Abstract
Objectives:
Recent technological advances have led to the capability of performing high resolution imaging of the tympanic membrane. Smartphone technologies and applications have provided the opportunity to capture digital images and easily share them. The smartphone otoscope device was developed as a simple system that can convert a smartphone into a digital otoscope. This device has the prospective ability to improve physician-patient communication and assist with the diagnosis and management of ear disease. Our objective was to evaluate the feasibility and physician/parental satisfaction
Methods:
Children between six months and 15 years of age at an urban tertiary children’s hospital that were scheduled for bilateral tympanostomy tube insertion or underwent bilateral tympanostomy tube surgery were prospectively enrolled in the study. Comparisons were made between parental home-recorded videos and findings during in-office otoscopy. Two independent otolaryngologists reviewed the videos and concordance between inter-rater agreements was calculated. Acceptability and use questionnaires were administered to physicians and parents.
Results:
There was good intra-rater agreement between traditional otoscopy and video-otoscopy for tube extruding, tube blocked and tube extruded with at least 80% agreement (p<0.05) and excellent inter-rater agreement between physicians for nearly all tube variables (p<0.0001) There was a high degree of satisfaction with this mode of surveillance. Parents and physicians agreed that the Cellscope® smartphone was easy to use, helpful with the occurrence of acute events, and appeared to improve quality of care.
Conclusions:
Oto is feasible for use in tympanostomy tube surveillance. Use of the Oto may allow otolaryngologists to easily follow a child’s tympanostomy tube remotely over time and offer greater parental satisfaction.
Keywords: tympanostomy tubes, smartphone otoscope, pediatric
1. INTRODUCTION
Tympanostomy tube (TT) placement is one of the most common pediatric surgical procedures performed in the United States1,2. Post-operative complications can occur with the use of both short and long term tubes and include otorrhea, tube blockage, premature tube extrusion, granulation tissue formation, tympanic membrane perforation, tympanic membrane atrophy, tympanic membrane retraction pocket and cholesteatoma3. With the exception of TT otorrhea, many of these complications are rare3. However, early detection and management of these sequelae are necessary to reduce long-term morbidity. It is estimated that a large number of children present to their otolaryngologist in a delayed fashion for treatment of a TT complication that could likely have been avoided.
To date, there is a paucity of evidence to guide the post-operative surveillance of tubes and controversy exists between physicians regarding practice guidelines4. The American Academy of Otolaryngology currently recommends routine otolaryngology examinations of a child with tympanostomy tubes at no longer than 6-month intervals until the tubes are extruded and complete tympanic membrane healing, adequate Eustachian tube function and normal hearing are established4. But additional follow-up visits may also be necessary for episodes of otorrhea or other otologic complaints. Follow-up care for tubes may not only be challenging but expensive for some families. The financial burden of TTs and acute otitis media events related to emergency room visits, clinic visits, antibiotic prescriptions, travel and missed work can be considerable.
With the recent unfolding of the COVID-19 pandemic, our healthcare system is in drastic need of measures to cut costs and establish mechanisms to deliver care remotely via telemedicine.
Recent technological advances have led to the capability of performing high resolution imaging of the tympanic membrane that provide the opportunity to not only capture digital images and video but also easily share them. The smartphone otoscope device was developed as a simple clip-on system that can convert a smartphone into a digital otoscope. This device has the prospective ability to improve physician-patient communication and assist with the diagnosis and management of ear disease. Its capacity for home use with transmission of images to a physician for review is another potential advantage.
This study evaluated the feasibility of the Cellscope® smartphone attachment (Oto) (CellScope, Inc. San Francisco, CA) for use in the surveillance of TTs in the home environment. The ability to capture images of the tympanic membrane and see them remotely may allow the otolaryngologist to easily follow a child’s tubes over time and offer greater parental satisfaction. Early identification of TT complications could also assist physicians in providing more effective treatment.
2. MATERIALS AND METHODS
2.1. Ethical considerations
This study was approved by the CHLA Institutional Review Board and written permission was obtained from all parents and assent from children over the age of seven.
