Abstract
Objective
Secukinumab provided sustained efficacy, low radiographic progression and consistent safety over 52 weeks in patients with psoriatic arthritis (PsA) in the FUTURE 5 study. Here, we report 2-year (end-of-study) results from this study.
Methods
Adults with active PsA were randomised 2:2:2:3 to receive subcutaneous secukinumab 300 mg load (300 mg), 150 mg load (150 mg), 150 mg no load or placebo at baseline; weeks 1, 2, 3 and 4; and every 4 weeks thereafter. Secukinumab could be escalated from 150 mg to 300 mg starting at week 52, if active signs of disease were observed based on physician’s assessment. Assessments at week 104 (2 years) included clinical end points and radiographic damage (mean change in van der Heijde-modified total Sharp score (vdH-mTSS)). Safety analysis included all patients who received ≥1 dose of study medication.
Results
Of the 996 patients randomised, 783 patients (78.6%) completed 2 years of treatment. Improvement in clinical end points was sustained through 2 years. The vdH-mTSS (mean change (SD)) was 0.10 (1.74; 300 mg), 0.52 (2.66; 150 mg) and 0.41 (2.20; 150 mg no load) at 2 years. The proportion of patients with no radiographic progression (change from baseline in vdH-mTSS ≤0.5) at 2 years was 89.5% (300 mg), 82.3% (150 mg) and 81.1% (150 mg no load).
Conclusion
Secukinumab with and without loading regimen provided sustained clinical efficacy and low radiographic progression through 2 years in patients with PsA. No new safety findings were reported.
Trial registration number
Keywords: biological therapy, cytokines, inflammation, arthritis, psoriatic
Key messages.
What is already known about this subject?
Secukinumab, a human monoclonal antibody that directly inhibits interleukin-17A, demonstrated sustained efficacy, low rate of radiographic progression and consistent safety over 52 weeks in patients with psoriatic arthritis (PsA) in the FUTURE 5 study.
What does this study add?
This large phase III study in patients with active PsA showed that subcutaneous secukinumab 300 mg and 150 mg, with or without loading dose, provided sustained clinical efficacy, low radiographic progression and consistent safety over 2 years of treatment, demonstrating the long-term clinical benefit of secukinumab treatment.
The unique aspects of this study are the loading or no loading regimes with option of dose escalation after 52 weeks. Improvement in American College of Rheumatology responses was observed in patients who escalated from secukinumab 150 mg to 300 mg, indicating a potential benefit for dose escalation in patients whose symptoms are not adequately controlled with the lower dose.
How might this impact on clinical practice or further developments?
The findings from this 2-year study strengthen the existing evidence on the safety and efficacy of long-term secukinumab treatment in patients with PsA. There can be a potential benefit in dose escalation if signs and symptoms of PsA are not controlled adequately with the lower dose.
Introduction
Psoriatic arthritis (PsA) is a chronic multifaceted disease characterised by peripheral arthritis, axial disease, dactylitis, enthesitis, and nail and skin psoriasis.1 2 Patients with PsA are affected by irreversible joint damage and disability, which have a substantial impact on quality of life.3–7 Structural damage in patients with PsA is characterised by bone erosions, joint space narrowing and new bone formation, which lead to increased disability.2 Destruction of bone and cartilage with pathological new bone formation is one of the distinctive features of PsA. The evidence of bone loss including eccentric erosions, joint space narrowing and new bone formation is often seen in radiographs of peripheral joints.7 8 In PsA, radiographic progression has been observed in the early course of the disease, and it has been reported that 67% of patients have at least one joint erosion at their first visit to the clinic9 10 and 47% of patients have bone erosions within the first 2 years of disease onset.7 11
Secukinumab, a human monoclonal antibody that directly inhibits interleukin-17A, has demonstrated rapid and sustained efficacy in patients with PsA across the phase III FUTURE studies,12–15 and recently published recommendations for the management of PsA include secukinumab as a first-line biological treatment option after failure of conventional synthetic disease-modifying antirheumatic drugs.16 In the FUTURE 1 study, secukinumab 150 mg provided a low rate of radiographic progression over 3 years and sustained clinical responses over 5 years.17 Secukinumab 300 mg and 150 mg reported sustained efficacy, low rate of radiographic progression and consistent safety over 52 weeks in the FUTURE 5 study.13 18 Here, we report the 2-year (end-of-study) efficacy, radiographic progression and safety results of secukinumab from the FUTURE 5 study.
Methods
Study design and patients
FUTURE 5 is a randomised, double-blind, placebo-controlled, multicentre, 2-year phase III study. The detailed inclusion and exclusion criteria and study design have been reported previously.13 The key exclusion criteria included active/history of ongoing infection, use of ≥3 anti-tumour necrosis factor (TNF) agents, active inflammatory disease other than PsA and prior use of a biologic other than an anti-TNF agent. All eligible patients (≥18 years of age) with active PsA for at least 6 months, who were stratified by prior anti-TNF (anti-TNF-naïve or inadequate response (IR)) use, were randomised (2:2:2:3) to one of the four treatment groups to receive subcutaneous secukinumab 300 mg with loading dose (300 mg), 150 mg with loading dose (150 mg), 150 mg without loading dose (150 mg no load) or placebo at baseline; weeks 1, 2 and 3; and every 4 weeks starting at week 4. At week 16, non-responders in the placebo group (<20% improvement from baseline in tender and swollen joint counts) were switched to receive either secukinumab 300 mg or 150 mg, and all the remaining patients in the placebo group (responders) were switched at week 24. Patients, investigators and assessors remained blinded to the treatment allocation until all patients reached week 52. Stratification was done according to prior use of anti-TNF therapy status (ie, patients who were naïve to anti-TNF therapy (anti-TNF-naïve) and those who were inadequate responders or stopped treatment due to safety or intolerance to an anti-TNF therapy (hereafter collectively referred as anti-TNF-IR)). The study was planned to enrol no more than 30% of anti-TNF-IR patients.
