions because it is a standardized location near the fecal waste in the containment chamber.15,16,53 Soils in low-income Maputo are characterized as coarse to fine sand or silty sand.54 While the fate and transport of pathogens through soils is dependent on the individual pathogen and environmental conditions55, the high porosity of Maputo’s sandy soils combined with a high water table in the study area44 offers potential for pathogen movement.56 This high risk of fecal contamination suggests we could plausibly observe a reduction in enteric pathogens in soil at latrine entrances if the intervention infrastructure performed better than controls at safely containing fecal wastes.57 Our study aim was to assess if the intervention reduced the detection of ≥1 pathogen gene, the total number of pathogens, or any individual pathogen in latrine entrance soils from MapSan intervention compounds compared to controls.
MATERIALS AND METHODS
Sample Collection
We prospectively collected latrine entrance soil samples – defined as a location one-meter away from the latrine entrance in the direction of entry or the nearest point not covered by cement – from 49 intervention and 51 control compounds at baseline (pre-intervention) and from the same compounds 24-months following the intervention, for a total of 200 samples (Text S1). We defined this sample location a priori as one that could be standardized across all compounds in the study. Compounds were selected using convenience sampling. Using a spade and ruler, we scooped soil from a 10 cm × 10 cm area to a depth of 1 cm into a Whirl-Pak® bag (Nasco, Fort Atkinson, WI). The spade and ruler were sterilized between uses with 10% bleach and 70% ethanol. At the time of sampling, enumerators recorded whether the soil was visibly wet and estimated the daily sun exposure (full sun, partially shaded, full shade).44 Samples were stored on ice for transport to the Ministry of Health in Maputo, Mozambique, frozen at −20°C for approximately six months, aliquoted into 2 ml cryovials while working on dry ice, and then stored at −80°C. During storage at −20°C, some samples (n = 21) were unable to be evaluated because the permanent marker labeling on some Whirl-Pak® bags wore off and some bags burst open. All aliquoted samples (n = 179) were shipped from the Mozambican Ministry of Health in Maputo, Mozambique to Atlanta, GA, USA on dry ice (-80° C) with temperature monitoring for molecular analysis. We obtained compound observation data and socioeconomic characteristics from the MapSan baseline and 24-month survey datasets, which were collected concurrent to soil samples.24,58
Sample Processing
At Georgia Institute of Technology in Atlanta, GA, USA, we incubated 250 mg of each soil sample at 105°C for 1 hour to determine moisture content13,59, then discarded the dry soil. We then extracted total nucleic acids from a separate 1-gram (calculated for dry weight) portion of each sample, and spiked samples with approximately 107 plaque-forming units MS2 (Luminex Corporation, Austin, TX) as an extraction control. Following the manufacturer’s protocol, we extracted RNA using the RNeasy PowerSoil Total RNA Kit and DNA using the RNeasy PowerSoil DNA Elution Kit (Qiagen, Hilden, Germany). On each day of extraction (approximately every 5–15 samples), we included one negative extraction control (sterile deionized water). We tested sample extracts for matrix inhibition using the Applied Biosystems Exogenous Internal Positive Control Assay60 (Applied Biosystems, Waltham, Massachusetts) before downstream molecular analysis (Text S2).
We assayed extracted nucleic acids from all samples using a custom TaqMan Array Card (TAC) (ThermoFisher Scientific, Waltham, MA) that tested for genes from 18 enteric pathogens in duplicate wells following Liu et al. 201361, including ten bacteria (Campylobacter jejuni/coli, Clostridium difficile [tcdA and tcdB gene], Enteroaggregative E. coli [EAEC, aaiC and aatA gene], Shigella/Enteroinvasive E. coli [EIEC, ipaH gene], Enteropathogenic E. coli [EPEC, bfpA and eae gene], Enterotoxigenic E. coli [ETEC, heat-labile and heat-stabile enterotoxin genes LT and ST], Shiga-toxin producing E. coli [STEC, stx1 and stx2], Salmonella spp., Vibrio cholerae, and Yersinia spp.), four viruses (adenovirus 40/41, astrovirus, norovirus [GI and GII], and rotavirus A), two protozoa (Entamoeba histolytica and Giardia duodenalis) and two soil-transmitted helminths (Ascaris lumbricoides, Trichuris trichiura) (Text S3, Table S1, Table S2).62 We combined and then added 25 μL of RNA eluant, 25 μL of DNA eluant, and 50 μL of mastermix (qScript XLT 1-Step RT-qPCR ToughMix Low-ROX, Quantabio, Beverly, MA) into each TAC port. We included a positive and negative control on each TAC. The positive control was a plasmid that included all assay gene sequences and the negative control was either extract from a negative extraction control or sterile water.63 We performed one-step reverse transcription qPCR on each TAC using a QuantStudio 7 (Thermo Fisher Scientific, Waltham, MA) with the following thermocycling conditions: 45°C for 10 minutes and 94°C for 10 minutes, followed by 45 cycles of 94°C for 30 seconds and 60°C for 1 minute, with a ramp rate of 1°C/second between each step. We visually compared exponential curves and multicomponent plots with the positive control plots to validate positive amplification12; positive amplification in one or both duplicate wells below a quantification cycle (Cq) of 40 was called as a positive for a target (Text S3).62,64 In addition, we ran a 5-fold dilution series of positive control material as a standard curve to determine the linearity and efficiency of each assay (Table S3).
Data analysis
We analyzed data in R version 4.0.0 (R Foundation for Statistical Computing, Vienna, Austria). We used a difference-in-difference (DID)65 approach to assess the impact of the intervention – our exposure variable – on our outcomes compared to the control group. DID is a quasi-experimental method that uses longitudinal data from intervention and control groups. Fundamental to the DID method is the parallel trend assumption, which assumes that the initial difference between the two groups remains constant over time. Our outcomes included the detection (i.e., binary presence/absence) of ≥1 of the enteric pathogen genes measured, the total number of pathogens detected out of 18, and each individual pathogen (Table S4). We used generalized estimating equations (GEE)66 to fit unadjusted and adjusted Poisson regression models with robust standard errors, with an exchangeable correlation structure. We accounted for clustering between compounds across the two study phases because the intervention was implemented at the compound level.67
To generate adjusted estimates, we selected nine covariates from the MapSan baseline and 24-month datasets based on their biological plausibility to impact the transport57 or persistence68 of pathogens in the domestic environment and previously reported associations in the literature36,44 (Table S4). We used the same nine covariates to adjust all DID models: compound population (a 10-person increase in compound population), wealth (one-quartile increase in wealth index69), soil moisture (assessed visually at the time of sampling), sun exposure status (estimated at the time of sampling; full sun, partially shaded, shaded44), the mean-centered average air temperature in Fahrenheit for the day of and day preceding sample collection (i.e., two-day average), a binary variable for the presence of cats, a binary variable for the presence of dogs, a binary variable for the presence of chickens or ducks, and a binary variable for the presence of visible animal or human feces in the compound (Table S4).
To estimate the intervention’s effect, we used the interaction of dummy variables representing treatment status (intervention vs. control) and trial phase (baseline or 24-month). Consequently, we present the effect estimates from our DID analysis as ratio measures (ratio of prevalence ratios, PR) instead of absolute differences. We fit separate GEE models to measure the association between intervention status and the detection of ≥1 pathogen gene and the total number of pathogens detected among the 18 targets we identified a priori (Table S4). Likewise, we fit DID models to estimate the intervention’s impact for each individual pathogen assessed, but we excluded any pathogen not detected in at least 5% of control and intervention samples during both phases.
Ethics
The study protocol was approved by the Comité Nacional de Bioética para a Saúde (CNBS), Ministério da Saúde (333/CNBS/14), the Research Ethics Committee of the London School of Hygiene and Tropical Medicine (reference # 8345), and the Institutional Review Board of the Georgia Institute of Technology (protocol # H15160). The overall trial was pre-registered at ClinicalTrials.gov (NCT02362932), but we did not pre-register this environmental analysis.
RESULTS
Matched samples
We analyzed latrine entrance soils collected at baseline from 48 control compounds and 43 intervention compounds, and soils collected at the 24-month phase from 45 control and 43 intervention compounds (Table S5). We did not analyze twelve intervention samples and nine control samples because they were either lost or damaged during storage. This resulted in some samples collected at either phase not having a matched sample from the same compound from the earlier or later phase. Among the 93 control samples analyzed, 42 compounds had samples from both phases (n=84), six baseline samples did not have a matched 24-month phase sample, and three 24-month samples did not have a matched baseline sample. Among the 86 intervention samples analyzed, 41 compounds had samples from both phases (n=82), two baseline samples did not have a matched 24-month phase sample, and two 24-month samples did not have a matched baseline sample. There was a mean of 788 days between the collection of matched control samples (sd = 36, min = 733, max = 860) and a mean of 789 days between matched intervention samples (sd = 56, min = 731, max = 953). Control and intervention samples were collected approximately during the same period of the year (Figure S1).
Compound characteristics
Control and intervention compounds had similar wealth indices at baseline (mean= 0.47 [sd=0.09] and mean=0.46 [sd=0.09], respectively, p=0.49) but control compounds had higher wealth indices at the 24-month phase (mean=0.46 [sd=0.12] and mean=0.40 [sd=0.09], respectively, p=0.05) (Table 1). The number of residents in the intervention compounds was greater than control compounds at baseline (mean=19 [sd=7.8] and mean=14 [sd=6.4], respectively, p=0.004) and at the 24-month phase (mean=16 [sd=7.9] and mean=13 [sd=7.0], respectively, p=0.02) (Table 1).
Table 1.