We conducted a prospective cohort pilot study utilizing convenience sampling in the setting of an urban tertiary children’s hospital, Children’s Hospital Los Angeles. Home videos were conducted by parents at their respective homes in the area. Children who were scheduled for bilateral TT insertion or underwent bilateral TT surgery within the previous six months were recruited for participation in the study via convenience sampling. All children had a history of recurrent acute otitis media and had unilateral or bilateral middle ear effusions at the time of initial assessment for tube candidacy. With the exception of two children who underwent a second set of tubes, the majority of children had no prior TT history. Parents were required to own a compatible iPhone and be fluent in written and spoken English. Children were excluded if they had a focal abnormality of the tympanic membrane; had cardiac, renal or neuromuscular disease; chromosomal abnormalities; autism or developmental delay; or any neurologic disorders.
2.2. Variables and Study Procedures
Information was extracted from participant medical records including date of birth, height and weight, gender, medications, surgical and medical history, and race. At enrollment, all parents were provided with the Cellscope Oto attachment (CellScope Inc., San Francisco, CA) (Figure 1) and given instructions on its use. Study staff assisted parents with downloading the app, registering the pre-determined study profile, and fitting the attachment on the parents’ iPhone with a demonstration and instruction on how to take a video. Parents were instructed to practice capturing videos at home and to take a monthly video of each of their child’s ears and upload the videos through the corresponding Cellscope smartphone application and HIPAA-compliant web portal. Reminders via email or phone calls from the study coordinator were made to parents prior to each monthly video. Both study physicians, who were board-certified otolaryngologists, reviewed these monthly videos and completed a corresponding data collection form for each video within 24–48 hours of it being sent. During video review, the otolaryngologists considered the following variables and noted whether it was present bilaterally (B), in the left (L) or right (R) ear, or neither ear (blank): “Tube in place,” “Tube patent,” “Tube extruding,” “Tube extruded,” “Tube blocked,” “Otorrhea/drainage,” Granulation tissue,” “Middle ear effusion,” “Acute otitis media,” “Tympanic membrane retraction,” “Tympanic membrane perforation,” “Cerumen,” and “Unable to visualize tympanic membrane”.
Figure 1.

The Cellscope Oto
Children were followed as per standard of care, with clinic visits at one month post-surgery and approximately every six months thereafter. For each in-office visit, a home video was taken one day prior for comparison to conventional in-office otoscopy. The video was reviewed and a data collection form completed by one of the study physician prior to the office visit. Pneumatic otoscopy was done routinely during the office visit by the same physician and a second data collection form was completed. Binocular microscopy was performed in those children who required concurrent cerumen removal.
Parents were also instructed to obtain and send videos for any acute, ear-related symptoms during the study period. Attached comments regarding their child’s symptoms were also sent via the web portal. Unscheduled videos were reviewed by a study physician within four hours and instructions regarding further care given via the web portal. For each video, parents were instructed to complete a corresponding paper log, documenting any associated symptoms and medications taken
2.2.1. Questionnaires
Three questionnaires were developed by the study team to assess the feasibility and acceptability of the Cellscope by parents and otolaryngologists. The questionnaires were administered to all parents at their second follow up visit (approximately six months after TT surgery) and again at the end of study follow up (either 24 months after TT surgery or sooner if subject left the study). The questionnaire included questions with 3-point Likert scale response options: 1- agree; 2- no opinion; 3- disagree options (Table 1). Additionally, parents were asked to take a questionnaire if they had sent an unscheduled video for an acute problem during the study period which assessed the utility of the Oto and web portal for acute ear-related symptoms (Table 2).
Table 1.
Subject characteristics
| Characteristic | Total N=16 |
|---|---|
| Age in years (median, IQR)(Range) | 1.7 (1.1–3.0) (8.4 months – 7 years) |
| Female (No., %) | 11 (69) |
| Race (No., %) | |
| Non-Hispanic White/White | 12 (75) |
| Type of tube inserted (No., %) | |
| Armstrong | 12 (75) |
| Other | 4 (25) |
| Duration of device use (average months, range) |
16 (6–24) |
| Time since TT surgery (average months, range) |
17 (6–24) |
Table 2.