Following a protocol amendment, the secukinumab dose could be escalated from 150 mg to 300 mg every 4 weeks at the beginning of week 52, if active signs of disease were observed in patients based on the physician’s judgement. Patients were not allowed to switch to a lower dose once dose escalation occurred. After week 52, patients were unblinded to the original randomised treatment assignment at randomisation. In addition, treatment was given as open-label, and patients continued to receive the same active dose of secukinumab as open-label treatment, administered until week 100. A follow-up visit was performed 12 weeks after last study treatment administration for all patients, regardless of whether they completed the entire study as planned or discontinued prematurely.
The study was conducted in accordance with the Declaration of Helsinki and was approved by institutional review boards or independent ethics committees at each participating centre. Written informed consent was obtained from all enrolled patients. Data were collected in accordance with Good Clinical Practice guidelines by the study investigators and were analysed by the sponsor.19
Assessments
Assessments at week 104 included the American College of Rheumatology (ACR) 20/50/70 responses, Psoriasis Area and Severity Index 90 and 100 responses, change in 28-joint Disease Activity Score using C reactive protein, Health Assessment Questionnaire–Disability Index scores, and resolution of dactylitis and enthesitis. In addition, the change in proportion of patients after dose escalation from any secukinumab 150 mg to 300 mg was evaluated at week 104 for each category of ACR response (defined as no response: ACR <20; low response: 20≤ACR<50; moderate response: 50≤ACR<70; and high response: ACR ≥70).
Radiographic structural damage was assessed by mean change from baseline in van der Heijde-modified total Sharp score (vdH-mTSS; sum of bone erosion (0–5 in the hands and 0–10 in the feet) and joint space narrowing (0–4) scores) for PsA.20 21 The vdH-mTSS assessment was based on hand/wrist/foot radiographs obtained at baseline and weeks 16 (non-responders), 24, 52 and 104, assessed by two blinded readers independently (plus an adjudicator if required) who were blinded to all patient information, treatment allocation and order of radiographs. The total radiographic score (hands and feet combined) ranged from 0 to 528, with higher scores indicating more articular damage. A change from baseline in vdH-mTSS ≤0.5 or ≤0.0 was defined as no structural progression, as recommended by van der Heijde et al.20 Overall safety and tolerability of secukinumab over 104 weeks were assessed by monitoring adverse events (AEs), serious AEs (SAEs), laboratory assessments and vital signs.
Statistical analyses
Data are presented for patients originally randomised to secukinumab including placebo switchers up to week 104. Clinical efficacy and radiographic results up to week 104 are reported as observed data (evaluable patients). For all patients originally randomised to secukinumab, ACR20 and ACR50 responses up to week 104 using multiple imputation (MI) are also reported. Available data after dose escalation were used (not censored) and missing responses were imputed using MI in a visit-by-visit manner. At each visit, a logistic regression model was used for imputation with a covariate of weight, baseline factors treatment and anti-TNF response status, and postbaseline factors of responses from previous visits and dose escalation status (yes or no) from previous and current visits. This regression model used a missing-at-random assumption, and multiply imputed data sets were combined according to Rubin’s rule. Cumulative probability plot was generated to show the vdH-mTSS for all patients according to dose group from baseline to week 104. Subgroup analyses stratified by anti-TNF therapy status (anti-TNF-naïve or anti-TNF-IR) were prespecified. Radiographic analysis included evaluable patients at baseline and weeks 24, 52 and 104. A sensitivity analysis of the radiographic data was performed after the statistical analysis of the data revealed that one patient exhibited extreme values. Safety analyses included all patients who received ≥1 dose of secukinumab and were summarised descriptively.
Results
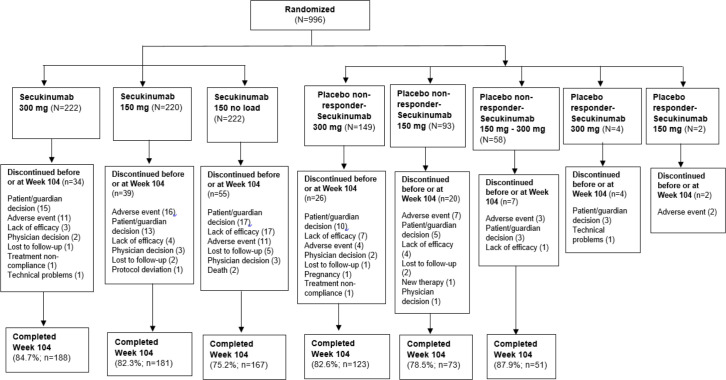
Of the 996 patients randomised at baseline, 783 patients (78.6%) completed 2 years (104 weeks) of treatment. A total of 84.7% (188/222), 82.3% (181/220) and 75.2% (167/222) patients originally randomised to secukinumab 300 mg, 150 mg and 150 mg no loading dose, respectively, completed 2 years of treatment (figure 1). Of the 664 patients originally randomised to secukinumab, 128 patients (19.3%) discontinued before or at week 104. The most common reason for premature discontinuation was patient/guardian decision: 6.8% in the 300 mg group, 5.9% in the 150 mg group and 7.7% in the 150 mg no load group. Lack of efficacy was reported in 1.4% of patients in 300 mg group, 1.8% of patients in 150 mg group and 7.7% of patients in 150 mg no load group.