Characteristics of MapSan trial compounds and households selected for soil sampling
| Baseline | 24-Month Phase | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Control | Intervention | Control | Intervention | |||||||
| Characteristic | Level | Metric | N | Summary | N | Summary | N | Summary | N | Summary |
| Wealth index (0–1) | household | mean (sd) | 48 | 0.47 (0.09) | 43 | 0.46 (0.09) | 45 | 0.44 (0.12) | 43 | 0.40 (0.09) |
| Compound population | compound | mean (sd) | 48 | 14 (6.4) | 43 | 19 (7.8) | 45 | 13 (7.0) | 43 | 16 (7.9) |
| Any animal(s) present | compound | n (%) | 48 | 28 (58%) | 43 | 28 (65%) | 45 | 32 (71%) | 43 | 35 (81%) |
| Cat(s) present | compound | n (%) | 48 | 24 (50%) | 43 | 23 (53%) | 45 | 32 (71%) | 43 | 30 (70%) |
| Chicken(s) or duck(s) present | compound | n (%) | 48 | 6 (13%) | 43 | 7 (16%) | 45 | 4 (8.9%) | 43 | 8 (19%) |
| Dog(s) present | compound | n (%) | 48 | 3 (6.3%) | 43 | 4 (9.3%) | 45 | 9 (20%) | 43 | 10 (23%) |
| Other animal(s) present | compound | n (%) | 48 | 1 (2.1%) | 43 | 2 (4.7%) | 45 | 1 (2.2%) | 43 | 0 (0%) |
| Visible human or animal feces | compound | n (%) | 48 | 22 (46%) | 43 | 22 (51%) | 45 | 4 (8.9%) | 43 | 4 (9.3%) |
| Visibly wet soil | sample | n (%) | 48 | 37 (77%) | 43 | 34 (79%) | 45 | 37 (82%) | 43 | 34 (79%) |
| Partially shaded soil | sample | n (%) | 48 | 24 (50%) | 43 | 13 (30%) | 45 | 30 (67%) | 43 | 28 (65%) |
| Fully shaded soil | sample | n (%) | 48 | 14 (29%) | 43 | 20 (47%) | 45 | 10 (22%) | 43 | 9 (21%) |
| Temperature (°F) | date | mean (sd) | 48 | 72 (4.5) | 43 | 70 (4.3) | 45 | 72 (4.7) | 43 | 73 (5.3) |
| No useable sanitation infrastructure | compound | n (%) | 48 | 3 (6.3%) | 43 | 4 (9.3%) | 45 | 0 (0%) | 43 | 0 (0%) |
| Pit latrine with slab | compound | n (%) | 48 | 27 (56%) | 43 | 14 (14%) | 45 | 18 (40%) | 43 | 0 (0%) |
| Pit latrine without slab | compound | n (%) | 48 | 16 (33%) | 43 | 24 (56%) | 45 | 14 (31%) | 43 | 0 (0%) |
| Pour-flush toilet (non-intervention) | compound | n (%) | 48 | 2 (4.2%) | 43 | 1 (2.2%) | 45 | 13 (29%) | 43 | 0 (0%) |
| Intervention infrastructure | compound | n (%) | 48 | 0 (0%) | 43 | 0 (0%) | 45 | 0 (0%) | 43 | 43 (100%) |
Note: Wealth index created using the 2013 Simple Poverty Scorecard© for Mozambique
Reported or observed animal ownership was high across trial arms during both phases (Table 1). Most compounds had at least one animal at baseline (62% [56/91]) including cats (50% [24/48] control, 53% [23/43] intervention), chickens or ducks (13% [6/48] control, 16% [7/43] intervention), and dogs (6.3% [3/48] control, 9.3% [4/43] intervention). Three-quarters of compounds had at least one animal 24-months post intervention (76% [67/88]): cats were most common (71% [32/45] control, 70% intervention [30/43]), followed by dogs (20% [9/45] control, 23% [10/43] intervention), and chickens or ducks (8.9% [4/45] control, 19% [8/43] intervention).
At baseline seven compounds had no useable sanitation infrastructure (6.3% [3/48] control, 9.3% [4/43] intervention) and three compounds had pour-flush sanitation (4.2% [2/48] control, 2.3% [1/43] intervention) (Table 1). Control compounds more often had pit latrines with slabs (56%, [27/48]) than without slabs (33%, [16/48]), compared to intervention compounds, which more often had pit latrines without slabs (56%, [24/43]) than with slabs (33%, [14/43]) (p=0.09). At the 24-month phase, most control compounds had a pit latrine (with slab 40%, [18/45]; without slab 31%, [14/45]), but some (29%, [13/45]) had independently upgraded their pit latrines to pour-flush toilets. All intervention compounds (100%, [43/43]) still had the intervention sanitation infrastructure at the 24-month phase.
Laboratory Controls
We did not observe inhibition in any sample (Text S2). We observed positive amplification for all assays using our positive controls (n = 32). We did not observe positive amplification for any assay in our extraction controls (n=16), nor any no template controls (n=16) below a Cq of 40. Although we did observe positive amplification for EPEC (eae gene) in two no template controls above a Cq of 40.
All Pathogens
We detected at least one pathogen-associated gene in 91% (163/179) of latrine entrance soils, genes from two or more pathogens in 75% (134/179), and a mean of 3.3 out of 18 measured pathogen targets (IQR=4). The four most frequently detected pathogens were Ascaris lumbricoides (62%, [111/179]), EAEC (46%, [82/179]), Giardia duodenalis (36%, [64/179]), and astrovirus (26%, [47/179]). We found evidence that the intervention reduced the detection of ≥1 pathogen gene in latrine entrance soils by 15% (aPR = 0.85, 95% CI [0.70, 1.0]) and the total number of pathogens by 35% (aPR = 0.65, 95% CI [0.44, 0.95]) (Table 2). The mean Cq values of detected pathogen genes were similar across trial arms and phases (Table S6).
Table 2.
Detection of pathogens at baseline and 24-month
| Detection | ||||
|---|---|---|---|---|
| Baseline Detection | 24-month Detection | Unadjusted BL-24M DID estimate | Adjusted BL-24M DID estimate | |
| ≥1 pathogen gene | ||||
| control | 0.88 (42/48) | 0.96 (43/45) | 0.82 (0.68, 1.0) p = 0.05 |
0.85 (0.70, 1.0) p = 0.11 |
| intervention | 0.95 (41/43) | 0.86 (37/43) | ||
| Total pathogen detects (out of 18) | Mean (IQR) | Mean (IQR) | ||
| control | 3.5 (4) | 3.8 (3) | 0.67 (0.45, 1.0) p = 0.05 |
0.65 (0.44, 0.95) p = 0.03 |
| intervention | 3.5 (3) | 2.5 (2.5) |
Note: DID: difference-in-difference. BL: baseline. 24M: 24-month. IQR: Inter-quartile range
There was a consistent trend among all individual pathogens except for astrovirus: the adjusted point estimates for nine of the ten most frequently detected suggest the intervention reduced the prevalence of these pathogens in soils compared to controls (Table 3). Among these nine pathogens, we observed a significant reduction in Ascaris lumbricoides (aPR = 0.62, 95% CI [0.39, 0.98]), EAEC (aPR=0.51, 95% CI [0.27, 0.94]), and EPEC (aPR = 0.20 95% CI [0.05, 0.82]).
Table 3.
Detection of individual pathogens at baseline and 24-month. Sorted by detection in control soils at the 24-month phase.
| Pathogen | ||||
|---|---|---|---|---|
| Baseline Detection | 24-month Detection | Unadjusted BL-24M DID estimate╪ | Adjusted BL-24M DID estimate╪ | |
| Ascaris lumbricoides | ||||
| control | 0.65 (31/48) | 0.76 (34/45) | 0.64 (0.40, 1.0) p = 0.06 |
0.62 (0.39, 0.98) p = 0.04 |
| intervention | 0.63 (27/43) | 0.44 (19/43) | ||
| Enteroaggregative E. coli | ||||
| control | 0.42 (20/48) | 0.53 (24/45) | 0.57 (0.30, 1.1) p = 0.08 |
0.51 (0.27, 0.94) p = 0.03 |
| intervention | 0.51 (22/43) | 0.37 (16/43) | ||
| Giardia duodenalis | ||||
| control | 0.42 (20/48) | 0.38 (17/45) | 0.76 (0.34, 1.7) p = 0.50 |
0.85 (0.37, 1.9) p = 0.69 |
| intervention | 0.37 (16/43) | 0.26 (11/43) | ||
| Shigella/Enteroinvasive E. coli | ||||
| control | 0.33 (16/48) | 0.33 (15/45) | 0.58 (0.17, 1.9) p = 0.37 |
0.59 (0.18, 1.9) p= 0.38 |
| intervention | 0.16 (7/43) | 0.09 (4/43) | ||
| Enterotoxigenic E. coli | ||||
| control | 0.25 (12/48) | 0.33 (15/45) | 0.45 (0.17, 1.2) p = 0.10 |
0.44 (0.17, 1.1) p = 0.09 |
| intervention | 0.35 (15/43) | 0.21 (9/43) | ||
| adenovirus 40/41 | ||||
| control | 0.23 (11/48) | 0.33 (15/45) | 0.34 (0.08, 1.5) p = 0.19 |
0.32 (0.07, 1.5) p = 0.14 |
| intervention | 0.14 (6/43) | 0.07 (3/43) | ||
| astrovirus | ||||
| control | 0.23 (11/48) | 0.27 (12/45) | 1.3 (0.51, 3.1) p = 0.62 |
1.6 (0.60, 4.0) p = 0.36 |
| intervention | 0.23 (10/43) | 0.33 (14/43) | ||
| Enteropathogenic E. coli | ||||
| control | 0.15 (7/48) | 0.24 (11/45) | 0.20 (0.05, 0.88) p = 0.02 |
0.20 (0.05, 0.82) p = 0.03 |
| intervention | 0.21 (9/43) | 0.07 (3/43) | ||
| Trichuris trichiura | ||||
| control | 0.31 (15/48) | 0.18 (8/45) | 1.0 (0.33, 3.2) p = 0.96 |
0.95 (0.32, 2.9) p = 0.93 |
| intervention | 0.28 (12/43) | 0.16 (7/43) | ||
| Clostridium difficile | ||||
| control | 0.13 (6/48) | 0.16 (7/45) | 0.68 (0.17, 2.8) p = 0.59 |
0.70 (0.16, 3.0) p = 0.62 |
| intervention | 0.16 (7/43) | 0.14 (6/43) | ||
| Salmonella spp. | ||||
| control | 0.02 (1/48) | 0.09 (4/45) | NA | |
| intervention | 0.05 (2/43) | 0.05 (2/43) | ||
| Shiga-toxin producing E. coli | ||||
| control | 0.02 (1/48) | 0.07 (3/45) | NA | |
| intervention | 0 (0/43) | 0.02 (1/43) | ||
|
Campylobacter jejuni/coli |
||||
| control | 0.15 (7/48) | 0.04 (2/45) | NA | |
| intervention | 0.09 (4/43) | 0.09 (4/43) | ||
| Yersinia spp. | ||||
| control | 0.02 (1/48) | 0.04 (2/45) | NA | |
| intervention | 0.05 (2/43) | 0.05 (2/43) | ||
| norovirus GI/GII | ||||
| control | 0.06 (3/48) | 0.02 (1/45) | NA | |
| intervention | 0.07 (3/43) | 0.02 (1/43) | ||
| rotavirus A | ||||
| control | 0.08 (4/48) | 0 (0/45) | NA | |
| intervention | 0.14 (6/43) | 0.09 (4/43) | ||
| Entamoeba histolytica | ||||
| control | 0.02 (1/48) | 0 (0/45) | NA | |
| intervention | 0.02 (1/43) | 0.02 (1/43) | ||
| Vibrio cholerae | ||||
| control | 0 (0/48) | 0 (0/45) | NA | |
| intervention | 0 (0/43) | 0 (0/43) |
Note: DID: difference-in-difference.
