Abstract
Objective:
To determine whether temperature screening is useful in detecting and reducing workplace transmission of SARS-CoV-2.
Methods:
A survey was conducted to determine whether temperature screening successfully identified workers with coronavirus disease 2019 (COVID-19) among a convenience sample of medical directors of multinational corporations in a wide range of industries.
Results:
More than 15 million screenings were performed by 14 companies. Fewer than 700 episodes of fever were identified. Of these, only about 53 cases of COVID-19 were detected. By contrast about 2000 workers with diagnosed COVID-19 were in the workplace and not detected by screening.
Conclusions:
One case of COVID-19 was identified by screening for approximately every 40 cases that were missed. Worksite temperature screening was ineffective for detecting workers with COVID-19 and is not recommended.
Keywords: COVID-19 detection, employee temperature checks, fever screening
Learning Objectives
Discuss the methods of and responses to the survey of corporate medical directors regarding worksite temperature screening for COVID-19.
Summarize the findings in terms of screenings performed, episodes of fever identified, and cases of COVID-19 detected.
Discuss the implications for temperature screening as part of an evidence-based program to prevent workplace transmission of SARS-CoV-2.
Over the course of the global pandemic caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), employers have sought ways to limit the impact of coronavirus disease 2019 (COVID-19) on their workforce while also minimizing business interruption. Fever was recognized as a common early symptom of COVID-19, leading several countries, states, and cities to mandate temperature screening. Many employers decided to implement temperature screening for worksites beyond those where it was required by law. This study sought to determine the effectiveness of worksite temperature screening for detection of COVID-19.
METHODS
A survey was sent using Qualtrics to a convenience sample of medical directors from large multinational companies. The survey was completed between February 23 and March 9, 2021 by 20 medical directors from companies in a variety of industry sectors including chemicals, energy, entertainment, finance, manufacturing, mining, and pharmaceuticals. The survey requested information on the conduct and results of temperature screening, rationale for screening, and other aspects of company policy and practice intended to limit the impact of COVID-19 in the workplace.
RESULTS
Company Policies
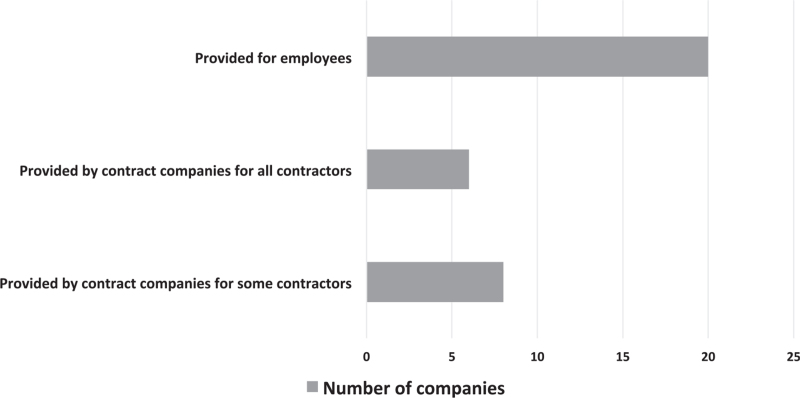
Respondents reported that their companies followed all of the commonly recommended policies to reduce the risk of workplace transmission of SARS-CoV-2 including use of masks and physical distancing (Table 1). One company also conducted onsite SARS-CoV-2 testing. All companies of respondents provided employees paid sick leave. At most companies, contractors received paid sick leave through their employers (Fig. 1). Symptom screening was conducted for most or all employees at 17 companies and only where required by law at three companies. One company did not conduct symptom screening.
TABLE 1.
Measures to Reduce Workplace Transmission of SAR-CoV-2 Reported by All Respondents
| Required use of masks |
| Physical distancing |
| Decreased occupancy |
| Limits on group meetings |
| Encouraging handwashing |
| Enhanced cleaning |
| Enhanced ventilation |
| Limits on business travel |
FIGURE 1.
Paid sick leave policy.