Figure 1.
Patients’ disposition through week 104. Twenty-six patients from placebo groups discontinued on or before week 16 and were not classified as responders or non-responders.
The disposition of patients up to week 104 is presented in figure 1; disposition up to week 52 was reported previously.13 18 Overall, 39% (86/220) of patients from secukinumab 150 mg load group and 41% (92/222) of patients from secukinumab 150 mg no load group were escalated to secukinumab 300 mg beginning at week 52. Demographics and baseline disease characteristics of patients were balanced between treatment groups and have been reported previously.13 At baseline, approximately 50% of patients were receiving concomitant methotrexate across all treatment groups, and nearly one-third of patients were on anti-TNF-IR across all treatment groups.
Clinical efficacy
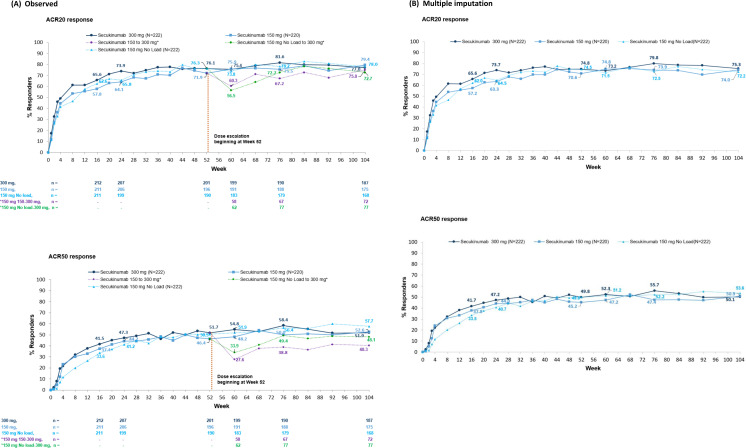
Clinical improvements reported at week 16 were sustained through 2 years in those patients who were originally randomised to secukinumab and continued to receive secukinumab treatment through 2 years (figure 2 and table 1).
Figure 2.
ACR20 and ACR50 responses through 2 years. All data through week 104 calculated using (A) observed and (B) multiple imputation for patients originally randomised to secukinumab 300 mg, 150 mg and 150 mg no loading dose. *In observed data (A), ‘150 mg group’ included patients who were originally randomised and those who had dose escalation and ‘150 mg No load’ group included patients who were originally randomised and those who had dose escalation from week 60 to week 104, where available data after dose escalation were used (not censored). ACR, American College of Rheumatology. n, number of patients in the treatment group with ACR evaluation.
Table 1.
Summary of clinical efficacy through week 104, data as observed
| Efficacy end points | Week 16 | Week 52 | Week 104 | ||||||
| 300 mg (N=222) |
150 mg (N=220) |
150 mg no load (N=222) |
300 mg (N=222) |
150 mg (N=220) |
150 mg no load (N=222) |
300 mg (N=222) |
150 mg* group (N=220) |
150 mg* no load group (N=222) | |
| ACR70 response, % (n) | 21.2 (212) | 19.0 (211) | 15.6 (211) | 31.8 (201) | 29.1 (196) | 28.9 (190) | 34.8 (187) | 33.1 (175) | 44.0 (168) |
| PASI 90 response†, % (n) | 54.6 (108) | 38.0 (121) | 32.7 (113) | 61.8 (102) | 52.7 (112) | 47.1 (102) | 70.1 (97) | 59.2 (103) | 62.6 (91) |
| PASI 100 response†, % (n) | 34.3 (108) | 22.1 (122) | 19.5 (113) | 48.0 (102) | 36.3 (113) | 35.3 (102) | 49.5 (97) | 44.2 (104) | 40.7 (91) |
| DAS28-CRP score, mean change from BL±SD (n) | −1.5±1.3 (209) | −1.4±1.2 (208) | −1.3±1.2 (210) | −1.9±1.2 (201) |
−1.8±1.1 (194) |
−1.9±1.3 (189) | −2.1±1.2 (182) | −2.1±1.1 (172) |
−2.2±1.1 (165) |
| HAQ-DI score, mean change from BL±SD (n) | −0.55±0.57 (211) | −0.46±0.55 (210) | −0.49±0.57 (211) | −0.58±0.6 (199) | −0.53±0.6 (195) | −0.60±0.7 (190) | −0.58±0.6 (186) | −0.57±0.6 (177) | −0.62±0.7 (169) |
| Enthesitis resolution‡, % (n) | 56.5 (138) | 56.2 (137) | 44.3 (122) | 78.0 (127) | 69.0 (129) | 68.7 (115) | 78.0 (118) | 80.3 (117) | 69.5 (95) |
| Dactylitis resolution‡, % (n) | 66.7 (81) | 58.2 (79) | 58.0 (100) | 80.6 (72) |
82.9 (70) |
81.6 (87) | 82.8 (64) | 85.5 (62) |
89.3 (75) |
Results are reported as observed data.
*150 mg groups include patients who escalated to 300 mg.
†Analysis performed in randomised patients with psoriasis (psoriasis subset) affecting ≥3% body surface area at baseline; n=110 (300 mg), 125 (150 mg) and 117 (150 mg no load).
