Abstract
Introduction:
Periprosthetic joint infections (PJI) following total hip (THA) and knee (TKA) arthroplasty are associated with significant morbidity. A better understanding of costs of PJI treatment can inform prevention, treatment and reimbursement strategies. The purpose of this study was to describe direct inpatient medical costs associated with treatment of hip and knee PJI.
Methods:
At a single tertiary care institution, 176 hips and 266 knees that underwent two-stage revisions for PJI between 2009 and 2015 were compared with 1611 hips and 1276 knees that underwent revisions for aseptic indications. Additionally, 84 hips and 137 knees that underwent irrigation and debridement (I&D) with partial component exchange were compared with 39 hips and 138 knees that underwent partial component exchange for aseptic indications. Line-item details of services billed during hospitalization were retrieved, and standardized direct medical costs were calculated in 2018 inflation-adjusted dollars.
Results:
Mean direct medical costs for two-stage revision THA performed for PJI was significantly higher than for aseptic revision THA ($58,369 versus $22,846, p<0.001). Similarly, costs for two-stage revision TKA performed for PJI was significantly higher than for aseptic revision TKA ($56,900 versus $24,630, p<0.001). Even when the total costs of aseptic revisions were doubled for a representative comparison to two stage procedures, the costs of PJI procedures were 15% to 28% higher than that for the doubled cost of aseptic revisions (p < 0.001). The mean direct medical costs of I&D procedures for PJI was about two-fold higher than for partial component exchange for aseptic indications.
Conclusion:
The direct medical costs for operative treatment of an infected THA and TKA are two-fold higher than the costs of similar aseptic revisions. The high economic burden of PJI warrants efforts to reduce the incidence of PJI. Reimbursement schemes should account for the high costs of managing PJI in order to ensure sustainable patient care.
Level of Evidence:
III
Introduction
Periprosthetic joint infections (PJI) following total hip (THA) and total knee (TKA) arthroplasty are associated with significant morbidity and economic burden[1]. Accurately characterizing the medical costs of managing PJI is challenging. Existing cost estimates largely rely on hospital charge data, frequently exclude physician services, and typically use pooled data from multiple sources to indirectly estimate costs[1–12]. While large administrative databases allow for increased sample size and capture a diverse group of patients and healthcare systems, they are limited by source-dependent variation in reporting and data quality. Calculation methodology is also variable. Cost calculations typically rely on patient diaries, hospital accounting systems, and/or reimbursement rates and charges. However, these methods measure charges to payers, not true care-associated costs [13, 14]. This is commonly overcome with a single overall cost-charge ratio conversion. While this has the advantage of simplicity; cost-charge ratios vary significantly (from 0.2 to 3.0) across departments or cost centers [13, 15, 16]. Instead, the use of bottom-up, micro-costing valuation techniques can provide more precise and accurate estimates of medical costs [17].
The high costs of treating PJI may create a financial disincentive that could affect access to care [18, 19]. Currently, Medicare is the largest payer for the revision TKA and THA procedures [20–22]. Due to limitations of the current Diagnosis-Related Groups (DRGs) coding system, revision arthroplasties for PJI are coded under a variety of codes and unadjusted DRGs may not meet hospital costs [8]. The reimbursement system does not distinguish between revision indications despite the inherent differences between revision cases performed for different indications. A better understanding of PJI-associated costs would inform prevention efforts and more effective treatment and reimbursement strategies. In this single-institution study, we used a bottom-up, micro-costing valuation technique to determine the direct medical costs associated with PJI care in comparison to aseptic revisions.
Materials and Methods
This was a retrospective study of patients treated at a single tertiary institution from 2009 to 2015. All patients who underwent THA or TKA irrigation and debridement (I&D) or two-stage revision THA or TKA for PJI were eligible for inclusion. These patients were compared to patients who underwent aseptic partial component exchange (i.e., head/liner exchange in the hip and polyethylene insert exchange in the knee) or aseptic revision THA or TKA. All patients who underwent two-stage revision had the procedure performed for treatment of PJI. Following Institutional Review Board approval, patients’ records were obtained from an institutional registry which is maintained by a dedicated staff using standardized data collection processes. This registry contains prospectively obtained data regarding surgical indication, prosthesis, clinical data, examination findings, radiographic follow-up and a variety of post-operative complications. Exclusion criteria were patients who refused use of their medical records for research and patients with suspected PJI but did not meet Musculoskeletal Infection Society (MSIS) criteria for PJI [23].