Agreement between scheduled home video and in-office evaluation of same rater
| Variable | Number of videos on which both methods agree | Number of videos on which methods disagree | Cohen’s kappa | P-value |
|---|---|---|---|---|
| Cerumen | 37 (84%) | 7 (16%) | NA | - |
| Tube patent | 30 (68%) | 14 (32%) | 0.48 | <0.0001 |
| Tube in place | 34 (77%) | 10 (23%) | 0.54 | <0.0001 |
| Unable to visualize TM | 38 (86%) | 6 (14%) | NA | - |
| Tube extruding | 36 (82%) | 8 (18%) | 0.58 | <0.0001 |
| Tube blocked | 37 (84%) | 7 (16%) | 0.24 | 0.0077 |
| Tube extruded | 39 (89%) | 5 (11%) | 0.41 | <0.0001 |
| Acute OM with effusion | 44 (100%) | 0 (0%) | - | - |
| Middle ear effusion | 42 (95%) | 2 (4%) | NA | - |
| Ear drum retraction | 44 (100%) | 0 (0%) | NA | - |
| Ottorhea/drainage present | 43 (98%) | 1 (2%) | NA | - |
| Granulation tissue present | 44 (100%) | 0 (0%) | NA | - |
Calculated for variables with 4 or more disagreements, where possible
And finally, both study physicians completed acceptability questionnaires six months after the start of the study utilizing a 3-point Likert scale with 1- agree; 2- no opinion; 3- disagree options. Eight questions assessed their comfort making remote diagnoses and the time to review videos, among other related questions.
2.3. Statistical methods
Kappa statistics were utilized to evaluate the inter-rater agreement between two independent otolaryngologists of home scheduled videos as well as the intra-rater agreement between scheduled home video and in-office evaluation by the same otolaryngologist. A Cohen’s kappa value of 1.0 indicates perfect agreement and 0.0, complete disagreement, decreasing in size as the proportion of disagreements increase thereby sensitive to the actual proportions within the data. Cohen’s kappa was calculated for all variables showing four or more cases in which the raters disagreed. A high inter-rater reliability was assumed for any variable which had 3 or fewer cases in which the raters disagreed. Further descriptive statistics were utilized for unscheduled videos and questionnaires.
3. RESULTS
3.1. Participants
Twenty-one children were enrolled between January and June of 2016 from the Otolaryngology – Head and Neck Surgery Division of Children’s Hospital Los Angeles. Five subjects withdrew for the following reasons: incompatibility of their new iPhone version and the attachments (two); extenuating family circumstances that prevented them from taking regular videos (two); and technical difficulties uploading videos and asked to withdraw (one).
3.2. Descriptive data
The mean duration of follow up was 16 months (range 6–24 months), while the average duration of follow up after TT placement was 17 months (range 6–24 months, Table 3). There were 11 female and five male participants with a median age of 1.7 years (IQR 1.1 – 3.0 years, Table 3), and 15 of the 16 subjects were under four years of age (Figure 2). Two otolaryngologists reviewed a total of 206 monthly videos, while one otolaryngologist evaluated 44 prior to office visit videos and 25 unscheduled videos.
Table 3.
Agreement between two independent otolaryngologist raters of scheduled videos
| Variable | Number of videos on which both raters agree | Number of videos on which raters disagree | Cohen’s kappa | P-value |
|---|---|---|---|---|
| Cerumen | 126 (61%) | 80 (39%) | 0.31 | <0.0001 |
| Tube patent | 128 (62%) | 78 (38%) | 0.48 | <0.0001 |
| Tube in place | 164 (80%) | 42 (20%) | 0.65 | <0.0001 |
| Unable to visualize TM | 167 (81%) | 39 (19%) | 0.43 | <0.0001 |
| Tube extruding | 172 (83%) | 34 (16%) | 0.19 | <0.0001 |
| Tube blocked | 191 (93%) | 15 (7%) | 0.49 | <0.0001 |
| Tube extruded | 191 (93%) | 15 (7%) | 0.57 | <0.0001 |
| Acute OM with effusion | 206 (100%) | 0 (0%) | NA | - |
| Middle ear effusion | 205 (99.5%) | 1 (0.5%) | NA | - |
| Ear drum retraction | 203 (98%) | 3 (1%) | NA | - |
| Ottorhea/drainage present | 199 (97%) | 7 (3%) | 0.58 | <0.0001 |
| Granulation tissue present | 206 (100%) | 0 (0%) | NA | |
Calculated for variables with 4 or more disagreements, where possible
Figure 2.