‡Resolution of enthesitis and dactylitis is shown for patients with symptoms at baseline.
%, percentage of responses; ACR, American College of Rheumatology response criteria; BL, baseline; DAS28-CRP, 28-joint Disease Activity Score using C reactive protein; HAQ-DI, HAQ–Disability Index; n, number of patients in the treatment group with evaluation at weeks 16, 52 and 104; N, number of randomised patients; PASI, Psoriasis Area and Severity Index.
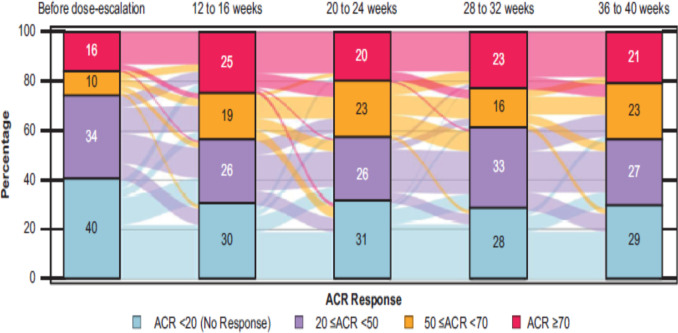
An increase in ACR20 (56.5% to 72.7%) and ACR50 (33.9% to 48.1%) responses was observed from week 60 to week 104 in patients who had dose escalation from secukinumab 150 mg no load to 300 mg (figure 2A). At week 104, ACR20/50 response rates using MI in the secukinumab 300 mg, 150 mg, and 150 mg no load groups were 75.3%/50.1%, 74.0%/50.9% and 72.2%/53.6%, respectively (figure 2B). Clinical efficacy in placebo switchers (patients originally randomised to placebo who switched to secukinumab) was also sustained through 2 years (online supplemental table 1). Sustained efficacy was observed in both anti-TNF-naïve and anti-TNF-IR patients (online supplemental table 2). In patients whose dose was escalated from secukinumab 150 mg to 300 mg, ACR20 and ACR50 responses increased from 60.3% (ACR20) and 27.6% (ACR50) to 75% (ACR20) and 40.3% (ACR50), respectively, from week 60 to week 104. The Sankey-style plot presented in figure 3 shows the proportion of patients with different levels of ACR response before and up to 36–40 weeks after dose escalation among patients with ACR assessment within all corresponding week intervals. The proportion of ACR responders increased from 60% before dose escalation to 71% after 36–40 weeks following escalation from secukinumab 150 mg to 300 mg. Improvements in the proportions of ACR responders increased in both anti-TNF-naïve and anti-TNF-IR subgroups (online supplemental tables 3 and 4).
Figure 3.
ACR response up to 36–40 weeks after dose escalation from 150 mg to 300 mg. ACR, American College of Rheumatology. Before dose-escalation is defined as the last assessment done on or before a patient took the 300 mg dose. The colors flowing in the background indicate the proportion of patients changing the response over time. Number of subjects evaluated, n=137. First dose-escalation observed at study week 52.
rmdopen-2021-001600supp001.pdf (67.3KB, pdf)
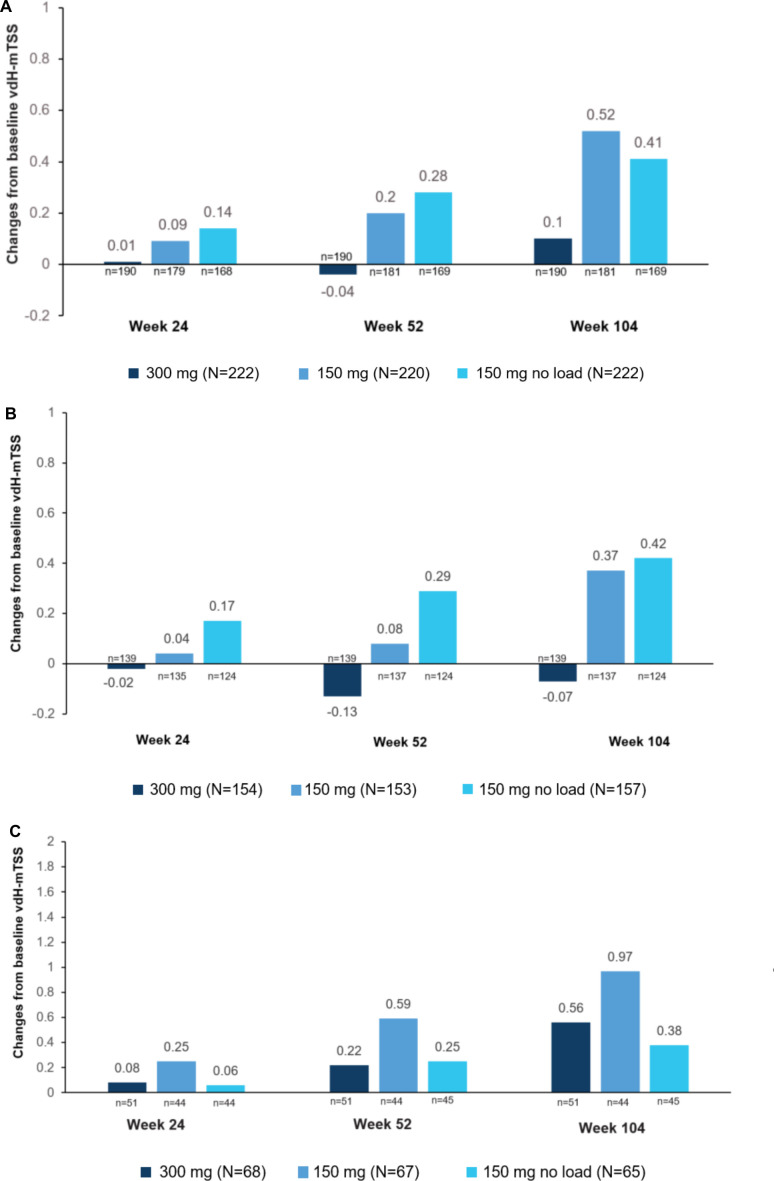
Radiographic progression
Sustained low rates of radiographic progression were observed through week 104. Mean changes from baseline in vdH-mTSS through 2 years in the overall population and by anti-TNF status are shown in figure 4. At week 52, mean changes from baseline in vdH-mTSS (observed data (SD)) were −0.04 (1.02), 0.20 (1.83) and 0.28 (1.34) in the secukinumab 300 mg, 150 mg and 150 mg no load groups, respectively, in the overall population. At week 104, mean changes from baseline in vdH-mTSS (observed data (SD)) were 0.10 (1.74), 0.52 (2.66) and 0.41 (2.20) in the secukinumab 300 mg, 150 mg and 150 mg no load groups, respectively. The proportion of patients with no radiographic progression (change from baseline in vdH-mTSS ≤0.5) with secukinumab at 104 weeks was 89.5% (300 mg), 82.3% (150 mg) and 81.1% (150 mg no load), respectively. The proportion of patients with change from baseline in vdH-mTSS ≤0.0 was 81.2% (300 mg), 69.1% (150 mg) and 73.4% (150 mg no load), respectively.
