Abstract
Objective:
To investigate the epidemiological characteristics of human infection with corona virus disease 2019 (COVID-19) in Moscow, Lima, Kuwait, and Singapore to analyze the effects of climate factors on the incidence of COVID-19.
Methods:
Collect the daily incidence of COVID-19 and related climate data in four areas, construct a negative binomial regression model, and analyze the correlation between the incidence of COVID-19 and meteorological factors.
Results:
AH was the climate factor affecting the incidence of COVID-19 in Moscow, Lima, and Singapore; Ta and RH were the climate factors affecting the incidence of COVID-19 in Kuwait.
Conclusions:
The incidence of COVID-19 in four areas were all associated with the humidity, and climate factors should be taken into consideration when epidemic prevention measures are taken, and environment humidification may be a feasible approach to decrease COVID-19 virus transmission.
Keywords: absolute humidity, atmospheric pressure, climate factor, COVID-19, PM2.5
Abbreviations: AH, absolute humidity, CO, carbon monoxide, COVID-19, corona virus disease 2019, MERS-CoV, Middle East Respiratory Syndrome, O3, Ozone, PM10, particulate matter with particle size below 10 μm, PM2.5, Fine Particulate Matter, RH, relative humidity, SARS, Severe Acute Respiratory Syndrome, SO2, sulfur dioxide, Ta, average temperature, Td, dew Point, WS, wind speed
Corona virus disease 2019 (COVID-19) broke out on a global scale, spreading rapidly and widely, with outbreaks occurring in regions with various climate types. It is currently believed that COVID-19 can be spread in the air in the form of droplets or aerosols.1 Thus, climatic factors may have a certain impact on the spread of COVID-19, but the specific impact is still unclear. Studies on influenza have shown that temperature and humidity are somewhat related to the spread of influenza. Specifically, lower absolute humidity (AH) is especially conducive to the survival and spread of influenza viruses.2–4 Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS-CoV) are also coronaviruses. Studies have also show that meteorological factors have a certain influence on the spread of both. The spread of SARS related to appropriate temperature, relative humidity (RH), and has a seasonal trend.5 Lower RH and high temperature enhance the transmission of MERS-CoV among individuals.6 Therefore, it is necessary to study the relationship between COVID-19 and climate factors.
An earlier study show that temperature is an important factor on the infectivity of human coronavirus.7 Chan et al's results8 found that when the dried SARS virus at temperatures of 22 to 25°C and RH of 40% to 50%, the virus on smooth surfaces retained its viability for over 5 days. However, virus viability was rapidly lost at higher temperatures and higher RH, the low temperature and low humidity environment may facilitate SARS coronavirus's stability of transmission. A study found that the spread of COVID-19 in Hubei has a significant negative correlation with daily average temperature and RH, and there is a significant interaction between the two.9 Goswami et al10 found that the interaction between average daily temperature and RH affects the incidence of COVID-19. However, inconsistencies in the results among Indian states led the authors to conclude that further analyses of the impact of other meteorological factors are needed. Another study of 10 provinces in China show that the relationship between temperature and COVID-19 is mostly positive for Hubei, Hunan, and Anhui, while mostly negative for Zhejiang and Shandong provinces, and other provinces are showing the mixed trends. These differences can be explained by the differences in the number of cases, temperature, and the province's overall hospital facilitations.11 Some result is contrary that temperature may not be related to the COVID-19's transmission. Iqbal et al's results12 show that increase in temperature did not play any significant role in containing the COVID-19 spread in Wuhan at temperature range between 3 and 21°C. Dogan et al's study of New Jersey in the United States13 shows that temperature may not be the only determinant of COVID-19. Therefore, the evaluation of the impact of temperature on COVID-19 should be treated with caution. The epidemic in the southern hemisphere after the beginning of winter has made the problem more complicated, the role of temperature needs to be further evaluated. An earlier study of all of the countries affected by COVID-19 revealed that average temperature is negatively correlated with the spread of COVID-19, while precipitation is positively correlated with the spread of COVID-19.14 A study showed that the fall in cases due to rising humidity can be effective in COVID-19's transmission.15 Ahmadi et al's results16 show that the average disease transmission rate in humid provinces is higher than that in other areas in Iran. However, the humidity has an inverse relationship with disease infection rates in regions with droughts.
Regarding the impact of humidity on the COVID-19 epidemic, many studies have adopted RH, while AH is less involved in these studies. Deyle et al's results17 show that low AH promotes the spread of influenza when temperature is low, and AH is a better predictor for influenza. Although there is less studies on the relationship between AH and COVID-19, there are few study data still show that AH has a possible impact on the COVID-19 virus. Ma et al's results18 show that AH may be one important factor affecting the COVID-19 mortality. The role of AH in the spread of COVID-19 is necessary. AH is a value that cannot be directly measured, it is inconvenient to obtain, and this may be one of the reasons why AH is less involved in many studies.
Research has also shown that there is a significant relationship between air pollution and COVID-19 infection. Air quality indicators such as atmospheric Fine Particulate Matter (PM2.5) with a diameter of less than 2.5 are important predictors of confirmed COVID-19,19 hence it is necessary to estimate the impact of PM 2.5 incidence on exposed populations in almost every country through epidemiological and experimental studies.20 In another study, NO2 and PM 10 had also showed possible correlations with COVID-19 cases and deaths.21 Many studies found a relationship between climate and air pollution, including temperature, wind speed and humidity, and changes in climate may have important impacts on PM2.5 concentrations. PM2.5 ordinarily concentrations decreases as temperature increases, and changes in wind speed and AH also had appreciable effects on it.22,23 Another study showed that particulate matter with particle size below 10 μm (PM10) also showed negative association with RH and positive with wind speed and temperature.24 Therefore, it is necessary to comprehensively consider the impact of climate and air quality on the COVID-19 epidemic.