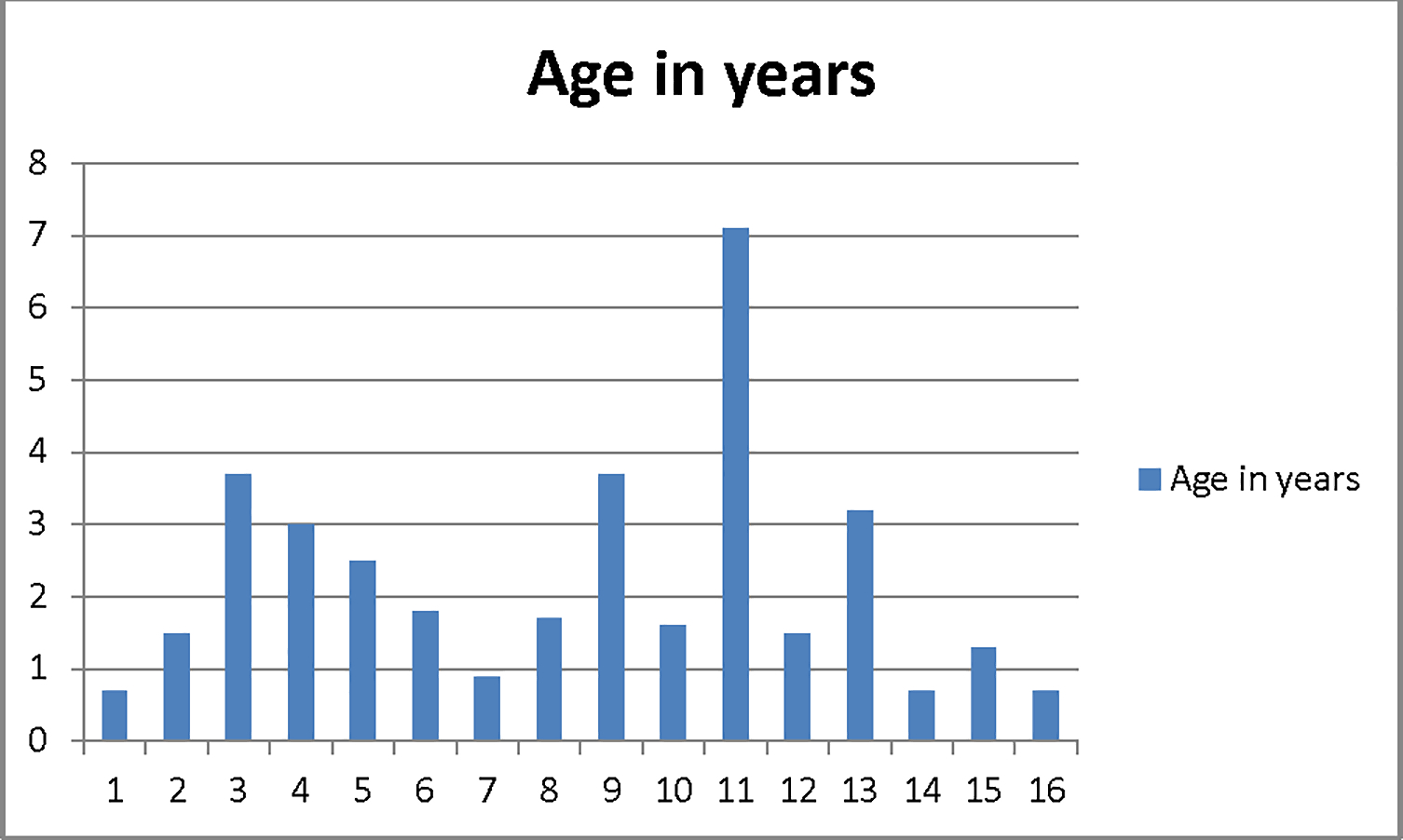
Distribution of subject ages in years
3.3. Main results
3.3.1. Intra-rater agreement
For intra-rater agreement, Cohen’s kappa could not be calculated for a few variables due to an abnormal distribution of data. Among the 44 videos taken preceding an office visit and compared to standard otoscopy, tube extruding, tube blocked and tube extruded had at least 80% agreement between the two evaluations and they were significant (p<0.05, Table 4). One video was of poor quality and in one subject the in-office exam revealed a blocked left tube not noted on the home video. The median time between video and in-office exam was 1 day (IQR 0–1day).