Temperature Screening
Seventeen respondents reported that their company conducted temperature screening of most or all employees, although in some cases this was limited to specific sites. Two respondents indicated that their company only performed screening when required by law and one company did not conduct screening at any location. Five companies provided most or all employees with thermometers for use at home. A few companies provided thermometers for a limited number of sites. Companies that provided thermometers had employees complete home screening, although one also conducted screening at the worksite.
For temperature screening, 16 companies used handheld thermal scanners (non-contact Infrared thermometers—NCIT). Ten companies used fixed position thermal cameras (infrared thermal detection systems—ITDS). Four of the companies using IDTS used NCIT at some sites.
Fourteen respondents provided information on the number of screenings conducted and the results of screening for detecting cases of COVID-19. One company conducted 5 million screenings and detected only 75 cases of fever, but did not track how many were diagnosed with COVID-19. Another conducted about 2.5 million screenings, identifying about 100 workers with fever, and also did not track diagnoses. Among the companies that tracked disease status, more than 15 million screenings were conducted, detecting only around 600 cases of fever (Table 2). Of these, fewer than 53 cases of COVID-19 were identified, representing 8% of those with fever. This is the equivalent of conducting 300,000 screenings to detect one case. At the same time, these companies identified more than 2000 cases of COVID-19 in the workplace that were not identified through screening. Approximately one case of COVID-19 was identified by temperature screening for every 40 cases that were missed.
TABLE 2.
Detection of COVID-19 With Worksite Temperature Screening (Some Numbers are Estimates)
| Company | Employees Screened | Total Number of Screenings | Number With Fever | Fever and COVID-19 | No Fever and COVID-19 |
| 1 | 11,000 | – | 85 | 1 | 55 |
| 2 | 142,000 | 2,480,000 | 400 | 40 | 250 |
| 3 | >20,000 | 4,800,000 | <10 | <10 | – |
| 4 | 15,000 | 4,000,000 | 5 | 0 | Hundreds |
| 5 | 10,000 | 30,000 | 0 | 0 | 500 |
| 6 | 600 | 45,000 | 2 | 0 | 1493∗ |
| 7 | Hundreds | Thousands | 5 | 1 | 500 |
| 8 | 5000 | 1,000,000 | 0 | 0 | 0 |
| 9 | 10,000 | 1,500,000 | 5 | 1 | 300 |
| 10 | 5000 | >1,000,000 | Rare | 0 | – |
| 11 | 1800 | >20,000 | 79 | 0 | 40 |
| 12 | 8000 | >50,000 | 0 | 0 | 200 |
| 13 | – | 570,000 | 51 | 0 | 88 |
| 14 | 1200 | >100,000 | 0 | 0 | 0 |
Includes sites where temperature screening is not conducted.
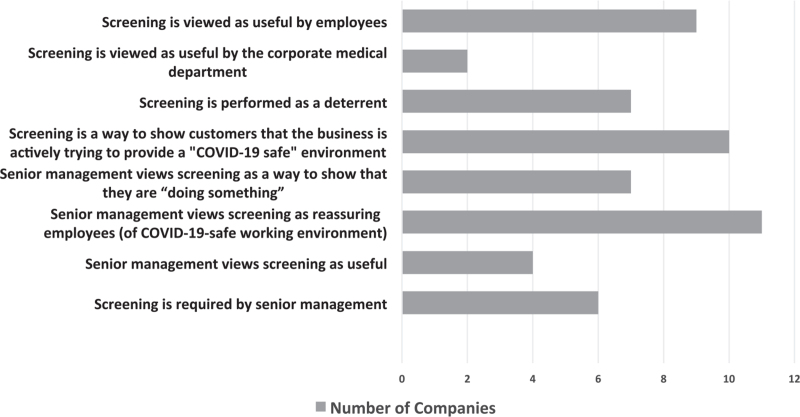
Perceived Value
Respondents of most corporate medical departments did not perceive worksite temperature screening to be valuable (Fig. 2). However, senior management at many companies viewed these programs favorably and often saw this as a way to show employees and customers that they were trying to provide a “COVID-19 safe” environment.
FIGURE 2.
Views on the value of temperature screening (the total numbers exceed the number of companies since respondents were asked to select all applicable statements).