At present, many studies have found that the spread of COVID-19 is related to climatic factors. However, due to the complex and different environmental factors in which the epidemic occurs, there is certain heterogeneity in the results. Notably, the regional impact of global climate varies by region, and climates also vary at different latitudes and altitudes. With the epidemic's progression, the outbreak of COVID-19 has appeared in both dry and low-temperature regions and humid and high-temperature regions. Therefore, it is necessary to conduct an in-depth analysis of the impact of climatic factors on COVID-19 in different parts of the world. Comparing data across different climates will help shed light on the similarities and differences in which varying climates affect the spread of COVID-19 and how different climates in endemic areas may lead to different conclusions. For example, an earlier study found that precipitation is an important factor in the spread of the virus. As daily precipitation increased by 1 in., the number of sick patients increased by 56.01 people/day, leading to suggestions that health services or social isolation protocols should be altered in accordance with precipitation patterns.14 However, the outbreaks in Kuwait and other areas with dry climates and very little rainfall in the Middle East and other regions such as Peru's capital (known as the “rainless capital”) seem to challenge this research. According to the cases data from the Johns Hopkins University Center for Systems Science and Engineering,25 and the world climate zones by Balasubramanian,26 as of October 1, 2020, the areas most severely affected by the global pandemic are mainly concentrated in tropical wet or moist environments, tropical dry environments, and temperate moist environments. Our present study examined similarities and differences in the impact of meteorological factors on the incidence of COVID-19 in four COVID-19 endemic areas with very different climate types (ie, Moscow, Lima, Kuwait, and Singapore). These areas were selected because they are differentially situated in the northern (ie, Moscow and Kuwait) and southern hemispheres (ie, Lima), as well as near the equator (ie, Singapore), and for the varying characteristics of their climates, the climate in Moscow is classified as warm humid continental climate by the Köppen-Geiger system with short warm summers and long cold winters, and the Köppen-Geiger climate classification in Singapore is tropical rainforest climate with no distinctive seasons, uniform temperature, and high humidity. The climate in Kuwait is a desert climate with extremely hot summers and mild winters, there is virtually no rainfall during the year. Lima is also considered to have a desert climate, and the difference with Kuwait is that due to the characteristics of the ocean area, Lima can maintain a certain humidity,27–31 they have different geographical and location climatic status to examine the COVID-19 epidemic variability facing different climatic environments. Another reason related to the similarity in the characteristic of population migration. They serve as the political, economic, cultural, and scientific center of their respective countries, and have more visited with the large hub in the world air network. Furthermore, a similar ratio of total confirmed cases to a total population is not over until October 1, 2020 (about 1.0–1.6%).28,32–38
This study aimed to: (1) compare different climatic areas to identify commonalities in climatic factors that affect the spread of COVID-19; (2) conduct an in-depth analysis of the differences in the impact of AH on the COVID-19 epidemic in different climate types; and (3) provide data to help formulate policies that incorporatic climatic factors to control COVID-19. This study compared the impact of climatic factors on the spread of COVID-19 in four regions. Additionally, we also considered the impact of population level measures that affect population movement such as isolation and curfews. We found that humidity had an important impact on the spread of COVID-19. This finding, combined with those of previous studies investigating the relation between humidity and respiratory viruses, can be applied to inform interventions focused on the role of environmental humidity in the spread of COVID-19. We hope that these findings will lay the foundation for further determining the key role of climate variables in the spread of COVID-19, and provide a reference for the development of more targeted isolation and curfews, so that relevant policies can fully consider climatic and environmental conditions.
MATERIALS AND METHODS
Daily-Cases, Climate Data, Air Quality Index Collection
The epidemics in Moscow, Lima, Kuwait, and Singapore occurred as early as early March. However, due to the popularity of testing, the number of people tested is relatively small. Therefore, we collected the 6 months from March 20 to September 30, 2020. Number of new cases per day in four places.35–38 (Since these data were only available in Lima is as of July 24, we only collected the daily number of cases in this area for March 20 to July 24, 2020.) In addition, we did not include imported cases from various regions in the analysis. We used the software Wheat A (version 1.2.5, https://www.xiaomaiya.cc/)39 to collect the daily average temperature (Ta), wind speed (WS), dew point (Td), and other weather factors obtained from relevant weather stations. RH and AH were calculated using humidity conversion software (version 3.0, http://www.zzdibang.com/).40 We also collected the air quality index PM2.5, PM10, and ozone (O3), sulfur dioxide (SO2), carbon monoxide (CO) of the four regions, we collect these data from World air quality index (https://aqicn.org).41 (Moscow only has PM2.5 and PM10 data; Lima has no SO2, CO data; Kuwait only has PM2.5 data.)
On March 30, Moscow required residents to self-isolate. Only Moscow residents were allowed to leave their homes for medical treatment, grocery shopping, and other reasons, and those who left home were advised to keep at least 1.5 m away from others. The decree was lifted on June 942,43 (recorded as 1 during the isolation period and otherwise was set to 0).
Peru began to implement a national curfew on March 18. On May 23, the government decided to establish a 24-hour curfew every Sunday (until June 30). On June 27, the government announced the cancellation of the 24-hour curfew every Sunday44 (the 24-hour curfew was recorded as 2, the curfew was recorded as 1, and otherwise was set to 0).
In March, Kuwaiti authorities implemented curfew measures to curb the spread of the virus. On August 30, Kuwait lifted the curfew45,46 (the curfew was recorded as 1 and otherwise was set to 0).
On April 3, Singapore announced a partial blockade across the country. From April 7, all non-essential workplaces were closed, and essential workplaces remained open. The blockade was relaxed on June 247 (the blockade was recorded as 1 and otherwise was set to 0).
Statistical Analysis
First, a correlation analysis of meteorological factors and COVID-19 incidence was carried out. Then AH was analyzed using the local weighted regression scatter smoothing method. After investigating the multicollinearity through the variance expansion factor test, we modeled the event intensity λ (assuming the factors that affect λ are X1, X2,…, Xm, and the connection function is logarithmic: Log (λ) = β0 + β1X1 + β2X2 + … + βmXm in the negative binomial) with a negative binomial regression. In the regression, the variance of the number of events is equal to λ (1 + κλ), where κ is a discrete parameter of the negative binomial distribution and indicates the degree of ultra-discreteness. When κ = 0, it degenerates into a Poisson regression, and the two are compared using the likelihood ratio test. If P < 0.05, it indicates that the data fit a negative binomial regression model better than the Poisson regression model. The prediction effect of the model can be judged by the distribution and normality of the scatter points of the deviation residual plot of the regression analysis. According to the current knowledge of the incubation period of COVID-19, we chose to analyze the lag effect using 14 days. All analyses were conducted using Stata 16.0 (College Station, TX: Stata Corp).48
RESULTS
Spearman Correlation Analyses of Daily-Cases and Climate Data
The trend of the number of daily-cases in each region is shown in Figure 1.
FIGURE 1.
Daily COVID-19 incidence trends in four regions.
The climate factors in each region are shown in Table 1, and the change trend of Ta, Td, RH, and AH is shown in Figures 2 and 3.
TABLE 1.
