Abstract
Objective:
To ascertain the level of psychological distress, using validated psychology tools, among British National healthcare workers (HCW) during the first wave of the Covid-19 crisis.
Methods:
A multi-centre, anonymized, all-comer staff survey across 3 hospitals in Lancashire, England during the Covid-19 first wave (April to June 2020), consisting of Patient Health Questionnaire (PHQ-9), Perceived Stress Scale-10 (PSS-10), Generalized Anxiety Disorder-7 (GAD-7), and Impact of Events Scale (IES-6).
Results:
Among 1113 HCW, median (IQR) PHQ-9, GAD-7, PSS-10, and IES-6 score was 7 (3 to 11), 6 (3 to 11), 19 (13 to 24), and 9 (5 to 14), respectively. Potential predictors of higher levels of psychological distress included living alone, disabled dependents, history of depression/anxiety, and being female.
Conclusions:
The study indicates a high prevalence of psychological distress during the acute Covid-19 period among HCW, identifies groups at risk and areas of future research.
Keywords: anxiety, Covid-19, depression, healthcare workers, mental health
Covid-19 has impacted healthcare on a scale not seen in our lifetimes and has affected the physical and psychological wellbeing of patients and the general population.1–6 Healthcare workers (HCW) have been at the forefront of the fight against Covid-19. Previous studies on the psychological impact on healthcare workers during the Severe Acute Respiratory Syndrome (SARS) virus outbreak in 2003–04 have shown a high prevalence of psychological distress among HCW.7–9 Since the onset of the Covid-19 pandemic, several studies, including ours, and systematic reviews have now reported on the impact of the pandemic on the mental health of healthcare workers worldwide.10–14 Studies show a high prevalence of psychological distress among healthcare workers, with levels of depression, anxiety, insomnia, stress, post-traumatic stress disorder (PTSD) and burnout in around a third of HCWs in some reports.10 There is considerable heterogeneity in study methodology including variation in the timing of the studies in relation to the pandemic, the use of different psychology assessment tools, and inclusion of non-physician and nursing staff. Furthermore, the vast majority of these studies were undertaken outside the United Kingdom. The National Health Service (NHS) is one of the largest employers in the world and has a workforce of 1.28 million in England alone (as of Jan 2020).15 Considering the size of the NHS workforce, not many studies have reported on the psychological distress levels among staff during Covid-19. Research on the impact of Covid-19 on the mental health of healthcare workers and the public is recommended by mental health experts and data gathered from such surveys will help inform planning for future such pandemics.16,17 A study from West Midlands, England conducted after the first wave, using psychology tools, reported a high prevalence of anxiety, depression, and PTSD among the healthcare workers in the region.18 We conducted a survey in the North-West of England during the peak of the first wave of Covid-19 using different psychology assessment tools looking at depression, stress, anxiety, and PTSD along with associated demographic variables. The first wave of Covid-19 in England lasted from March to May 2020. At the start of data collection (April 2nd, 2020), there were 4066 daily new cases in England (cumulative number 40,885) and 731 daily deaths.19 The peak of first wave in England in terms of daily death toll was 6 days into the study period (April 8th, 2020) with 973 deaths and in terms of daily cases it was 20 days into the study period (April 22nd, 2020) with 4803 new cases. At the end of study period (June 8th, 2020) there were 994 daily cases (cumulative number 226,857) and 111 daily deaths (cumulative number 34,828). Our aim was to describe the burden of depressive symptoms, anxiety, stress, and PTSD during the very peak of the first wave across three NHS Hospital Trusts in Lancashire in North-West England, UK. Also, we endeavored to identify the subgroups at the highest risk of developing adverse mental health sequelae. In this article, we present the results of the survey.
METHODS
Study Design and Participants
A multi-centre, cross-sectional health care staff survey was conducted across three large hospitals in the North West of England from April 02, 2020 to June 08, 2020. The survey was also distributed to adjacent primary care practices in Lancashire. The survey was sent to employees of the three NHS Foundation Trusts via the hospital communications teams in the form of an explanatory email containing a web-based link to the survey. The overall response rate was estimated at 5%. The survey made it clear to the participant that all responses were voluntary and anonymized and that should a participant feel suicidal then they should seek immediate medical attention. Responses to all questions were required to complete the survey hence there were no missing responses to any of the questions. The survey was deemed as posing minimal risk to participants and, as such, did not require written consent. In the cover information provided with the link and on the front page of the survey, the participants were given the following information: the names of individuals and organizations performing the survey with the contact details, explanation that the survey is anonymous and voluntary and that the survey data will be kept secure, and confidentiality will be ensured. Present study did not require National Health Service Research Ethics Committee review as confirmed by the Health Research Authority decision tool.