DISCUSSION
In this analysis of the experience of medical directors of multinational companies, worksite temperature screening identified very few workers with fever who tested positive for SARS-CoV-2. By contrast, many employees with COVID-19 were identified in the workplace, yet not detected through temperature screening.
Temperature screening uses tools that measure skin surface temperature and not core temperature. Some infrared thermal detection systems are reasonably accurate for detecting fever.1 The majority of respondents reported using non-contact infrared thermometers for temperature screening. However, many are less accurate than they are claimed to be and have a low sensitivity to detect fever.2
During the initial phase of the COVID-19 pandemic, fever was common among hospitalized patients with severe disease. The first report from Wuhan, China indicated that 98.6% of 138 hospitalized patients had fever.3 A subsequent study from China of 1099 patients reported that 43.8% had fever on admission, increasing to 88.7% during their hospitalization.4 As less severe illness was identified, fever was observed to be less common at the time of hospitalization. At Kaiser Permanente Northern California, fever was present in 33.7% of 377 patients seen in the emergency department in March 2020.5 Similarly, among 5644 patients admitted to the hospital in New York from March 1 to April 4, 2020, 30.7% had fever on presentation.6
Most studies reporting the prevalence of fever as a presenting symptom focus on those hospitalized. It is possible that the frequency of fever is even lower in workers who have SARS-CoV-2 infection and feel well enough to come into a workplace. The experience of passengers on an Antarctica cruise provides more insight into the frequency of fever in an infected population. While 128 (59%) of the passengers and crew tested positive for SARS-CoV-2, fever and mild symptoms were present in only 16 (12.5%). Eight had more serious illness. The majority of the population that tested positive were asymptomatic (104 patients or 81%).7 While the percentage of those infected with SARS-CoV-2 in a population group who are asymptomatic may vary based on demographics and other factors, a review suggested that asymptomatic persons may account for approximately 40% to 45% of SARS-CoV-2 infections.8
Symptom and temperature screening will not detect workers with asymptomatic infection and those who are pre-symptomatic. This is particularly problematic in COVID-19 as, unlike most other respiratory illnesses, people can transmit SARS-CoV-2 infection despite having no symptoms.
Any screening effort will perform poorly when the prevalence of the condition being sought is low. Even during the largest waves of the pandemic, the percentage of workers who completed symptom screening and felt well enough to come to a worksite, yet had a fever was likely to be low. Temperature measurement in this setting likely has a low sensitivity for identifying COVID-19. This would explain why the positive predictive value for temperature screening seen here was about 2%. While the negative predictive value seems high, screening failed to identify nearly all workers who subsequently tested positive for COVID-19 while at the worksite.
Respondents participating in this survey had comprehensive multi-layered programs at their companies to reduce the risk of SARS-CoV-2 transmission in the workplace. It was evident that the companies were making substantial and visible changes to protect employees. Yet senior management at many companies chose to pursue worksite temperature screening in locations where this was not required by law, even though corporate medical departments did not see this as valuable. Senior executives that viewed worksite temperature screening to be valuable often viewed these efforts to be reassuring for employees and customers. While senior management has the prerogative to pursue non-evidence-based approaches, this comes at a cost. The time and money spent on temperature screening is not available for other purposes. There may also be some risk that the trust and credibility of the advice from the corporate medical department may be eroded, when evidence-based recommendations are not followed.