The COVID-19 with Meteorological Factor of Negative Binomial Regression
| Areas | Climate Factor | March 20–April 30 | May | June | July | August | September |
| Moscow | Ta (°F) | 38.92 ± 6.50 | 78.1 (75.3–81.6) | 67.5 (60.7–70.9) | 65.16 ± 4.89 | 63.02 ± 4.15 | 56.14 ± 5.37 |
| RH (%) | 50.83 ± 16.77 | 71.32 ± 14.11 | 72.91 ± 11.29 | 80.24 ± 9.04 | 74.12 ± 9.49 | 73.53 ± 12.31 | |
| AH (g/m3) | 3.71 ± 1.08 | 7.45 ± 2.26 | 11.59 ± 2.27 | 12.68 ± 1.92 | 10.85 ± 1.29 | 8.53 ± 1.43 | |
| Td (°F) | 26.3 (19.1–31.4) | 42.99 ± 7.96 | 56.06 ± 5.81 | 58.2 (56.3–61.7) | 54.58 ± 3.58 | 47.41 ± 4.68 | |
| WS (mi/hour) | 8.45 ± 3.04 | 7.41 ± 2.76 | 6.57 ± 3.04 | 6.02 ± 1.85 | 5.29 ± 1.42 | 8.1 (5.3–9.2) | |
| Lima∗ | Ta (°F) | 72.31 ± 2.02 | 66.85 ± 2.24 | 64.3 (62.6–64.5) | 61.12 ± 0.74 | – | – |
| RH (%) | 78.23 ± 4.11 | 80.9 (78.7–82.4) | 80.78 ± 3.06 | 80.65 ± 4.21 | – | – | |
| AH (g/m3) | 15.9 (14.5–16.4) | 13.32 ± 0.80 | 12.14 ± 0.52 | 11.09 ± 0.39 | – | – | |
| Td (°F) | 65.9 (63.2–66.7) | 60.46 ± 1.79 | 57.72 ± 1.22 | 55.01 ± 0.92 | – | – | |
| WS (mi/hour) | 7.22 ± 1.54 | 6.4 (5.8–7.6) | 6.25 ± 1.39 | 6.10 ± 1.30 | – | – | |
| Kuwait | Ta (°F) | 77.41 ± 5.50 | 91.21 ± 4.91 | 99.26 ± 2.04 | 102.17 ± 2.63 | 101.15 ± 2.62 | 96.98 ± 2.34 |
| RH (%) | 42.4 (32.7–54.7) | 22.5 (20.5–26.2) | 19.92 ± 3.11 | 23.2 (20.5–35.1) | 19.1 (17.2–21.9) | 26.6 (22.5–30.9) | |
| AH (g/m3) | 9.5 (7.9–12.2) | 8.42 ± 1.39 | 8.84 ± 0.98 | 11.1 (9.6–17.0) | 8.8 (8.2–10.3) | 11.0 (9.8–12.6) | |
| Td (°F) | 51.5 (46.8–58.5) | 48.81 ± 4.45 | 50.69 ± 2.96 | 57.2 (23.3–69.5) | 50.8 (48.8–55.0) | 56.7 (53.6–60.3) | |
| WS (mi/hour) | 3.0 (2.2–4.3) | 3.12 ± 1.25 | 3.48 ± 1.41 | 2.6 (2.1–3.7) | 3.76 ± 1.52 | 2.4 (1.8–2.7) | |
| Singapore | Ta (°F) | 85.26 ± 1.61 | 85.29 ± 1.63 | 83.7 (81.7–85.3) | 83.33 ± 1.94 | 83.79 ± 2.38 | 83.1 (81.3–84.1) |
| RH (%) | 75.7 (71.7–79.2) | 78.40 ± 3.95 | 81.03 ± 4.91 | 78.63 ± 4.02 | 77.2 (76.0–80.1) | 80.10 ± 5.41 | |
| AH (g/m3) | 22.46 ± 0.66 | 23.24 ± 0.70 | 22.68 ± 0.51 | 21.96 ± 0.48 | 22.19 ± 0.89 | 21.84 ± 0.56 | |
| Td (°F) | 76.72 ± 0.87 | 77.75 ± 0.94 | 76.92 ± 0.75 | 75.93 ± 0.72 | 76.23 ± 1.32 | 75.80 ± 0.78 | |
| WS (mi/hour) | 4.05 ± 1.12 | 3.28 ± 0.95 | 3.95 ± 1.30 | 3.82 ± 1.07 | 4.69 ± 1.29 | 4.05 ± 1.25 |
AH, absolute humidity; Ta, average temperature; Td, dew point; WS, wind speed.
Lima only data from March 20th to July 24th.
FIGURE 2.
Ta (A) and Td (B) in the four regions. Ta, average temperature; Td, dew point.
FIGURE 3.
RH (a) and AH (b) in the four regions. AH, absolute humidity.
In Moscow, the largest daily-cases were recorded on May 7 (6703 cases), and the day with the least number of daily-cases was March 21 (16 cases). Daily-cases had a non-normal distribution (W = 0.75, P < 0.001). Spearman correlation analyses between daily-cases and climate data showed that daily-cases was positively correlated with Ta (58.50 [47.50 to 64.40]°F, r = −0.18, P = 0.010), AH (9.04 [5.57 to 11.69] g/m3, r = −0.19, P = 0.010), and Td (49.50 [35.90 to 56.70]°F, r = −0.19, P = 0.009). No significantly related to RH (71.68 [62.19 to 81.18]%, r = 0.01, P = 0.938), WS (6.60 [4.80 to 8.60] mi/hour, r = 0.08, P = 0.283), PM2.5 (9.10 [4.50 to 14.40], r = −0.07, P = 0.331), PM10 (10.00 [5.10 to 15.90], r = −0.08, P = 0.300).
In Lima, the largest daily-cases were recorded on May 29 (4579 cases), and the day with the least number of daily-cases was March 24 (15 cases). Daily-cases had a non-normal distribution (W = 0.93, P < 0.001). Spearman correlation analyses between daily-cases and climate data revealed that daily-cases were positively correlated with Ta (65.60 [62.60 to 71.30]°F, r = −0.51, P < 0.001), RH (80.40 [78.36 to 82.40]%, r = 0.19, P = 0.035), AH (13.03 [11.81 to 14.56] g/m3, r = −0.48, P < 0.001), Td (59.80 [56.90 to 63.20]°F, r = −0.49, P < 0.001), WS (6.50 [5.50 to 7.60]mi/hour, r = −0.19, P = 0.031), and PM2.5 (16.30 [13.55 to 20.65] μg/m3, r = 0.23, P = 0.013). No significantly related to PM10 (22.90 [18.95 to 28.05], r = 0.17, P = 0.074), O3 (57.86 ± 9.05 μg/m3, r = 0.09, P = 0.361).