Outcomes
Participant characteristics were determined in this survey (age, gender, ethnicity, living status, work setting and position, pre-existing depression/anxiety, children/elderly/disabled occupant at home, and previous isolation due to Covid-19). The main outcomes were to assess the prevalence and predictive factors for depression, stress, anxiety, and PTSD among HCW during the peak of Covid-19. Validated assessment tools were used. The Patient Health Questionnaire (PHQ-9; range, 0 to 27),20 the Perceived Stress Scale (PSS-10),21 the Generalized Anxiety Disorder (GAD-7; range, 0 to 21),22 and the Impact of Event Scale (IES-6)1,23 were used respectively to assess these outcomes. The total scores of these measurement tools were interpreted as medians and as following categories: PHQ-9, normal (0 to 4), mild (5 to 9), moderate (10 to 14), moderately severe (15 to 19), and severe (20 to 27) depression; PSS-10, low (0 to 13), moderate (14 to 26), and severe (27 to 40), a higher score indicates a higher level of stress; GAD-7, normal (0 to 4), mild (5 to 9), moderate (10 to 14), and severe (15 to 21) anxiety; IES-6 was assessed on a linear scale.
Statistical Analysis
Categorical variables were presented as frequencies and percentages. The normality assumption for continuous variables was evaluated with the Shapiro–Wilk test. Non-parametric data were presented as medians with interquartile ranges (IQRs) and compared with Mann–Whitney U tests or Kruskal–Wallis tests as appropriate. Post hoc pairwise tests using the Bonferroni correction were used to determine differences in scores in different professions. We used proportional odds model to assess outcomes recorded on ordinal scale since naïve dichotomization of the full ordinal scale leads to loss of information and efficiency while analyzing such outcomes. The proportional odds assumptions were met for depression and stress regression models whereas they were violated for anxiety. Therefore, a multivariable binary logistic regression analysis was performed with one category of GAD-7 between 0 and 9 and the other category with GAD-7 between 10 and 21 to determine potential risk factors for significant symptoms of anxiety. The association between risk factors and these outcomes are presented as ORs and 95% CI. For PTSD, multiple linear regression was used with the total IES-6 score as the outcome. There was no serious violation of the assumptions in any of the above-mentioned regression model. No interactions were considered. Internal consistency was assessed using Cronbach's alpha and McDonald's omega. Convergent validity was assessed by calculating Spearman's rho pairwise between PHQ-9, GAD-7, PSS-10, and IES-6. For all analyses, a 2-sided P < 0.05 was considered statistically significant. All data were processed using StataMP 16.1 software (Stata Corp., College Station, TX).
RESULTS
Characteristics of the Respondents
A total of 1113 respondents completed the survey (estimated response rate of 5%). Of 1113 participants, there were 110 (10%) physicians, 268 (24%) nurses, 354 (32%) allied health professionals (AHP), 59 (5%) ancillary staff, and 322 (29%) employees working in administration and management positions. The characteristics of the respondents are presented in Table 1 and e-Table 1.
TABLE 1.
Baseline Characteristics
| Parameter | TotalN, 1113 |
| Male gender | 192 (17.3) |
| Female | 915 (82.2) |
| Prefer not to say | 6 (0.5) |
| Age (yrs) | 48 (36–54) |
| Years in the NHS (yrs) | 15 (5–25) |
| Primary care | 105 (9.4) |
| Living alone/single | 267 (24.0) |
| Ethnicity—BAME | 99 (8.9) |
| Children at home | 591 (53.1) |
| Elderly dependent | 54 (4.9) |
| Disabled dependent | 70 (6.3) |
| Previous isolation | 320 (28.8) |
| Direct patient contact | 688 (61.8) |
Results are presented as n (%) or median (IQR).
Occupational Category-Related Differences
The majority of physicians were men (60%) whereas all other groups were predominantly female. Other statistically significant differences across all five occupational groups were noted with regard to age (doctors being the youngest), years in NHS employment, ethnicity (BAME [Black, Asian, and Minority Ethnic] staff most prevalent among physicians), prior isolation (most frequent among physicians) and direct patient caregivers (least prevalent among administration/management and ancillary staff) (e-Table 2). e-Tables 3 and 4 show differences in the scores in relation to other baseline characteristics.
