Abstract
The purpose of this study was to examine patterns of COVID-19 vaccination in Israel and how these relate to different proposals made about benefits for those vaccinated, and to present the legal and ethical dilemmas surrounding these issues.
A retrospective study of COVID-19 vaccination rates in Israel was conducted, with data obtained from the Ministry of Health (MOH). Information on benefits proposed or offered for vaccination and restrictions for non-vaccination were obtained from the MOH and presented in a timeline.
By March 1st, 51% of the total population, and 91% of those aged 60 and over, had received their first COVID-19 vaccine. Exemption from quarantine was granted to vaccinated or recovered people from 17th January 2021. The ‘green pass’ incentive scheme, granting access to social, cultural and sporting events for those fully vaccinated or immune, was proposed in December 2020, and came into effect on February 21st 2021.
Incentive schemes which impose limitations on those who choose not to vaccinate may motivate some people to take action. Policymakers should use a measured approach to protect public health, with minimum infringement on citizens' rights. Providing transparent and culturally appropriate information on immunization and ensuring maximal and equitable access to COVID-19 vaccines may help build trust.
Keywords: COVID-19 vaccine, Incentives, Penalties
1. Background
Vaccine hesitancy was identified in recent years by the World Health Organization (WHO) as one of the top ten threats to public health (WHO, 2019). Now, in the wake of the COVID-19 pandemic, the issue has become even more salient, with several vaccines now available, yet with many concerns and much hesitancy surrounding this new disease and new technology.
The first two COVID-19 vaccines BNT162b2 and mRNA-1273 were authorized in an emergency approval process by the American Food and Drug Administration (FDA) in December 2020 (Moderna COVID-19 Vaccine, 2021; Pfizer-BioNTech COVID-19 Vaccine, 2021), twelve months after the first COVID-19 cases were identified in China and 9 months after the WHO declared a pandemic, resulting in over 130 million confirmed cases and 2.5 million deaths so far (COVID-19 Map - Johns Hopkins Coronavirus Resource Center, 2020). Although the approval of vaccines with high efficacy and safety was accepted around the globe as a “miracle bullet”, the voices of vaccine opponents and sceptics rose concomitantly.
A representative survey found that COVID-19 vaccine hesitancy or resistance ranged from 31% in England to 35% in Ireland (Murphy et al., 2021). In the United Kingdom (UK), 25% reported vaccine hesitancy while 6% reported vaccine resistance (Murphy et al., 2021). A study in Jordan, Kuwait and Saudi Arabia also found high rates of COVID vaccine hesitancy (Sallam et al., 2021).
Governments aim to achieve as high a proportion of their population vaccinated against COVID-19 in the shortest time possible, in order to reduce morbidity and mortality, reduce burden on hospitals, and remove restrictions, having witnessed the devastating health, economic and social effects of the pandemic (Amit et al., 2021).
Incentives have been used previously in an attempt to encourage people to vaccinate against other diseases. Most previous research on incentives for vaccination have concerned childhood vaccines. Some countries have implemented reward schemes, while others applied penalties for non-vaccination.
Since 1998 the Australian government, in a bid to improve vaccination rates, made certain childcare payments and benefits dependent on children being vaccinated according to schedule (‘no jab no pay’ policy). In 2015, the exemption for conscientious objection was revoked. This has contributed to high vaccination rates (‘No Jab No Pay’ and other immunisation measures – Parliament of Australia, 2021). A review conducted in Australia which looked at both financial and non-financial incentives found both to be effective in raising child immunization rates (Achat et al., 1999). However a more recent study showed that while it encouraged some parents to vaccinate on time, the policy did not change the position of those opposed to immunization (Australia's “no jab, no pay” rule has little effect on anti-vaxxer parents – study, 2021).
The U.S. Department of Health and Human Services' Healthy People 2020 programme, which provides evidence-based resources for health promotion, recommended client or family incentive rewards for vaccination, including financial or other incentives, such as food vouchers or baby products. This was based on recommendations from the Community Preventive Services Task Force which found sufficient evidence of effectiveness in raising vaccination rates, based on 7 studies (Increasing Appropriate Vaccination, 2021; Vaccination Programs, 2021).