We identified 176 two-stage revision THA and 266 two-stage revision TKA procedures where both stages were performed at our institution. Two-stage procedures where one stage was performed elsewhere (n-81) were excluded. Of the 176 two-stage revision THA procedures, 55% received articulated spacers. Of the 266 two-stage revision TKA procedures, 20% received articulated spacers. Remaining patients received static spacers or no spacers. All spacers were handmade in the operating room, and there were no commercially manufactured antibiotic articulated spacers. Antibiotic spacers were created using 3 g of vancomycin and 3.6 g of gentamicin per one batch of cement. These procedures were compared to 1611 revision THA and 1276 revision TKA for aseptic indications (Table 1). Mean age was 65 years and comparable across the four groups. The proportion of males was higher in the two-stage revision THA and TKA groups than in aseptic revisions. Median length of stay (two hospitalizations combined) was 8 days for two-stage revisions and 3 days for revisions for aseptic indications. Additionally, we identified 84 THA and 137 TKA that underwent I&D and compared their medical costs with 39 THA and 138 TKA that underwent partial component exchange for aseptic indications (head/liner exchange in the hip and polyethylene insert exchange in the knee).
Table 1.
Characteristics of the revision total hip arthroplasty (THA) and total knee arthroplasty (TKA) study populations.
| Characteristic | Two-Stage Revision THA | Aseptic Revision THA | Two-Stage Revision TKA | Aseptic Revision TKA |
|---|---|---|---|---|
| Number of patients | 176 | 1611 | 266 | 1276 |
| Male (%) | 109 (62%) | 738 (46%) | 162 (61%) | 562 (44%) |
| Age (years) ± SD | 65 ± 12 | 66 ± 13 | 65 ± 11 | 65 ± 12 |
| Race: White | 163 (93%) | 1526 (95%) | 249 (94%) | 1202 (94%) |
| Mean operative time (minutes) ± SD | 176 ± 69 | 146 ± 82 | 168 ± 59 | 139 ± 59 |
| Body mass index (kg/m2), mean ± SD | 31 ± 7 | 30 ± 7 | 34 ± 12 | 33 ± 8 |
| LOS, median (IQR) | 8 (7, 10) | 3 (2, 4) | 8 (7,10) | 3 (2,3) |
| Charlson Comorbidity Index | ||||
| Patients with no comorbidities* | 99/160 (62%) | 1002/1606 (62%) | 158/254 (62%) | 820/1275 (64%) |
| Mean no comorbidities per patient | <1 | < 1 | <1 | <1 |
SD = Standard Deviation, LOS = Length of Stay, IQR = Interquartile range. LOS for two-stage revisions calculated combining two hospital episodes.
Percentage calculated out of patients with any diagnoses in year before surgery
We obtained clinical data from the institutional registry and electronic medical records. Comorbidities were ascertained during the 1 year period before surgery using the Elixhauser comorbidity index which includes 30 comorbid conditions and commonly used in health care utilization and cost studies [24].
In-hospital direct medical costs were calculated using a hybrid approach[16, 17]. Medicare Part A items (i.e., hospital-billed services and procedures), were valued by multiplying billed charges by individual year and cost center-specific cost-to-charge ratios. Cost-to-charge ratios for each cost center were obtained from published Medicare cost reports. Part B services and procedures, which consisted primarily of services billed by physicians, were valued using national average Medicare reimbursement rates. The costing algorithm applied the gross domestic product price deflator (i.e. an economic metric to account for inflation) for Part A and Part B services in order to express the costs for each year in 2018 US dollars. Using Unified Billing (UB) codes, costs were then further stratified into the following cost subcategories: hospital services, professional services, room and board, operating room and anesthesia costs, supplies and implant costs, medications, and laboratory and pathology services. As an example, a hemoglobin blood test is a professional service, and assigned the national Medicare reimbursement amount for the year of the service and then that amount is inflated to the final study year with the gross domestic product price deflator. On the other hand, time in the operating room is a hospital billed service and is assigned a standardized cost by multiplying the charge for that service by the operating room cost-to charge ratio from the Medicare cost report and then inflated to the final study year. Anesthesia is a professional service, so it is calculated by using the national Medicare conversion factors for the service years. Implant charges are multiplied by the Medicare cost report implant cost-to-charge ratios and then inflated to the final study year. We are not reporting actual internal costs of implants.
Statistical Methods
Patient characteristics are presented as means ± standard deviations (SDs), medians with interquartile ranges (IQR), and frequencies and percentages. Costs are presented as means with 95% bootstrap confidence intervals (CI). Univariate analyses were used to compare overall costs and each cost subcategory. All analyses were performed using R version 3.4.0 and SAS version 9.4.