Figure 4.
Mean changes in vdH-mTSS scores from baseline through week 104. (A) Overall population, (B) anti-TNF-naïve and (C) anti-TNF-IR. Analyses at weeks 24, 52 and 104 were done by observed data. In the 300 mg dose group there was one outlier (anti-TNF-IR patient) with a very high mTSS change from baseline (week 104 analysis). Analysis was based on the patients with evaluable X-rays at both baseline and week 104. n, number of patients with evaluable X-rays at both baseline and week 104. At each time point, only patients with a value at both baseline and that time point are included. TNF, tumour necrosis factor; vdH-mTSS, van der Heijde-modified total Sharp score.
In patients with prior anti-TNF therapy status, mean changes from baseline in vdH-mTSS followed a similar trend of low radiographic progression (figure 4). The anti-TNF-naïve group showed lower radiographic progression than the anti-TNF-IR group. At week 104, no radiographic progression (change from baseline in vdH-mTSS ≤0.5) was observed in 92.8% (300 mg), 83.9% (150 mg) and 84.7% (150 mg no load) of anti-TNF-naïve patients and in 80.8% (300 mg), 77.3% (150 mg) and 71.1% (150 mg no load) of anti-TNF-IR patients, respectively. The proportion of patients with change from baseline in vdH-mTSS ≤0.0 was 83.5% (300 mg), 70.8% (150 mg) and 75% (150 mg no load) in anti-TNF-naïve patients and 75% (300 mg), 63.6% (150 mg) and 68.9% (150 mg no load) in anti-TNF-IR patients, respectively.
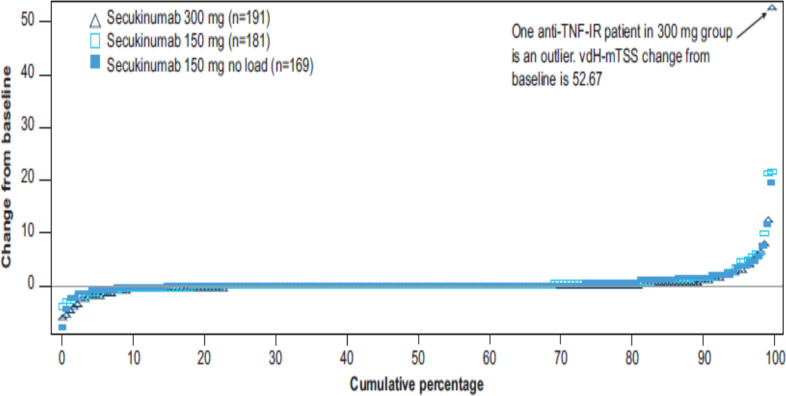
Cumulative probability plots in vdH-mTSS change from baseline to week 104 showed the scores of the individual patients in different secukinumab doses over 104 weeks of treatment. The structural progression of individual patients at week 104 is presented in figure 5. In the 300 mg dose group, there was one outlier (anti-TNF-IR patient) with a very high mTSS change from baseline to week 104 (change from baseline was 52.67). The outlier in the secukinumab 300 mg group drove the mean change from baseline for this group at week 104 compared with weeks 24 and 52. The mean vdH-mTSS change at week 104 from baseline with the patient included is 1.56 and without the patient included is 0.56.
Figure 5.
Cumulative probability plot of vdH-mTSS at week 104. TNF-IR, tumour necrosis factor inadequate response; vdH-mTSS, van der Heijde-modified total Sharp score.300 mg (N=222), 150 mg (N=220), 150 no load (N=222); N: randomised patients; n: number of patients with evaluable X-rays at both baseline and week 104. 150 mg and 150 mg no load groups included 77 and 79 patients with radiographic results, respectively, who had dose escalation at week 52 or later.