Table 4.
Parental Questionnaire for unscheduled visits
| Question | *N=16 |
|---|---|
| Did you use the remote diagnosis service in place of the following? (n, %) | |
| ER visit | 2 (12) |
| Urgent care | 8 (50) |
| After hours clinic visit | 1 (6) |
| Primary care provider | 10 (62) |
| Nurse visit | 4 (25) |
| None of the above | 0 |
| If the answer to the above question is yes, please estimate how much time (in hours) you saved by using the remote diagnosis service (average hours, range) |
4 (2–20) |
| How much money in co-pays or doctor’s fees did you save by using the remote diagnosis service? (average US$, range) |
40 (15–200) |
| How much money in transportation and/or parking did the remote diagnosis save you? (average US$, range) |
10 (0–100) |
| How much money in lost wages did the remote diagnosis save you? (average US$, range) |
77 (0–300) |
| Do you wish your current medical insurance would cover this service? (n, %) | |
| Yes | 15 (94) |
| No | 0 |
| No opinion | 1 (6) |
| If you had a choice to pay $60 for the CellScope remote diagnosis visit or to use alternative care provider (Doctor visit, urgent care, ER), which would you have chosen? | |
| I would have paid the $60 for a remote visit | 11 (69) |
| I would have chosen to go to the doctor’s office, Urgent care or ER | 3 (19) |
4 parents completed the questionnaire once, 6 parents completed the questionnaire twice
3.3.2. Inter-rater agreement
The two otolaryngologists exhibited a high degree of concordance for the appearance of the TT and tympanic membrane for all 206 videos. Tube in place, unable to visualize tympanic membrane, tube extruding, tube blocked, tube extruded and otorrhea present had at least 80% agreement between the two independent raters and they were all significant (p<0.0001, Table 5). The two independent raters agreed on only about 60% of videos whether the tube was patent yet this still constituted a significant level of agreement (p<0.0001, Table 5). The highest rate of disagreement occurred for the observation “cerumen” with nearly 40% of videos demonstrating a discrepancy (Cohen’s kappa = 0.31, p<0.001). All other variables showed near perfect agreement (Table 5).
Table 5.
Parental Use and Acceptability Questionnaire
| Question | Agree N=16 |
|
|---|---|---|
| I liked seeing inside of child’s ear | 16(100) | |
| The device is easy to use | 16(100) | |
| I would pay a copay for remote diagnosis using a picture taken with the device | 14(88) | |
| Seeing a picture helped with understanding my child’s treatment | 15(94) | |
| I have a desire to follow child’s ear images over time | 11(69) | |
| I was comfortable using smartphone otoscope device to take a picture | 16(100) | |
| I was comfortable sending provider a picture taken with smartphone otoscope device | 16(100) | |
| I prefer using a smartphone otoscope device at home to taking child to a provider | 12(75) | |
| I would recommend smartphone otoscope device to friends | 16(100) | |
| Amount willing to pay for smartphone otoscope device | 1(6) | > $10 |
| 4(25) | > $20 | |
| 8(50) | > $50 | |
| 2(13) | > $75 | |
| 1(6) | > $100 | |
| Overall, did you like using the smartphone otoscope? (Yes) | 16(100) | |
| Thought the device provided you any useful information about your child’s health? | 16 (100) | |
| Thought using the device had an impact on your child’s health? | 13(81) | |
| Thought using the device had a positive impact on your child’s medical care? | 16(100) | |
| While using this device, do you think your child had better than normal health | 13(81) | |
3.3.3. Unscheduled use and questionnaire
Seven of the 16 enrolled parents sent a total of 25 videos outside of the monthly videos required by the study. The main reasons for the unscheduled videos were either general illness (four cases) or ear specific symptoms such as ear drainage, otalgia or tugging on ears (seven cases). Of the seven cases of videos sent for ear-specific symptoms, four were advised to begin topical antibiotic therapy based on the videos and the remaining three had no visible problem with the ears and were advised watch waiting without treatment.