Results
THA two-stage revision versus aseptic revision THA
The mean overall direct hospitalization costs of two-stage revision THA for PJI ($58,369; 95% confidence interval (CI): $55,150-$62,743) was significantly higher than for aseptic revision THA ($22,846; 95% CI: $22,321-$23,467, p<0.001). Mean costs for the first inpatient episode of care (resection, $30,912) were slightly higher for the second episode of care (reimplantation, $27,457). Of note, 55% of patients received articulating spacers. Even when the total costs of aseptic revision THA were doubled for a representative comparison to two stage procedures, the costs of PJI procedures were 28% ($12,677) higher than that for the doubled cost of aseptic revision THA (p<0.001; Table 2). Surgeon and professional costs for two-stage revisions for PJI ($7,347) constituted only 13% of the total costs whereas operating room/anesthesia (29%), room and board (24%) and implants (17%) constituted the largest proportion of costs. Costs for aseptic revision THA were significantly lower than two-stage procedures across all service categories (Table 2).
Table 2.
2018 mean adjusted direct hospital costs (95% confidence intervals) of two stage revision for periprosthetic joint infection (PJI) compared to aseptic revision in total hip arthroplasty (THA).
| Characteristic | Two Stage Revision THA for PJI Costs (95% CI) |
Aseptic Revision THA Costs (95% CI) |
|---|---|---|
| Total costs | $58,369 ($55,150 – $62,743) | $22,846 ($22,321 – $23,467) |
| 2 hospital episodes | Resection: $30,912 Reimplantation: $27,457 |
|
| Medicare part A hospital services | $50,553 ($47,579 – $54,642) | $19,450 ($18,975 – $20,020) |
| Medicare part B professional costs | $7,347 ($7,519 – $8,175) | $3,397 ($3,345 – $3,458) |
| Costs by service category | ||
| Room and board | $14,120 ($12,246 – $16,982) | $4,971 ($4,790 – $5,208) |
| Operating room and anesthesia | $17,128 ($16,730 – $17,587) | $7,563 ($7,479 – $7,668) |
| Implants | $9,901 ($9,293 – $10,495) | $4,085 ($3,965 – $4,212) |
| Pharmacy and medications | $4,676 ($4,300 – $4,471) | $1,393 ($1,281 – $1,571) |
| Laboratory and pathology | $2,345 ($2,140 – $2,604) | $770 ($728 – $827) |
| Radiology | $814 ($640 – $1,066) | $249 ($226 – $273) |
| Physical and occupational therapy | $1,867 ($1,688 – $2,113) | $845 ($827 – $865) |
| ICU [number of patients] | [N=20] $9,190 ($5,466 – $14,640) |
[N=51] $9,214 ($5,369 – $14,523) |
| Transfusion | $626 ($548 – $713) | $254 ($229 – $289) |
Notes: Costs for two-stage revision THA are calculated by combining two hospitalization episodes (resection and reimplantation). Costs for aseptic revision THA are calculated per hospital episode. The 1,611 aseptic revision THA include 953 revisions for wear, loosening, 249 for dislocation and 174 fractures.
We also examined direct medical costs incurred in our institution during the one week before, in-between, and one week after the two-stage procedures. Of the 176 two-stage revision THA patients, 133 (76%) received services during the week before resection at a mean cost of $1,258. All 176 patients received services between the resection and reimplantation episodes, consisting of outpatient IV antibiotics (4–6 weeks) and peripherally inserted central catheter care at a mean cost of $6,053. A total of 29 (17%) patients received services during the week after reimplantation at a mean cost of $960.
TKA two-stage revision versus aseptic revision TKA
The mean direct hospitalization costs of two-stage revision TKA for PJI ($56,900, 95% CI $54,213-$61,014) was significantly higher than for aseptic revision TKA ($24,630, 95% CI $24,212-$25,030, p<0.001). Mean costs for the first inpatient episode of care (resection, $25,520) were slightly lower than for the second episode of care (reimplantation, $31,381). Even when the total costs of aseptic revision TKA were, the costs of PJI procedures were 15% ($7,640) higher than that for the doubled cost of aseptic revision TKA (p < 0.001; Table 3). Professional costs were a small proportion (12%) of total costs whereas room and board (23%), operating room (27%), and implant costs (24%) were main categorical drivers of cost (Table 3).
Table 3.