In Singapore a study offered monetary incentives to encourage adult vaccination against influenza and found this could boost vaccination rates, though in a limited sample (Yue et al., 2020). A review of methods to increase flu vaccination among health workers included 46 studies and found mandatory vaccination to be most effective, while incentives did not make a significant difference in vaccination rates (Lytras et al., 2016).
The case of COVID-19 vaccination differs from other established vaccines: First, during the study period, COVID-19 vaccines were recommended only in adults aged 16 plus so cannot benefit from the lessons accumulated in childhood immunization schemes. Second, and no less important, COVID-19 vaccines have been developed in a rapid international effort, with less than one year from start to conditional market authorization, raising concerns about this fast-tracked development process in comparison to other vaccines which traditionally take years to come to market (Lefebvre et al., 2021).
Furthermore, the COVID-19 vaccine makes use of novel messenger RNA (m-RNA) technology, the first of its kind to be approved (Lefebvre et al., 2021).
These two unique characteristics fuel concerns that are superimposed on long standing vaccine resistance movements. Social media is another factor that facilitates the rapid spread of anti-establishment and conspiracy theories. Indeed, organized anti-vaccination groups that often have a strong presence on social media have contributed to the drop in vaccination compliance and anxieties concerning vaccination (Evrony and Caplan, 2017).
Though incentives may increase vaccination rates somewhat, they may not be sufficient to overcome health concerns or doubts regarding efficiency in this novel vaccine, especially in light of strong social media presence of anti-vaccine movements.
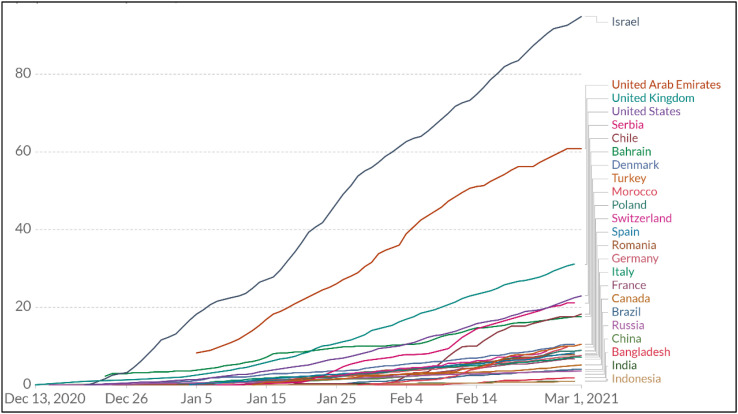
The debate over COVID-19 vaccination has wakened many ethical and legal issues that come into play with regard to possible incentives and restrictions linked to non-vaccination. Israel, with the highest coverage of its total population in the first two months of the vaccination drive (Rosen et al., 2021), could be an “early adopter laboratory” to examine these issues.
Vaccination in Israel began on the 20th December 2020 with the Pfizer BioNTech COVID-19 vaccine, given in two doses with a three-week interval. Since Israel was among the first nations to start a widely implemented operation, aimed at gradually reaching all citizens aged 16 years and over, the follow-up of the evolution of incentives and penalties around vaccination are relatively more well-defined. They center around free access to social, sports and cultural activities and events, a novel strategy not used before in vaccine drives.
The aims of the study were 1) to examine patterns of COVID vaccination in Israel and how these relate to different proposals and statements made about benefits for those vaccinated and 2) to present the legal and ethical dilemmas around these issues.
2. Methods
A retrospective study of COVID-19 vaccinations in Israel was conducted from 20/12/20 (date of the first vaccination in Israel) up to 01/03/21.
Details on the rate of vaccination in Israeli were obtained from the Ministry of Health (MOH) database website – Israel COVID-19 Data Tracker”, with the total Israeli population (not including the Palestinian Authority) of 9.291 million used as denominator for the calculation of rates (COVID dashboard, 2021). These data were collated and presented in graph form, detailing numbers of people receiving the first and second vaccine doses by date, between 20/12/20–01/3/21.
Details on the rate of vaccination in the Israeli population and worldwide were obtained from the Our World in Data database (Coronavirus (COVID-19) Vaccinations, 2021).
Information on benefits proposed or offered for vaccination and restrictions for non-vaccination were obtained from the MOH website (https://www.gov.il/he/departments/topics/corona-main-sub, n.d.). Data were collated including the nature of the incentive or penalty, source and whether it was implemented and on which date, and presented in table format.