Safety
Over the entire treatment period, the mean secukinumab exposure was 667.4 days (1761.5 patient-years). The rate of discontinuation due to any AE was low and similar between secukinumab 300 mg (4.4%) and 150 mg (4.6%) dose groups. Exposure-adjusted incidence rates (EAIRs) for treatment emergent SAEs were 8.0 in secukinumab 300 mg group and 8.6 in secukinumab 150 mg group. The most frequently reported AEs in any secukinumab group (EAIR ≥5) were nasopharyngitis and upper respiratory tract infection (table 2).
Table 2.
Safety with secukinumab during the entire treatment period through week 104
| Parameter | Any secukinumab 300 mg (N=607) |
Any secukinumab 150 mg (N=593) |
Any secukinumab (N=964) |
| Exposure | |||
| Mean, days±SD | 542.2±214.76 | 529.9±224.86 | 667.4±184.35 |
| Pt-yrs | 901.1 | 860.3 | 1761.5 |
| AEs, n (EAIR/100 pt-yrs) | 448 (129.2) | 478 (163.0) | 792 (139.8) |
| SAEs, n (EAIR/100 pt-yrs) | 68 (8.0) | 70 (8.6) | 131 (7.9) |
| AEs leading to discontinuation, n (%) | 27 (4.4) | 27 (4.6) | 54 (5.6) |
| Deaths, n (%) | 1 (0.2) | 2 (0.3) | 3 (0.3) |
| Most frequent AEs, n (EAIR/100 pt-yrs)* | |||
| Nasopharyngitis | 73 (8.9) | 80 (10.3) | 148 (9.4) |
| Upper respiratory tract infection | 57 (6.7) | 71 (9.0) | 121 (7.5) |
| AEs of special interest, n (EAIR/100 pt-yrs) | |||
| Neutropenia | 5 (0.6) | 10 (1.2) | 15 (0.9) |
| Oral candidiasis | 8 (0.9) | 3 (0.4) | 11 (0.6) |
| MACE | 2 (0.2) | 1 (0.1) | 3 (0.2) |
| Crohn’s disease† | 1 (0.1) | 2 (0.2) | 2 (0.1) |
| Ulcerative colitis | 0 | 1 (0.1) | 1 (0.1) |
The ‘any secukinumab’ group includes patients who experienced AEs at least once on either of the doses.
Patient-years (pt-yrs) is calculated as a sum of individual patient durations in days divided by 365.25. If a patient experienced an AE after dose escalation, the corresponding AE was counted in 300 mg group.
*AEs that occurred with an EAIR of at least 5.0 cases per 100 pt-yrs in either any secukinumab 300 mg or 150 mg mg group over the entire treatment period
†There is one patient in 150 mg no load arm who reported Crohn’s disease. After the dose escalated to 300 mg, the same patient reported Crohn’s disease again. So essentially the same patient counted in any 300 mg group and in any 150 mg group.
AEs, adverse events; EAIR, exposure-adjusted incidence rates; MACE, major adverse cardiovascular event; SAEs, serious adverse events.
The EAIRs of selected AEs of interest observed with secukinumab are shown in table 2. A total of three MACE events were reported. One patient in any secukinumab 300 mg group was adjudicated as spontaneous myocardial infarction. Of the two patients who were reported to have (possible) stroke and identified for adjudication, one patient in any secukinumab 300 mg group was reported to have a cerebral haemorrhage that was confirmed as a stroke, and another patient in any secukinumab 150 mg group was reported to have a lacunar infarction that was adjudicated as not a stroke. One patient in any secukinumab 150 mg was reported to have cardiopulmonary arrest that was confirmed as a sudden cardiovascular death. Inflammatory bowel disease was reported in five patients; two patients reported Crohn’s disease (one with a history of Crohn’s disease and another with a history of colitis), one with a new diagnosis of ulcerative colitis, one colonic abscess and one ulcerative proctitis. Oesophageal candidiasis was reported in one patient in secukinumab 150 mg group. A total of three deaths were reported, one in any secukinumab 300 mg due to sepsis and two in any secukinumab 150 mg due to acute myocardial infarction and cardiorespiratory arrest; none were considered related to study drug as assessed by the investigator. The safety profile of secukinumab in this study showed no new or unexpected safety signals.
Discussion
In this large phase III study in patients with active PsA, secukinumab 300 mg and 150 mg, with or without loading dose, provided sustained clinical efficacy, low radiographic progression and consistent safety over 2 years of treatment, demonstrating the long-term clinical benefit of secukinumab treatment. The majority (78.6%) of patients remained in the study for the full 2 years. A slightly lower completion rate was observed in the 150 mg no load group with patient/guardian decision and lack of efficacy the main reasons for discontinuation. After secukinumab dose escalation from 150 mg to 300 mg, the proportion of ACR20 and ACR50 responders increased. Notably, the percentage of patients with ACR response ≥50 (ACR50 and ACR70 responders) increased after dose escalation in both anti-TNF-naïve and anti-TNF-IR subgroups.
Sustained improvement was observed in secukinumab-treated patients across efficacy end points through 2 years, which is in agreement with the findings of previous secukinumab studies in PsA.15 17 22–25 The majority (81.1%–89.5%) of secukinumab-treated patients in the overall population showed no radiographic progression (change from baseline in vdH-mTSS ≤0.5) at 2 years. Low rates of radiographic progression were observed in secukinumab-treated patients with PsA regardless of the previous anti-TNF treatment status, with lower radiographic progression observed in the anti-TNF-naïve subgroup than in the anti-TNF-IR subgroup. These results are consistent with previous results with secukinumab.13 17 18 26
The safety profile was consistent with previous reports from secukinumab trials and with the results of a retrospective safety analysis of 21 secukinumab clinical trials across different indications.12–15 27
This study was not designed to compare between treatment regimens (secukinumab load vs no load) or to assess treatment differences by previous anti-TNF therapy status, so these data need to be interpreted with caution. Furthermore, minimal clinically important differences are not reported in the article, which may limit the value of results in clinical practice.