2018 mean adjusted direct hospital costs (95% confidence intervals) of two stage revision for periprosthetic joint infection (PJI) compared to aseptic revision in total knee arthroplasty (TKA).
| Characteristic | Two Stage Revision TKA for PJI Costs (95% CI) |
Aseptic Revision TKA Costs (95% CI) |
|---|---|---|
| Total costs | $56,900 ($54,213 – $61,014) | $24,630 ($24,212 – $25,030) |
| 2 hospital episodes | Resection: $25,520 Reimplantation: $31,381 |
|
| Medicare part A hospital services | $50,160 ($47,739 – $53,870) | $21,533 ($21,156 – $21,914) |
| Medicare part B professional costs | $6,742 ($6,455 – $7,153) | $3,099 ($3,061 – $3,136) |
| Costs by service category | ||
| Room and board | $12,937 ($11,807 – $14,693) | $4,307 ($4,197 – $4,422) |
| Operating room and anesthesia | $15,350 ($14,953 – $15,844) | $7,430 ($7,369 – $7,494) |
| Implants | $13,511 ($12,983 – $14,041) | $8,106 ($7,835 – $8,376) |
| Pharmacy and medications | $4,568 ($4,204 – $5,121) | $1,297 ($1,257 – $1,347) |
| Laboratory and pathology | $2,077 ($1,896 – $2,344) | $612 ($590 – $639) |
| Radiology | $548 ($443 – $709) | $188 ($170 – $206) |
| Physical and occupational therapy | $1,554 ($1,451 – $1,672) | $690 ($674 – $705) |
| ICU [number of patients] | [N=13] $24,836 ($8,080 – $47,806) |
[N=26] $4,396 ($3,118 – $6,045) |
| Transfusion | $433 ($384 – $492) | $199 ($171 – $234) |
Notes: Costs for two-stage revision TKA are calculated by combining two hospitalization episodes (resection and reimplantation). Costs for aseptic revision TKA are calculated per hospital episode. The 1,276 aseptic revision TKA include 586 revisions for wear, loosening, 366 instability and 74 fractures.
We examined costs during the one week before, after and in-between the two-stage TKA procedures. Of the 266 patients who underwent two-stage reimplantation, 223 received services during the 1 week before resection for a total mean cost of $848. Two hundred and sixty-four two-stage revision TKA patients received services between resection and reimplantation at a mean cost of $7,150, which was statistically similar to that for the THA cohort (p = 0.117). The costs of 2 patients who received this portion of care at a different institution were not captured. Sixty-four patients received services during the 1 week after reimplantation for a total mean cost of $366.
Irrigation and debridement versus aseptic partial component exchange