We did not calculate DID estimates for pathogens with <5% detection
DISCUSSION
We found evidence that the onsite shared urban sanitation intervention evaluated in the MapSan trial was somewhat protective against the detection of ≥1 pathogen gene and against the total number of pathogens in latrine entrance soils. Though the confidence intervals for the detection of ≥1 pathogen gene included one, meaning that there may have been no true effect of the intervention on this outcome. The adjusted estimates for nine of the ten most common pathogens suggest the intervention reduced their presence in soils compared to controls (DID estimates = 0.20–0.95) and pathogen-specific effect estimates from adjusted models indicated a significant reduction in Ascaris lumbricoides, EAEC, and EPEC. This suggests that intervention septic tanks may have better sequestered or inactivated these pathogens, which are passed in stool, compared with controls.
Seven of the ten pathogens we most frequently detected in soils were measured in child stools via multiplex end-point PCR as part of the MapSan trial. These seven include Ascaris lumbricoides, Giardia duodenalis, Shigella/EIEC, ETEC, adenovirus 40/41, Trichuris trichiura, and Clostridium difficile, while EAEC, EPEC, and astrovirus were not measured in stools. At baseline, Shigella/EIEC (44%) and Trichuris trichiura (37%) – generally thought to be transmitted human-to-human – were the second and third most common pathogens detected in child stool24,50, following Giardia (51%) which can be zoonotic70. Given the high prevalence of these anthroponotic enteric pathogens in stools and the lack of a zoonotic reservoir for Shigella/EIEC and Trichuris trichiura71,72, the trial may have had greater power to observe an effect on Shigella/EIEC and Trichuris trichiura compared with other pathogens. For children born into study compounds before the 24-month visit, the intervention reduced the detection of Shigella/EIEC in children’s stools by 51% and Trichuris trichiura by 76%.58 Results from soils in this study differ from trial findings in stools: we observed a 41% reduction in the point estimate for Shigella/EIEC detection but the wide confidence interval indicates this result was not significant, and we identified no difference with respect to detection of Trichuris trichiura. This absence of impact on Trichuris trichiura in soils may have been due to limited power from infrequent detection; we did observe a reduction in the other STH assessed, Ascaris lumbricoides, which was the most frequently detected individual pathogen in soils. The MapSan trial found the sanitation intervention reduced the detection of Ascaris lumbricoides by 32% among children born into study compounds before the 24-month visit, but the confidence interval extended above one indicating the intervention may have had no true effect or may even have increased children’s risk of infection.58 Overall, the protective trend we observed in soils, therefore, is consistent with the enteric infection data for children born into trial compounds. This may suggest that the intervention reduced the transport of pathogens to latrine entrance soils, and subsequently contributed to a reduction in children’s exposures, but our small sample size and the resulting uncertainty of point estimates suggest results should be interpreted with caution.
Compared to other recent large-scale, rigorous trials of onsite sanitation improvements in rural Bangladesh (pour flush to double-pit latrine)2, rural Kenya (single unlined pit latrine with plastic slab and hole-lid)3, and rural Zimbabwe (ventilated improved pit latrine)4, we evaluated a more sophisticated intervention that included site-specific engineered septic tanks and subsurface discharge of aqueous effluent to a soakaway pit24,73, and it is the only recent controlled health impact trial of onsite sanitation to take place in an urban setting. In the early 2000s, Barreto et al. observed health benefits from household sewerage connections in urban Brazil in an uncontrolled trial74,75. However, the scope, complexity, and cost of that intervention make it an imperfect point of comparison.
The WASH Benefits Trial (WASH-B) evaluated the impact of single and combined water, sanitation, and handwashing intervention arms in rural Bangladesh and Kenya. In Bangladesh, a molecular analysis of household entrance soils, hand rinses, and stored water from the sanitation arm found no significant reductions in enteric pathogens (EAEC, EPEC, STEC, Shigella/EIEC, ETEC, norovirus, Cryptosporidium spp., Giardia duodenalis) or microbial source tracking markers (HumM2, BacCow).38 The combined WASH arm and individual water treatment arm observed a reduction in E. coli prevalence and concentration in stored drinking water; the individual water treatment and handwashing arms reduced E. coli prevalence and concentration in food. WASH-B trial arms in Bangladesh did not observe reductions in E. coli in courtyard soil, ambient waters, child hands, or sentinel objects.76,77 Likewise, WASH-B Kenya found the individual water treatment arm and combined WASH arm reduced culturable E. coli in stored drinking water, but not along other transmission pathways.18 The Sanitation, Hygiene, Infant Nutrition Efficacy Project (SHINE) trial in rural Zimbabwe has not yet published the results from a sub-study on environmental fecal contamination. In separate analyses of environmental samples collected during MapSan baseline15 and the 24-month phase13,21,44 we found widespread fecal contamination in soils and other environmental compartments. At the 12-month MapSan trial phase Holcomb et al. 2021 found the intervention reduced E. coli gene densities by more than 1-log10 in latrine entrance soils, but observed no reduction in culturable E. coli or human microbial source tracking markers.78 Our study is the first controlled evaluation of an urban onsite sanitation intervention to show a decrease in the detection of enteric pathogens, via molecular methods, in soils from the domestic living environment.
The intervention may have reduced the presence of enteric pathogens in soils compared with controls because the intervention may have better sequestered or treated fecal material than control latrines. In high-income countries, properly designed, constructed, and maintained septic tank systems have been demonstrated to be efficient and economic alternatives to public sewage disposal systems.79 Although some pathogen die-off will occur in pit latrines, the primary purpose of pit latrines is to sequester human feces and reduce exposures, and they are not designed to achieve a specific level of pathogen reduction.80 Design features of the intervention septic tanks may have resulted in better treatment of fecal wastes than control systems. Intervention septic tanks contained inlet and outlet pipes configured to maximize detention time, baffles to direct incoming waste downward, t-pipes to ensure sequestration of solids and floatable materials, and a sealed containment chamber to promote anaerobic treatment of stored solids and non-settleable materials. In addition, the intervention septic tank systems represented an upgrade to a more permanent sanitation infrastructure. The construction included masonry block walls, a concrete floor, masonry block lined septic tank, masonry block lined soakaway pit, tin roof, and a water seal squat pan.20,24,53,73 These features may have acted as a physical barrier that prevented the contamination of soils by enteric pathogens. At the 24-month phase, most control compounds used a pit latrine with or without a slab, and therefore lacked similar physical barriers such as a water seal. In addition, the control compounds that did upgrade to pour flush sanitation may not have used the same rigorous design criteria as intervention septic tanks.50
Pit latrines in low-income Maputo are often covered when full and rebuilt, or the fecal sludge is emptied and buried or dumped nearby.20 The intervention included programming to encourage hygienic pit emptying and provided equipment and training to local organizations to offer hygienic emptying services.73 During the 24-month phase, only 5.6% of intervention compounds had emptied their sanitation systems in the previous year, compared to 30% of controls.20 In addition, intervention compounds were 3.8 more likely to have their onsite systems emptied hygienically than control compounds.20 Less frequent emptying would have been beneficial for two reasons. First, longer residence times would likely have resulted in greater pathogen die-off.80 Second, less frequent emptying would have created fewer opportunities for environmental fecal contamination to occur and hygienic emptying may have reduced the quantity of fecal sludge that contaminated soils during emptying. In addition, intervention systems contained a drain for bathing, which may have prevented fecally contaminated graywater from flowing into nearby soils, and the concrete floors were likely easier to clean than control systems with dirt floors.56
Although our findings suggest that some pathogens appeared to be reduced by the latrine improvements, it is likely that the potential for exposure remains high in this setting.13 While we detected some individual pathogens, such as Ascaris lumbricoides, EAEC, Shigella/EIEC and EPEC, in intervention soils less frequently compared to controls during the 24-month phase, we also detected one or more enteric pathogens in 86% of intervention latrine entrance soils two years post-intervention. Fecal waste from children unable to use the latrines was not addressed by the intervention.28,81 At the 24-month follow-up, 29% (289/980) of children reported defecating into a latrine, 29% (281/980) defecated into a child potty which was emptied into a latrine, 20% (192/980) used disposable diapers that were disposed with solid waste, 7.3% defecated on the ground (72/980), and 2.7% (26/980) defecated into diapers that were washed and reused (Table S7). In addition, the intervention did not address animal feces. While we adjusted for animals in our DID estimates, many animals are not penned in this setting and may defecate outside of their respective compounds, which was not accounted for in our analysis.30 Live chickens are also commonly purchased and stored in the compound for consumption.82 We may not have adequately captured this intermittent chicken ownership in our cross-sectional surveys.