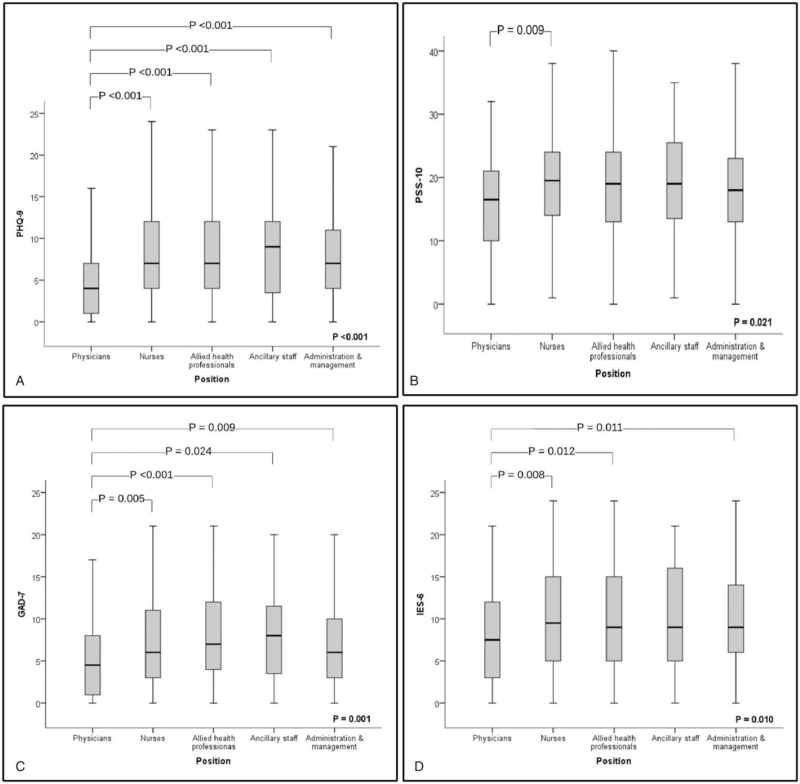
DEPRESSION
Median PHQ-9 scale score was 7 (3 to 11) and PHQ-9 scores of 5 or more were present in two-thirds of the respondents (67%) with a total of 5% showing signs of severe depression (e-Table 2). A significant difference in PHQ-9 was noted based on occupational category (P < 0.001): doctors had a lower median score than the other four positions (each adj. P < 0.001). Differences between PHQ-9 scores of nurses, AHP, admin, and ancillary staff were not statistically significant (Fig. 1).
FIGURE 1.
Boxplots of outcome scores according to the position. A: PHQ-9; B: PSS-10; C: GAD-7; D: IES-6. Kruskal–Wallis and Bonferroni corrected pairwise comparisons are reported. The thick line in the middle is the median. The top and bottom box lines show the first and third quartiles. The whiskers show the maximum and minimum values.
An ordinal logistic regression analysis was conducted to investigate the relationship between severity of depression and baseline covariates based on 1077 responses (after exclusion of 36 responses with “Prefer not to say” selection in gender and pre-existing depression questions). Physicians had lower odds of more serious depression than admin/management staff. Those with children at home also had lower odds of more severe depression than those with no children at home. On the other hand, odds ratio suggested a more severe PHQ-9 outcome in those living alone compared to living with partner, disabled dependent at home versus no disabled dependent, pre-existing depression versus no prior diagnosis of depression. An increase in NHS experience (expressed in years) was associated with a decrease in the odds of more severe stage of depression (Table 2 and e-Table 5).
TABLE 2.
Risk Factors for Higher Category of Depression Identified by Ordinal Logistic Regression Analysis—PHQ9
| 95% Confidence Interval | ||||
| Parameter | Odds Ratio | Lower | Upper | P |
| Position—ancillary | 1.045 | 0.615 | 1.775 | 0.870 |
| Position—AHP | 0.698 | 0.478 | 1.020 | 0.063 |
| Position—nurse | 0.939 | 0.627 | 1.406 | 0.759 |
| Position—doctor | 0.284 | 0.159 | 0.507 | <0.001 |
| Reference category—position admin/management | 1 | – | – | – |
| Living status—alone | 1.574 | 1.201 | 2.063 | 0.001 |
| Reference category—living status—partner | 1 | – | – | – |
| Children at home—yes | 0.786 | 0.625 | 0.990 | 0.041 |
| Reference category—children at home—no | 1 | – | – | – |
| Disabled—yes | 2.100 | 1.323 | 3.335 | 0.002 |
| Reference category—disabled—no | 1 | – | – | – |
| Pre-existing depression—yes | 2.911 | 2.257 | 3.754 | <0.001 |
| Reference category—pre-existing depression—no | 1 | – | – | – |
| Patient facing—yes | 1.595 | 1.149 | 2.215 | 0.005 |
| Years in NHS—1-yr increase | 0.987 | 0.974 | 0.999 | 0.044 |
The common odds were estimated in an ordinal logistic–regression model and indicate the increase in odds of moving from a lower category of PHQ-9 to a higher one relative to the reference category. N = 1077 cases used in estimation. NHS, National Health Service.