For THA patients, the mean overall direct hospitalization costs of I&D ($39,597, 95% CI $33,386-$47,448) was significantly higher than for aseptic head/liner exchange ($19,297, 95% CI $17,672-$21,218, p<0.001; Figure 1A). For TKA patients, the mean overall direct hospitalization costs of I&D ($38,776, 95% CI $30,784-$49,669) was significantly higher than for aseptic polyethylene insert exchange ($16,870, 95% CI $15,333-$17,480, p<0.001; Figure 1B).
Figure 1.
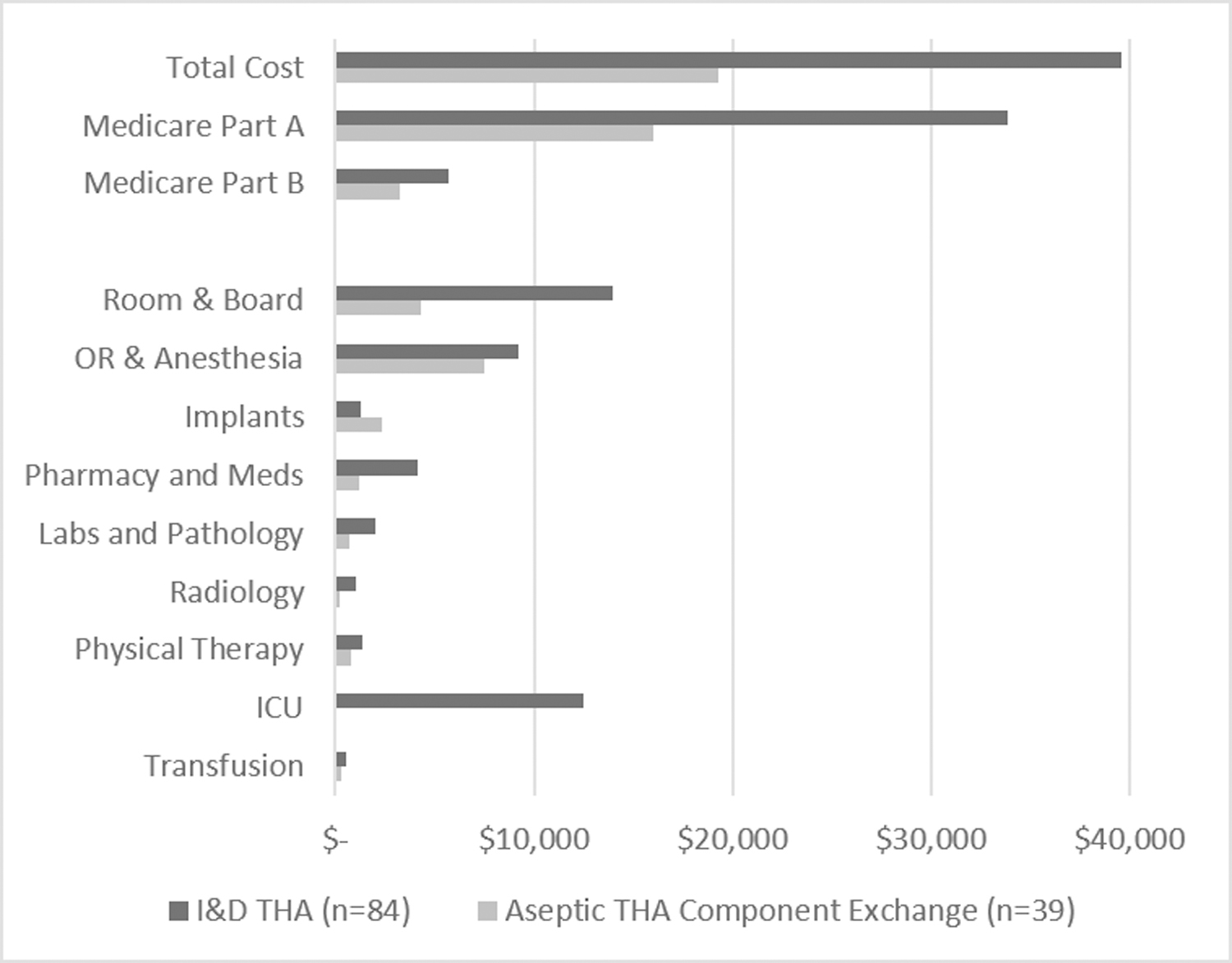
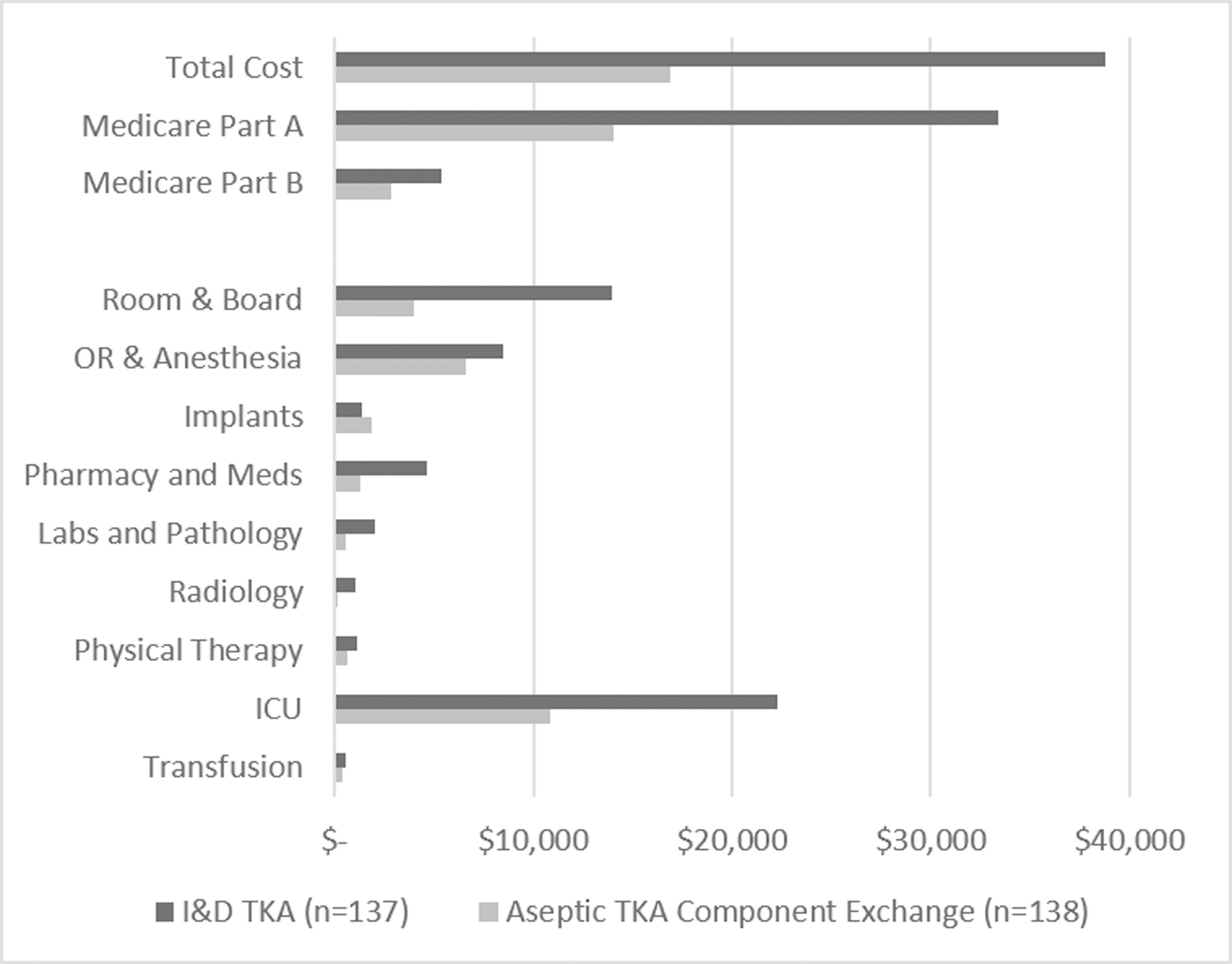
2018 adjusted mean direct hospital costs of irrigation and debridement (I&D) compared to aseptic partial component exchange in total hip arthroplasty (THA; Figure 1A) and total knee arthroplasty (TKA; Figure 1B)
Discussion
A better understanding of PJI-associated costs is essential to inform prevention efforts, effective treatment, and reimbursement strategies. We found that the total direct medical costs associated with treatment of PJI are significantly higher than costs associated with comparable aseptic revision THA and TKA procedures. Two-stage reimplantations cost 130 – 155% more than all-cause aseptic revision TKA and THA, respectively. Even when the hospital costs of aseptic revision THA and TKA were doubled to account for the two hospitalizations involved in staged procedures, PJI patients had 15% and 28% higher medical costs. Although this difference is in part driven by longer hospitalizations and associated room and board, cost differences persisted across all categories of services.
While the costs of primary THA and TKA have been described, there is a paucity of data regarding septic revision procedures. Available studies are either based on administrative data from the Nationwide Inpatient Sample, small single-center studies, or other methodologies which did not include operating room, recovery room, intensive care unit, hospital room space, or clinical lab charges[1–12]. Using 2001–2009 data from the Nationwide Inpatient Sample and converting charges to 2011 costs using crude cost-to-charge ratios, Kurtz and colleagues estimated the cost of PJI hospitalizations in $25,000-$30,000 range with costs higher for THA than TKA, comparable to the values in the present study[25]. Of note, our estimated two stage reimplantation costs are lower than most previous reports of PJI costs [2–4, 8, 16, 25–29]. This is likely due to key methodological differences and our use of detailed line-item costs instead of charges, allowing for more accurate analysis as opposed to crude cost-to-charge ratios [16, 17]. Furthermore, practice variation in antibiotic use, clinical practice and other factors likely also contribute to this difference. For example, high-volume institutions are better able to contain the