In conclusion, subcutaneous secukinumab 300 mg and 150 mg with and without loading dose provided sustained improvement in clinical responses and low rates of radiographic progression through 2 years of therapy in patients with PsA who remain on the treatment for 2 years. Improvement in ACR responses was observed in patients who escalated from secukinumab 150 mg to 300 mg, indicating a potential benefit for dose escalation in patients whose symptoms were not adequately controlled with the lower dose. Secukinumab was well tolerated with no new or unexpected safety signals reported. Overall, the findings from this study strengthen the existing evidence on the efficacy of long-term secukinumab treatment in patients with PsA.
Acknowledgments
We thank the patients who participated in this study and the study investigators for their contributions. Rajeeb Ghosh (Novartis) provided medical writing support and John Gallagher (Novartis) provided medical and editorial guidance in accordance with Good Publication Practice guidelines.
Footnotes
Funding: This study was supported by Novartis Pharma AG, Switzerland.
Competing interests: PJM has received research grants, consulting and speaking fees from AbbVie, Amgen, Eli Lilly, Janssen, Novartis, Pfizer and UCB; research grants and consulting fees from Bristol-Myers Squibb, Galapagos, Gilead and Sun; and consulting fees from Boehringer Ingelheim and GlaxoSmithKliine. RBL has received consulting fees from AbbVie, Novartis, EliLilly, UCB, Pfizer, Galapagos and Gilead. PR has received research grants from Janssen and Novartis, and consulting and speaking fees from AbbVie, Amgen, BMS, Celgene, Eli Lilly, Janssen, Merck, Novartis, Pfizer and UCB. HT, AS and EB have nothing to disclose. SN has received research grants from Novartis and Johnson & Johnson, and consulting fees from Novartis, Johnson & Johnson and Pfizer. AR is an employee of Novartis, with Novartis stock. SM is an employee of Novartis, with Novartis stock. EMD was an employee of Novartis and LP is an employee of Novartis. DvdH has received consulting fees from AbbVie, Amgen, Astellas, AstraZeneca, Bayer, BMS, Boehringer Ingelheim, Celgene, Cyxone, Daiichi, Eisai, Eli-Lilly, Galapagos, Gilead, Glaxo-Smith-Kline, Janssen, Merck, Novartis, Pfizer, Regeneron, Roche, Sanofi, Takeda and UCB Pharma. DvdH is a Director of Imaging Rheumatology
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
The data sets generated and/or analysed during this study are not publicly available. Novartis is committed to sharing with qualified external researchers the access to patient-level data and supporting clinical documents from eligible studies. These requests are reviewed and approved on the basis of scientific merit. All data provided are anonymised to respect the privacy of patients who have participated in the trial, in line with applicable laws and regulations. The data may be requested from the corresponding author of the manuscript.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Taylor W, Gladman D, Helliwell P, et al. Classification criteria for psoriatic arthritis: development of new criteria from a large international study. Arthritis Rheum 2006;54:2665–73. 10.1002/art.21972 [DOI] [PubMed] [Google Scholar]
- 2.Gladman DD, et al. Psoriatic arthritis: epidemiology, clinical features, course, and outcome. Ann Rheum Dis 2005;64:ii14–17. 10.1136/ard.2004.032482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gladman DD. Psoriatic arthritis. Rheum Dis Clin North Am 1998;24:829–44. 10.1016/S0889-857X(05)70044-2 [DOI] [PubMed] [Google Scholar]
- 4.Kavanaugh A, Helliwell P, Ritchlin CT. Psoriatic arthritis and burden of disease: patient perspectives from the population-based multinational assessment of psoriasis and psoriatic arthritis (MAPP) survey. Rheumatol Ther 2016;3:91–102. 10.1007/s40744-016-0029-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coates LC, Kavanaugh A, Mease PJ, et al. Group for research and assessment of psoriasis and psoriatic arthritis 2015 treatment recommendations for psoriatic arthritis. Arthritis Rheumatol 2016;68:1060–71. 10.1002/art.39573 [DOI] [PubMed] [Google Scholar]
- 6.Bond SJ, Farewell VT, Schentag CT, et al. Predictors for radiological damage in psoriatic arthritis: results from a single centre. Ann Rheum Dis 2007;66:370–6. 10.1136/ard.2006.056457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ritchlin CT, Colbert RA, Gladman DD. Psoriatic arthritis. N Engl J Med 2017;376:957–70. 10.1056/NEJMra1505557 [DOI] [PubMed] [Google Scholar]
- 8.Poggenborg RP, Østergaard M, Terslev L. Imaging in psoriatic arthritis. Rheum Dis Clin North Am 2015;41:593–613. 10.1016/j.rdc.2015.07.007 [DOI] [PubMed] [Google Scholar]
- 9.Gladman DD, Shuckett R, Russell ML, et al. Psoriatic arthritis (PSA)--an analysis of 220 patients. Q J Med 1987;62:127–41. [PubMed] [Google Scholar]
- 10.Alonso JCT, Perez AR, Castrillo JMA, et al. Psoriatic arthritis (PA): a clinical, immunological and radiological study of 180 patients. Rheumatology 1991;30:245–50. 10.1093/rheumatology/30.4.245 [DOI] [PubMed] [Google Scholar]