3. Results
By March 1, 2021, 4.78 million Israelis (51% of the total 9.3 million population, and 92% of those aged 60+) had received their first dose of the vaccine, and 3.45 million (37% of total population) had received the second vaccine dose, leading the global vaccine effort in vaccines per population. Vaccination rates were also fairly high in younger age groups, including 83% of 50–59 year olds, 77% of 40–49 year olds, 71% age 30–39, 64% age 20–29, and 18% of 10–19 year olds having received their first dose during this period. Fig. 1 presents the rate of vaccination per 100 of the population with the COVID-19 vaccine in Israel and around the world.
Fig. 1.
Rate of vaccination per 100 population with the first dose of COVID-19 vaccine in Israel and around the world.
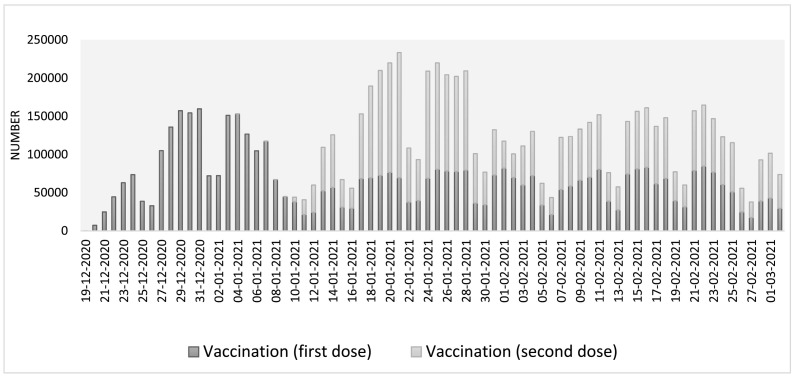
Vaccination was rolled out in Israel in stages according to age groups. The first priority groups from 20th December included medical staff, people aged 60 and over, and risk groups (patients with lung disease, diabetes, immunodeficiency). At the beginning of the vaccination drive, the Prime Minster, President, Minister of Health and other senior officials publicly received their vaccinations. This was followed by eligibility for age 50+ from the 13th January, pregnant women and age 40+ from 19th January, age 35+ from 20th January, and age 16–18 from the 22nd January. On 4th February, vaccination was opened up to all eligible (16+) age groups. Fig. 2 presents the vaccination drive rollout, showing the daily number of people receiving their first and second doses, with numbers peaking in late December and early January for the first dose, and in later January for the second dose.
Fig. 2.
Daily numbers of people receiving the first and second vaccine doses. Israel, December 19, 2020 to March 1, 2021.
Table 1 presents, in a timely order, various statements that were made by the government on benefits and incentives that would be given for vaccination within the ‘Green pass’ program, and restrictions that would limit entrance to certain social, sports and cultural activities for non-vaccinated people as well as proposed legislation. It also presents the date when the relevant regulations and legislation came into effect. The most prominent dates were the 17th January when exemption from quarantine for vaccinated persons who were in contact with an infected person or returned from travel abroad was officially declared; and the 21st of February when the ‘Green pass’ was officially implemented. After the 17th January there was a peak in second dose vaccinations, rising to over 200,000 per day. High vaccination rates continued following the highest daily number of new confirmed cases since the pandemic began (10,117 cases or 1088 cases per million population on 18th January) and highest fatality rate was reported on 24th January (https://datadashboard.health.gov.il/COVID-19/general, n.d.).
Table 1.
Benefits and restrictions for vaccination and non-vaccination.