costs for primary THA and TKA and the same holds for revision procedures [30]. We believe our large, tertiary referral center status may in part contribute to cost efficiency. In fact, the combined number of revision THA and TKA cases for PJI indications has been at or above 60 procedures every year between 2009 and 2015. However, despite a large institutional volume of cases and extensive institutional experience, the costs of two stage reimplantation for PJI remain strikingly high.
Similarly, hospital costs for I&D related hospitalizations are more than twice those of aseptic head/liner exchange in the hip and polyethylene insert exchange in the knee. The largest drivers of this cost difference are room and board as well as intensive care costs. There is also a paucity of data regarding the costs of I&D [4, 31–33]. It is worth noting that patients treated with I&D are clinically different than those treated with two-stage reimplantation. They typically present with an acute infection or perioperative risk which precludes two-stage revision. Furthermore, I&D has been shown to have higher rates of persistent infection and subsequent revisions potentially contributing to higher costs in these patients[34–36].
With the growing number of primary THA and TKA procedures, and the large number of patients at risk; the corresponding incidence of revisions for septic indications is expected to increase [25, 37]. In the modern, cost-conscious healthcare era, it is of great importance to create value-based reimbursement schedules that disincentivize reimbursement-specific referral practices while supporting patient-centric care by accounting for differences present between various septic and aseptic indications for revisions. These increased costs, along with the risk for poor clinical outcomes in infected THA and TKA patients suggest that efforts to prevent PJI should remain a high priority for orthopedic surgeons and hospital systems. Additionally, the current DRG scheme does not provide risk-adjustment for PJI revisions and associated complications, which may disincentivize and make PJI care less sustainable. This is particularly concerning given the Centers for Medicare & Medicaid Services (CMS) CY 2021 Medicare Physician Fee Schedule (PFS) proposed rule which will decrease the value assigned to THA and TKA. As we demonstrate in this study, managing infectious complications of THA and TKA is resource intensive and costly, and future reimbursement schemes should account for the high costs in order to ensure sustainable access and effective care of patients with PJI.