Of the parents who completed the unscheduled use questionnaire, 62% reported using the Oto in place of a visit to their primary care provider and estimated a time saving of at least four hours (Table 2). They also reported estimated financial savings in co-pays, transportation and lost wages by using the Oto and 69% preferred to use the Oto remotely in place of an Urgent care or Emergency Room visit (Table 2).
3.3.4. Acceptability questionnaires
All 16 parents completed the acceptability questionnaire at least once (Table 1). One hundred percent liked using the device overall and would recommend the device to friends. All parents agreed they were comfortable taking and sending videos with the device and were willing to pay a fee for using the device and 75% preferred using the device instead of taking the child for an office visit. All parents thought that the device provided useful information about their child’s health and that it had a positive impact on their medical care, with 81% reporting they thought their child had better than normal health care as a result of using the device. Parents commented that the device “gave them comfort” and that they liked the monthly monitoring and getting “quick answers”, particularly noting their satisfaction with having direct communication with their doctor.
Both study otolaryngologists completed the physician questionnaire and reported feeling comfortable making diagnoses using the Oto videos and reported that they would be comfortable monitoring TTs remotely. Both also reported taking about one to three minutes to make a diagnosis using the Oto and were interested in potentially reviewing patient images for compensation in the future.
3.3.5. Feasibility and technical issues
Overall there were very few technical issues related to the parents’ monthly use of the Oto. The majority of difficulties were related to uploading the videos to the web portal through the smartphone application. Six parents sent videos, but were unsuccessful in uploading them because of internet connectivity problems or use of unsupported text included in their accompanying comments. In each case, parents were able to later retake and resend videos successfully. Twice a parent reported that they were unable to take a video due to a lack of storage space on their phone. Of the 206 monthly videos, the tympanic membrane and/or TT could not be visualized due to poor video quality in 7 (3%) and cerumen partially or fully blocking in at least one ear in 38 (18%).
4. DISCUSSION
4.1. Synopsis of key findings
This appears to be the first prospective clinical trial to evaluate the use of the Cellscope® smartphone attachment (Oto) for surveillance of TTs in a home environment. We found it feasible for the Oto to accurately capture images of the tympanic membrane and TT. We demonstrated excellent agreement rates between in-office traditional otoscopy and the Oto video images and a very high degree of inter-rater agreement between two otolaryngologists. Over a prolonged follow-up period, we also discovered that the Oto could correctly diagnose TT conditions such as whether the tube was extruding, blocked or extruded.
4.2. Strengths of the study
One unique characteristic of our study is the use of smartphone technology and web portal that permits the images and comments to be sent electronically for immediate review by a physician. With the ability to attach comments related to a child’s symptoms to a video image, the Oto may likely improve the accuracy of diagnosis. This feature provided exceptional parental satisfaction with the majority of parents finding the Oto to be very helpful. They appreciated the capacity to see real-time images of their child’s ears and get immediate feedback. Most parents also thought that the Oto improved the quality of their child’s care. The Oto appeared to prevent unnecessary and costly emergency room, urgent care or office visits for at least a few of our patients. Because the Oto probably influenced diagnosis in these cases, needless oral or topical antibiotic usage may have been avoided for these children. Furthermore, identification of TT otorrhea in a few children may have allowed for early treatment with prevention of complications, such as tube blockage or granulation tissue formation.
