Objective
Pregnant and lactating women were excluded from the initial clinical trials in which the safety and efficacy of the BNT162b2 messenger RNA vaccine were evaluated. Consequently, recommendations regarding vaccination of pregnant and lactating women were equivocal.1 Therefore, our aim was to assess whether SARS-CoV-2 immunoglobulins (Igs) can be detected in breastmilk samples of lactating women following SARS-CoV-2 vaccination and whether it can be detected in the serum and oral mucosal secretions of their breastfed infants.
Study Design
This was a longitudinal cohort study, conducted between December 2020 and April 2021. Samples were collected from lactating women who were vaccinated against COVID-19 after delivery and their breastfed infants. Blood samples and breastmilk were obtained from all study participants, and dried blood spot (DBS) samples from breastfed infants were collected on Guthrie cards. In addition, the saliva of infants was collected from oral mucosa immediately after breastfeeding and at 30, 90, and 150 minutes after breastfeeding. All serum samples were tested for the presence of SARS-CoV-2 IgG. DBS and milk samples were tested for SARS-CoV-2 IgG and IgA by a receptor-binding domain enzyme-linked immunosorbent assay, and a sample cutoff (S/Co) of ≥1.1 was considered a positive result. In addition, a neutralization assay was performed on milk samples using a green fluorescent protein reporter-based pseudotyped virus with a vesicular stomatitis virus backbone coated with SARS-CoV-2 spike protein. Sera, not capable of reducing viral replication by 50% at a dilution of 1 to 8, were considered nonneutralizing. Women who were diagnosed with COVID-19 infection and those who were vaccinated before birth were excluded.
Results
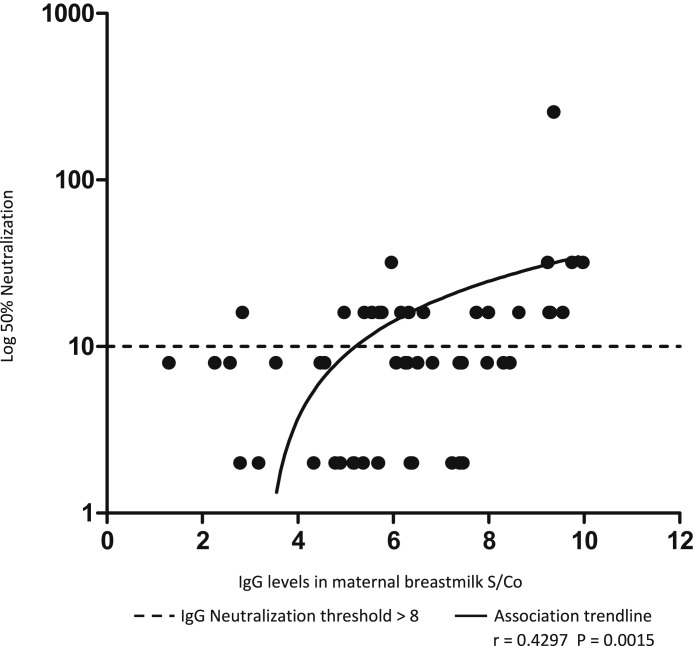
Maternal sera and breastmilk samples were obtained from 61 participating women. All maternal serum and breastmilk samples were positive for SARS-CoV-2 IgG with median concentrations of 31.7 S/Co (interquartile range [IQR], 25.1–38.1) and 6.3 S/Co (IQR, 5.1–7.4), respectively. There was a significant positive correlation between the SARS-CoV-2 IgG levels in the maternal serum samples and those in breastmilk samples (r=0.514; P=.0001). Moreover, 18 of 47 milk samples (38.3%) were found to neutralize SARS-CoV-2 infectivity (Figure ). SARS-CoV-2 IgG was detected in the oral mucosa of 3 of 5 (60%) breastfed infants. However, all of the DBS samples obtained from 21 infants were negative for these antibodies. SARS-CoV-2 IgA in secretory form was detected in 15% of the breastmilk samples with a median of 0.4 S/Co (IQR, 0.3–0.7).
Figure.
Association between SARS-CoV-2 IgG levels in breast-milk of vaccinated women to neutralization capacity
IgG, immunoglobulin G; S/Co, sample cutoff.
Schwartz. SARS-CoV-2 antibodies in lactating women and their infants following BNT162b2 vaccine. Am J Obstet Gynecol 2021.
Conclusion
In this longitudinal cohort study, lactating women vaccinated against COVID-19 were found to have SARS-CoV-2 IgG in their breastmilk samples, and nearly half of the samples enabled neutralization of SARS-CoV-2 infectivity. IgG antibodies were found in the oral mucosa of 3 (60%) of the infants’ samples, but IgG antibodies were not found in their circulation. To date, there are 3 studies of vaccinated lactating women, which enrolled 5, 31, and 84 women, respectively. All of these studies found vaccine-generated IgG and IgA antibodies in breastmilk samples,2, 3, 4 however, none evaluated the neutralizing capacity of breastmilk antibodies or the presence of antibodies in the infants’ serum or oral mucosa. Our findings may suggest that breastfed infants acquire passive immunity against COVID-19. However, in view of our observation that SARS-CoV-2 IgG was not detected in the infants’ serum, it seems that vaccination during pregnancy may provide better protection to the infants through transplacental passage of antibodies.5
Footnotes
The authors report no conflict of interest.
This study did not receive any financial support.
References
- 1.The American College of Obstetricians and Gynecologists Practice Advisory COVID-19 vaccination considerations for obstetric gynecologic care. 2020. https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2020/12/vaccinating-pregnant-and-lactating-patients-against-covid-19 Available at: Accessed March 6, 2021.
- 2.Gray K.J., Bordt E.A., Atyeo C., et al. Coronavirus disease 2019 vaccine response in pregnant and lactating women: a cohort study. Am J Obstet Gynecol. 2021;225:303.e1–303.e17. doi: 10.1016/j.ajog.2021.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perl S.H., Uzan-Yulzari A., Klainer H., et al. SARS-CoV-2-specific antibodies in breast milk after COVID-19 vaccination of breastfeeding women. JAMA. 2021;325:2013–2014. doi: 10.1001/jama.2021.5782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kelly J.C., Carter E.B., Raghuraman N., et al. Anti-severe acute respiratory syndrome coronavirus 2 antibodies induced in breast milk after Pfizer-BioNTech/BNT162b2 vaccination. Am J Obstet Gynecol. 2021;225:101–103. doi: 10.1016/j.ajog.2021.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prabhu M., Murphy E.A., Sukhu A.C., et al. Antibody response to coronavirus disease 2019 (COVID-19) messenger RNA vaccination in pregnant women and transplacental passage into cord blood. Obstet Gynecol. 2021;138:278–280. doi: 10.1097/AOG.0000000000004438. [DOI] [PMC free article] [PubMed] [Google Scholar]