Our findings have important limitations. First, cost analyses would ideally include indirect medical costs in addition to direct medical costs. Outpatient medical costs and indirect costs, including the opportunity costs of lost productivity and other inconveniences, have significant societal impacts. However, our hospital-based data has limited value in estimating outpatient costs and indirect costs since most patients in this cohort are referral patients and also receive care elsewhere. Therefore, our cost estimates are an underestimate of the true economic burden of PJI. Second, this cohort was assembled at a single large tertiary care hospital. While the advantages of single institution studies in obtaining highly detailed cost data, has already been described [16, 17, 33], the generalizability of our results is limited due to differences in practice patterns. Practice patterns in our institution may not be representative of those in a variety of practice settings across the United States. Multi-center studies using similar granular costing methodology are necessary. Third, many PJI patients treated at our institution were referred from outside centers. We have limited information about how much treatment these patients received before presentation to our center. Likely, at least a minority of these patients would have received antibiotic treatment and/or surgical intervention before evaluation at our center. The costs of previous treatments are not completely accounted in our analysis. Fourth, although this paper reports boot-strapped confidence intervals and p-values for mean costs, the cost data were skewed to the right and the median costs were in general lower than the mean costs.
In summary, this study confirms the high economic burden of PJI with two-fold higher direct medical costs compared to aseptic revision procedures. The high economic burden of PJI warrants efforts to reduce the incidence of PJI. Current and future reimbursement schedules should account for the high costs of managing PJI in order to ensure sustainable patient care.
Source of Funding
Research was supported by the National Institutes of Health (NIH) under grant P30AR76312. The content is solely the responsibility of the authors and does not necessarily represent the views of the NIH.
References:
- 1.Parisi TJ, Konopka JF, and Bedair HS, What is the Long-term Economic Societal Effect of Periprosthetic Infections After THA? A Markov Analysis. Clin Orthop Relat Res, 2017. 475(7): p. 1891–1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hebert CK, et al. , Cost of treating an infected total knee replacement. Clin Orthop Relat Res, 1996(331): p. 140–5. [DOI] [PubMed] [Google Scholar]
- 3.Lavernia C, Lee DJ, and Hernandez VH, The increasing financial burden of knee revision surgery in the United States. Clin Orthop Relat Res, 2006. 446: p. 221–6. [DOI] [PubMed] [Google Scholar]
- 4.Lavernia CJ, et al. , Revision and primary hip and knee arthroplasty. A cost analysis. Clin Orthop Relat Res, 1995(311): p. 136–41. [PubMed] [Google Scholar]
- 5.Bozic KJ, et al. , Comparative Epidemiology of Revision Arthroplasty: Failed THA Poses Greater Clinical and Economic Burdens Than Failed TKA. Clin Orthop Relat Res, 2015. 473(6): p. 2131–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kasch R, et al. , Comparative Analysis of Direct Hospital Care Costs between Aseptic and Two-Stage Septic Knee Revision. PLoS One, 2017. 12(1): p. e0169558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rennert-May ED, et al. , The cost of managing complex surgical site infections following primary hip and knee arthroplasty: A population-based cohort study in Alberta, Canada. Infect Control Hosp Epidemiol, 2018. 39(10): p. 1183–1188. [DOI] [PubMed] [Google Scholar]
- 8.Hellmann M, et al. , The estimated magnitude and direct hospital costs of prosthetic joint infections in the United States, 1997 to 2004. J Arthroplasty, 2010. 25(5): p. 766–71 e1. [DOI] [PubMed] [Google Scholar]
- 9.Kapadia BH, et al. , The Economic Impact of Periprosthetic Infections After Total Hip Arthroplasty at a Specialized Tertiary-Care Center. J Arthroplasty, 2016. 31(7): p. 1422–6. [DOI] [PubMed] [Google Scholar]
- 10.Puhto T, et al. , Infection triples the cost of a primary joint arthroplasty. Infect Dis (Lond), 2019. 51(5): p. 348–355. [DOI] [PubMed] [Google Scholar]
- 11.Merollini KM, Crawford RW, and Graves N, Surgical treatment approaches and reimbursement costs of surgical site infections post hip arthroplasty in Australia: a retrospective analysis. BMC Health Serv Res, 2013. 13: p. 91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carducci MP, et al. , Variation in the Cost of Care for Different Types of Joint Arthroplasty. J Bone Joint Surg Am, 2020. 102(5): p. 404–409. [DOI] [PubMed] [Google Scholar]