In Kuwait the largest daily-cases were recorded on May 19 (1073 cases), and the day with the least number of daily-cases was March 23 (1 case). The daily-cases had a non-normal distribution (W = 0.94, P < 0.001). Spearman correlation analyses between daily-cases and climate data found that daily-cases were positively correlated with Ta (97.90 [87.20 to 100.70]°F, r = 0.49, P < 0.001), RH (24.59 [19.97 to 33.12]%, r = −0.44, P < 0.001), and PM2.5 (38.90 [28.60 to 50.60] μg/m3, r = 0.41, P < 0.001). No significantly related to AH (9.41 [8.30 to 11.26] g/m3, r = 0.03, P = 0.706). WS (2.70 [2.10 to 4.20] mi/hour, r = −0.03, P = 0.668). Td (52.40 [48.80 to 57.20]°F, r = 0.07, P = 0.305).
In Singapore, the largest daily-cases were recorded on April 20 (1426 cases), and the day with the least number of daily-cases was September 23 (8 cases). Daily-cases had a non-normal distribution (W = 0.87, P < 0.001). Spearman correlation analyses between daily-cases and climate data showed that the daily-cases were positively correlated with Ta (84.30 [82.80 to 85.70]°F, r = 0.29, P < 0.001); AH (22.40 ± 0.78 g/m3, r = 0.44, P < 0.001); Td (76.57 ± 1.11°F, r = 0.43, P < 0.001); WS (3.90 [3.08 to 4.90] mi/hour, r = −0.19, P = 0.010); PM2.5 (10.20 [8.40 to 12.00] μg/m3, r = −0.23, P = 0.002); O3 (8.60 [6.60 to 11.80] μg/m3, r = 0.26, P < 0.001); SO2 (3.00 [2.20 to 4.00] μg/m3, r = 0.45, P < 0.001); and CO (4.60 [4.00 to 5.10] μg/m3, r = −0.18, P = 0.013). No significantly related to RH (77.94 [75.50 to 81.35]%, r = −0.05, P = 0.469); PM10 (23.10 [20.06 to 25.40], r = −0.07, P = 0.370).
Negative Binomial Regression Model Analysis
We introduced relevant meteorological factors into the negative binomial regression model (see Table 2).
TABLE 2.
Estimates from Negative Binomial Regression
| Areas | Effective Variable | Parameter | z | P | 95% CI | Log Likelihood | Akaike Information Criterion |
| Moscow | Constant | 7.13 | 29.96 | <0.001 | 6.66–7.59 | −1352.79 | 2717.59 |
| AH | −0.14 | −3.66 | <0.001 | −0.21 to −0.06 | |||
| Td | 0.02 | 2.30 | 0.022 | 0.003–0.04 | |||
| Lockdown | 1.02 | 14.08 | <0.001 | 0.88–1.16 | |||
| Lima | Constant | −17.60 | −0.67 | 0.502 | −68.92–33.72 | −902.08 | 1822.16 |
| AH | −3.47 | −7.45 | <0.001 | −4.39 to −2.56 | |||
| Td | 2.17 | 2.44 | 0.015 | 0.42–3.91 | |||
| Kuwait | Constant | 4.16 | 7.25 | <0.001 | 2.60–4.93 | −1251.47 | 2514.95 |
| Ta | 0.03 | 4.86 | <0.001 | 0.01–0.04 | |||
| RH | −0.01 | −2.95 | 0.003 | −0.02 to −0.004 | |||
| Singapore | Constant | −73.80 | −2.21 | 0.027 | −139.49 to −8.51 | −1160.13 | 2342.26 |
| AH | −2.29 | −2.10 | 0.035 | −4.43 to −0.16 | |||
| Td | 1.77 | 2.19 | 0.029 | 0.18–3.35 | |||
| PM2.5 | −0.13 | −6.04 | <0.001 | −0.17 to −0.09 | |||
| O3 | 0.05 | 2.56 | 0.010 | 0.01–0.09 | |||
| Lockdown | 0.75 | 4.48 | <0.001 | 0.42–1.08 |
The normality test on the residual, Moscow: W = 0.84, P < 0.001; Lima: W = 0.94, P < 0.001; Kuwait: W = 0.96, P < 0.001; Singapore: W = 0.87, P < 0.001. AH, absolute humidity; Ta, average temperature; Td, dew point.
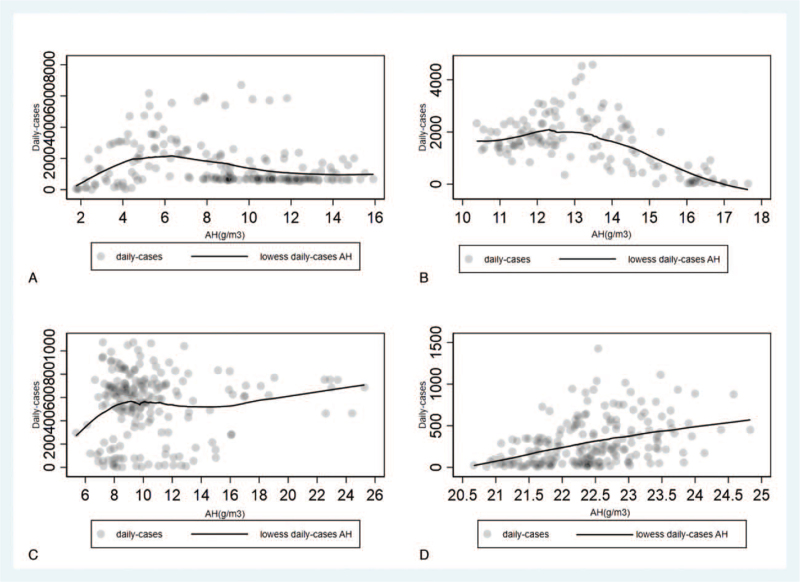
Local Weighted Regression Scatter Smoothing Method
Local weighted regression scatter smoothing method shows that when AH exceeds the range of 9 to 13 g/m3 in Moscow and Lima, the cases decrease with the increase of AH, when AH exceeds 20 g/m3, Kuwait and Singapore's cases show an upward trend as AH increases (see Fig. 4).
FIGURE 4.
Local weighted regression scatter smoothing method cases-AH of Moscow (A), Lima (B), Kuwait (C), and Singapore (D). AH, absolute humidity.