| Date | Proposal | Incentive | Legislation/restriction/penalty | Source | Implementation |
|---|---|---|---|---|---|
| 10.12.20 | Corona vaccination law | Law that would mandate compulsory vaccination for all citizens and compensate anyone harmed by the vaccine, aiming to state a clear position and create norms regarding the importance of vaccination. | https://finance.walla.co.il/item/3404183 | Not passeda | |
| 14.12.20 | Green passport | Opening of the economy including social, sports and cultural events to those who are immune. Exemption from quarantine after exposure to a confirmed case or when returning from abroad. |
https://www.news1.co.il/Archive/001-D-434692-00.html | 21.2.21 | |
| 17.12.20 | Exemption from quarantine and from airport tests | Vaccinated people and those recovered from COVID will be eligible for benefits which will be piloted in January allowing entrance to tourist sites, Exemption from quarantine and exemption from testing before travelling abroad. |
https://www.gov.il/he/departments/general/corona-recovered-patients | ||
| 4.1.21 | Green passport | Ministry of Health launched a green passport app, which would allow entrance to sports and cultural activities. Still under discussion restaurants and cafes, malls, hotels, gyms and swimming pools. Vaccination certificate valid from the 2nd dose for 6 months gives exemption from quarantine. |
https://www.haaretz.co.il/health/corona/.premium-1.9422299 | ||
| 17.1.21 | Exemption from quarantine | Official exemption from quarantine for those with vaccination certificate. | https://www.calcalist.co.il/local/articles/0,7340,L-3888290,00.Html | 17.1.21 | |
| 24.1.21 | Travel restrictionsb | Ben Gurion airport closed for incoming and outward flights. Few exceptions defined (i.e. humanitarian reasons) | https://www.calcalist.co.il/local/articles/0,7340,L-3889350,00.Html | ||
| 10.2.21 | Green pass | Statement by minister of health, vaccinated and recovered individuals will be entitled to the green pass, granting entrance to certain entertainment venues and cultural events, including shows, cinemas, gyms and restaurants. | Proposal of law that would allow employers to prevent unvaccinated employees from coming to work | https://www.themarker.com/news/health/.premium-1.9527932 | 21.2.21 |
| 15.2.21 | Green pass due to come into effect 23/2/21 | Statement by prime minister: All those vaccinated with two doses or recovered, will be allowed entrance to gyms, cultural and sporting events, exhibitions, places of worship, hotels and swimming pools from 21/2/21. Entrance with the green pass to restaurants, wedding halls from the 7/3/21. | Ministry of Health expected to discuss penalties and fines for people entering certain venues without a vaccination certificate. Proposal to make forgery of vaccination certificate a criminal offence. | https://www.gov.il/he/departments/news/spoke_joint_statement150221 | 21.2.21 |
| 24.02.21 | Bill passed allowing passing details of non-vaccinated to local authorities and the Ministry of Educationc | https://www.calcalist.co.il/local/articles/0,7340,L-3895340,00.html | Passed |
Hadassah hospital was the first to inform employees that those eligible but refusing to vaccinate would be put on unpaid leave.
Highest fatality rate in Israel since start of pandemic.
Identifying information and contact details will serve local authorities to target efforts to increase vaccination; information on educational staff will be passed to the Ministry of Education to encourage staff to receive the vaccine doses.
4. Discussion
Israel has been a leader in COVID-19 vaccination achieving a very high rate per population in a short period of time, due to both a sufficient supply of vaccines, and to efficient rollout through the four Health Maintenance Organizations, as well as hospitals and the Israeli Red Cross. Ahead of most other countries, Israel achieved vaccination of 50% of the population, and 90% of those aged over 60, within the first two months.
The Israeli government decided to use incentives and restrictions with the aim of increasing vaccination rates, especially in younger age groups, allowing reduced health burden, re-opening of the economy, and going some way toward reaching herd immunity. Prior to implementation of the ‘Green pass’, the Ministry of Health released a series of announcements heralding its forthcoming incentive scheme for vaccinated and recovered individuals. Following months of restrictions and lockdowns, and even in the absence of definitive details on what exactly the incentive would entail, there was great interest in the coming green pass.
While we cannot surmise a causal relationship, patterns of vaccination seem to be somewhat influenced by announcements on exemption from quarantine (a “pure” incentive”) and on the ‘Green pass’ (both an incentive for those who hold the pass and a penalty for those who are not eligible to hold it). It is reasonable to assume that some people were motivated to vaccinate based on the promise of benefits and access to social and cultural events as well as sports and entertainment venues. These incentives are likely to have more of an impact on the younger population, who may need more reasons to get vaccinated, since they are at lower risk. Changes in infection and fatality rates likely also had an impact on vaccination uptake and we cannot isolate the impact of either of these influences.