- 11.Kane D, et al. A prospective, clinical and radiological study of early psoriatic arthritis: an early synovitis clinic experience. Rheumatology 2003;42:1460–8. 10.1093/rheumatology/keg384 [DOI] [PubMed] [Google Scholar]
- 12.McInnes IB, Mease PJ, Kirkham B, et al. Secukinumab, a human anti-interleukin-17A monoclonal antibody, in patients with psoriatic arthritis (FUTURE 2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2015;386:1137–46. 10.1016/S0140-6736(15)61134-5 [DOI] [PubMed] [Google Scholar]
- 13.Mease P, van der Heijde D, Landewé R, et al. Secukinumab improves active psoriatic arthritis symptoms and inhibits radiographic progression: primary results from the randomised, double-blind, phase III FUTURE 5 study. Ann Rheum Dis 2018;77:890–7. 10.1136/annrheumdis-2017-212687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mease PJ, McInnes IB, Kirkham B, et al. Secukinumab inhibition of interleukin-17A in patients with psoriatic arthritis. N Engl J Med 2015;373:1329–39. 10.1056/NEJMoa1412679 [DOI] [PubMed] [Google Scholar]
- 15.Nash P, Mease PJ, McInnes IB, et al. Efficacy and safety of secukinumab administration by autoinjector in patients with psoriatic arthritis: results from a randomized, placebo-controlled trial (FUTURE 3). Arthritis Res Ther 2018;20:47. 10.1186/s13075-018-1551-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gossec L, Baraliakos X, Kerschbaumer A, et al. EULAR recommendations for the management of psoriatic arthritis with pharmacological therapies: 2019 update. Ann Rheum Dis 2020;79:700.1–12. 10.1136/annrheumdis-2020-217159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mease PJ, Kavanaugh A, Reimold A, et al. Secukinumab in the treatment of psoriatic arthritis: efficacy and safety results through 3 years from the year 1 extension of the randomised phase III FUTURE 1 trial. RMD Open 2018;4:e000723. 10.1136/rmdopen-2018-000723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van der Heijde D, Mease PJ, Landewé RBM, et al. Secukinumab provides sustained low rates of radiographic progression in psoriatic arthritis: 52-week results from a phase 3 study, FUTURE 5. Rheumatology 2020;59:1325–34. 10.1093/rheumatology/kez420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Medical Association . World Medical association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 2013;310:2191–4. 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 20.van der Heijde D, Landewé R, Klareskog L, et al. Presentation and analysis of data on radiographic outcome in clinical trials: experience from the tempo study. Arthritis Rheum 2005;52:49–60. 10.1002/art.20775 [DOI] [PubMed] [Google Scholar]
- 21.van der Heijde D. How to read radiographs according to the Sharp/van Der Heijde method. J Rheumatol 1999;26:261–3. [PubMed] [Google Scholar]
- 22.McInnes IB, Mease PJ, Kivitz AJ, et al. Long-Term efficacy and safety of secukinumab in patients with psoriatic arthritis: 5-year (end-of-study) results from the phase 3 FUTURE 2 study. Lancet Rheumatol 2020;2:e227–35. 10.1016/S2665-9913(20)30036-9 [DOI] [PubMed] [Google Scholar]
- 23.Kivitz AJ, Nash P, Tahir H, et al. Efficacy and Safety of Subcutaneous Secukinumab 150 mg with or Without Loading Regimen in Psoriatic Arthritis: Results from the FUTURE 4 Study. Rheumatol Ther 2019;6:393–407. 10.1007/s40744-019-0163-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McInnes IB, Mease PJ, Ritchlin CT, et al. Secukinumab sustains improvement in signs and symptoms of psoriatic arthritis: 2 year results from the phase 3 FUTURE 2 study. Rheumatology 2017;56:1993–2003. 10.1093/rheumatology/kex301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kavanaugh A, Mease PJ, Reimold AM, et al. Secukinumab for long-term treatment of psoriatic arthritis: a two-year followup from a phase III, randomized, double-blind placebo-controlled study. Arthritis Care Res 2017;69:347–55. 10.1002/acr.23111 [DOI] [PubMed] [Google Scholar]
- 26.van der Heijde D, Landewé RB, Mease PJ, et al. Brief report: Secukinumab provides significant and sustained inhibition of joint structural damage in a phase III study of active psoriatic arthritis. Arthritis Rheumatol 2016;68:1914–21. 10.1002/art.39685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Deodhar A, Mease PJ, McInnes IB, et al. Long-Term safety of secukinumab in patients with moderate-to-severe plaque psoriasis, psoriatic arthritis, and ankylosing spondylitis: integrated pooled clinical trial and post-marketing surveillance data. Arthritis Res Ther 2019;21:111. 10.1186/s13075-019-1882-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
rmdopen-2021-001600supp001.pdf (67.3KB, pdf)
Data Availability Statement
The data sets generated and/or analysed during this study are not publicly available. Novartis is committed to sharing with qualified external researchers the access to patient-level data and supporting clinical documents from eligible studies. These requests are reviewed and approved on the basis of scientific merit. All data provided are anonymised to respect the privacy of patients who have participated in the trial, in line with applicable laws and regulations. The data may be requested from the corresponding author of the manuscript.