Also of importance, the otolaryngologists involved in this study were comfortable monitoring TTs using the Oto images and platform. Both physicians had no difficulties reviewing the videos nor did they find this process to be overly time consuming. However, real world utilization of the Oto for TT surveillance will need to make allowance for an otolaryngologist’s compensation. Thus far in other medical fields, because it has been shown to decrease healthcare costs, the review of digital video images has resulted in reimbursement from major payers5,6. A similar paradigm might be considered in the future in which use of the Oto is compensated and incorporated into a busy otolaryngology practice, potentially improving physician access and preventing unnecessary office visits.
One limitation in this study is that because our objective was directed towards the surveillance of TTs, definitive conclusions about the ability of the Oto to diagnose acute otitis media or other middle ear or tympanic membrane pathologies in the home environment cannot be made. Logically, examination of the tympanic membrane with the TT in place is a much simpler task than the nuanced diagnosis of acute otitis media in a young child. Therefore, further studies are needed to evaluate the efficacy of the Oto to diagnose acute otitis media via home parental use. We also acknowledge that a shortcoming of the study was our patient sample. Because all parents were English-speaking and required a compatible iPhone, the socioeconomic characteristics of our families may make it difficult to extend and generalize these results to all populations. Lastly, our small sample size also precluded our ability to conduct any cost-benefit analyses.
4.3. Comparisons with other studies
Previous studies documented the diagnostic precision of the Oto in comparison to traditional otoscopy in the emergency room setting7,8. Other studies investigated the capability of Oto and other types of video-otoscopy to provide tympanic membrane images for remote telemedicine purposes9–13. Only one study, however, used video-otoscopy to assess TT status remotely and compared this with conventional otomicroscopy9. The accuracy of the Oto noted in our investigation appears to be in concordance with these prior studies. However, aside from its diagnostic efficiency, our study differs from others primarily because parents used the Oto in a home environment. The majority of preceding studies investigated the use of Oto by trained health care professionals. Only one prior study investigated parental in-office use after a brief tutorial14. The results of these authors demonstrated a low agreement between parental acquired images and those captured by a physician when both were compared to standard pneumatic otoscopy performed by an otolaryngologist. In contrast, our findings document the feasibility for parents to capture images at home that are fairly comparable to conventional otoscopy in the office setting. This discrepancy may be due to the possibility that with repeated use and practice in the home setting, parents can capture images with improved quality. In addition, image capture with the TT as the primary visualized target may have made use of the Oto easier for parents.
4.4. Clinical applicability of the study
In summary, the Oto is feasible to use for TT surveillance. The Oto can allow otolaryngologists to monitor a child’s TT remotely over time. As medicine shifts towards a greater emphasis on patient centered care and we are forced to increasingly rely on telemedicine, the Oto’s utilization of smartphone technology can encourage patient autonomy, improve patient-physician communication and increase patient satisfaction. Subsequent mechanisms to allow for physician reimbursement and research strategies to evaluate the real world clinical, economic and societal impact of the Oto will ultimately be needed.
FUNDING/CONFLICT of INTEREST
This study was completed without external financial support. However, CellScope, Inc. provided the study team with the devices (US value $299). All investigators have declared no conflict of interests. CellScope, Inc. had no involvement in study design, data collection, data analysis or manuscript preparation.