The similar reduction in pathogen detection in soils and child stools may be informative about exposures. At two years post-intervention in the MapSan cohort, children born into study compounds were 1–24 months old, while children born previously and enrolled at baseline were 25–73 months old.58 Considering the consistent reduction in the detection of pathogens observed in soils and stools from children 1–24 months old, the dominant exposure pathways for these younger children may be inside the compound or soil ingestion may have represented a more important transmission pathway for these children.83 Older children are more mobile than younger children, and their potential exposures outside of study compounds may explain why the intervention did not reduce the prevalence of pathogen carriage among them.
Our study had several limitations, including a relatively small sample size that was not intended to observe small reductions in pathogen detection. Nevertheless, in high burden settings, sanitation interventions may need to achieve a large reduction in environmental fecal contamination both within households and in the larger community to reduce exposure risks and yield improved health outcomes.84 Further, intervention compounds had lower wealth indices and higher compound populations 24-months post intervention compared to control. This may suggest we underestimated changes due to sanitation improvements, but we adjusted for these in our regression analyses and did not observe substantial differences between unadjusted and adjusted point estimates that would indicate confounding. In addition, we assessed gene targets via molecular assays – which may not be 100% sensitive or specific61,85,86 – that can be effected by target specific inhibitors87 and did not assess pathogen viability or infectivity.
There is substantial evidence that city-wide upgrades to sewerage infrastructure improve health outcomes.74,75,88 However, the high capital and maintenance costs89, and water usage requirements90 of such improvements suggest they are currently impractical for many LMICs. Until sewerage becomes widely feasible in high-burden settings, onsite sanitation systems remain necessary to achieve safely managed sanitation in many urban areas. The results of this study – and other rigorous environmental impact evaluations of onsite sanitation interventions18,38,77 – suggest that fecal contamination is transported into the environment through multiple complex pathways that may vary among settings.91 In urban Maputo – and similar settings with poor sanitation infrastructure, widespread environmental fecal contamination, and a high burden of enteric infection – other, more transformative interventions interrupting multiple transmission pathways may need to accompany improvements to onsite sanitation infrastructure. These improvements likely require an integrated and incremental approach that might include legal protections (e.g. land tenure)92, contact control interventions (e.g. hardscape cleanable flooring)13,93,94, public infrastructure (e.g. drainage, and improvements in quality, quantity, and access to water)95, and public services (e.g. education, hygienic fecal sludge and solid waste management)20,96,97. Such improvements may reduce the transport of enteric pathogens into the environment through site-specific pathways and subsequently reduce children’s infection risks.
Supplementary Material
Text S1. Compound enrollment at baseline
Text S2. Test for Matrix Inhibition
Text S3. Custom TaqMan Array Card (TAC)
Table S1. Assays used on the custom TAC
Table S2. Interpretation of gene targets on the TAC
Table S3. Standard curve
Table S4. Description of variables and their respective sources
Table S5. Soils samples matched at baseline and 24-month trial periods
Figure S1. Histogram of dates that latrine entrance soils were collected
Table S6. Mean Cq Values
Table S7. Child feces disposal at 24-month phase
SYNOPSIS.
Widespread fecal contamination in urban slums presents exposure risks. Effective onsite sanitation can reduce enteric pathogen detection in soils.
Acknowledgments
This study was funded by the United States Agency for International Development (www.usaid.gov) under Translating Research into Action (Cooperative Agreement No. GHS-A-00-09-00015-00) and the Bill and Melinda Gates Foundation (www.gatesfoundation.org) grant OPP1137224. DC was supported in part by T32ES007018. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- (1).Wagner E; Lanoix J Excreta Disposal for Rural Areas and Small Communities. Monogr Ser World Heal. Organ 1958, 39, 1–182. [PubMed] [Google Scholar]
- (2).Luby SP; Rahman M; Arnold BF; Unicomb L; Ashraf S; Winch PJ; Stewart CP; Begum F; Hussain F; Benjamin-Chung J; Leontsini E; Naser AM; Parvez SM; Hubbard AE; Lin A; Nizame FA; Jannat K; Ercumen A; Ram PK; Das KK; Abedin J; Clasen TF; Dewey KG; Fernald LC; Null C; Ahmed T; Colford JM Effects of Water Quality, Sanitation, Handwashing, and Nutritional Interventions on Diarrhoea and Child Growth in Rural Bangladesh: A Cluster Randomised Controlled Trial. Lancet Glob. Heal 2018, 6 (3), e302–e315. 10.1016/S2214-109X(17)30490-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (3).Null C; Stewart CP; Pickering AJ; Dentz HN; Arnold BF; Arnold CD; Benjamin-Chung J; Clasen T; Dewey KG; Fernald LCH; Hubbard AE; Kariger P; Lin A; Luby SP; Mertens A; Njenga SM; Nyambane G; Ram PK; Colford JM Effects of Water Quality, Sanitation, Handwashing, and Nutritional Interventions on Diarrhoea and Child Growth in Rural Kenya: A Cluster-Randomised Controlled Trial. Lancet Glob. Heal 2018, 6 (3), e316–e329. 10.1016/S2214-109X(18)30005-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (4).Humphrey JH; Mbuya MNN; Ntozini R; Moulton LH; Stoltzfus RJ; Tavengwa NV; Mutasa K; Majo F; Mutasa B; Mangwadu G; Chasokela CM; Chigumira A; Chasekwa B; Smith LE; Tielsch JM; Jones AD; Manges AR; Maluccio JA; Prendergast AJ; Humphrey JH; Jones AD; Manges A; Mangwadu G; Maluccio JA; Mbuya MNN; Moulton LH; Ntozini R; Prendergast AJ; Stoltzfus RJ; Tielsch JM; Chasokela C; Chigumira A; Heylar W; Hwena P; Kembo G; Majo FD; Mutasa B; Mutasa K; Rambanepasi P; Sauramba V; Tavengwa NV; Van Der Keilen F; Zambezi C; Chidhanguro D; Chigodora D; Chipanga JF; Gerema G; Magara T; Mandava M; Mavhudzi T; Mazhanga C; Muzaradope G; Mwapaura MT; Phiri S; Tengende A; Banda C; Chasekwa B; Chidamba L; Chidawanyika T; Chikwindi E; Chingaona LK; Chiorera CK; Dandadzi A; Govha M; Gumbo H; Gwanzura KT; Kasaru S; Makasi R; Matsika AM; Maunze D; Mazarura E; Mpofu E; Mushonga J; Mushore TE; Muzira T; Nembaware N; Nkiwane S; Nyamwino P; Rukobo SD; Runodamoto T; Seremwe S; Simango P; Tome J; Tsenesa B; Amadu U; Bangira B; Chiveza D; Hove P; Jombe HA; Kujenga D; Madhuyu L; Makoni PM; Maramba N; Maregere B; Marumani E; Masakadze E; Mazula P; Munyanyi C; Musanhu G; Mushanawani RC; Mutsando S; Nazare F; Nyarambi M; Nzuda W; Sigauke T; Solomon M; Tavengwa T; Biri F; Chafanza M; Chaitezvi C; Chauke T; Chidzomba C; Dadirai T; Fundira C; Gambiza AC; Godzongere T; Kuona M; Mafuratidze T; Mapurisa I; Mashedze T; Moyo N; Musariri C; Mushambadope M; Mutsonziwa TR; Muzondo A; Mwareka R; Nyamupfukudza J; Saidi B; Sakuhwehwe T; Sikalima G; Tembe J; Chekera TE; Chihombe O; Chikombingo M; Chirinda T; Chivizhe A; Hove R; Kufa R; Machikopa TF; Mandaza W; Mandongwe L; Manhiyo F; Manyaga E; Mapuranga P; Matimba FS; Matonhodze P; Mhuri S; Mike J; Ncube B; Nderecha WTS; Noah M; Nyamadzawo C; Penda J; Saidi A; Shonhayi S; Simon C; Tichagwa M; Chamakono R; Chauke A; Gatsi AF; Hwena B; Jawi H; Kaisa B; Kamutanho S; Kaswa T; Kayeruza P; Lunga J; Magogo N; Manyeruke D; Mazani P; Mhuriyengwe F; Mlambo F; Moyo S; Mpofu T; Mugava M; Mukungwa Y; Muroyiwa F; Mushonga E; Nyekete S; Rinashe T; Sibanda K; Chemhuru M; Chikunya J; Chikwavaire VF; Chikwiriro C; Chimusoro A; Chinyama J; Gwinji G; Hoko-Sibanda N; Kandawasvika R; Madzimure T; Maponga B; Mapuranga A; Marembo J; Matsunge L; Maunga S; Muchekeza M; Muti M; Nyamana M; Azhuda E; Bhoroma U; Biriyadi A; Chafota E; Chakwizira A; Chamhamiwa A; Champion T; Chazuza S; Chikwira B; Chingozho