Survey data shows that not all people will be persuaded by incentives to get vaccinated, for example a survey conducted in Israel found that among 500 respondents, 21% reported not intending to vaccinate, and of these 31% said the offer of a green pass would possibly or definitely convince them, while 46% said it would not (N12 news and Midgam, 2021). Further surveys may be used to assess people's reasons for vaccinating and whether the incentive scheme had the desired effect.
Penalties are less commonly used to boost vaccination rates, though punitive measures were used to halt measles outbreaks in Europe. A 2019 paper examining vaccine policies including those that require vaccination for the provision of social goods, argued that, “It is reasonable to restrict access to public institutions (e.g. schools) with appropriate recourse for medical, philosophical and religious exemptions in contexts where vaccination coverage is low and outbreaks likely,” (Chantler et al., 2019) but that these must go hand in hand with strategies to improve trust.
4.1. Issues of trust
Trust in the vaccine is influenced by many factors, including social norms and acceptance of the vaccine among peers, trust in governmental policymakers, and in the medical/pharmaceutical industries (Latkin et al., 2021). A US study found demographic differences, with men having higher trust in the vaccine, while minority groups demonstrated lower trust (Latkin et al., 2021). Furthermore individuals who had greater trust in the information received about COVID-19 from the health department and government institutions were more likely to have higher trust in the vaccine. A high rate of distrust has been found in regard to the new COVID-19 vaccines, and it has been suggested that role-modelling by public officials and targeted public education could help build trust (Vergara and Sarmiento JDNL, 2021). Indeed in Israel, the public vaccination of senior government officials was intended to convey a message and set an example to the public.
4.2. Issues of equality
Certain communities may already have lower trust in government institutions, including minority groups, which may translate into lower uptake of vaccines. Indeed, data have shown lower uptake among the Arab minority population and in the ultra-Orthodox sector. A recently published analysis of the nationwide public data from the first 12 months of the pandemic in Israel (March 2020 to February 2021) and the first 3 months of the vaccine drive demonstrated that the risk of SARS-CoV-2 infection was higher in towns with predominantly Arab and ultra-Orthodox Jewish populations than in the general Jewish population, and in low socioeconomic status (SES) communities. COVID-19 mortality rate was highest among Arabs. Conversely, vaccine uptake was lower among Arab and ultra-Orthodox Jewish populations and low SES communities (Muhsen et al., 2021). The authors emphasize that “these inequalities were evident even in settings with universal health insurance and high accessibility to healthcare, including COVID-19 diagnostics, treatment and immunization, like Israel” (Muhsen et al., 2021).
4.3. Reaching the reluctant
The WHO recently published guidelines for developing a proactive COVID vaccination strategy, which includes behavior change planning, audience targeting, analysis of barriers, mobilization, building vaccine demand, community engagement, access to vaccines, marketing strategy, media outreach and digital media strategy, which when combined are likely to lead to a more effective vaccination campaign (French et al., 2020). It is important to identify which groups are reticent to vaccinate, and examine their reasons. Fournet et al (Fournet et al., 2018) described four types of non-vaccinators: ‘The hesitant’–who have concerns about perceived safety issues and are unsure about needs, procedures and timings for immunizing; ‘The unconcerned’–who consider immunization a low priority and see no real perceived risk of vaccine-preventable diseases – this group may be persuaded by incentives; ‘The poorly reached’–who have limited or difficult access to services, related to social exclusion, poverty, unique cultural or religious background or campaigns that are not culturally appropriate, and, in the case of more integrated and affluent populations, factors related to convenience – outreach and improved access and cultural targeting could help reach this group; ‘The active resisters’–for whom personal, cultural, or religious beliefs discourage them from vaccinating. Incentives may help convince some groups (for example the unconcerned, the poorly reached) but likely not those who are opposed in principle. For other groups we need to listen to and address people's concerns.
Beyond individuals' motivation to vaccinate lie factors of access to the vaccine and practical/logistic issues. In Israel, access has been broader and quicker than in many other countries, indeed many countries still do not have sufficient access to the vaccine.
4.4. Legal and ethical aspects
There has been much criticism of the policy of excluding non-vaccinated people from certain venues and events –an appeal was already submitted to the supreme court on this issue in Israel. Several legal and ethical issues are raised by this strategy.