DISCUSSION
This study found that the COVID-19 epidemic in four regions (ie, Moscow, Lima, Singapore, and Kuwait) was affected by humidity. The daily-cases in Moscow, Lima, and Singapore were all negatively correlated with AH (ie, decreased with the increase of AH), while in Kuwait, daily-cases were affected by RH. Studies have shown that AH may directly characterize air's water vapor content. This is of great significance to the study since droplets and aerosols may transmit the virus. Higher AH will cause the surface of lipid-containing viruses to inactivate. Studies on influenza have shown that 50% of influenza virus transmission variability and 90% of influenza virus survival variability could be explained by AH variation, whereas only 12% and 36% could be explained by relative humidity.4,49 Therefore, AH has the potential to predict the spread of COVID-19. Liu et al's research50 on Chinese provinces found that AH was negatively related to the increase of COVID-19 transmission. A study on the COVID-19 epidemic in Japan also showed that AH differences was the dominant ambient factors characterizing morbidity and mortality rates, higher AH areas with lower morbidity and mortality rates.51 Zhu et al52 reported a significant negative correlation between daily-cases and absolute humidity in Lima, which is consistent with our research. After the quarantine was lifted in Moscow in June, the epidemic showed a trend of relief from July to August. However, after September, the AH began to decrease (see Table 1 and Figs. 1 and 2), and the epidemic began to show a rebound. In Lima, after the epidemic began to ease in June, the AH began to decrease, the epidemic also began to rebound along with the winter in the southern hemisphere in July (see Table 1 and Figs. 1 and 2). This occurred not withstanding the curfew measures, which indicates that AH played a role in the spread of COVID-19 in Lima. Local weighted regression scatter smoothing method shows that when AH exceeds the range of 9 to 13 g/m3 in Moscow and Lima (see Fig. 4), the cases decrease with the increase of AH. Shaman et al4 found that AH constrains influenza virus transmission much more significantly. Another study also showed that the AH is related to the survival rate of influenza viruses, and if made the elapsed time when the survival rate is reduced to 50% is defined as the virus half-life, and there is a high relationship between absolute humidity and half-life.53 A study on the relationship between climate and air quality shows that the increase in AH favors the atmospheric wet deposition got stronger and particle concentration was reduced, and many studies indicated that an increased particle concentration concentration causes an increased risk of respiratory diseases,54–56 and PM2.5 has also been found to be related to the COVID-19 epidemic.19–20 But Singapore's cases show an upward trend as AH increases (see Fig. 4), this is contrary to the results of negative binomial regression analysis, the underlying factors may be more complicated; however, Singapore, which has a higher AH, as we must consider that higher absolute humidity may make people feel extremely uncomfortable and affect the flow of people outside, therefore, more influencing factors need to be included for analysis later.
The difference from these results, Kuwait's epidemic does not seem to be affected by AH. Meo et al57 found that Covid-19 daily-cases in Kuwait were negatively correlated with RH and positively correlated with temperature. This is consistent with our analysis of Kuwait. RH can regulate the area of the air–liquid interface available for virus accumulation, and higher RH can cause inactivation of enveloped viruses58 (eg, COVID-1959). Kuwait's negative binomial regression analysis result is the only one that includes Ta factor. There is currently much controversy about the influence of temperature on the spread of COVID-19. A study on Kuwait's neighboring Iraq showed that R-value of COVID-19 is reduced with a decrease in temperature and increased RH.60 These results may indicate that the spread of COVID-19 in Middle East is affected by temperature and RH, a study of Saudi Arabia, which is in the same tropical desert climate, found that PM10 and PM2.5 showed negative association with RH and positive with temperature,61 we conclude, these two factors may jointly affect particulate matter and thus affect the spread of COVID-19 in the Middle East. However, Kuwait and Lima also with the same climate type, the climatic factors affecting the COVID-19 epidemic are different, this may be related to the measures taken by the local government. Due to the geographical environment, Lima will be affected by the ocean there will be differences with Kuwait in humidity,29–31 this is also a possible reason.
Sahoo et al62 found the COVID-19 spreading incidences were positively correlated with Td. At present, there is not much research on dew point. In our study, in Kuwait, where Td was low, Td did not seem to have a significant effect on the spread of the virus. In contrast, in Lima and Singapore, which have a high Td, daily-cases of COVID-19 were correlated with Td. Dew point is the temperature at which air cooling reaches saturation when the water vapor content in the air and the air pressure are constant. Studies have shown that the most comfortable Td temperature of the human body is 50 to 59°F.63 A higher dew point temperature will cause extreme discomfort to the human body, affecting people's movements outdoors. Lima with Singapore has opposite seasonal climates. That is, when it is winter in Lima it is summer in Singapore. In the study of the impact of cold, humid, and hot environments, the use of heating and cooling equipment may complicate Td's apparent impact on the epidemic. Studies have shown that influenza activity is highly correlated with low Td in temperate and frigid regions, while the situation in tropical regions is more complicated. High Td may cause people to gather indoors, get close, breathe the turbid air, and be exposed to indoor air-conditioning systems. Yet low Td promotes the spread of the virus.64 Therefore, for isolation and curfew measures, it seems that we should pay attention to adjustments in the indoor environment. In the negative binomial regression, lockdown is positively correlated with the increase of daily-cases in Moscow and Singapore, this may also need to be considered comprehensively from the living environment after lockdown, for example, the epidemic of foreign workers in Singapore may be related to their living environment, Singapore has also made a positive response to this.65,66 During the COVID-19 pandemic, lockdown and curfews were key policies aimed at reducing exposure to the virus, but there seems a potential for greater exposure to pollutants and fine particles indoors under lockdown, it cannot be ignored.67,68 This also requires in-depth consideration in order to facilitate the development of relevant epidemic prevention measures in the future.
Zhu et al19 observed positive associations between daily-cases and PM2.5, PM10, CO, NO2, and O3. However, SO2 was negatively associated with the number of daily-cases. PM2.5 damages the first line of defense of the upper respiratory tract (ie, the cilia) and may weaken the immune response, making the body less effective against diseases caused by viruses.20 In this study's Spearman correlation analyses, daily-cases were positively correlated with PM2.5 in Lima and Kuwait, where PM2.5 is relatively high. In contrast, daily-cases were negatively correlated with PM2.5 in Singapore, where PM2.5 was relatively low. Finally, only Singapore's negative binomial regression analysis included PM2.5. Our results are contrary to many studies, daily-cases were negatively correlated with PM2.5 in Singapore, although it is not clear yet, we believe that this may be related to people strengthen protection in high-concentration PM2.5 environment that reduced the probability of people being exposed to PM2.5, and Singapore's high temperature and high humidity may also limit it. However, we still need more research data to explore the reasons. In short, the impact of PM2.5 on the spread of COVID-19 still warrants further investigation before definitive conclusions can be drawn. Adhikari et al's findings69 indicate that short-term exposures to ozone can influence COVID-19 transmission and initiation of the disease, Wolcott et al's research70 shows that exposure to ozone reduces influenza disease severity. This study only collected ozone data for Lima and Singapore, and Singapore's daily-cases are related to ozone.