C; Chitabwa A; Dhurumba A; Furidzirai A; Gandanga A; Gukuta C; Macheche B; Marihwi B; Masike B; Mutangandura E; Mutodza B; Mutsindikwa A; Mwale A; Ndhlovu R; Nduna N; Nyamandi C; Ruvata E; Sithole B; Urayai R; Vengesa B; Zorounye M; Bamule M; Bande M; Chahuruva K; Chidumba L; Chigove Z; Chiguri K; Chikuni S; Chikwanda R; Chimbi T; Chingozho M; Chinhamo O; Chinokuramba R; Chinyoka C; Chipenzi X; Chipute R; Chiribhani G; Chitsinga M; Chiwanga C; Chiza A; Chombe F; Denhere M; Dhamba E; Dhamba M; Dube J; Dzimbanhete F; Dzingai G; Fusira S; Gonese M; Gota J; Gumure K; Gwaidza P; Gwangwava M; Gwara W; Gwauya M; Gwiba M; Hamauswa J; Hlasera S; Hlukani E; Hotera J; Jakwa L; Jangara G; Janyure M; Jari C; Juru D; Kapuma T; Konzai P; Mabhodha M; Maburutse S; Macheka C; Machigaya T; Machingauta F; Machokoto E; Madhumba E; Madziise L; Madziva C; Madzivire M; Mafukise M; Maganga M; Maganga S; Mageja E; Mahanya M; Mahaso E; Mahleka S; Makanhiwa P; Makarudze M; Makeche C; Makopa N; Makumbe R; Mandire M; Mandiyanike E; Mangena E; Mangiro F; Mangwadu A; Mangwengwe T; Manhidza J; Manhovo F; Manono I; Mapako S; Mapfumo E; Mapfumo T; Mapuka J; Masama D; Masenge G; Mashasha M; Mashivire V; Matunhu M; Mavhoro P; Mawuka G; Mazango I; Mazhata N; Mazuva D; Mazuva M; Mbinda F; Mborera J; Mfiri U; Mhandu F; Mhike C; Mhike T; Mhuka A; Midzi J; Moyo S; Mpundu M; Msekiwa N; Msindo D; Mtisi C; Muchemwa G; Mujere N; Mukaro E; Muketiwa K; Mungoi S; Munzava E; Muoki R; Mupura H; Murerwa E; Murisi C; Muroyiwa L; Muruvi M; Musemwa N; Mushure C; Mutero J; Mutero P; Mutumbu P; Mutya C; Muzanango L; Muzembi M; Muzungunye D; Mwazha V; Ncube T; Ndava T; Ndlovu N; Nehowa P; Ngara D; Nguruve L; Nhigo P; Nkiwane S; Nyanyai L; Nzombe J; Office E; Paul B; Pavari S; Ranganai S; Ratisai S; Rugara M; Rusere P; Sakala J; Sango P; Shava S; Shekede M; Shizha C; Sibanda T; Tapambwa N; Tembo J; Tinago N; Tinago V; Toindepi T; Tovigepi J; Tuhwe M; Tumbo K; Zaranyika T; Zaru T; Zimidzi K; Zindo M; Zindonda M; Zinhumwe N; Zishiri L; Ziyambi E; Zvinowanda J; Bepete E; Chiwira C; Chuma N; Fari A; Gavi S; Gunha V; Hakunandava F; Huku C; Hungwe G; Maduke G; Manyewe E; Mapfumo T; Marufu I; Mashiri C; Mazenge S; Mbinda E; Mhuri A; Muguti C; Munemo L; Musindo L; Ngada L; Nyembe D; Taruvinga R; Tobaiwa E; Banda S; Chaipa J; Chakaza P; Chandigere M; Changunduma A; Chibi C; Chidyagwai O; Chidza E; Chigatse N; Chikoto L; Chingware V; Chinhamo J; Chinhoro M; Chiripamberi A; Chitavati E; Chitiga R; Chivanga N; Chivese T; Chizema F; Dera S; Dhliwayo A; Dhononga P; Dimingo E; Dziyani M; Fambi T; Gambagamba L; Gandiyari S; Gomo C; Gore S; Gundani J; Gundani R; Gwarima L; Gwaringa C; Gwenya S; Hamilton R; Hlabano A; Hofisi E; Hofisi F; Hungwe S; Hwacha S; Hwara A; Jogwe R; Kanikani A; Kuchicha L; Kutsira M; Kuziyamisa K; Kuziyamisa M; Kwangware B; Lozani P; Mabuto J; Mabuto V; Mabvurwa L; Machacha R; Machaya C; Madembo R; Madya S; Madzingira S; Mafa L; Mafuta F; Mafuta J; Mahara A; Mahonye S; Maisva A; Makara A; Makover M; Mambongo E; Mambure M; Mandizvidza E; Mangena G; Manjengwa E; Manomano J; Mapfumo M; Mapfurire A; Maphosa L; Mapundo J; Mare D; Marecha F; Marecha S; Mashiri C; Masiya M; Masuku T; Masvimbo P; Matambo S; Matarise G; Matinanga L; Matizanadzo J; Maunganidze M; Mawere B; Mawire C; Mazvanya Y; Mbasera M; Mbono M; Mhakayakora C; Mhlanga N; Mhosva B; Moyo N; Moyo O; Moyo R; Mpakami C; Mpedzisi R; Mpofu E; Mpofu E; Mtetwa M; Muchakachi J; Mudadada T; Mudzingwa K; Mugwira M; Mukarati T; Munana A; Munazo J; Munyeki O; Mupfeka P; Murangandi G; Muranganwa M; Murenjekwa J; Muringo N; Mushaninga T; Mutaja F; Mutanha D; Mutemeri P; Mutero B; Muteya E; Muvembi S; Muzenda T; Mwenjota A; Ncube S; Ndabambi T; Ndava N; Ndlovu E; Nene E; Ngazimbi E; Ngwalati A; Nyama T; Nzembe A; Pabwaungana E; Phiri S; Pukuta R; Rambanapasi M; Rera T; Samanga V; Shirichena S; Shoko C; Shonhe M; Shuro C; Sibanda J; Sibangani E; Sibangani N; Sibindi N; Sitotombe M; Siwawa P; Tagwirei M; Taruvinga P; Tavagwisa A; Tete E; Tete Y; Thandiwe E; Tibugari A; Timothy S; Tongogara R; Tshuma L; Tsikira M; Tumba C; Watinaye R; Zhiradzango E; Zimunya E; Zinengwa L; Ziupfu M; Ziyambe J; Church JA; Desai A; Fundira D; Gough E; Kambarami RA; Matare CR; Malaba TR; Mupfudze T; Ngure F; Smith LE; Curtis V; Dickin KL; Habicht J-P; Masimirembwa C; Morgan P; Pelto GH; Sheffner-Rogers C; Thelingwani R; Turner P; Zungu L; Makadzange T; Mujuru HA; Nyachowe C; Chakadai R; Chanyau G; Makamure MG; Chiwariro H; Mtetwa T; Chikunya J; Maguwu L; Nyadundu S; Moyo T; Chayima B; Mvindi L; Rwenhamo P; Muzvarwandoga S; Chimukangara R; Njovo H; Makoni T Independent and Combined Effects of Improved Water, Sanitation, and Hygiene, and Improved Complementary Feeding, on Child Stunting and Anaemia in Rural Zimbabwe: A Cluster-Randomised Trial. Lancet Glob. Heal 2019, 7 (1), e132–e147. 10.1016/S2214-109X(18)30374-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (5).Clasen T; Boisson S; Routray P; Torondel B; Bell M; Cumming O; Ensink J; Freeman M; Jenkins M; Odagiri M; Ray S; Sinha A; Suar M; Schmidt WP Effectiveness of a Rural Sanitation Programme on Diarrhoea, Soil-Transmitted Helminth Infection, and Child Malnutrition in Odisha, India: A Cluster-Randomised Trial. Lancet Glob. Heal 2014, 2 (11), e645–e653. 10.1016/S2214-109X(14)70307-9. [DOI] [PubMed] [Google Scholar]
- (6).Patil SR; Arnold BF; Salvatore AL; Briceno B; Ganguly S; Colford JM; Gertler PJ The Effect of India’s Total Sanitation Campaign on Defecation Behaviors and Child Health in Rural Madhya Pradesh: A Cluster Randomized Controlled Trial. PLoS Med. 2014, 11 (8), e1001709. 10.1371/journal.pmed.1001709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (7).Pickering AJ; Djebbari H; Lopez C; Coulibaly M; Alzua ML Effect of a Community-Led Sanitation Intervention on Child Diarrhoea and Child Growth in Rural Mali: A Cluster-Randomised Controlled Trial. Lancet. Glob. Heal 2015, 3 (11), e701–11. 10.1016/S2214-109X(15)00144-8. [DOI] [PubMed] [Google Scholar]
- (8).Goddard FGB; Ban R; Barr DB; Brown J; Cannon J; Colford JM; Eisenberg JNS; Ercumen A; Petach H; Freeman MC; Levy K; Luby SP; Moe C; Pickering AJ; Sarnat JA; Stewart J; Thomas E; Taniuchi M; Clasen T Measuring Environmental Exposure to Enteric Pathogens in Low-Income Settings: Review and Recommendations of an Interdisciplinary Working Group. Environmental Science and Technology. American Chemical Society; October 6, 2020, pp 11673–11691. 10.1021/acs.est.0c02421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (9).Mattioli MCM; Davis J; Boehm AB Hand-to-Mouth Contacts Result in Greater Ingestion of Feces than Dietary Water Consumption in Tanzania: A Quantitative Fecal Exposure Assessment Model. Environ. Sci. Technol 2015, 49 (3), 1912–1920. 10.1021/es505555f. [DOI] [PubMed] [Google Scholar]
- (10).Katukiza AY; Ronteltap M; van der Steen P; Foppen JWA; Lens PNL Quantification of Microbial Risks to Human Health Caused by Waterborne Viruses and Bacteria in an Urban Slum. J. Appl. Microbiol 2014, 116 (2), 447–463. 10.1111/jam.12368. [DOI] [PubMed] [Google Scholar]
- (11).Cairncross S; Blumenthal U; Kolsky P; Moraes L; Tayeh A The Public and Domestic Domains in the Transmission of Disease. Trop. Med. Int. Heal 1996, 1 (1), 27–34. 10.1046/j.1365-3156.1996.d01-9.x. [DOI] [PubMed] [Google Scholar]