References
- 1.Van Dongen TMA, van der Heijden GJMG, Venekamp RP, Rovers MM, Schilder AGM. A Trial of Treatment for Acute Otorrhea in Children with Tympanostomy Tubes. N Engl J Med. 2014;370(8):723–733. doi: 10.1056/NEJMoa1301630 [DOI] [PubMed] [Google Scholar]
- 2.Isaacson G, Rosenfeld RM. CARE OF THE CHILD WITH TYMPANOSTOMY TUBES. Pediatr Clin North Am. 1996;43(6):1183–1193. doi: 10.1016/S0031-3955(05)70513-7 [DOI] [PubMed] [Google Scholar]
- 3.Spielmann PM, McKee H, Adamson RM, Thiel G, Schenk D, Hussain SSM. Follow up after middle-ear ventilation tube insertion: what is needed and when? J Laryngol Otol. 2008;122(06):580–583. doi: 10.1017/S0022215107001168 [DOI] [PubMed] [Google Scholar]
- 4.Derkay CS, Carron JD, Wiatrak BJ, Choi SS, Jones JE. Postsurgical follow-up of children with tympanostomy tubes: results of the American Academy of Otolaryngology-Head and Neck Surgery Pediatric Otolaryngology Committee National Survey. Otolaryngol--Head Neck Surg Off J Am Acad Otolaryngol-Head Neck Surg. 2000;122(3):313–318. [DOI] [PubMed] [Google Scholar]
- 5.Datta SK, Warshaw EM, Edison KE, et al. Cost and Utility Analysis of a Store-and-Forward Teledermatology Referral System: A Randomized Clinical Trial. JAMA Dermatol. 2015;151(12):1323–1329. doi: 10.1001/jamadermatol.2015.2362 [DOI] [PubMed] [Google Scholar]
- 6.Armstrong AW, Wu J, Kovarik CL, et al. State of teledermatology programs in the United States. J Am Acad Dermatol. 2012;67(5):939–944. doi: 10.1016/j.jaad.2012.02.019 [DOI] [PubMed] [Google Scholar]
- 7.Richards JR, Gaylor KA, Pilgrim AJ. Comparison of traditional otoscope to iPhone otoscope in the pediatric ED. Am J Emerg Med. 2015;33(8):1089–1092. doi: 10.1016/j.ajem.2015.04.063 [DOI] [PubMed] [Google Scholar]
- 8.Mousseau S, Lapointe A, Gravel J. Diagnosing acute otitis media using a smartphone otoscope; a randomized controlled trial. Am J Emerg Med. 2018;36(10):1796–1801. doi: 10.1016/j.ajem.2018.01.093 [DOI] [PubMed] [Google Scholar]
- 9.Kokesh J, Ferguson AS, Patricoski C, et al. Digital images for postsurgical follow-up of tympanostomy tubes in remote Alaska. Otolaryngol -- Head Neck Surg. 2008;139(1):87–93. doi: 10.1016/j.otohns.2008.04.008 [DOI] [PubMed] [Google Scholar]
- 10.Patricoski C, Kokesh J, Ferguson AS, et al. A Comparison of In-Person Examination and Video Otoscope Imaging for Tympanostomy Tube Follow-Up. Telemed J E Health. 2003;9(4):331–344. doi: 10.1089/153056203772744653 [DOI] [PubMed] [Google Scholar]
- 11.Eikelboom RH, Mbao MN, Coates HL, Atlas MD, Gallop MA. Validation of tele-otology to diagnose ear disease in children. Int J Pediatr Otorhinolaryngol. 2005;69(6):739–744. doi: 10.1016/j.ijporl.2004.12.008 [DOI] [PubMed] [Google Scholar]
- 12.Biagio L, Swanepoel DW, Laurent C, Lundberg T. Video-otoscopy recordings for diagnosis of childhood ear disease using telehealth at primary health care level. J Telemed Telecare. 2014;20(6):300–306. doi: 10.1177/1357633X14541038 [DOI] [PubMed] [Google Scholar]
- 13.Moshtaghi O, Sahyouni R, Haidar YM, et al. Smartphone-Enabled Otoscopy in Neurotology/Otology. Otolaryngol Neck Surg. 2017;156(3):554–558. doi: 10.1177/0194599816687740 [DOI] [PubMed] [Google Scholar]
- 14.Shah MU, Sohal M, Valdez TA, Grindle CR. iPhone otoscopes: Currently available, but reliable for tele-otoscopy in the hands of parents? Int J Pediatr Otorhinolaryngol. 2018;106:59–63. doi: 10.1016/j.ijporl.2018.01.003 [DOI] [PubMed] [Google Scholar]