The green pass system provides external motivation (as opposed to internal motivation for vaccination) which rewards a desired behavior, and penalizes undesirable behavior (non-vaccination). While intrinsic motivation is considered a stronger motivator of behavior, particularly when it requires long-term maintenance such as smoking cessation or weight loss (Curry et al., 1997), external incentives can boost motivation and may be effective for one-off behaviors like vaccination (Leahey et al., 2017). The incentive system is intended to speed up the vaccination process and thus facilitate a quicker recovery of the economy and improve population health. While vaccinated individuals will enjoy unlimited access to entertainment venues, as well as certain holiday destinations (termed ‘green islands’), the non-vaccinated will face restrictions. Those with a green pass will also benefit from exemption from 14-day quarantine following contact with a confirmed COVID-19 case.
The use of incentives to encourage desirable behavior is legitimate, and some would say essential in order to protect public health in the case of the COVID-19 vaccine against a highly infectious disease. Some would consider it the state's duty to do all it can to encourage vaccination in order to protect the health and lives of its citizens (Enoch et al., 2021).
While laws and regulations devised during the pandemic (including but not limited to the green pass) were made to protect the health of all citizens, their implementation may sometimes infringe upon human rights, for example freedom of movement, freedom to gather, and with regard to vaccination – the right to autonomy over one's body.
In Israel the sanctity of life is one of the founding principles anchored in the law of human dignity and liberty (Shultziner, 2006). This includes the right to autonomy over one's body and to make autonomous decisions. This principle is protected by constitutional law, and includes the right to choose whether to vaccinate (for COVID or any other disease) without coercion or manipulation. Since the “green pass” regulation involves a penalty (negative) versus a benefit (positive), the tendency is to see this as a violation of the individual's autonomy. A purely positive incentive would not be considered an infringement on autonomy, but once sanctions are imposed on one group (the non-vaccinated) involving removing some of their rights (eg. Free movement, freedom to work), this could lead someone to feel they have no option but to take the vaccine – which would be an attack on rights. However, rights do not exist in a vacuum and must be considered in light of conflicting interests.
According to the Israeli fundamental law on “Human Dignity and Liberty” (Basic Law, 2021), clause 8, four conditions must be met to prevent the unconstitutionality of a law that is alleged to be a violation: 1) The violation was committed by law or by virtue of an explicit authorization; 2) the law is in line with the principles of the state; 3) the law is for a worthy purpose; 4) proportional harm (and no more than absolutely necessary) (Barak, 2014).
A law whose purpose is to protect the public interest (in this case its health) could be considered a worthy purpose, in addition to getting the pandemic under control, preventing further lockdowns etc. If so, it would still need to meet the other three conditions including proportionality. While the non-eligible population are physically restricted from some places, they have access to alternatives, such as online shopping, or they have the option of presenting a negative COVID test to gain access.
5. Policy implications
Israel has already achieved relatively high COVID-19 vaccination rates in a short period of time. However, vaccination rates are slowing and in order to reach herd immunity, new strategies may be required. If the state decides to use drastic means, which may be justified in order to protect public health and for the common good, it must do so with the minimum of infringement on citizens' rights, while balancing conflicting interests and maintaining proportionality. Furthermore, research has shown that the use of rewards and penalties may displace other motivations for desirable behavior, such as altruism or civic duty. Policymakers may consider whether reinforcing mutual social responsibility may raise intrinsic motivation to vaccinate, alongside external incentives (Underhill, 2011).
Individuals must be allowed to voice their concerns, and clear culturally appropriate information should be readily available, regarding immunization, and the relative risks of adverse vaccine effects and of COVID-19, to help people make an informed decision. Full and equitable access to vaccination must also be ensured to underpin the incentives scheme.
Governments implementing incentive schemes have to deliver on the promise of benefits to those vaccinated, which may further encourage an increase in vaccination rates of those who have yet to take the plunge. If the benefits do not materialize, already low public trust in governmental bodies during handling of the pandemic may be further eroded.
Current data do not allow analysis of causal relations between incentives and their effect on vaccination rate and pace. Since implementation of measures to increase population vaccination during a pandemic could not be managed as a randomized controlled trial, other research methodologies like surveys performed close to uptake of vaccines by a large population sample could shed light on the effects of incentives on the decision to vaccinate. Qualitative research should be designed to better understand the challenges and barriers to vaccination among those populations who need it most and the impact of incentives and penalties. This is important to minimize the impact of future health crises on widening existing gaps in health.