- (12).Baker KK; Senesac R; Sewell D; Sen Gupta A; Cumming O; Mumma J Fecal Fingerprints of Enteric Pathogen Contamination in Public Environments of Kisumu, Kenya Associated with Human Sanitation Conditions and Domestic Animals. Environ. Sci. Technol 2018, acs.est.8b01528. 10.1021/acs.est.8b01528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (13).Capone D; Bivins A; Knee J; Cumming O; Nalá R; Brown J Quantitative Microbial Risk Assessment of Pediatric Infections Attributable to Ingestion of Fecally Contaminated Domestic Soils in Low-Income Urban Maputo, Mozambique. Environ. Sci. Technol 2021, 55 (3), 1941–1952. 10.1021/acs.est.0c06972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (14).Steinbaum L; Njenga SM; Kihara J; Boehm AB; Davis J; Null C; Pickering AJ Soil-Transmitted Helminth Eggs Are Present in Soil at Multiple Locations within Households in Rural Kenya. PLoS One 2016, 11 (6), e0157780. 10.1371/journal.pone.0157780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (15).Holcomb DA; Knee J; Sumner T; Adriano Z; de Bruijn E; Nalá R; Cumming O; Brown J; Stewart JR Human Fecal Contamination of Water, Soil, and Surfaces in Households Sharing Poor-Quality Sanitation Facilities in Maputo, Mozambique. Int. J. Hyg. Environ. Health 2020, 226, 113496. 10.1016/j.ijheh.2020.113496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (16).Pickering AJ; Julian TR; Marks SJ; Mattioli MC; Boehm AB; Schwab KJ; Davis J Fecal Contamination and Diarrheal Pathogens on Surfaces and in Soils among Tanzanian Households with and without Improved Sanitation. Environ. Sci. Technol 2012, 46 (11), 5736–5743. 10.1021/es300022c. [DOI] [PubMed] [Google Scholar]
- (17).Ercumen A; Pickering AJ; Kwong LH; Mertens A; Arnold BF; Benjamin-Chung J; Hubbard AE; Alam M; Sen D; Islam S; Rahman MZ; Kullmann C; Chase C; Ahmed R; Parvez SM; Unicomb L; Rahman M; Ram PK; Clasen T; Luby SP; Colford JM Do Sanitation Improvements Reduce Fecal Contamination of Water, Hands, Food, Soil, and Flies? Evidence from a Cluster-Randomized Controlled Trial in Rural Bangladesh. Environ. Sci. Technol 2018, 52 (21), 12089–12097. 10.1021/acs.est.8b02988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (18).Pickering AJ; Swarthout J; Mureithi M; Mboya J; Arnold BF; Wolfe M; Dentz HN; Lin A; Arnold CD; Rao G; Stewart CP; Ram PK; Clasen T; Colford JM; Null C Can Individual and Integrated Water, Sanitation, and Handwashing Interventions Reduce Fecal Contamination in the Household Environment? Evidence from the WASH Benefits Cluster-Randomized Trial in Rural Kenya. bioRxiv 2019, 731992. 10.1101/731992. [DOI] [Google Scholar]
- (19).World Health Organization. Guidelines on Sanitation and Health; Geneva, 2018. [Google Scholar]
- (20).Capone D; Buxton H; Cumming O; Dreibelbis R; Knee J; Nalá R; Ross I; Brown J Impact of an Intervention to Improve Pit Latrine Emptying Practices in Low Income Urban Neighborhoods of Maputo, Mozambique. Int. J. Hyg. Environ. Health 2020, 226. 10.1016/j.ijheh.2020.113480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (21).Capone D; Berendes D; Cumming O; Knee J; Nalá R; Risk BB; Stauber C; Zhu K; Brown J Analysis of Fecal Sludges Reveals Common Enteric Pathogens in Urban Maputo, Mozambique. Environ. Sci. Technol. Lett 2020. 10.1021/acs.estlett.0c00610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (22).Alexander KA; Godrej A Greywater Disposal Practices in Northern Botswana--The Silent Spring? Int. J. Environ. Res. Public Health 2015, 12 (11), 14529–14540. 10.3390/ijerph121114529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (23).Carden K; Armitage N; Sichone O; Winter K The Use and Disposal of Greywater in the Non-Sewered Areas of South Africa: Part 2 – Greywater Management Options. Water SA 2010, 33 (4). 10.4314/wsa.v33i4.52936. [DOI] [Google Scholar]
- (24).Knee J; Sumner T; Adriano Z; Berendes D; de Bruijn E; Schmidt W-P; Nalá R; Cumming O; Brown J Risk Factors for Childhood Enteric Infection in Urban Maputo, Mozambique: A Cross-Sectional Study. PLoS Negl. Trop. Dis 2018, 12 (11), e0006956. 10.1371/journal.pntd.0006956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (25).Miller-Petrie MK; Voigt L; McLennan L; Cairncross S; Jenkins MW Infant and Young Child Feces Management and Enabling Products for Their Hygienic Collection, Transport, and Disposal in Cambodia. Am. J. Trop. Med. Hyg 2016, 94 (2), 456–465. 10.4269/ajtmh.15-0423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (26).Borges Pedro JP; Oliveira C. A. da S.; de Lima SCRB; von Sperling MA Review of Sanitation Technologies for Flood-Prone Areas. J. Water, Sanit. Hyg. Dev 2020, 10 (3), 397–412. 10.2166/washdev.2020.019. [DOI] [Google Scholar]
- (27).Levy K; Woster AP; Goldstein RS; Carlton EJ Untangling the Impacts of Climate Change on Waterborne Diseases: A Systematic Review of Relationships between Diarrheal Diseases and Temperature, Rainfall, Flooding, and Drought. Environ. Sci. Technol 2016, 50 (10), 4905–4922. 10.1021/acs.est.5b06186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (28).Penakalapati G; Swarthout J; Delahoy MJ; McAliley L; Wodnik B; Levy K; Freeman MC Exposure to Animal Feces and Human Health: A Systematic Review and Proposed Research Priorities. Environ. Sci. Technol 2017, 51 (20), 11537–11552. 10.1021/acs.est.7b02811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (29).Berendes DM; Yang PJ; Lai A; Hu D; Brown J Estimation of Global Recoverable Human and Animal Faecal Biomass. Nat. Sustain 2018, 1 (11), 679–685. 10.1038/s41893-018-0167-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (30).Delahoy MJ; Wodnik B; McAliley L; Penakalapati G; Swarthout J; Freeman MC; Levy K Pathogens Transmitted in Animal Feces in Low- and Middle-Income Countries. Int. J. Hyg. Environ. Health 2018, 221 (4), 661–676. 10.1016/j.ijheh.2018.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (31).Graham JP; Polizzotto ML Pit Latrines and Their Impacts on Groundwater Quality: A Systematic Review. Environmnetal Heal. Perspect 2013, 5 (121), 521–530. 10.1289/ehp.1206028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (32).Nichols DS; Prettyman D; Gross M Movement of Bacteria and Nutrients from Pit Latrines in the Boundary Waters Canoe Area Wilderness. Water. Air. Soil Pollut 1983, 20 (2), 171–180. 10.1007/BF00279627. [DOI] [Google Scholar]
- (33).Chaúque BJM; Chicumbe CM; Cossa VC; Rott MB Spatial Arrangement of Well and Latrine and Their Influence on Water Quality in Clayey Soil – a Study in Low-Income Peri-Urban Neighborhoods in Lichinga, Mozambique. J. Water, Sanit. Hyg. Dev 2021. 10.2166/washdev.2021.137. [DOI] [Google Scholar]
- (34).Wang Y; Moe CL; Null C; Raj SJ; Baker KK; Robb KA; Yakubu H; Ampofo JA; Wellington N; Freeman MC; Armah G; Reese HE; Peprah D; Teunis PFM Multipathway Quantitative Assessment of Exposure to Fecal Contamination for Young Children in Low-Income Urban Environments in Accra, Ghana: The Sanipath Analytical Approach. Am. J. Trop. Med. Hyg 2017, 97 (4), 1009–1019. 10.4269/ajtmh.16-0408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (35).Kwong LH; Ercumen A; Pickering AJ; Unicomb L; Davis J; Leckie JO; Luby SP Soil Ingestion among Young Children in Rural Bangladesh. J. Expo. Sci. Environ. Epidemiol 2021, 31 (1), 82–93. 10.1038/s41370-019-0177-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (36).Ercumen A; Pickering AJ; Kwong LH; Arnold BF; Parvez SM; Alam M; Sen D; Islam S; Kullmann C; Chase C; Ahmed R; Unicomb L; Luby SP; Colford JM Animal Feces Contribute to Domestic Fecal Contamination: Evidence from E. Coli Measured in Water, Hands, Food, Flies, and Soil in Bangladesh. Environ. Sci. Technol 2017, 51 (15), 8725–8734. 10.1021/acs.est.7b01710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (37).Berendes DM; Kirby AE; Clennon JA; Agbemabiese C; Ampofo JA; Armah GE; Baker KK; Liu P; Reese HE; Robb KA; Wellington N; Yakubu H; Moe CL Urban Sanitation Coverage and Environmental Fecal Contamination: Links between the Household and Public Environments of Accra, Ghana. PLoS One 2018, 13 (7), e0199304. 10.1371/journal.pone.0199304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (38).Fuhrmeister ER; Ercumen A; Pickering AJ; Jeanis KM; Crider Y; Ahmed M; Brown S; Alam M; Sen D; Islam S; Kabir H; Islam M; Rahman M; Kwong LH; Arnold BF; Luby SP; Colford JM; Nelson KL Effect of Sanitation Improvements on Pathogens and Microbial Source Tracking Markers in the Rural Bangladeshi Household Environment. Cite This Environ. Sci. Technol 2020, 54, 4316–4326. 10.1021/acs.est.9b04835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (39).Bauza V; Madadi V; Ocharo R; Nguyen TH; Guest JS Enteric Pathogens from Water, Hands, Surface, Soil, Drainage Ditch, and Stream Exposure Points in a Low-Income Neighborhood of Nairobi, Kenya. Sci. Total Environ 2020, 709, 135344. 10.1016/j.scitotenv.2019.135344. [DOI] [PubMed] [Google Scholar]