Stress
Total median (IQR) PSS-10 for the entire population was 19 (13 to 24) which represents moderate stress (e-Table 2). Low, moderate, and severe stress levels were present in 27%, 60%, and 14%, respectively. Median PSS-10 scores differed statistically significantly between the five analyzed occupational groups (P = 0.021). Post hoc pairwise tests showed a statistically significant difference only between doctors and nurses (adj. P = 0.009) (Fig. 1).
Based on ordinal logistic regression the independent predictors associated with decreased odds of higher category of stress were AHP, physician, and nurse positions compared to administrative/management and age whereas BAME ethnicity compared to white, living with elderly and disabled at home, pre-existing depression, and patient-facing role were associated with increased odds of higher category of stress (Table 3 and e-Table 6).
TABLE 3.
Risk Factors for Higher Category of Stress Identified by Ordinal Regression—PSS-10
| 95% Confidence Interval | ||||
| Parameter | Odds Ratio | Lower | Upper | P |
| Position—ancillary | 1.005 | 0.848 | 1.190 | 0.957 |
| Position—AHP | 0.833 | 0.737 | 0.940 | 0.003 |
| Position—nurse | 0.877 | 0.770 | 0.999 | 0.048 |
| Position—doctor | 0.692 | 0.578 | 0.827 | <0.001 |
| Reference category—position admin/management | 1 | – | – | – |
| Ethnicity—other | 1.191 | 1.026 | 1.383 | 0.022 |
| Reference category—Ethnicity—white | 1 | – | – | – |
| Elderly at home—yes | 1.197 | 1.013 | 1.413 | 0.034 |
| Reference category—Elderly—no | 1 | – | – | – |
| Disabled—yes | 1.198 | 1.030 | 1.393 | 0.019 |
| Reference category—Disabled—no | 1 | – | – | – |
| Pre-existing depression—yes | 1.272 | 1.175 | 1.378 | <0.001 |
| Reference category—pre-existing depression—no | 1 | – | – | – |
| Patient facing—yes | 1.209 | 1.090 | 1.342 | <0.001 |
| Reference category—patient facing—no | 1 | – | – | – |
| Age—1-yr increase | 0.992 | 0.988 | 0.996 | <0.001 |
The common odds were estimated in an ordinal logistic–regression model and indicate the increase in odds of moving from a lower category of PSS-10 to a higher one relative to the reference category. N = 1077 cases used in estimation.
Anxiety
Median (IQR) anxiety assessed with GAD-7 scale was 6 (3 to 11) (e-Table 2). Moderate to severe anxiety (GAD-7 > 9) was present in 30%. Median GAD-7 score differed statistically significantly between five occupational groups (P = 0.001). Doctors had lower median score than nurses (adj. P = 0.005), AHP (adj. P < 0.001), ancillary staff (adj. P = 0.024), and administrative/management staff (adj. P = 0.009) (Fig. 1).
Binary logistic regression indicated that position, living status, disabled at home, pre-existing depression, and patient-facing roles were significant predictors of having a GAD-7 result of more than 9. The other eight predictors namely setting (primary vs secondary), gender, ethnicity, children at home, elderly at home, prior isolation, age, and NHS experience were not significantly associated with GAD-7 scores. The odds ratio for physicians was significantly lower compared to administration/management. Other positions were not statistically significant compared to reference position (Table 4 and e-Table 7).
TABLE 4.
Risk Factors for GAD-7 Result More Than or Equal to 10 Identified by Multivariable Regression Analysis
| 95% Confidence Interval | ||||
| Parameter | Odds Ratio | Lower | Upper | P |
| Position—ancillary | 1.018 | 0.528 | 1.963 | 0.958 |
| Position—AHP | 0.658 | 0.401 | 1.080 | 0.098 |
| Position—nurse | 0.725 | 0.430 | 1.224 | 0.229 |
| Position—doctor | 0.264 | 0.119 | 0.586 | 0.001 |
| Reference category—position admin/management | 1 | – | – | – |
| Living status—alone | 1.479 | 1.072 | 2.040 | 0.017 |
| Reference category—living status—partner | 1 | – | – | – |
| Disabled—yes | 1.820 | 1.044 | 3.170 | 0.035 |
| Reference category—disabled—no | 1 | – | – | – |
| Pre-existing depression—yes | 2.454 | 1.826 | 3.298 | <0.001 |
| Reference category—pre-existing depression—no | 1 | – | – | – |
| Patient facing—yes | 2.370 | 1.530 | 3.671 | <0.001 |
| Reference category—patient facing—no | 1 | – | – | – |
N = 1077 cases used in estimation; Chi-square 6.264, df = 8, P = 0.618; R-squared 0.129; correct predictions: 72.3%.