Some countries which have achieved high rates of vaccination, and a consequent sharp drop in COVID-19 infection numbers, have been able to remove restrictions (and equally limitations on the non-vaccinated). Various strategies employed, including incentives, could be a useful short-term measure, a means to an end, which ultimately benefits the whole population.
Data access and integrity
The authors declares that they had full access to all of the data in this study and the authors takes complete responsibility for the integrity of the data and the accuracy of the data analysis.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgement
None.
References
- ‘No Jab No Pay’ and other immunisation measures – Parliament of Australia 2021. https://www.aph.gov.au/about_parliament/parliamentary_departments/parliamentary_library/pubs/rp/budgetreview201516/vaccination Published 2021. Accessed February 21.
- Achat H., McIntyre P., Burgess M. Health care incentives in immunisation. Aust. N. Z. J. Public Health. 1999;23(3):285–288. doi: 10.1111/j.1467-842X.1999.tb01257.x. [DOI] [PubMed] [Google Scholar]
- Amit S., Regev-Yochay G., Afek A., Kreiss Y., Leshem E. Early rate reductions of SARS-CoV-2 infection and COVID-19 in BNT162b2 vaccine recipients. Lancet. 2021;0(0) doi: 10.1016/S0140-6736(21)00448-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Australia'’s “no jab, no pay” rule has little effect on anti-vaxxer parents – study Australia News|The Guardian. 2021. https://www.theguardian.com/australia-news/2020/oct/05/australias-no-jab-no-pay-rule-has-little-effect-on-anti-vaxxer-parents-study Published 2020. Accessed February 21.
- Barak A. 2014. Human Dignity: Constitutional Rights. [Google Scholar]
- Basic Law Human Dignity and Liberty. 2021. https://www.knesset.gov.il/laws/special/eng/basic3_eng.htm Published 1992. Accessed March 4.
- Chantler T., Karafillakis E., Wilson J. Vaccination: is there a place for penalties for non-compliance? Appl. Heal. Econ. Heal. Pol. 2019;17(3):265. doi: 10.1007/s40258-019-00460-z. [DOI] [PubMed] [Google Scholar]
- Coronavirus (COVID-19) Vaccinations Statistics and Research - Our World in Data. 2021. https://ourworldindata.org/covid-vaccinations Accessed February 26.
- COVID dashboard 2021. https://datadashboard.health.gov.il/COVID-19/general?utm_source=go.gov.il&utm_medium=referral
- COVID-19 Map - Johns Hopkins Coronavirus Resource Center 2020. https://coronavirus.jhu.edu/map.html Published 2020. Accessed August 30.
- Curry S.J., Grothaus L., McBride C. Reasons for quitting: intrinsic and extrinsic motivation for smoking cessation in a population-based sample of smokers. Addict. Behav. 1997;22(6):727–739. doi: 10.1016/S0306-4603(97)00059-2. [DOI] [PubMed] [Google Scholar]
- Enoch D., Barak Koren N., Shor Ofri M., Had D.M.O. 2021. A Position Paper: Vaccines, Conditions and Cost-Bearing. Jerusalem. [Google Scholar]
- Evrony A., Caplan A. The overlooked dangers of anti-vaccination groups’ social media presence. Hum. Vacc. Immunother. 2017;13(6):1475–1476. doi: 10.1080/21645515.2017.1283467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fournet N., Mollema L., Ruijs W.L., et al. Under-vaccinated groups in Europe and their beliefs, attitudes and reasons for non-vaccination; two systematic reviews. BMC Public Health. 2018;18:196. doi: 10.1186/s12889-018-5103-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French J., Deshpande S., Evans W., Obregon R. Key guidelines in developing a pre-emptive COVID-19 vaccination uptake promotion strategy. Int. J. Environ. Res. Public Health. 2020;17:5893. doi: 10.3390/ijerph17165893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- https://datadashboard.health.gov.il/COVID-19/general
- https://www.gov.il/he/departments/topics/corona-main-sub
- Increasing Appropriate Vaccination Client or Family Incentive Rewards. Community Preventive Services Task. 2021. https://www.thecommunityguide.org/sites/default/files/assets/Vaccination-Incentive-Rewards.pdf Published 2015. Accessed February 21.