- (40).Pickering AJ; Ercumen A; Arnold BF; Kwong LH; Parvez SM; Alam M; Sen D; Islam S; Kullmann C; Chase C; Ahmed R; Unicomb L; Colford JM; Luby SP Fecal Indicator Bacteria along Multiple Environmental Transmission Pathways (Water, Hands, Food, Soil, Flies) and Subsequent Child Diarrhea in Rural Bangladesh. Environ. Sci. Technol 2018, 52 (14), 7928–7936. 10.1021/acs.est.8b00928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (41).Ngure FM; Humphrey JH; Mbuya MNN; Majo F; Mutasa K; Govha M; Mazarura E; Chasekwa B; Prendergast AJ; Curtis V; Boor KJ; Stoltzfus RJ Formative Research on Hygiene Behaviors and Geophagy among Infants and Young Children and Implications of Exposure to Fecal Bacteria. Am. J. Trop. Med. Hyg 2013, 89 (4), 709–716. 10.4269/ajtmh.12-0568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (42).Navab-Daneshmand T; Friedrich MND; Gächter M; Montealegre MC; Mlambo LS; Nhiwatiwa T; Mosler HJ; Julian TR Escherichia Coli Contamination across Multiple Environmental Compartments (Soil, Hands, Drinking Water, and Handwashing Water) in Urban Harare: Correlations and Risk Factors. Am. J. Trop. Med. Hyg 2018, 98 (3), 803–813. 10.4269/ajtmh.17-0521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (43).Sclar GD; Penakalapati G; Amato HK; Garn JV; Alexander K; Freeman MC; Boisson S; Medlicott KO; Clasen T Assessing the Impact of Sanitation on Indicators of Fecal Exposure along Principal Transmission Pathways: A Systematic Review. Int. J. Hyg. Environ. Health 2016, 219 (8), 709–723. 10.1016/j.ijheh.2016.09.021. [DOI] [PubMed] [Google Scholar]
- (44).Capone D; Adriano Z; Berendes D; Cumming O; Dreibelbis R; Holcomb DA; Knee J; Ross I; Brown J A Localized Sanitation Status Index as a Proxy for Fecal Contamination in Urban Maputo, Mozambique. PLoS One 2019, 14 (10). 10.1371/journal.pone.0224333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (45).Montealegre MC; Roy S; Böni F; Hossain MI; Navab-Daneshmand T; Caduff L; Faruque ASG; Islam MA; Julian TR Risk Factors for Detection, Survival, and Growth of Antibiotic-Resistant and Pathogenic Escherichia Coli in Household Soils in Rural Bangladesh. Appl. Environ. Microbiol 2018. 10.1128/AEM.01978-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (46).Odagiri M; Schriewer A; Daniels ME; Wuertz S; Smith WA; Clasen T; Schmidt WP; Jin Y; Torondel B; Misra PR; Panigrahi P; Jenkins MW Human Fecal and Pathogen Exposure Pathways in Rural Indian Villages and the Effect of Increased Latrine Coverage. Water Res. 2016, 100, 232–244. 10.1016/j.watres.2016.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (47).Ishii S; Ksoll WB; Hicks RE; Sadowsky MJ Presence and Growth of Naturalized Escherichia Coli in Temperate Soils from Lake Superior Watersheds. Appl. Environ. Microbiol 2006, 72 (1), 612–621. 10.1128/AEM.72.1.612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (48).Byappanahalli MN; Yan T; Hamilton MJ; Ishii S; Fujioka RS; Whitman RL; Sadowsky MJ The Population Structure of Escherichia Coli Isolated from Subtropical and Temperate Soils. Sci. Total Environ 2012, 417–418, 273–279. 10.1016/j.scitotenv.2011.12.041. [DOI] [PubMed] [Google Scholar]
- (49).Nowicki S; DeLaurent ZR; de Villiers EP; Githinji G; Charles KJ The Utility of Escherichia Coli as a Contamination Indicator for Rural Drinking Water: Evidence from Whole Genome Sequencing. PLoS One 2021, 16 (1), e0245910. 10.1371/journal.pone.0245910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (50).Knee J; Sumner T; Adriano Z; Anderson C; Capone D; Eng B; Casmo V; Holcomb D; Macdougall A; Molotkova E; Monteiro Braga J; Russo C; Peter Schmidt W; Stewart J; Zambrana W; Zuin V; Nalá R; Cumming O; Brown J Effects of an Urban Sanitation Intervention on Childhood Enteric Infection and Diarrhoea in Mozambique. medRxiv 2020. 10.1101/2020.08.20.20178608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (51).Brown J; Cumming O; Bartram J; Cairncross S; Ensink J; Holcomb D; Knee J; Kolsky P; Liang K; Liang S; Nala R; Norman G; Rheingans R; Stewart J; Zavale O; Zuin V; Schmidt W-P A Controlled, before-and-after Trial of an Urban Sanitation Intervention to Reduce Enteric Infections in Children: Research Protocol for the Maputo Sanitation (MapSan) Study, Mozambique. BMJ Open 2015, 5 (6), e008215–e008215. 10.1136/bmjopen-2015-008215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (52).Augusto G; Nalá R; Casmo V; Sabonete A; Mapaco L; Monteiro J Geographic Distribution and Prevalence of Schistosomiasis and Soil-Transmitted Helminths among Schoolchildren in Mozambique. Am. J. Trop. Med. Hyg 2009, 81 (5), 799–803. 10.4269/ajtmh.2009.08-0344. [DOI] [PubMed] [Google Scholar]
- (53).Capone D; Adriano Z; Berendes D; Cumming O; Dreibelbis R; Holcomb DA; Knee J; Ross I; Brown J A Localized Sanitation Status Index as a Proxy for Fecal Contamination in Urban Maputo, Mozambique. PLoS One 2019, 14 (10), e0224333. 10.1371/journal.pone.0224333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (54).Vicente EM; Jermy CA; Schreiner HD Urban Geology of Maputo, Mocambique. In 10th Congress of the International Association for Engineering Geology and the Environment; London Geological Society: London, 2006. [Google Scholar]
- (55).Bition G; Harvey RW Transport of Pathogens through Soils and Aquifers. Environ. Microbiol 1992, 103–124. [Google Scholar]
- (56).Abu-Ashour J; Joy DM; Lee H; Whiteley HR; Zelin S Transport of Microorganisms through Soil. Water, Air, Soil Pollut. 1994, 75 (1–2), 141–158. 10.1007/BF01100406. [DOI] [Google Scholar]
- (57).Williams AR; Overbo A Unsafe Return of Human Excreta to the Environment: A Literature Review; 2015.
- (58).Knee JS Quantifying the Impact of an Urban Onsite Shared Sanitaiton Intervention on Child Health in Maputo, Mozambique: The MapSan Trial, Georgia Institute of Technology, 2019.
- (59).ASTM, D. 2216–98 Standard Test Method for Laboratory Determination of Water (Moisture) Content of Soil and Rock by Mass; 1998.
- (60).Aoyagi K; Livak KJ Methods Using Exogenous, Internal Controls and Analogue Blocks during Nucleic Acid Amplification. US5952202A, March 26, 1998. [Google Scholar]
- (61).Liu J; Gratz J; Amour C; Kibiki G; Becker S; Janaki L; Verweij JJ; Taniuchi M; Sobuz SU; Haque R; Haverstick DM; Houpt ER A Laboratory-Developed Taqman Array Card for Simultaneous Detection of 19 Enteropathogens. J. Clin. Microbiol 2013, 51 (2), 472–480. 10.1128/JCM.02658-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (62).Capone D; Berendes D; Cumming O; Knee J; Nalá R; Risk BB; Stauber C; Zhu K; Brown J Analysis of Fecal Sludges Reveals Common Enteric Pathogens in Urban Maputo, Mozambique. Environ. Sci. Technol. Lett 2020, acs.estlett.0c00610. 10.1021/acs.estlett.0c00610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (63).Kodani M; Winchell JM Engineered Combined-Positive-Control Template for Real-Time Reverse Transcription-PCR in Multiple-Pathogen-Detection Assays. J. Clin. Microbiol 2012, 50 (3), 1057–1060. 10.1128/JCM.05987-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (64).Capone D; Chigwechokha P; de los Reyes FL; Holm RH; Risk BB; Tilley E; Brown J Impact of Sampling Depth on Pathogen Detection in Pit Latrines. PLoS Negl. Trop. Dis 2021, 15 (3), e0009176. 10.1371/journal.pntd.0009176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (65).Wing C; Simon K; Bello-Gomez RA Designing Difference in Difference Studies: Best Practices for Public Health Policy Research. Annu. Rev. Public Health 2018, 39 (1), 453–469. 10.1146/annurev-publhealth-040617-013507. [DOI] [PubMed] [Google Scholar]
- (66).Halekoh U; Højsgaard S; Yan J The R Package Geepack for Generalized Estimating Equations. J. Stat. Softw 2006, 15 (2), 1–11. [Google Scholar]
- (67).Bottomley C; Kirby MJ; Lindsay SW; Alexander N Can the Buck Always Be Passed to the Highest Level of Clustering? BMC Med. Res. Methodol 2016, 16, 29. 10.1186/s12874-016-0127-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (68).Rose J; Jiménez-Cisneros B; Murphy H Persistence of Pathogens in Sewage and Other Water Types. In Global Water Pathogen Project; Michigan State University, 2019. 10.14321/waterpathogens.51. [DOI] [Google Scholar]
- (69).Schreiner M Simple Poverty Scorecard ® Poverty-Assessment Tool Mozambique; 2013.