IES-6
The median (IQR) IES-6 result was 9 (5 to 14) (Table 2). The median IES 6 score differed statistically significantly between the five occupational groups (P = 0.010). Post hoc pairwise tests using the Bonferroni correction revealed that doctors had lower median score than all other four positions (each adj. P < 0.001) and the differences between PHQ-9 scores of nurses, AHP, admin, and ancillary staff were not statistically significant (Fig. 1).
Multiple linear regression was performed utilizing IES-6 as diagnostic tool for PTSD to determine if IES-6 scores could be predicted as a function of baseline characteristics. Respondents’ total IES-6 decreased by 3.067 (P < 0.001) for physicians compared to administration/management (reference) and decreased by 1.401 (P = 0.016) for AHP compared to the reference group. Additionally, pre-existing depression (B = 2.302, P < 0.001) and patient-facing role (B = 1.706, P = 0.001) were significant predictors. Table 5 and e-Table 8 summarize the results of the multiple linear regression model.
TABLE 5.
Risk Factors for Higher Result of IES-6 Identified by Linear Regression-IES-6
| 95% B Confidence Interval | |||||||
| Parameter | B | SE | Lower | Upper | β | t | P |
| Constant | 9.193 | 1.160 | 6.917 | 11.470 | 7.925 | <0.001 | |
| Position—ancillary | −0.607 | 0.811 | −2.198 | 0.984 | −0.024 | −0.749 | 0.454 |
| Position—AHP | −1.401 | 0.580 | −2.539 | −0.263 | −0.115 | −2.415 | 0.016 |
| Position—nurse | −0.901 | 0.621 | −2.120 | 0.318 | −0.068 | −1.450 | 0.147 |
| Position—doctor | −3.067 | 0.857 | −4.748 | −1.386 | −0.162 | −3.580 | 0.000 |
| Reference category—position admin/management | 0 | 0 | – | – | – | – | – |
| Pre-existing depression—yes | 2.302 | 0.381 | 1.554 | 3.050 | 0.185 | 6.041 | <0.001 |
| Reference category—pre-existing depression—no | 0 | 0 | – | – | – | – | – |
| Patient facing—yes | 1.706 | 0.497 | .0730 | 2.682 | 0.146 | 3.429 | 0.001 |
| Reference category—patient facing—no | 0 | 0 | – | – | – | – | – |
The B coefficients indicate how much a dependent variable (total IES 6) changes per each unit variation of the independent variable, taking into account the effect of the other independent variables in the model. For categorical variables, B coefficients represent the effect of moving from the reference category to another. N = 1077 cases used in estimation; F(16,1060) = 5.676; P < 0.001; R-squared 0.079.
Reliability and Validity
As shown in e-Table 9, McDonald's omega and Cronbach's alpha ranged from 0.88 to 0.92 indicating an excellent internal consistency. PHQ-9, GAD-7, PSS-10, and IES-R were statistically significantly correlated between each of them indicating adequate convergent validity (Spearman's rho between 0.62 and 0.79 for all comparisons, P < 0.001).
DISCUSSION
The results of the multi-centre, all-comer survey of 1113 staff working in NHS hospitals in Lancashire shows a marked prevalence of psychological distress among staff during the peak of the Covid-19 pandemic in the region. Features suggestive of depression (67%), moderate to severe anxiety (30%), and elevated levels of stress (moderate–severe) (73%) were noted among the majority of staff. Of all the occupational groups, physicians appear to be the group with the least psychological distress. The survey provides a valuable insight into the psychological wellbeing in healthcare staff during the acute stage of a pandemic and the findings are likely to be representative of the level of psychological distress in general across the NHS during the peak Covid-19 period.