- Latkin C.A., Dayton L., Yi G., Konstantopoulos A., Boodramd B. Trust in a COVID-19 vaccine in the U.S.: a social-ecological perspective. Soc. Sci. Med. 2021;270:113684. doi: 10.1016/j.socscimed.2021.113684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leahey T.M., LaRose J.G., Lanoye A., Fava J.L., Wing R.R. Secondary data analysis from a randomized trial examining the effects of small financial incentives on intrinsic and extrinsic motivation for weight loss. Heal. Psychol. Behav. Med. 2017;5(1):129–144. doi: 10.1080/21642850.2016.1276460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lefebvre M., Vignier N., Pitard B., Botelho-Nevers E., Cohen R., Epaulard O. Covid-19 vaccines: frequently asked questions and updated answers. Infect. Dis. Now. February 2021 doi: 10.1016/j.idnow.2021.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lytras T., Kopsachilis F., Mouratidou E., Papamichail D., Bonovas S. Interventions to increase seasonal influenza vaccine coverage in healthcare workers: a systematic review and meta-regression analysis. Hum. Vacc. Immunother. 2016;12(3):671–681. doi: 10.1080/21645515.2015.1106656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moderna COVID-19 Vaccine FDA. 2021. https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/moderna-covid-19-vaccine Published 2021. Accessed February 21.
- Muhsen K., Na’aminh W., Lapidot Y. A nationwide analysis of population group differences in the COVID-19 epidemic in Israel, February 2020–February 2021. Lancet Reg. 2021;7:100–130. doi: 10.1016/j.lanepe.2021.100130. https://www.sciencedirect.com/science/article/pii/S2666776221001071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy J., Vallières F., Bentall R.P., et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat. Commun. 2021;12(1):1–15. doi: 10.1038/s41467-020-20226-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- N12 news and Midgam . 2021. COVID-19 Vaccine hesitancy in Israel. [Google Scholar]
- Pfizer-BioNTech COVID-19 Vaccine FDA. 2021. https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/pfizer-biontech-covid-19-vaccine Published 2021. Accessed February 21.
- Rosen B., Waitzberg R., Israeli A. Israel’s rapid rollout of vaccinations for COVID-19. Isr. J. Health Policy Res. 2021;10(1) doi: 10.1186/s13584-021-00440-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallam M., Dababseh D., Eid H., et al. High rates of covid-19 vaccine hesitancy and its association with conspiracy beliefs: a study in Jordan and Kuwait among other Arab countries. Vaccines. 2021;9(1):1–16. doi: 10.3390/vaccines9010042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shultziner D. A Jewish conception of human dignity. J. Relig Ethics. 2006;34(4):663–683. doi: 10.1111/j.1467-9795.2006.00289.x. [DOI] [Google Scholar]
- Underhill K. When Extrinsic Incentives Displace Intrinsic Motivation: Designing Legal Carrots and Sticks to Confront the Challenge of Motivational Crowding-Out. 2011. https://heinonline.org/hol-cgi-bin/get_pdf.cgi?handle=hein.journals/yjor33§ion=8 Accessed March 4, 2021.
- Vaccination Programs . Healthy People.gov; 2021. Client or Family Incentive Rewards|Healthy People 2020.https://www.healthypeople.gov/2020/tools-resources/evidence-based-resource/vaccination-programs-client-or-family-incentive-rewards Published 2015. Accessed February 21. [Google Scholar]
- Vergara Raymond John D., Sarmiento JDNL Philip Joseph D. Building public trust: a response to COVID-19 vaccine hesitancy predicament. J. Public Health. 2021 doi: 10.1093/pubmed/fdaa282. (fdaa282) [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2019. Top Ten Threats to Global Health. [Google Scholar]
- Yue M., Wang Y., Low C.K., Yin Yoong J.S., Cook A.R. Optimal design of population-level financial incentives of influenza vaccination for the elderly. Value Health. 2020;23(2):200–208. doi: 10.1016/j.jval.2019.08.006. [DOI] [PubMed] [Google Scholar]