- (70).Yaoyu F; Xiao L Zoonotic Potential and Molecular Epidemiology of Giardia Species and Giardiasis. Clin. Microbiol. Rev 2011, 24 (1), 110–140. 10.1128/CMR.00033-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (71).Izurieta R; Reina-Ortiz M; Ochoa-Capello T Trichuris Trichiura. In Global Water Pathogen Project; Michigan State University, 2019. 10.14321/waterpathogens.43. [DOI] [Google Scholar]
- (72).Kotloff KL; Riddle MS; Platts-Mills JA; Pavlinac P; Zaidi AKM Shigellosis. Lancet 2018, 391 (10122), 801–812. 10.1016/S0140-6736(17)33296-8. [DOI] [PubMed] [Google Scholar]
- (73).Water and Sanitation for the Urban Poor. An Integrated Approach to Peri-Urban Sanitation and Hygiene in Maputo: Working with City Authorities to Improve Services and Practices; Maputo, 2018. [Google Scholar]
- (74).Barreto ML; Genser B; Strina A; Teixeira MG; Assis AMO; Rego RF; Teles CA; Prado MS; Matos SMA; Alcântara-Neves NM; Cairncross S Impact of a Citywide Sanitation Program in Northeast Brazil on Intestinal Parasites Infection in Young Children. Environ. Health Perspect 2010, 118 (11), 1637–1642. 10.1289/ehp.1002058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (75).Barreto ML; Genser B; Strina A; Teixeira MG; Assis AMO; Rego RF; Teles CA; Prado MS; Matos SM; Santos DN; dos Santos LA; Cairncross S Effect of City-Wide Sanitation Programme on Reduction in Rate of Childhood Diarrhoea in Northeast Brazil: Assessment by Two Cohort Studies. Lancet 2007, 370 (9599), 1622–1628. 10.1016/S0140-6736(07)61638-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (76).Ercumen A; Mertens A; Arnold BF; Benjamin-chung J; Alan E; Ahmed MA; Kabir MH; Khalil MR; Rahman S; Parvez SM; Unicomb L; Ram P; Clasen TF; Luby SP; Colford JM Characterization of Natural and Affected Environments Effects of Single and Combined Water , Sanitation and Handwashing Interventions on Fecal Contamination in the Domestic Environment : A Cluster-Randomized Controlled Trial in Rural Bangladesh. Environ. Sci. Technol 2018. 10.1021/acs.est.8b05153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (77).Ercumen A; Pickering A; Kwong LH; Mertens A; Arnold BF; Benjamin- J; Hubbard AE; Alam M; Sen D; Islam S; Rahman M; Kullmann C; Chase C; Ahmed R; Parvez SM; Unicomb L; Rahman M; Ram P; Clasen TF; Luby SP; Colford JM Characterization of Natural and Affected Environments Do Sanitation Improvements Reduce Fecal Contamination of Water , Hands , Food , Soil and Flies ? Evidence from a Cluster-Randomized Controlled Trial in Rural Bangladesh. Environ. Sci. Technol 2018. 10.1021/acs.est.8b02988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (78).Holcomb DA; Knee J; Capone D; Sumner T; Adriano Z; Nalá R; Cumming O; Brown J; Stewart JR Bayesian Analysis of Source Tracking Markers to Estimate the Effects of an Urban Sanitation Intervention on Human Fecal Contamination in Mozambique. bioRxiv 2021, 2021.02.19.432000. 10.1101/2021.02.19.432000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (79).Canter L; Knox RC Evaluation of Septic Tank System Effects on Ground Water Quality; Norman, OK, 1984. [Google Scholar]
- (80).Orner K; Naughton C; Stenstrom T-A Pit Toilets (Latrines). In Water and Sanitation for the 21st Century: Health and Microbiological Aspects of Excreta and Wastewater Management (Global Water Pathogen Project); Mihelcic JR, Verbyla ME, Eds.; Michigan State University: Lansing, MI, 2018. 10.14321/waterpathogens.56. [DOI] [Google Scholar]
- (81).Ritter RL; Peprah D; Null C; Moe CL; Armah G; Ampofo J; Wellington N; Yakubu H; Robb K; Kirby AE; Wang Y; Roguski K; Reese H; Agbemabiese CA; Asantewa Lady; Adomako B; Freeman MC; Baker KK Within-Compound Versus Public Latrine Access and Child Feces Disposal Practices in Low-Income Neighborhoods of Accra, Ghana. Am. J. Trop. Med. Hyg 2018, 98 (5), 1250–1259. 10.4269/ajtmh.17-0654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (82).Lamar F; Freeman MC; Levy K Conceptualizing Chickflows in Maputo, Mozambique: High Risk Behaviors and Pathways for Childhood Exposure to Chicken Feces. In American Society of Tropical Medicine and Hygiene 2019; American Journal of Tropical Medicine and Hygiene: Mclean, VA, 2019; p 573. [Google Scholar]
- (83).Kwong LH; Ercumen A; Pickering AJ; Arsenault JE; Islam M; Parvez SM; Unicomb L; Rahman M; Davis J; Luby SP Ingestion of Fecal Bacteria along Multiple Pathways by Young Children in Rural Bangladesh Participating in a Cluster-Randomized Trial of Water, Sanitation, and Hygiene Interventions (WASH Benefits). Environ. Sci. Technol 2020, 54 (21), 13828–13838. 10.1021/acs.est.0c02606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (84).Arnold BF; Null C; Luby SP; Colford JM Implications of WASH Benefits Trials for Water and Sanitation – Authors’ Reply. Lancet Glob. Heal 2018, 6 (6), e616–e617. 10.1016/S2214-109X(18)30229-8. [DOI] [PubMed] [Google Scholar]
- (85).Liu J; Gratz J; Amour C; Nshama R; Walongo T; Maro A; Mduma E; Platts-Mills J; Boisen N; Nataro J; Haverstick DM; Kabir F; Lertsethtakarn P; Silapong S; Jeamwattanalert P; Bodhidatta L; Mason C; Begum S; Haque R; Praharaj I; Kang G; Houpt ER Optimization of Quantitative PCR Methods for Enteropathogen Detection. PLoS One 2016, 11 (6), e0158199. 10.1371/journal.pone.0158199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (86).Lappan R; Henry R; Chown SL; Luby SP; Higginson EE; Bata L; Jirapanjawat T; Schang C; Openshaw JJ; O’Toole J; Lin A; Tela A; Turagabeci A; Wong THF; French MA; Brown RR; Leder K; Greening C; McCarthy D TaqMan Array Cards Enable Monitoring of Diverse Enteric Pathogens across Environmental and Host Reservoirs. bioRxiv 2020, 2020.10.27.356642. 10.1101/2020.10.27.356642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (87).Schrader C; Schielke A; Ellerbroek L; Johne R PCR Inhibitors - Occurrence, Properties and Removal. J. Appl. Microbiol 2012, 113 (5), 1014–1026. 10.1111/j.1365-2672.2012.05384.x. [DOI] [PubMed] [Google Scholar]
- (88).Cutler D; Miller G The Role of Public Health Improvements in Health Advances: The 20th Century United States; Cambridge, MA, 2004. 10.3386/w10511. [DOI] [PubMed] [Google Scholar]
- (89).Dodane PH; Mbéguéré M; Sow O; Strande L Capital and Operating Costs of Full-Scale Fecal Sludge Management and Wastewater Treatment Systems in Dakar, Senegal. Environ. Sci. Technol 2012, 46 (7), 3705–3711. 10.1021/es2045234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (90).Mafuta C; Formo RK; Nellemann C; Li F Green Hills, Blue Cities: An Ecosystems Approach to Water Resources Management for African Cities; United Nations Environment Programme, GRID-Arendal, 2011. [Google Scholar]
- (91).Cumming O; Arnold BF; Ban R; Clasen T; Esteves Mills J; Freeman MC; Gordon B; Guiteras R; Howard G; Hunter PR; Johnston RB; Pickering AJ; Prendergast AJ; Prüss-Ustün A; Rosenboom JW; Spears D; Sundberg S; Wolf J; Null C; Luby SP; Humphrey JH; Colford JM The Implications of Three Major New Trials for the Effect of Water, Sanitation and Hygiene on Childhood Diarrhea and Stunting: A Consensus Statement. BMC Med. 2019, 17 (1), 173. 10.1186/s12916-019-1410-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (92).Un-Habitat. The Challenge of Slums - Global Report on Human Settlements; 2003. 10.1108/meq.2004.15.3.337.3. [DOI]
- (93).Ngure FM; Reid BM; Humphrey JH; Mbuya MN; Pelto G; Stoltzfus RJ Water, Sanitation, and Hygiene (WASH), Environmental Enteropathy, Nutrition, and Early Child Development: Making the Links. Ann. N. Y. Acad. Sci 2014, 1308 (1), 118–128. 10.1111/nyas.12330. [DOI] [PubMed] [Google Scholar]
- (94).Titiunik R; Martinez S; Gertler PJ; Galiano S; Cattaneo MD Housing, Health, And Happiness; Policy Research Working Papers; The World Bank, 2007. 10.1596/1813-9450-4214. [DOI] [Google Scholar]
- (95).Kolsky P Performance-Based Evaluation of Surface Water Drainage for Low Income Communities: A Case Study in Indore, Madhya Pradesh, London School of Hygiene and Tropical Medicine, 1999. 10.13140/2.1.1136.6721. [DOI]
- (96).Voth-Gaeddert LE; Divelbiss DW; Oerther DB Utilizing Structural Equation Modeling to Correlate Biosand Filter Performance and Occurrence of Diarrhea in the Village of Enseado Do Aritapera in Para, Brazil. Water Supply 2015, 15 (1), 164–172. 10.2166/ws.2014.101. [DOI] [Google Scholar]
- (97).Peal A; Evans B; Blackett I; Hawkins P; Heymans C A Review of Fecal Sludge Management in 12 Cities. Water Sanit. Progr 2015, No. June, 563. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Text S1. Compound enrollment at baseline
Text S2. Test for Matrix Inhibition
Text S3. Custom TaqMan Array Card (TAC)
Table S1. Assays used on the custom TAC
Table S2. Interpretation of gene targets on the TAC
Table S3. Standard curve
Table S4. Description of variables and their respective sources
Table S5. Soils samples matched at baseline and 24-month trial periods
Figure S1. Histogram of dates that latrine entrance soils were collected
Table S6. Mean Cq Values
Table S7. Child feces disposal at 24-month phase