The results are similar to the findings in China.24 However, the study in China was done solely on nurses and physicians. A similar study in Italy found a lower level of psychological distress compared to our survey.25 A meta-analysis of studies on the mental health of HCW during Covid-19 showed a prevalence of anxiety of 23.2% and depression of 22.8%.13 The meta-analysis was for studies conducted in the earlier phase of Covid-19 and is similar to the findings in Italy. Subsequent systematic reviews have reported on a multitude of studies with reported prevalence of depression ranging from 13.5% to 44.7%, anxiety from 12.3% to 35.6%, PTSD from 7.4% to 37.4%, insomnia from 33.8% to 36.1%, and stress from 5.2% to 32.9%.14 Our survey suggests the HCWs in the region are facing psychological distress at levels at the higher end of the range in the systematic reviews, perhaps linked to the timing of the survey during the peaking of the first wave in the region.
The current survey highlights several key findings of the five occupational groups studied, physicians had the lowest median scores for all questionnaires. The physician group had a median score of 4 on the PHQ-9. Exactly why physicians are less psychologically distressed than other HCW is unclear. To date, a number of studies during Covid-19 have reported similar findings with physicians showing less psychological distress than nurses despite both being frontline.10,12,13 It remains to be seen if post-traumatic stress emerges at a time remote from the pandemic in this group of HCW. Nurses who are also front-facing showed increased distress and the difference in demographics between the two groups (eg, majority of nurses were females as compared to majority of physicians who were males) might have contributed to the differing distress levels. Females have shown greater levels of psychological distress compared to males in a number of studies, including this survey. Furthermore, physicians tend to have greater control of whether or not they have patient contact and for how long (especially in an inpatient setting) and this might also be a contributory factor. The bulk of outpatient work was changed to remote consultations and a lot of elective work was cancelled, perhaps resulting in less anxiety about patient exposure. Whether seniority in physician status and physician training had any influence on “mental hardiness and readiness” was not assessed but might be a contributory factor. All other occupational groups, including ancillary and administration staff, had higher scores than physicians in all four questionnaires. Studies, such as the one from Wuhan, which primarily focus on the physicians, nurses, and AHP-considered the “frontline” staff are likely to miss these other important groups. The lack of focus on these groups also raises the question as to whether they are prone to get side lined in support provision. Furthermore, as they are not always directly involved in dealing with patients and do not have clinical training, they may have less psychological resilience in dealing with a major disease outbreak.
Particularly worrying was the finding of moderate to severe stress levels in almost three-quarters (73%) of the survey participants with a median PSS-10 score of 19.13–24 Whether the persistent presence of Covid-19 and the possibility of a second wave will convert the acute stress reaction to a more chronic form and, hence, increase the risk of staff burnout remains to be seen. However, lessons from previous large-scale outbreaks have demonstrated higher levels of long-term psychological distress well beyond the actual disease outbreak.26
The survey also highlights certain groups who are at higher risk of psychological distress. The majority of participants in the survey were female (82%). Females had higher prevalence of depression, anxiety, and stress compared to their male counterparts, in keeping with the trends in the general population.27 Younger HCW (<40 years) also had higher prevalence of depression, stress, and anxiety compared to their older counterparts. Older age, and the associated experiences of withstanding previous adversity, may be contributing to the latter group's relative resilience. A recent meta-analysis of studies looking at psychological distress during infectious disease outbreaks has shown younger age as a risk factor for psychological distress among HCW.28 Participants who live alone had significantly higher prevalence of psychological distress compared to those living with a companion. A possible reason for this observation could be the lack of emotional support at home given the restrictions on inter-household social interaction imposed by lockdown measures. Concern for the health of family members has previously been shown to be associated with increased psychological distress during the SARS outbreak.29 As evidenced in this survey, the presence of a disabled family member significantly increased the risk of more severe depression, anxiety, and stress, and the presence of elderly family members increased the risk of the level of stress. Whether the Covid-19 outbreak per se affects the level of psychological distress in staff with disabled family members or those living alone or whether the latter are independent risk factors for psychological distress anyway is unknown and is a limitation of the survey findings. Working in secondary care and in direct patient contact were two other factors associated with increased depression/stress and stress/anxiety, respectively. During the Covid-19 outbreak, primary services have been mainly conducted over the phone with physical patient contact only where strictly necessary. Although secondary care services have also been restricted, acute presentations have continued and the fear of the most critically unwell Covid-19 patients coming into hospital might be a factor contributing to the increased anxiety in secondary care. A particularly vulnerable group were the participants with pre-existing depression and anxiety. They report more severe depression, anxiety, and stress. Thus, the survey highlights several groups of HCW who might require “extra” attention in terms of mental health support and includes females, those with disabled or elderly family members, the younger HCW population, those working in direct patient care and those with pre-existing mental health issues. At the same time, it also highlights the importance of not overlooking staff in administration and ancillary staff who are also experiencing high levels of psychological distress “behind the scenes.”