- 13.Finkler SA, The distinction between cost and charges. Ann Intern Med, 1982. 96(1): p. 102–9. [DOI] [PubMed] [Google Scholar]
- 14.Riley GF, Administrative and claims records as sources of health care cost data. Med Care, 2009. 47(7 Suppl 1): p. S51–5. [DOI] [PubMed] [Google Scholar]
- 15.Shwartz M, et al. , The importance of comorbidities in explaining differences in patient costs. Med Care, 1996. 34(8): p. 767–82. [DOI] [PubMed] [Google Scholar]
- 16.Maradit Kremers H, et al. , Determinants of direct medical costs in primary and revision total knee arthroplasty. Clin Orthop Relat Res, 2013. 471(1): p. 206–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Visscher SL, et al. , Developing a standardized healthcare cost data warehouse. BMC Health Serv Res, 2017. 17(1): p. 396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sculco TP, The economic impact of infected total joint arthroplasty. Instr Course Lect, 1993. 42: p. 349–51. [PubMed] [Google Scholar]
- 19.Bozic KJ and Ries MD, The impact of infection after total hip arthroplasty on hospital and surgeon resource utilization. J Bone Joint Surg Am, 2005. 87(8): p. 1746–51. [DOI] [PubMed] [Google Scholar]
- 20.Bozic KJ, et al. , The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res, 2010. 468(1): p. 45–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bozic KJ, et al. , The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am, 2009. 91(1): p. 128–33. [DOI] [PubMed] [Google Scholar]
- 22.Kowalik TD, et al. , The Epidemiology of Primary and Revision Total Hip Arthroplasty in Teaching and Nonteaching Hospitals in the United States. J Am Acad Orthop Surg, 2016. 24(6): p. 393–8. [DOI] [PubMed] [Google Scholar]
- 23.Parvizi J, et al. , New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res, 2011. 469(11): p. 2992–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Elixhauser A, et al. , Comorbidity measures for use with administrative data. Medical Care, 1998. 36(1): p. 8–27. [DOI] [PubMed] [Google Scholar]
- 25.Kurtz SM, et al. , Economic burden of periprosthetic joint infection in the United States. J Arthroplasty, 2012. 27(8 Suppl): p. 61–5 e1. [DOI] [PubMed] [Google Scholar]
- 26.Culler SD, et al. , Predicting the Incremental Hospital Cost of Adverse Events Among Medicare Beneficiaries in the Comprehensive Joint Replacement Program During Fiscal Year 2014. J Arthroplasty, 2017. 32(6): p. 1732–1738 e1. [DOI] [PubMed] [Google Scholar]
- 27.Kapadia BH, et al. , The economic impact of periprosthetic infections following total knee arthroplasty at a specialized tertiary-care center. J Arthroplasty, 2014. 29(5): p. 929–32. [DOI] [PubMed] [Google Scholar]
- 28.Oduwole KO, et al. , Increasing financial burden of revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc, 2010. 18(7): p. 945–8. [DOI] [PubMed] [Google Scholar]
- 29.Parvizi J, et al. , Periprosthetic joint infection: the economic impact of methicillin-resistant infections. The Journal of arthroplasty, 2010. 25(6): p. 103–107. [DOI] [PubMed] [Google Scholar]
- 30.Losina E, et al. , Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med, 2009. 169(12): p. 1113–21; discussion 1121–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.O’Shea K, Bale E, and Murray P, Cost analysis of primary total hip replacement. Ir Med J, 2002. 95(6): p. 177–80. [PubMed] [Google Scholar]
- 32.Martineau P, et al. , Primary hip arthroplasty costs are greater in low-volume than in high-volume Canadian hospitals. Clin Orthop Relat Res, 2005(437): p. 152–6. [DOI] [PubMed] [Google Scholar]
- 33.Daigle ME, et al. , The cost-effectiveness of total joint arthroplasty: a systematic review of published literature. Best practice & research. Clinical rheumatology, 2012. 26(5): p. 10.1016/j.berh.2012.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Urish KL, et al. , A Multicenter Study of Irrigation and Debridement in Total Knee Arthroplasty Periprosthetic Joint Infection: Treatment Failure Is High. J Arthroplasty, 2018. 33(4): p. 1154–1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bradbury T, et al. , The fate of acute methicillin-resistant Staphylococcus aureus periprosthetic knee infections treated by open debridement and retention of components. J Arthroplasty, 2009. 24(6 Suppl): p. 101–4. [DOI] [PubMed] [Google Scholar]
- 36.Kuiper JW, et al. , Prosthetic joint-associated infections treated with DAIR (debridement, antibiotics, irrigation, and retention): analysis of risk factors and local antibiotic carriers in 91 patients. Acta Orthop, 2013. 84(4): p. 380–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Maradit Kremers H, et al. , Prevalence of Total Hip and Knee Replacement in the United States. J Bone Joint Surg Am, 2015. 97(17): p. 1386–97. [DOI] [PMC free article] [PubMed] [Google Scholar]