While no published studies of worksite temperature screening during the SARS epidemic of 2003 were identified in a literature search, the results of this study are consistent with the experience of airport screening for SARS. From March through July 2003, 763,082 persons arriving or departing Toronto and Vancouver airports were screened by the thermal scanners. Of these, 191 had an initial temperature reading >38°C, yet no cases of SARS were identified at border entry points. Subsequent analysis of travel histories of suspected and probable SARS patients showed that illness was evident only after arrival and would not have been detected by screening at the airport.9 In Singapore, temperature screening at the airport and sea terminals identified 4044 travelers with temperatures >37.5°C. Of these travelers, no cases of SARS were detected.10
Airport screening for COVID-19 in 2020 was similarly resource-intensive with a low yield of laboratory-diagnosed cases. Passenger entry screening at US airports from January 17 to September 13, 2020 detected only one case per 85,000 travelers screened.11 Of 766,044 travelers, only 298 (0.04%) met Center for Disease Control and Prevention (CDC) criteria for referral based on symptoms or history. Of this 298, only 60 had fever detected by non-contact infrared thermometer and just 10 tested positive for SARS-CoV-2 infection.11 Of the 48 travelers with fever detected by screening and no other symptoms, 5 tested positive for SARS-CoV-2 infection.11 The World Health Organization (WHO) does not support temperature measurement as an effective measure for COVID-19 for entry screening “because people may be traveling during the incubation period (between exposure and symptom onset), may not exhibit fever early in the course of the disease or may reduce fever through the use of antipyretic medications.”12
The key elements of a program to prevent workplace transmission of SARS-CoV-2 are: 1) physical distancing; 2) mask use; 3) appropriate hygiene; 4) supporting work from home when feasible; 5) paid sick leave; 6) contact tracing; and 7) testing for symptoms and close contacts. Workers should also be encouraged to maintain safe practices when outside the workplace. Temperature screening contributes little to detecting infected workers or preventing transmission.
This study has several limitations. Only a relatively small number of companies are represented, although they have conducted a very large number of temperature screenings in a broad array of businesses. This study includes large companies with sophisticated corporate medical programs. These companies also implemented extensive programs to reduce the risk of workplace transmission. Companies that have not instituted these preventive measures were not included.
It is possible that temperature screening has a deterrent value that contributes to the low rate of fever detection. While there is no way to exclude this possibility, the companies surveyed offered paid sick leave, conducted symptom screening, and discouraged workers from coming to the workplace if they had symptoms.
CONCLUSION
In this survey of a convenience sample of large multinational companies in a wide variety of business sectors, temperature screening of workers identified very few true positives while missing many more workers with COVID-19.
Footnotes
G. Stave received consulting fees from Novartis and royalties from John Wiley and Sons which had no bearing on the content of this article.
Stave, Smith, Hymel, and Heron have no relationships/conditions/circumstances that present potential conflict of interest.
The JOEM editorial board and planners have no financial interest related to this research.
Clinical significance: Temperature screening identifies few cases of COVID-19 for worksites that conduct symptom screening and reduce the incentive to come to work when sick by providing paid sick leave. Measures that reduce the risk of workplace transmission remain critical, as screening does not detect asymptomatic, pre-symptomatic, or some mildly symptomatic workers.
REFERENCES
- 1.Nguyen AV, Cohen NJ, Lipman H, et al. Comparison of 3 infrared thermal detection systems and self-report for mass fever screening. Emerg Infect Dis 2010; 16:1710–1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aw J. The non-contact handheld cutaneous infra-red thermometer for fever screening during the COVID-19 global emergency. J Hosp Infect 2020; 104:451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020; 323:1061–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; 382:1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Myers LC, Parodi SM, Escobar GJ, Liu VX. Characteristics of hospitalized adults with COVID-19 in an integrated health care system in California. JAMA 2020; 323:2195–2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA 2020; 323:2052–2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ing AJ, Cocks C, Green JP. COVID-19: in the footsteps of Ernest Shackleton. Thorax 2020; 75:693–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oran DP, Topol EJ. Prevalence of asymptomatic SARS-CoV-2 infection: a narrative review. Ann Intern Med 2020; 173:362–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.St John RK, King A, de Jong D, Bodie-Collins M, Squires SG, Tam TW. Border screening for SARS. Emerg Infect Dis 2005; 11:6–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tan CC. SARS in Singapore – key lessons from an epidemic. Ann Acad Med Singap 2006; 35:345–349. [PubMed] [Google Scholar]
- 11.Dollard P, Griffin I, Berro A, et al. Risk assessment and management of COVID-19 among travelers arriving at designated U.S. airports, January 17–September 13, 2020. MMWR Morb Mortal Wkly Rep 2020; 69:1681–1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. World Health Organization. (2020). Considerations for implementing a risk-based approach to international travel in the context of COVID-19: interim guidance, 16 December 2020. World Health Organization. Available at: https://apps.who.int/iris/handle/10665/337858. License: CC BY-NC-SA 3.0 IGO. Accessed March 12, 2021. [Google Scholar]