Covid-19 poses an increased risk of morale injury and mental health problems in healthcare workers.30 Managing one's psychological health and psychological wellbeing at this time is as important as managing one's physical health.31 In a previous paper summarizing our findings of a much smaller, department based survey, we have discussed the urgent need for mental health support and early recognition of psychological distress among HCW and various factors that contribute to increased psychological stress during such major disease outbreaks including interpersonal isolation, fear of contagion, quarantine, stigma, concern for family, and non-infectious specialty workers being drafted into infectious wards.11,26 We have acted on our current survey by disseminating the results to the respective NHS Trusts for action on enhancing support services for staff. Examples include, senior staff members attending psychological first aid courses, sessions for staff on psychological support, and recognition of psychological distress by trained counsellors, a prominent web link on the Trust intranet, detailing support services available for all staff who need help and are feeling psychologically distressed. The exact measures put in place and the recommended measures are beyond the scope of this paper. The purpose of this paper is to bring to the forefront an analysis of the psychological status of HCW during the peak of the pandemic to enable specialist teams in occupational health and staff wellbeing across the NHS to increase and adjust their support services and provide extra support to certain vulnerable groups.
Limitations
This survey represents a picture of the level of psychological distress during the peak of Covid-19 among more than 1000 NHS workers in a large area across the North-West of England. However, there are limitations. The response rate was low, there might have been undersampling of certain groups (physicians and nurses). As our study involved self-reporting by participants there is a considerable risk of response bias. Furthermore, the survey did not allow to determine the temporal changes in levels of depression, anxiety, stress, and PTSD. Despite the limitations, the findings are still likely to give a “representative snapshot” of the NHS workforce as a whole at the time.
CONCLUSION
The present survey of a large number of HCW across multiple NHS trusts in the North-West of England shows a high prevalence of psychological distress among staff during the peak of the Covid-19 pandemic. The results suggest certain staff characteristics and groups with increased risk of psychological distress. The survey results should provide a valuable insight into the mental health status of staff across the NHS and better enable policy makers, clinical staff, and managers to enhance the mental health support services available for all staff. The cumulative data gathered on this topic from this, and multiple other studies will help better prepare the NHS and other healthcare systems for future outbreaks of a similar scale. Future areas of research should focus on longer-term follow-up and data collection to assess the chronic, psychological sequelae of Covid-19 on HCW as well as undertaking studies on at-risk groups. Furthermore, future research and planning should focus on optimal methods and timing of training of future HCW in mental preparedness, resilience, and psychological first aid.
Supplementary Material
Footnotes
The authors report no funding and conflicts of interest.
Role of authors: Conceptualization: TC; Survey design: TC, MD, SW, JS; Data collection, analysis, and supervision: MD, RT; Manuscript preparation: TC, MD, HKA; Manuscript review and editing: TP, OA, AW, AN, AA, GS, SK, GG, GGal, JE, RM, BP, SC; Project administration/logistics: GS, KM, JG, SC.
Supplemental digital contents are available for this article.
Clinical significance: The report indicates high prevalence of depression, anxiety, stress, and post-traumatic psychological distress among British healthcare workers during the Covid-19 first wave and highlights at-risk groups. The findings could help guide policymaking to prepare the workforce for future pandemics in terms of psychological distress recognition and provision of psychological support.