After controlling for curfews and quarantine measures related to the epidemic, our study found that humidity (especially AH and Td) had the greatest impact on COVID-19, irrespective of the fact that the areas under study had different climates. This study is one of the few to report the impact of AH on the spread of COVID-19. Some studies showed that the relationship between indoor and outdoor temperatures is nonlinear; however, the relationships were linear for RH and AH, especially indoor AH has a strong correlation with outdoor AH year-round, indoor AH fluctuations are associated primarily with changes in outdoor AH,71,72 these results suggest that underscore the importance of quarantine measures that incorporate environmental management during curfews and quarantine, including the regulation of humidity. Refer to research on influenza virus, properly increasing the AH of the environment may be effective for virus control.72 Guan et al73 found that the increase of AH can enhance the inactivation of avian influenza virus. We suggest that we can consider reducing COVID-19's transmission may be reduced with humidity control of buildings. Air-conditioning systems increase the risk of infection possibility,74 and a study about A/H1N1 virus report an air humidifier in the living room was a possible protective factor,75 despite the lack of more results support, increase AH by air humidifier may play a role in controlling the spread of COVID-19. Further research is needed to directly investigate the association of AH with COVID-19 virus survival to support this hypothesis. Td is another climate factor that needs attention, Td is frequently used as a measure of human comfort, high Td may cause people to gather indoors and be exposed to indoor air-conditioning systems and promotes the spread of the COVID-19. This is a factor to consider when formulating lockdown and curfew measures.
Our research has some shortcomings. Although we considered the impact of the air quality index, some indicators were missing in some areas due to the data sources. In addition, although we included the restrictive measures adopted by various regions, we were unable to include both mobility and demographic factors in the analysis due to a lack of information.
CONCLUSION
In our methodology, except for Kuwait, we did not find significant associations of temperature with the spread of COVID-19, rising temperatures may not reduce the spread of COVID-19. After controlling for restrictive measures, humidity is still the biggest factor influencing the incidence of daily-cases of COVID-19. The results suggest the significantly of an increase in humidity (AH or RH) to contain or slow down the COVID-19's transmission. Environment humidification may be a feasible approach to decrease COVID-19 virus transmission.
Acknowledgments
The authors would like to express their gratitude to Edit Springs (https://www.editsprings.com/) for the expert linguistic services provided and express their gratitude to World air quality index (https://aqicn.org) for air quality data provided.
Footnotes
LZC and ZL are the cofirst authors.
The authors report no conflicts of interest.
Zhenchao Liu: Conceptualization, Methodology, Software, Writing – original draft, Formal analysis. Lin Zhu: Software, Visualization, Writing – original draft. Yue Wang: Software, Validation. Zhen Zhou: Software, Validation. Yunliang Guo: Writing – review and editing, Methodology, Validation.
Clinical significance: Existing studies have found that climate factors have an important influence on the spread of the COVID-19 virus. This study found that humidity has an important effect on the spread of COVID-19 in several different climate types, and environment humidification may be a feasible approach to decrease COVID-19 virus transmission.
REFERENCES
- 1.Anderson EL, Turnham P, Griffin JR, Clarke CC. Consideration of the aerosol transmission for COVID-19 and public health. Risk Anal 2020; 40:902–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lowen AC, Mubareka S, Steel J, Palese P. Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog 2007; 3:1470–1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huy C, Kuhn D, Zöllner SSI. Seasonal waves of influenza and cause-specific mortality in Germany. Cent Eur J Med 2012; 7:450–456. [Google Scholar]
- 4.Shaman J, Kohn M. Absolute humidity modulates influenza survival, transmission, and seasonality. Proc Natl Acad Sci USA 2009; 106:3243–3248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yuan JS, Yun HM, Lan W, et al. Epidemiological study of association between climate determinants and spread of Severe Acute Respiratory Syndrome (SARS) in Beijing. J Grad School Chin Acad Sci 2005; 22:579–588. (in Chinese). [Google Scholar]
- 6.Alghamdi IG, Hussain II, Almalki SS, Almalki S, Alghamdi M, Elsheemy M. The pattern of Middle East respiratory syndrome coronavirus in Saudi Arabia: a descriptive epidemiological analysis of data from the Saudi Ministry of Health. Int J Gen Med 2014; 7:417–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lamarre A, Talbot PJ. Effect of pH and temperature on the infectivity of human coronavirus 229E. Can J Microbiol 1989; 35:972–974. [DOI] [PubMed] [Google Scholar]
- 8.Chan KH, Peiris JS, Lam SY, Poon LLM, Seto WH. The effects of temperature and relative humidity on the viability of the SARS coronavirus. Adv Virol 2011; 2011:734690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Qi HC, Xiao S, Shi R, et al. COVID-19 transmission in Mainland China is associated with temperature and humidity: a time-series analysis. Sci Total Environ 2020; 728:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goswami K, Bharali S, Hazarika J. Projections for COVID-19 pandemic in India and effect of temperature and humidity. Diabetes Metab Res 2020; 14:801–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shahzad F, Shahzad U, Faree Z. Asymmetric nexus between temperature and COVID-19 in the top ten affected provinces of China: a current application of quantile-on-quantile approach. Sci Total Environ 2020; 736:139115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Iqbal N, Fareed Z, Shahzad F, He X, Shahzad U, Lina M. The nexus between COVID-19, temperature and exchange rate in Wuhan city: new findings from partial and multiple wavelet coherence. Sci Total Environ 2020; 729:138916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dogan B, Jebli MB, Shahzad K. Investigating the effects of meteorological parameters on COVID-19: case study of New Jersey, United States. Environ Res 2020; 191:110148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sobral MFF, Duarte GB, da Penha Sobral