REFERENCES
- 1.Wang C, Pan R, Wan X, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun 2020; 87:40–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhu S, Wu Y, Zhu CY, et al. The immediate mental health impacts of the COVID-19 pandemic among people with or without quarantine managements. Brain Behav Immun 2020; 87:56–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nobles J, Martin F, Dawson S, Moran P, Savovic J. The potential impact of COVID-19 on mental health outcomes and the implications for service solutions. 15 April 2020. Available at: https://arc-w.nihr.ac.uk/research-and-implementation/covid-19-response/potential-impact-of-covid-19-on-mental-health-outcomes-and-the-implications-for-service-solutions (accessed December 10, 2020). [Google Scholar]
- 4. Ipsos MORI. Covid-19 and Mental Wellbeing. Available at: https://www.ipsos.com/ipsos-mori/en-uk/Covid-19-and-mental-wellbeing. Accessed December 10, 2020. [Google Scholar]
- 5.Ueda M, Stickley A, Sueki H, Matsubayashi T. Mental Health Status of the General Population during the COVID-19 Pandemic: A Cross-sectional National Survey in Japan. Psychiatry Clin Neurosci 2020; 74:505–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. The Academy of Medical Sciences. Available at: http://www.acmedsci.ac.uk/COVIDmentalhealthsurveys (accessed December 10, 2020). [Google Scholar]
- 7.Maunder R. The experience of the 2003 SARS outbreak as a traumatic stress among frontline healthcare workers in Toronto: lessons learned. Philos Trans R Soc Lond B Biol Sci 2004; 359:1117–1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maunder R, Hunter J, Vincent L, et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ 2003; 168:1245–1251. [PMC free article] [PubMed] [Google Scholar]
- 9.McAlonan GM, Lee AM, Cheung V, et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry 2007; 52:241–247. [DOI] [PubMed] [Google Scholar]
- 10.Cabarkapa S, Nadjidai SE, Murgier J, Ng CH. The psychological impact of COVID-19 and other viral epidemics on frontline healthcare workers and ways to address it: a rapid systematic review. Brain Behav Immun Health 2020; 8:100144.DOI 10.1016/j.bbih.2020.100144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choudhury T, Debski M, Wiper A, et al. Covid-19 pandemic: looking after the mental health of our healthcare workers. J Occup Environ Med 2020; 62:e373–e376. [DOI] [PubMed] [Google Scholar]
- 12.Moitra M, Rahman M, Collins PY, et al. Mental health consequences for healthcare workers during the COVID-19 pandemic: a scoping review to draw lessons for LMICs. Front Psychiatry 2021; 12:602614.DOI 10.3389/fpsyt.2021.602614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pappa S, Ntella V, Giannakas T, et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun 2020; 88:901–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sanghera J, Pattani N, Hashmi Y, et al. The impact of SARS-CoV-2 on the mental health of healthcare workers in a hospital setting – a systematic review. J Occup Health 2020; 62:e12175.DOI 10.1002/1348-9585.12175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. NHS_Digital. NHS Workforce Statistics. 2020. Available at: https://digital.nhs.uk/data-and-information/publications/statistical/nhs-workforce-statistics/january-2020. Accessed December 10, 2020. [Google Scholar]
- 16.Holmes EA, O’Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 2020; 7:547–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hotopf M, Bullmore E, O’Connor RC, Holmes EA. The scope of mental health research in the COVID-19 pandemic and its aftermath. Br J Psychiatry 2020; 217:540–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wanigasooriya K, Palimar P, Naumann DN, et al. Mental health symptoms in a cohort of hospital healthcare workers following the first peak of the COVID-19 pandemic in the UK. BJPsych Open 2020; 7:e24.DOI 10.1192/bjo.2020.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. The Official UK Government Website for Data and Insights on Coronavirus (COVID-19). Available at: https://coronavirus.data.gov.uk (accessed May 5, 2021). [Google Scholar]
- 20.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA 1999; 282:1737–1744. [DOI] [PubMed] [Google Scholar]
- 21.Cohen S, Williamson G. Spacapan S, Oskamp S. Perceived stress in a probability sample of the United States. Sage, The Social Psychology of Health. Newbury Park, CA: 1988. [Google Scholar]
- 22.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006; 166:1092–1097. [DOI] [PubMed] [Google Scholar]
- 23.Thoresen S, Tambs K, Hussain A, Heir T, Johansen VA, Bisson JI. Brief measure of posttraumatic stress reactions: impact of Event Scale-6. Soc Psychiatry Psychiatr Epidemiol 2010; 45:405–412. [DOI] [PubMed] [Google Scholar]
- 24.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 2020; 3:e203976.DOI 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rossi R, Socci V, Pacitti F, et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw Open 2020; 3:e2010185.DOI 10.1001/jamanetworkopen.2020.10185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maunder RG, Lancee WJ, Balderson KE, et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis 2006; 12:1924–1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. WHO. Gender and Women's Mental Health. 2020. Available at: https://www.who.int/mental_health/prevention/genderwomen/en/. Accessed December 10, 2020. [Google Scholar]
- 28.Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ 2020; 369:m1642.DOI 10.1136/bmj.m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wong TW, Yau JK, Chan CL, et al. The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. Eur J Emerg Med 2005; 12:13–18. [DOI] [PubMed] [Google Scholar]
- 30.Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ 2020; 368:m1211.DOI 10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]
- 31. WHO. Mental Health and Psychosocial Considerations During the COVID-19 Outbreak. 2020. WHO reference number: WHO/2019-nCoV/MentalHealth/2020.1 Available at: https://www.who.int/publications/i/item/WHO-2019-nCoV-MentalHealth-2020.1. Accessed December 10, 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.