AIG, Marinho MLM, de Souza Melo A. Association between climate variables and global transmission of SARS-CoV-2. Sci Total Environ 2020; 729:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sajadi MM, Habibzadeh P, Vintzileos A, Shokouhi S. Temperature and latitude analysis to predict potential spread and seasonality for COVID-19. SSRN Electron J 2020; DOI 10.2139/ssrn.3550308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ahmadi M, Sharifi A, Dorosti S, Ghoushchi SJ, Ghanbari N. Investigation of effective climatology parameters on COVID-19 outbreak in Iran. Sci Total Environ 2020; 729:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deyle ER, Maher MC, Hernandez RD, Basu S, Sugihara G. Global environmental drivers of influenza. Proc Natl Acad Sci USA 2016; 113:13081–13086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shakoor A, Chen X, Farooq TH, et al. Fluctuations in environmental pollutants and air quality during the lockdown in the USA and China: two sides of COVID-19 pandemic. Air Qual Atmos Health 2020; 13:1335–1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhu YJ, Xie JG, Huang FM, Cao L. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci Total Environ 2020; 727:138704.DOI 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mehmood K, Saifullah, Iqbal M, Abrar MM. Can exposure to PM2.5 particles increase the incidence of coronavirus disease 2019 (COVID-19)? Sci Total Environ 2020; 741:140441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ma YL, Zhao YD, Liu JT, et al. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Sci Total Environ 2020; 724:138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Megaritis AG, Fountoukis C, Charalampidis PE, et al. Linking climate and air quality over Europe: effects of meteorology on PM2.5 concentrations. Atmos Chem Phys 2014; 14:10345–10391. [Google Scholar]
- 23.Dawson JP, Adams PJ, Pandis SN. Sensitivity of PM2.5 to climate in the Eastern US: a modeling case study. Atmos Chem Phys 2007; 7:6487–6525. [Google Scholar]
- 24.Munir S, Habeebullah TM, Mohammed AMF, Morsy E. Analysing PM2.5 and its association with PM10 and meteorology in the arid climate of Makkah, Saudi Arabia. Aerosol Air Qual Res 2016; 17:453–464. [Google Scholar]
- 25. Pettersson H, Manley B, Hernandez S. Tracking Covid-19's Global Spread [CNN health/CNN web site]. October 1, 2020. Available at: https://www.cnn.com/interactive/2020/health/coronavirus-maps-and-cases/ (accessed October 1, 2020). [Google Scholar]
- 26.Balasubramanian A. World Climate Zones. Mysuru India: University of Mysore; 2013. [Google Scholar]
- 27.Beck HE, Zimmermann NE, McVicar TR, Vergopolan N, Berg A, Wood EF. Present and future Köppen-Geiger climate classification maps at 1-km resolution. Sci Data 2018; 5:180214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Choudhary K, Boori MS, Kupriyanov AV. Mapping and evaluating urban density patterns in Moscow, Russia. Comput Opt 2017; 41:528–534. [Google Scholar]
- 29.Siña M, Wood RC, Saldarriaga E, et al. Understanding perceptions of climate change, priorities, and decision-making among municipalities in Lima, Peru to better inform adaptation and mitigation planning. PLoS One 2016; 11:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goubanova K, Echevin V, Dewitte B, Codron F, Vrac M. Statistical downscaling of sea-surface wind over the Peru-Chile upwelling region: diagnosing the impact of climate change from the IPSL-CM4 model. Clim Dynam 2011; 36:1365–1378. [Google Scholar]
- 31.Romero Y, Diaz C, Meldrum I, Arias Velasquez R, Noel J. Temporal and spatial analysis of traffic – related pollutant under the influence of the seasonality and meteorological variables over an urban city in Peru. Heliyon 2020; 6:e04029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Darido G, Pulido D, Targa F, Alvim B, Peralta-Quirós T. Lima urban transport: on the way to transformation. Connections [serial online]. October 2015; 22:102769. Available from: https://www.worldbank.org/en/topic/transport/brief/connections (accessed April 25, 2021). [Google Scholar]
- 33.Rode P, Gomes A, Adeel M, et al. Resource Urbanisms: Asia's Divergent City Models of Kuwait, Abu Dhabi, Singapore and Hong Kong. Leeds, UK: The University of Leeds; 2017. [Google Scholar]
- 34.Guimera R, Mossa S, Turtschi A, Amaral LAN. The worldwide air transportation network: anomalous centrality, community structure, and cities’ global roles. Proc Natl Acad Sci USA 2003; 102:7794–7799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Онлайн статистика коронавируса Covid-19 в Москве на сегодня [CNN Health/Coronavirus-Monitor Web site]. October 2, 2020. Available at: https://coronavirus-monitor.ru (accessed October 2, 2020). [Google Scholar]
- 36. Ministerio de Salud. Minsa: Casos confirmados por coronavirus Covid-19 [gob.pe web site]. October 2, 2020. Available at: https://www.gob.pe (accessed October 2, 2020). [Google Scholar]
- 37. Cases by Date [corona.e.gov web site]. October 2, 2020. Available at: https://corona.e.gov.kw (accessed October 2, 2020). [Google Scholar]
- 38. Situation Report [moh.gov.sg web site]. October 2, 2020. Available at: https://www.moh.gov.sg/covid-19/situation-report/ (accessed October 2, 2020). [Google Scholar]
- 39.Wheat A [computer program]. Version 1.2.5. 2020; Ningbo: Wheat Bud Big Data Information Co., Ltd, Updated October 7, 2020. [Google Scholar]
- 40. Humidity Conversion Software [computer program]. Version 3.0. Zhengzhou: Dibang Technology; 2015. Updated January 8, 2015. [Google Scholar]
- 41. World Air Quality Index project [database online]. World Air Quality Index team; 2007. Updated October 6, 2020. [Google Scholar]
- 42.Kiselyov S. Moscow Orders Citywide lockdown Starting March 30 [themoscowtimes web site]. March 30, 2020. Available at: https://www.themoscowtimes.com/2020/03/29/moscow-orders-citywide-lockdown-starting-march-30-a69789 (accessed October 8, 2020). [Google Scholar]
- 43.Jovanovic D. Strict Lockdown Measures in Moscow Lifted as Russian Coronavirus Cases Approach Half a Million [abcnews web site]. June 9, 2020. Available at: https://abcnews.go.com/International/strict-lockdown-measures-moscow-lifted-russian-coronavirus-cases/story?id=71153954 (accessed October 8, 2020). [Google Scholar]
- 44. Pandemia de COVID-19 en Perú [wikipedia web site]. October 8, 2020. Available at: https://es.wikipedia.org/wiki/Pandemia_de_COVID-19_en_Per%C3%BA#Toque_de_queda (accessed October 8, 2020). [Google Scholar]
- 45.Sherbini RA. COVID-19: Kuwait's Curfew to End on August 30 [gulfnews web site]. August 21, 2020. Available at: https://gulfnews.com/world/gulf/kuwait/covid-19-kuwaits-curfew-to-end-on-august-30-1.73329258 (accessed October 8, 2020). [Google Scholar]
- 46.Mulla YA. COVID-19: Kuwait Shortens Curfew, Extends Shopping Mall Hours [gulfnews web site]. July 28, 2020. Available at: https://gulfnews.com/world/mena/covid-19-kuwait-shortens-curfew-extends-shopping-mall-hours-1.72840922 (accessed October 8, 2020). [Google Scholar]
- 47. Singapore Circuit Breaker Measures [wikipedia web site]. October 8, 2020. Available at: https://en.wikipedia.org/wiki/2020_Singapore_circuit_breaker_measures (accessed October 8, 2020). [Google Scholar]
- 48. Stata [computer program]. Version 16.0. Texas: College Station, TX; 1985. Updated July 9, 2019. [Google Scholar]
- 49.Benjamin DD, Stephen K, Julia RG, et al. Urbanization and humidity shape the intensity of influenza epidemics in U.S. cities. Science 2018; 362:75–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liu JT, Zhou J, Yao JX, et al. Impact of meteorological factors on the COVID-19 transmission: a multi-city study in China. Sci Total Environ 2020; 726:138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kodera S, Rashed EA, Hirata A. Correlation between COVID-19 morbidity and mortality rates in Japan and local population density, temperature, and absolute humidity. Int J Environ Res Public Health 2020; 17:5477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhu LT, Liu XB, Huang HN, Avellán-Llaguno RD, Zhu YG. Meteorological impact on the COVID-19 pandemic: a study across eight severely affected regions in South America. Sci Total Environ 2020; 744:140881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kurabuchi T, Ogasawara T, Kumagai K, Asari Y. Relationship between absolute humidity and virus survival rate affecting lnfluenza transmission. SHASE 2009; 2:1339–1342. (in Japanese). [Google Scholar]
- 54.Wang C, Xiao TG, Luo Q, Wu LB, Zhang YC, Wen XH. Characteristics of urban air humidity and its impact on particle. Environ Eng 2018; 36:116–121,127. (in Chinese). [Google Scholar]
- 55.Chen G, Zhang W, Li S, Zhang Y, Guo Y. The impact of ambient fine particles on influenza transmission and the modification effects of temperature in China: a multi-city study. Environ Int 2017; 98:82–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lung CC, Chen SC, Yang CH, et al. Using atmospheric visibility to assess the effects of air pollution on hospital admissions for respiratory diseases. Aerosol Air Qual Res 2016; 16:2237–2244. [Google Scholar]
- 57.Meo SA, Abukhalaf AA, Alomar AA. Effect of temperature and humidity on the dynamics of daily new cases and deaths due to COVID-19 outbreak in Gulf countries in Middle East Region. Eur Rev Med Pharmacol 2020; 24:7524–7533. [DOI] [PubMed] [Google Scholar]
- 58.Yang W, Marr LC. Mechanisms by which ambient humidity may affect viruses in aerosols. Appl Environ Microb 2020; 78:6781–6788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Das UN. Bioactive lipids in COVID-19 – further evidence. Arch Med Res 2020; 52:107–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jebril N. Predict the transmission of COVID-19 under the effect of air temperature and relative humidity over the year in Baghdad, Iraq. SSRN Electron J 2020. 1–13. doi: 10.2139/ssrn.3579718. [Google Scholar]
- 61.Munir S, Habeebullah TM, Mohammed AMF, Morsy EA, Ali K. Analysing PM2.5 and its association with PM10 and meteorology in the arid climate of Makkah, Saudi Arabia. Aerosol Air Qual Res 2016; 17:453–464. [Google Scholar]
- 62.Sahoo PK, Mangla S, Pathak AK, Salomo GN, Sarkar D. Pre-to-post lockdown impact on air quality and the role of environmental factors in spreading the COVID-19 cases – a study from a worst-hit state of India. Int J Climatol 2020; 65:205–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Salvador PM, Kilpatrick J, Allie K, Rivas E. Skin temperature and high dew point in hot environments affects self-paced exercise. IJES 2009; 2:46. [Google Scholar]
- 64.Zhou SZ. A seasonal influenza theory and mathematical model incorporating meteorological and socio-behavioral factors. J Trop Meteorol 2009; 25:706–716. [Google Scholar]
- 65. Covid-19: Some foreign Workers in Singapore feel ‘safer’ in Dorms, Others Lament Lack of Enforcement, Cramped Spaces [malaymail web site]. April 18, 2020. Available at: https://www.malaymail.com/news/world/2020/04/18/covid-19-some-foreign-workers-in-singapore-feel-safer-in-dorms-others-lamen/1857873 (accessed October 16, 2020). [Google Scholar]
- 66. MOM Introduces More Targeted COVID-19 Quarantine Approach for Foreign Worker Dormitories [channelnewsasia web site]. September 25, 2020. Available at: https://www.channelnewsasia.com/news/singapore/mom-more-targeted-covid-19-quarantine-approach-dorms-13149102 (accessed October 16, 2020). [Google Scholar]
- 67.Du W, Wang G. Indoor air pollution was nonnegligible during COVID-19 lockdown. Aerosol Air Qual Res 2020; 20:1851–1855. [Google Scholar]
- 68.Ezani E, Brimblecombe P, Asha’Ari ZH, et al. Indoor and outdoor exposure to PM2.5 during COVID-19 lockdown in suburban Malaysia. Aerosol Air Qual Res 2020; 21:21.DOI 10.4209/aaqr.2020.07.0476. [Google Scholar]
- 69.Adhikari A, Yin JJ. Short-term effects of ambient ozone, PM2.5, and meteorological factors on COVID-19 confirmed cases and deaths in Queens, New York. Int J Environ Res Public Health 2020; 17:4047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wolcott JA, Zee YC, Osebold JW. Exposure to ozone reduces influenza disease severity and alters distribution of influenza viral antigens in murine lungs. Appl Environ Microb 1982; 44:723–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nguyen JL, Schwartz J, Dockery DW. The relationship between indoor and outdoor temperature, apparent temperature, relative humidity, and absolute humidity. Indoor Air 2014; 24:103–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Koep TH, Enders FT, Pierret C, et al. Predictors of indoor absolute humidity and estimated effects on influenza virus survival in grade schools. BMC Infect Dis 2013; 13:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Guan J, Chan M, VanderZaag A. Inactivation of Avian Influenza Viruses on porous and non-porous surfaces is enhanced by elevating absolute humidity. Transbound Emerg Dis 2017; 64:1254–1261. [DOI] [PubMed] [Google Scholar]
- 74.Marcone V. Reduction of contagion risks by SARS-Cov-2 (COVID-19) in air-conditioned work environments. Pain Physician 2020; 23:S475–S482. [PubMed] [Google Scholar]
- 75.Lapidus N, de Lamballerie X, Salez N, et al. Factors associated with post-seasonal serological titer and risk factors for infection with the pandemic A/H1N1 virus in the French general population. PLoS One 2013; 8:e60127. [DOI] [PMC free article] [PubMed] [Google Scholar]